Abstract
Background:
Adverse childhood experiences (ACEs) are a public health crisis, affecting nearly half of children in the United States. Long-term effects of ACEs on psychological well-being, engagement in risk behaviors, and physical health have been observed. Moreover, many individuals exposed to ACEs are also affected by an accumulation of stressors due to broader structural inequities.
Objective:
The current study examined heterogeneity in patterns of ACEs, explored how these patterns varied based on race, gender, and socioeconomic status, and assessed how ACE patterns were associated with physical health, mental health, and risk-related outcomes in adulthood.
Participants:
Drawing on the Add Health dataset, survey data from Waves I, III, IV (n = 12,288) was analyzed. Mean age of participants was 28.3 (SD = 1.9), more than half were female (54.4%), and a little less than half identified as youth of color (46.7%).
Method:
Multigroup latent class analysis explored heterogeneity in ACE exposure and variations based on structural inequity. Latent class regression assessed associations between ACE classes and outcomes.
Results:
A four-class solution was identified. Class sizes and latent structures differed by gender. Among males and females, the low adversity class had more positive outcomes compared to all classes, while the childhood maltreatment and high adversity/community violence classes engaged in more risk-related behaviors. Among females, the childhood maltreatment class had worse physical health outcomes. Very small to medium effects were observed.
Conclusion:
Findings highlight the importance of examining heterogeneity in ACE exposure, and how patterns of ACEs may differentially affect outcomes in adulthood.
Background
Adverse childhood experiences (ACEs) are potentially traumatic events an individual may be exposed to during childhood (Felitti et al., 1998). While the ACE framework has brought attention to the harmful effects of childhood adversity on well-being, several critiques of this framework have been noted. A primary critique is that the ACE framework fails to recognize other sources of stress that emerge from oppressive social contexts that may account for adversity exposure in disadvantaged populations and give rise to continuity of exposure to stressful events throughout the lifespan (Bateson et al., 2020; Finkelhor et al., 2015). Acknowledging these additional sources of hardship is important considering that lack of access to resources likely contributes to youth’s ability to physically and psychologically respond to environmental stressors (e.g., Metzler et al., 2017). Additionally, the use of an overall ACE count does not acknowledge the differential impact of various types of adverse experiences. Several recent studies have taken a person-centered approach to examine patterns of ACEs and have found a childhood maltreatment class, a household dysfunction/caregiver absence class, and low adversity class across different samples (e.g., Cavanaugh et al., 2015; Lacey et al., 2020; Lee et al., 2020; Merians et al., 2019; Shin et al., 2018). Across these studies, the low ACE class has typically demonstrated more positive psychological, physical, and risk-related outcomes compared to the childhood maltreatment class, with fewer differences seen compared to the household dysfunction/caregiver absence class, highlighting the need to further explore how heterogeneity in ACEs may differentially impact youth.
Research has highlighted the impairing physiological and psychosocial consequences that may result from ACE exposure (e.g., Kim et al., 2013; Marusak et al., 2015; Wilson et al., 2012). Considering the substantial disruptions to development of areas of the brain responsible for regulatory processes (Kim et al., 2013), children exposed to adversity often have difficulties with emotion regulation (e.g., Cloitre et al., 2008; Ehring & Quack, 2010), as well as behavioral and psychological health issues (Nelson et al., 2020). Moreover, given the significant impact of early adversity on immune functioning (Elwenspoek et al., 2017), associations between ACE exposure and severe physical health problems in adulthood have also been noted (Baker et al., 2009; Kalmakis & Chandler, 2015). However, when interpreting these associations, it is important to consider that adversity may emerge out of oppressive contexts which facilitate continued chronic stress exposure and other negative outcomes.
Cumulative inequality theory highlights how oppressive systems perpetuate inequality and maintain adversity exposure and negative effects of stress across the lifespan (e.g., Ferraro & Shippee, 2009; Hughes et al., 2017; Nurius et al., 2012; Schafer et al., 2011). This theory emphasizes the importance of considering broader social contexts, such as inequity related to race, gender, and SES, that may produce differences in opportunities and access to resources and increased exposure to adversity, which in turn affect life trajectories in terms of health and well-being (Dannefer, 2003; Ferraro et al., 2016; Jackson, 2015). Thus, it is important to examine relationships between forms of adversity and structural inequities, defined as the systemic disadvantages experienced by individuals from groups impacted by social risk factors related to race, ethnicity, gender, class, as well as other domains (National Academies of Sciences, Engineering, and Medicine, 2017).
Miller and colleagues’ (2011) theoretical model of childhood adversity focuses on the impact of stress related to structural inequities as well as forms of childhood maltreatment on both behavioral and biological outcomes. Their model indicates that people who face more adversity in childhood, due to structural inequities and/or maltreatment, are more likely to experience stress in adulthood. Walsh and colleagues (2019) systematic review supports these findings, highlighting how youth who grow up in a lower socioeconomic position are at greater risk for exposure to adversity during childhood. Umberson and colleagues (2014, 2016) went further to build on Miller et al.’s (2011) model and examine the role of race in the context of adversity exposure. Their work highlighted how Black children are disproportionately exposed to higher levels of adversity, are more vulnerable to the impact of adversity on relationships in adulthood, and experience greater accumulation of additional daily life stressors in terms of racism and discrimination, all of which foster social isolation, conflict, and limit access to resources that are typically available through social ties (e.g., Umberson et al., 2014; Umberson et al. 2016; Slopen et al., 2015). Kim and Drake (2018) found racial differences in maltreatment rates, though disparities in maltreatment rates based on race were no longer significant when controlling for SES. These findings suggest that accumulation of structural inequities related to poverty may account for differences in exposure to maltreatment. Thus, more research is needed examining patterns of adversity exposure, looking at how different forms of adversity may influence individual health and well-being, as well as how structural inequities may account for differences in adversity exposure.
One recent study also examined how ACE classes may vary when considering race, with findings indicating differences in proportions of youth within each class and configural differences in ACE classes (Maguire-Jack et al. 2019). Specifically, White youth had lower exposure to ACEs and lower total number of ACEs compared to Latinx and Black youth. Examination of the latent class structure within the full sample and separately for each racial group also showed structural differences in the classes, such that Black and Latinx youth were more likely to experience neighborhood violence, racial discrimination, and parental incarceration, while White youth were more likely to have a parent with substance use problems. As noted by the authors, exposure to discrimination and neighborhood violence, and increased rates of parental incarceration are linked to racial inequities that perpetuate harm and cause continued stress and exposure to youth of color. Therefore, these findings highlight the need to examine how structural inequities related to race may impact the types of ACEs to which youth are exposed.
Moreover, ACE studies have shown variation in patterns of risk and psychological symptomatology based on gender (e.g., Cavanagh et al., 2015; Garrazza et al., 2011; Haahr-Pederson et al., 2020; Walrath et al., 2004). Walrath et al. (2004) used latent class analysis to identify risk classes based on gender and found that while similar patterns of risk were observed (low-risk, status-offense, abuse, high-risk), the proportions of girls and boys in each class varied, with fewer girls being in the low-risk class and fewer boys in the abuse and high-risk classes. Adding to this work, Garrazza and colleagues (2011) found the same patterns of risk and noted that there were more girls in the high-risk class as compared to boy, as well as differences in the probability of endorsing risk items. Cavanaugh and colleagues (2015) looked at associations between classes of ACEs and mental and substance use disorders. They found that while patterns were similar across genders, classes of mental health differed such that females were more likely to experience internalizing disorders while males were more likely to experience externalizing disorders. Additionally, Haahr-Pederson et al., (2020) saw both configural and structural differences in ACE class between males and females, such that males only had a low adversity and mixed adversity class, while females had a four-class solution consistent with past work examining ACE patterns. However, across genders, those in the low adversity class demonstrated more positive socioemotional and psychological wellbeing.
Looking at socioeconomic differences, Wolff and colleagues (2018) identified differences in ACE exposure for youth involved in the juvenile justice system when considering concentrated disadvantage and affluence, measured by variables including living below the poverty line, family income, female-headed households, unemployment rates, high school degree, and receipt of public assistance. Findings demonstrated that concentrated disadvantage was positively associated with a high adversity class, greater family violence and household incarceration, but less physical and sexual abuse.
While recent studies have examined class differences based on race, gender, and socioeconomic status (e.g., Cavanaugh et al., 2015; Haahr-Pederson et al., 2020; Maguire-Jack et al., 2020; Wolff et al., 2018), these studies did not test for measurement equivalence using constrained versus unconstrained models, and instead ran latent class analyses within groups separately. Building on this previous research, this study aimed to examine heterogeneity in ACE patterns, how these patterns may vary based on structural inequities, and associations between different types of ACEs psychological, risk-related, and physical health outcomes in adulthood. To investigate these research questions, secondary data analysis was conducted using de-identified data from the Add Health dataset.
