Abstract
Introduction
The strength of the evidence base for the comparative effectiveness of three common surgical modalities for paediatric nephrolithiasis (ureteroscopy, shockwave lithotripsy and percutaneous nephrolithotomy) and its relevance to patients and caregivers are insufficient. We describe the methods and rationale for the Pediatric KIDney Stone (PKIDS) Care Improvement Network Trial with the aim to compare effectiveness of surgical modalities in paediatric nephrolithiasis based on stone clearance and lived patient experiences. This protocol serves as a patient-centred alternative to randomised controlled trials for interventions where clinical equipoise is lacking.
Methods and analysis
The PKIDS is a collaborative learning organisation composed of 26 hospitals that is conducting a prospective pragmatic clinical trial comparing the effectiveness of ureteroscopy, shockwave lithotripsy and percutaneous nephrolithotomy for youth aged 8–21 years with kidney and/or ureteral stones. Embedded within clinical care, the PKIDS trial will collect granular patient-level, surgeon-level and institution-level data, with a goal enrolment of 1290 participants over a 21-month period. The primary study outcome is stone clearance, defined as absence of a residual calculus of >4 mm on postoperative ultrasound. Secondary outcomes include patient-reported physical, emotional and social health outcomes (primarily using the Patient-Reported Outcome Measurement Information System), analgesic use and healthcare resource use. Timing and content of secondary outcomes assessments were set based on feedback from patient partners. Heterogeneity of treatment effect for stone clearance and patient-reported outcomes by participant and stone characteristics will be assessed.
Ethics and dissemination
This study is approved by the central institutional review board with reliance across participating sites. Participating stakeholders will review results and contribute to development dissemination at regional, national and international meetings.
Trial registration number
Keywords: Protocols & guidelines, Clinical trials, UROLOGY
Strengths and limitations of this study.
Pragmatic trial design embedded within clinical care allows accumulation of real-world data (strength).
Observational studies may be subject to biases based on surgeon or patient preferences for procedural decision making (weakness).
Voluminous data collection plans, subject to heterogeneity by site and missing data (weakness).
Patient engagement in trial design adds to the impact of the research to key stakeholders (ie, patients and caregivers themselves) as well as to address potential barriers to study recruitment (strength).
Introduction
Although the incidence of paediatric kidney stone disease has risen rapidly in recent years, the evidence base for the comparative effectiveness of surgical management of this disease in children is poor.1 Ureteroscopy, shockwave lithotripsy and percutaneous nephrolithotomy are three surgical modalities currently used in clinical care, each with overlapping indications and competing complication profiles.2 Smaller anatomy, different procedural risks, high prevalence of medical complexity, and the unique lived experiences of children all influence treatment decisions and effectiveness, and therefore limit extrapolation from studies conducted in adult populations.2 3 The American Urological Association (AUA) Guidelines for Surgical Management of Stones developed recommendations based on a systematic review of literature up to 2015. Notably, only eight recommendations are paediatric-specific and none of these eight are guided by high-quality randomised controlled or observational trials.2 Very few recommendations were informed by studies that assessed patient-reported outcomes (PROs), and none were codesigned by patients and/or caregivers. A more recent systematic review, published in 2019, identified just 13 published articles comparing surgical modalities for nephrolithiasis in children with the highest level of evidence identified as ‘2b’. Of these 13 articles, 3 were randomised controlled trials (RCTs); 1 was a prospective observational trial; and the remainder were retrospective reviews.4
In response to this knowledge gap,5 the Pediatric KIDney Stone (PKIDS) Care Improvement Network was funded by the Patient-Centered Outcomes Research Institute to conduct an expansive, 3-year prospective pragmatic clinical trial of youth undergoing surgery for kidney and/or ureteral stones.6 This PCORnet Designated trial (the Comparative Effectiveness in Paediatric Kidney Stone Surgery trial, henceforth referred to as the ‘PKIDS trial’) will compare stone clearance and patient-selected experiences after ureteroscopy, shockwave lithotripsy and percutaneous nephrolithotomy. Embedded in clinical care across 24 sites, the PKIDS trial harnesses natural variations in surgical management7–9 and will generate real-world evidence to guide shared decision making. Here we report the design of the PKIDS trial and present a rationale for developing patient-centred pragmatic studies that are embedded within clinical care, a framework of particular importance for studies with unique recruitment considerations such as those involving surgical interventions where clinical equipoise may not exist, vulnerable populations and/or rare diseases.
Methods
Aims
The primary aim of the PKIDS trial is to compare the effectiveness of stone clearance for all three surgical modalities in youth with kidney stones and to evaluate heterogeneity of treatment effect by stone size and location. The secondary trial aim will compare patients’ experiences after the same three surgeries, measured using validated and novel questionnaires, unanticipated healthcare encounters and analgesic medication administration. We will investigate the heterogeneity of treatment effect of the patient experience by age and sex. For each aim, we will evaluate modifiable surgical techniques associated with outcomes. The PKIDS trial (current Protocol V.3.0, version date 3 November 2020) started recruitment in August 2020 with an anticipated completion date of June 2022.
Setting
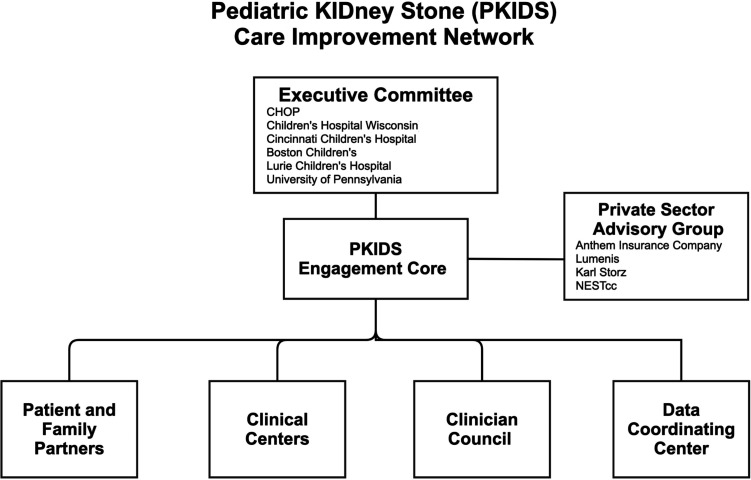
The PKIDS network comprises 26 North American hospitals providing care for youth with kidney stones across 24 unique healthcare systems, spanning broad spectrums of location, practice setting and size. A full list of participating sites can be found at https://wwwresearchchopedu/pkids. Each clinical centre is supported by a site principal investigator. The PKIDS network is a collaborative learning health system supported by an advisory council of specialty physicians in urology, nephrology and radiology, as well as by key stakeholders and end users such as patients, members of industry, health insurers and the National Evaluation System for Health Technology Coordinating Centre10 11 (figure 1). In addition, seven PKIDS sites are also members of PEDSnet, a clinical research network designed to support the generation and application of knowledge to improve outcomes for paediatric disease.12 13
Figure 1.
