Abstract
Purpose:
Multiparametric magnetic resonance imaging (mp-MRI) and MRI/Ultrasound (US) fusion-guided biopsy are relatively new techniques for improved detection, staging, and active surveillance of prostate cancer (PCa). As with all imaging modalities, MRI reveals incidental findings (IFs) which carry the risk of increased cost, patient anxiety, and iatrogenic morbidity due to workup of IFs. Herein, we report the IFs from 684 MRIs for evaluation of PCa and consider their characteristics and clinical significance.
Methods:
Patients underwent mp-MRI prostate protocol incorporating triplanar T2-weighted, diffusion-weighted, and dynamic contrast-enhanced pelvic MRI as well as a post-contrast abdominopelvic MRI with the primary indication of detection or evaluation of PCa. A total of 684 consecutive prostate MRI reports performed in a series of 580 patients were reviewed. All extraprostatic findings reported were logged and then categorized by organ system and potential clinical significance.
Results:
There were 349 true IFs found in 233 (40%) of the 580 patients. One hundred nineteen additional extraprostatic findings were unsuspected but directly related to PCa staging, while the 349 IFs were unrelated and thus truly incidental beyond study indication. While the majority of true IFs were non-urologic, only 6.6% of IFs were considered clinically significant, non-urologic findings, and more than a third of MRI reports had urologic IFs not related to PCa.
Conclusions:
Rates of incidental findings on prostate indication MRI are similar to other abdominopelvic imaging studies. However, only 6.6% of the IFs were considered to be clinically significant non-urologic findings. Further investigations are needed to assess downstream workup of these IFs and resulting costs.
Keywords: Prostate adenocarcinoma, Cancer staging, Incidental findings, Public health
Prostate cancer (PCa) is the most common solid-organ malignancy diagnosed in American men, estimated at 161,360 new cases diagnosed in the United States in 2017 [1]. Since multiple management options exist for early staged PCa, early detection with proper risk stratification is critical for selecting the most appropriate treatment options [2]. Currently, PCa is commonly diagnosed using systematic transrectal ultrasound (TRUS)-guided prostate biopsies, usually prompted by elevated serum prostate-specific antigen (PSA) or abnormal digital rectal exam (DRE) findings. However, this traditional approach can result in high rates of false negative results, undergrading, or understaging of the disease, especially with cancer located in occult regions of the gland: distal apical, midline, subcapsular, and anterior areas [3–7]. The use of multiparametric magnetic resonance imaging (mp-MRI) and MRI/US fusion-guided prostate biopsy is gaining traction at many centers [8]. This technology allows for image-guided targeting of cancer suspicious lesions with proven improvement in detection of PCa, particularly clinically significant cancer foci, compared to random TRUS guided biopsy [9, 10]. This ultimately allows for more accurate detection, localization, staging, risk stratification, and treatment counseling for men with PCa [7].
As with all imaging modalities, MRI has the potential for revealing both clinically significant and indolent incidental findings (IFs). In addition to the prostate gland, mp-MRI performed for evaluation of prostate cancer can also identify possible pathologies in the field of view: abdominal and pelvic organs, bones, and vasculature. This has the potential benefit of improving PCa staging through evaluation of the seminal vesicles, bones, and regional pelvic lymph nodes for potential PCa involvement. However, there is also the risk of patient anxiety, increased cost burden, and iatrogenic morbidity due to work up prompted by IFs that are not clinically significant, potentially leading to an increased public health burden [11]. Previous studies have elicited the costs of IFs in various imaging modalities [12–20]. However, there are no previous studies comprehensively evaluating and reporting IFs found on mp-MRI done for evaluation of PCa. Herein, we report the incidence, anatomic distribution, and clinical significance of incidental findings found on 684 consecutive mp-MRI studies performed in a series of 580 patients for the evaluation of prostate cancer at a single center.
Methods
An IRB-approved, HIPAA-compliant retrospective review of prostate mp-MRI records spanning a three-year period from July 2013–June 2016 was performed. All patients included in the study underwent mp-MRI with the primary indications of detecting or risk-stratifying cases of PCa; this included patients with clinical suspicion of prostate cancer based upon elevated PSA or abnormal DRE who were either biopsy naïve or had prior negative prostate biopsy sessions as well as men with prostate cancer diagnoses on active surveillance or seeking MRI for pre-treatment planning. Prostate indication mp-MRI studies for men who had already undergone primary definitive therapy were excluded. Figure 1 shows how these inclusion criteria were used to select the mp-MRI records used for final analysis in this study.