Method
Participants completed surveys at and in-home interviews that covered a range of topics including health, relationships, behaviors, and academic and vocational outcomes. Wave I collected data from youth between ages 11 and 21 during 1994–1995. Wave II involved in-home interviews with youth in 1996, with all participants being eligible aside from those who graduated in 1995 (n = 14,738). Wave III collected data from all eligible participants between 2001 to 2002 (n = 15,197) who were anywhere from 18 to 28 years old. Between 2008 to 2009, Wave IV was collected data from participants who were ages 24 to 34 (n = 15,701). All participants included in the Add Health dataset will be included in secondary data analysis. This study was determined exempt by the Suffolk University Institutional Review Board.
Participants
The dataset includes information from a nationally representative sample of 80 high schools and 52 middle schools from the United States. The sample includes 20,745 participants, with four waves of data including information from participants during childhood and adulthood and caregivers. The current study utilizes data collected from children and their caregivers during Waves I, III, and IV. Following Add Health guidelines to best preserve the nationally representative nature of the sample, participants without valid sample weights were excluded from analyses (n = 8,457).
Measures
Adverse childhood experiences (Waves I, III, and IV).
Twelve binary indicators were used to identify whether or not participants had been exposed to adversity during childhood. Items were consistent with those used by Lee and colleagues (2020), including supervisory neglect, emotional neglect, physical abuse, emotional abuse, sexual abuse, suicide attempt of household adult, parental alcohol abuse, parental separation/divorce, incarceration of household adult, experience in the foster care system, witnessing of violence, and exposure to violence.
Psychological Outcomes (Wave IV)
Psychological Outcomes (Wave IV) included a binary item reflecting a lifetime mental health diagnosis, as well as continuous scales assessing depression, anxiety, and stress.
Depression
Depression was assessed with five items rated on a four-point Likert scale assessing frequency of experiencing symptoms of depression during the past seven days. Sample items included: “You were bothered by things that usually don’t bother you” and “You could not shake off the blues, even with help from your family and your friends”. The scale demonstrated acceptable reliability (alpha = .79).
Anxiety
Anxiety was assessed with four items rated on a five-point Likert scale assessing how much participants agreed with statements reflecting symptoms of anxiety “as you generally are now”. Sample items included: “I worry about things” and “I get stressed out easily”. The scale demonstrated acceptable reliability (alpha = .70).
Stress
Stress was assessed with four items rated on a five-point Likert scale from the Perceived Stress Scale (Cohen et al., 1994) asking participants “In the last 30 days, how often have you…” with sample items including “…felt that you were unable to control the important things in your life?” and “…felt that difficulties were piling up so high that you could not overcome them?” The scale demonstrated acceptable reliability (alpha = .72).
Risk-Related Outcomes (Wave IV)
Risk-Related Outcomes (Wave IV) included binary items reflecting engagement of non-violent behaviors, engagement in violent behaviors, and diagnosis of a sexually transmitted illness (STI) within the past 12 months, as well as recent alcohol-related difficulties.
Physical Health Outcomes (Wave IV)
Physical Health Outcomes (Wave IV) included binary items representing engagement in health-related help-seeking behavior, having a lifetime physical health diagnosis, and having high blood pressure, as well as continuous measures of body mass index (BMI), waist circumference, and C-reactive protein and Epstein-Barr Virus as biomarkers of stress and inflammation.
Structural Inequities (Wave I)
Structural Inequities (Wave I) were assessed with various demographic measures. Participant race/ethnicity was assessed with questions asking, “What is your race?” and “Are you of Hispanic or Latino origin?” For the purposes of the multigroup latent class analyses (LCA), individuals were recoded into categories of White, non-Black person of color, and Black. Participant gender was identified by interviewers who were asked to confirm participants’ sex, which was coded as male, female, refused or don’t know. Challenges with this approach to measuring both race and gender are discussed in the limitations section. A binary indicator of childhood socioeconomic disadvantage was based on items from Wave I, including family income and receipt of public assistance (following recommendations from Raposa et al., 2018). Family income was assessed with the following question: “How much income, before taxes, did your family receive in [past year]? Include your own income, the income of everyone else in your household, and income from welfare benefits, dividends, and all other sources.” Given that there were no items asking about number of household dependents, family income below the poverty line was based on the average poverty line threshold between 1994 and 1995 for a two person household including one person under the age of 65 ($10,118), collected from the US census data (https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html). This number was rounded up to the nearest 1,000. Receipt of public assistance included the following forms: Social Security or Railroad Retirement, Supplemental Security Income, Aid to Families with Dependent Children, food stamps, unemployment or worker’s compensations, or a housing subsidy or public housing. Individuals with reports of family income below the federal poverty line, receiving any of the aforementioned forms public assistance, or neighborhood poverty will be coded as experiencing economic disadvantage.
Potential covariates (Waves I, IV).
Potential covariates (Waves I, IV). Race and current socioeconomic status (SES) were used as covariates in path analyses. Current SES was assessed with questions asking participants to share whether they or anyone in their household had received any public assistance, welfare payments, or food stamps since the time of the last interview. Participants were also asked to indicate whether in the last 12 months there was a time when they were unable to pay for phone service, rent or mortgage, household bills, or were concerned about food running out before they could get money to buy more. Participants who received public assistance, welfare payments, food stamps, or were unable to pay for bills or basic needs within the last 12 months were coded as lacking current socioeconomic stability.
Data Analysis
Data management, descriptive statistics, and normality were conducted in SPSS version 25.0 (IBM Corp., 1985–2017) and Mplus version 8.2 (Muthén & Muthén, 2012–2018). Normality for continuous variables was assessed with skew and kurtosis. Longitudinal sampling weights for participants at waves I, III, and IV (GSWGT134) were used to compensate for oversampling and adjust for bias, allowing for representation of the population as much as possible.
Given that multistage sampling was used, clustered observations of data were collected. Moreover, while the survey was probability-based, certain groups were oversampled, thus not all people had equal probability of selection. Of the 26,666 high schools in the United States sorted by size, school type, region, location, and percent White, a sample of 132 schools was chosen. Thus, school was used as a cluster identifier (the primary sampling unit). Oversampled subgroups included high SES Black, Cuban, Puerto Rican, and Chinese adolescents, youth with disabilities, half siblings, and unrelated individuals in the same household. Sixteen schools were selected which accommodated such oversampling. While the Add Health sampling plan did not include a stratification variable, post-stratification adjustments to sampling weights were necessary so that region of country could be used as post-stratification variable (Chen, 2018). To account for these aspects of the complex survey design, design-based modeling was employed. School ID was accounted for as a clustering variable and region was included as the post-stratification variable in all analyses. Design-based models are used when relations of variables within clusters (i.e. schools) are not of interest. Adjusted sampling variances can be obtained taking into account sampling design as opposed to modeling the sampling design (Stapleton, 2020). No time-varying covariates were included in the model. Missing data was managed using full information maximum likelihood estimation with robust standard errors (MLR). This was the chosen estimator given that it is robust to non-normality when doing complex modeling.
Odds ratios and standardized beta coefficients are reported as measures of effect size for direct effects. Interpretation of effect sizes for odds ratios were OR < 1.68 is very small, OR < 3.47 is small, 3.47 ≤ OR < 6.71 is medium, OR ≥ 6.71 is large (Chen et al., 2010). Cutoffs for magnitude of beta coefficients for direct effects were β < .2 is small, .2 ≤ β < .5 is medium, and β ≥ .5 is large (Acock, 2014).
LCA was employed to identify underlying latent classes of ACEs using 12 binary indicators. Model fit indices were used to determine which classes would be retained including: Akaike Information Criteria (AIC; Akaike, 1981), Bayesian Information Criteria (BIC; Schwarz, 1978), Sample-Size Adjusted BIC (SSA-BIC; Sclove, 1987), and the Vuong-Lo-Mendell-Rubin likelihood ratio test (VLMR; Lo et al., 2001). Lower values on the AIC, BIC, and SSA-BIC are indicative of better model fit (Vermunt, 2010). Several studies have shown that the BIC and SSA-BIC perform far better than the AIC, entropy statistics, and VLMR for model selection, particularly with large sample sizes (Nylund et al. 2007; Padgett & Tipton, 2020; Weller et al. 2020). Entropy statistics were evaluated to determine the accuracy of group classification, with higher entropy statistic scores reflecting better class separation (Lanza et al., 2013) and values > 0.80 suggest a highly discriminating model though entropy should not be favored for selecting the number of classes as it is not a reliable method for selecting classes (Tein et al., 2013). Significance of VLMR reflect whether the model with k latent classes is a better fit to than a model with k -1 classes (Nylund et al., 2007). Other criteria were assessed as needed, such as removal of solutions containing classes with a small proportion of the sample, as these may present challenges related to interpretability and replication of findings (Lanza et al., 2013). However, there are no consistent guidelines on determining class sizes and recent publications have included class sizes containing less than five percent of the sample (see review by O’Donnell et al., 2017), assuming the small class sizes conceptually makes sense and substantively contributes to data interpretation (Weller et al., 2020).
