Abstract
Background
There has been substantial discussion as to whether the mental health and socio-economic consequences of the COVID-19 pandemic might impact suicide rates. Although India accounts for the largest proportion of global suicides, the early impacts of the COVID-19 pandemic on suicide rates in this country are unknown.
Methods
National Crime Records Bureau (NCRB) data were used to calculate annual suicide rates for the period 2010–2020, stratified by sex and state. Rate Ratios (RRs) stratified by sex and state were calculated to estimate the extent of change in suicide rates.
Results
Suicide rates in India generally showed a decreasing trend from 2010 until 2017, with the trend reversing after this period, particularly for males. Among males and females, the highest increase post 2017 was noted in 2020 (compared to 2017) (males: RR = 1.18 95% UI 1.17–1.19; females: RR = 1.05 95% UI 1.03–1.06).
Limitation
Suicide rates based on the NCRB data might be an underestimation of the true suicide rates.
Conclusion
Suicide rates in India increased during the first year of the COVID-19 pandemic, and although the increase in suicide rates, especially among males, predates the pandemic, the increase in suicide rates was highest in 2020, compared to increases in previous years. Further research is warranted to understand the potential ongoing impact of the COVID-19 pandemic on suicide in India.
Keywords: Suicide, COVID-19, India, National Crime Records Bureau (NCRB)
1. Introduction
Suicide is a major public health issue in India (Dandona et al., 2017; Arya et al., 2018; India State-Level Disease Burden Initiative Suicide Collaborators, 2018; Armstrong and Vijayakumar, 2018; Vijayakumar et al., 2021). An estimated 230,314 suicides occurred in India in 2016, accounting for 37% and 25% of global female and male suicides, respectively (India State-Level Disease Burden Initiative Suicide Collaborators, 2018).
India reported its first case of COVID-19 on 30th January 2020 in the southern state of Kerala, while the first two COVID-19 deaths were reported on 14th March 2020 (Siddiqui et al., 2020). India's initial response to the pandemic included closure of borders and advisories around social distancing before rapid increase in cases prompted a two-month national lockdown (25th March 2020–31st May 2020). The national lockdown was implemented in four different phases, with the first phase (25th March–14th April) being most strict in terms of restrictions compared to phase two (15th April–3rd May), phase three (4th May–17th May) and phase four (18th May-31st May), which accompanied eventual easing of restrictions (Salvatore et al., 2020). The Indian government announced fiscal stimulus packages such as cash transfers to lower income households and insurance for healthcare workers to address the widespread economic disruption caused by the pandemic, especially during the lockdown phase (Ramakumar and Kanitkar, 2021; Sharma et al., 2020). By the end of 2020, India had reported ~10 million COVID-19 cases and ~150,000 COVID-19 deaths (worldometers.info, 2022). However, these numbers are likely an underestimation of the true burden of COVID-19 cases and deaths in India (Shewade et al., 2021).
The COVID-19 pandemic has had an adverse impact on population mental health (Santomauro et al., 2021) however, evidence from upper-middle income and high-income countries suggests that suicide rates either remained stable or reduced during the early phase of the pandemic (Pirkis et al., 2021). To date, there is limited evidence investigating the potential impacts of the COVID-19 pandemic on suicide in lower income countries, including India (Knipe et al., 2021). A study conducted in Nepal reported an increase in suicide rates in the country during the COVID-19 pandemic compared to previous years (Acharya et al., 2022). The latest National Crime Records Bureau (NCRB) data, which is the administrative data source of unnatural deaths in India based on police reports, also reported an increase in number of suicides in India 2020 compared to 2019 (Menon et al., 2021). However, none of the studies hitherto have reported on the change in suicide rates in India in 2020 compared to preceding years, and whether or not these changes differ by sex and region. This is an important gap as the change in suicide rates is more informative in assessing any ongoing impacts of COVID-19 on suicide rates in India. This study uses recently published NCRB data for India to investigate trends in suicide rates in India from 2010 until the end of the first year of the COVID-19 pandemic in 2020, stratified by sex and state.