PKIDS Care Improvement Network organisational chart. CHOP, Children’s Hospital of Philadelphia; PKIDS, Pediatric KIDney Stone.
Study design
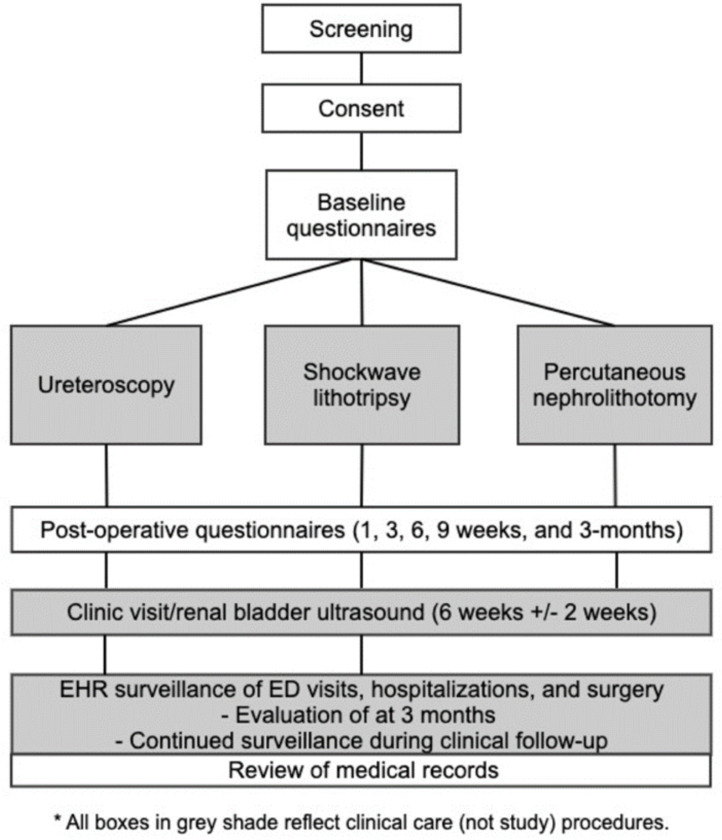
The PKIDS trial is a pragmatic prospective observational trial embedded within clinical care, aspiring to maximise participation and generate knowledge reflective of real-world experiences. Over a 21-month enrolment period, the trial will accrue 1290 participants undergoing ureteroscopy, shockwave lithotripsy or percutaneous nephrolithotomy. Participants are followed up for 3 months after their surgical intervention (figure 2). Choice of procedure will be determined by decision making between the surgeon and the patient and caregivers, reflective of the standard of care at each clinical centre. Each surgical intervention will be performed by a surgeon familiar with the procedure, without proscribed technical standardisation to ensure generalised applicability of results and the opportunity to identify modifiable parameters to improve care within each surgical intervention. No treatment decisions within kidney stone care or otherwise are impacted by trial enrolment. The sample size of 1290 will provide 80% power to detect an expected difference of 80%14 vs 65%15 in stone clearance between ureteroscopy and shockwave lithotripsy, and to detect a difference of 90%16 vs 65%15 in stone clearance between percutaneous nephrolithotomy and shock wave lithotripsy at=0.05, accounting for multiple comparisons and loss to follow-up. Assuming a 10% loss to follow-up and 10% PRO missingness, 39 patients in each group will have 80% power to detect an expected difference of 2 points in each of the Patient-Reported Outcomes Measurement Information System (PROMIS) measures across treatment options at 0.05, adjusting for multiple comparisons.
Figure 2.
Comparative effectiveness of Pediatric KIDney Stone surgery study flowchart. ED, emergency department; EHR, electronic health record.
Patient and public involvement
Patient and caregiver engagement is central to aspects of a collaborative learning health system, from design to dissemination to improvement strategies.17 To this end, the PKIDS Patient and Family Partners (PFP) is composed of seven members (four parents of children with nephrolithiasis and three adolescents with nephrolithiasis) who have undergone partnership-based research training using Fyreworks (https://www.fyreworkstraining.com/), an online module-based platform, and are paid consultant fees as partners on the research team. The PFP had decision-making authority on several key aspects of trial design, including the timing of PRO assessments, choice of specific PRO instruments and identification of relevant content gaps within these available PRO instruments. This process was a structured, iterative process involving both open-ended feedback (for timing and content gaps) and rank–list prioritisation (for choice of PRO measures). A summary of key methodological choices supported by collaboration with our patient and caregiver collaborators is highlighted in table 1. Our PFP continue to be engaged with the PKIDS network and have helped refine trial procedures and provide the patient voice throughout the conduct of the trial. The PFP will be involved in the evaluation of results, dissemination of our findings and optimising colearning within the improvement phase of this trial.
Table 1.
PKIDS PFP perspectives and corresponding action items
| Patient perspective | Network/study action |
| ‘I have more anxiety. I have pain and when I do, I always wonder if it is related to a kidney stone. I have missed school. It has also affected my social life, not always feeling well, I’m not sure about doing things’. |
PRO instrument selection Timing of PRO assessment |
| ‘Procedures and recovery were unpleasant, it helped to know what I didn’t want to have happen again and what I hope to have happen’. | PRO instrument selection timing of PRO assessment |
| ‘Would they be able to get the stone? Would I need stents again? Would I have to come back in for another procedure?’ | Surgical outcome selection |
| ‘I wanted to help the researchers understand the patient’s viewpoint, small concerns could be big ones for a patient. Hope to make it easier for my future procedures and for others’. | Expansion of PFP responsibilities Symposium keynote speaker Authorship for academic publication |
PFP, Patient and Family Partners; PKIDS, Pediatric KIDney Stone; PRO, patient-reported outcome.