Fig. 1.
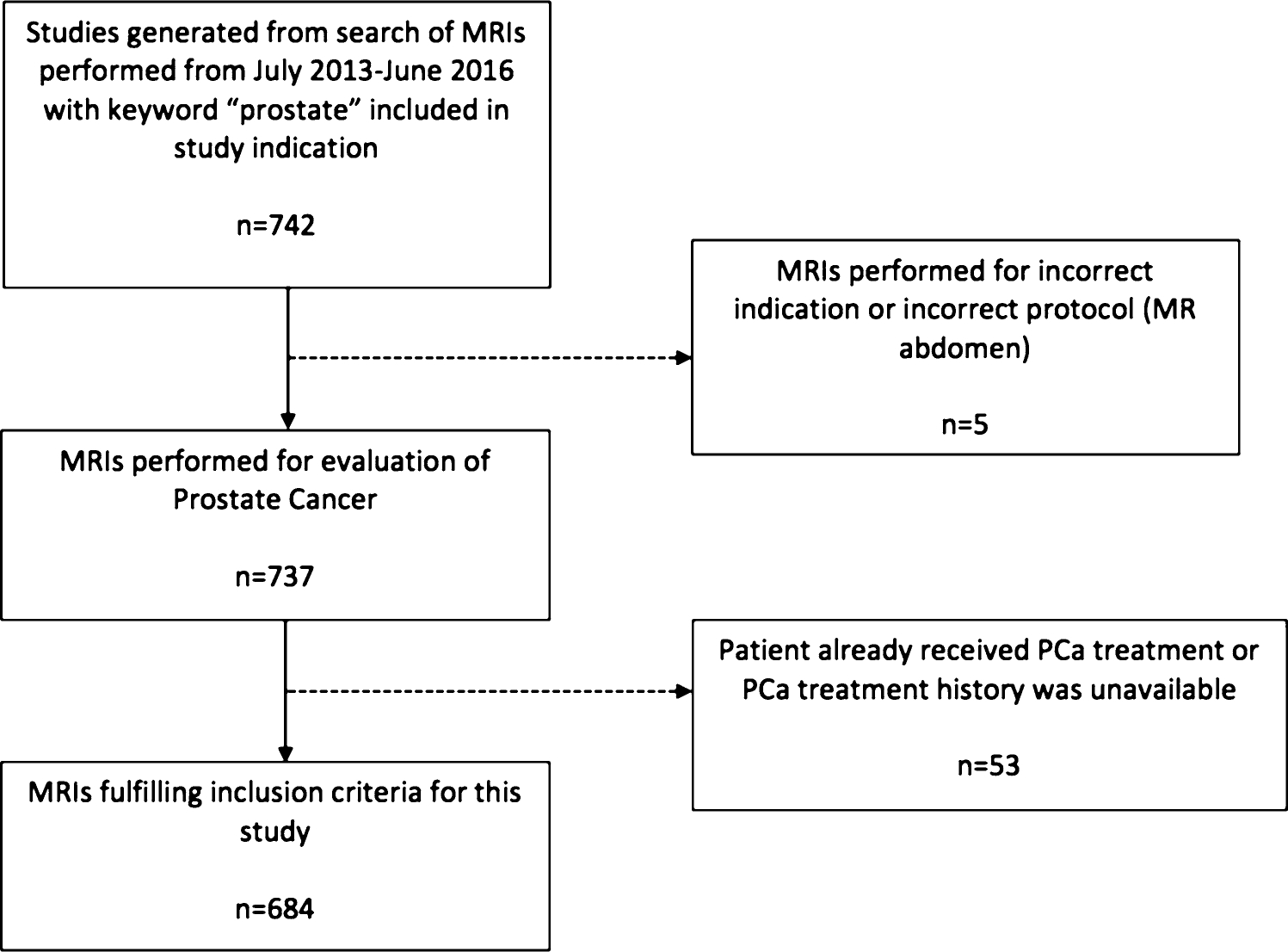
Inclusion and exclusion criteria for mp-MRIs included in study.