2. Method
2.1. Data
Police reports on suicides from each state and union territory in India are collated at the national level and presented as yearly reports by the NCRB (NCRB, 2020). Suicide data for the period 2010–2020, stratified by sex, were obtained from the NCRB website. Age-specific suicide rates could not be calculated as suicide data stratified by age-groups (by state) has not been published by the NCRB since 2015. In 2014, the state of Andhra Pradesh was split to form two separate states (Andhra Pradesh and Telangana) and the state of Jammu and Kashmir was dissolved in 2019 and reorganised into two union territories (Jammu and Kashmir and Ladakh). Suicide cases from Andhra Pradesh and Telangana as well as from Jammu and Kashmir and Ladakh were combined for 2014–2020 and 2020 respectively, to ensure geographic consistency in the analysis with previous years. Corresponding population data were extracted from Ministry of Health and Family Welfare population estimates for 2011–2020 (National Health Profile, 2020) with 2010 population calculated via retrospective projection (using linear extrapolation which estimated an average change over time).
2.2. Analysis
Crude suicide rates stratified by sex were calculated from 2010 to 2020 to provide context to trends in suicide rates in India before 2020. Crude suicide rates from 2010 to 2020 were also calculated for the three specific groups of Indian states categories based on their Sociodemographic Index (SDI); low SDI, middle SDI and high SDI, with the low SDI states being the most underdeveloped in terms of per capita income and literacy and fertility rates (GBD 2017 DALYs and HALE Collaborators, 2018; India State-Level Disease Burden Initiative Air Pollution Collaborators, 2019).
Firstly, joinpoint regression analysis was conducted to empirically identify joinpoints of continuous change in suicide trends in India between 2010 and 2020 by sex and region (Kim et al., 2000), and also to explore whether the year 2020 was associated with a joinpoint change (Web appendix, 1–3). Based on the results, rate ratios (RR) of crude suicide rates, stratified by sex and state, were calculated for 2018, 2019 and 2020, with 2017 as the reference year (i.e., the start of change in suicide trends), to identify whether the increase in suicide rates in 2020 was higher or lower compared to increases in previous years (Web appendix 4). RRs were also calculated for the three specific SDI state groups. To account for uncertainty around the RR estimates, all the RRs were reported with 95% uncertainty intervals (UIs), based on Monte Carlo simulations using Ersatz software (Barendregt, 2009). The ErRelativeRisk function (assuming normal distribution for the In(RR) with an SD of SE[In(RR)]), was used to estimate the 95% UIs after 1000 iterations, ensuring convergence of model outcomes. Analyses were conducted in MS Excel, Joinpoint Regression Program, STATA 15.1, and Ersatz 1.35 (Mitchell, 2008; Barendregt, 2009; Joinpoint Regression Program, 2019).
3. Results
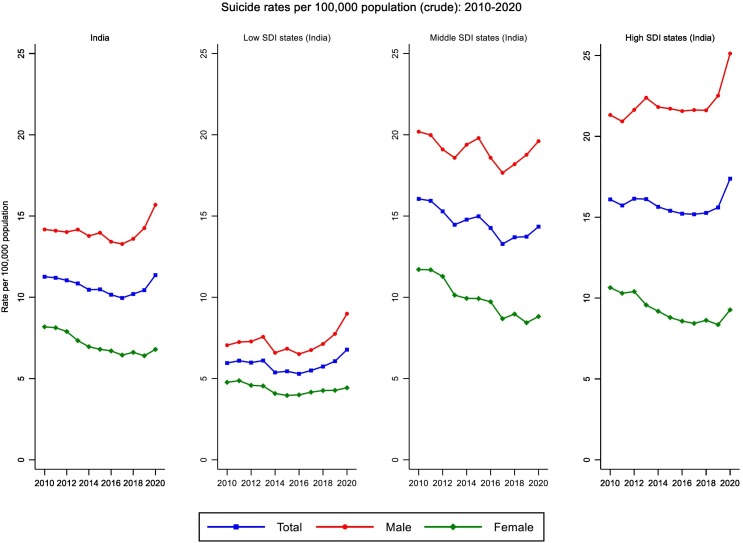
Overall crude suicide rates in India decreased moderately between 2010 and 2017 (decreasing from 11.26 to 9.95 per 100,000 population), with male suicide rates decreasing from 14.17 to 13.28 per 100,000 population and female suicide rates decreasing from 8.18 to 6.44 per 100,000 population (Fig. 1 ; Web appendix 5–8). Among males, suicide rates consistently increased post 2017, with the highest increase noted in 2020 (RR = 1.18 95% UI 1.17–1.19) (Fig. 1; Table 1 ; Web appendix 4). Among females, there was an increase in suicide rates in 2018 (RR = 1.02 95% UI 1.01–1.03), followed by an insignificant decrease in 2019 (RR = 0.99 95% UI 0.98–1.00), and then an increase again in 2020 (RR = 1.05 95% UI 1.03–1.06) (Fig. 1; Table 1; Web appendix 4). The largest increase in 2020 was noted among males in low SDI states (RR = 1.33 95% UI 1.30–1.35), and among males (RR = 1.16 95% UI 1.14–1.17) and females (RR = 1.09 95% UI 1.07–1.12) in high SDI states (Fig. 1; Table 1).
