Abstract
Purpose:
This study tested self-efficacy and social support for activity and dietary changes as mediators of changes in type 2 diabetes related outcomes following a lifestyle intervention among Latino youth.
Setting and Intervention:
Latino adolescents (14–16 years) with obesity (BMI% = 98.1 ± 1.4) were randomized to a 3-month intervention (n = 67) that fostered self-efficacy and social support through weekly, family-centered sessions or a comparison condition (n = 69).
Measures:
Primary outcomes included insulin sensitivity and weight specific quality of life. Mediators included self-efficacy, friend, and family social support for health behaviors. Data was collected at baseline, 3-months, 6-months, and 12-months.
Analysis:
Sequential path analysis was used to examine mediators as mechanisms by which the intervention influenced primary outcomes.
Results:
The intervention had a direct effect on family (β = 0.33, P < .01) and friend social support (β = 0.22, P < .001) immediately following the intervention (3-months). Increased family social support mediated the intervention’s effect on self-efficacy at 6-months (β = 0.09, P < .01). However, social support and self-efficacy did not mediate long-term changes in primary outcomes (P > .05) at 12-months.
Conclusions:
Family social support may improve self-efficacy for health behaviors in high-risk Latino youth, highlighting the important role of family diabetes prevention. Fostering family social support is a critical intervention target and more research is needed to understand family-level factors that have the potential to lead to long-term metabolic and psychosocial outcome in vulnerable youth.
Keywords: Latino health, adolescents, family, diabetes prevention, theory
Purpose
Obesity and type 2 diabetes (T2D) disproportionately impact Latino populations. The prevalence of T2D is twice as high in Latino adults (22.6%) compared to non-Hispanic whites (11.3%).1 These disparities emerge early as Latino youth exhibit higher rates of prediabetes (22.9%) compared to white youth (15.1%).2 Given that the estimated yearly costs of T2D is ~$327 billion and that Latino youth are the fastest growing pediatric subpopulation in the U.S., preventing T2D in high-risk Latino youth is a public health priority.3
Theory-based lifestyle interventions are the first-line approach for the prevention and management of pediatric obesity. Social Cognitive Theory (SCT) is the most widely applied theory in pediatric obesity interventions and one of the most commonly used theoretical frameworks in interventions designed for Latino youth.4,5 Previous literature has demonstrated that SCT constructs like social support and self-efficacy are associated with changes in obesity-related health behaviors in youth, but limited evidence has extended to changes in disease outcomes.6 Social support is defined as the provision of material and/or interpersonal resources through social connections or linkages.7 The primary processes for fostering social support within obesity interventions among youth include providing informational support through knowledge on healthy eating and activity, instrumental support by providing resources for engaging in health behaviors, modeling support from instructors and family members by demonstrating or participating in health behaviors with youth, and emotional support by providing praise or encouragement for behavior change.6,7 Social support for youth primarily comes from family and friends and it is hypothesized that different sources of support may have different influences on health.8 Family support is strongly linked to health behaviors in youth, and this construct may be particularly salient within the context of Latino culture where familismo (familism) is a core value.9 Self-efficacy is defined as confidence in one’s ability to perform a behavior.10 The primary processes within obesity prevention interventions for fostering self-efficacy include building mastery experiences through activities like cooking demonstrations and exercises sessions, developing health knowledge and behavior change skills, and addressing beliefs about one’s ability to make healthy lifestyle changes.4 According to the SCT, interpersonal processes such as social support can lead to increased self-efficacy.11,12 For example, social supports that include role modeling, verbal encouragement, or engaging together in behaviors, provide opportunities to observe others and have the mastery experiences needed to build one’s confidence in their ability to perform that behavior.13
Given the associations of social support and self-efficacy with health behaviors, these constructs are hypothesized as theoretical mechanisms that contribute to health outcomes and have been used to develop successful diabetes prevention programs for adults.14 Given the effectiveness of diabetes prevention programs for reducing diabetes risk in adults, similar programs grounded in SCT have been proposed for high-risk youth.15 However, there is a lack of prospective empirical studies in both adults and youth that test whether changes in self-efficacy and social support are the underlying mechanisms by which diabetes prevention programs are efficacious.16,17 This gap limits the field from identifying intervention inputs that drive and support changes in disease outcomes in high-risk populations like Latino youth.
Following participation in a 12-week, culturally-grounded, lifestyle intervention, we observed significant short-term improvements (12-week) in insulin sensitivity and short- and long-term (12-months) improvements in weight-specific quality of life (QoL-W). The intervention impact on primary outcomes has been previously published.18 Therefore, the purpose of the current study is to test self-efficacy and social support for health behaviors as mediators of long-term changes in diabetes risk and weight-specific quality of life (QoL-W) following a culturally-grounded diabetes prevention program for Latino youth with obesity. We hypothesize that the intervention will lead to increases in self-efficacy and social support, which will mediate long-term changes in insulin sensitivity and QoL-W.
Methods
Study Design
Participants.
Latino youth were recruited through clinical, community, and media outlets. Clinical referral sites included Latino-serving ambulatory pediatric clinics, Federally Qualified Health Centers, school-based health clinics, safety net clinics, and a tertiary care children’s hospital. Community recruitment efforts included health coalitions, health fairs, churches, and community-based organizations. The media strategy used Spanish-language advertisements in local magazines and newspapers. Collectively, these strategies yielded 913 referrals who were screened initially by phone and then in person for the following inclusion criteria: 1) self-identify as Latino, 2) age 14–16, and 3) obese (BMI >95th percentile for age and sex). Exclusion criteria included: 1) taking medication(s) or diagnosed with a condition that influenced carbohydrate metabolism, physical activity (PA), and/or cognition, 2) diagnosed with T2D, 3) enrolled in a weight loss program, or 4) diagnosed with depression or any other condition that may impact quality of life. A total of 160 Latino youth met all inclusion / exclusion criteria and agreed to participate. From this sample, 24 youth were found to have prediabetes and, by protocol, were automatically assigned to the lifestyle intervention arm of the study. Since these youth were not included in the randomization schedule, the current analysis includes 136 Latino youth with obesity who were randomized to either the 3-month lifestyle intervention or comparison control condition (described below).
