Abstract
Dry eye disease has been recognized to be a global public health problem, as it has many consequences starting from daily life activities restrictions to economical costs of management. At present, there is a lack of knowledge regarding the most important risk factors for eye dryness. This problem is becoming important worldwide especially with the increase use of technology, smartphones, computers, and contact lenses. The aim of this systematic review is to determine the most relevant factors associated with dry eye symptoms to help in its early recognition, prevention and reduce its subsequent implications. PRIMSA 2009 checklist was used to conduct this systematic review. The inclusion and exclusion criteria were implemented first. Then, PubMed Database was explored for articles. The data extraction was based on three categories: Sociodemographic, diseases, and medications in the form of odds ratios. Predictive values, confidence intervals, and prevalence were recorded when the data were sufficient. This systematic review included 6 Articles and 48 evaluated variables. Female gender, contact lenses, use of computers, thyroid abnormalities, hypertension, antidepressant, and antihistamine were identified to be the strongest and the most common risk factors for dry eye syndrome.
Keywords: Dry eye, Risk factors, review, ophthalmology
INTRODUCTION
Dry eye disease is one of the most prevalent diagnoses in ophthalmology clinics. Recently, it has been recognized as a global public health problem.[1,2] The United States epidemiological studies identified the condition in 5%–30% of the population[1,2] which makes it more prevalent than diabetes (10.5% of US population),[3] heart diseases (7% of US population),[4] and cancer (3% of US population).[5] It is a multifactorial disease of the preocular tear film with possible damage to the ocular surface.[6] Dry eye symptoms range from simple transient irritation to persistent discomfort, fatigue, visual disturbance, and tear film instability.[6] As well as that, it has been found that severe eye symptoms were associated with difficulties in social, physical, and mental functioning.[7] Several socio-economic implications might result from dry eye symptoms such as increased health care costs and decrease in quality of life measures such as driving, watching television, using mobile phones, reading, computer work, and emotional well-being.[8] Dry eye Management in US has been estimated to cost US$700000 per million patients. Moreover, the total annual cost reported to range from US$270000 in France to US$1.10 million in the United Kingdom per 1000 patients.[9,10]
In the 21st century, much environmental behavior developed including smoking and technology spread such as smartphones and computers. Furthermore, the average human lifespan increased, and thus chronic diseases and medications intake expanded. These factors might have attributed to the rise in dry eye syndrome (DES) percentage worldwide.
Therefore, early recognition and prevention are important to reduce the consequences burden of DES. For instance, primary prevention through education and elimination of the risk factors can ameliorate the symptoms.[11] Thus, it can reduce unnecessary emotional, psychological, and functional issues.
The main aim of this systematic review is to identify the frequently reported risk factors that contribute to the development of DES and to recognize the strongest and the most common factors among all. Identifying the risk factors might help in the prevention and detection of DES.
Searching databases revealed very few systematic reviews around the same topic. Some of them focused on one risk factor only. Other systematic reviews focused on females risk factors. Nevertheless, none has tackled dry eye disease risk factors in both genders and different countries. In addition, there is a lack of knowledge about this topic among physicians, patients, and the whole community.
Search strategy and selection criteria
This systematic review articles were found through an electronic based search. PubMed database was explored. At First, two subsets of citations were applied “risk factors of DES” and “Dry eye risk factors”. Then, they were combined together and the search was narrowed to articles published in the last 10 years and in English language. Further filtrations Humans species. The remaining articles were screened by titles and abstracts. Also, I E-mailed the authors of one article through research gate to read the full text. Later, the identified articles were assessed for their suitability with the inclusion and exclusion criteria. As well as that, some articles reference list was examined to check for related articles. In addition, in this systematic review PRIMSA 2009 checklist was used.[12]
Inclusion and exclusion criteria
Published observational studies.(cohort, case-control and cross sectional)
Studies published in the past 10 years
English articles
Studies tested risk factors of
Sample size: Any.
Animal studies were excluded from this systematic review and also studies that measured the risk factors in certain occupation environment. Also, Same study group articles were excluded.
Quality assessment
The studies that were used were assessed for their quality using Newcastle Ottawa quality scale.[13] We considered a study to be of a good quality if it contained the description of the population and scored 6 out of 9 points or 5 out of 8.