Multigroup LCA was then be used to compare the latent structure of item responses between multiple groups. For the purposes of this study, this procedure tested whether class structures could be considered the same based on differences in gender (male or female), SES (low or high), and race (non-Hispanic White, non-Black people of color [Hispanic, American Indian, Native American, Asian, Pacific Islander, Other], and non-Hispanic Black). The number of classes were kept the same in these models, however models were rerun either unconstrained (where probabilities and class proportions are free to vary), semiconstrained (where probabilities are constrained to be equal, but class proportions are free to vary), and fully constrained (where the probabilities and class proportions are constrained to be equal across groups). In these models, if the semiconstrained model fits better than the unconstrained model, this supports the assumption of measurement equivalence (i.e., the structure of the latent classes does not differ based on group). If the fully constrained model fits better than the semiconstrained model, this suggests that there are no differences by group in class size. Comparisons of model fit for unconstrained, semiconstrained, and fully constrained models were done using BIC and SSA-BIC values. Results were used to inform the inclusion of various covariates in the model, and subsequent analyses were run for each class and group depending on whether differences emerge when considering broader structural contexts.
Finally, logistic regressions, in which the outcome variable is categorical, and linear regressions, in which the outcome variable is continuous, were used to understand the association between ACE classes and outcomes in adulthood. Analyses were run using maximum likelihood estimation (MLR) with numerical integration, the recommended approach for models with a combination of categorical observed variables and continuous latent variables. Monte Carlo integration was necessary given that the model had more than three dimensions of integration. This method uses random resampling procedures to estimate the standard errors for coefficients (Muthén & Muthén, 2012–2018). Models were run with all outcome variables included to reduce the number of tests and therefore number of Type I errors. The low adversity class was first included as the reference condition, though comparisons among all classes were examined.
Results
Descriptive Statistics
The final analytical sample included participants who had valid survey weights from Waves I, III, and IV in-home interview data (n = 12,288). Mean age of participants was 28.3 (SD = 1.9) and approximately 54.4% were female. Racial/ethnic identification of participants included 53.7% non-Hispanic White, 20.3% non-Hispanic Black, 15.6% Hispanic, 7.3% Asian or Pacific Islander, and 3.5% American Indian. Rates of adversity exposure were as follows: approximately 8.0% of the sample had been exposed to sexual abuse, 34.9% had been exposed to physical abuse, 46.5% had been exposed to emotional abuse, 38.0% had experienced supervisory neglect, 7.7% had experienced emotional neglect, 6.5% had a family member who attempted suicide, 12.7% had a caregiver who struggled with alcohol abuse, 23.6% had caregivers who were separated or unmarried, 17.4% had a caregiver who was incarcerated, 2.3% had lived in foster care, 5.2% had witnessed violence in the community, and 6.3% had directly experienced violence in the community.
Single-group LCA
The model fit for the one to seven class solutions for the entire sample are shared in Table 1. Results show that compared to a two-class and three-class solutions, the four-class solution had lower AIC, BIC, and SSA-BIC values, and higher entropy. While the five-class, six-class, and seven-class solutions had lower AIC, BIC, and SSA-BIC, entropy values for these classes were lower and one of the classes included less than 5% of the sample. Considering both model fit, substantive interpretability, and consistency with previous findings (e.g., Lee et al., 2020), the four-class solution was chosen as the best model for the data. Class labels were given based on previous studies (Cavanaugh et al., 2015; Lee et al., 2020; Merians et al., 2019) and were named based on the type of ACEs that had the highest proportions for that class, though as described below, some ACE categories were seen at moderate levels within other classes.
Table 1.
Full sample latent class analysis model fit
| Model | AIC | BIC | Sample Size-Adjusted BIC | Entropy | VLMRT p-value |
|---|---|---|---|---|---|
| 2-class | 107161.19 | 107346.60 | 107267.15 | 0.58 | .000 |
| 3-class | 106239.11 | 106520.93 | 106400.17 | 0.63 | .003 |
| 4-class | 105596.54 | 105974.77 | 105812.70 | 0.69 | .228 |
| 5-class | 105240.77 | 105715.41 | 105512.03 | 0.65 | .126 |
| 6-class | 105108.42 | 105679.47 | 105434.77 | 0.67 | .433 |
| 7-class | 105026.19 | 105693.65 | 105407.64 | 0.68 | .730 |
The first class included 23.1% of the sample (n = 2833) and was labeled the ‘childhood maltreatment’ class, with higher proportions of physical abuse, emotional abuse, and supervisory neglect compared to all other classes. The second class included 13.4% of the sample (n = 1643) and was labeled the ‘caregiver absence’ class, with higher proportions of caregiver alcohol misuse, caregiver separation or divorce, and caregiver incarceration, and moderate levels of physical abuse, emotional abuse, and supervisory neglect (labeled household dysfunction in previous studies [e.g., Lee et al., 2020]). The third class included 2.8% of the sample (n = 346) and was labeled the ‘community violence’ class, characterized by high proportions of witnessing and directly experiencing community violence, as well as moderate rates of physical abuse, emotional abuse, supervisory neglect, caregiver separation or divorce, and caregiver incarceration. Finally, the fourth class, including 60.7% of the sample (n = 7464), was labeled the ‘low adversity’ class, with low rates of adversity overall.
Multigroup LCA
The four-class solution chosen for the entire sample was further explored to see whether the same latent structures and class sizes held across various demographic characteristics representing structural inequities. BIC values for the multigroup models were compared to assess model fit (Nylund et al., 2007), and chi-square difference tests were conducted to compare nested models (Eid et al., 2003).
Gender.
Multigroup LCA models were examined for females and males. Models were rerun for females and males separately to determine if there were the same number of classes in each group. Model fit indices based on lower BIC values supported a four-class solution for both females and males. Class structures generally identified a childhood maltreatment class, a caregiver absence class, and a low adversity class, however, for males a community violence class emerged, while for females the fourth class represented a high adversity class, with notably higher proportions of childhood maltreatment including sexual abuse, physical abuse, emotional abuse, supervisory neglect, emotional neglect, as well as higher proportions of caregiver absence including caregiver separation or divorce and caregiver incarceration.
As the next step, a multigroup LCA was estimated with both males and females included in the same model. The separate models indicated a four-class solution was appropriate for both samples, and based on the separate models, it was apparent that there were fundamental differences in exposure to community violence based on gender. Given the clear variation in adversity exposure across genders, there was no need to run fully constrained model. Thus, the multigroup LCA was run unconstrained and semiconstrained. When comparing the BIC across the unconstrained and semiconstrained models, the unconstrained model had a lower BIC value. Moreover, the Chi-square difference test was significant (ΔS-Bχ2 = 160.70, p < .001), suggesting that the unconstrained model was better fitting than the semiconstrained model. Therefore, the unconstrained model was chosen, suggesting that latent class prevalence and conditional probabilities of ACEs differed between females and males. Consistent with the original model, the first class was representative of the ‘childhood maltreatment class’ and included 21.1% of females (n = 1411) and 25.9% of males (n = 1454). The second class was characteristic of the ‘caregiver absence’ class and included 14.2% of females (n = 946) and 8.3% of males (n = 468). The third class was similar to the original ‘community violence’ class for males but represented a generally ‘high adversity’ class for females with low proportions of community violence, including 8.5% of females (n = 570) and 6.6% of males (n = 368). Finally, the fourth class was the ‘low adversity’ class which include 56.2% of females (n = 3755) and 59.1% of males (n = 3314). Figures 1a and 1b present class probabilities for the female and male samples separately.
Figure 1.