Procedures.
All study procedures and materials were approved by the Institutional Review Board at Arizona State University. Written informed consent and assent were obtained from parents and youth prior to study procedures. This study is registered at www.clinicaltrials.gov (Clinicaltrials.gov Identifier: NCT02039141) and the protocol has been previously published.19 Data collection was performed in the clinical research unit at Arizona State University by trained research staff using identical procedures as baseline (T1), 3-months (T2), 6-months (T3), and 12-months (T4). Obesity was assessed as BMI and BMI percentiles from height and weight measures and percent fat using bioelectrical impedance analysis.
Primary Outcomes
Diabetes Risk.
A 2-hour 75-gram Oral Glucose Tolerance Test (OGTT) was used to estimate insulin sensitivity using insulin and glucose concentrations collected every 30 minutes. This measure of insulin sensitivity calculates a range from 0–12 with smaller values corresponding to lower levels of insulin sensitivity or higher risk for diabetes.20
Quality of life.
QoL-W was a mean scale calculated from 26-items that measured quality of life in the domains of self, social relationships, and environment as they pertain to weight-related concerns.21 This mean scale has been validated in adolescents in community and clinic settings with Latino youth.21 Examples of questions include, “I feel depressed about how much I weigh;” “Because of my weight other people think I am unattractive;” and “Because of my weight I avoid being seen in a swim suit.” Response categories ranged from (0) “Not at all” to (10) “Very much”21 with higher scores reflecting greater QoL. At T4, quality of life showed good reliability (Cronbach’s α = 0.968).
Mediators
Self-efficacy.
Self-efficacy was assessed using the previously validated Physician-based Assessment & Counseling for Exercise (PACE+): Physical Activity and Diet Surveys for Adolescents.22 This survey assesses participant’s confidence in their ability to change behaviors relating to physical activity (6-items) and fruit, vegetable, and fat intake (18-items), using a 5-point Likert scale with (1) ‘I’m sure I can’t’ to (5) ‘I’m sure I can’ with higher scores indicating greater self-efficacy. This 24-item mean scale included questions like, “Rate how sure you are that you can do physical activity when you feel sad” and “Rate how sure you are that you can choose low-fat foods when you are craving high fat?”23 Self-efficacy had high reliability at both T2 (Cronbach’s α = 0.947) and T3 (Cronbach’s α = 0.937).
Social support.
Social support for physical activity and healthy eating habits was also assessed using the PACE+ Physical Activity and Diet Survey for Adolescents.22 This instrument measures 2 separate mean scales-social support from family (13-items) and social support from friends (9-items). These items ask the frequency with which a family member or friend encourages, participates, or provides assistance (e.g. transportation) for physical activity in a typical week. Response categories for all questions were on a 5-point Likert scale from (1) “never” to (5) “every day” with greater scores indicating greater social support.22 Social support from family members included questions like, “During a typical week, how often has a member of your household provided fruits and vegetables as a snack?” Social support from family members demonstrated good reliability at T2 (Cronbach’s α = 0.904) and T3 (Cronbach’s α = 0.890). An example of friend social support questions include “During a typical week, do your friends tell you that you are doing well in physical activity or sports?” Social support from friends also showed high reliability at T2 (Cronbach’s α = 0.829) and T3 (Cronbach’s α = 0.863).
Group Assignment
Intervention group.
The intervention was delivered to families at a local YMCA by bilingual/bicultural community health educators. The sessions were delivered in both Spanish and English as the majority of the parents preferred communicating in Spanish while the majority of the youth preferred communicating in English. The intervention consisted of nutrition and health education, exercise, and behavior change strategies. The curriculum was informed by the SCT, mainly self-efficacy and social support,19 and was culturally-grounded, integrating Latino cultural values such as familismo (familism) and respeto (respect) into activities and content.19 Self-efficacy was integrated into the curriculum with families participating in weekly goal-setting, self-monitoring, and through mastery experiences such as preparing a meal and exercising together as a family. Intervention implementers provided participants with various forms of social support by discussing roles and responsibilities, skills development for building confidence for making healthy changes in physical activities and dietary behaviors. Social support within and between families was fostered through activities such as discussing how to overcome challenges and barriers to meeting behavior change goals.19 Following the 3-month intervention, youth participated in monthly booster sessions, which were designed to reinforce and celebrate behavior changes, address challenges in maintaining healthy behaviors, and provide ongoing social support and encouragement for behavior change.
Comparison group.
Youth in the comparison group received their lab results and a one-page handout on healthy lifestyle behaviors. Comparison youth also received monthly contact from a research team member and were given a 1-year YMCA membership and the opportunity to participate in an abridged version of the intervention at the conclusion of the study.
Statistical Analyzes
Using Mplus 7.0, sequential multivariate linear regression path analyzes were conducted to examine the direct effects of the intervention on social support and self-efficacy and the indirect, mediation effects of the intervention on insulin sensitivity and quality of life through social support and self-efficacy. Global model fit was assessed using the chi-square goodness of fit statistic, the root mean square error of approximation (RMSEA), and the comparative fit index (CFI). To reduce bias of the parameter estimates, 95% bias corrected confidence intervals were calculated based on 10,000 bootstrap samples. The standardized betas (β) are reported for the direct and indirect paths, and all models control for T1 outcomes of interest, age, and sex. Overall, missingness at T4 was low (19%); nonetheless, to avoid list-wise deletion and maximize available data, we utilized the full-information maximum likelihood (FIML)24 estimation to handle missing data. FIML accounts and adjusts for attrition over time and allows for intent-to-treat analyzes of the data (N = 136).