Data extraction
Several Data were selected from the articles. First of all, the characteristics of each study including the country, publishing date, the title and the authors were taken from the front page and the introduction of each study. The demographic features of the study population was selected from the methodology of all articles and compared to each other. Also, the risk factors with the P values, odds ratio (OR) and confidence interval (CI) were extracted from the results and then they were categorised into (1) sociodemographic factors (2) chronic diseases and (3) medications. The heterogeneity of this systematic review might be due to different patient's backgrounds, diverse study countries and different methodologies. Also, it might be explained by the use of different questionnaires and the diversity of risk factors including occupation, age and smoking. The data were taken from graphs, tables, and forest plots or after reading the full text several times.
Data analysis
ORs were compared after identifying the most significant risk factors. Also, tables and bar graphs were used. As well as that, carefully chosen data were analysed by Comprehensive-Meta-Analysis-v3. Data included OR in which they were presented in a forest plot that present the most significant risk factors for developing DES. P values, CIs and prevalence were recorded when sufficient data was available.
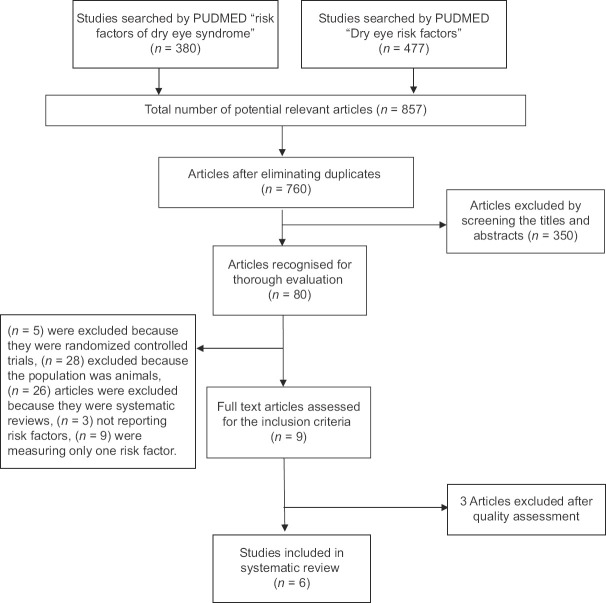
Search strategy [Figure 1]
Figure 1.
Systematic review search strategy flow chart
The literature search yielded 857 studies [Figure 1]. However, 9 studies met the inclusion criteria and were further assessed for their quality. At the end, 6 articles were chosen to be included in the systematic review by two reviewers after discussion with a third reviewer.
Quality assessment
The articles were assessed for their quality using the Newcastle Ottawa quality score.
Evaluation of cohort and cross sectional studies [Table 1]
Table 1.
Evaluation of cohort and cross sectional studies
| Study | Score | Included/excluded | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Selection | Comparability | Outcome | Total number of points | ||||||||
|
|
|
|
|||||||||
| Representation of exposed patients (number points) | Selection of unexposed patients (number points) | Ascertainment of exposure (number points) | Outcome was not present at start (number points) | Symptoms are controlled (number of point) | Therapy of patients controlled (number of points) | Assessment of outcome (number points) | Follow up long enough for outcome to occur (number points) | Adequacy of follow up of cohorts (number points) | |||
| Adam J.paulsen et al., 2014[16] | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 7/9 | Included |
| Uchino et al., 2008[15] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | NA | 4/8 | Excluded |
| Li Li tan et al., 2014[17] | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 6/8 | Included | |
| Ji Min Ahn et al., 2014[20] | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 5/8 | Included | |
| Zhang et al., 2012[18] | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 4/8 | Excluded | |
| Li et al., 2015[19] | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 4/8 | Excluded | |
| Eloy Viso et al., 2009[21] | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 6/8 | Included | |
| Miki Uchino et al., 2011[22] | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 7/8 | Included | |
NA: Not applicable
Evaluation of case control studies [Table 2]
Table 2.
Evaluation of case control studies
| Study | Score | Included/excluded | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Selection | Comparability | Exposure | Total number of points | |||||||
|
|
|
|
||||||||
| Is the case definition adequate? | Representativeness of the cases | Selection of controls | Definition of controls | Comparability of cases and controls on the basis of the design or analysis | Ascertainment of exposure | Same method of ascertainment for cases and controls | Nonresponse rate | |||
| Anat Galor et al., 2011[14] | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 6/8 | Included |
Study characteristics [Table 3]
Table 3.
