Abstract
Objective
To define the prevalence and seizure subtypes among children with cerebral palsy (CP) in rural Bangladesh and explore barriers to optimum epilepsy control.
Design
Prospective cohort study.
Setting
The study was conducted in Shahjadpur, a rural subdistrict of Bangladesh.
Participants
Children (<18 years) with CP and epilepsy identified using the Bangladesh CP Register (BCPR) in the study site.
Methods
Assessments were conducted in three focused epilepsy clinics overseen by a paediatric neurologist between December 2016 and January 2018, with intervening phone and video-conference follow-ups. Details of event type, frequency and medication compliance were collected. Antiepileptic drugs (AEDs) were prescribed based on seizure type, family income, comorbidity and medication availability.
Results
23.4% (170/726) of the BCPR cohort had a clinical diagnosis of epilepsy of whom 166 were assessed. Following the focused epilepsy clinics, 62.0% (103/166) children were clinically determined to have ongoing epileptic seizures. 62.1% (64/103) had generalised onset tonic clonic seizures, 27.2% (28/103) had focal onset seizures with impaired awareness and 10.7% (11/103) had other seizure types. None of the children with prolonged seizures (31/103) had an emergency seizure management plan. Non-epileptic events were being pharmacologically treated as seizures in 18.1% (30/166) children. Financial constraints were the main reason for non-compliance on follow-up.
Conclusions
Gaps in optimum epilepsy management in rural Bangladesh are amenable to improvement anchored with local healthcare workers. Training and clinical care focused on recognition of common seizure types, seizure mimics and rationalising use of available AEDs can be facilitated by better referral pathways and telehealth support.
Keywords: Epilepsy, Developmental neurology & neurodisability, PUBLIC HEALTH
Strengths and limitations of this study.
Children with cerebral palsy and epilepsy identified through an ongoing population-based surveillance.
Specialist clinical assessments were conducted overseen by a paediatric neurologist.
Phone follow-ups were conducted.
The study provided opportunity for continuing local capacity building.
The clinical diagnoses relied on clinical impression and were not corroborated by investigations.
Introduction
Cerebral palsy (CP) is a term that defines a heterogeneous group of early-onset, non-progressive, neurodevelopmental disorders secondary to injury to the developing brain.1 Studies show that among children with CP epilepsy is associated with greater impairment of cognitive function, poorer motor outcomes, more profound behavioural and psychological problems, and poorer quality of life, all of which collectively contribute to a greater burden of disability and care.2 In comparison to children with epilepsy only, children with CP and epilepsy tend to have early onset of seizures which can often be difficult to control.3
Recent estimates from a population-based study in Bangladesh showed a high burden of CP with an estimated prevalence of 3.4 per 1000 children.4 Bangladesh is one of the most densely populated and under resourced countries in the world.5 WHO classified Bangladesh as one of the countries with severe shortages of health workers. There is inequity in the skill mix and distribution of health workers between urban and rural Bangladesh.6 One of the four axes of the value-based framework for global health delivery highlights the need for alignment of care delivery to the local context.7
Resources for the diagnosis and management of neurologic disorders such as epilepsy are often limited in low-income and middle-income countries such as Bangladesh.8 Several aspects of epilepsy management that may be considered routine in tertiary or specialist settings are not applicable to community-based settings.9 There is a substantial epilepsy treatment gap in low resource settings owing to a wide spectrum of factors including shortage of doctors particularly in the rural areas,6 lack of available investigation and inpatient treatment facilities as well as decreased service utilisation due to the stigma around a disability diagnosis.10
We aimed to define the prevalence, clinical phenotypes and barriers to optimum epilepsy control among children with CP in a community-based setting in Bangladesh.
Methods and analysis
Cohort compilation
We used the Bangladesh CP Register (BCPR); a prospective population-based surveillance of children with CP in Shahjadpur a northern subdistrict of Rajshahi division in Bangladesh for identification of children with CP and epilepsy.
