Abstract
Purposes
The study examined the relationship between depression, diabetes distress and psychological well-being and also assessed the mediating role of diabetes distress on depression relationship with psychological well-being among persons with diabetes during the covid-19 pandemic.
Methods
The study conducted a cross-sectional survey design. A total of 223 (age 35 to 73 years, mean = 53.26 years and SD = 11.05 years) people living with diabetes who are registered patients and were attending the clinic in Department of medicine, Ondo State Specialist Hospital, Okitipupa were selected for the study using the convenient sampling technique. The data were analysed using Pearson Multiple correlation and mediation model 4 of PROCESS macro. The analyses were carried out with ROCESS macro for IBM/SPSS Version 25.0.
Results
Showed psychological well-being has negative significant relationship between diabetes distress (r = −0.42, p < .05) and depression (r = 0.52, p < .05) among persons with diabetes during covid-19 pandemic. The result showed significant and negative direct relationship between depression and diabetes distress (β = −0.47, p < 0.05), 95% Cl: = −0.60 (−0.34). The results also showed significant direct relationship depression and psychological well-being (β = 0.36, p < 0.05), 95% Cl: = 0.26 (0.47) and further that diabetes distress significantly mediate indirect relationship between depression and psychological well-being among persons with diabetes during covid-19 pandemic (β = −0.19, p < .05), 95% Cl: = 0.29 (−0.09).
Conclusion
Depression and diabetes distress associated with the psychological well-being of persons with diabetes during covid-19 pandemic and diabetes distress may play vital role on the association between depression and with the psychological well-being of persons with diabetes during covid-19 pandemic.
Keywords: Psychological well-being, Depression, And diabetes distress
Introduction
The devastation of covid-19 infection can obliterate the psychological well-being of persons with diabetes. Covid-19 infected persons diabetes were found to be suffered a strain of coronavirus called Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [8]. Studies showed that diabetes is a common risk factor of covid-19 and 51% persons with diabetes who suffered covid-19 experienced hyperglycemia [4, 11, 13]. Evidence showed that persons with diabetes experiencing poor psychological well-being [10, 12]. The psychological well-being of persons with diabetes that involves their ability to experience deep happiness, resilience, adequate diabetes-related self-care, good decision-making can be affected by diabetes distress and depression during covid-19 pandemic.
Psychological well-being is about perceived life going well satisfactory by the individual. It is the combination of feeling good and functioning effectively [3]. Prior to the covid-19 pandemic, studies showed that depression significantly decreased the psychological well-being of persons with diabetes [6, 22]. Evidence showed that psychological disorders such as anxiety and depression were found to be common among persons with diabetes, which decreased their psychological well-being [17, 22]. Studies that examined the relationship between depression and psychological well-being were more documented among non-diabetes individual than persons with diabetes [5, 26].
The presence of diabetes distress in depression may worsen the general well-being of persons with diabetes. Diabetes distress involved the emotional burden (fear about managing the demands of diabetes overtime), regimen distress (feeling that they are failing by managing their diabetes properly via feeding regimen, medication regimen, adequate exercising, and self-monitoring of blood glucose levels), interpersonal distress (worries about receiving sufficient support from family and friends) and physician distress (worries about healthcare and receiving expert medical care and support from health care providers) that stunts their psychological resilience to easily manage their present health condition [20].
Severe diabetes distress may be associated with adverse medical and psychological outcomes such as suboptimal self-management (reduced physical activity, poor eating habits, contrivance of medication instructions, and irregular blood glucose checks), elevated Haemoglobin, and frequent and severe hypoglycaemia; all of which may reduce the general well-being of diabetics [2, 18]. Alvani, Zaharim & Kimura, [1] study showed that diabetes distress significantly associated with psychological well-being of persons with diabetes. Peyrot et al., [19] found significant relationship between individual with worst psychological well-being and diabetes- related distress in persons with diabetes. Rahimi, et al., [21] study revealed significant mediating role of resilience and diabetes distress in relationship between depression and treatment adherence. Van Bastelaar, et al. [25] research found diabetes-specific emotional distress as mediating association between depression and glycaemic control.
Objectives of the study
The main objective was to assess psychological well-being in persons with diabetes during the covid-19 pandemic because it can devastate their psychological well-being. The specific objectives were to examine the relationship between depression, diabetes distress and psychological well-being also assessed the mediating role of diabetes distress on depression relationship with psychological well-being among persons with diabetes during the covid-19 pandemic.