The mp-MRI prostate protocol included triplanar T2-weighted, diffusion-weighted, and dynamic contrast-enhanced pelvic MRI as well as a post-contrast abdominopelvic T1-weighted MRI as previously described [21]. All MRIs were reviewed by an MRI specialized body radiologist on an Intellispace Portal (Philips Medical systems, Eindhoven, The Netherlands) Picture Archiving Communications System (PACS).
The radiologist’s written report for each MRI was then reviewed and all extraprostatic findings were recorded. An incidental finding was defined as an asymptomatic, unrelated imaging abnormality discovered during workup for prostate cancer detection and risk stratification. Additionally, PCa-related findings important for staging were also recorded and analyzed separately. For patients who underwent more than one prostate MRI, IFs were only counted for the first report in which they were mentioned. IFs were then categorized by clinical significance based on a classification system used in previous similar studies [12–14].
Subsequently, a retrospective review of the medical record was also performed for patients who had IFs reported documenting patient demographics. Patients were also stratified by biopsy status, specifically biopsy naïve, prior negative biopsy, or pre-MRI biopsy-proven PCa.
Results
There were 580 male patients who underwent 684 MRI studies that were included in this study, with a mean age of 63.3 years (range 40–84 years) and mean PSA of 8.42 ng/mL (range 0.3–76.34 ng/mL). For each MRI report, the patient’s prostate biopsy and PCa history were recorded. In 87 (13%) reports, the patient was biopsy naïve, 219 (32%) had at least one previous negative biopsy, 372 (54%) had needle core biopsy-proven PCa, and 6 (1%) had PCa diagnosed in a manner other than biopsy (i.e., TURP specimen). Ninety-three (16%) patients underwent more than one prostate indication mp-MRI study, whether for continued monitoring of PCa on AS or because of a previously terminated incomplete mp-MRI study. The average number of MRIs in patients who had more than one was 2.12, and there were 104 repeat MRIs total. The patient’s age at exam correlated with the number of IFs (p = 0.016). The number of MRI studies performed per patient did not correlate with the number of IFs found (p = 0.584). However, prior biopsy history (biopsy naïve, prior negative biopsy, and PCa-proven cases) at time of mp-MRI was significantly associated with number of IFs (p = 0.025); patients with prior PCa-positive biopsies had a significantly higher average of IFs (0.87) compared to those with negative biopsies (0.57) and who were biopsy naïve (0.60).
There were 349 incidental findings total in 233 (40%) of the 580 patients. 347 (60%) patients had no IFs, 145 (25%) patients had one IF, and 88 (15%) patients had two or more IFs (Fig. 2). For MRI reports in which the patient was biopsy naïve at the time of the study, there was an average of 0.60 findings per MRI, patients with a previous negative biopsy had an average of 0.57 findings per MRI, and patients with prior diagnoses of PCa had an average of 0.87 findings per MRI. In addition to the 349 truly incidental findings, there were also 119 extraprostatic findings directly related to PCa staging (suspected cancer spread to seminal vesicles, lymph nodes, bones, and any other metastases), which were not truly incidental outside the indication of the study performed. 170 (49%) of the non-PCa-related extraprostatic IFs were considered related to the genitourinary system. A summary of PCa-related findings and urologic non-PCa-related IFs is reported in Table 1.
Fig. 2.