Medical assessment camps are conducted on a regular basis in the surveillance sites for BCPR. A multidisciplinary medical assessment team including a paediatrician, a physiotherapist, and a counsellor conduct detailed assessment for data collection for the BCPR. Data on the presence of associated impairments including epilepsy are also documented based on review of limited available medical records, report by the parents or primary caregivers of the children with CP, and clinical assessment by the medical assessment team. Detailed account of the BCPR study protocol and findings have been described in previous publications.4
During the BCPR medical assessment camps preceding this study, a diagnosis of epilepsy had been based on history of one or more unprovoked seizures in the previous 3 months recorded by medical practitioners and review of any available medical records.4
Clinical assessment of epilepsy
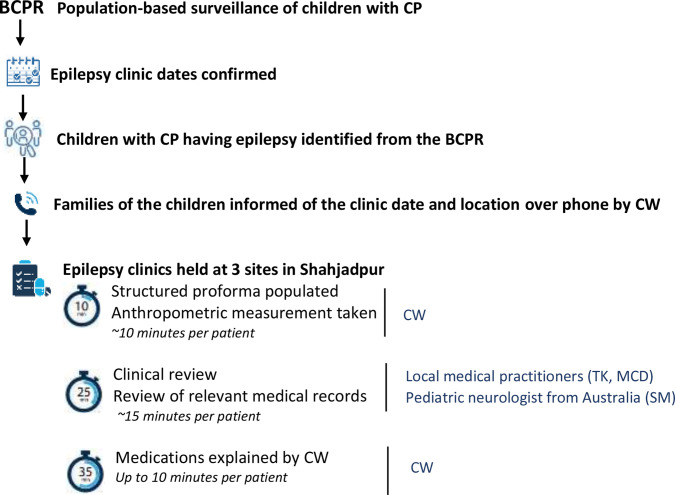
Children with CP and epilepsy identified via the BCPR were clinically reviewed in three focused epilepsy clinics held for 3 days each time at three different locations within the BCPR study site. Specialist clinical assessments at the clinics were overseen by a paediatric neurologist from Australia (SSM) who travelled to Bangladesh for the focused epilepsy clinics during the study period. Diagnoses of epilepsy and seizure like events were reviewed during assessment in the clinics. Details of seizure/event type, frequency, medication use and compliance were collected according to a predesigned standard proforma (online supplemental appendix A). Workflow during the clinic is outlined in figure 1.
Figure 1.
Clinical assessment of epilepsy in children with CP in Shahjadpur. BCPR Bangladesh Cerebral Palsy Register; CP cerebral palsy; CW community worker.
bmjopen-2021-052578supp001.pdf (213.2KB, pdf)
Local capacity building
Two physicians (TK and MCD) were trained by the paediatric neurologist in classifying seizure types according to the 2017 International League Against Epilepsy (ILAE) guidelines,11 demonstration of clinical signs during the epilepsy clinics, and discussions around seizure mimics and drug choice (online supplemental appendix B). One community worker based in the study area was also trained to conduct phone follow ups of the children on antiepileptic drugs (AEDs).
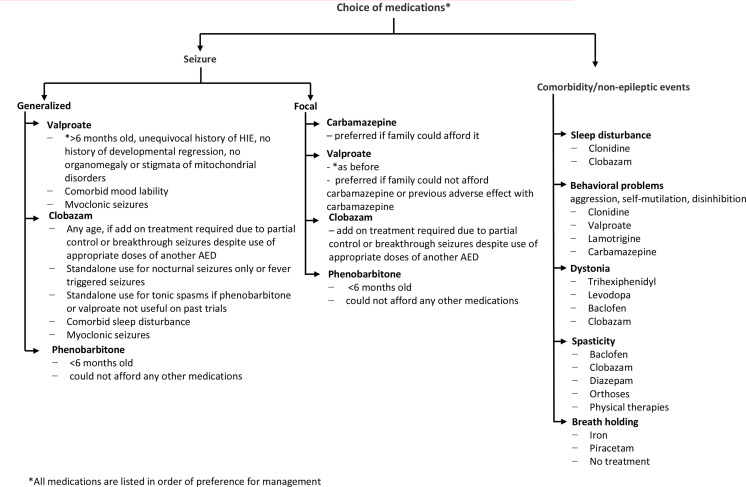
Selection of AED
Before the clinics, the community worker collected information on availability and cost of AED in local pharmacies within the study area between December 2016 and January 2018. A dose equivalence table was drawn up for easy prescription in the clinic along with notes on important side effects and interactions. During the clinics, AED were prescribed based on seizure type, medication availability and family income. The approach undertaken for shared decision making in AED prescription is outlined in figure 2.