Design
The study conducted a cross-sectional survey design. Primary data was collected through the administration of a set of standardised psychological scales on a convenient sample of the study population. Also, patients’ data such as diagnosis, and socio-demographic were collected from their medical files. Each file contains patient’s age, sex, and type of diabetes.
Participants
A total of 223 diabetes patients receiving follow-up clinical treatment in medicine unit, State specialist Hospital, Okitipupa were purposively selected for the study. Ondo State Teaching Hospital, Akure and Federal Medical Centre, Lokoja provide wide range of medical services to patients in different departments. A total of 223 (165 male and 58 female) participants were selected for the study using the convenient sampling technique whereby only patients available on four consecutive clinic days were approached individually and those who consented were included in the study.
The sample comprised of 118 (52.9%) persons with T2DM and 105 (47.1%) and person with T1DM participants in study. The age of the 223 respondents ranged from 35 to 73 years, mean = 53.26 years and SD = 11.05 years.
Instruments
Scales of psychological well-being
Scales of Psychological Well-Being (SPWB) is a structured, self-report instrument based on the six dimensions of psychological well-being and developed by Ryff [23, 1995]. The SPWB consists of 18 items phase in the form of sentences with which respondents could agree or disagree. Each item is respondent to on 6-point Like-type scale ranging from ‘strongly disagree’ to ‘strongly agree’. These responses were scored as follows: strongly disagree = 1, moderately disagree = 2, slightly disagree = 3, slightly agree = 4 moderately agree = 5 and strongly agree = 6.
The SPWB could be scored for its six (6) dimensions of the scales are autonomy, positive relationship with other, environment mastery, self-acceptance, personal growth, and purpose in life. The self-acceptance dimension assesses positive attitudes held toward the self” (Akin, 2008). It can also be scored in such a way as to obtain a global psychological well-being.
In this case items scores are summarized across all 18 items to obtain a total. This scoring pattern was adopted in this study. The higher these total scores the better the psychological well-being of the respondent. Internal consistency values provided by Dierendonck, (2005) for the 18 items scale were significantly higher than the values of other versions; reliability coefficient of sub-scales range between 0.72 (personal growth) and 0.81 (self-acceptance, autonomy and purpose in life). The internal consistency reliability coefficients as reported by Ryff [23] ranges from .86 to .93 for the six sub-scales. Reliability coefficient of .63 for the entire scale was found by Onyedibe et al. [15] in Nigeria. The SPWB was used also Oyeleke and Pius [16] on Children with Disabilities in South-Western Nigeria. The current study found reliability coefficient of 0.57 for persons with diabetes.
Center for Epidemiologic Studies-Depressed Mood Scale (CES-D)
The Center for Epidemiologic Studies Depression Scale (CES-D) was developed by Radloff (1977). The CES-Dis 20-item self-report depression scale was developed to identify depression in the general population. Each item is rated on a 4-point Likert-type scale ranging from zero to three. Estimated administration times range from seven to 12 min (the higher figures being for elderly people) [7]. The CES-D is easily scored by reverse-scoring items 4, 8, 12, and 16, and then summing the scores on all items. This produces a range of zero to 60 with higher scores indicating greater depression.
The CES-D has very good internal consistency with alphas of roughly 0.85 for the general population, and 0.90 for the psychiatric population [14]. Split-half and Spearman-Brown reliability coefficients ranged from 0.77 to 0.92. The CES-D has fair stability with test-retest correlations that range from 0.51 to 0.67 (tested over two to eight weeks) and 0.32 to 0.54 (tested over 3 months to one year) [14].
Diabetes distress scale (DDS)
Diabetes Distress (DDS) was developed by Polonsky, et al. [20]. The DDS is a 17-item self-report measure designed to assess diabetes distress. The responses to each item are rated on a 6-point Likert-type scale (1 = not a problem, 2 = a slight problem, 3 = a moderate problem, 4 = somewhat serious problem, 5 = a serious problem, and 6 = a very serious problem). The minimum and the maximum scores of the scale were 17 and 102. In this regard, higher scores indicate high distress. Polonsky et al. [20] found high internal consistency of Cronbach’s (α = 0.87) for the whole DDS. Lin et al. [9] reported good reliability (Cronbach’s α = 0.81) for DDS. Schmitt et al. [24] reported good reliability Cronbach’s (α = 0.89) for DDS. The overall DDS-17 Cronbach’s α = 0.92, and the Cronbach’s α values for the subscales ranged from 0.784 to 0.859 as Chin et al. (2017).