Fig. 1.
Suicide rates (crude): India and by Socio-Demographic Index (SDI) state categories (2010–2020).
Table 1.
Suicide rate ratios for 2018 versus 2017, 2019 versus 2017, and 2020 versus 2017, with 95% UI by sex, and SDI state groups.
| Total | RR 95% UI (2018–2017) | RR 95% UI (2019–2017) | RR 95% UI (2020–2017) |
|---|---|---|---|
| India | 1.02 (1.01–1.03) | 1.04 (1.04–1.05) | 1.14 (1.13–1.14) |
| Low SDI | 1.04 (1.02–1.05) | 1.1 (1.08–1.11) | 1.23 (1.21–1.25) |
| Middle SDI | 1.03 (1.01–1.04) | 1.03 (1.01–1.04) | 1.08 (1.06–1.09) |
| High SDI | 1 (0.99–1.01) | 1.02 (1.01–1.04) | 1.14 (1.13–1.15) |
| Male | |||
| India | 1.02 (1.01–1.03) | 1.07 (1.06–1.08) | 1.18 (1.17–1.19) |
| Low SDI | 1.05 (1.03–1.07) | 1.14 (1.12–1.16) | 1.33 (1.3–1.35) |
| Middle SDI | 1.03 (1.01–1.04) | 1.06 (1.04–1.07) | 1.11 (1.09–1.12) |
| High SDI | 0.99 (0.98–1.01) | 1.04 (1.02–1.05) | 1.16 (1.14–1.17) |
| Female | |||
| India | 1.02 (1.01–1.03) | 0.99 (0.98–1) | 1.05 (1.03–1.06) |
| Low SDI | 1.02 (1–1.04) | 1.02 (1–1.05) | 1.06 (1.03–1.09) |
| Middle SDI | 1.03 (1.01–1.05) | 0.97 (0.95–0.99) | 1.01 (0.99–1.03) |
| High SDI | 1.02 (0.99–1.04) | 0.99 (0.96–1.01) | 1.09 (1.07–1.12) |
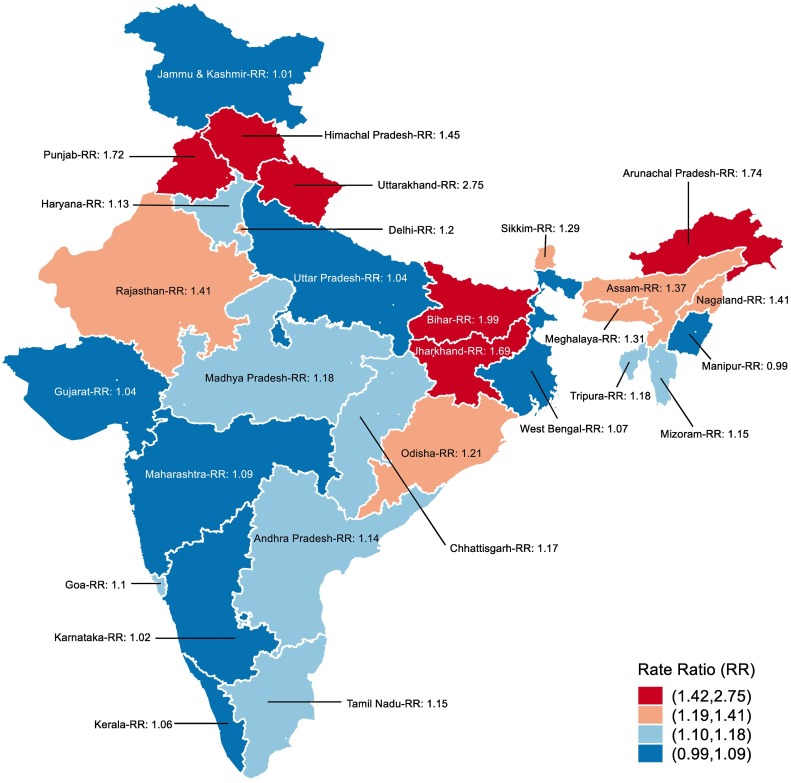
States with the largest increase in suicide in 2020 included the low SDI states of Bihar (RR = 1.99 95% UI 1.74–2.25), Jharkhand (RR = 1.69 95% UI 1.56–1.81), the middle SDI state of Arunachal Pradesh (RR = 1.74 95% UI 1.33–2.27); and the high SDI states of Uttarakhand (RR = 2.75 95% UI 2.41–3.10), Punjab (RR = 1.72 95% UI 1.61–1.83), and Himachal Pradesh (RR = 1.45 95% UI 1.30–1.61) (Fig. 2 ; Table 2 ).
Fig. 2.
Suicide rate ratios for 2020 versus 2017: Total.
Table 2.
Suicide rate ratios for 2020 versus 2017 with 95% UI: Total.
| State | 2017 suicide rates with 95% CI | 2020 suicide rates with 95% CI | RRa (95% UI) |
|---|---|---|---|
| India | 9.95 (9.9–10.01) | 11.36 (11.3–11.42) | 1.14 (1.13–1.14) |
| Andhra Pradeshb | 14.68 (14.43–14.93) | 16.78 (16.51–17.05) | 1.14 (1.11–1.17) |
| Arunachal Pradesh | 6.03 (4.84–7.43) | 10.53 (8.96–12.29) | 1.74 (1.33–2.27) |
| Assam | 6.78 (6.5–7.06) | 9.35 (9.03–9.68) | 1.37 (1.3–1.45) |
| Bihar | 0.33 (0.3–0.36) | 0.66 (0.62–0.71) | 1.99 (1.74–2.25) |
| Chhattisgarh | 22.57 (22.02–23.14) | 26.48 (25.89–27.08) | 1.17 (1.13–1.21) |
| Delhi | 12.91 (12.41–13.44) | 15.55 (15.02–16.11) | 1.2 (1.14–1.27) |
| Goa | 17.94 (15.88–20.2) | 19.88 (17.72–22.23) | 1.1 (0.93–1.3) |