Figure 2.
Suggested considerations in choice of medications for seizures and comorbidity in children with cerebral palsy. AED, antiepileptic drug.
Telehealth supported follow-up and clinics
Phone follow-up
Targeted phone follow ups of the children on AED were conducted by the trained community health worker every 3 months during the study period, following the initial specialist assessment at the focused epilepsy clinics. The phone follow ups were semi-structured. The design, conduct and the outcome measures for the follow ups were additionally informed by the study team’s experience and input from the primary caregivers (online supplemental appendix C). Seizure control was documented during phone follow ups. In our study seizure control was defined as no reported seizure between the clinic and follow-up.
Patient and public involvement
This work was informed by the priorities, experience and preferences of the primary caregivers of the children with CP and epilepsy who participated in the study. The design and implementation of the follow ups, including outcome measures important to the study participants, relied on feedback from families of children with CP and epilepsy. Baseline information was communicated to the primary caregivers by the study team. This informed shared decision making related to the treatment and follow-up for their children. Furthermore, the follow ups were conducted by a local community worker and local physician, which enhanced community involvement during and beyond the study.
Statistical analysis
Descriptive analyses were carried out. All statistical analysis was conducted using SPSS V.24 (IBM).
Results
Prevalence and basic demographic characteristics
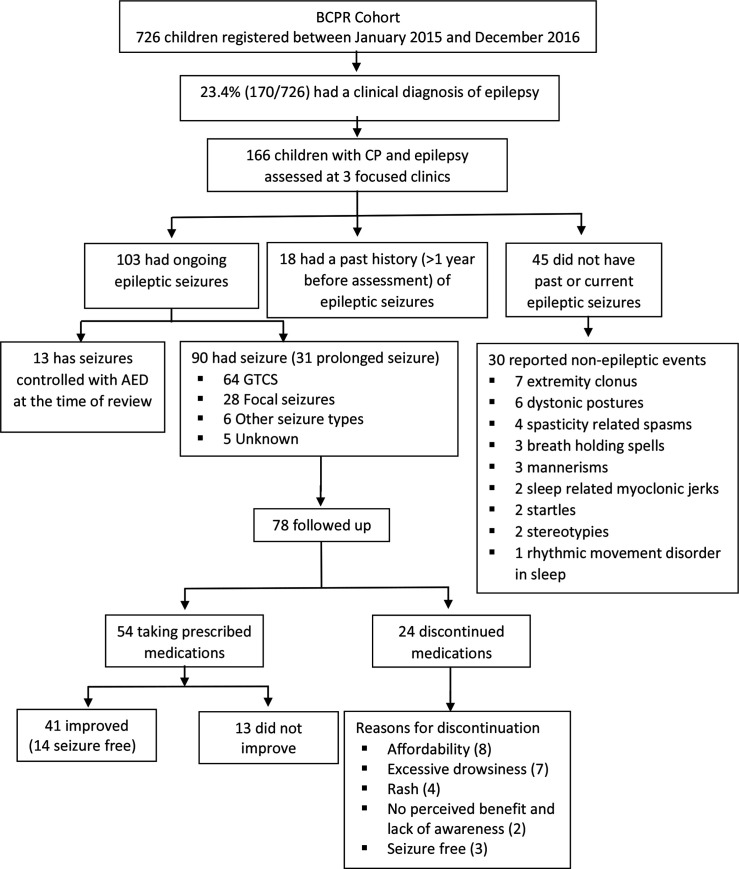
A total of 726 children with CP were registered into the BCPR between January 2015 and December 2016, 23.4% (170/726) of whom had a clinical diagnosis of epilepsy. A total of 166 of these children attended the three focused epilepsy clinics between December 2016 and January 2018 and form the study cohort. Fifty-five (33.1%) were female. The mean age of the children was 6 years 10 months (SD: 4 years 5 months) years.
