Abstract
Acute exacerbations of psychosis have been reported with COVID-19 infection and medications used for its treatment. Terms “psychosis”, “psychotic”, “COVID-19″ and “coronavirus” were searched on “PubMed” and “GOOGLE SCHOLAR”, yielding 84 articles. 14 case reports were selected based on pre-defined criteria and analyzed. Among selected articles,10 attributed psychosis to COVID-19 infection. In 3 articles, psychosis was diagnosed despite concurrent delirium. In 8 and 3 articles respectively, a clear temporal demarcation of psychosis and COVID-19 infection and steroid use was not described. Psychosis can occur secondary to GMC, or exposure to medication. Due process should be followed to ascertain the same.
Introduction
Neurotropic coronavirus infection is associated with numerous neurological and neuropsychiatric manifestations. Such presentations before, during and after the infection have been reported. Among these presentations, acute exacerbations of psychosis have been reportedly linked with COVID-19 infection and medications used for its treatment.
Methodology
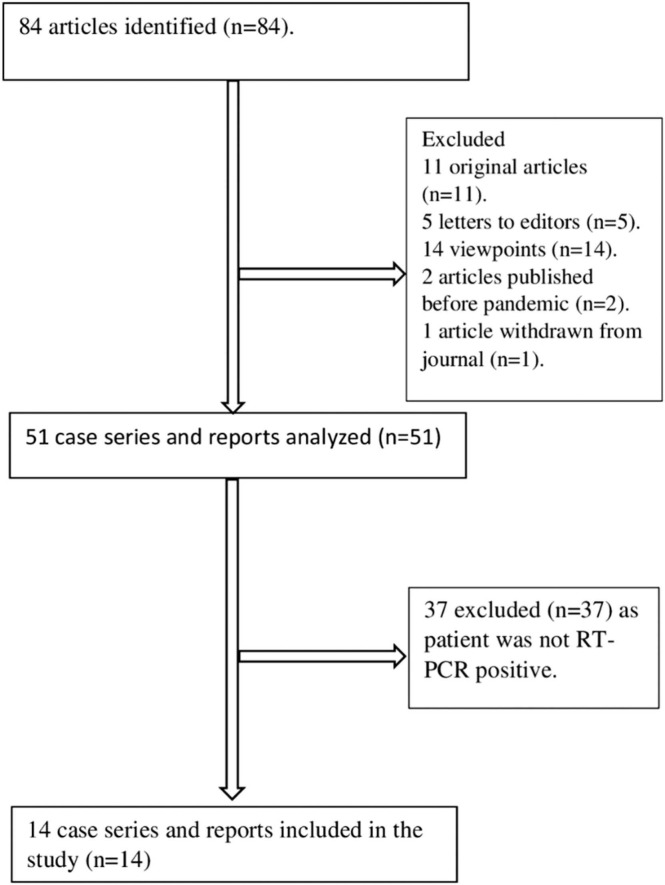
Search engines “PubMed” AND “GOOGLE SCHOLAR” were searched using specific search terms during June 2021. Out of 84 articles that came up, we selected 14 articles based on pre-determined inclusion and exclusion criteria. Selected articles were analysed and discussed in the departmental journal club.
Results
In 10 articles, diagnosis of psychosis was attributed to COVID-19 infection. In 3 of those articles, despite reporting concurrent delirium like presentation, diagnosis was still reported as psychosis. In 8 articles, the temporal correlation between onset of psychosis, onset of COVID-19 was not clearly demarcated. In 3 articles, clear demarcation between psychosis associated with steroid use and with a general medical condition (COVID-19) was not clearly presented. Only 2 articles did mention using a structured diagnostic system. In patients (3/17) with prior history of psychiatric illness, diagnosis was reported as relapse of psychosis (2/17), without specifying the criteria used for diagnosing a relapse.
Conclusion
Acute exacerbation of psychosis can occur secondary to a general medical condition (GMC), or after exposure to a medication. However, due process should be followed to ascertain that the psychosis is indeed secondary to a GMC, or a medication, and not a de-novo presentation, or delirium.