| Gujarat | 11.22 (10.97–11.48) | 11.69 (11.43–11.94) | 1.04 (1–1.07) |
| Haryana | 12.15 (11.75–12.57) | 13.76 (13.33–14.19) | 1.13 (1.08–1.18) |
| Himachal Pradesh | 7.99 (7.35–8.67) | 11.66 (10.89–12.47) | 1.45 (1.3–1.61) |
| Jammu & Kashmirc | 2.2 (1.95–2.47) | 2.24 (1.99–2.51) | 1.01 (0.86–1.18) |
| Jharkhand | 3.34 (3.15–3.53) | 5.65 (5.41–5.89) | 1.69 (1.56–1.81) |
| Karnataka | 18.09 (17.76–18.42) | 18.48 (18.15–18.81) | 1.02 (0.99–1.04) |
| Kerala | 22.64 (22.14–23.14) | 24.07 (23.56–24.59) | 1.06 (1.03–1.09) |
| Madhya Pradesh | 14.72 (14.45–14.99) | 17.48 (17.2–17.77) | 1.18 (1.15–1.21) |
| Maharashtra | 14.72 (14.5–14.93) | 16.14 (15.92–16.37) | 1.09 (1.07–1.11) |
| Manipur | 1.41 (1.02–1.9) | 1.4 (1.02–1.88) | 0.99 (0.62–1.5) |
| Meghalaya | 5.21 (4.45–6.07) | 6.87 (6–7.84) | 1.31 (1.06–1.61) |
| Mizoram | 7.78 (6.26–9.55) | 8.97 (7.35–10.82) | 1.15 (0.86–1.54) |
| Nagaland | 1.56 (1.07–2.19) | 2.21 (1.63–2.93) | 1.41 (0.87–2.1) |
| Odisha | 10.37 (10.07–10.68) | 12.64 (12.31–12.98) | 1.21 (1.17–1.26) |
| Punjab | 5.04 (4.78–5.3) | 8.69 (8.36–9.03) | 1.72 (1.61–1.83) |
| Rajasthan | 5.1 (4.94–5.26) | 7.22 (7.04–7.41) | 1.41 (1.36–1.47) |
| Sikkim | 32.92 (28.65–37.64) | 42.53 (37.74–47.77) | 1.29 (1.05–1.53) |
| Tamil Nadu | 19.28 (18.96–19.59) | 22.2 (21.86–22.53) | 1.15 (1.12–1.17) |
| Tripura | 17.68 (16.38–19.04) | 20.95 (19.56–22.41) | 1.18 (1.06–1.29) |
| Uttar Pradesh | 2.02 (1.96–2.08) | 2.1 (2.04–2.16) | 1.04 (1–1.08) |
| Uttarakhand | 3.04 (2.72–3.38) | 8.36 (7.84–8.91) | 2.75 (2.41–3.1) |
| West Bengal | 12.55 (12.33–12.78) | 13.43 (13.2–13.66) | 1.07 (1.04–1.09) |
Rate ratio: Calculated by dividing crude suicide rates for 2020 by crude suicide rates of 2017.
Including the state of Telangana.
Including the union territory of Ladakh.
4. Discussion
This study investigated trends in Indian suicide rates from 2010 to 2020, which included the first year of the COVID-19 pandemic. We observed that suicide rates in India, especially among males, increased in 2020, and although this occurred in the context of increasing trends in suicide, the increase in suicide rates was higher in 2020 compared to preceding years. Among females, the increase in 2020 was smaller than for males with instability in the pattern from the prior years (i.e. an increase and then a decrease). This increase in 2020 was greatest among all the SDI state groups, and was particularly evident among males in low SDI states and among males and females in the high SDI states.