After the focused epilepsy clinics, 62.0% (103/166) children were clinically determined to have ongoing epileptic seizures based on review of their history, existing medical records and specialist clinical evaluation (figure 3). Therefore, the revised prevalence of epilepsy among the BCPR cohort during the study period was 14.3%.
Figure 3.
Study diagram. AED, antiepileptic drugs; BPCR, Bangladesh Cerebral Palsy Register; CP, cerebral palsy; GTCS, generalised onset tonic clonic seizures.
Seizure subtypes
62.1% (64/103) had generalised onset tonic clonic seizure, 27.2% (28/103) had focal onset seizures with impaired awareness and 5.8% (6/103) had other seizure types (focal onset aware seizures, epileptic spasms, generalised onset myoclonic seizures and generalised onset tonic seizures). 11.6% (12/103) had multiple seizure types. Data on seizure type was unclear on history for 4.9% (5/103). At the time of first assessment, seizures were already controlled with AED in 5.8% (6/103) children. 30.1% (31/103) of children had a history of prolonged seizures (>30 min) and none of these patients had an emergency seizure plan. Their caregivers tended to wait at home till the seizures settled and did not seek emergency medical assistance due to geographical or financial constraints.
Barriers to optimum epilepsy control
Non-epileptic events among children with CP
Non-epileptic events were determined to have been mislabeled as seizures in 18.1% (30/166) children which included extremity clonus (n=7), dystonic postures (n=6), spasticity related spasms (n=4), breath holding spells (n=3), mannerisms (n=3), sleep related myoclonic jerks (n=2), startles (n=2), stereotypies (n=2) and rhythmic movement disorders in sleep (n=1). 23.3% (7/30) of these children were being treated with AED. AED was stopped for all seven of them. At follow-up none of them worsened, thereby, further confirming the misdiagnosis of epilepsy and unnecessary administration of AED to these children.
Epilepsy control
Of the 103 children with seizures, 62 were already on AEDs at the time of our clinical review. Polypharmacy with more than two concurrent AED was commonly observed and AED changes were made for the majority of them. Advised AED changes consisted of dose alteration in 54.8% (34/62) and medication change in 17.7% (11/62). 27.4% (17/62) were advised to continue treatment already initiated by various providers. We initiated treatment for 39/41 children not previously on AED who were clinically determined to still be having epileptic seizures; 2/41 only had short seizures once or twice a year and were not put on AED.
Telehealth supported follow-up and clinics
Phone follow-up
We were able to review 75.8% (78/90) children with epileptic seizures on follow-up during the study period. On follow-up (median 6.0 months), 69.2% (54/78) were taking prescribed medications as advised. Among them 75.9% (41/54) showed improvement in seizure control (>50% seizure reduction), including 14 children whose seizures were controlled. 30.8% (24/78) families had discontinued the advised treatment due to affordability (8/24, 33.3%), excessive drowsiness (7/24, 29.2%), development of a rash (4/24, 16.7%), no perceived benefit with medication and lack of understanding behind the use of regular medications (2/24, 8.3%). Three (3/24, 12.5%) children who discontinued medications were reported to no longer have seizures. None of the families reported any adverse effects that led to reported cardiorespiratory compromise, hospital presentation or death.
Two children from our cohort died during the follow-up period, one due to meningitis and the other due to a lower respiratory tract infection. Their cause of death was determined by verbal autopsy conducted as part of a separate study.12
Discussion
Epilepsy is a significant comorbidity in some individuals with CP. Previous studies have described a prevalence of 15%–90% epilepsy in CP cohorts.13 14 Methodological differences in identification of children with CP (population-based vs institutional based recruitment) and use of variable definitions of epilepsy in studies contribute further to the reported differences in rates of epilepsy among children with CP. The Australian CP register defined epilepsy as ‘two or more afebrile seizures before age 5 years; excluding neonatal seizures’ while other definitions for epilepsy used across the literature include use of AED, insurance claims and parent reported diagnosis.15 As one of the most common associated impairments of CP, we recommend the use of a harmonised definition that is, the ILAE definition for description of epilepsy within CP registers to enable accurate estimation of rates of and meaningful comparisons.
