Abstract
Background: Rates of opioid addiction and overdose continue to climb in the United States, increasing pressure on prescribers to identify solutions to decrease postoperative opioid consumption. Hand and upper extremity surgeries are high-volume surgeries with a predilection for inadvertent overprescribing. Recent investigations have shown that preoperative opioid counseling may decrease postoperative opioid consumption. In order to test this hypothesis, a prospective randomized trial was undertaken to determine the effect of preoperative opioid counseling on postoperative opioid consumption. Methods: Eligible patients undergoing outpatient upper extremity surgery were randomized to either receive preoperative opioid counseling or to receive no counseling. Surgeons were blinded to their patient’s counseling status. Preoperatively, patient demographics, surgical and prescription details were recorded. Postoperatively, patients’ pain experience including opioid consumption, pain levels, and satisfaction was recorded. Results: There were 131 total patients enrolled, with 62 in the counseling group and 69 in the control group. Patients receiving counseling consumed 11.8 pills compared to 17.4 pills in the control group (P = .007), which translated to 93.7 Morphine Equivalent Units (MEU) in the counseling group compared to 143.2 MEU in the control group (P = .01). There was no difference in pain scores at any time point between groups. Among all study patients a total of 3767 opioid pills were prescribed with approximately 50% left unused. Conclusion: Patients receiving preoperative counseling consumed significantly fewer opioids postoperatively. Inadvertant overprescribing remains high. Routine use of preoperative counseling should be implemented along with prescribing fewer opioids overall to prevent overprescribing.
Keywords: opioid, upper extremity, opioid counseling, opioid counseling upper extremity, preoperative counseling
Introduction
In recent years, there have been significant increases in opioid-related dependence, abuse, and death. 1 Rates of opioid sales, overdoses, and addiction treatment have more than tripled since the early 2000s. 1 There are a number of factors contributing to these alarming statistics including dependency from prescription opioids. 1 Excess prescription opioids can result in dependency and abuse by the patient, or diversion to other friends and family members of the patient. 2 Upper extremity surgery in particular has been found to be prone to inadvertent overprescribing. 3 Additionally, use of an opioid postoperatively has been shown to increase risk of long-term continued use, particularly when the initial dose and prescription quantity is high.4,5 Heightened awareness and increasing pressure on the medical community has resulted in a significant decrease in initial opioid prescriptions since 2012. 6 However, the problem still remains, with greater than 40 deaths each day related to prescription opioid overdose, indicating the need to continue to pursue opioid-abuse risk reduction strategies. 7
A recent study has shown that preoperative opioid counseling can reduce postoperative opioid consumption by two-thirds following carpal tunnel release surgery. 8 To further investigate the effects of preoperative opioid counseling, a prospective randomized trial was undertaken with the hypothesis that preoperative opioid counseling would result in decreased postoperative opioid consumption after outpatient upper extremity surgery. A secondary study goal was to determine average opioid consumption patterns after various upper extremity surgeries to inform future prescribing patterns.
Methods
With institutional review board approval, a prospective randomized trial was conducted at a single academic medical center. The findings presented here represent analysis of the upper extremity cohort of a larger study. Study inclusion criteria included patients aged between 18 and 89, English-speaking, and indicated to undergo elective outpatient upper extremity surgery by 1 of 5 board certified and fellowship-trained orthopedic surgeons. Exclusion criteria included surgeries performed under only local anesthesia, preoperative opioid use, and inpatient surgery.
Patients were recruited the day of surgery preoperatively. After ensuring informed consent, patient demographic information and surgical plan details were collected, including type of surgery and anesthesia. Enrolled patients were then randomized to either receive preoperative opioid counseling or not. Patients were therefore not blinded to their treatment arm, but their treating surgeons were blinded. Subsequently, their surgeon prescribed postoperative opioids per their typical protocol. The type and amount of opioids, and other agents prescribed, were also collected.
Patients randomized to preoperative counseling were given a pretaped standardized 5-minute video (https://youtu.be/3wnF4JlFNBc) played on a digital tablet in the preoperative area that educated the patient as to the nature of opioids, statistics on the “Opioid Epidemic” in America, how to safely consume opioids, nonopioid pain management strategies, and how to avoid opioid dependence.
Postoperatively, patients were queried about their postoperative pain experience, opioid consumption, nonopioid medication consumption, and any adverse effects related to their pain management experience. The same questionnaire was given to both study groups. However, patients who were randomized to the counseling group were also asked a series of questions regarding the preoperative presentation they watched.