Research on the potential impact of the COVID-19 pandemic on suicide rates has been mostly restricted to high income countries. Findings have suggested that generally, suicide rates did not increase during the initial months of the pandemic, with Japan and Hungary being notable exceptions (Pirkis et al., 2021; Sakamoto et al., 2021; Osváth et al., 2021). In fact, in several locations suicide rates have decreased in contrast to initial concerns (Pirkis et al., 2021). Potential explanations offered for lack of increase in suicide rates elsewhere in the world include timely responses by governments to the psychological, social, and economic impacts of the pandemic, including the strengthening of mental health services and the implementation of economic support schemes, and a sense of collectiveness or banding/rallying together in facing the common challenge of the pandemic (Pirkis et al., 2021).
Our study found that suicide rates increased in India in 2020. We observed that the increase in suicide rates was substantially greater among males compared to females. The traditional role of males as the—“breadwinners”—of the family in India and the pressures of providing for the family has been highlighted as a potential reason for male suicides in India (Arya et al., 2018). While untested, it is possible that the economic consequences of the pandemic (e.g., loss of job/income) and the associated role strain and shame might have been experienced more severely, on average, among males.
Mental health services in India have undergone a period of scaling up over the past decade (Pandya et al., 2020), and new initiatives were commenced during the COVID-19 pandemic (Ransing et al., 2020). Yet, as in many middle-income countries, critical shortages remain in mental health personnel and other health system infrastructure in several parts of the country (WHO, 2017; India State-Level Disease Burden Initiative Mental Disorders Collaborators, 2020). It is possible that the mental health system in less developed parts of India was less able to be as responsive to the increased mental health burden in the community during the COVID-19 pandemic compared to settings with more resourced mental health systems. Moreover, mental health issues are highly stigmatised in India, contributing further to gaps in help-seeking and service provision.