Keywords: Covid-19, Psychosis, Review
1. Introduction
Coronaviruses have been linked to neuropsychiatric manifestations during and after the infection (Lahiri and Ardila, 2020; Ellul et al., 2020; Niazkar et al., 2020; Rehman et al., 2021; Rentero et al., 2021; Hyland et al., 2020; Kozloff et al., 2020; Bodnar et al., 2021). Immunological mechanisms, COVID-19 treatment, cognitive impairment, poor psychosocial functioning, pre-existing psychiatric or neurological disorder and adverse geopolitical situations due to the pandemic were hypothesized to be causally associated with presentations of psychosis (Bodnar et al., 2021).
Here we present discussions, deliberations and observations at a departmental journal club, focussing on scientific literature reporting psychosis in patients diagnosed with COVID-19.
2. Methodology
We searched ‘PubMed’ and ‘GOOGLE SCHOLAR’ from June 1st-15th 2021 with keywords “COVID 19″, “CORONAVIRUS”, “PSYCHOSIS”, “PSYCHOTIC”. Fig. 1.
Fig. 1.
Procedure of data extraction.
All the articles relevant to the study, as per inclusion and exclusion criteria, were taken up and analysed. Concerns with regards to reporting psychosis in COVID-19 pandemic were highlighted.
3. Results and discussion
We used the guidelines and criteria mentioned in DSM-5 (American Psychiatric Association et al., 2013) for psychotic disorders due to other medical conditions, and judged (Supplementary Table 1) whether there exist with psychosis;.
-
1.
A temporal relationship after COVID-19 infection.
-
2.
Symptoms that are atypical in nature and course.
-
3.
A possible link with a medication/substance of abuse.
-
4.
a pathophysiological relationship with COVID-19 infection.
In most articles the title hinted at a link between psychosis and COVID 19 (Hansen et al., 2020 Jun 1, Parker et al., 2021, Alba et al., 2021, Noone et al., 2020, Kozato et al., 2021, Smith et al., 2020, Lim et al., 2020, Lanier et al., 2020, Majadas et al., 2020,Correa-Palacio et al., 2020). Two articles suggested a possible role of quarantine in onset of psychosis (Sanchez et al., 2020; Baral et al., 2021). Psychosis was reported in some articles as the presenting feature of COVID-19, (Parker et al., 2021, Noone et al., 2020, Lanier et al., 2020; Correea et al., 2020; Ferrando et al., 2020; Saje et al., 2021), whereas, some reported psychosis as a neuropsychiatric manifestation following symptoms of COVID-19 (Hansen et al., 2020 Jun 1, Alba et al., 2021, Noone et al., 2020, Kozato et al., 2021, Smith et al., 2020, Lim et al., 2020, Majadas et al., 2020 Baral et al., 2020).
3.1. Observation 1: establishment of temporal association
To diagnose psychosis due to a general medical condition, a temporal association between the two has to be established. We found articles that mentioned psychosis as the presenting feature of COVID-19 (Parker et al., 2021; Noone et al., 2020b; Lanier et al., 2020; Correa-Placio et al., 2020; Ferrando et al.; Saje et al., 2021).
Eight (Hansen et al., 2020; Alba et al., 2021; Noone et al., 2020a; Kozato et al., 2021; Smith et al., 2020; Lim et al., 2020; Majadas et al., 2020; Baral et al., 2021) have reported COVID-19 like illness prior to onset of psychotic symptoms. Eight have not shared the details regarding duration passed between a positive RT PCR swab and onset of psychosis (Sanchez et al., 2020; Parker et al., 2021; Kozato et al., 2021; Lanier et al., 2020; Majadas et al., 2020; Correa- et al. 2020; Ferrando et al., 2020; Saje et al., 2021).
The stressors in workplace/life and infections, metabolic imbalances, chronic debilitating diseases act as psychological stressors and hence precipitate psychosis (Phillips et al., 2007 Apr 1, Corcoran et al., 2003 Jan 1). Loss of livelihood, separation from loved ones during mandated quarantine can trigger psychosis in vulnerable individuals (Martin et al., 2021). Also, hallucinations, delusions might predispose patients to disregard COVID-19 safety protocols (American Psychiatric Association et al., 2013; Valdés-Florido et al., 2020). Thus, it is questionable what came first, the infection or the psychosis, while reporting such clinical phenomena.