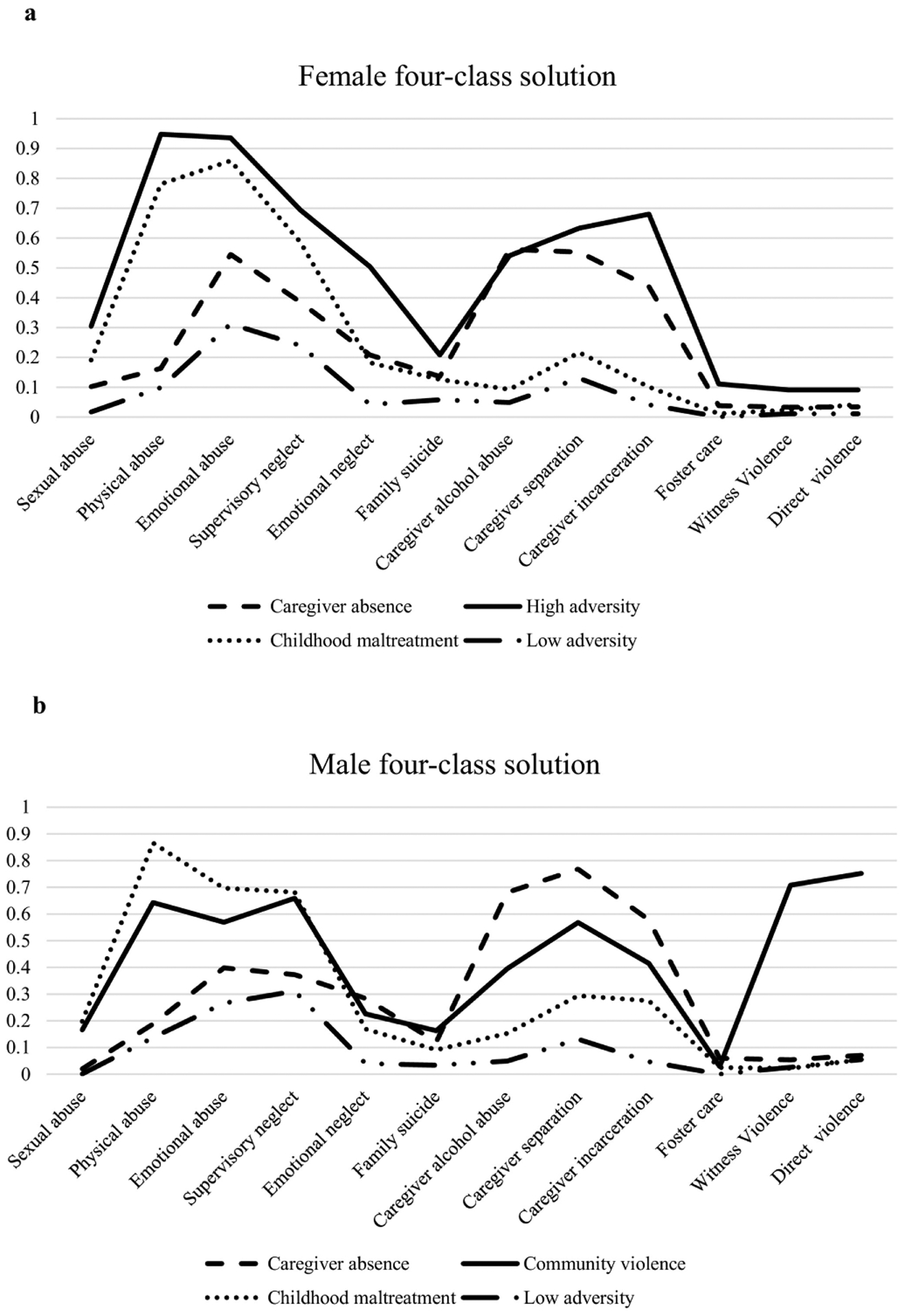
a. Four-class solution (female sample). b. Four-class solution (male sample).
Socioeconomic status.
Multigroup LCA models were then estimated for individuals who experience socioeconomic disadvantage and those with socioeconomic stability. Latent class models were run separately for both groups. The four-class solution was identified as the best fit for both models based on lower BIC values compared to the two-class solution and three-class solutions, though in both groups one class comprised less than 5% of the sample. Measurement invariance between groups was assessed by comparing unconstrained, semiconstrained, and fully constrained models. The semiconstrained model and fully constrained models had lower BIC values compared to the unconstrained model. While the semiconstrained model had a lower BIC value compared to the fully constrained model, the Chi-square difference test was non-significant (ΔS-Bχ2 = 5.07, p = .407), suggesting that the semiconstrained model was not necessarily better fitting than the fully constrained model. Thus, measurement equivalence could be assumed for both probabilities and class sizes. The four-class solution was consistent with the original model, with a childhood maltreatment class including 23.5% of socioeconomically disadvantaged youth (n = 1006) and 24.1% of socioeconomically stable youth (n = 1378), a caregiver absence class, including 16.0% of socioeconomically disadvantaged youth (n = 686) and 14.6% of socioeconomically stable youth (n = 834), a community violence class including 3.9% of socioeconomically disadvantaged youth (n = 168) and 4.5% of socioeconomically stable youth (n = 256), and a low adversity class including 56.6% of socioeconomically disadvantaged youth (n = 2428) and 56.8% of socioeconomically stable youth (n = 3244).
Race.
Finally, multigroup LCA models were run for three racial categories: individuals who identify as White (53.7%), individuals who identify as Black (20.3%), and individuals who identify as non-Black people of color (26.0%). Separate latent class models supported a four-class solution for White people, non-Black people of color, and Black people given the lower BIC values and higher entropy statistics, though it is worth noting that the one class in the four-class solution for both White people and non-Black people of color comprised less than 5% of the sample. Ultimately, given fit statistics and substantive interpretability of the additional class, the four-class solution was chosen. Across groups, the four classes were similar to the original model, though non-Black people of color had lower proportions of community violence and the class that did emerge with moderate levels of community violence included lower proportions of maltreatment or caregiver absence compared to what was seen for White youth and Black youth. Given that there were clear differences among groups based on the separate LCA models, there was no need to run a fully constrained model. The semiconstrained model had a lower BIC value compared to the unconstrained model and the Chi-square difference test was non-significant (ΔS-Bχ2 =59.05, p = .205). Therefore, the semiconstrained model was determined to be more appropriate than the unconstrained model. This suggests that while the profile sizes varied across race, the structure of the profiles was generally consistent. The childhood maltreatment class included 23.7% (n = 1565) of White youth, 32.0% (n = 1023) of non-Black youth of color, and 21.4% (n = 534) Black youth. The caregiver absence class was comprised of 13.3 % (n = 874) of White youth, 11.2% (n = 357) of non-Black youth of color, and 39.1% (n = 973) Black youth. The community violence class included 2.0% (n = 129) of White youth, 4.3% (n = 136) non-Black youth of color, and 10.2% (n = 254) of Black youth. Lastly, the low adversity class was made up of 61.1% (n = 4028) of White youth, 52.5% (n = 1676) of non-Black youth of color, and 29.3% (n = 730) Black youth. Considering that the structures of the latent classes were similar across groups for race and socioeconomic disadvantage, models were only run separately looking at differences in gender. Correlations among study variables are included in Tables 2a and 2b.
Table 2a.
Correlations among study variables for female sample
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child maltreatment | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 2. Caregiver absence | −.21** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 3. High adversity | −.16** | −.12** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 4. Low adversity | −.59** | −.46** | −.35** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 5. Mentor | .04** | −.02 | −.01 | −.01 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 6. Maternal relationship | −.12** | −.02 | −.14** | .18** | .01 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 7. Lifetime physical health | .04** | .02 | .05** | −.07** | .00 | .00 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 8. Lifetime mental health | .09** | .01 | .09** | −.14** | .01 | −.07** | .21** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 9. C-reactive protein | −.01 | .01 | −.01 | .00 | .00 | .04** | .06** | .00 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 10. Epstein-Barr virus | .00 | .02 | .02 | −.02 | .00 | .00 | .04** | −.01 | .05** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 11. Stress | .10** | .05** | .11** | −.18** | −.04** | −.12** | .10** | .28** | .01 | .03* | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 12. Depression | .09** | .04** | .12** | −.17** | −.04** | −.08** | .11** | .31** | .03* | .01 | .62** | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 13. Anxiety | .06** | .02 | .06** | −.11** | .00 | −.06** | .10** | .29** | .00 | −.02 | .42** | .40** | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 14. Alcohol difficulties | .09** | −.01 | .03 | −.08** | .06** | −.06** | .00 | .12** | −.02 | −.02 | .05* | .06** | .08** | - | - | - | - | - | - | - | - | - | - | - | - |
| 15.Health help-seeking | .00 | −.02 | −.02 | .03* | .02 | .03* | .04** | −.04** | .02 | .00 | −.07** | −.03** | −.03** | −.04 | - | - | - | - | - | - | - | - | - | - | - |
| 16. Nonviolent behaviors | .01 | .01 | .06** | −.05** | −.01 | −.01 | .03* | .07** | .00 | .00 | .09** | .09** | .05** | .05** | −.01 | - | - | - | - | - | - | - | - | - | - |
| 17. Violent behaviors | .03* | .04** | .11** | −.11** | .00 | −.04** | .04** | .08** | .01 | .03* | .13** | .15** | .05** | .03 | −.02 | .15** | - | - | - | - | - | - | - | - | - |
| 18. Sexually transmitted illness | .05** | .05** | .10** | −.13** | .00 | −.06** | .04** | .09** | −.02 | .05** | .09** | .10** | .04** | .13** | .05** | .08** | .08** | - | - | - | - | - | - | - | - |
| 19. Body mass index | .03* | .03** | .04** | −.06** | −.02 | .01 | .13** | .03* | .37** | .09** | .06** | .08** | −.01 | −.11** | .01 | .01 | .04** | −.01 | - | - | - | - | - | - | - |
| 20. Blood pressure | .00 | .00 | −.01 | .01 | −.02 | .01 | .09** | .03* | .13** | .03* | .02 | .01 | −.01 | −.06** | .00 | .01 | .05** | −.01 | .33** | - | - | - | - | - | - |
| 21. Waist circumference | .03** | .04** | .03* | −.07** | −.01 | .00 | .12** | .04** | .33** | .09** | .06** | .08** | −.01 | −.12** | .00 | .01 | .03* | −.02 | .86** | .31** | - | - | - | - | - |
| 22. White | −.01 | −.05** | −.05** | .07** | .07** | .02 | .05** | .16** | −.04** | −.10** | −.06** | −.06** | .10** | .10** | −.09** | .00 | −.07** | −.13** | −.12** | −.02 | −.06** | - | - | - | - |
| 23. Non-black person of color | −.06** | .11** | .07** | −.07** | −.02 | .04** | .00 | −.12** | .05** | .10** | .06** | .07** | −.10** | −.12** | .11** | .00 | .10** | .22** | .17** | .07** | .12** | −.60** | - | - | - |
| 24. Black | .07** | −.06** | −.01 | −.01 | −.07** | −.06** | −.06** | −.07** | .00 | .01 | .01 | .00 | −.02 | −.01 | −.01 | .00 | −.01 | −.06** | −.03* | −.04** | −.06** | −.58** | −.30 | - | - |
| 25. Child low SES | .00 | .02 | .00 | −.01 | −.02 | .02 | .02 | −.01 | .01 | .00 | .01 | .02 | .01 | .01 | −.01 | .00 | .01 | .01 | .01 | −.01 | .00 | −.02 | .03* | −.01 | - |
| 26. Current low SES | .02 | .14** | .15** | −.21** | −.04** | −.07** | .08** | .14** | .04** | .06** | .28** | .23** | .08** | .00 | −.04** | .07** | .14** | .18** | .18** | .07** | .18** | −.09** | .20 | −.09 | .04** |
p < .01.
p < .05.