Economic and welfare initiatives, which are speculated to have had a protective effect in high-income countries during the initial months of COVID-19 (Pirkis et al., 2021), were also undertaken in India. The Indian government commissioned substantial economic relief schemes, such as the Pradhan Mantri Garib Kalyan Yojana (PMGKY) (translated as ‘Prime Minister's relief fund for the poor’), which included direct cash transfers to bank accounts and in-kind social assistance to vulnerable households (Khan, 2020). Such schemes were observed to have provided essential relief, particularly to those in the vulnerable agricultural sector during the early phase of the pandemic (Varshney et al., 2021). While there may have been issues related to the coverage of such schemes (Chaudhary et al., 2020), they may have played an important role in curtailing the increases in suicides that have been observed.
Evidence from other countries has highlighted that there has been a differential impact of the pandemic on suicide rates across diverse population groups, and that national level analyses may overlook important differences among sub-populations. For example, in the state of Maryland (USA), suicide rates decreased among White residents between March and July in 2020 while conversely, they increased among Black residents (Bray et al., 2021). Similarly, in the state of Connecticut (USA), the proportion of suicides from racial minority groups increased during the lockdown period (Mitchell and Li, 2021). It is possible that socio-economically disadvantaged populations may have also been disproportionally impacted by the effects of the pandemic in India such as loss of work and income. For example, the adverse impacts of COVID-19, especially during lockdowns, might have been more severe among people from disadvantaged households who were already experiencing financial insecurity and reliance on daily wage work (Cash and Patel, 2020). In Nepal, the highest increases in suicide rates during the COVID-19 pandemic were noted in the two provinces with high poverty rates and low human development index as well as a high proportion of seasonal migrant workers (Acharya et al., 2022). Similarly, in India, the higher increase in male suicide rates in low SDI states, compared to middle and high SDI states, might be reflective of the severity of the negative social and economic impacts of the pandemic among already disadvantaged households.
There are important methodological limitations to this study. Firstly, the data were based on the NCRB reports which are likely an underestimation of suicide cases in India (Arya et al., 2021), especially since the beginning of the pandemic (Kallakuri and Maulik, 2020). Secondly, age-specific data were not available, reducing the ability of this study to explore age-specific patterns of suicide rates. For example, during the Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong, an increase in suicide rates was noted among the older age groups (Yip et al., 2010). Thirdly, lack of additional data restricts our ability to rule out any other potential factors, other than the social disruption caused by COVID-19, that might have driven the increase in suicide rates in India in 2020. Despite these limitations, this is an important study towards assessing the potential ongoing impact, or lack of impact, of the COVID-19 pandemic on suicide rates in LMIC settings.
In conclusion, suicide rates in India increased in 2020, and although this occurred in the context of increasing trends in suicide, the increase in suicide rates was higher in 2020 compared to preceding years. The increase was more pronounced among males compared to females. The reasons for an increase in suicides in 2020 are not clear but the social disruptions caused by the COVID-19 pandemic might have, in part, contributed towards this increase above what would otherwise have been expected. However, further research is required to measure potential impact of COVID-19 on suicide rates in India. Ongoing monitoring and consideration of specific sub-populations (e.g., age-groups, religion, and caste) remains paramount in order to determine any ongoing impacts of the COVID-19 pandemic on suicide rates in India.
CRediT authorship contribution statement
Vikas Arya - Conceptualization, Data curation, Formal analysis, Writing-original draft, Writing-review & editing
Andrew Page - Conceptualization, Writing-review & editing
Matthew J. Spittal - Writing-review & editing
Rakhi Dandona - Writing-review & editing
Lakshmi Vijayakumar - Writing-review & editing
Sithum Munasinghe - Writing-review & editing
Ann John - Writing-review & editing
David Gunnell - Writing-review & editing
Jane Pirkis - Writing-review & editing
Gregory Armstrong - Conceptualization, Writing-review & editing.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Acknowledgments
Acknowledgements
None.
Funding
Matthew J. Spittal is a recipient of an Australian Research Council Future Fellowship (project number FT180100075) funded by the Australian Government.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.03.066.
