Abstract
The Japanese government's latest manual on COVID-19 management mentions non-invasive ventilation (NIV). Before this version, we experienced three cases in which COVID-19 was a concern. Each case had one of the following conditions: obesity hypoventilation syndrome, amyotrophic lateral sclerosis, acute heart failure with acute kidney injury with hypercapnia. The guidelines indicate that patients with these diseases are good candidates for NIV. NIV was used in a negative pressure room with staff in personal protective equipment. We describe the use of NIV instruments with anti-viral filters and a non-vented mask, including a new NIV machine for COVID-19 respiratory care.
Keywords: Continuous positive airway pressure, Non-invasive positive pressure ventilation, High flow nasal cannula, Obstructive sleep apnea
Abbreviations: CPAP, continuous positive airway pressure; EPAP, expiratory positive airway pressure; HFNC, high flow nasal cannula; IPAP, inspiratory positive airway pressure; NIRS, non-invasive respiratory support; NIV, non-invasive ventilation; NPPV, non-invasive positive pressure ventilation
1. Introduction
While non-invasive ventilation (NIV; continuous positive airway pressure (CPAP), or non-invasive positive pressure ventilation, NPPV) is useful for managing respiratory failure [1], the use of NIV for patients with coronavirus disease 2019 (COVID-19) is controversial due to the possibility of aerosols escaping from the equipment. NIV has usually been avoided in Japan because the government's manual on COVID-19 did not discuss the use of NIV for the respiratory care of patients with COVID-19 [2] until version 6.0 [3], even though high flow nasal cannula (HFNC) oxygen therapy and NIV have been considered useful for treating COVID-19 patients in other countries [[4], [5], [6]]. HFNC can provide oxygen at concentrations nearing 100%, but expiratory positive airway pressure (EPAP) is only 2 or 3 cmH2O. The most recent study comprising 13,931 patients showed that overall, non-invasive respiratory support (NIRS) in patients with COVID-19 was safe, improved resource utilization, and was associated with possibly better outcomes than conventional oxygen therapy [7]. For patients with COVID-19, NIV with inlet and outlet anti-virus filters in addition to non-vented filters with an artificial nose or anti-virus filters is suitable. Since NIRS, including NIV, will be used more frequently in the management of COVID-19 patients in Japan in the near future, pulmonologists in Japan need to know how to use NIV machines to prevent the spread of aerosols and contamination of the ventilator. Here, we describe three cases in whom a new NIV machine suitable for COVID-19 patients was used.
2. Case presentations
2.1. Case 1
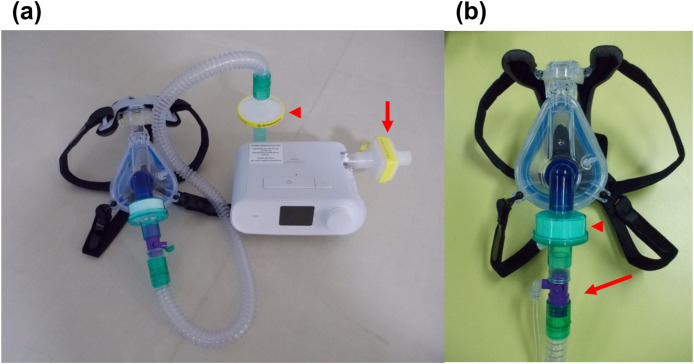
A 57-year-old obese (body mass index 34.4 kg/m2) male underwent treatment for asthma, diabetes, and obstructive sleep apnea treated by CPAP. Fifteen days before coming to our hospital, he tested positive for COVID-19 in a severe acute respiratory syndrome coronavirus two polymerase chain reaction (SARS-CoV-2 PCR) test during the second wave of the COVID-19 pandemic in Japan (August 2020). His condition worsened, and he was transferred to our hospital. On admission, his SpO2 was 99% (oxygen via nasal cannula 3 L/min), and PaCO2 was 38.7 mmHg. Chest X-ray and computed tomography showed bilateral pneumonia, decreased right lung volume, and elevation of the right diaphragm (Fig. 1-a-1 ). CPAP was stopped as advised by the Japanese government manual at the time [8]. Within three days, he developed right lung atelectasis. CPAP treatment was initiated intermittently in a negative pressure room from day three, including oxygen with a new Philips Respironics E30 ventilator (Respironics, Inc., Murrysville, PA, USA). This was a new NIV machine for COVID-19 with inlet and outlet filters and an AF811 SE gel full face mask (Respironics, Inc.), which was a non-vented full face mask (Fig. 2 -a, and b) with an artificial nose. The patient only used CPAP for 3 h during the middle of the day because the medical staff feared that an air leak with aerosols could easily occur during the night. Although the patient's respiratory condition worsened until day eight (PaCO2 reached 50 mmHg with oxygen 6 L/min with a simple-oxygen-mask), he gradually recovered as indicated by chest X-ray changes (Fig. 1-a-2-3). Oxygen therapy was discontinued on day 17.