Procedure
Ethical clearance was obtained from the Research Ethics Committee of the hospital. Participants gave informed consent before they were enrolled in the study. The researchers were introduced by the consultant to the nurses, patients and other members of the staff in the department of endocrinology. This was to ensure the maximum support of the nurses and other staff of the hospital. The study questionnaire was administered individually by the researchers on clinic days within the hospital premise. The participants filled questionnaires during their waiting time to see their doctors for consultations. In order to ensure an anonymous process while collecting the data, a drop box was placed in the waiting room. Participants were informed about the drop box and the importance of anonymity. The study data were collected between 8th of April to 22th of July, 2021.
Data analysis
The data were analysed using Pearson Multiple correlation and mediation model 4 of PROCESS macro. The analyses were carried out with ROCESS macro for IBM/SPSS Version 25.0.
Results
Table 1 presented the results of study hypothesis that states there is no relationship between diabetes distress, depression and psychological well-being among persons with diabetes during covid-19 pandemic. The results showed psychological well-being negative and significant relationship with diabetes distress (r = −0.42, p < .05) and depression (r = 0.52, p < .05). The alternative hypothesis which state there is significant r relationship between diabetes distress depression and psychological well-being among persons with diabetes during covid-19 pandemic was accepted, while the null hypothesis was rejected.
Table 1.
Summary of multiple Pearson correlation analysis between the diabetes distress depression and psychological well-being (N = 223)
| Variables | Mean (SD) | 1 | 2 | 3 |
|---|---|---|---|---|
| 1. Diabetes Distress | 60.61 (29.51) | 1 | ||
| 2. Depression | 36.24 (27.16) | −0.43** | 1 | |
| 3. Psychological Well-Being | 32.78 (23.68) | −0.42** | 0.52** | 1 |
Notes
Table 2 presented the results of the hypothesis that states there is no significant mediating role of diabetes distress on the relationship between depression and psychological well-being in persons with diabetes during covid-19 pandemic. This hypothesis was tested with Model 4 mediation, moderation, and conditional process analysis (Hayes, 2018). Diabetes distress among persons with diabetes during covid-19 pandemic was explained by the model at a rate of 19% (R2 = 0.19) of the total variance of depression, (F1, 221) 51.15, p < 0.05. Also, Psychological well-being among persons with diabetes during covid-19 pandemic was explained by the model at a rate of 19% (R2 = 0.19) of the total variance of depression and diabetes, (F1, 220) 50.24, p < .05.
Table 2.
Summary of mediation analysis diabetes distress and depression on psychological well-being (model 4 of PROCESS macro; N = 223)
| Explained Variables | ||||||
|---|---|---|---|---|---|---|
| Diabetes Distress | Psychological Well-being | |||||
| Model | β | SE | 95% CI | Β | SE | 95% CI |
| LLCI (ULCI) | LLCI (ULCI) | |||||
| Constant | 77.67** | 2.98 | 71.80(83.55) | 31.18** | 4.45 | 22.41(39.94) |
| Depression | −0.47** | 0.07 | −0.60(−0.34) | 0.36** | 0.05 | 0.26 (0.47) |
| Diabetes Distress | −0.19 ** | 0.05 | 0.29(−0.09) | |||
| R | 0.43 | R | 0.24 | |||
| R2 | 0.19 | R2 | 0.06 | |||
| F(df) | F(1, 221) = 51.15 ** | F(df) | F(2, 220) = 50.24 ** | |||
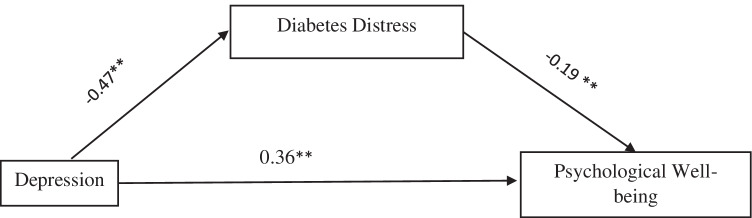
Mediation analysis presented in Table 2 revealed significant and negative direct relationship between depression and diabetes distress (β = −0.47, p < 0.05), 95% Cl: = −0.60(−0.34) see Fig. 1. The results also showed significant direct relationship depression and psychological well-being (β = 0.36, p < 0.05), 95% Cl: = 0.26 (0.47) and further revealed significant indirect relationship between depression and psychological well-being which occur via diabetes distress among persons with diabetes during covid-19 pandemic (β = −0.19, p < .05), 95% Cl: = 0.29 (−0.09) see Fig. 1.