Studies characteristics
| Study country | Study type | Population size | Population age | Test used | |
|---|---|---|---|---|---|
| Anat Galor et al., 2011 | US | Case control | 16,862 patients (2056 cases) (14806 controls) | Not limited | ICD9 code |
| Adam J.paulsen et al., 2014 | US | Cohort | 3285 | 21-84 years | Questionnaire |
| Li Li tan et al., 2014 | Singapore | Cross sectional | 1004 | 15-83 years | McMonnie dry eye questionnaire |
| Ji Min Ahn et al., 2014 | Korea | Cross sectional | 11,666 | 19-95 | Survey and full ocular examination |
| Eloy Viso et al., 2009 | Spain | Cross sectional | 654 | +40 | Questionnaire, Schimer test, fluorescein |
| Miki Uchino et al., 2011 | Japan | Cross sectional | 3294 | +40 | Questionnaire |
Six studies were involved in this systematic review reporting on 36765 patients. One study was cohort, one study was case control and 4 studies were cross sectional studies. All the studies population included patients with dry eye symptoms. The sample size range was 654–168,62. Age was reported in all studies as a range except two studies (Eloy Viso et al.) and (Miki Uchino et al.) in which it was + 40. Participants from the largest population studied were 21-84 years old. Also, gender was mentioned and assessed in all of the studies with females being predominant. Moreover, most of the studies used a questionnaire but one study (Anat Galor et al.) used ICD9 code for the assessment of dry eye symptoms. 2 studies were established in US, 1 in Singapore, 1 in Korea, 1 in Spain and 1 in Japan. Different study country among the articles might have led to the heterogeneity in this systematic review.
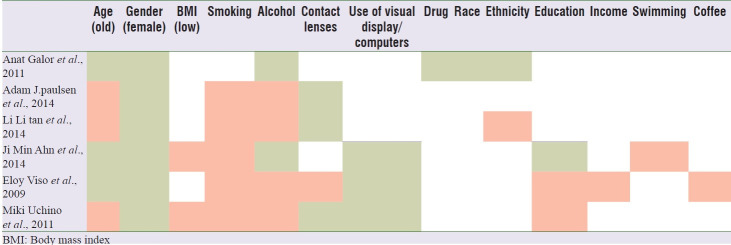
Sociodemographic factors [Table 4] [Figure 2]
Table 4.
Demonstration of the sociodemographic variables in every study
Figure 2.
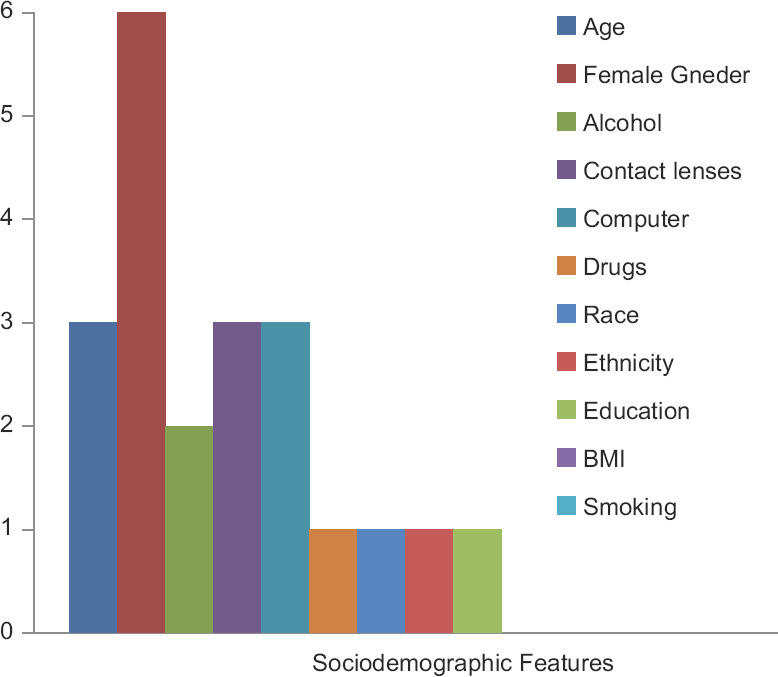
Illustration of sociodemographic features as risk factors in the studies (X axis: risk factors- Y axis: Number of studies they were significant in)
Age, gender and alcohol were tested in all of the included studies for their association with the development of dry eye disease. Female gender was a significant risk factor in all of the studies with prevalence range from 11.9% to 22%. As for alcohol, it was only significant in 2 studies Anat Galor et al. (OR 1.5, 95% CI 1.1–2.1 P < 0.01) and Ji Min Ahn et al. (OR 0.76, 95% CI 0.44–1.31 P = 0.001). The significance of age among the studies was of 3:3 which might be due to the difference in the populations studied. All the six studies that measured smoking showed no significant relation to DES prevalence. Statistical significance of contact lenses and the use of computers were proved in 3 studies. Current and past Contact lens use found to be related with dry eye symptoms in comparison with those who had never use them in Adam J. Paulsen et al. study, OR = 2.14 (95% CI = 1.65,2.77) and OR = 1.34 (95% CI = 1.05,1.71) respectively. However, one study Eloy Viso et al. showed no association between contact lens use and DES when examined by Schirmer ≤5 test OR = 0.69 (95%CI = 0.17–2.84) and TBUT ≤10 OR = 0.33 (95%CI = 0.04–2.60). Visual display terminal and the use of computers were correlated with Dry eye symptoms and the correlation is directly proportional to the using duration as it increased significantly after 2 h in females OR = 2.33 (95% CI = 1.12–4.85) and after 4 h in males OR = 1.1 (95%CI = 0.54–2.24) in Miki Uchino et al., 2011.