At each sequential stage, we performed model optimization, trimming non-significant paths. Paths were deemed superfluous if there was no significant contribution to model fit.25 To compare the more complex model to the trimmed parsimonious model, a chi-square difference test was performed.25 A non-significant chi-square difference test indicated the trimmed paths were not contributing to overall model fit and could be omitted from the model without loss of model fit. The process of model optimization aims to find a more parsimonious model that still explains relationships in the data, 6-months post-intervention.
Results
A total of 136 Latino adolescents (14–16 years old) with obesity (BMI% = 98.1 ± 1.4), were randomized to the intervention (n = 67) or comparison (n = 69). Table 1 presents demographic, anthropometric, metabolic, quality of life, self-efficacy, and social support data. There were no significant differences on any of these variables between youth in the intervention and comparison group.
Table 1.
Baseline Participant Characteristics.
| Variable | Control (M ± SD) | Intervention (M ± SD) | P |
|---|---|---|---|
|
| |||
| Age (years) Sex (%) | 15.1 ± 0.9 | 15.4 ± 1.0 | .10 |
| Boys | 50.7% | 40.3% | .22 |
| Girls | 49.3% | 59.7% | |
| County of origin—youth (%) | |||
| U.S-born | 73.9% | 81.8% | .27 |
| Foreign-born | 26.1% | 18.2% | |
| County of origin-parent (%) | |||
| U.S-born | 9.0% | 12.3% | .53 |
| Foreign-born | 91.0% | 87.7% | |
| Body mass index (%) | 98.3 ± 1.2 | 98.1 ± 1.4 | .36 |
| Body fat (%) | 44.7 ± 7.6 | 45.2 ± 7.2 | .67 |
| Insulin sensitivity | 1.6 ± 1.2 | 1.7 ± 1.0 | .60 |
| Weight-specific quality of life | 64.6 ± 25.7 | 63.9 ± 24.0 | .86 |
| Self-efficacy for health behaviors | 3.6 ± 0.8 | 3.8 ± 0.8 | .11 |
| Family social support for health behaviors | 3.0 ± 0.8 | 3.1 ± 0.9 | .56 |
| Friend social support for health behaviors | 2.2 ± 0.8 | 2.3 ± 0.8 | .77 |
The direct effect of the intervention on T2 family social support, friend social support, and self-efficacy are presented in Figure 1. Compared to the comparison group, youth in the intervention group reported significant increases in family (β = 0.33, P < .01) and friend social support for health behaviors (β = 0.22, P < .001) at T2. In contrast, the intervention had no direct effect on self-efficacy for health behaviors (β = 0.05, P > .05) immediately following the intervention. This model exhibited good fit (χ2[11] = 14.18, P = .22; CFI = .986; RMSEA = 0.046). A more parsimonious model that did not include self-efficacy at T2 (χ2[6] = 4.27) indicated that self-efficacy for health behaviors at T2 can be omitted from the model (Δ χ2[5] = 9.91, P = .08).
Figure 1.
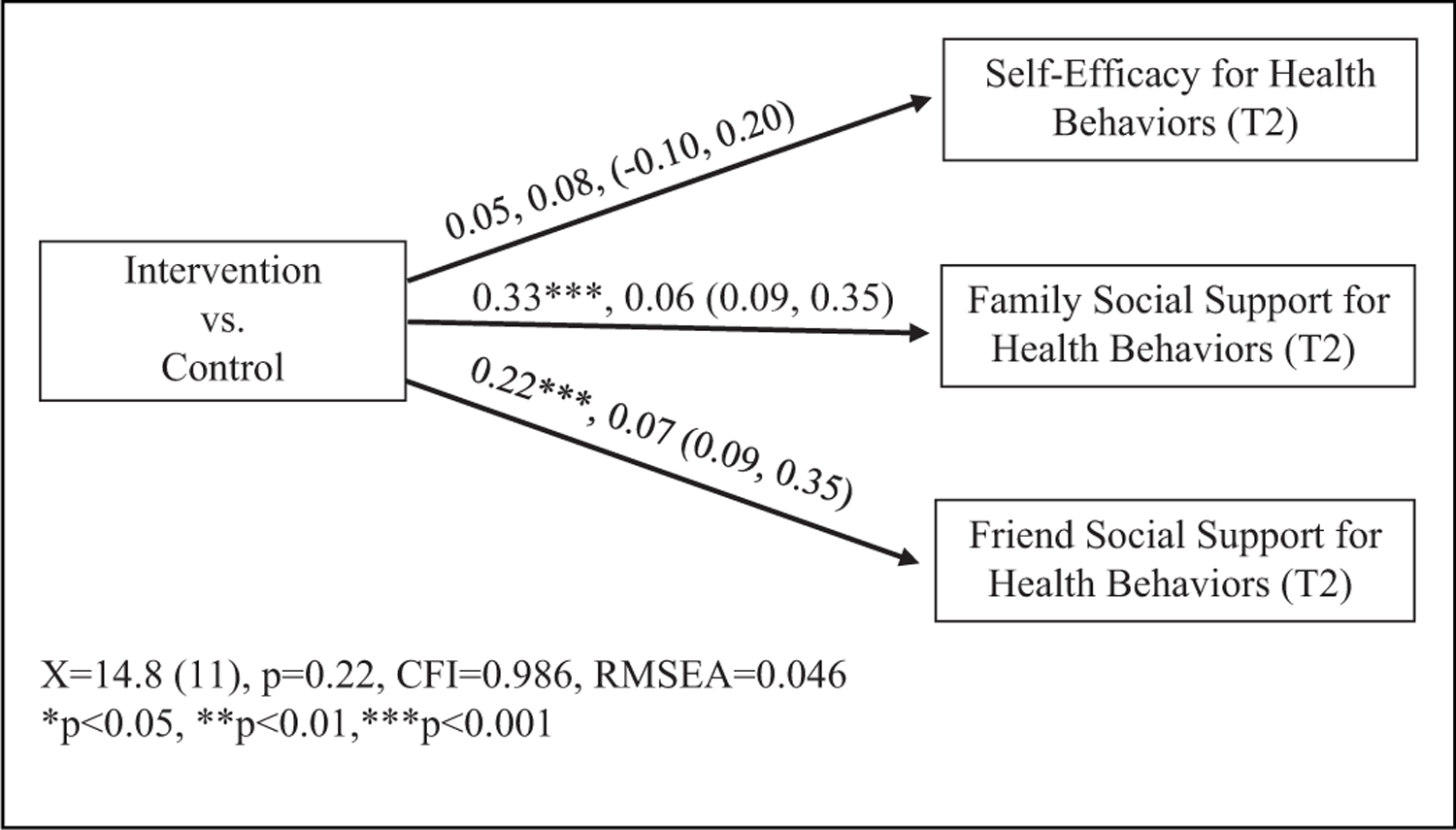
Direct effects of the intervention on self-efficacy for health behaviors and friend and family social support for health behaviors.