SES = Socioeconomic status.
Table 2b.
Correlations among study variables for male sample
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child maltreatment | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 2. Caregiver absence | −.20** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 3. Community violence | −.1.6** | −.08** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 4. Low adversity | −.71** | −.36** | −.32** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 5. Mentor | .03** | −.04** | −.01 | .00 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 6. Maternal relationship | −.11** | −.02 | −.03* | .12** | .02 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 7. Lifetime physical health | .02 | .01 | .03* | −.04** | .02 | −.02 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 8. Lifetime mental health | .10** | .01 | .04** | −.11** | .01 | −.04** | .13** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 9. C-reactive protein | −.01 | .01 | .04** | −.02 | .00 | .03* | .08** | .02 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 10. Epstein-Barr virus | .01 | .03* | .04** | −.05** | −.01 | .02 | .02 | .01 | .04** | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 11. Stress | .11** | .03* | .07** | −.15** | −.03* | −.06** | .08** | .24** | .04** | .02 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 12. Depression | .11** | .01 | .08** | −.15** | −.02 | −.03* | .09** | .29** | .04** | .03* | .57** | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 13. Anxiety | .07** | .00 | .03 | −.08** | −.02 | −.03 | .08** | .24** | .02 | .01 | .40** | .40** | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 14. Alcohol difficulties | .09** | −.01 | .03 | −.10** | .06** | −.06** | .03 | .09** | .01 | .00 | .11** | .10** | .08** | - | - | - | - | - | - | - | - | - | - | - | - |
| 15.Health help-seeking | .01 | .01 | .03* | −.03* | .01 | .03* | .13** | .03* | .05** | .02 | −.03* | .02 | .02 | −.02 | - | - | - | - | - | - | - | - | - | - | - |
| 16. Nonviolent behaviors | .04** | −.01 | .07** | −.07** | .00 | .01 | .04** | .10** | .04** | −.01 | .10** | .10** | .04** | .07** | −.02 | - | - | - | - | - | - | - | - | - | - |
| 17. Violent behaviors | .05** | .01 | .17** | −.14** | −.01 | .00 | .02 | .10** | .05** | .00 | .09** | .12** | .06** | .06* | −.03 | .19** | - | - | - | - | - | - | - | - | - |
| 18. Sexually transmitted illness | .04** | .02 | .06** | −.07** | .00 | −.04** | .00 | .07** | .00 | .05** | .07** | .09** | .03* | .11** | .03* | .08** | .07** | - | - | - | - | - | - | - | - |
| 19. Body mass index | .02 | −.02 | .01 | −.02 | .00 | .02 | .15** | −.02 | .23** | .07** | −.01 | −.02 | −.02 | −.07** | .03* | .00 | .00 | −.05** | - | - | - | - | - | - | - |
| 20. Blood pressure | .00 | −.01 | .01 | .00 | −.01 | −.01 | .05** | .02 | .04** | .01 | −.01 | −.01 | −.02 | −.04* | −.02 | .01 | .02 | .00 | .21** | - | - | - | - | - | - |
| 21. Waist circumference | .02 | −.01 | .02 | −.03* | .00 | .02 | .16** | .02 | .25** | .07** | −.01 | −.01 | .00 | −.05** | .02 | .00 | −.01 | −.06** | .84** | .19** | - | - | - | - | - |
| 22. White | −.04** | −.01 | −.10** | .10** | .09** | −.04** | .00 | .15** | −.03* | −.08** | −.05** | −.07** | .05** | .06** | −.09** | −.03* | −.04** | −.12** | −.07** | .02 | .00 | - | - | - | - |
| 23. Non-black person of color | −.01 | .04** | .13** | −.08** | −.01 | .08** | .01 | −.09** | .03* | .11** | .06** | .09** | −.08** | −.04 | .09** | .04** | .04** | .20** | .01 | .00 | −.03* | −.54** | - | - | - |
| 24. Black | .06** | −.03* | .00 | −.04** | −.08** | −.02 | −.01 | −.09** | .01 | −.01 | .01 | .00 | .02 | −.04* | .02 | .00 | .01 | −.04** | .07** | −.02 | .02 | −.65** | −.29** | - | - |
| 25. Child low SES | .00 | .00 | .00 | .00 | .00 | .01 | .00 | −.01 | −.01 | −.01 | .00 | .01 | .03* | −.05* | .03 | −.01 | −.01 | .02 | .00 | .01 | .01 | −.01 | .05** | −.03 | - |
| 26. Current low SES | .07** | .07** | .09** | −.15** | −.02 | −.02 | .06** | .15** | .07** | .06** | .28** | .22** | .11** | .03 | −.04** | .13** | .09** | .05** | .03** | −.01 | .04** | −.02 | .10** | −.07** | .01 |
p < .01.
p < .05.
SES = Socioeconomic status.
Associations between ACEs and outcomes in adulthood
The relationship between ACE classes and outcomes in adulthood was examined among the female and male samples separately. Significant results are summarized below. See Table 3 for coefficients and significance values with all outcomes. First examining mental health outcomes within the female sample, youth in the low adversity class generally had better mental health, including lower levels of depression, anxiety, and stress, and lower likelihood of a lifetime mental health condition compared to the childhood maltreatment, household dysfunction, and high adversity classes. The household dysfunction class also had more positive mental health outcomes compared to the childhood maltreatment and high adversity classes. Examining risk-related outcomes, the low adversity class had a lower likelihood of engagement risk-related behaviors including lower likelihood of alcohol-related difficulties, lower likelihood of nonviolent delinquent behaviors, and/or lower likelihood of violent delinquent behaviors compared to the household dysfunction, childhood maltreatment, and high adversity classes. The childhood maltreatment class also had a lower likelihood of risk-related behaviors compared to the high adversity, including lower likelihood of engaging in both nonviolent and violent delinquent behaviors.
Table 3.