Anat Galor et al. studied drug dependence and race as risk factors for DES and the results revealed important link for drugs with n = 651/2056, 13% prevalence OR = 1.28 P = 0.0001. Although, race information was available for only 30% of patients, black patients had increased prevalence over white (20% vs. 18%, OR = 1.42, 95% CI 1.21–1.66). Same study with the limitation of ethnicity details showed increase prevalence among Hispanic 21%, P = 0.032. Nevertheless, Li Li Tan et al. study appeared no bond between the different type of ethnicity that was included in it and dry eye symptoms P = 0.667. High education level was not a significant risk factor in 2 out of 3 studies but it was an essential risk factor in Ji Min Ahn et al. study, OR = 1.5 (95% CI = 1.1–2) P = 0.02. Income, coffee, and swimming were not significant and each was only assessed in one study. Low income was associated with only 14% and coffee OR = 1 P = 0.95 in Ji Min Ahn et al. On the other hand, swimming in Li Li Tan et al. had a prevalence of 13.6% and a total number of 21 P = 0.487, CI = (8.6–20.0).
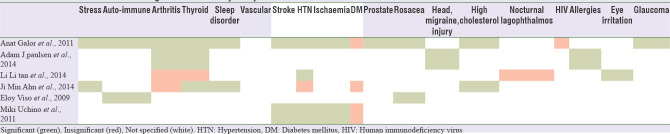
Diseases [Table 5] [Figure 3]
Table 5.
Demonstration of diseases significance in every study
Figure 3.
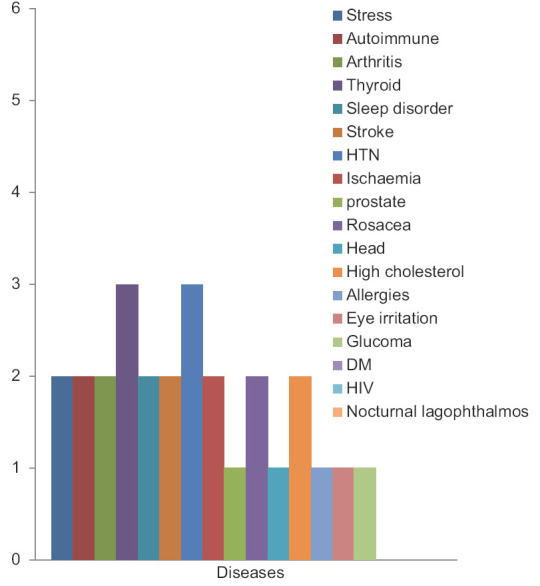
Illustration of Diseases as risk factors in the studies (X axis: risk factors- Y axis: Number of studies they were significant in)
Each study assessed the risk ratio of variable diseases. Most frequently evaluated diseases were arthritis, thyroid, hypertension and diabetes mellitus. Among these 4 diseases, thyroid disorders and hypertension showed significant impact on DES manifestation. Thyroid abnormalities variable was insignificant in only one out of four studies (Li Li tan et al.) with a percentage of 5.9% P = 0.498 (95% CI 0.7–19.7).Three studies established the association between hypertension and dry eye symptoms. However, Ji Min Ahn et al. study found no link OR = 0.8 P < 0.01.In regard to diabetes, it is unrelated to dry eye symptoms based on the agreement of the three studies that included the measurement of its OR. Two studies revealed a link between arthritis and DES, while two other studies showed no significant influence.
The insignificantly of HIV and Nocturnal lagophthalmos was recognized in one study for each. HIV appeared to have an odd ratio = 0.003 in Anat Galor et al. study. In Li Li tan et al., nocturnal lagophthalmos was inconsequential with prevalence of 17.7% and P = 0.443.
All the other diseases were found to be linked to dry eye symptoms in the studies that measured their OR s or prevalence.