3.2. Observation 2: presence/absence of atypical symptoms
Atypical symptoms such as, hallucinations (other than auditory) and delusions with themes like somatic, grandiose, religious and persecutory (American Psychiatric Association et al., 2013), points towards diagnosis of psychosis due to another medical condition. Most articles have reported this specific symptom profile except two (Alba et al., 2021; Lanier et al., 2020).
Atypical age at onset, is one of the guidelines for considering psychosis due to another medical condition (American Psychiatric Association et al., 2013). In this study, mean age at onset of psychotic episodes was above 40 years, which is within the second of the bimodal peaks of schizophrenia onset (Sham et al., 1994). Psychotic disorders show a marked prevalence between 15 and 17 years (American Psychiatric Association et al., 2013; Kessler et al., 2007, World Health Organization et al., 2004), higher age at onset can be atypical for onset of psychosis.
3.2.1. Observation 3: presence of psychosis due to general medical condition, or Substance/Medication Induced Psychotic Disorder
Use of steroids is a mainstay of treatment in severe COVID- 19. (Mølhave et al., 2021). It is known to cause psychosis (American Psychiatric Association et al., 2013), which manifest within one to two weeks of initiation (Kenna et al., 2011). Three articles mentioned the use of steroids in treatment of COVID-19, without mentioning dose, and duration of time between initiation of steroids and onset of COVID-19 (Kozato et al., 2021; Majadas et al., 2021; Correa et al., 2020).
Incidence of psychiatric symptoms with steroid use averages to about 28% (Lewis et al., 1983). Increasing doses of prednisone (> 40 mg) and dexamethasone (>15 mg) are associated with increased psychosis (Lewis et al., 1983; Janes et al., 2019). Overall, psychiatric manifestations can occur early in the course of treatment or even after cessation of the drug (Lewis et al., 1983). Various routes of administration have shown variable incidences of psychosis, with parenteral routes showing the most (Janes et al., 2019; Upadhyaya and James, 2019).
Antivirals are also reported to cause psychosis (Caubet et al., 2011).
Hence, while reporting psychosis due to another medical condition, background treatment modalities and their side effect profiles should be considered.
3.3. Observation 4: establishment of pathophysiological relation- Inflammatory markers
Patients with COVID-19 have raised inflammatory markers such as D-dimer, CRP, BUN, IL-6 (Parker et al., 2021, ICMR COVID 19 National Task Force). Five articles did not give details about inflammatory markers (Hansen et al., 2020; Sanchez et al., 2020; Alba et al., 2021; Correa-Palacio et al., 2020; Saje et al., 2021), while in others, inflammatory markers were within normal limits (Noone et al., 2020; Kozato et a, 2021; Smith et al., 2021, Lim et al., 2021). Among inflammatory markers, CRP was most often raised (Majadas et al., 2020; Ferrando et al., 2020; Baral et al., 2021) followed by BUN (Parker et al., 2021).
Inflammatory markers such as IL-1 beta, IL-6 and growth factors like GF beta can be raised during acute exacerbations in schizophrenia (Kirkpatrick et al., 2013). Stress due to infections or metabolic instability can also raise inflammatory markers and cytokines (Marsland et al., 2017). Further, remission of psychosis is accompanied by reduction in level of inflammatory markers (Haring et al., 2015). Fluvoxamine, an antidepressant gained a brief spotlight during the pandemic and it was hypothesized that fluvoxamine, due to its activation of S1R-IRE1 pathway, reduced the inflammatory markers, thus alleviating symptoms of COVID-19 (Lenze et al., 2020). It may therefore be prudent to consider that, inflammatory markers, though elevated in acute infections, can also be elevated in psychiatric disorders themselves.