A mediation analysis (Figure 2) to test the indirect effect of the intervention on T3 self-efficacy demonstrated that changes in self-efficacy for health behaviors at T3 were mediated by family social support for health behaviors at T2 (β = 0.09, P < .01). In contrast, the indirect path for changes in self-efficacy at T3 mediated through friend social support at T2 was not significant (β = −0.03, P > .05). This revised model exhibited a good fit (χ2[12] = 11.61, P = .48; CFI = 1.00; RMSEA = 0.00). The chi-square difference test indicates that friend social support at T2 could be omitted from the model (Δ χ2[5] = 3.70, P = .59).
Figure 2.
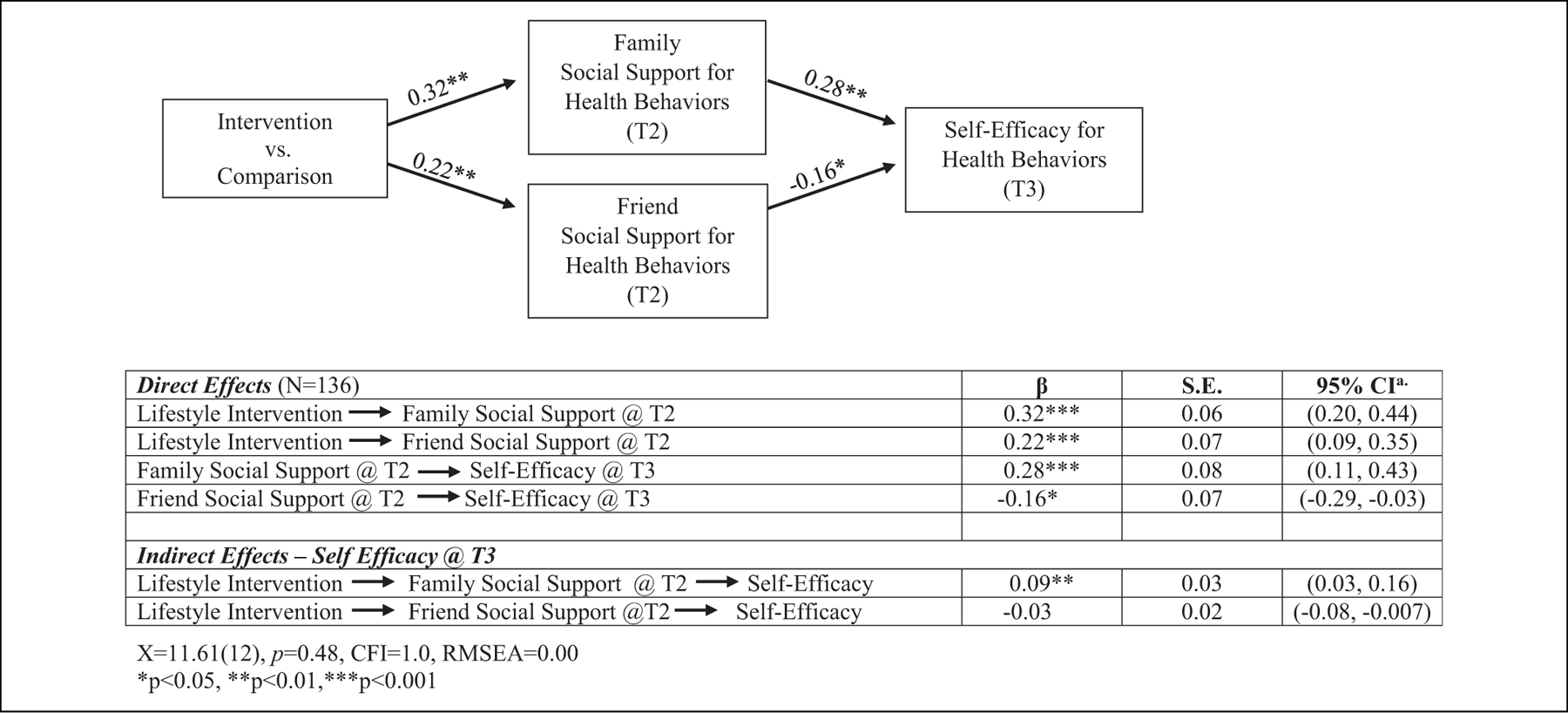
The indirect effect of the intervention on self-efficacy for health behaviors through family and friend social support.