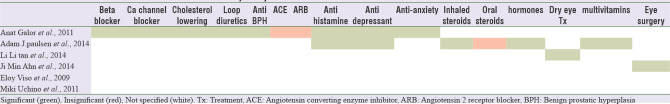
Medications [Table 6 and Figure 4]
Table 6.
Demonstration of medications association in every study
Figure 4.
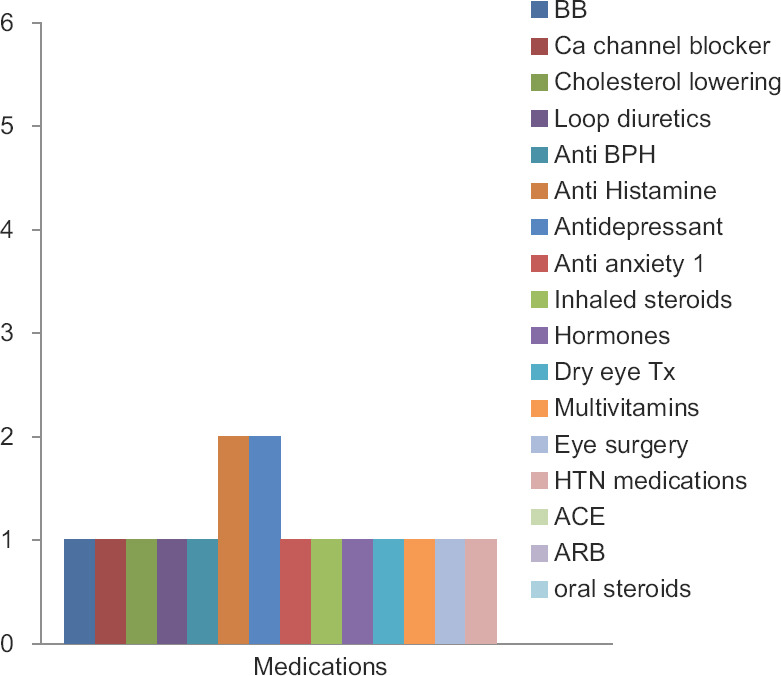
Illustration of medications as risk factors in the studies (X axis: risk factors- Y axis: Number of studies they were significant in)
Medications were evaluated comprehensively in Only 2 studies, Anat Galor et al. and Adam J. paulsen et al. However, only two types of medications were assessed in both of the studies, antihistamines and antidepressant. Anat Galor et al. study results were substantial in respect to both antihistamines and antidepressant, (prevalance22%, OR = 2.53 (95%CI 2.28–2.80), P < 0.0001) and (prevalence 17% OR = 1.97 (95%CI 1.79–2.17) P < 0.0001) correspondingly. In Adam J. Paulsen et al. study, Antihistamine use was related to DES (OR, 1.54; 95% CI, 1.18–2.02) and also antidepressant (OR = 1.68; 95%CI, 1.15, 2.45). Moreover, Anat Galor et al. study identified the significant of anti-anxiety beta blockers, Ca channel blockers, loop diuretics and cholesterol lowering as risk factors. The association of steroids use with dry eye symptoms was studied in Adam J. Paulsen et al. It was only significant with inhaled steroids, OR = 2.04 (95% CI = 1.24, 3.33). as oral steroids did not exhibit a statistically significantly association, OR = 1.47 (95% CI = 0.63, 3.42). In the same study, hormones and multivitamins use was also significant. Hypertension medications and previous eye treatment were correlated to dry eye symptoms in Li Li Tan et al., 2014. History of eye surgery linkage with DES was proved in Ji Min Ahn et al., 2014 (OR = 2.2).
DISCUSSION
Sociodemographic, Environmental and medical factors play an important role on the development of dry eye symptoms which has a huge impact on the patient's daily life.
This systematic review examined the correlation between several risk factors and dry eye disease, aiming to produce a predictive model in order to prevent and early recognise DES to reduce its subsequent complications. Six articles met the occlusion criteria and they were evaluated. The ORs of 48 variables were recognised, 7 were accredited as the commonest risk factors: Female gender, contact lenses, use of computers, thyroid abnormalities, hypertension, antidepressants and antihistamines. The predominant risk factors were in the sociodemographic category. Other risk factors evidences were inadequate to come up with a certain association.