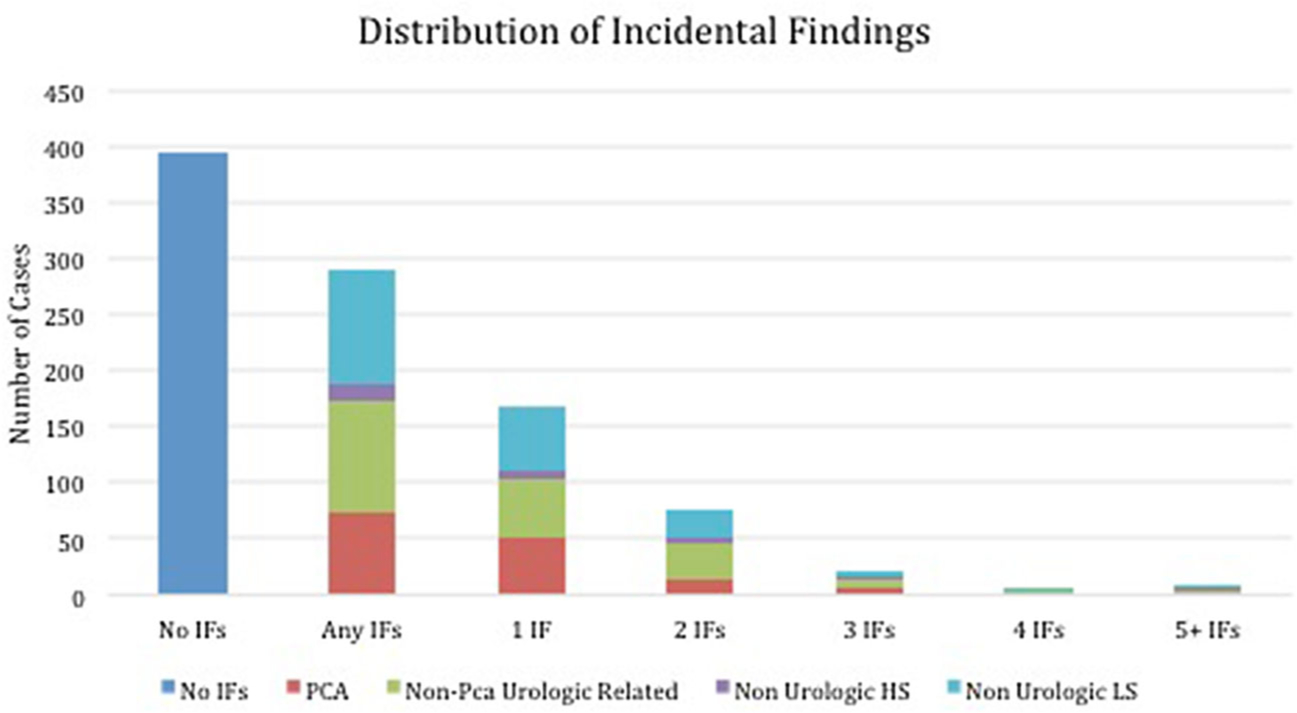
Graphic representation of the distribution of incidental findings in multiparametric MRI studies with a prostate indication.
Table 1.
PCa-related extraprostatic imaging findings and urologic incidental findings found on multiparametric MRI studies with a prostate indication
| Extraprostatic finding related to prostate cancer | 119 |
| Suspected osseous metastasis | 31 |
| Pelvic lymphadenopathy, suspected metastases | 20 |
| Borderline pelvic lymphadenopathy, indeterminate for metastases | 17 |
| Suspected seminal vesicle invasion | 40 |
| Suspected rectal invasion | 2 |
| Suspected bladder invasion | 4 |
| Soft tissue nodule anterior to bladder suspicious for metastasis | 1 |
| Suspected invasion of urethra | 2 |
| Suspected invasion of ejaculatory ducts | 2 |
| Non-prostate cancer related urologic incidental findings | 170 |
| Bladder diverticulum | 8 |
| Bladder wall thickening/trabeculation | 89 |
| Bladder/kidney stones | 3 |
| Bladder mass | 2 |
| Ureteral diverticulum | 1 |
| Ureterocele | 2 |
| Renal cysts | 39 |
| Solid renal masses | 5 |
| Atrophic transplant kidney | 1 |
| Atrophic native kidneys | 1 |
| Hydroureteronephrosis | 2 |
| Benign scrotal pathology (hydrocele, varicocele, epididymal cyst) | 6 |
| Prostatic utricle cyst, ejaculatory duct cyst, Mullerian duct cyst | 10 |
| Urachal remnant/cyst | 1 |
Table 2 shows the non-urologic IFs organized by clinical significance. Of these 179 non-urologic IFs, 23 (13%) were classified as bearing high clinical significance, and 156 (87%) were classified as low to moderate clinical significance.
Table 2.