Statistical Analysis
Data collected in the postoperative period were analyzed using Pearson’s chi squared test and Student t test for categorical and continuous variables, respectively. A P value of < .05 was considered to be statistically significant. Prestudy power analysis determined that a minimum of 100 patients would be needed to detect a 3 pill difference between study groups.
Source of Funding
No sources of external funding were utilized in the completion of this study.
Results
During the course of the study, 188 patients were approached, of which 32 declined to participate. The remaining 156 patients were enrolled and randomized; however, 25 were lost to follow-up or subsequently excluded based on the above criteria. The final study population consisted of 131 patients, with 62 patients receiving counseling and 69 patients serving as controls. This population consisted of 40% women and 60% men, which were evenly distributed between the 2 arms (Table 1). The average age of the counseled and control groups was 50.9 (range: 18-84) and 49.8 years (range: 18-82), respectively. There was no significant difference in the age, body mass index, procedure type, and anesthesia type between the 2 groups (Table 1). Bone procedures consisted of fracture, arthroscopy, arthroplasty, and arthrodesis. Soft tissue procedures consist of nerve and tendon procedures.
Table 1.
Demographic Information Comparing the Counseled and Control Groups.
| Characteristic | Counseling group | Control group | Statistical Value |
|---|---|---|---|
| Patients enrolled | 62 | 69 | |
| Male | 36 | 42 | χ2 = 0.107 |
| Female | 26 | 27 | P = .744 |
| Average age | 50.9 | 49.8 | P = .695 |
| BMI | 28.4 | 28.6 | P = .800 |
| Procedure type | |||
| Bone | 14 | 16 | χ2 = 0.007 |
| Soft tissue | 48 | 53 | P = .934 |
| Anesthesia type | |||
| General | 22 | 25 | |
| Regional | 6 | 4 | χ2 = 4.870 |
| General + regional | 27 | 38 | P = .182 |
| Other | 7 | 2 | |
| Anatomic location | |||
| Wrist | 16 | 12 | χ2 = 2.236 |
| Elbow | 16 | 15 | P = .326 |
| Shoulder | 30 | 42 | |
Note. BMI: body mass index.
Patients in the counseling group consumed 11.8 pills (SD = 10.2) compared to 17.4 pills (SD = 12.6) in the control group (P = .007) (Table 2). After conversion to morphine equivalent units (MEU), the counseling group consumed 93.5 MEU (SD = 97.6) compared to 143.2 MEU (SD = 123.0) in the control group (P = .013) (Table 2). Moreover, patients in the counseling group discontinued their opioids an average of 2 days earlier than control patients (P = .013). There was no difference in the amount of opioids prescribed between the groups (Table 3) or pain level reported in the first 5 postoperative days (Table 4).
Table 2.
Comparison of the Number of Opioids Prescribed and Consumed by Patients in the Counseling and Control Groups as Well as the Total Number of Pills Used by All Study Subjects.
| Opioid Consumption Characteristic | Counseling (n pills) | Control (n pills) | P value |
|---|---|---|---|
| Opioids prescribed per patient | 26.45 | 29.52 | .108 |
| Opioids consumed per person (day 0-14) | 11.77 143.2 MEU |
17.35 93.65 MEU |
.007 .013 |
| Total days of opioid consumption | 4.34 | 6.25 | .013 |
| Total leftover opioids | 1876 | ||
Note. MEU = morphine equivalent units.
Table 3.
Average Reported Opioid Consumption Following Surgery per Patient in the Counseling and Control Groups. Total Opioid Consumption was Reported Daily Over the First Five Postoperative Days and Then a Total Consumption was Reported 14 Days After Surgery.
| Postoperative day | Counseling (n pills) | Control (n pills) | P value |
|---|---|---|---|
| Surgery day | 1.63 | 2.39 | .037 |
| Day 1 | 3.17 | 3.67 | .244 |
| Day 2 | 2.63 | 2.99 | .408 |
| Day 3 | 1.93 | 2.43 | .213 |
| Day 4 | 1.49 | 1.81 | .389 |
| Day 5 | 1.00 | 1.58 | .072 |
| Total (0-14 days) | 11.77 | 17.35 | .007 |
Table 4.