Study participants
Any youth aged 8–21 years undergoing ureteroscopy, shockwave lithotripsy or percutaneous nephrolithotomy at a PKIDS site is eligible for inclusion. The age limit of 8 years is reflective of the lower age limit of self-report for the paediatric-validated PROMIS measures, while the limit of 21 years reflects the upper age limit of adolescence defined by the American Academy of Pediatrics.18 19 We will exclude patients for whom obtaining informed consent delays access to emergent surgical care (eg, obstructing ureteral stone with fever requiring emergency surgery), although these patients could be recruited following initial decompression and prior to definitive surgical intervention. Additionally, individuals who are not proficient in either Spanish or English will be excluded, as well as those rare individuals who are scheduled to undergo simultaneous dual-modality surgical interventions (ie, concomitant shock wave lithotripsy and ureteroscopy). A recruitment strategy enhanced by automated electronic health record (EHR) alerts for eligible patients and bolstered by the pragmatic trial design and reach of the PKIDS network will ensure a diverse population with respect to sex, race, geography and comorbidities (ie, spina bifida and cystinuria), thereby representing the broad spectrum of youth with nephrolithiasis in the USA. For patients who experience multiple stone events over the 21-month enrolment period, we will restrict enrolment to one episode requiring kidney stone surgery to avoid patient-level clustering.
Outcomes
Stone clearance
Stone clearance, the primary outcome, will be assessed by ultrasound 6 weeks (±2 weeks) following definitive stone surgery, reflecting existing standard postoperative imaging practices across the network and allowing for effective postoperative imaging while minimising concerns of ionising radiation in children.20 The radiological criteria for defining a stone are (1) hyperechoic focus with (2) twinkle artefact, an intense Doppler-generated multicolour signal overlying calculi.21 22 To reduce variation inherent to ultrasound, all PKIDS site investigators agreed to adopt with minor modifications the standardised ultrasound protocol that was developed for the Urinary Stone Disease Research Network (USDRN) Prevention of Urinary Stones with Hydration trial (online supplemental figure 1).23 Stone clearance is defined as the absence of any stone of >4 mm. This cut point was chosen because ultrasound overestimates stone size by 2 mm, and 2 mm is a commonly used conservative size for clinically insignificant stone fragments measured by CT.24–26 A flexible window of imaging capture of up to 3 months will be allowable to reduce missingness of data.
bmjopen-2021-056789supp001.pdf (38.8KB, pdf)
Patient-reported outcomes
Secondary outcomes of PROs measuring physical, emotional and social health will be assessed at baseline and at prespecified postoperative intervals as described in table 2. Six PROMIS measures were selected from a preliminary list of 10 based on input from the PFP: pain intensity, pain interference, anxiety, peer relationships, psychological stress experiences and sleep disturbances.27 28 Urinary symptoms are not specifically measured by PROMIS but are known to be a significant source of burden in patients with nephrolithiasis.29 The Dysfunctional Voiding Scoring System (DVSS) is a paediatric-specific validated questionnaire assessing urinary symptoms favoured by the PFP and is designed for direct patient completion with limited assistance from a parent or guardian.30
Table 2.
Patient-facing inventories and administration schedule, based on a single index surgical intervention
| Baseline* | Week 1 | Week 3 | Week 6 | Week 9 | Week 12 | |
| Baseline Intake Questionnaire | X | |||||
| PROMIS Pain Interference V.2.0† | X | X | X | X | X | |
| PROMIS Anxiety V.2.0† | X | X | X | X | X | |
| PROMIS Psych Stress Experiences V.1.0† | X | X | X | X | X | |
| PROMIS Sleep Disturbance V.1.0† | X | X | X | X | X | |
| PROMIS Peer Relationships V.2.0† | X | X | X | X | X | |
| PROMIS Pain Intensity V.1.0† | X | X | X | X | X | |
| PROMIS Prescription Pain Med Misuse V.1.0‡ | X | |||||
| DVSS† | X | X | X | X | X | |
| QUIKSS | X | X | X | X | X | |
| Post-Op Patient-Reported Event Capture | X | X | X | X | X | |
| COVID −19 Anxiety Assessment§ | X | X | X | X | X |
Alternative administration schedules exist for staged surgical intervention, with the postoperative assessments being reset following the final staged treatment procedure.
*Baseline questionnaires administered within 1 week of study index operation.
†Validated questionnaires in the paediatric population.
‡Validated questionnaire in the adult population.
§Single question on a 5-point Likert scale, ‘How concerned are you about COVID impacting your life?’.
DVSS, Dysfunctional Voiding Scoring System; PROMIS, Patient-Reported Outcome Measure Information System; QUIKSS, Questionnaire for Urinary Issues–Kidney Stone Surgery.
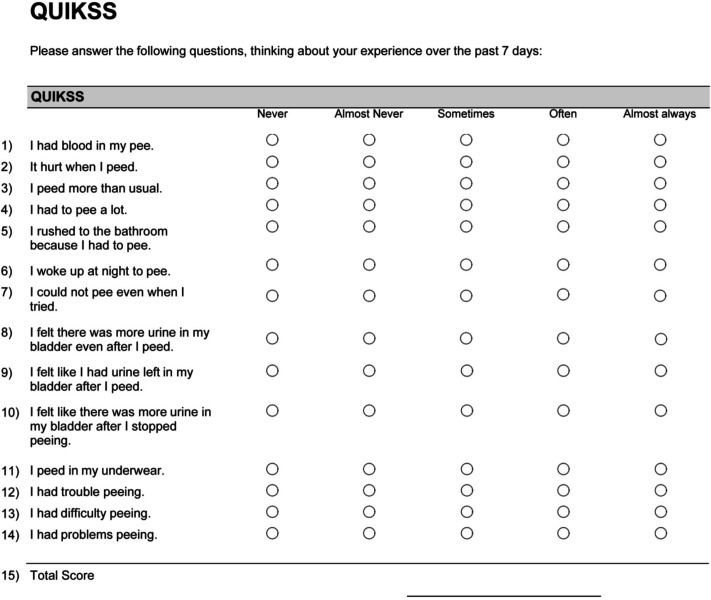
Acknowledging the DVSS may not assess certain urinary symptoms (eg, haematuria and dysuria), the PFP and content were asked to provide input on key concerns following recovery from previous kidney stone surgery, resulting in development in the Questionnaire for Urinary Issues–Kidney Stone Surgery (QUIKSS) (figure 3). Data collected from QUIKSS will be iteratively evaluated for reliability and reproducibility throughout the time course of the trial using DVSS and PROMIS scores as referents, although we do not at this time plan to fully validate this instrument.
Figure 3.
QUIKKS. QUIKKS, Questionnaire for Urinary Issues–Kidney Stone Surgery.
PRO assessment will be administered via the Research Electronic Data Capture (REDCap) system in order to minimise questionnaire burden and to enable near real-time assessment.31 32 Participants undergoing staged surgery will complete PROs 1 week after their first procedure. After their second procedure, participants will complete all assessments at the standard timelines benchmarked using the second procedure date.