The rate of epilepsy observed among children with CP in our study is consistent with rates reported in other low-resource settings such as Indonesia where 13.5% of children with CP had epilepsy.16 The Australian CP Register reports that epilepsy was more common among children with postneonatally acquired CP compared with prenatally/perinatally acquired CP (50% vs 30%). This eludes into the potential role of antecedents of CP on the proportion of children with epilepsy in CP cohorts. There is a growing body of evidence on the differences in the prevailing risk factors and timing of acquisition of CP among children in low resource settings compared with high income countries.4 16 17 These factors are often associated with varied likelihood of having epilepsy, therefore, further contribute to the wide-ranging reported rates of epilepsy among children with CP globally.
Overall, epilepsy contributes more significantly to the global burden of disease in resource poor settings as evident from the 2015 Global burden of disease studies. We found an initial prevalence of epilepsy of 23.4% in our cohort. Interestingly, following reassessment in our clinics, as described, this was revised to 14.3%. Previous studies have also noted such discrepancy between determination of a clinical diagnosis of epilepsy between specialist and community-based settings with a misdiagnosis of epilepsy being made in as many as 25% of cases.18 This has flow on impacts as we noted in terms of incorrect, often excessive use of medications. Epilepsy poses substantial economic burden on families.19 When families devote a significant proportion of their finances, attention, time or all of these towards one aspect of their child’s management, other aspects of care such as physical therapy, nutrition, pain and musculoskeletal management are likely to be neglected, more so in resource poor settings.20
As demonstrated by recent innovative projects in neighbouring Nepal, education of community-level workers and general medical practitioners can lead to more consistent clinical diagnosis of epilepsy.21 In our experience, rationalisation or cessation of medications after focused clinical assessments led to changes in family finances diverted towards medication use. We envision that the development of simplified print and multimedia based educational resources for healthcare workers and medical practitioners hold the potential to improve epilepsy diagnosis in resource scarce settings such as our study site.
Polypharmacy with more than two concurrent AEDs is unlikely to contribute significantly to seizure control.22 In countries like Bangladesh with a mismatch of clinical care practices between urban and rural areas, the use of less conventional or alternative medications is very likely to be encountered.
AED availability is very limited in rural Bangladesh.23 Medications need to be purchased by families and hence, cost per month for AEDs is a significant consideration when choosing medications for chronic use to ensure good compliance. The cheapest and most readily available AEDs are phenobarbitone, clobazam and sodium valproate. If a diagnosis of CP is very likely based on clinical evaluation and history, earlier use of sodium valproate or clobazam in this setting is a viable option for transitioning from phenobarbitone which is most commonly prescribed in infancy. As outlined in our methods and figure 2, AED choice can be rationalised based not only on the seizure type but also existing comorbidity as some AEDs can help improve comorbid psychiatric symptoms or sleep disturbance.
Our experience highlighted a gap in the recognition and management of prolonged seizures in settings like ours compared with conventional management in urban and resource rich settings. Benzodiazepines are the mainstay of out of hospital, particularly health worker or parent led management of prolonged seizures. However, midazolam or lorazepam are not available at all in rural Bangladesh. Diazepam is only available in glass ampoules through restricted prescriptions in some pharmacy outlets. In our and wider reported experience caregivers are often reluctant to use glass ampoules or follow several steps in medication administration to a child at home.24 Other readily available benzodiazepines are cheap (clobazam: US$0.042 per 10 mg tablet and clonazepam: US$0.048 per 1 mg tablet; prices mid 2018) but there is very little evidence regarding their use in the setting of prolonged seizures.25 26 Status epilepticus can significantly add to the burden of cumulative brain injury and therefore warrants a solution.27 This may be in the form of a per-rectal, oral or, alternative routes for delivery of well-established medications for status epilepticus such as phenobarbitone, valproate or midazolam. Alternatively, the use of medications such as clonazepam drops via open label trials requires urgent exploration for such settings.
Our model has demonstrated that immediate positive impact on epilepsy management and reduction in burden of care on families can be achieved through structured assessments by medical and allied personnel who are trained to assess children for epilepsy and use available medications according to a structured framework. This can be achieved for a population base such as in our study area with limited personnel and without additional investigation or formalised healthcare facilities, though these would be desirable to further improve patient outcomes.