Fig. 1.
Theoretical research model with standard coefficients (β) Model 4
4. Discussion
The present study examined the relationship between depression, diabetes distress and psychological well-being among persons with diabetes during Covid-19 pandemic and also assessed the mediating role of diabetes distress on depression relationship with psychological well-being among persons with diabetes during the covid-19 pandemic in Nigeria.
The study results showed that psychological well-being has negative significant relationship between diabetes distress and depression which is congruent with existing literature of Ramkisson et al. [22] that found strong negative correlation between anxiety and depression and psychologically well-being which pointed in their study that an increase in anxiety and depressive features results in a decrease in psychological well-being. On the other hand, the study results are in accordance with the previous study which established that relationship between emotional distress, psychological well-being and depression of people with diabetes [6].
The study results also supported findings that showed the existing relationship between depression and psychological well-being among non-diabetes persons. Young [26] found significant relationship between depression and psychological well-being mediated by college student’s negative emotional experiences. Joseph and De Guzman [5] found significant relationship between depression and psychological well-being that impaired the mental health of adolescents.
The study results also revealed the diabetes distress significantly mediate indirect relationship between depression and psychological well-being among persons with diabetes during covid-19 pandemic. The study results supported a previous finding by Rahimi et al. [21] who concluded that depression has an indirect effect on the adherence to treatment by mediating role of resilience and diabetes distress. This study results also is in the accordance with study by Van Bastelaar, et al. [25] who admitted diabetes-specific emotional distress as mediating association between depression and glycaemic control.
Conclusions
Depression and diabetes distress associated with the psychological well-being of persons with diabetes during covid-19 pandemic and diabetes distress may play vital role on the association between depression and with the psychological well-being of persons with diabetes during covid-19 pandemic.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alvani SR, Zaharim NM, Kimura LW. Defining the relationship of psychological well-being and diabetes distress with glycemic control among Malaysian type 2 diabetes. Pract Clin Psychol. 2015;3(5):167–175. [Google Scholar]
- 2.Berry E, et al. Diabetes distress: understanding the hidden struggles of living with diabetes and exploring intervention strategies. Postgrad Med J. 2015;91(1075):278–283. doi: 10.1136/postgradmedj-2014-133017. [DOI] [PubMed] [Google Scholar]
- 3.Girum T. Psychological wellbeing as a function of religious involvement, spirituality and personal meaning in life among community - residing elders in Dessie Town MA. thesis 2012
- 4.Iacobellis G, Penaherrera CA, Bermudez LE, Bernal ME. Admission hyperglycemia and radiological findings of SARS-COv2 in patients with and without diabetes. Diabetes Res Clin Pract. 2020;164:108185. doi: 10.1016/j.diabres.2020.108185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joseph S, De Guzman R. Relationship between psychological well-being and depression among selected adolescents. Indian J Positive Psychol. 2021;12(3):232–235. [Google Scholar]
- 6.Kalra S, Jena BN, Yeravdekar R. Emotional and psychological needs of people with diabetes. Indian J Endocrinol Metabol. 2018;22(5):696–704. doi: 10.4103/ijem.IJEM_579_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5(2):179–93. 10.1177/089826439300500202. [DOI] [PubMed]
- 8.Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021;17(1):11–30. 10.1038/s41574-020-00435-4. [DOI] [PMC free article] [PubMed]