ACE classes predicting outcomes in adulthood
| Female | Male | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | Outcome | B | SE | Beta/[OR] | p value | B | SE | Beta/[OR] | p value |
| Low adversity vs. childhood maltreatment | |||||||||
| LT mental health | 0.67 | 0.10 | [1.95] | 0.000 | 0.51 | 0.12 | [1.66] | 0.000 | |
| Stress | 0.95 | 0.14 | 0.31 | 0.000 | 0.65 | 0.13 | 0.23 | 0.000 | |
| Depression | 0.88 | 0.11 | 0.33 | 0.000 | 0.60 | 0.10 | 0.26 | 0.000 | |
| Anxiety | 0.64 | 0.13 | 0.23 | 0.000 | 0.47 | 0.13 | 0.16 | 0.000 | |
| LT physical health | 0.35 | 0.08 | [1.43] | 0.000 | 0.17 | 0.09 | [1.18] | 0.076 | |
| Health help-seeking | −0.09 | 0.09 | [0.91] | 0.278 | 0.15 | 0.10 | [1.16] | 0.123 | |
| High blood pressure | 0.07 | 0.09 | [1.07] | 0.451 | 0.00 | 0.11 | [1.00] | 0.999 | |
| BMI | 0.61 | 0.34 | 0.07 | 0.075 | 0.52 | 0.35 | 0.08 | 0.139 | |
| Waist circumference | 1.31 | 0.80 | 0.07 | 0.104 | 1.62 | 0.73 | 0.10 | 0.026 | |
| CRP | −0.20 | 0.43 | −0.02 | 0.645 | 0.02 | 0.21 | 0.00 | 0.917 | |
| EBV | −3.89 | 4.39 | −0.04 | 0.375 | 4.23 | 4.71 | 0.05 | 0.347 | |
| STI | 0.30 | 0.09 | [1.34] | 0.001 | 0.36 | 0.12 | [1.43] | 0.003 | |
| Alcohol difficulties | 0.75 | 0.17 | [2.12] | 0.000 | 0.53 | 0.15 | [1.69] | 0.000 | |
| Nonviolent behaviors | 0.21 | 0.37 | [1.24] | 0.566 | 0.75 | 0.25 | [2.11] | 0.003 | |
| Violent behaviors | 0.68 | 0.22 | [1.98] | 0.002 | 1.60 | 0.22 | [1.68] | 0.000 | |
| Low adversity vs. household dysfunction | |||||||||
| LT mental health | 0.26 | 0.13 | [1.29] | 0.040 | 0.06 | 0.17 | [1.06] | 0.740 | |
| Stress | 0.61 | 0.16 | 0.20 | 0.000 | 0.42 | 0.16 | 0.15 | 0.010 | |
| Depression | 0.45 | 0.15 | 0.17 | 0.002 | 0.15 | 0.14 | 0.06 | 0.297 | |
| Anxiety | 0.44 | 0.17 | 0.16 | 0.011 | 0.15 | 0.18 | 0.05 | 0.400 | |
| LT physical health | 0.19 | 0.10 | [1.21] | 0.062 | 0.12 | 0.14 | [1.13] | 0.391 | |
| Health help-seeking | −0.12 | 0.10 | [0.89] | 0.218 | 0.25 | 0.14 | [1.29] | 0.071 | |
| High blood pressure | −0.09 | 0.10 | [0.92] | 0.392 | −0.20 | 0.18 | [0.82] | 0.253 | |
| BMI | −0.15 | 0.40 | −0.02 | 0.708 | −0.14 | 0.40 | −0.02 | 0.733 | |
| Waist circumference | 0.30 | 0.88 | 0.02 | 0.731 | 0.56 | 0.98 | 0.04 | 0.568 | |
| CRP | 0.16 | 0.61 | 0.02 | 0.790 | 0.50 | 0.48 | 0.08 | 0.299 | |
| EBV | 0.42 | 5.75 | 0.00 | 0.942 | 3.62 | 7.07 | 0.04 | 0.608 | |
| STI | 0.26 | 0.13 | [1.30] | 0.037 | 0.20 | 0.18 | [1.22] | 0.273 | |
| Alcohol difficulties | 0.40 | 0.21 | [1.49] | 0.062 | 0.28 | 0.21 | [1.32] | 0.191 | |
| Nonviolent behaviors | 0.66 | 0.55 | [1.93] | 0.231 | 0.11 | 0.47 | [1.12] | 0.813 | |
| Violent behaviors | 0.73 | 0.22 | [2.07] | 0.001 | 0.32 | 0.19 | [1.38] | 0.086 | |
| Low adversity vs. high adversity/community violence | |||||||||
| LT mental health | 0.84 | 0.14 | [2.31] | 0.000 | 0.97 | 0.19 | [2.38] | 0.000 | |
| Stress | 1.17 | 0.21 | 0.39 | 0.000 | 0.63 | 0.25 | 0.22 | 0.013 | |
| Depression | 1.19 | 0.16 | 0.44 | 0.000 | 0.78 | 0.23 | 0.33 | 0.001 | |
| Anxiety | 0.88 | 0.15 | 0.32 | 0.000 | 0.78 | 0.21 | 0.28 | 0.000 | |
| LT physical health | 0.40 | 0.12 | [1.49] | 0.001 | 0.43 | 0.16 | [1.54] | 0.007 | |
| Health help-seeking | −0.36 | 0.12 | [0.70] | 0.003 | 0.18 | 0.17 | [1.19] | 0.294 | |
| High blood pressure | −0.24 | 0.14 | [0.79] | 0.086 | −0.27 | 0.23 | [0.77] | 0.251 | |
| BMI | −0.04 | 0.54 | −0.00 | 0.945 | −0.33 | 0.55 | −0.05 | 0.550 | |
| Waist circumference | 0.50 | 1.22 | 0.00 | 0.967 | 1.27 | 1.30 | 0.08 | 0.332 | |
| CRP | −0.51 | 0.60 | −0.05 | 0.392 | 0.24 | 0.49 | 0.04 | 0.627 | |
| EBV | 4.48 | 7.21 | 0.04 | 0.534 | 13.19 | 9.69 | 0.14 | 0.173 | |
| STI | 0.58 | 0.13 | [1.79] | 0.000 | 0.44 | 0.22 | [1.55] | 0.043 | |
| Alcohol difficulties | 0.72 | 0.21 | [2.05] | 0.001 | 0.57 | 0.27 | [1.77] | 0.035 | |
| Nonviolent behaviors | 1.10 | 0.38 | [3.00] | 0.004 | 0.97 | 0.35 | [2.64] | 0.006 | |
| Violent behaviors | 1.25 | 0.22 | [3.47] | 0.000 | 1.60 | 0.22 | [4.97] | 0.000 | |
| Childhood maltreatment vs household dysfunction | |||||||||
| LT mental health | −0.41 | 0.13 | [0.66] | 0.002 | −0.45 | 0.17 | [0.64] | 0.008 | |
| Stress | −0.35 | 0.18 | −0.11 | 0.057 | −0.23 | 0.17 | −0.02 | 0.183 | |
| Depression | −0.43 | 0.17 | −0.16 | 0.009 | −0.45 | 0.15 | −0.06 | 0.003 | |
| Anxiety | −0.20 | 0.29 | −0.07 | 0.299 | −0.31 | 0.2 | −0.03 | 0.117 | |
| LT physical health | −0.17 | 0.13 | [0.85] | 0.187 | −0.05 | 0.14 | [0.95] | 0.721 | |
| Health help-seeking | −0.03 | 0.12 | [0.97] | 0.807 | 0.11 | 0.15 | [1.11] | 0.468 | |
| High blood pressure | −0.16 | 0.12 | [0.86] | 0.180 | −0.20 | 0.18 | [0.82] | 0.273 | |
| BMI | −0.76 | 0.48 | −0.09 | 0.113 | −0.66 | 0.47 | −0.03 | 0.165 | |
| Waist circumference | −1.00 | 1.03 | −0.05 | 0.328 | −1.06 | 1.13 | −0.02 | 0.348 | |
| CRP | 0.36 | 0.66 | 0.04 | 0.588 | 0.48 | 0.48 | 0.20 | 0.321 | |
| EBV | 4.31 | 6.05 | 0.04 | 0.477 | −0.80 | 7.48 | −0.00 | 0.915 | |
| STI | −0.04 | 0.12 | [0.97] | 0.776 | −0.16 | 0.20 | [0.85] | 0.431 | |
| Alcohol difficulties | −0.35 | 0.21 | [0.70] | 0.087 | −0.25 | 0.25 | [0.78] | 0.314 | |
| Nonviolent behaviors | 0.45 | 0.58 | [1.56] | 0.442 | −0.63 | 0.44 | [0.53] | 0.153 | |
| Violent behaviors | 0.04 | 0.23 | [1.04] | 0.849 | −0.20 | 0.21 | [0.82] | 0.349 | |
| Childhood maltreatment vs high adversity/community violence | |||||||||
| LT mental health | 0.17 | 0.15 | [1.19] | 0.250 | 0.36 | 0.19 | [1.43] | 0.055 | |
| Stress | 0.22 | 0.21 | 0.07 | 0.296 | −0.02 | 0.24 | −0.01 | 0.930 | |
| Depression | 0.31 | 0.19 | 0.12 | 0.097 | 0.18 | 0.23 | 0.08 | 0.441 | |
| Anxiety | 0.24 | 0.19 | 0.09 | 0.199 | 0.32 | 0.23 | 0.11 | 0.170 | |
| LT physical health | 0.04 | 0.12 | [1.05] | 0.719 | 0.27 | 0.18 | [1.31] | 0.128 | |
| Health help-seeking | −0.27 | 0.13 | [0.77] | 0.033 | 0.03 | 0.17 | [1.03] | 0.867 | |
| High blood pressure | −0.31 | 0.16 | [0.74] | 0.048 | −0.27 | 0.24 | [0.77] | 0.265 | |
| BMI | −0.76 | 0.48 | −0.08 | 0.113 | −0.85 | 0.56 | −0.12 | 0.132 | |
| Waist circumference | −1.27 | 1.41 | −0.07 | 0.374 | −0.35 | 1.36 | −0.02 | 0.796 | |
| CRP | −0.31 | 0.67 | −0.03 | 0.637 | 0.21 | 0.52 | 0.04 | 0.682 | |
| EBV | 8.36 | 7.57 | 0.08 | 0.269 | 8.77 | 10.1 | [1.00] | 0.387 | |
| STI | 0.28 | 0.15 | [1.33] | 0.051 | 0.08 | 0.25 | [1.08] | 0.749 | |
| Alcohol difficulties | −0.04 | 0.23 | [0.97] | 0.875 | 0.04 | 0.28 | [1.04] | 0.879 | |
| Nonviolent behaviors | 0.89 | 0.42 | [2.42] | 0.035 | 0.23 | 0.34 | [1.25] | 0.512 | |
| Violent behaviors | 0.56 | 0.27 | [1.75] | 0.035 | 1.09 | 0.22 | [2.96] | 0.000 | |
| Household dysfunction vs high adversity/community violence | |||||||||
| LT mental health | 0.58 | 0.17 | [1.79] | 0.001 | 0.81 | 0.22 | [2.25] | 0.001 | |
| Stress | 0.57 | 0.25 | 0.19 | 0.025 | 0.21 | 0.29 | 0.02 | 0.469 | |
| Depression | 0.75 | 0.20 | 0.28 | 0.001 | 0.63 | 0.26 | 0.07 | 0.014 | |
| Anxiety | 0.44 | 0.19 | 0.16 | 0.022 | 0.63 | 0.27 | 0.06 | 0.020 | |
| LT physical health | 0.21 | 0.15 | [1.23] | 0.164 | 0.32 | 0.21 | [1.37] | 0.128 | |
| Health help-seeking | −0.24 | 0.14 | [0.79] | 0.088 | −0.08 | 0.19 | [0.92] | 0.675 | |
| High blood pressure | −0.15 | 0.16 | [0.86] | 0.354 | −0.06 | 0.27 | [0.94] | 0.818 | |
| BMI | 0.11 | 0.68 | 0.01 | 0.867 | −0.19 | 0.64 | −0.03 | 0.765 | |
| Waist circumference | −0.25 | 1.56 | −0.01 | 0.871 | 0.71 | 1.56 | 0.04 | 0.651 | |
| CRP | −0.67 | 0.77 | −0.07 | 0.380 | −0.26 | 0.66 | −0.04 | 0.693 | |
| EBV | 4.06 | 8.03 | 0.04 | 0.613 | 9.57 | 11.5 | 0.10 | 0.406 | |
| STI | 0.32 | 0.17 | [1.38] | 0.054 | 0.24 | 0.25 | [1.27] | 0.343 | |
| Alcohol difficulties | 0.32 | 0.26 | [1.37] | 0.217 | 0.29 | 0.30 | [1.34] | 0.327 | |
| Nonviolent behaviors | 0.44 | 0.57 | [1.55] | 0.439 | 0.86 | 0.48 | [2.36] | 0.073 | |
| Violent behaviors | 0.52 | 0.26 | [1.68] | 0.046 | 1.28 | 0.26 | [3.61] | 0.001 | |
Note. LT = lifetime. BMI = Body mass index. CRP = C-reactive protein. EBV = Epstein-Barr virus. STI = Sexually transmitted illness.