3.4. Observation 5: diagnosis attributed to delirium or psychosis?
Three reports stated that patients had signs and symptoms of delirium in concurrence with psychosis (Noone et al., 2020a; Lim et al., 2020, Majadas et al., 2020), yet all 3 reported the diagnosis as psychosis. In one, a patient admitted in an ICU reported behavioural symptoms, with fluctuating orientation, yet the diagnosis reported was psychosis (Kozato et al., 2021).
The criteria for diagnosing delirium include disturbance of awareness, change in baseline cognition and a fluctuating course (American Psychiatric Association et al., 2013). Despite the occurrence of delusions and hallucinations in both delirium and psychosis, the differentiating feature is the background of clear consciousness in psychosis. (American Psychiatric Association, & American Psychiatric Association, 2013, World Health Organization, 2004 Dec 31). COVID-19 patients admitted in isolation or in the ICU can experience sensory deprivation. This, along with multitudes of medications used in treatment and their interactions may predispose patients to delirium or more often sub-syndromal delirium, which can be overlooked or missed (Sepulveda et al., 2017). Thus, there is a possibility of delirium masking or masquerading as psychosis in COVID-19 infection.
3.5. Observation 6: miscellaneous
One article reported case of an adult male with pre-existing schizoaffective disorder, on a maintenance dose of clozapine, who presented with psychosis during mandated quarantine after a febrile illness (Sanchez et al., 2020). It was reported as a relapse of psychosis. However, schizoaffective disorder require coexistence of either depressive or manic episode with core symptoms of schizophrenia for at least a month (American Psychiatric Association et al., 2013), which was not fulfilled in the clinical presentation described. In the same report, details about whether clozapine was discontinued, or down-titrated during the febrile illness were not mentioned. This history is relevant, since high grade fever (101 F) in a patient taking clozapine warrants investigations to rule out agranulocytosis, or Neuroleptic Malignant Syndrome (NMS) (Karagianis et al., 1999). These can mimic symptoms of COVID-19 and the following psychotic episode could have been due to, reduction/discontinuation of clozapine, or physical/psychological burden of febrile illness.
In some articles, chronic and severe metabolic, infectious and degenerative disorders were reported during the clinical work-up, such as hepatic encephalopathy, Lewy Body Dementia and Toxoplasmosis (Parker et al., 2021). All these can present with behavioural disturbances or delirium caused by the disease process, yet, the diagnosis was reported as psychosis due to COVID-19.
There is handful literature that explained these issues previously (Dinakaran et al., 2020; Megahed et al., 2020; Ashrafi et al., 2020; Banerjee et al., 2020). This article highlights important concerns about reporting a clinical phenomenon occurring concurrently with another comorbid illness. This is perhaps the first such effort in this domain. It is vital for scientific writers not to engage in the age old fallacy; Event X happened after Event Y; therefore, Event Y must have caused Event X!.
In any review of a scientific database, first thing one gets to see are the titles of manuscripts (Dewan and Gupta, 2016; Chapnick et al., 2019; Andrade et al., 2011), and then the abstracts. Hence, it is important that they reflect what the manuscript reports in detail. Heightened emotions and fear among masses are a part and parcel of any pandemic, especially when the causative factor is unknown and thus, over-representation and hype from misleading titles can deviate research from their imperative goal (Boutron et al., 2018).
This manuscript also has some limitations. Due to heterogeneity in design, we limited our research only to case reports and series and excluded randomised trials and observational studies. Since our search was conducted in the month of June 2021, articles published on later dates might have employed a more exploratory and indirect approach in reporting this clinical phenomenon.
4. Conclusion
Patients with COVID-19 can present with psychosis or other psychiatric symptoms at any stage of the infection. However, it is important to differentiate the presentations as, (1) de novo presentation of psychosis, (2) psychosis due to psychological or physiological burden of COVID-19, (3) psychosis due to various geopolitical changes associated with the pandemic, (4) psychosis as a consequence of various medications used in treatment of COVID-19 and (5) delirium.
All ethical guidelines were followed thoroughly during this research and respective authors for each article were cited appropriately.
Financial disclosure
The authors hereby declare that there is no financial disagreement among authors and the project is self-financed.
Conflict of interest
There is no conflict of interest from any authors.