The final model tested direct and indirect effects of the intervention on changes in insulin sensitivity and QoL-W at T4. Although the intervention demonstrated significant direct effects on increasing insulin sensitivity (β = 0.15, P < .05) and QoL-W (β = 0.25, P < .001), there were no mediated pathways through family social support or self-efficacy on insulin sensitivity or QoL-W (P’s > .05) at T4 (Figure 3). This model exhibited a good fit χ2[21] = 15.03, P = .82; CFI = 1 .00; RMSEA = 0.00).
Figure 3.
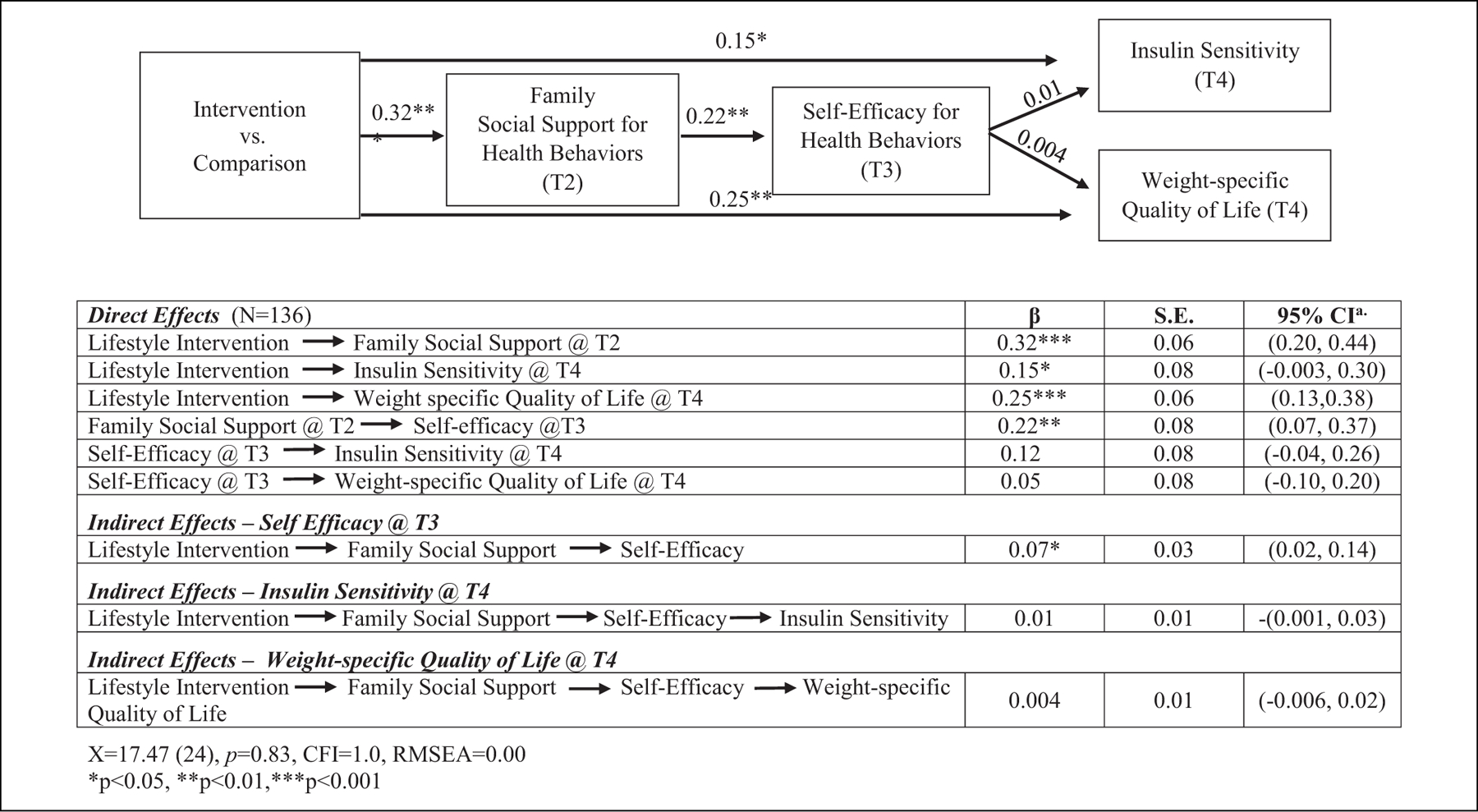
The indirect effect of the intervention on insulin sensitivity (T4) and weight-specific quality of life (T4) through family social support for health behaviors (T2) and self-efficacy for health behaviors (T3).
Discussion
Few studies have tested the mechanisms that underpin successful diabetes prevention interventions. This study tested social support and self-efficacy for healthy behaviors as mediators of long-term changes in insulin sensitivity and QoL-W following a culturally grounded diabetes prevention program. Although the intervention had a direct effect on family and friend social support for health behaviors, neither social support nor self-efficacy mediated improvements in health outcomes. We did observe that family social support increased self-efficacy for health behaviors in high-risk Latino youth, which is in line with SCT and affirms that social support is an important mechanism for fostering self-efficacy in this population. More research is needed to elucidate the role that these theoretical constructs play in mediating long-term changes in metabolic and psychosocial outcomes in youth.