Non-urologic incidental findings found on multiparametric MRI studies with a prostate indication stratified by clinical significance
| Non-urologic incidental findings (high clinical significance) | 23 |
| Mesenteric mass | 1 |
| Psoas mass | 1 |
| Possible colonic neoplasm | 1 |
| Indeterminate liver lesion | 4 |
| Abdominal aortic aneurysm > 3 cm | 3 |
| Common iliac aneurysms | 1 |
| Femoral artery aneurysms | 1 |
| Panniculitis | 1 |
| Diverticulitis | 2 |
| Osteonecrosis | 3 |
| Bowel-containing inguinal hernia | 3 |
| Bowel-containing ventral hernia | 1 |
| Bladder-containing inguinal hernia | 1 |
| Non-urologic incidental findings (low to moderate clinical significance) | 156 |
| Diverticulosis | 71 |
| Fat-containing inguinal hernia | 62 |
| Hiatal hernia | 1 |
| Fat-containing ventral hernia | 1 |
| Gallstones | 2 |
| Hepatic cysts | 3 |
| Adrenal cystic lesion | 1 |
| Ectasia of abdominal aorta | 1 |
| Double IVC variant | 1 |
| Pelvic venous varices | 1 |
| Femoral artery filling defect (prior vascular closure device) | 1 |
| Tarlov cyst | 3 |
| Enchondroma | 1 |
| Small amount of pelvic free fluid | 4 |
| Lipomatosis | 1 |
| Lipoma | 2 |
The most frequent of the 119 imaging findings related to PCa staging was suspected seminal vesicle invasion, which accounted for 40 (34%) of PCa staging-related findings reported. The most common of the 170 urologic IFs not related to PCa staging were bladder wall thickening/trabeculation (n = 89, 52%) and renal cysts (n = 39, 23%). Indeterminate liver lesion (n = 4, 17%), abdominal aortic aneurysm greater than 3 cm (n = 3, 13%), osteonecrosis (n = 3, 13%), and bowel-containing inguinal hernia (n = 3, 13%) were the most common of the 23 non-urologic IFs considered to carry higher clinical significance. The most frequent IFs of low to moderate clinical significance, which were also the most frequent IFs overall, were colonic diverticulosis (n = 71, 46%) and fat-containing patent inguinal hernia (n = 62, 40%).
Of the 684 MRI reports, 58 (8.5%) included a total of 71 specific recommendations for follow-up by the radiologist, including bone scan (n = 24, 34%), clinical correlation (n = 15, 21%), ultrasound (n = 9, 13%), CT (n = 8, 11%), plain film radiography (n = 6, 8%), correlation with prior imaging (n = 3, 4%), follow-up MRI (n = 2, 3%), clinical follow-up (n = 2, 3%), colonoscopy (n = 1, 1%), and urinalysis (n = 1, 1%). Twenty-five (3.7%) imaging studies were considered incomplete, most were prematurely stopped prior to completion of the scan due to residual hemorrhage from previous prostate biopsy (n = 18, 72%) or patient intolerance of the MRI study related to discomfort or claustrophobia (n = 5, 20%).
Discussion
Mp-MRI and MRI/US fusion-guided biopsies are relatively new techniques for improved detection, staging, and active surveillance of PCa [2, 21, 22]. As with all imaging modalities, MRI has the potential for detecting clinically insignificant IFs. This can prompt additional clinical encounters and imaging studies, which in turn can lead to increased costs, patient anxiety, and potentially iatrogenic morbidity.
Previous studies have investigated such downstream effects of IFs found on various imaging modalities. Yee et al. reported extracolonic findings in 63.0% of patients undergoing CT colonography of which 9.0% were considered clinically impactful IFs. In our study, 42% of mp-MRIs had incidental findings and 6.6% of the IFs were clinically significant. Our study populations were similar: all male patients with a similar age distribution (mean age 62.5 years, range 30–90 in the study of CT colonography and mean age 63.3 years, range 40–84 in the current study of mp-MRI of the prostate). Additionally, we used a similar system of categorization of IFs as reported by Yee and colleagues: findings not related to the study indication were sorted into two categories of clinical relevance (high clinical significance and low to moderate clinical significance). Yee et al. recommended this system of categorization instead of a three-tier system used in other previous studies of IFs due to its simplicity and relevance to clinical management [19]. The primary difference found was the percentage of clinically significant findings identified: 9.0% in the CT colonography study vs. 6.6% in the current study. The increased visualization of the lungs in CT colonography vs. mp-MRI of the prostate may have contributed to this higher proportion of IF detection in the series of CT colonography, as approximately 20% of the IFs were pulmonary nodules.