Additional outcomes include healthcare use, such as clinic visits, acute care evaluations, hospital admissions and secondary procedures. These outcomes will be ascertained by a patient or caregiver self-report and abstraction from the EHR.33–35 Centers for Disease Control and Prevention definitions for nosocomial urinary tract infections and multidrug resistant organisms will be used.36 37
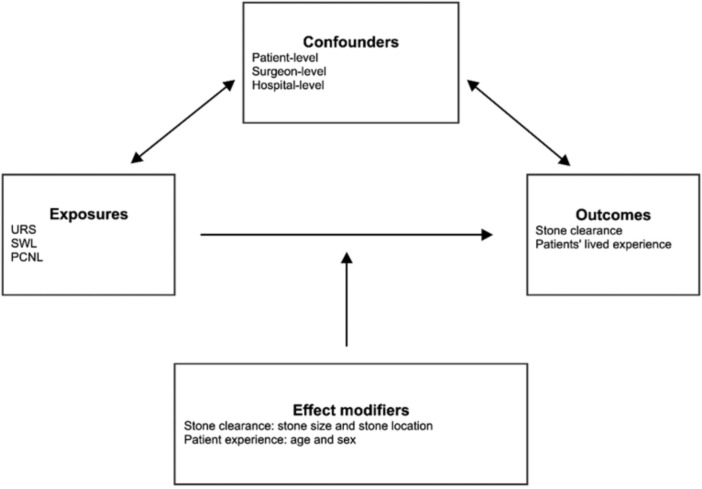
Confounders and effect modifiers
Many factors influence the selection of surgical intervention such as surgeon preference, local culture, patient comorbidities or kidney stone characteristics. The directed acyclic graph (figure 4) diagrams the hypothesised causal pathway between the interventions and outcomes. Therefore, we will measure baseline demographic, medical and kidney-stone specific histories provided by the participants and/or caregivers. Patients will complete a baseline intake questionnaire reflecting their medical history and prior surgical interventions. This questionnaire was reviewed for clarity by the PFP group. Medical comorbidities will be assessed via self-report and EHR-based data abstraction in a structure mirroring the National Surgical Quality Improvement Program-Paediatric surgical risk calculator.38 Surgeon characteristics (eg, experience, preferences for certain procedures, value placed on particular outcomes and complications) will be obtained by questionnaires completed by all participating urologists prior to study onset. Each site will submit a comprehensive assessment of the characteristics of the health system in which they practice (eg, surgical volume, presence of a multidisciplinary stone centre and availability of a particular surgical equipment).
Figure 4.
Conceptual framework for evaluating the effectiveness of URS, SWL and PCNL with factors that influence the impact on choice of surgical intervention and outcomes. PCNL, percutaneous nephrolithotomy; SWL, shockwave lithotripsy; URS, ureteroscopy.
Analgesic use is an important aspect of the patient experience, given the current focus on postoperative opioid use following urological surgery.39 Medication administration at the time of and following surgery will be assessed daily for up to 1 week postoperatively, based on the medication log developed for the Study to Enhance Understanding of Stent-associated Symptoms within the USDRN.40 Additionally, all participants >11 years of age will receive the PROMIS Prescription Pain Medication Misuse at the 12-week time point, which is a validated seven-item instrument intended to identify prescription pain medicine misuse.41
The COVID-19 pandemic has led to unprecedented challenges in healthcare, including shifts in management for routine medical conditions,42 limitations on research activity43 and increased levels of pandemic-related stress,44 all three of which may impact various aspects of delivery of surgical interventions and patients’ experiences. To this end, PKIDS will evaluate the impact of COVID-19 on three levels: (1) limitations on healthcare access, (2) limitations on research study conduct and (3) patient-based anxiety due to COVID-19 (table 2).
Data quality control during enrolment
During enrolment, distributions of each variable to be included in the analysis will be evaluated, aggregated across treatment groups and trial sites, to identify any outlying values that may require reconciliation. To the extent possible, inaccuracies will be resolved, and the database will be updated with the correct values. Data that are clearly incorrect but cannot be validated will be excluded from the analyses. Data that are unusual but not impossible and cannot either be verified or corrected will remain in the analysis. PRO tracking is enabled through REDCap and will be monitored by individual site study teams.
Interim analyses
All analyses will be conducted at the completion of the study as this pragmatic trial is embedded within clinical care and there would be no anticipated benefit to interim analyses.
Primary analysis of stone clearance
We will evaluate differences in stone clearance at 6 weeks after definitive stone surgery across treatments using logistic regression models weighted by the inverse of the estimated propensity score (see further). Should the number of ultrasounds that fall within the intended window of 4–8 weeks provide insufficient power for the analysis of stone clearance, we will extend the window to include all ultrasound imaging obtained within 3 months. Random intercepts will be used to account for the potential correlation among patients within the same hospital and patients operated on by the same surgeon.45–47 We will calculate the estimated OR with 95% CIs in stone clearance between ureteroscopy and shockwave lithotripsy and between percutaneous nephrolithotomy and shockwave lithotripsy, adjusting for potential confounders. Propensity score methods will be used to control potential confounders ascertained prior to surgery, using polytomous (multinomial) logistic regression based on the confounders at patient, surgeon and hospital levels. Additionally, we will examine modifiable operative techniques, within each treatment, that may improve stone clearance.
Primary analysis of PROs
The PROMIS measures will be scored using the Bayesian expected a posteriori estimation procedure48 and calibrated into the PROMIS T-scale.49 50 Weighted generalised linear mixed effects models will be used to test the difference in T-scores for each PROMIS measure and degree of urinary symptoms after surgery across treatments. We will use random intercepts to account for potential correlation among patients within the same hospital and surgeon. Separate models will be built for outcomes at 1, 3 and 6 weeks and 3 months after surgery. The comparison across treatments will be conducted similarly as in the primary analysis. We will calculate the SE of measurement (SEM) using PROs at baseline and use contingency tables to compare the proportion of patients whose score change exceeds 1 SEM across treatments at each time point after surgery. The change of PROs for more than 1 SEM is considered an approximation of the clinically meaningful minimum difference.51 52
Heterogeneity of treatment effect for stone clearance
We will test for pairwise interactions between the treatment and stone size and location, respectively, based on models constructed in the primary analysis. Subsequently, treatment effects will be estimated within each subgroup of stone size and location should any interaction be significant. Additionally, we will examine treatment-specific modifiable techniques that may improve stone clearance.