Environmental factors such as pollution, climate and humidity levels were absent in all of the studies included in this systematic review. However, they have been reported in other studies.[23,24] As well as that, other factors that have been proved to have a correlation with DES like omega3, connective tissue diseases, radiation therapy and vitamin A deficiency were not assessed.[25,26]
Female gender appeared to be the most effective risk factor and this is supported by many studies.[1,27,28] The high prevalent of DES among Females may be related to the hormonal effects[29] in which sex hormones especially androgens affect the lacrimal glands, Meibomian glands, conjunctival goblet cell density and ocular surface sensitivity.[28,30] However, two studies Schein et al.[31] and Lin et al.[32] did not find any link between gender and DES but their research was restricted to elderly when androgen levels are low in both genders. Although age was significant in 3 studies only, many previous studies reported its implication[27,33] as with aging lacrimal gland function reduces and thus increase in dry eye symptoms.[22,23] On the other hand, similar prevalence among young people compared to elderly might be associated with use of contact lenses, increasing computer and smart phones use and refractive surgeries which all have been linked to DES in many researches. Also, older age population systemic diseases and ocular sensitivity decline may have them underestimate eye dryness.[22] This systematic review findings were consistent with other studies regarding contact lenses and computer use importance.[34,35] One study conducted in Australia showed no association between contact lenses and DES.[33] Despite that Smoking and alcohol were not significant risk factors in most of the researches conducted;[33] some studies reported their significance.[36]
In the diseases category, thyroid abnormalities and hypertension appeared to be risk factors of dry eye symptoms. Several factors considered in dry eye in thyroid disease: Exophthalmos, lagophthalmous and increased palpebral fissure[37] and this correlation have been established in.[28] However, there is ambiguity in the relation of thyroid and DES in literature.[38] Regarding Hypertension, those who were found to be treated for hypertension are more prone to develop dry eye symptoms. Despite that only one study included in this review proved the significant between hypertension medications and DES, it has been reported in physician's health study.[27] Diabetes mellitus was not found to be a risk factor in this systematic review which might be explained by the results of a recent study in which it disclosed that 65.3% of diabetics have peripheral neuropathy and mild to severe corneal sensitivity reduction,[39] that might made them underevaluate their dry eye symptoms. Nevertheless, stress and arthritis was not proved as strong risk factors in this review, many studies demonstrated their strong correlation to dry eye symptoms.[1,8,28,33]
Anti-depressant and anti-histamine were the strongest indicators for DES symptoms in the medications category. Anti-depressant presented to increase DES risk and it is supported by other studies.[40,41] Human conjunctival epithelium contains both muscarinic and adrenergic receptors so there is biologic believability that anti-depression medications affect ocular surface. Likewise, antihistamines and steroids found to be associated with dry eye and many studies established such results.[36,41]
The limitations of this systematic review included missing of other factors like specific medications and specific diseases, menopause relation, contact lenses using hours, climate and humidity were not involved in the analysis as the data was insufficient. Furthermore, the articles included used different types of questionnaires that might also lead to heterogeneity. As well as that, different population characteristics among the studies contributed to the heterogeneity. Moreover, the severity and progression of dry eye in regards to the risk factors were not taken into consideration. In addition, the differences between symptomatic and diagnostic dry eye were not taken into account.
CONCLUSION
To sum up, Female gender, contact lenses, use of computers, thyroid abnormalities, hypertension, antidepressant and antihistamine were identified to be the strongest and commonest risk factors for DES.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
RCSI-MUB has guided me to write this systematic review.
REFERENCES
- 1.Smith JA, Albeitz J, Begley C, Caffery B, Nichols K, Schaumberg D, et al. The epidemiology of dry eye disease: Report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5:93–107. doi: 10.1016/s1542-0124(12)70082-4. [DOI] [PubMed] [Google Scholar]
- 2.Brewitt H, Sistani F. Dry eye disease: The scale of the problem. Surv Ophthalmol. 2001;45(Suppl 2):S199–202. doi: 10.1016/s0039-6257(00)00202-2. [DOI] [PubMed] [Google Scholar]
- 3.National Diabetes Statistics. 2011. Available from: https://www.cdc. gov/diabetes/data/statistics-report/index.html .
- 4.Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, et al. Bethesda, MD: SEER Cancer Statistics Review, 1975-2005, National Cancer Institute. https://seer.cancer.gov/ csr/1975_2005/ based on November 2007 SEER data submission, posted to the SEER web site, 2008. [Google Scholar]
- 5.JR Neyer, KJ Greenlund, CH Denny, NL Keenan, DR Labarthe, JB Croft. Div for Heart Disease and Stroke Prevention, National Center for Chronic Disease Prevention and Health Promotion, CDC. Prevalence of heart disease – United States. 2005. Available from: https://www.cdc. gov/mmwr/preview/mmwrhtml/mm5606a2.htm .