Fig. 1.
Chest x-rays of the cases. Case 1, from anterior to posterior, supine position on days one (a-1), seven (a-2), and 23 (a-3). (b) Case 3, from anterior to posterior supine position on day one.
Fig. 2.
NIV and interface for COVID-19. (a) E30 ventilator (Respironics, Inc., Murrysville, PA, USA; Non-invasive ventilation ventilator for COVID-19 patients), and AF811 SE gel full face mask (Respironics, Inc.) (non-vented full face mask). The bacterial filter is attached to the air inlet (arrow) and outlet (arrowhead) to avoid contamination of the ventilator from aerosols. (b) A circuit and non-vented full face mask. There is no exhalation leak port on the mask. Expiration is drained from an exhalation valve (arrow) after passing through an artificial nose filter (arrowhead) to avoid spreading aerosols.
2.2. Case 2
Case 2 was an 80-year-old female with amyotrophic lateral sclerosis who had refused to undergo invasive mechanical ventilation and was dependent on NPPV. The patient's caregiver was diagnosed with COVID-19 seven days before the patient was admitted to our hospital during the third wave of the COVID-19 pandemic in Japan (January 2021). She was provided with NPPV (inspiratory positive airway pressure [IPAP] 13 cmH2O, EPAP 4 cmH2O supplemental oxygen) using the same system used for case 1. During NPPV, PaCO2 increased up to 69.9 mmHg; thus, we increased IPAP to 17 cmH2O. The patient's SARS-CoV-2 PCR test was negative. She was discharged home on day nine.
2.3. Case 3
On admission to our hospital, a 78-year-old male with heart failure and kidney disease had a pH of 6.88, PaCO2 of 116.2 mmHg, PaO2 of 54.7 mmHg, HCO3− of 21.0 mmol/L, and BE of −11.9 mEq/L (oxygen administration 10 L/min with a mask). Normal NPPV was used at the first hospital, and the patient was transferred to our hospital for renal replacement therapy during the third wave of the COVID-19 pandemic in Japan (January 2021). Chest X-ray showed cardiomegaly, pulmonary edema, and bilateral pleural effusion (Fig. 1-b). After admission to our hospital, the new NIV (E-30 ventilator) with the non-vented mask was used because we could not exclude COVID-19 infection. His SARS-CoV-2 PCR test was negative on day two, and continuous hemodiafiltration was performed until day three. The patient was discharged home on day 19.
3. Discussion
Here, we have described three cases treated with novel NIV equipment with three filters (inlet, outlet, and an artificial nose) and a non-vented full face mask. Case 1 was positive for COVID-19, while the remaining two patients had the possibility of COVID-19 infection.
The most commonly used NIV machines take in outside air, and if used by a patient with COVID-19, the inside of the machine could become contaminated, and COVID-19 positive air could escape from the outlet. A new NIV (CPAP or NPPV) machine specifically for COVID-19 can be equipped with inlet and outlet anti-virus filters and non-vented masks with an artificial nose or anti-virus filter. Physicians should know how to use each NIV machine with appropriate filters and exhalation ports (Fig. 2).
The early Japanese government's manual recommended that COVID-19 patients be intubated and mechanically ventilated [8] if SpO2 could not be maintained ≥93% despite inhalation of 5 L/min O2 by nasal cannula or masks.
It is expected that NIV will be used more frequently in the near future after being cited in the latest manual by the Japanese government. Our three cases were good candidates for NIV according to the guidelines [1]. More than 500,000 patients are on home CPAP therapy in Japan, and more than 20,000 patients are treated by home NPPV therapy, including adaptive servo-ventilation (ASV) [9]. Therefore, including the usage of CPAP or NPPV in the intensive care unit (ICU), information on managing patients with respiratory care at home during the next pandemic should be more available. In addition, NIV may be useful for patients with hypoxemic COVID-19 as it can be administered with the patient in a prone position.
Although the feasibility and clinical impact of CPAP and NPPV were also reported in patients with COVID-19 pneumonia [5,6], an increased number of medical staff members with COVID-19, as determined by positive serology or pharyngeal swabs, was reported in non-ICU non-invasive respiratory support settings caring for patients with COVID-19. However, all infected workers recovered well [5]. In comparing CPAP with NPPV, it should be recognized that NPPV is usually associated with more aerosol leaks than CPAP. Therefore, NIV should be used in a negative pressure room or red zone with staff wearing personal protective equipment as with case 1, in which case there was no transmission to the medical staff.
There are several limitations to our report. First, only one patient was a true COVID-19 patient. Nevertheless, recent large-scale data have supported NIV as a significantly useful method for patients with COVID-19 [7,10]. Second, since the machine used was a new machine for patients with COVID-19, it might have a negative effect in supporting patients’ breathing, such as high circuit resistance, difficulty in patient synchronization, and loss of humidity. Indeed, the second case initially became hypercapnic following the start of this system but improved after the parameters of the machine were reset. Therefore, physicians should carefully observe patients when this machine is first used.