The intervention did not lead to direct improvements in self-efficacy for health behaviors. Previous health promotion and diabetes prevention interventions have reported increased self-efficacy following a lifestyle intervention.26 However, these interventions were focused on individuals whereas the current intervention is family-focused with group-based activities.26 Self-efficacy is an intrapersonal factor used to improve health behavior change at the individual level, which may explain why we did not observe a direct effect of the intervention on self-efficacy.27 While enhancing self-efficacy for healthy eating and physical activity was a behavioral change target in designing the curriculum, the group-based, family-focused nature of the intervention may have limited the intervention’s direct effect on self-efficacy. Our findings are consistent with other group-based physical activity and obesity prevention interventions among adolescents that also report no direct intervention effect on self-efficacy.28–30 In contrast, the intervention significantly improved family and friend social support for health behaviors. These findings are consistent with previous obesity prevention interventions that have reported increases in perceived support from family and friends.31 The intervention enhanced social support within families by delivering content in a family-oriented, collectivist manner, and through activities like team sports and preparing a meal together.19 Fostering a supportive social environment allowed family and peers to serve as role models for one another, build social connections with each other, and share encouragement.32
Interestingly, family social support mediated changes in self-efficacy after the intervention. SCT holds that social processes such as social support can facilitate reciprocal determinism, observational learning, and modeling as mechanisms to increase self-efficacy and, in turn support behavior change.10 Our findings are consistent with multiple studies among youth and young adults that have demonstrated increases in social support contribute to subsequent increases in self-efficacy.33–36 Findings from these studies and ours suggest that there may be a sequential order from enhanced social support to increased self-efficacy and that social support from family may be the pathway by which self-efficacy for health behaviors is increased among Latino adolescents.35 This finding provides novel information about the timing by which theoretical constructs within SCT may operate in this vulnerable, high-risk population.10,35 While increased family social support led to increased self-efficacy, there was no relationship between friend social support and self-efficacy. Previous studies have shown that family social support for health behaviors is more influential in early adolescence compared to late adolescence, which is traditionally marked by a shift in social ties toward friends.37 However, our data suggest that family support remains an important leverage point for enhancing self-efficacy and promoting healthy lifestyle behaviors in Latino youth. Because parental support for health behaviors typically declines during this developmental period,37 enhancing family social support during adolescence is critical, particularly among high-risk Latino youth who report lower levels of family social support for health behaviors compared to Non-Hispanic white youth. Fostering and sustaining family social support represents an important intervention input given that familism is a strong Latino cultural value and that social support is consistently associated with improved dietary habits and physical activity in Latinos.38
It is important to note that while the intervention led to increased family social support, which in turn led to increased self-efficacy, this pathway did not mediate long-term changes in insulin sensitivity or QoL-W. Recent reviews of obesity prevention interventions have reported that there is a lack of evidence supporting theoretical constructs as mediators of intervention effects.39 Using this study as an example, we highlight critical next steps for behavioral interventions to promote the testing of theoretical mediators that guide the intervention. Greater consideration for the operationalization and evaluation of theoretical constructs is needed to adapt and refine constructs so that intervention inputs can be better aligned with intervention strategies.40 In the current study, retrospective intervention mapping revealed that social support was more deeply integrated throughout all intervention components compared to self-efficacy. This may explain why we did not observe a direct intervention effect on self-efficacy. Future iterations of the intervention should improve the operationalization of this construct to ensure that intervention strategies effectively target this mediator to avoid misinterpretations of the effectiveness of theoretical mediators.41
Future studies should also more rigorously evaluate theoretical mediators using formal mediation analyzes to identify the underlying mechanisms by which lifestyle interventions reduce disease outcomes.16 However, for underrepresented populations in particular, this also includes the need for researchers to obtain a deeper understanding of the appropriateness of theoretical mediators within the sociocultural context of the population of interest.42 While our measures of social support and self-efficacy were validated in Latino youth, these validation studies took place before the current sample of youth was born and these measures alone may not fully capture contemporary issues or cultural nuances that influence these relevant constructs within this population. For example, theoretical constructs may be influenced by broader social factors like acculturation or other social determinants experienced by Latino families.43 Thus, the ongoing evaluation and adaptation of mediators should take contemporary issues and broader social influences into consideration. Embedding qualitative and mixed-methods approaches may be helpful in gaining a deeper understanding of theoretical mediators, potential mechanisms, and other important constructs that may be operational within intervention trials.44
In addition to providing a deeper understanding of theoretical mediators, the rich, contextual insight gained from qualitative methods may point to the need to adapt evidence-based interventions to better meet the sociocultural needs of ethnic minority groups. For example, the SCT emphasizes individual and intrapersonal factors as opposed to broader social and environmental variables.10 Health disparities research has shown that individual-level strategies may not be efficacious within vulnerable communities where there is a clear need to leverage social and familial connectedness for health promotion and disease prevention.45 In fact, the most effective strategies for vulnerable, minority populations recognize that health behaviors occur in the context of relationships with family and friends.46 Thus, interventions grounded in the SCT may need to be adapted to account for social and familial factors in order to maximize intervention effectiveness.32 Culturally adapting evidence-based interventions has been identified as a key strategy for addressing health disparities.47 Frameworks like the Ecologic Validity Model provide a systematic process for culturally adapting and rigorously evaluating evidence-based interventions.42 Systematically documenting the adaptation process is critical for evaluating the pathways by which mediators and adapted intervention components interact with and influence biological systems.
Conclusion
Advancing diabetes prevention science focusing on minority youth is particularly urgent considering the growing costs of T2D in the U.S. and the widening disparities among high-risk youth. The recent vision report published by the National Advisory Council on Minority Health and Health Disparities underscored the importance of advancing the knowledge base for effective disease prevention interventions and the mechanisms by which these interventions affect disease outcomes.46 Therefore, the purpose of this study was to test self-efficacy and friend and family social support for healthy eating and physical activity as mediators of long-term changes in diabetes risk and QoL-W following a culturally-grounded diabetes prevention program for Latino youth. While social support and self-efficacy did not mediate long-term changes in insulin sensitivity or QoL-W, our findings suggest that family support plays an important role in the context of health promotion and disease prevention for Latino youth. Coordinated efforts to enhance social support within and between high-risk families living in vulnerable and underserved communities is an important framework and potential mechanism to increase the efficacy and effect size of prevention programs that aim to advance health equity.