- 9.Lin K, Park C, Li M, Wang X, Li X, Li W, Quinn L. Effects of depression, diabetes distress, diabetes self-efficacy, and diabetes self-management on glycemic control among Chinese population with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2017;131:179–186. 10.1016/j.diabres.2017.03.013. [DOI] [PubMed]
- 10.Massey CN, Feig EH, Duque-Serrano L, Wexler D, Moskowitz JT, Huffman JC. Well-being interventions for individuals with diabetes: A systematic review. Diabetes Res Clin Pract. 2019;147:118-133. 10.1016/j.diabres.2018.11.014. [DOI] [PMC free article] [PubMed]
- 11.Means C. Mechanisms of increased morbidity and mortality of SARS-CoV-2 infection in individuals with diabetes: what this means for an effective management strategy. Metabolism. 2020;108:154254. doi: 10.1016/j.metabol.2020.154254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mirahmadizadeh A, Banihashemi SA, Hashemi M, Amiri S, Basir S, Heiran AM, Keshavarzian O. Estimating the prevalence and incidence of treated type 2 diabetes using prescription data as a proxy: A stepwise approach on Iranian data. Heliyon 7 2021;e07260 10.1016/j.heliyon.2021.e07260. [DOI] [PMC free article] [PubMed]
- 13.Muniangi-Muhitu H, Akalestou E, Salem V, Misra S, Oliver NS, Rutter GA. Covid-19 and diabetes: a complex bidirectional relationship. Front Endocrinol. 2020;11:582936. doi: 10.3389/fendo.2020.582936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okun A, Stein RE, Bauman LJ, Silver EJ. Content validity of the Psychiatric Symptom Index, CES-depression Scale, and State-Trait Anxiety Inventory from the perspective of DSM-IV. Psychol Rep. 1996;79(3 Pt 1):1059–69. 10.2466/pr0.1996.79.3.1059. [DOI] [PubMed]
- 15.Onyidibe MCC, Ugwu LL. An Evaluation of the Relationship Between Coping, Emotional Intelligence and Psychological Well-being Among University Undergraduates 2015;3(5)
- 16.Oyeleke AI, Pius TT. Income and Occupation as Correlates of Well-Being of Caregivers of Children with Disabilities in South-Western Nigeria. Mediterranean Journal of Social Sciences 2012;5(2):111–119
- 17.Ozder A. The well-being and depression status of diabetic patients in primary health care. Acta Medica Mediterranea. 2015;31(1):23–29. [Google Scholar]
- 18.Pandit AU, et al. Disease-related distress, self-care and clinical outcomes among low-income patients with diabetes. J Epidemiol Community Health. 2014;68(6):557–564. doi: 10.1136/jech-2013-203063. [DOI] [PubMed] [Google Scholar]
- 19.Peyrot M, Skovlund SE, Radzio R, Kokoszka A. Psychological well-being and diabetes-related distress in states of type 2 diabetes in the DAWN study. Clin Diabetol. 2019;8(3):167–175. doi: 10.5603/DK.2019.0012. [DOI] [Google Scholar]
- 20.Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, Jackson RA. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28(3):626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 21.Rahimi M, Jalali M, Nouri R, Rahimi M. The mediating role of resilience and diabetes distress in relationship between depression and treatment adherence in type 2 diabetic among Iranian patients. J Commun Health Res. 2020;9(2):107–118. [Google Scholar]
- 22.Ramkisson S, Pillay BJ, Sartorius B. Anxiety, depression and psychological well-being in a cohort of south African adults with type 2 diabetes mellitus. S Afr J Psychiatry. 2016;22(1). 10.4102/sajpsychiatry.v22i1.935. [DOI] [PMC free article] [PubMed]
- 23.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081.
- 24.Schmitt A, Reimer A, Kulzer B, Haak T, Gahr A, Hermanns N. Assessment of diabetes acceptance can help identify patients with ineffective diabetes self-care and poor diabetes control. Diabet Med. 2014;31(11):1446–51. 10.1111/dme.12553. [DOI] [PubMed]
- 25.Van Bastelaar KMP, Pouwer F, Geelhoed-Duijvestijn PHLM, Tack CJ, Bazelmans E, Beekman A, Heine TRJ, Snoek FJ. Diabetes-specific emotional distress mediates the association between depressive symptoms and glycaemic control in type 1 and type 2 diabetes. Diabet Med. 2010;27:798–803. doi: 10.1111/j.1464-5491.2010.03025.x. [DOI] [PubMed] [Google Scholar]
- 26.Young JL (2020). The effects of depression and anxiety on psychological well-being of college students: focusing on the emotional perception clarity. Medico Legal Update. 20(1):2149–2154. 10.37506/mlu.v20i1.699.