Analysis of medication administration, resource use and complications
These outcomes will be compared across treatments using weighted zero-inflated negative binomial regression models. The zero-inflated model can account for the large number of zero events for most of the patients, and the negative binomial regression model is more flexible than Poisson regression model, as it allows conditional variance of the rate of event to be different from the conditional mean.
Methods to control confounders, process evaluations, addressing missing data and secondary analysis
Because of the heterogenous nature of the prospective clinical trial design, specific a priori plans to control for cofounding, assess the heterogeneity of surgical approaches, address data missingness and perform secondary analysis are described in the online supplemental methods.
bmjopen-2021-056789supp002.pdf (159.2KB, pdf)
Ethics and dissemination
Data abstraction, access and storage
All data are stored using encrypted, secured and regulatory-approved platforms and methods via the REDCap platform. Data will be available to the funding agency as well as PKIDS investigators, as approved by the data coordinating centre and the publications and study initiation committee of PKIDS.
Regulatory and study oversight
The data coordinating centre (Children’s Hospital of Philadelphia) maintains the central institutional review board (IRB) approval (IRB # 19–0 16 832), on which all other sites rely with acknowledgement from individual IRBS for local context (see online supplemental regulatory information). Updates to the trial protocol will be approved by the central IRB and then communicated to relying sites. As there are no risks beyond data security and privacy, a data safety monitoring plan has been implemented in lieu of an external data safety monitoring board, overseen by the data coordinating centre. Consent and assent (when applicable) will be obtained by appropriately trained and registered study team members. Consent will occur prior to, up to the day of, surgical intervention via remote or in-person protocols. Individuals will be offered to opt in to allow for contact regarding future studies performed by the PKIDS network.
bmjopen-2021-056789supp003.pdf (55.9KB, pdf)
Dissemination
Results will be reviewed with participating clinicians, researchers and the PFP, who will contribute to development of clinical guidelines to be disseminated at regional, national and international urological meetings as well as to be considered by the AUA Guidelines Committee. Authorship will be determined by the International Committee of Medical Journal Editors’ guidelines.53
Discussion
The lack of high-level patient-focused evidence on the comparative effectiveness of surgical interventions for paediatric nephrolithiasis impairs shared decision making about the choice of surgical intervention, introduces uncertainty about intra-operative technical choices that lead to better outcomes, and precludes development of effective post-operative management strategies that improve patient experiences. To bridge these knowledge gaps, the PKIDS network has initiated a pragmatic clinical trial co-produced by patients and caregivers and embedded in clinical care to compare the effectiveness of these procedures. The real-world evidence generated will contribute substantially improve patient-centred outcomes and facilitate shared decision-making processes. Specifically, our primary aim will elucidate the most effective treatment to remove stones based on stone size and location, while our secondary aim will provide comparative data on patient experiences following surgical interventions. Both aspects of clinical care will inform treatment recommendations, including enhancing shared decision making when stone clearance outcomes are equal across modalities. Furthermore, PKIDS provides an infrastructure to incorporate best practices at each of the participating 26 sites and to rapidly disseminate evidence and reappraise subsequent outcomes, thus achieving a surgical learning cycle.10 54
Of interest to the broader scientific community, PKIDS offers a model of a collaborative learning health network, which offers several advantages over the traditional model of RCTs in the generation and dissemination of knowledge. While RCTs are regarded as yielding the strongest evidence for efficacy and effectiveness, the methodological limitations of RCTs make such efforts impractical to evaluate the comparative effectiveness in certain clinical situations, such as procedural interventions where clinical equipoise does not exist, rare disease or high-intensity situations with potentially vulnerable populations including children.55–57 Furthermore, RCTs are highly structured environments that frequently produce results not reflective of real-world practice and often have limited accrual, resulting in trial failure.58 59 A prospective observational trial with extensive characterisation of providers, patients and health systems that incorporate principles of learning health systems has the potential to reflect real-world care, improve enrolment and provide for a platform of knowledge generation and application.
Patient engagement in research design further enhances the feasibility and impact of trial design by creating constructive frameworks for education, informed consent and trial design.60 Integrating research within a collaborative learning health system has been particularly valuable for paediatric and rare diseases, empowering colearning across a diverse and experienced network of collaborators.17 For instance, patient reflections on the informed consent process during randomisation for high-acuity neonatal trials have suggested lapses and misunderstanding in the consent process, situations that were potentially further complicated by placing burden of consent for a child on the parent(s). These circumstances pose both practical and ethical dilemmas to recruitment.56 Embedding a prospective cohort trial within clinical care may alleviate parental or patient concerns regarding randomisation, allowing the care team and patients to focus on clinical care.
Our goal to improve patient-centred outcomes is reflected by our choice of endpoints. PROs are not frequently used in comparative effectiveness studies for kidney stone disease.61 We have involved patients and caregivers in the research process to heighten the relevance and impact of the study results. Stone clearance is a key clinical outcome for assessing success following interventions for nephrolithiasis, as residual fragments may result in symptomatic stone events or need for subsequent surgery.62–64 Prior studies in children have been limited by heterogeneity in definitions of stone clearances as well as imaging modalities to access for residual fragments. By standardising follow-up imaging processes and applying an unambiguous a priori-stated definition of stone clearance, we aimed to minimise heterogeneity yet still generate real-world data. Second, the PKIDS trial, for the first time, will assess patient experiences after surgery using a comprehensive patient-prioritised set of outcome measures of physical, social and emotional health. These measures were selected by our collaborating patient and caregiver stakeholders and thus represent outcomes that matter most to youth following surgery for kidney stones. These data will provide invaluable information to improve shared decision making about the choice of surgical intervention and will also support surgeons’ intraoperative making.
Knowledge dissemination and integration remain major barriers to improving care following traditional RCTs. These challenges are even more problematic for surgical intervention due to procedural learning curves and the rapid promulgation of technology.65 The PKIDS network, by applying the principles of learning health systems, can enable rapid knowledge generation and application throughout participating institutions by providing process and outcomes assessments at individual, institutional and network-wide levels, identifying surgical best practices, and encouraging care improvement via iterative plan–do–study–act cycles.10 This engagement will be accomplished by engaging key individuals such as site investigators and research coordinators at each step in the study design and conduct, thereby engendering a robust collaborative culture and an infrastructure for centralised data management and decentralised implementation.