Acknowledgements
Department of Psychiatry, DY Patil Medical College Hospital and Research Institute, Kolhapur.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ajp.2022.103099.
Appendix A. Supporting information
Supplementary material
References
- American Psychiatric Association, & American Psychiatric Association, 2013, Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, VA.
- Alba L., Coll C., Sáez S., Alonso L., Pérez H., Palma S., Ortiz S. New-onset Psychosis: A case report of brief psychosis related to COVID-19 infection. Psychiatry Res. 2021 doi: 10.1016/j.psychres.2021.113975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashrafi M.R., Azizimalamiri R., Badv R.S., Tavasoli A.R., Nikkhah A., Montazerlotfelahi H., Heidari M. Coronavirus, its neurologic manifestations, and complications. Iran. J. Pediatr. 2020;30(2):1–4. [Google Scholar]
- Andrade C. How to write a good abstract for a scientific paper or conference presentation. Indian J. Psychiatry. 2011;53(2):172. doi: 10.4103/0019-5545.82558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee D., Viswanath B. Neuropsychiatric manifestations of COVID-19 and possible pathogenic mechanisms: insights from other coronaviruses. Asian J. Psychiatry. 2020;54 doi: 10.1016/j.ajp.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral N., Adhikari G., Karki S., Champine A., Sud P. Does social stigma and neglect post-COVID-19 matter? A case report on brief psychotic disorder Post-COVID-19 and self-quarantine. Cureus. 2021;13:1. doi: 10.7759/cureus.12973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodnar B., Patel K., Ho W., Luo J.J., Hu W. Cellular mechanisms underlying Neurological/neuropsychiatric manifestations of COVID‐19. J. Med. Virol. 2021;93(4):1983–1998. doi: 10.1002/jmv.26720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutron I., Ravaud P. Misrepresentation and distortion of research in biomedical literature. Proc. Natl. Acad. Sci. 2018;115(11) doi: 10.1073/pnas.1710755115. 2613-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caubet J.V., Garrido O.B., Mayor M.M., Fuentenebro J.S. Acyclovir-induced psychosis with manic symptoms after treating adult chickenpox. Eur. Psychiatry. 2011;26(S2) 894-894. [Google Scholar]
- Chapnick, J.D., 2019, The abstract and title page.
- Corcoran C., Walker E., Huot R., Mittal V., Tessner K., Kestler L., Malaspina D. The stress cascade and schizophrenia: etiology and onset. Schizophr. Bull. 2003 1;29(4):671–679. doi: 10.1093/oxfordjournals.schbul.a007038. [DOI] [PubMed] [Google Scholar]
- Correa-Palacio A.F., Hernandez-Huerta D., Gómez-Arnau J., Loeck C., Caballero I. Affective psychosis after COVID-19 infection in a previously healthy patient: a case report. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewan P., Gupta P. Writing the title, abstract and introduction: Looks matter! Indian Pediatr. 2016;53(3):235–241. doi: 10.1007/s13312-016-0827-y. [DOI] [PubMed] [Google Scholar]
- Dinakaran D., Manjunatha N., Kumar C.N., Suresh B.M. Neuropsychiatric aspects of COVID-19 pandemic: A selective review. Asian J. Psychiatry. 2020;53 doi: 10.1016/j.ajp.2020.102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellul M.A., Benjamin L., Singh B., Lant S., Michael B.D., Easton A., Kneen R., Defres S., Sejvar J., Solomon T. Neurological associations of COVID-19. Lancet Neurol. 2020 doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrando S.J., Klepacz L., Lynch S., Tavakkoli M., Dornbush R., Baharani R., Bartell A. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? Psychosomatics. 2020;61(5):551. doi: 10.1016/j.psym.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen D.H., Baandrup L., Hageman I. COVID-19 associated severe psychotic relapse. Ugeskrift. 2020;182:24. [PubMed] [Google Scholar]