We piloted the use of videoconference-based telemedicine clinics after initial face to face clinics. Telemedicine clinics were initiated in May 2018 and held on a monthly basis using Skype as part of ongoing capacity building to improve epilepsy control among the study cohort. The local trained physician saw the patients face to face in the study site and used a handheld, internet connected tablet to videoconference with the paediatric neurologist in Australia. Patient interview for new and follow-up patients followed a set format (online supplemental appendix C). New patient data from the telemedicine clinics are not included in this paper. Five telemedicine clinics undertaken in 2018 contributed to patient follow-up and clinical capacity building. During these clinics 47 patients were seen by a local medical practitioner with internet-based videoconference support from the paediatric neurologist in Australia. Each clinic was of 3 hours duration during which patient interview was undertaken in the same manner as in the focused epilepsy clinics. Thirty minutes were marked during each clinic for discussion regarding clinical signs, history taking and AED choice. Clinical details for new patients reviewed during telemedicine clinics were not included in this cohort. These clinics created mentoring opportunity for the local team which is a substantial contribution towards for long-term sustainability. Unfortunately, this process was interrupted due to limited local team and patient mobility in 2020 and 2021 due to the pandemic, therefore, limiting structured data from this phase. We aim to resume this approach to maintain a sustainable model for ongoing care.
With some prior training in the use of a structured clinical approach, this method can be very time-efficient in reviewing patients led by a non-specialist medical practitioner/community worker and supported by a specialist. In our experience, this not only provided continuity of clinical support with existing personnel but also provided an opportunity for continuing professional development and capacity building. We hope that in the post-COVID era, implementation and incorporation of telemedicine should be easier and more acceptable to providers, policy-makers and the community.
We summarise the key barriers identified and proposed or already implemented solutions in table 1. Development of multimedia or mobile application-based resources that may simply illustrate clinical assessment of children with epilepsy, examples of non-epileptic events and emergency seizure management will provide convenient means for translation of our findings to the wider population in Bangladesh and, with language translation, to similar resource poor settings across the world.
Table 1.
Barriers to epilepsy control and suggested interventions
| Barriers | Suggested interventions |
| AED availability | Selection of locally available medications for management through a structured guideline |
| Lack of skilled personnel for epilepsy management and follow-up locally | Capacity building and engagement of local medical practitioners and community health workers Development of multimedia or mobile application-based resources Telemedicine |
| Affordability | Rationalisation of drugs |
| Poor treatment compliance | Rationalisation of drugs |
| Training and engagement of health workers for follow-up | |
| Caregiver education | |
| Prolonged seizure management | Development of guideline and resources for management of prolonged seizure for training of local health workers |
| Misidentification of non-epileptic episodes as seizures | Development of video resources describing seizures and non-epileptic events |
| Lack of parental understanding regarding epilepsy treatment | Parent education on epilepsy treatment |
AED, antiepileptic drug.
We have engaged with tertiary paediatric neurology centres in Bangladesh to support some families with requisite investigations or more frequent specialist review. However, this will always be limited to financial and logistic constraints of rural families.
Study limitations
We did not systematically collect baseline investigation information for this cohort as a small proportion had any previous tests such as electroencephalography or neuroimaging. The clinical diagnosis of seizures and non-epileptic events were not corroborated by investigations as they were unavailable in this resource limited setting. We acknowledge that there is a potential for having underdiagnosed seizures if they had last occurred several months prior to our assessment and also being dependent on parental recall and description. We had to rely on the clinical impression of a limited number of observers. Although we utilised standard criteria to assess seizure reduction, the collection of the follow-up data was based on reporting by the primary caregiver which may have been a source of potential bias.
Conclusion
Epilepsy is prevalent among children with CP in rural Bangladesh and the various gaps in optimum epilepsy management are lack regular follow-up, recognition of common seizure types and non-epileptic seizure mimics, familiarisation with commonly available, affordable AED and availability of guidelines for prolonged seizure management. These gaps are amenable to proposed low cost, educational interventions. Healthcare workers can improve epilepsy management with regular follow-up, education on common seizure types, seizure mimics, use of commonly available, affordable AED and guidelines for prolonged seizure management.