Each patient in this report had a different pathophysiologically severe condition, was effectively treated, and recovered satisfactorily. The latest government manual for COVID-19 indicates the use of NIV. The safety of staff caring for confirmed or suspected COVID-19 patients on NIV should be addressed.
Disclosure statement
This study was financially supported by a Grant-in-Aid from the Ministry of Health, Labor and Welfare of Japan (H30-iryo-ippan-009, 21FA1004), Japan Agency for Medical Research and Development (AMED) (ek0210116, ek0210150 and wm0425018), and Grant-in-Aid for Scientific Research (17H04182, 20H03690, 20K17860) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Conflict of Interest
Takuma Minami, Shinichi Kai, Tomoharu Tanaka, Isao Ito, Genta Kato, Miki Nagao, Hiroshi Date, Toyohiro Hirai, and Shigeru Ohtsuru have no conflicts of interest to declare. Kazuo Chin belonged to departments supported by Philips Respironics, ResMed, Fukuda Denshi, and Fukuda Lifetec-Keiji and Tokyo.
Acknowledgments
The authors would like to thank Hiroyasu Kubo (Division of Medical Equipment, Kyoto University Hospital), Hirotoshi Watanabe and Hideyuki Kinoshita (Department of Cardiovascular Medicine, Kyoto University Graduate School of Medicine), Takashi Ayaki (Department of Neurology, Kyoto University Graduate School of Medicine), Yohei Korogi and Naoya Tanabe (Department of Respiratory Medicine, Kyoto University Graduate School of Medicine), Hironobu Sunadome and Susumu Sato (Department of Respiratory Care and Sleep Control Medicine, Kyoto University Graduate School of Medicine), Satoshi Hamada (Department of Advanced Medicine for Respiratory Failure, Kyoto University Graduate School of Medicine), Ken Shinozuka and Tomoyuki Yunoki (Department of Primary Care and Emergency Medicine, Kyoto University Graduate School of Medicine), and all physicians, pharmacists, physiotherapists, nurses, and medical social workers that took care of patients.
References
- 1.Akashiba T., Ishikawa Y., Ishihara H., Imanaka H., Ohi M., Ochiai R., et al. The Japanese respiratory society noninvasive positive pressure ventilation (NPPV) guidelines (second revised edition) Respir Investig. 2017;55:83–92. doi: 10.1016/j.resinv.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Japanese Ministry of Health, Labor and Welfare . 2021. Singata corona virus kansensyou sinryou no tebiki dai 5.3 han. [Japanese] [Google Scholar]
- 3.Japanese Ministry of Health, Labor and Welfare . 2021. Singata corona virus kansensyou sinryou no tebiki dai 6 han. [Japanese] [Google Scholar]
- 4.Durie M. The National Health Service. NHS Guidance on use of NIV in adults with coronavirus | INTENSIVE Review, https://intensiveblog.com/nhs-guidance-on-use-of-niv-in-adults-with-coronavirus-intensive-review/ [accessed 6 January 2022].
- 5.Franco C., Facciolongo N., Tonelli R., Dongilli R., Vianello A., Pisani L., et al. Feasibility and clinical impact of out-of-ICU noninvasive respiratory support in patients with COVID-19-related pneumonia. Eur Respir J. 2020;56:2002130. doi: 10.1183/13993003.02130-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oranger M., Gonzalez-Bermejo J., Dacosta-Noble P., Llontop C., Guerder A., Trosini-Desert V., et al. Continuous positive airway pressure to avoid intubation in SARS-CoV-2 pneumonia: a two-period retrospective case-control study. Eur Respir J. 2020;56:2001692. doi: 10.1183/13993003.01692-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weerakkody S., Arina P., Glenister J., Cottrell S., Boscaini-Gilroy G., Singer M., et al. Non-invasive respiratory support in the management of acute COVID-19 pneumonia: considerations for clinical practice and priorities for research. Lancet Respir Med. 2022;10:199–213. doi: 10.1016/S2213-2600(21)00414-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Japanese Ministry of Health, Labor and Welfare . 2020. Singata corona virus kansensyou sinryou no tebiki dai 2.2 han. [Japanese] [Google Scholar]
- 9.e-Stat. Statistics of Medical Care Activities in Public Health Insurance, https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450048&tstat=000001029602&cycle=7&tclass1=000001154766&tclass2=000001154771&tclass3=000001154772&tclass4val=0 [Japanese]. [accessed 6 January 2022].
- 10.Perkins G.D., Ji C., Connolly B.A., Couper K., Lall R., Baillie J.K., et al. Effect of noninvasive respiratory strategies on intubation or mortality among patients with acute hypoxemic respiratory failure and COVID-19: the RECOVERY-RS randomized clinical trial. JAMA. 2022;327:546–558. doi: 10.1001/jama.2022.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]