So What?
What is already known on this topic?
Latino youth and families are disproportionately impacted by type 2 diabetes. Interventions that are theoretically-driven are a first-line approach for diabetes prevention. The Social Cognitive Theory (SCT) has been widely applied and associated with improved health behaviors.
What does this article add?
This study examined SCT constructs (social support and self-efficacy) as mediators of diabetes related outcomes in Latino youth following a lifestyle intervention. SCT constructs did not mediate long-term outcomes; however, increased family social support led to increased self-efficacy, suggesting social support may be needed to increase self-efficacy.
What are the implications for health promotion practice or research?
Fostering family social support for health behaviors is a critical intervention target for diabetes prevention programs in high-risk Latino youth. More research is needed to understand theoretical constructs like family-level social factors and their mediating role on disease outcomes in Latino families.
Acknowledgments
We are grateful to our collaborators from the Family Wellness Program at the St. Vincent de Paul Medical and Dental Clinic and the Valley of the Sun YMCA. We are indebted to the children and families who participated in this study.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the National Institutes of Health through the National Institute on Minority Health and Health Disparities (P20MD002316; U54MD002316) and the National Institute on Diabetes and Digestive and Kidney Diseases (R01DK107579). This work is also a publication of the United States Department of Agriculture, Agricultural Research Service (USDA/ARS), Children’s Nutrition Research Center, Department of Pediatrics, Baylor College of Medicine, Houston, Texas, and funded in part with federal funds from the USDA/ARS under Cooperative Agreement No. 58-3092-0-001.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA. 2015;314(10):1021–1029. [DOI] [PubMed] [Google Scholar]
- 2.Menke A, Casagrande S, Cowie CC. Prevalence of diabetes in adolescents aged 12 to 19 years in the United States, 2005–2014. JAMA. 2016;316(3):344–345. [DOI] [PubMed] [Google Scholar]
- 3.Rhodes ET, Goran MI, Lieu TA, et al. Health-related quality of life in adolescents with or at risk for type 2 diabetes mellitus. J Pediatr. 2012;160(6):911–917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Contento IR, Koch PA, Lee H, Calabrese-Barton A. Adolescents demonstrate improvement in obesity risk behaviors after completion of choice, control & change, a curriculum addressing personal agency and autonomous motivation. J Am Diet Assoc. 2010; 110(12):1830–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bandura A Social cognitive theory of self-regulation. Organ Behav Hum Decis Process. 1991;50(2):248–287. [Google Scholar]
- 6.Donnelly R, Springer A. Parental social support, ethnicity, and energy balance-related behaviors in ethnically diverse, low-income, urban elementary schoolchildren. J Nutr Educ Behav. 2015;47(1):10–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thompson RA, Flood MF, Goodvin R. Social support and developmental psychopathology. In: Cicchetti D, Cohen DJ, eds. Developmental Psychopathology: Volume Three: Risk, Disorder, and Adaptation. John Wiley & Sons; 2006:1–37. [Google Scholar]
- 8.Nelson EE, Leibenluft E, McClure EB, Pine DS. The social reorientation of adolescence: a neuroscience perspective on the process and its relation to psychopathology. Psychol Med. 2005; 35(2):163–174. [DOI] [PubMed] [Google Scholar]
- 9.Hu J, Amirehsani KA, Wallace DC, McCoy TP, Silva Z. A family-based, culturally tailored diabetes intervention for Hispanics and their family members. Diabetes Educ. 2016; 42(3):299–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bandura A Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. [DOI] [PubMed] [Google Scholar]
- 11.Bandura A Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. [DOI] [PubMed] [Google Scholar]
- 12.Welk GJ, Almeida J, Morss G. Laboratory calibration and validation of the Biotrainer and Actitrac activity monitors. Med Sci Sports Exerc. 2003;35(6):1057–1064. [DOI] [PubMed] [Google Scholar]
- 13.Dishman RK, Saunders RP, Motl RW, Dowda M, Pate RR. Self-efficacy moderates the relation between declines in physical activity and perceived social support in high school girls. J Pediatr Psychol. 2009;34(4):441–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franks PW, Huang TT, Ball GD. Lifestyle intervention for type 2 diabetes risk reduction: using the diabetes prevention program to inform new directions in pediatric research. Can J Diabetes. 2007;31(3):242–251. [Google Scholar]
- 16.Katzmarzyk PT, Baur LA, Blair SN, et al. International conference on physical activity and obesity in children: summary statement and recommendations. Int J Pediatr Obes. 2008; 3(1):3–21. [DOI] [PubMed] [Google Scholar]
- 17.Bowen PG, Clay OJ, Lee LT, Vice J, Ovalle F, Crowe M. Associations of social support and self-efficacy with quality of life in older adults with diabetes. J Gerontol Nurs. 2015;41(12): 21–29; quiz 30–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soltero EG, Olson ML, Williams AN, et al. Effects of a community-based diabetes prevention program for Latino youth with obesity: a randomized controlled trial. Obesity (Silver Spring). 2018;26(12):1856–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams AN, Konopken YP, Keller CS, et al. Culturally-grounded diabetes prevention program for obese Latino youth: rationale, design, and methods. Contemp Clin Trials. 2017;54: 68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22(9):1462–1470. [DOI] [PubMed] [Google Scholar]