Supplementary Material
Acknowledgments
We would like to acknowledge the CSF Global team in Bangladesh for their cordial support in implementing this project and supporting the families of children with CP in referrals and access to services. We also want to acknowledge the primary caregivers of the children with CP and epilepsy who participated in the study. Their input was invaluable to the design and conduct of this study.
Footnotes
Contributors: All listed authors meet the appropriate authorship criteria, and nobody who qualifies for authorship has been omitted. GK and SSM conceptualised and established this research study. They also contributed to study design, development of the study materials and overall conduct of the study supported by TK. SSM, TK and MCD were responsible for assessment of study participants and data collection. SSM, GK, NB and MM provided specialist advice in this study. TK, SSM and GK completed data analysis, interpretation of the data and drafted the initial and revised manuscript with input from all the coauthors. All authors have read and approved the final manuscript. SSM is a guarantor for this work and takes responsibility for the work and the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This study has been conducted as part of the BCPR study funded by the Cerebral Palsy Alliance Research Foundation (PG4314) and through internal funding from CSF Global, Bangladesh. TK is supported by the Cerebral Palsy Alliance Research Foundation (CDG04617, PHD02119). SSM is supported by Cerebral Palsy Alliance Research Foundation Career Development Grant (CDG7916).
Disclaimer: The study funders played no role in the design of the study and collection, analysis, interpretation of data and in the preparation of the manuscript, and in the decision to submit the paper for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. No additional data are available.
Ethics statements
Patient consent for publication
Consent obtained from parent(s)/guardian(s)
Ethics approval
This study involves human participants and was approved by This study was conducted as part of the Bangladesh Cerebral Palsy Register Study which has been approved by the Bangladesh Medical Research Council (BMRC) Human Research Ethics Committee (Ref no. BMRC/NREC/2013–2016/1267) in Bangladesh, and by the Cerebral Palsy Alliance NHRMC Human Research Ethics Committee (Ref no.2015–03-02) in Australia. Written informed consent was taken from the primary caregiver/parents/guardian of the children with CP. Participants gave informed consent to participate in the study before taking part.
References
- 1.Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol 2005;47:571–6. 10.1017/S001216220500112X [DOI] [PubMed] [Google Scholar]
- 2.Mesraoua B, Ali M, Deleu D. Epilepsy and cerebral palsy. Neurodevelopment and Neurodevelopmental Disorder 2019. [Google Scholar]
- 3.Singhi P, Jagirdar S, Khandelwal N, et al. Epilepsy in children with cerebral palsy. J Child Neurol 2003;18:174–9. 10.1177/08830738030180030601 [DOI] [PubMed] [Google Scholar]
- 4.Khandaker G, Muhit M, Karim T, et al. Epidemiology of cerebral palsy in Bangladesh: a population-based surveillance study. Dev Med Child Neurol 2019;61:601–9. 10.1111/dmcn.14013 [DOI] [PubMed] [Google Scholar]
- 5.National Institute of Population Research and Training (NIPORT) . The demographic and health surveys (DHS) program. Dhaka, Bangladesh; 2014. [Google Scholar]
- 6.Ahmed SM, Hossain MA, Rajachowdhury AM, et al. The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health 2011;9:3. 10.1186/1478-4491-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JY, Farmer P, Porter ME. Redefining global health-care delivery. Lancet 2013;382:1060–9. 10.1016/S0140-6736(13)61047-8 [DOI] [PubMed] [Google Scholar]
- 8.Bearden DR. Pediatric neurology in resource-limited settings: a systematic review. Curr Pediatr Rep 2018;6:34–9. 10.1007/s40124-018-0155-x [DOI] [Google Scholar]
- 9.Cochran MF, Berkowitz AL, Kim JY FP. A global health delivery framework approach to epilepsy care in resource-limited settings. J Neurol Sci 2015;358:263–5. 10.1016/j.jns.2015.09.007 [DOI] [PubMed] [Google Scholar]
- 10.Patel P, Baier J, Baranov E, et al. Health beliefs regarding pediatric cerebral palsy among caregivers in Botswana: a qualitative study. Child Care Health Dev 2017;43:861–8. 10.1111/cch.12490 [DOI] [PubMed] [Google Scholar]
- 11.Fisher RS, Cross JH, French JA, et al. Operational classification of seizure types by the International League against epilepsy: position paper of the ILAE Commission for classification and terminology. Epilepsia 2017;58:522–30. 10.1111/epi.13670 [DOI] [PubMed] [Google Scholar]
- 12.Jahan I, Karim T, Das MC, et al. Mortality in children with cerebral palsy in rural Bangladesh: a population-based surveillance study. Dev Med Child Neurol 2019;61:1336–43. 10.1111/dmcn.14256 [DOI] [PubMed] [Google Scholar]
- 13.Aicardi J. Epilepsy in brain-injured children. Developmental Medicine Child Neurology 2010;32:191–202. 10.1111/j.1469-8749.1990.tb16925.x [DOI] [PubMed] [Google Scholar]
- 14.Aksu F. Nature and prognosis of seizures in patients with cerebral palsy. Developmental Medicine Child Neurology 2008;32:661–8. 10.1111/j.1469-8749.1990.tb08426.x [DOI] [PubMed] [Google Scholar]
- 15.Report of the Australian cerebral palsy register birth years 1995-2012 2018.