Lai et al. assessed the IFs discovered on abdominopelvic imaging for another urologic indication: CT urography for evaluation of asymptomatic microscopic hematuria (AMH). One major difference between our studies lies in the expected yield of the imaging study. While they reported that the etiology of AMH is often not elicited on CT urogram, mp-MRI for the evaluation of PCa frequently yields clinically useful information for the indication intended: intraprostatic lesions for biopsy targeting and/or PCa staging by means of assessing seminal vesicle invasion, lymph node spread, and bony metastatic lesions in the region of the pelvis. On the other hand, the CT urograms in the study reported by Lai and colleagues revealed a higher percentage of clinically significant findings: 14.8% vs. our series with only 6.6%. While this may be in part due to the inclusion of female patients and therefore female pathology in their imaging reports (4 of 30, 13% of their highly clinically significant findings were related to female pelvic anatomy), they reported that overall there was no significant difference in the number of IFs between males and females. Additionally, they found IFs in a higher overall percentage of their patients. Only 11.38% of patients in their study had no IFs at all, whereas 394 of 684 (58%) of MRIs in our study had no IFs. Renal cysts were one of the most common urologic IFs in both studies (68/172, 39.5% in Lai et al.; 39/170, 22.9% in the current study). This may be due to the limited imaging series performed (a single post-contrast T1 W scan for staging purposes) which images the upper abdomen as part of the mp-MRI studies with prostate indication evaluated in this current study.
Further workup of IFs can be of great benefit to the patient. One patient in our current population was found to have a pedunculated lesion incidentally discovered along the posterior left bladder wall protruding into the bladder luminal cavity. This patient was then found to have high-grade, non-muscle invasive bladder carcinoma and subsequently underwent surgical resection and intravesical BCG therapy with surveillance follow-up negative for malignancy.
In another patient, an indeterminate lesion within the left kidney was incidentally noted on mp-MRI for evaluation of PCa with a recommendation to have dedicated renal imaging. On follow-up renal ultrasound, a non-obstructing renal calculus as well as a solid heterogeneously mass with internal vascularity was seen, consistent with neoplasm in the region of the upper pole of the left kidney and left adrenal gland. While on mp-MRI the mass was reported to arise from the kidney, on ultrasound it appeared to be more likely adrenal in origin, and a multiphasic CT or dedicated MRI was recommended for further evaluation and characterization of the mass. CT imaging was performed which revealed a 4.7 cm heterogeneous enhancing left adrenal mass. On clinical follow-up, the patient had elevated normetanephrine and metanephrine levels and long-standing panic attacks. Considering the likelihood of pheochromocytoma, he was premedicated with alpha-blockade and then underwent a laparoscopic left adrenalectomy with pathology confirmed pheochromocytoma. His clinical symptoms and serum markers normalized after surgical resection.
These two patients benefitted from the additional workup, demonstrating the potential benefit of following up on incidental findings. These cases also show how an incidental finding can lead to a cascade of further workup such as imaging, referrals, labs, and procedures. While these patients did benefit from IF workup and treatment, this is not always the case. One patient with biopsy-proven Gleason 4 + 3 = 7 PCa underwent mp-MRI, in which there was a thickened, nodular appearance of the inferior bladder wall. The patient was asymptomatic at the time, but underwent cystoscopy for workup of the imaging findings which was negative for gross tumor. Cytology from bladder washings was also negative for malignancy. In this case, the further diagnostic workup prompted by the IF was not clinically beneficial to the patient. Bladder wall thickening may be a non-specific IF more frequently encountered in this patient population undergoing MRI most often due to elevated PSA or known history of PCa. In these patients, bladder outlet obstruction via prostate enlargement or non-compliant nodularity can increase the likelihood of bladder muscle trabeculations seen as diffuse wall thickening on imaging. This most common urologic IF may be of low yield on further workup, and hence, clinical correlation with assessment of hematuria, prostate volume, urinary flow rate, and post-void residual urine volume may potentially be of high utility in risk stratification.