Appendix A. Supplementary data
Supplementary Material
References
- Acharya B., Subedi K., Acharya P., Ghimire S. Association between COVID-19 pandemic and the suicide rates in Nepal. PloS one. 2022;17(1) doi: 10.1371/journal.pone.0262958. Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong G., Vijayakumar L. Suicide in India: a complex public health tragedy in need of a plan. Lancet Public Health. 2018;3(10):e459–e460. doi: 10.1016/S2468-2667(18)30142-7. Oct 1. [DOI] [PubMed] [Google Scholar]
- Arya V., Page A., Armstrong G., Kumar G.A., Dandona R. Estimating patterns in the under-reporting of suicide deaths in India: comparison of administrative data and Global Burden of Disease Study estimates, 2005–2015. J. Epidemiol. Community Health. 2021;75(6):550–555. doi: 10.1136/jech-2020-215260. Jun 1. [DOI] [PubMed] [Google Scholar]
- Arya V., Page A., River J., Armstrong G., Mayer P. Trends and socio-economic determinants of suicide in India: 2001–2013. Soc. Psychiatry Psychiatr. Epidemiol. 2018;53(3):269–278. doi: 10.1007/s00127-017-1466-x. Mar. [DOI] [PubMed] [Google Scholar]
- Barendregt J.J. EpiGear; Brisbane: 2009. Ersatz User Guide. [Google Scholar]
- Bray M.J., Daneshvari N.O., Radhakrishnan I., Cubbage J., Eagle M., Southall P., Nestadt P.S. Racial differences in statewide suicide mortality trends in Maryland during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Psychiatry. 2021;78(4):444–447. doi: 10.1001/jamapsychiatry.2020.3938. Apr 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash R., Patel V. Has COVID-19 subverted global health? Lancet. 2020;395(10238):1687–1688. doi: 10.1016/S0140-6736(20)31089-8. May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhary M., Sodani P.R., Das S. Effect of COVID-19 on economy in India: some reflections for policy and programme. J. Health Manag. 2020;22(2):169–180. Jun. [Google Scholar]
- Dandona R., Bertozzi-Villa A., Kumar G.A., Dandona L. Lessons from a decade of suicide surveillance in India: who, why and how? Int. J. Epidemiol. 2017;46(3):983–993. doi: 10.1093/ije/dyw113. Jun 1. [DOI] [PubMed] [Google Scholar]
- India State-Level Disease Burden Initiative Mental Disorders Collaborators The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. Lancet Psychiatry. 2020;7(2):148–161. doi: 10.1016/S2215-0366(19)30475-4. Feb 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- India State-Level Disease Burden Initiative Suicide Collaborators Gender differentials and state variations in suicide deaths in India: the global burden of disease study 1990–2016. Lancet Public Health. 2018;3(10):e478–e489. doi: 10.1016/S2468-2667(18)30138-5. Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joinpoint Regression Program . National Cancer Institute; 2019. Statistical Research And Applications Branch. [Google Scholar]
- Kallakuri S., Maulik P.K. Challenges facing individuals and researchers: suicide in India in the COVID-19 pandemic. Lancet Psychiatry. 2020;7(8) doi: 10.1016/S2215-0366(20)30254-6. Aug 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan Q.M. The World Bank; 2020. Appraisal Program Information Document (PID)-Accelerating India’s COVID-19 Social Protection Response Program (PMGKY)-P173943. Apr 27. [Google Scholar]
- Kim H.J., Fay M.P., Feuer E.J., Midthune D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000;19(3):335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Knipe D., John A., Padmanathan P., Eyles E., Dekel D., Higgins J.P., Bantjes J., Dandona R., Macleod-Hall C., McGuinness L.A., Schmidt L. 2021. Suicide and self-harm in low-and middle-income countries during the COVID-19 pandemic: a systematic review. medRxiv. Jan 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon V., Cherian A.V., Vijayakumar L. Rising incidence and changing demographics of suicide in India: time to recalibrate prevention policies? Asian J. Psychiatr. 2021;25(69) doi: 10.1016/j.ajp.2021.102983. Dec. [DOI] [PubMed] [Google Scholar]
- Mitchell M.N. Stata Press; 2008. A Visual Guide to Stata Graphics. [Google Scholar]
- Mitchell T.O., Li L. State-level data on suicide mortality during COVID-19 quarantine: early evidence of a disproportionate impact on racial minorities. Psychiatry Res. 2021;1(295) doi: 10.1016/j.psychres.2020.113629. Jan. [DOI] [PubMed] [Google Scholar]
- National Crime Records Bureau Accidental deaths and suicides in India. Government of India, New Delhi. 2010-2020. https://ncrb.gov.in/en/adsi-reports-of-previous-years Available.