- 16.Jahan I, Al Imam MH, Karim T, et al. Epidemiology of cerebral palsy in Sumba Island, Indonesia. Dev Med Child Neurol 2020;62:1414–22. 10.1111/dmcn.14616 [DOI] [PubMed] [Google Scholar]
- 17.Karim T, Dossetor R, Huong Giang NT, et al. Data on cerebral palsy in Vietnam will inform clinical practice and policy in low and middle-income countries. Disabil Rehabil 2021;9:1–8. 10.1080/09638288.2020.1854872 [DOI] [PubMed] [Google Scholar]
- 18.National Clinical Guideline Centre . The epilepsies: the diagnosis and management of the epilepsies in adults and children in primary and secondary care. Available: http://www.nice.org.uk/nicemedia/live/13635/57784/57784.pdf [Accessed March 2021].
- 19.Allers K, Essue BM, Hackett ML, et al. The economic impact of epilepsy: a systematic review. BMC Neurol 2015;15:245. 10.1186/s12883-015-0494-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nuri RP, Aldersey HM, Ghahari S. Needs of families of children with cerebral palsy in Bangladesh: a qualitative study. Child Care Health Dev 2019;45:36–44. 10.1111/cch.12624 [DOI] [PubMed] [Google Scholar]
- 21.Rajbhandari H, Joshi S, Malakar S, et al. Epilepsy field workers, a smartphone application and telephone telemedicine: safe and effective epilepsy care in rural Nepal. Seizure 2019;64:54–8. 10.1016/j.seizure.2018.12.005 [DOI] [PubMed] [Google Scholar]
- 22.Patsalos PN, Perucca E. Clinically important drug interactions in epilepsy: general features and interactions between antiepileptic drugs. Lancet Neurol 2003;2:347–56. 10.1016/S1474-4422(03)00409-5 [DOI] [PubMed] [Google Scholar]
- 23.Hussain ME. Burden of epilepsy in Bangladesh: current approach. J Curr Adv Med Res 2018;4:1–2. 10.3329/jcamr.v4i1.36249 [DOI] [Google Scholar]
- 24.Chiang L-M, Wang H-S, Shen H-H, et al. Rectal diazepam solution is as good as rectal administration of intravenous diazepam in the first-aid cessation of seizures in children with intractable epilepsy. Pediatr Neonatol 2011;52:30–3. 10.1016/j.pedneo.2010.12.009 [DOI] [PubMed] [Google Scholar]
- 25.Shangguan Y, Liao H, Wang X. Clonazepam in the treatment of status epilepticus. Expert Rev Neurother 2015;15:733–40. 10.1586/14737175.2015.1056781 [DOI] [PubMed] [Google Scholar]
- 26.Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus. N Engl J Med Overseas Ed 1998;339:792–8. 10.1056/NEJM199809173391202 [DOI] [PubMed] [Google Scholar]
- 27.Kwong KL, Wong SN, So KT. Epilepsy in children with cerebral palsy. Pediatr Neurol 1998;19:31–6. 10.1016/S0887-8994(98)00011-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-052578supp001.pdf (213.2KB, pdf)
Data Availability Statement
No data are available. No additional data are available.