Hemorrhage due to prostate biopsy was mentioned in MRI reports as limiting the study quality in some cases. Of the 25 studies that had to be discontinued and rescheduled, 18 were due to residual hemorrhage from recent prostate biopsy. While this only makes up 2.6% of the total MRIs in this study, these account for 72% of all the incomplete exams. In the studies that were completed, 29 (4.4%) specifically mentioned that residual blood products limited the quality of the exam. Therefore, hemorrhage from recent prostate biopsy negatively impacted the feasibility or quality of 7.9% (54/684) of the MRIs. Since MRI is an expensive imaging modality, it seems sensible to wait for post-biopsy hemorrhage to clear when possible in order to attain the most informative, clinically useful, sensitive, and specific study possible. However, Feng and colleagues reported that while hemorrhage is prevalent post-prostate biopsy, present in 52% of 36 cases even after 6 weeks, there was no difference in detection of extracapsular extension on mp-MRI as compared with pathology regardless of time elapsed since prostate biopsy [23]. Larger studies may be beneficial for evaluating the impact of post-biopsy hemorrhage on mp-MRI diagnostic value particularly for detection of intraprostatic pathology since a recent consensus panel recommended MRI to be postponed at least 6 weeks though the majority of panelists thought imaging quality would still be impaired at this timepoint [24].
One of the limitations of this study was the interpretation of the imaging studies by multiple (n = 15) radiologists. Each radiologist used different wording to report his or her findings, making systematic classification of these findings challenging. This could be prevented by having one or two radiologists interpret each MRI used in the study, but this was not possible for this study due to the retrospective nature of the chart review and high volume of imaging studies reviewed for this analysis. Also, whereas some studies reviewed the actual images in addition to imaging reports, we reviewed reports only possibly limiting our findings [14, 15, 19]. Additionally, there is some variation in previous studies in classification of IFs by clinical significance. Since this is not standardized, it may introduce some bias in the comparison of various studies, such as the comparisons discussed above. A standardized classification method for IFs would be beneficial for more accurate comparison between studies.
In addition to patient anxiety and iatrogenic morbidity, increased costs are also a potential consequence of IF workup. In order to evaluate the financial burden on both the public health system and the patient, more research is needed examining the cost of follow-up imaging, diagnostic studies, and treatment. A cost analysis would allow for more informed follow-up choices in which the benefits merit the costs required. Such a study looking at the results of IF workup and consequent costs, morbidity, and mortality could help identify what follow-up actually helps the patient, and which interventions cause more morbidity. With this new information on IFs from prostate MRIs and more research on the costs and results of workup of these IFs, improved guidelines for follow-up of IFs could be created and implemented to improve both patient outcomes and efficient use of resources.
Conclusions
Incidental findings are inevitable when employing any imaging. Prostate indication MRI demonstrates rates of incidental findings in 42% of cases, commensurate with other abdominal and pelvic imaging studies done for other indications. However, only 6.6% of these IF were considered to be highly clinically significant.
Abbreviations
- AMH
asymptomatic microscopic hematuria
- AS
active surveillance
- CT
computed tomography
- DRE
digital rectal examination
- IF
incidental finding
- MRI
magnetic resonance imaging
- mp-MRI
multiparametric magnetic resonance imaging
- PCa
prostate cancer
- PSA
prostate-specific antigen
- TRUS
transrectal ultrasound
- US
ultrasound
Footnotes
Compliance with ethical standards
Conflicts of interest Soroush Rais-Bahrami and Jeffrey W. Nix are consultants for Philips/InVivo Corp. Rachael L. Sherrer, Win Shun Lai, and John V. Thomas have no conflicts of interest to declare.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Siegel RL, Miller KD, Jemal A (2017) Cancer statistics. CA Cancer J Clin 67:7. [DOI] [PubMed] [Google Scholar]