Our trial design is limited by the non-randomised design, which may result in unmeasured confounding and selection bias. We mitigate this risk by deeply phenotyping patients, surgeons and health systems, data which are unavailable in administrative datasets or registries. Furthermore, inverse probability treatment weighting methodology to balance treatment groups and multiple planned sensitivity analyses will further reduce confounding and bias and increase rigour. Additionally, management of such large volumes of data pose challenges in terms of both data acquisition and missingness. We address these challenges through a multimodal approach to data acquisition that included EHR-based data abstraction, technical reports of procedures completed by surgeons and self-report from patients. These procedures have the dual purpose of decreasing missingness while reducing the burden on clinician and research team members. Finally, the PRO schedule is ambitious and places additional burden on patients and families in the surgical recovery period. However, we have collaborated with our PFPs to select highly relevant PROs and to optimise time points of assessment. Additionally, our trial is powered to accommodate our anticipated questionnaire drop-out rate.
In conclusion, a prospective pragmatic clinical trial of the comparative effectiveness of surgeries for paediatric nephrolithiasis has the potential to generate high-level evidence and to establish a surgical learning cycle. A collaborative learning health system model of comparative effectiveness research could be applied to other areas of investigation, particularly in patient populations or interventions where the traditional research model may be ill-suited to optimise the timely, patient-centred impact of study findings.
Footnotes
Twitter: @ReneaSturm
Collaborators: The authors acknowledge the members of the PKIDS Data Coordinating Centre as well as PKIDS principle and coinvestigators for their investment in this project, without which this work would not be feasible: Arun K Srinivasan, MBBS, MRCS; Michelle Denburg, MD, MSCE; Susan J Back, MD; Amy Kratchman MD; Christina B Ching, MD; William Robert DeFoor, Jr, MD, MPH; Ahmad H Bani-Hani, MD; Pamela I Ellsworth, MD; Andrew A Stec, MD; Nicolás Fernández MD, PhD; Kyle Rove, MD; Caleb P Nelson, MD, MPH; Douglas E Coplen, MD; Christopher E Bayne, MD; Pankaj P Dangle, MD; Aaron Krill, MD; Linda A Baker, MD; Nicolette K Janzen MD; Abby S Taylor, MD; Wolfgang H Cerwinka, MD; Eric D Nelson, MD; Justin B Ziemba, MD; Pasquale Casale, MD, MHA; Rosalia Misseri, MD; Kate H Kraft, MD; Bhalaajee Meenakshi-Sundaram, MD; Armando Lorenzo, MD; and Antoine Selman Fermin, MD, CCRP.
Contributors: Protocol design, protocol review and approval, and Critical manuscript review: JSE, ML, DIC, CF, JH, MK, TL, RS, GT, HB, RB, LK, AKu and AKr, PKIDS Care Improvement Network Investigators. Funding support: GT and CF. Manuscript production: JSE, ML, DIC, CF, JH, MK, TL, RS and GT.
Funding: The PCORnet Designated Study reported in this publication was conducted using PCORnet, the National Patient-Centred Clinical Research Network. PCORnet has been developed with funding from the Patient-Centered Outcomes Research Institute (PCORI). The study was funded by PCORI through PCORI Award (CER-2018C3-14778).
Disclaimer: The views, statements and opinions presented in this Viewpoint are solely the responsibility of the authors and do not necessarily represent the views of other organisations participating in, collaborating with or funding PCORnet or of the Patient-Centered Outcomes Research Institute (PCORI). PCORI was not involved in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Competing interests: JSE is a consultant for Dicerna Pharmaceuticals and Alnylam Pharmaceuticals. TL is cofounder of MicrobiomX and Singletto. GT is on the Scientific Advisory Board for Allena Pharmaceuticals, Dicerna Pharmaceuticals and Novome Biotechnology. The other authors have no relevant conflicts of interest to disclose.
Patient and public involvement: Patients and the public were involved in the design, conduct, reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
the Pediatric KIDney Stone Care Improvement Network:
Arun K Srinivasan, Michelle Denburg, Susan J Back, Amy Kratchman, Christina B Ching, William Robert DeFoor, Ahmad H Bani-Hani, Pamela I Ellsworth, Andrew A Stec, Nicolás Fernández, Kyle Rove, Caleb P Nelson, Douglas E Coplen, Christopher E Bayne, Pankaj P Dangle, Aaron Krill, Linda A Baker, Nicolette K Janzen, Abby S Taylor, Wolfgang H Cerwinka, Eric D Nelson, Justin B Ziemba, Pasquale Casale, Rosalia Misseri, Kate H Kraft, Bhalaajee Meenakshi-Sundaram, Armando Lorenzo, and Antoine Selman Fermin
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Tasian GE, Ross ME, Song L, et al. Annual incidence of nephrolithiasis among children and adults in South Carolina from 1997 to 2012. Clin J Am Soc Nephrol 2016;11:488-96. 10.2215/CJN.07610715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: American urological Association/Endourological Society guideline, part I. J Urol 2016;196:1153–60. 10.1016/j.juro.2016.05.090 [DOI] [PubMed] [Google Scholar]
- 3. Silay MS, Ellison JS, Tailly T, et al. Update on urinary stones in children: current and future concepts in surgical treatment and shockwave lithotripsy. Eur Urol Focus 2017;3:164–71. 10.1016/j.euf.2017.07.005 [DOI] [PubMed] [Google Scholar]
- 4. He Q, Xiao K, Chen Y, et al. Which is the best treatment of pediatric upper urinary tract stones among extracorporeal shockwave lithotripsy, percutaneous nephrolithotomy and retrograde intrarenal surgery: a systematic review. BMC Urol 2019;19:98. 10.1186/s12894-019-0520-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schaeffer AJ, Freeman M, Giambarresi L. Introduction to the National urology research agenda: a roadmap for priorities in urological disease research. Philadelphia, PA: Wolters Kluwer, 2010. [DOI] [PubMed] [Google Scholar]
- 6. ClinicalTrials.gov . Pediatric kidney stone (PKIDS) care improvement network (PKIDS) Bethesda MD: National library of medicine (US), 2020. Available: https://clinicaltrials.gov/ct2/show/NCT04285658
- 7. Baird R, Eeson G, Safavi A, et al. Institutional practice and outcome variation in the management of congenital diaphragmatic hernia and gastroschisis in Canada: a report from the Canadian pediatric surgery network. J Pediatr Surg 2011;46:801–7. 10.1016/j.jpedsurg.2011.02.008 [DOI] [PubMed] [Google Scholar]