- 6.Lemp MA, Baudouin C, Baum J, Dogru M, Foulks GN, Kinoshita S, et al. The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5:75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 7.Rajagopalan K, Abetz L, Mertzanis P, Espindle D, Begley C, Chalmers R, et al. Comparing the discriminative validity of two generic and one disease-specific health-related quality of life measures in a sample of patients with dry eye. Value Health. 2005;8:168–74. doi: 10.1111/j.1524-4733.2005.03074.x. [DOI] [PubMed] [Google Scholar]
- 8.Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143:409–15. doi: 10.1016/j.ajo.2006.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muñoz B, West SK, Rubin GS. Causes of blindness and visual impairment in a population of older Americans: The Salisbury Eye Evaluation Study. Arch Ophthalmol. 2000;118:1264–8. doi: 10.1001/archopht.118.6.819. [DOI] [PubMed] [Google Scholar]
- 10.Clegg JP, Guest JF, Lehman A, Smith AF. The annual cost of dry eye syndrome in France, Germany, Italy, Spain, Sweden and the United Kingdom among patients managed by ophthalmologists. Ophthalmic Epidemiol. 2006;13:263–74. doi: 10.1080/09286580600801044. [DOI] [PubMed] [Google Scholar]
- 11.Pflugfelder SC, Geerling G, Kinoshita S, Lemp MA, McCulley J, Nelson D, et al. Management and therapy of dry eye disease: Report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5:163–78. doi: 10.1016/s1542-0124(12)70085-x. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wells GA, Shea B, O'connell D, Peterson J, Welch V, Losos M, et al. Ottawa Hospital Research Institute. 2014. Available from: http://www. ohri.ca/programs/clinical_epidemiology/oxford.asp .
- 14.Galor A, Feuer W, Lee DJ, Florez H, Carter D, Pouyeh B, et al. Prevalence and risk factors of dry eye syndrome in a united states veterans affairs population. Am J Ophthalmol. 2011;152:377–84. doi: 10.1016/j.ajo.2011.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uchino M, Schaumberg DA, Dogru M, Uchino Y, Fukagawa K, Shimmura S, et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology. 2008;115:1982–8. doi: 10.1016/j.ophtha.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 16.Paulsen AJ, Cruickshanks KJ, Fischer ME, Huang GH, Klein BE, Klein R, et al. Dry eye in the beaver dam offspring study: Prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157:799–806. doi: 10.1016/j.ajo.2013.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tan LL, Morgan P, Cai ZQ, Straughan RA. Prevalence of and risk factors for symptomatic dry eye disease in Singapore. Clin Exp Optom. 2014;98:45–53. doi: 10.1111/cxo.12210. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Chen H, Wu X. Prevalence and risk factors associated with dry eye syndrome among senior high school students in a county of Shandong Province, China. Ophthalmic Epidemiol. 2012;19:226–30. doi: 10.3109/09286586.2012.670742. [DOI] [PubMed] [Google Scholar]
- 19.Li J, Zheng K, Deng Z, Zheng J, Ma H, Sun L, et al. Prevalence and risk factors of dry eye disease among a hospital-based population in southeast China. Eye Contact Lens. 2015;41:44–50. doi: 10.1097/ICL.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 20.Ahn JM, Lee SH, Rim TH, Park RJ, Yang HS, Kim TI, et al. Prevalence of and risk factors associated with dry eye: The Korea National Health and Nutrition Examination Survey 2010–2011. Am J Ophthalmol. 2014;158:1205–14.e7. doi: 10.1016/j.ajo.2014.08.021. [DOI] [PubMed] [Google Scholar]
- 21.Viso E, Rodriguez-Ares MT, Gude F. Prevalence of and associated factors for dry eye in a Spanish adult population (the Salnes Eye Study) Ophthalmic Epidemiol. 2009;16:15–21. doi: 10.1080/09286580802228509. [DOI] [PubMed] [Google Scholar]