- National Health Profile . Ministry of Health and Family Welfare, Government of India; 2020. Central Bureau of Health Intelligence.http://www.indiaenvironmentportal.org.in/content/470474/national-health-profile-2020/ 2020. Available. [Google Scholar]
- Osváth P., Bálint L., Németh A., Kapitány B., Rihmer Z., Döme P. A magyarországi öngyilkossági halálozás változásai a COVID–19-járvány első évében. Orv. Hetil. 2021;162(41):1631–1636. doi: 10.1556/650.2021.32346. Oct 10. [DOI] [PubMed] [Google Scholar]
- Pandya A., Shah K., Chauhan A., Saha S. Innovative mental health initiatives in India: a scope for strengthening primary healthcare services. J.Fam.Med.Primary Care. 2020;9(2):502. doi: 10.4103/jfmpc.jfmpc_977_19. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M., et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579–588. doi: 10.1016/S2215-0366(21)00091-2. Jul 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramakumar R., Kanitkar T. Impact of COVID-19 pandemic on the Indian economy: a critical analysis. Investig.Econ. 2021;80(315):3–32. Mar. [Google Scholar]
- Ransing R., Kar S.K., Menon V. National helpline for mental health during COVID-19 pandemic in India: new opportunity and challenges ahead. Asian J. Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102447. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamoto H., Ishikane M., Ghaznavi C., Ueda P. Assessment of suicide in Japan during the COVID-19 pandemic vs previous years. JAMA Netw. Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.37378. Feb 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvatore M., Basu D., Ray D., Kleinsasser M., Purkayastha S., Bhattacharyya R., Mukherjee B. Comprehensive public health evaluation of lockdown as a non-pharmaceutical intervention on COVID-19 spread in India: national trends masking state-level variations. BMJ Open. 2020;10(12) doi: 10.1136/bmjopen-2020-041778. Dec 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santomauro D.F., Herrera A.M., Shadid J., Zheng P., Ashbaugh C., Pigott D.M., Abbafati C., Adolph C., Amlag J.O., Aravkin A.Y., Bang-Jensen B.L. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. Nov 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma G.D., Talan G., Jain M. Policy response to the economic challenge from COVID-19 in India: a qualitative enquiry. J. Public Aff. 2020;20(4) doi: 10.1002/pa.2195. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shewade H.D., Parameswaran G.G., Mazumder A., Gupta M. Adjusting reported COVID-19 deaths for the prevailing routine death surveillance in India. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.641991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui A.F., Wiederkehr M., Rozanova L., Flahault A. Situation of India in the COVID-19 pandemic: India's initial pandemic experience. Int. J. Environ. Res. Public Health. 2020;17(23):8994. doi: 10.3390/ijerph17238994. Jan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varshney D., Kumar A., Mishra A.K., Rashid S., Joshi P.K. COVID-19, government transfer payments, and investment decisions in farming business: evidence from northern India. Appl.Econ.Perspect.Policy. 2021;43(1):248–269. doi: 10.1002/aepp.13144. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayakumar L., Chandra P.S., Kumar M.S., Pathare S., Banerjee D., Goswami T., Dandona R. The national suicide prevention strategy in India: context and considerations for urgent action. Lancet Psychiatry. 2021 Dec 8 doi: 10.1016/S2215-0366(21)00152-8. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2017. Mental Health Atlas 2017. [Google Scholar]
- Worldometers.info Coronavirus cases and deaths: India. 2022. https://www.worldometers.info/coronavirus/country/india/ Available.
- Yip P.S., Cheung Y.T., Chau P.H., Law Y.W. The Impact of Epidemic Outbreak: The Case of Severe Acute Respiratory Syndrome (SARS) and Suicide Among Older Adults in Hong Kong. Crisis. 2010;31(2):86–92. doi: 10.1027/0227-5910/a000015. Apr 23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material