- 8. Routh JC, Joseph DB, Liu T, et al. Variation in surgical management of neurogenic bowel among centers participating in national spina bifida patient registry. J Pediatr Rehabil Med 2017;10:303–12. 10.3233/PRM-170460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang H-HS, Huang L, Routh JC, et al. Shock wave lithotripsy vs ureteroscopy: variation in surgical management of kidney stones at freestanding children's hospitals. J Urol 2012;187:1402–7. 10.1016/j.juro.2011.12.010 [DOI] [PubMed] [Google Scholar]
- 10. Tasian GE, Ellison JS, Pediatric KIDney Stone (PKIDS) Care Improvement Network . The surgical improvement cycle: improving surgical outcomes through partnerships and rigor. J Urol 2021;205:1554-1556. 10.1097/JU.0000000000001626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Britto MT, Fuller SC, Kaplan HC, et al. Using a network organisational architecture to support the development of learning healthcare systems. BMJ Qual Saf 2018;27:937–46. 10.1136/bmjqs-2017-007219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Forrest CB, Margolis PA, Bailey LC, et al. PEDSnet: a national pediatric learning health system. J Am Med Inform Assoc 2014;21:602–6. 10.1136/amiajnl-2014-002743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Forrest CB, Margolis P, Seid M, et al. PEDSnet: how a prototype pediatric learning health system is being expanded into a national network. Health Aff 2014;33:1171–7. 10.1377/hlthaff.2014.0127 [DOI] [PubMed] [Google Scholar]
- 14. Freton L, Peyronnet B, Arnaud A, et al. Extracorporeal shockwave lithotripsy versus flexible ureteroscopy for the management of upper tract urinary stones in children. J Endourol 2017;31:1–6. 10.1089/end.2016.0313 [DOI] [PubMed] [Google Scholar]
- 15. Dogan HS, Altan M, Citamak B, et al. A new nomogram for prediction of outcome of pediatric shock-wave lithotripsy. J Pediatr Urol 2015;11:84 e1–6. 10.1016/j.jpurol.2015.01.004 [DOI] [PubMed] [Google Scholar]
- 16. Bilen CY, Koçak B, Kitirci G, et al. Percutaneous nephrolithotomy in children: lessons learned in 5 years at a single institution. J Urol 2007;177:1867–71. 10.1016/j.juro.2007.01.052 [DOI] [PubMed] [Google Scholar]
- 17. Seid M, Hartley DM, Margolis PA. A science of collaborative learning health systems. Learn Health Syst 2021;5. 10.1002/lrh2.10278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Irwin DE, Stucky BD, Thissen D, et al. Sampling plan and patient characteristics of the PROMIS pediatrics large-scale survey. Qual Life Res 2010;19:585–94. 10.1007/s11136-010-9618-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hardin AP, Hackell JM, Committee On P, COMMITTEE ON PRACTICE AND AMBULATORY MEDICINE . Age limit of pediatrics. Pediatrics 2017;140. 10.1542/peds.2017-2151. [Epub ahead of print: 21 08 2017]. [DOI] [PubMed] [Google Scholar]
- 20. Fulgham PF, Assimos DG, Pearle MS, et al. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. J Urol 2013;189:1203-13. 10.1016/j.juro.2012.10.031 [DOI] [PubMed] [Google Scholar]
- 21. Masch WR, Cohan RH, Ellis JH, et al. Clinical effectiveness of prospectively reported sonographic Twinkling artifact for the diagnosis of renal calculus in patients without known urolithiasis. AJR Am J Roentgenol 2016;206:326–31. 10.2214/AJR.15.14998 [DOI] [PubMed] [Google Scholar]
- 22. Gliga ML, Chirila CN, Podeanu DM, et al. Twinkle, Twinkle little stone: an artifact improves the ultrasound performance! Med Ultrason 2017;19:272–5. 10.11152/mu-984 [DOI] [PubMed] [Google Scholar]
- 23. Scales CD, Desai AC, Harper JD, et al. Prevention of urinary stones with hydration (push): design and rationale of a clinical trial. Am J Kidney Dis 2021;77:898-906.e1. 10.1053/j.ajkd.2020.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dunmire B, Lee FC, Hsi RS, et al. Tools to improve the accuracy of kidney stone sizing with ultrasound. J Endourol 2015;29:147–52. 10.1089/end.2014.0332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dunmire B, Harper JD, Cunitz BW, et al. Use of the acoustic shadow width to determine kidney stone size with ultrasound. J Urol 2016;195:171-7. 10.1016/j.juro.2015.05.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Raman JD, Bagrodia A, Gupta A, et al. Natural history of residual fragments following percutaneous nephrostolithotomy. J Urol 2009;181:1163–8. 10.1016/j.juro.2008.10.162 [DOI] [PubMed] [Google Scholar]
- 27. DeWalt DA, Gross HE, Gipson DS, et al. PROMIS(®) pediatric self-report scales distinguish subgroups of children within and across six common pediatric chronic health conditions. Qual Life Res 2015;24:2195–208. 10.1007/s11136-015-0953-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Broderick JE, DeWitt EM, Rothrock N, et al. Advances in Patient-Reported Outcomes: The NIH PROMIS(®) Measures. EGEMS 2013;1:1015. 10.13063/2327-9214.1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Park J, Shin DW, Chung JH, et al. Shock wave lithotripsy versus ureteroscopy for ureteral calculi: a prospective assessment of patient-reported outcomes. World J Urol 2013;31:1569–74. 10.1007/s00345-012-0966-2 [DOI] [PubMed] [Google Scholar]
- 30. Farhat W, Bägli DJ, Capolicchio G, et al. The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol 2000;164:1011–5. 10.1097/00005392-200009020-00023 [DOI] [PubMed] [Google Scholar]
- 31. Revicki DA, Cella DF. Health status assessment for the twenty-first century: item response theory, item banking and computer adaptive testing. Qual Life Res 1997;6:595–600. 10.1023/a:1018420418455 [DOI] [PubMed] [Google Scholar]
- 32. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Heo SM, Naylor JM, Harris IA, et al. Reliability of patient-reported complications following hip or knee arthroplasty procedures. BMC Med Res Methodol 2019;19:15. 10.1186/s12874-018-0645-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dokter EM, Goosen EE, van der Zanden LF, et al. Level of agreement on postoperative complications after one-stage hypospadias correction comparing medical records and parent reports. J Pediatr Surg 2019;54:1825–31. 10.1016/j.jpedsurg.2019.01.057 [DOI] [PubMed] [Google Scholar]
- 35. Dang KLT, Badge H, Harris IA. Validity of patient-reported complications after total hip and knee arthroplasty. J Orthop Surg 2018;26:2309499018802493. 10.1177/2309499018802493 [DOI] [PubMed] [Google Scholar]