- 22.Uchino M, Nishiwaki Y, Michikawa T, Shirakawa K, Kuwahara E, Yamada M, et al. Prevalence and risk factors of dry eye disease in Japan: Koumi study. Ophthalmology. 2011;118:2361–7. doi: 10.1016/j.ophtha.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 23.Lekhanont K, Rojanaporn D, Chuck RS, Vongthongsri A. Prevalence of dry eye in Bangkok, Thailand. Cornea. 2006;25:1162–7. doi: 10.1097/01.ico.0000244875.92879.1a. [DOI] [PubMed] [Google Scholar]
- 24.Saxena R, Srivastava S, Trivedi D, Anand E, Joshi S, Gupta SK. Impact of environmental pollution on the eye. Acta Ophthalmol Scand. 2003;81:491–4. doi: 10.1034/j.1600-0420.2003.00119.x. [DOI] [PubMed] [Google Scholar]
- 25.Sommer A. Vitamin A deficiency and the global response. Forum Nutr. 2003;56:33–5. [PubMed] [Google Scholar]
- 26.Pal R, Sagar V. Antecedent risk factors of xerophthalmia among Indian rural preschool children. Eye Contact Lens. 2008;34:106–8. doi: 10.1097/ICL.0b013e3181379fd7. [DOI] [PubMed] [Google Scholar]
- 27.Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–26. doi: 10.1016/s0002-9394(03)00218-6. [DOI] [PubMed] [Google Scholar]
- 28.Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264–8. doi: 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- 29.Schaumberg DA, Sullivan D, Buring JE, Dana MR. Hormone replacement therapy (HRT) and the prevalence of dry eye symptoms. Invest Ophthalmol Vis Sci. 2000;41:3939. [Google Scholar]
- 30.Sullivan DA, Sullivan BD, Evans JE, Schirra F, Yamagami H, Liu M, et al. Androgen deficiency, Meibomian gland dysfunction, and evaporative dry eye. Ann N Y Acad Sci. 2002;966:211–22. doi: 10.1111/j.1749-6632.2002.tb04217.x. [DOI] [PubMed] [Google Scholar]
- 31.Schein OD, Mu~noz B, Tielsch JM, Bandeen-Roche K, West S. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997;124:723–8. doi: 10.1016/s0002-9394(14)71688-5. [DOI] [PubMed] [Google Scholar]
- 32.Lin PY, Tsai SY, Cheng CY, Liu JH, Chou P, Hsu WM. Prevalence of dry eye among an elderly Chinese population in Taiwan: The Shihpai Eye Study. Ophthalmology. 2003;110:1096–101. doi: 10.1016/S0161-6420(03)00262-8. [DOI] [PubMed] [Google Scholar]
- 33.McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology. 1998;105:1114–9. doi: 10.1016/S0161-6420(98)96016-X. [DOI] [PubMed] [Google Scholar]
- 34.Brennan NA, Efron N. Symptomatology of HEMA contact lens wear. Optom Vis Sci. 1989;66:834–8. doi: 10.1097/00006324-198912000-00006. [DOI] [PubMed] [Google Scholar]
- 35.McMonnies CW, Ho A. Marginal dry eye diagnosis: History versus symptomatology. In: Holly FJ, editor. The Pre-ocular Tear Film in Health, Disease and Contact Lens Wear. Lubbock, Texas: Dry Eye Institute; 1986. [Google Scholar]
- 36.Moss SE, Klein R, Klein BE. Incidence of dry eye in an older population. Arch Ophthalmol. 2004;122:369–73. doi: 10.1001/archopht.122.3.369. [DOI] [PubMed] [Google Scholar]
- 37.Eckstein AK, Finkenrath A, Heiligenhaus A, Renzing-Köhler K, Esser J, Krüger C, et al. Dry eye syndrome in thyroid-associated ophthalmopathy: Lacrimal expression of TSH receptor suggests involvement of TSHR-specific autoantibodies. Acta Ophthalmol Scand. 2004;82:291–7. doi: 10.1111/j.1395-3907.2004.00268.x. [DOI] [PubMed] [Google Scholar]
- 38.Ismailova DS, Fedorov AA, Grusha YO. Ocular surface changes in thyroid eye disease. Orbit. 2013;32:87–90. doi: 10.3109/01676830.2013.764440. [DOI] [PubMed] [Google Scholar]
- 39.Tavakoli M, Kallinikos PA, Efron N, Boulton AJ, Malik RA. Corneal sensitivity is reduced and relates to the severity of neuropathy in patients with diabetes. Diabetes Care. 2007;30:1895–7. doi: 10.2337/dc07-0175. [DOI] [PubMed] [Google Scholar]
- 40.Chia EM, Mitchell P, Rochtchina E, Lee AJ, Maroun R, Wang JJ. Prevalence and associations of dry eye syndrome in an older population: The Blue Mountains Eye Study. Clin Exp Ophthalmol. 2003;31:229–32. doi: 10.1046/j.1442-9071.2003.00634.x. [DOI] [PubMed] [Google Scholar]
- 41.Moss SE, Klein R, Klein BE. Long-term incidence of dry eye in an older population. Optom Vis Sci. 2008;85:668–74. doi: 10.1097/OPX.0b013e318181a947. [DOI] [PubMed] [Google Scholar]