- 2.Rais-Bahrami S, Siddiqui MM, Turkbey B, et al. (2013) Utility of multiparametric magnetic resonance imaging suspicion levels for detecting prostate cancer. J Urol 190:1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nix JW, Turkbey B, Hoang A, et al. (2012) Very distal apical prostate tumours: identification on multiparametric MRI at 3 Tesla. BJU Int 110:E694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muthigi A, Sidana A, George AK, et al. (2016) Midline lesions of the prostate: role of MRI/TRUS fusion biopsy and implications in Gleason risk stratification. Int Urol Nephrol 48:1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sankineni S, George AK, Brown AM, et al. (2015) Posterior subcapsular prostate cancer: identification with mpMRI and MRI/TRUS fusion-guided biopsy. Abdom Imaging 40:2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volkin D, Turkbey B, Hoang AN, et al. (2014) Multiparametric magnetic resonance imaging (MRI) and subsequent MRI/ultrasonography fusion-guided biopsy increase the detection of anteriorly located prostate cancers. BJU Int 114:E43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoeks CMA, Barentsz JO, Hambrock T, et al. (2011) Prostate cancer: multiparametric MR imaging for detection, localization, and staging. Radiology 261:46. [DOI] [PubMed] [Google Scholar]
- 8.Muthigi A, Sidana A, George AK, et al. (2017) Current beliefs and practice patterns among urologists regarding prostate magnetic resonance imaging and magnetic resonance-targeted biopsy. Urol Oncol 35(32):e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schoots IG, Roobol MJ, Nieboer D, et al. (2015) Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol 68:438. [DOI] [PubMed] [Google Scholar]
- 10.Siddiqui Mm, Rais-Bahrami S, Turkbey B, et al. (2015) Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 313:390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westbrook JI, Braithwaite J, McIntosh JH (1998) The outcomes for patients with incidental lesions: serendipitous or iatrogenic? AJR 171:1193. [DOI] [PubMed] [Google Scholar]
- 12.Lai WS, Ellenburg J, Lockhart ME, et al. (2016) Assessing the costs of extraurinary findings of computed tomography urogram in the evaluation of asymptomatic microscopic hematuria. Urology 95:34. [DOI] [PubMed] [Google Scholar]
- 13.Morgan AE, Berland LL, Ananyev SS, et al. (2015) Extraurinary incidental findings on CT for hematuria: the radiologist’s role and downstream cost analysis. AJR Am J Roentgenol 204:1160. [DOI] [PubMed] [Google Scholar]
- 14.Yee J, Kumar NN, Godara S, et al. (2005) Extracolonic abnormalities discovered incidentally at CT colonography in a male population. Radiology 236:519. [DOI] [PubMed] [Google Scholar]
- 15.Priola AM, Priola sM, Giaj-Levra M, et al. (2013) Clinical implications and added costs of incidental findings in an early detection study of lung cancer by using low-dose spiral computed tomography. Clin Lung Cancer 14:139. [DOI] [PubMed] [Google Scholar]
- 16.MacHaalany J, Yam Y, Ruddy TD, et al. (2009) Potential clinical and economic consequences of noncardiac incidental findings on cardiac computed tomography. JACC 54:1533. [DOI] [PubMed] [Google Scholar]
- 17.Lumbreras B, Donat L, Hernández-Aguado I (2010) Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol 83:276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hara AK, Johnson CD, MacCarty RL, et al. (2000) Incidental extracolonic findings at CT conolonography. Radiology 215:353. [DOI] [PubMed] [Google Scholar]
- 19.Gleucker TM, Johnson CD, Wilson LA, et al. (2003) Extracolonic findings at CT colonography: evaluation of prevalence and cost in a screening population. Gastroenterology 124:911. [DOI] [PubMed] [Google Scholar]
- 20.Lee CI, Tsai EB, Sigal BM, et al. (2010) Incidental extracardiac findings at coronary CT: clinical and economic impact. AJR Am J Roentgenol 194:1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lai WS, Gordetsky JB, Thomas JV, et al. (2017) Factors predicting prostate cancer upgrading on magnetic resonance imaging-targeted biopsy in an active surveillance population. Cancer 123:1941. [DOI] [PubMed] [Google Scholar]
- 22.Wang L, Hricak H, Kattan MW, et al. (2006) Prediction of organ-confined prostate cancer: incremental value of MR imaging and MR spectroscopic imaging to staging nomograms. Radiology 238:597. [DOI] [PubMed] [Google Scholar]
- 23.Feng T, Koopman S, Kim HL (2015) Impact of post prostate biopsy hemorrhage on multiparametric magnetic resonance imaging. Can J Urol 22:5. [PubMed] [Google Scholar]
- 24.Scheltema MJ, Tay KJ, Postema AW, et al. (2017) Utilization of multiparametric prostate magnetic resonance imaging in clinical practice and focal therapy: report from a Delphi consensus project. World J Urol 35:695. [DOI] [PMC free article] [PubMed] [Google Scholar]