Within the male sample, looking first at mental health, the low adversity class had more positive mental health outcomes, including lower levels of depression, anxiety, and stress, and a lower likelihood of having a lifetime mental health diagnosis compared to the childhood maltreatment and community violence classes. Few differences were observed between the low adversity and household dysfunction class, though the household dysfunction class reported higher levels of stress. The household dysfunction class had more positive mental health outcomes compared childhood maltreatment and community violence classes. Focusing on risk-related behaviors, the low adversity class also had a lower likelihood of engagement risk-related behaviors including either lower likelihood of alcohol-related difficulties, lower likelihood of nonviolent delinquent behaviors, and/or lower likelihood of violent delinquent behaviors compared to the childhood maltreatment and community violence classes. The community violence class was more likely to engage in violent behaviors compared to the childhood maltreatment class. Finally looking at physical health outcomes, the low adversity class also had a lower waist circumference compared to the childhood maltreatment class, a lower likelihood of physical health diagnosis compared to the high adversity class, and a lower likelihood of STI diagnosis compared to the childhood maltreatment and high adversity classes.
Discussion
Overall, the results of the current study identified four classes of ACEs. These classes were similar in structure when examining measurement invariance across race and SES, though the proportion of youth in each class varied when considering race. However, gender differences were observed, such that three classes had a similar configuration, representing low adversity, childhood maltreatment, and caregiver absence, but a community violence class emerged among male youth while a high adversity class emerged among female youth. For both male and female youth, the low adversity class generally had more positive psychological, risk-related, and physical health outcomes in adulthood compared to all other classes, Moreover, the caregiver absence class had more positive psychological and risk-related outcomes compared to the childhood maltreatment and high adversity (for females) and community violence (for males) classes. Finally, females in the high adversity class and males in the community violence class had a higher likelihood of engaging in risk-related behaviors.
The current findings contribute to the ACEs literature in several key ways. First, the exploration of ACE classes using multi-group, person-centered analysis is a novel approach that further explores the nuances in ACE exposure beyond count scores or examination of differences using single items. Within the present study and across studies (Cavanaugh et al., 2015; Merians et al., 2019; Lacey et al., 2020; Shin et al., 2018)., ACE classes have included a childhood maltreatment class, household dysfunction/caregiver absence class, and low adversity class. The fourth class has varied, with Lee and colleagues finding a community violence class, Cavanaugh et al., Merians et al., and Lacey and colleagues finding a high ACEs or polyadversity class, and Shin and colleagues identifying a combined caregiver absence/community violence class as well as a high ACE class. While recent studies have examined class differences based on race, gender, and SES (e.g., Cavanaugh et al., 2015; Haahr-Pederson et al., 2020; Maguire-Jack et al., 2019; Walsh et al., 2019), these studies did not test for measurement equivalence using constrained versus unconstrained models, and instead ran latent class analyses within groups separately. In fact, results of the current study, in which a community violence class emerged for males while a high adversity class emerged for females, may help reconcile the variation in the fourth class that has been seen in previous studies (Cavanaugh et al., 2015; Merians et al., 2019; Lacey et al., 2020; Lee et al., 2020; Shin et al., 2018). National survey data has pointed to differences in gender with regard to witnessing violence and assault victimization, such that males are more likely than females to be victims of and witness community violence, though both are equally as likely to be exposed to maltreatment and violence during their lifetimes (Finkelhor et al., 2015). When examining measurement equivalence based on race, while the structure of classes was fairly similar, the number of youth in each class varied. Differences in classes were not observed based on SES, in contrast to findings by Walsh and colleagues (2019), though it is important to note that these findings do not speak to differences in frequency of adversity exposure (e.g., socioeconomically disadvantaged youth may experience more chronic ACE exposure versus several single incidents of ACEs or multiple ACEs that occur in one incident).
Results also point to differences in how adversity exposure impacts outcomes in adulthood. The current findings suggest that exposure to childhood maltreatment is most predictive of physical health difficulties in adulthood, though for males, exposure to community violence can also have negative effects. Moreover, compared to adversity related to caregiver absence, childhood maltreatment has more negative effects on mental health, while high adversity exposure among females and community violence among males are more predictive of engagement in risk-related behaviors. These results are supported by work indicating that exposure to adversity characterized by abuse and neglect are associated with increased risk of obesity (e.g., Bentley & Widom, 2009; Danese & Tan, 2014), as well as higher likelihood of STIs (e.g., Haydon et al., 2011; Norman et al., 2012), while exposure to community violence has been linked to increased likelihood of asthma (Sternthal et al., 2010). Greater differences in psychological outcomes rather than physical health outcomes were also seen in a study by Merians et al. (2019), who found similar ACE classes but only saw small physical health differences. Overall, the current findings provide further evidence for the need to examine heterogeneity in ACE exposure, as not all types of adversity will have equal short- and long-term effects. Furthermore, the differences seen in the impact of ACEs by gender underscore the importance of examining how structural dimensions related to youth characteristics may play a role in how ACEs affect outcomes later in life.
Limitations and future directions
While the current study had several strengths, limitations must be considered. First, outcome variables were not measured across all timepoints, thus lack of baseline data precludes examination of change over time. Future work should collect data from early childhood to inform how baseline physical and psychological challenges may contribute to later outcomes. Additionally, several aspects of adversity would be important to consider for future studies, such as timing of adversity exposure or the duration of adversity exposure. Additionally, while the current study emphasized the importance of broadening the ACEs framework, it is necessary to recognize that the ways in which structural inequities are represented in most social science research generally and in the current analyses have important limitations. Specifically, group membership based on social constructs are rough proxies for experiences associated with these group identifications. Additionally, in the current dataset, the variable used for assessing gender was not representative of gender identity but was identified by the assessor in the study based on biological sex and only included a gender binary. There are notable limitations in the use of biological sex as a proxy for gender, especially considering that gender is a social construct and that sex alone does not determine gender (Lindqvist et al., 2020). Additional limitations include the use of self-report data, as well as retrospective reporting on ACE exposure.