- 36. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36:309–32. 10.1016/j.ajic.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 37. Magiorakos A-P, Srinivasan A, Carey RB, et al. Multidrug-Resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 2012;18:268–81. 10.1111/j.1469-0691.2011.03570.x [DOI] [PubMed] [Google Scholar]
- 38. Kraemer K, Cohen ME, Liu Y, et al. Development and evaluation of the American College of surgeons NSQIP pediatric surgical risk calculator. J Am Coll Surg 2016;223:685–93. 10.1016/j.jamcollsurg.2016.08.542 [DOI] [PubMed] [Google Scholar]
- 39. Tam CA, Dauw CA, Ghani KR, et al. New persistent opioid use after outpatient ureteroscopy for upper tract stone treatment. Urology 2019;134:103–8. 10.1016/j.urology.2019.08.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Scales CD, Lai HH, Desai AC, et al. Study to enhance understanding of Stent-Associated symptoms: rationale and study design. J Endourol 2021;35:761-768. 10.1089/end.2020.0776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Pilkonis PA, Yu L, Dodds NE, et al. An item bank for abuse of prescription pain medication from the patient-reported outcomes measurement information system (PROMIS®). Pain Med 2017;18:1516–27. 10.1093/pm/pnw233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tefik T, Guven S, Villa L, et al. Urolithiasis practice patterns following the COVID-19 pandemic: overview from the EULIS Collaborative research Working group. Eur Urol 2020;78:e21–4. 10.1016/j.eururo.2020.04.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Strujo E, Sanders M, Fiscella K, et al. COVID-19 impact on multi-site recruitment and enrollment. Clin Trials 2020;17:501–4. 10.1177/1740774520946270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kujawa A, Green H, Compas BE, et al. Exposure to COVID-19 pandemic stress: associations with depression and anxiety in emerging adults in the United States. Depress Anxiety 2020;37:1280–8. 10.1002/da.23109 [DOI] [PubMed] [Google Scholar]
- 45. Parzen M, Ghosh S, Lipsitz S, et al. A generalized linear mixed model for longitudinal binary data with a marginal logit link function. Ann Appl Stat 2011;5:449–67. 10.1214/10-AOAS390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000;11:550–60. 10.1097/00001648-200009000-00011 [DOI] [PubMed] [Google Scholar]
- 47. Kurth T, Walker AM, Glynn RJ, et al. Results of multivariable logistic regression, propensity matching, propensity adjustment, and propensity-based weighting under conditions of nonuniform effect. Am J Epidemiol 2006;163:262–70. 10.1093/aje/kwj047 [DOI] [PubMed] [Google Scholar]
- 48. Bock RD, Mislevy RJ. Adaptive EAP estimation of ability in a microcomputer environment. Appl Psychol Meas 1982;6:431–44. 10.1177/014662168200600405 [DOI] [Google Scholar]
- 49. Varni JW, Stucky BD, Thissen D, et al. Promis pediatric pain interference scale: an item response theory analysis of the pediatric pain item bank. J Pain 2010;11:1109–19. 10.1016/j.jpain.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol 2010;63:1179–94. 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wyrwich KW, Tierney WM, Wolinsky FD. Further evidence supporting an SEM-based criterion for identifying meaningful intra-individual changes in health-related quality of life. J Clin Epidemiol 1999;52:861–73. 10.1016/s0895-4356(99)00071-2 [DOI] [PubMed] [Google Scholar]
- 52. Wyrwich KW, Nienaber NA, Tierney WM, et al. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care 1999;37:469–78. 10.1097/00005650-199905000-00006 [DOI] [PubMed] [Google Scholar]
- 53. Editors ICoMJ . Available: http://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html
- 54. Mullins CD, Abdulhalim AM, Lavallee DC. Continuous patient engagement in comparative effectiveness research. JAMA 2012;307:1587–8. 10.1001/jama.2012.442 [DOI] [PubMed] [Google Scholar]
- 55. Van Mieghem T, Ryan G. The PLUTO trial: a missed opportunity. Lancet 2013;382:1471–3. 10.1016/S0140-6736(13)61446-4 [DOI] [PubMed] [Google Scholar]
- 56. Snowdon C, Garcia J, Elbourne D. Making sense of randomization; responses of parents of critically ill babies to random allocation of treatment in a clinical trial. Soc Sci Med 1997;45:1337–55. 10.1016/s0277-9536(97)00063-4 [DOI] [PubMed] [Google Scholar]
- 57. Wallis CJD, Detsky AS, Fan E. Establishing the effectiveness of procedural interventions: the limited role of randomized trials. JAMA 2018;320:2421–2. 10.1001/jama.2018.16329 [DOI] [PubMed] [Google Scholar]
- 58. Bandari J, Theisen KM, Maganty A, et al. Clinical trials in urology: predictors of successes and failures. J Urol 2020;204:805–10. 10.1097/JU.0000000000001072 [DOI] [PubMed] [Google Scholar]
- 59. Ingelfinger JR, Stapleton FB. Antibiotic prophylaxis for vesicoureteral reflux--answers, yet questions. N Engl J Med 2014;370:2440–1. 10.1056/NEJMe1404774 [DOI] [PubMed] [Google Scholar]
- 60. Lawton J, Snowdon C, Morrow S, et al. Recruiting and consenting into a peripartum trial in an emergency setting: a qualitative study of the experiences and views of women and healthcare professionals. Trials 2016;17. 10.1186/s13063-016-1323-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ellison JS, Williams M, Keeley FX. Patient-Reported outcomes in nephrolithiasis: can we do better? J Endourol 2018;32:10–20. 10.1089/end.2017.0241 [DOI] [PubMed] [Google Scholar]
- 62. Iremashvili V, Li S, Penniston KL, et al. Role of residual fragments on the risk of repeat surgery after flexible ureteroscopy and laser lithotripsy: single center study. J Urol 2019;201:358–63. 10.1016/j.juro.2018.09.053 [DOI] [PubMed] [Google Scholar]
- 63. Dincel N, Resorlu B, Unsal A, et al. Are small residual stone fragments really insignificant in children? J Pediatr Surg 2013;48:840–4. 10.1016/j.jpedsurg.2012.07.061 [DOI] [PubMed] [Google Scholar]
- 64. El-Assmy A, El-Nahas AR, Harraz AM, et al. Clinically insignificant residual fragments: is it an appropriate term in children?. Urology 2015;86:593–8. 10.1016/j.urology.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 65. Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a MAP? J Contin Educ Health Prof 2006;26:13–24. 10.1002/chp.47 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056789supp001.pdf (38.8KB, pdf)
bmjopen-2021-056789supp002.pdf (159.2KB, pdf)
bmjopen-2021-056789supp003.pdf (55.9KB, pdf)