- 21.Patrick DL, Skalicky AM, Edwards TC, et al. Weight loss and changes in generic and weight-specific quality of life in obese adolescents. Qual Life Res. 2011;20(6):961–968. [DOI] [PubMed] [Google Scholar]
- 22.Norman GJ, Sallis JF, Gaskins R. Comparability and reliability of paper- and computer-based measures of psychosocial constructs for adolescent physical activity and sedentary behaviors. Res Q Exerc Sport. 2005;76(3):315–323. [DOI] [PubMed] [Google Scholar]
- 23.Hagler AS, Norman GJ, Radick LR, Calfas KJ, Sallis JF. Comparability and reliability of paper- and computer-based measures of psychosocial constructs for adolescent fruit and vegetable and dietary fat intake. J Am Diet Assoc. 2005; 105(11):1758–1764. [DOI] [PubMed] [Google Scholar]
- 24.Graham JW. Missing data analysis: making it work in the real world. Ann Rev Psychol. 2009;60:549–576. [DOI] [PubMed] [Google Scholar]
- 25.Kline RB. Principles and Practice of Structural Equation Modeling. The Guilford Press; 1998. [Google Scholar]
- 26.Geria K, Beitz JM. Application of a modified diabetes prevention program with adolescents. Public Health Nurs. 2018;35(4): 337–343. [DOI] [PubMed] [Google Scholar]
- 27.Jurkowski JM, Lawson HA, Green Mills LL, Wilner PG III, Davison KK. The empowerment of low-income parents engaged in a childhood obesity intervention. Fam Community Health. 2014;37(2):104–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lubans DR, Morgan PJ, Callister R, Collins CE, Plotnikoff RC. Exploring the mechanisms of physical activity and dietary behavior change in the program x intervention for adolescents. J Adolesc Health. 2010;47(1):83–91. [DOI] [PubMed] [Google Scholar]
- 29.van Stralen MM, Yildirim M, te Velde SJ, et al. What works in school-based energy balance behaviour interventions and what does not? A systematic review of mediating mechanisms. Int J Obes (Lond). 2011;35(10):1251–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wieland ML, Biggs BK, Brockman TA, et al. Club fit: development of a physical activity and healthy eating intervention at a boys & girls club after school program. J Prim Prev. 2020;41(2): 153–170. [DOI] [PubMed] [Google Scholar]
- 31.Mendonça G, Cheng LA, Mélo EN, de Farias Júnior JC. Physical activity and social support in adolescents: a systematic review. Health Educ Res. 2014;29(5):822–839. [DOI] [PubMed] [Google Scholar]
- 32.Huang TT, Goran MI. Prevention of type 2 diabetes in young people: a theoretical perspective. Pediatr Diabetes. 2003; 4(1):38–56. [DOI] [PubMed] [Google Scholar]
- 33.Wang Y, Hager ER, Magder LS, Arbaiza R, Wilkes S, Black MM. A dyadic analysis on source discrepancy and a mediation analysis via self-efficacy in the parental support and physical activity relationship among black girls. Child Obes. 2019;15(2):123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trost SG, Sallis JF, Pate RR, Freedson PS, Taylor WC, Dowda M. Evaluating a model of parental influence on youth physical activity. Am J Prev Med. 2003;25(4):277–282. [DOI] [PubMed] [Google Scholar]
- 35.Rovniak LS, Anderson ES, Winett RA, Stephens RS. Social cognitive determinants of physical activity in young adults: a prospective structural equation analysis. Ann Behav Med. 2002; 24(2):149–156. [DOI] [PubMed] [Google Scholar]
- 36.Middelweerd A, te Velde SJ, Abbott G, Timperio A, Brug J, Ball K. Do intrapersonal factors mediate the association of social support with physical activity in young women living in socioeconomically disadvantaged neighbourhoods? A longitudinal mediation analysis. PLoS One. 2017;12(3):e0173231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davison KK, Jago R. Change in parent and peer support across ages 9 to 15yr and adolescent girls’ physical activity. Med Sci Sports Exerc. 2009;41(9):1816–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marquez B, Elder JP, Arredondo EM, Madanat H, Ji M, Ayala GX. Social network characteristics associated with health promoting behaviors among Latinos. Health Psychol. 2014;33(6): 544–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bagherniya M, Taghipour A, Sharma M, et al. Obesity intervention programs among adolescents using social cognitive theory: a systematic literature review. Health Educ Res. 2018;33(1):26–39. [DOI] [PubMed] [Google Scholar]
- 40.Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol. 2008;57(4):660–680. [Google Scholar]
- 41.Cerin E, Barnett A, Baranowski T. Testing theories of dietary behavior change in youth using the mediating variable model with intervention programs. J Nutr Educ Behav. 2009;41(5): 309–318. [DOI] [PubMed] [Google Scholar]
- 42.Bernal G, Sáez-Santiago E. Culturally centered psychosocial interventions. J Community Psychol. 2006;34(2):121–132. [Google Scholar]
- 43.Castro FG, Barrera M Jr, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence-based interventions. Annu Rev Clin Psychol. 2010;6:213–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 5th ed. Sage Publications, Inc.; 2017. [Google Scholar]
- 45.Kennedy L, Pinkney S, Suleman S, Mâsse LC, Naylor PJ, Amed S. Propagating change: using RE-FRAME to scale and sustain a community-based childhood obesity prevention initiative. Int J Environ Res Public Health. 2019;16(5):736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alvidrez J, Stinson N Jr. Sideways progress in intervention research is not sufficient to eliminate health disparities. Am J Public Health. 2019;109(S1):S102–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jones NL, Breen N, Das R, Farhat T, Palmer R. Cross-cutting themes to advance the science of minority health and health disparities. Am J Public Health. 2019;109(S1):S21–s24. [DOI] [PMC free article] [PubMed] [Google Scholar]