Conclusion
Despite these limitations, the current study is among the first to assess the heterogeneity in patterns of ACE exposure during childhood and how these patterns may vary based on structural inequities, and related to outcomes in adulthood, especially among a large, nationally representative sample. Findings suggest that not only do youth demonstrate various patterns of adversity exposure, but differences also emerge when considering youth gender. Moreover, these patterns of adversity exposure may influence adult physical, psychological, and risk-related outcomes. Generally, findings point to the complex interplay between gender and different types of adversity exposure in youth developmental processes and highlight the importance of targeting supports to meet the needs of youth based on their unique contexts.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
Financial disclosure: none
References
- Acock AC (2014). A Gentle Introduction to Stata (4th ed.). Texas: Stata Press. [Google Scholar]
- Akaike H (1981). Modern development of statistical methods. In Trends and progress in system identification (pp. 169–184). Pergamon. [Google Scholar]
- Baker CK, Norris FH, Jones EC, & Murphy AD (2009). Childhood trauma and adulthood physical health in Mexico. Journal of Behavioral Medicine, 32(3), 255. [DOI] [PubMed] [Google Scholar]
- Bateson K, McManus M, & Johnson G (2020). Understanding the use, and misuse, of Adverse Childhood Experiences (ACEs) in trauma-informed policing. The Police Journal: Theory, Practice, and Principles, 1–15. [Google Scholar]
- Bentley T, & Widom CS (2009). A 30‐year follow‐up of the effects of child abuse and neglect on obesity in adulthood. Obesity, 17(10), 1900–1905. [DOI] [PubMed] [Google Scholar]
- Cavanaugh CE, Petras H, & Martins SS (2015). Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the United States. Social Psychiatry and Psychiatric Epidemiology, 50(8), 1257–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough C, Zorbas P, & Charuvastra A (2008). Attachment organization, emotion regulation, and expectations of support in a clinical sample of women with childhood abuse histories. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 21(3), 282–289. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1994). Perceived stress scale. Measuring stress: A guide for health and social scientists, 10(2), 1–2. [Google Scholar]
- Danese A, & Tan M (2014). Childhood maltreatment and obesity: systematic review and meta-analysis. Molecular Psychiatry, 19(5), 544–554. [DOI] [PubMed] [Google Scholar]
- Dannefer D (2003). Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58(6), S327–S337. [DOI] [PubMed] [Google Scholar]
- Ehring T, & Quack D (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41(4), 587–598. [DOI] [PubMed] [Google Scholar]
- Elwenspoek M, Kuehn A, Muller CP, & Turner JD (2017). The effects of early life adversity on the immune system. Psychoneuroendocrinology, 82, 140–154. 10.1016/j.psyneuen.2017.05.012 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Schafer MH, & Wilkinson LR (2016). Childhood disadvantage and health problems in middle and later life: Early imprints on physical health? American Sociological Review, 81(1), 107–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, & Shippee TP (2009). Aging and cumulative inequality: How does inequality get under the skin? The Gerontologist, 49(3), 333–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2015). Prevalence of childhood exposure to violence, crime, and abuse: Results from the national survey of children’s exposure to violence. JAMA Pediatrics, 169(8), 746–754. [DOI] [PubMed] [Google Scholar]
- Garraza LG, Azur M, Stephens RL, & Walrath CM (2011). Gender differences in patterns of child risk across programmatic phases of the CMHI: A multiple group latent class analysis (LCA). The Journal of Behavioral Health Services & Research, 38(2), 265–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haahr-Pedersen I, Perera C, Hyland P, Vallières F, Murphy D, Hansen M, … & Cloitre M (2020). Females have more complex patterns of childhood adversity: Implications for mental, social, and emotional outcomes in adulthood. European Journal of Psychotraumatology, 11(1), 1708618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haydon AA, Hussey JM, & Halpern CT (2011). Childhood abuse and neglect and the risk of STDs in early adulthood. Perspectives on Sexual and Reproductive Health, 43(1), 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson MI (2015). Cumulative inequality in child health and academic achievement. Journal of Health and Social Behavior, 56(2), 262–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmakis KA, & Chandler GE (2015). Health consequences of adverse childhood experiences: A systematic review. Journal of the American Association of Nurse Practitioners, 27(8), 457–465. [DOI] [PubMed] [Google Scholar]
- IBM Corp. (1985– 2017). IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. [Google Scholar]
- Kim P, Evans GW, Angstadt M, Ho SS, Sripada CS, Swain JE, … & Phan KL (2013). Effects of childhood poverty and chronic stress on emotion regulatory brain function in adulthood. Proceedings of the National Academy of Sciences, 110(46), 18442–18447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, & Drake B (2018). Child maltreatment risk as a function of poverty and race/ethnicity in the USA. International Journal of Epidemiology, 47(3), 780–787. [DOI] [PubMed] [Google Scholar]
- Lacey RE, Pereira SMP, Li L, & Danese A (2020). Adverse childhood experiences and adult inflammation: single adversity, cumulative risk and latent class approaches. Brain, Behavior, and Immunity, 87, 820–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Bray BC, & Collins LM (2013). An introduction to latent class and latent transition analysis. Handbook of psychology, 2, 691–716. [Google Scholar]
- Lee H, Kim Y, & Terry J (2020). Adverse childhood experiences (ACEs) on mental disorders in young adulthood: latent classes and community violence exposure. Preventive Medicine, 134(2020), 1–7. [DOI] [PubMed] [Google Scholar]
- Lindqvist A, Sendén MG, & Renström EA (2020). What is gender, anyway: a review of the options for operationalising gender. Psychology & Sexuality, 1–13. [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. [Google Scholar]
- Maguire-Jack K, Lanier P, & Lombardi B (2020). Investigating racial differences in clusters of adverse childhood experiences. American Journal of Orthopsychiatry, 90(1), 106–114. [DOI] [PubMed] [Google Scholar]
- Marusak HA, Martin KR, Etkin A, & Thomason ME (2015). Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology, 40(5), 1250–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzler M, Merrick MT, Klevens J, Ports KA, & Ford DC (2017). Adverse childhood experiences and life opportunities: shifting the narrative. Children and Youth Services Review, 72, 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merians AN, Baker MR, Frazier P, & Lust K (2019). Outcomes related to adverse childhood experiences in college students: comparing latent class analysis and cumulative risk. Child Abuse & Neglect, 87, 51–64. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012–2017). Mplus User’s Guide: Statistical Analysis with Latent Variables (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2017). Communities in action: Pathways to health equity. [PubMed]
- Nelson CA, Scott RD, Bhutta ZA, Harris NB, Danese A, & Samara M (2020). Adversity in childhood is linked to mental and physical health throughout life. BMJ, 371, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS med, 9(11), e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurius PS, Logan-Greene P, & Green S (2012). Adverse childhood experiences (ACE) within a social disadvantage framework: Distinguishing unique, cumulative, and moderated contributions to adult mental health. Journal of Prevention & Intervention in the Community, 40(4), 278–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural equation modeling: A multidisciplinary Journal, 14(4), 535–569. [Google Scholar]
- O'Donnell ML, Schaefer I, Varker T, Kartal D, Forbes D, Bryant RA, … & Steel Z (2017). A systematic review of person-centered approaches to investigating patterns of trauma exposure. Clinical Psychology Review, 57, 208–225 [DOI] [PubMed] [Google Scholar]
- Padgett RN, & Tipton RJ (2020). Identifying latent classes with ordered categorical indicators. arXiv preprint arXiv:2009.07345. [Google Scholar]
- Schafer MH, Ferraro KF, & Mustillo SA (2011). Children of misfortune: Early adversity and cumulative inequality in perceived life trajectories. American Journal of Sociology, 116(4), 1053–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. The annals of statistics, 461–464. [Google Scholar]
- Sclove SL (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika, 52(3), 333–343. [Google Scholar]
- Shin SH, McDonald SE, & Conley D (2018). Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addictive Behaviors, 78, 187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Loucks EB, Appleton AA, Kawachi I, Kubzansky LD, Non AL, … & Gilman SE (2015). Early origins of inflammation: An examination of prenatal and childhood social adversity in a prospective cohort study. Psychoneuroendocrinology, 51, 403–413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapleton L (2020). Analysis of Complex Survey Data (from NCES) [PowerPoint slides]. Measurement, Statistics and Evaluation Program, Department of Human Development and Quantitative Methodology, University of Maryland. [Google Scholar]
- Sternthal MJ, Jun HJ, Earls F, & Wright RJ (2010). Community violence and urban childhood asthma: a multilevel analysis. European Respiratory Journal, 36(6), 1400–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tein JY, Coxe S, & Cham H (2013). Statistical power to detect the correct number of classes in latent profile analysis. Structural equation modeling: a multidisciplinary journal, 20(4), 640–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt JK (2010). Latent class modeling with covariates: Two improved three-step approaches. Political analysis, 18(4), 450–469. [Google Scholar]
- Walrath C, Petras H, Mandell DS, Stephens RL, Holden EW, & Leaf PJ (2004). Gender differences in patterns of risk factors among children receiving mental health services: Latent class analyses. The Journal of Behavioral Health Services & Research, 31(3), 297–311. [DOI] [PubMed] [Google Scholar]
- Walsh D, McCartney G, Smith M, & Armour G (2019). Relationship between childhood socioeconomic position and adverse childhood experiences (ACEs): a systematic review. J Epidemiol Community Health, 73(12), 1087–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weller BE, Bowen NK, & Faubert SJ (2020). Latent class analysis: a guide to best practice. Journal of Black Psychology, 46(4), 287–311. [Google Scholar]
- Wilson RS, Boyle PA, Levine SR, Yu L, Anagnos SE, Buchman AS, … & Bennett DA (2012). Emotional neglect in childhood and cerebral infarction in older age. Neurology, 79(15), 1534–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff KT, Cuevas C, Intravia J, Baglivio MT, & Epps N (2018). The effects of neighborhood context on exposure to adverse childhood experiences (ACE) among adolescents involved in the juvenile justice system: Latent classes and contextual effects. Journal of youth and adolescence, 47(11), 2279–2300. [DOI] [PubMed] [Google Scholar]