- Haring L., Koido K., Vasar V., Leping V., Zilmer K., Zilmer M., Vasar E. Antipsychotic treatment reduces psychotic symptoms and markers of low-grade inflammation in first episode psychosis patients, but increases their body mass index. Schizophr. Res. 2015;169(1–3):22–29. doi: 10.1016/j.schres.2015.08.027. [DOI] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Vallières F. Anxiety and depression in the Republic of Ireland during the COVID‐19 pandemic. Acta Psychiatr. Scand. 2020;142(3):249–256. doi: 10.1111/acps.13219. [DOI] [PubMed] [Google Scholar]
- Janes M., Kuster S., Goldson T.M., Forjuoh S.N. Vol. 32. Taylor & Francis,; 2019. October). Steroid-induced psychosis. pp. 614–615. (Baylor University Medical Center Proceedings). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick B., Miller B.J. Inflammation and schizophrenia. Schizophr. Bull. 2013;39(6):1174–1179. doi: 10.1093/schbul/sbt141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozato N., Mishra M., Firdosi M. New-onset psychosis due to COVID-19. BMJ Case Rep. CP. 2021;14(4) doi: 10.1136/bcr-2021-242538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozloff N., Mulsant B.H., Stergiopoulos V., Voineskos A.N. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr. Bull. 2020;46(4):752–757. doi: 10.1093/schbul/sbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenna H.A., Poon A.W., de los Angeles, C P., Koran L.M. Psychiatric complications of treatment with corticosteroids: review with case report. Psychiatry Clin. Neurosci. 2011;65(6):549–560. doi: 10.1111/j.1440-1819.2011.02260.x. [DOI] [PubMed] [Google Scholar]
- Karagianis J.L., Phillips L.C., Hogan K.P., LeDrew K.K. Clozapine-associated neuroleptic malignant syndrome: two new cases and a review of the literature. Ann. Pharmacother. 1999;33(5):623–630. doi: 10.1345/aph.18286. [DOI] [PubMed] [Google Scholar]
- Kessler R.C., Amminger G.P., Aguilar‐Gaxiola S., Alonso J., Lee S., Ustun T.B. Age of onset of mental disorders: a review of recent literature. Curr. Opin. Psychiatry. 2007;20(4):359. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahiri D., Ardila A. COVID-19 pandemic: a neurological perspective. Cureus. 2020;12:4. doi: 10.7759/cureus.7889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier C.G., Lewis S.A., Patel P.D., Ahmed A.M., Lewis P.O. An unusual case of COVID-19 presenting as acute psychosis. J. Pharm. Pract. 2020 doi: 10.1177/0897190020977721. [DOI] [PubMed] [Google Scholar]
- Lenze E.J., Mattar C., Zorumski C.F., Stevens A., Schweiger J., Nicol G.E., Reiersen A.M. Fluvoxamine vs placebo and clinical deterioration in outpatients with symptomatic COVID-19: a randomized clinical trial. Jama. 2020;324(22):2292–2300. doi: 10.1001/jama.2020.22760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis D.A., Smith R.E. Steroid-induced psychiatric syndromes: a report of 14 cases and a review of the literature. J. Affect. Disord. 1983;5(4):319–332. doi: 10.1016/0165-0327(83)90022-8. [DOI] [PubMed] [Google Scholar]
- Lim S.T., Janaway B., Costello H., Trip A., Price G. Persistent psychotic symptoms following COVID-19 infection. BJPsych Open. 2020;6(5) doi: 10.1192/bjo.2020.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majadas Susan, et al. “A case with psychotic disorder as a clinical presentation of COVID‐19.”. Psychiatry Clin. Neurosci. 2020 doi: 10.1111/pcn.13107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsland A.L., Walsh C., Lockwood K., John-Henderson N.A. The effects of acute psychological stress on circulating and stimulated inflammatory markers: a systematic review and meta-analysis. Brain, Behav., Immun. 2017;64:208–219. doi: 10.1016/j.bbi.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C., Andrés P., Bullón A., Villegas J.L., de la Iglesia-Larrad J.I., Bote B., Roncero C. COVID pandemic as an opportunity for improving mental health treatments of the homeless people. Int. J. Soc. Psychiatry. 2021:67. doi: 10.1177/0020764020950770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Megahed N.A., Ghoneim E.M. Antivirus-built environment: Lessons learned from Covid-19 pandemic. Sustain. Cities Soc. 2020;61 doi: 10.1016/j.scs.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mølhave M. June). Clinical Management of COVID-19 Patients-An Update. In. Semin. Nucl. Med. 2021 doi: 10.1053/j.semnuclmed.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niazkar H.R., Zibaee B., Nasimi A., Bahri N. The neurological manifestations of COVID-19: a review Article. Neurol. Sci. 2020;Jul;41 doi: 10.1007/s10072-020-04486-3. 1667-71.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noone R., Cabassa J.A., Gardner L., Schwartz B., Alpert J.E., Gabbay V., editors. Vol. 130. 2020. Letter to the Editor: New onset psychosis and mania following COVID-19 infection; p. 177. (Journal of Psychiatric Research). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker C., Slan A., Shalev D., Critchfield A. Abrupt late-onset psychosis as a presentation of coronavirus 2019 disease (COVID-19): a longitudinal case report. J. Psychiatr. Pract. 2021;27(2):131. doi: 10.1097/PRA.0000000000000533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips L.J., Francey S.M., Edwards J., McMurray N. Stress and psychosis: towards the development of new models of investigation. Clin. Psychol. Rev. 2007;27(3):307–317. doi: 10.1016/j.cpr.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Rehman U., Shahnawaz M.G., Khan N.H., Kharshiing K.D., Khursheed M., Gupta K., Kashyap D., Uniyal R. Depression, anxiety and stress among Indians in times of Covid-19 lockdown. Community Ment. J. 2021;57(1):42–48. doi: 10.1007/s10597-020-00664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentero D., Juanes A., Losada C.P., Álvarez S., Parra A., Santana V., Martí I., Urricelqui J. New-onset Psychosis in COVID-19 pandemic: a case series in Madrid. Psychiatry Res. 2021;290 doi: 10.1016/j.psychres.2020.113097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Alonso S., Ovejero S., Barrigon M.L., Baca-Garcia E. Psychotic relapse from COVID-19 quarantine, a case report. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C.M., Komisar J.R., Mourad A., Kincaid B.R. COVID-19-associated brief psychotic disorder. BMJ Case Rep. CP. 2020;13(8) doi: 10.1136/bcr-2020-236940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saje M., Prebil K., Plesnicar B.K. Time for lessons from the first wave of SARS-CoV-2 epidemic. A case report of a patient with acute psychosis and COVID19 and later virus reactivation. The. Eur. J. Psychiatry. 2021;35(3):197–199. doi: 10.1016/j.ejpsy.2020.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sham P.C., MacLean C.J., Kendler K.S. A typological model of schizophrenia based on age at onset, sex and familial morbidity. Acta Psychiatr. Scand. 1994;89(2):135–141. doi: 10.1111/j.1600-0447.1994.tb01501.x. [DOI] [PubMed] [Google Scholar]
- Sepulveda E., Leonard M., Franco J.G., Adamis D., McCarthy G., Dunne C., Meagher D.J. Subsyndromal delirium compared with delirium, dementia, and subjects without delirium or dementia in elderly general hospital admissions and nursing home residents. Alzheimer’s Dement.: Diagn., Assess. Dis. Monit. 2017;7:1–10. doi: 10.1016/j.dadm.2016.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Upadhyaya M., James M. Topical triamcinolone-induced psychosis. Am. J. Psychiatry Residents’ J. 2019;14(4):4–5. [Google Scholar]
- Valdés-Florido M.J., López-Díaz Á., Palermo-Zeballos F.J., Martínez-Molina I., Martín-Gil V.E., Crespo-Facorro B., Ruiz-Veguilla M. Reactive psychoses in the context of the COVID-19 pandemic: clinical perspectives from a case series. Rev. De. Psiquiatr. Salud Ment. 2020;13(2):90–94. doi: 10.1016/j.rpsm.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Volume 1. World Health Organization,; 2004. The International Statistical Classification of Diseases and Health Related Problems. ICD 10: Tenth Revision. (Tabular List). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material