Average VAS Pain Score Following Surgery in Patients in the Counseling and Control Groups.
| Postoperative day | Counseling (VAS pain score) | Control (VAS pain score) | P value |
|---|---|---|---|
| Surgery day | 3.75 | 4.29 | .371 |
| Day 1 | 5.66 | 5.63 | .958 |
| Day 2 | 5.39 | 5.45 | .909 |
| Day 3 | 4.73 | 4.80 | .881 |
| Day 4 | 4.22 | 4.26 | .934 |
| Day 5 | 3.81 | 3.98 | .721 |
Note. VAS = visual analog scale.
Anatomic location of surgery did not produce a significant difference in opioid consumption in either the counseling or control groups, though patients undergoing shoulder surgery took an average of 2 times more opioids than those having wrist surgery in both groups (Table 5). Among patients undergoing a soft tissue type procedure on their upper extremity, those receiving counseling took an average of 6 pills less than control patients (P = .005). The same was not seen for patients who had a bony procedure. General anesthesia alone in conjunction with preoperative counseling resulted in a 50% decrease (6.86 vs 13.56 pills) in opioid consumption postoperatively when compared to the control patients (P = .0112). This trend was not seen in patients receiving a combination of general and regional anesthesia, regional alone, or other varieties of anesthesia (Table 5).
Table 5.
Comparison of Total Opioid Consumption in the Counseling and Control Groups Broken Down by Other Factors Including Anatomic Location of Surgery, Procedure Type and Anesthesia Type.
| Surgical Characteristic | Counseling group (n pills) [SD] | Control group (n pills) [SD] | P value |
|---|---|---|---|
| Anatomic location | |||
| Shoulder | 15.85 [10.93] | 20.95 [13.49] | .092 |
| Elbow | 8.19 [8.03] | 13.67 [10.03] | .103 |
| Wrist | 7.69 [8.12] | 9.33 [6.56] | .570 |
| Procedure type | |||
| Soft tissue | 12.24 [10.53] | 18.96 [12.97] | .005 |
| Bone | 10.14 [9.36] | 12.00 [10.09] | .607 |
| Anesthesia type | |||
| General | 6.86 [7.26] | 13.56 [9.78] | .012 |
| Regional | 16.67 [12.56] | 9.50 [5.45] | .3203 |
| General + regional | 14.94 [9.98] | 21.05 [13.90] | .055 |
| Other | 10.71 [12.61] | 10.00 [9.90] | .944 |
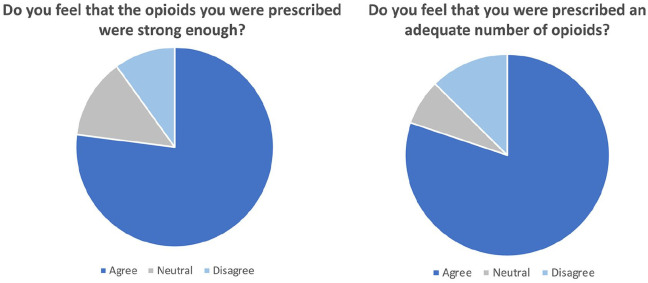
Among all patients who utilized opioid medications postoperatively, 77% of the patients felt that they received an adequate number of opioids and 73% found their opioids to be strong enough to relieve their pain (Figure 1). These findings were consistent between the counseling and control groups, with no significant difference in sentiment regarding quantity (P = .752) or strength (P = .647) of their opioid prescriptions.
Figure 1.
Results of survey of patient satisfaction with their opioid prescriptions. There was no difference in survey responses between counseling and control group patients for both strength (P = .647) and quantity (P = .752) of opioids given.
Of the patients in the group who received opioid counseling, 82% reported that the preoperative multimedia presentation was helpful, despite two-thirds of the patients feeling that the video already contained information they were familiar with. Nearly 90% of this group agreed that all patients should be required to watch an opioid education presentation prior to undergoing surgery.
Refill rates were 4.8% in the counseling group compared to 13% in the control group (P = .104). Patients in the counseling group needing refills received an average of 15 additional pills, while control group patients received 24 on average. Of the 13 patients needing refills following surgery, 10 had undergone arthroscopic rotator cuff repair.
During the course of the study period, there were a total of 3767 opioid pills prescribed. Of these, 1876 went unused, equating to more than 14 pills leftover per patient.
Discussion
Opioid dependency, abuse, and overdose has become a major problem across the United States. In 2017 alone, nearly 50 000 deaths were attributed to opioid overdose, a number that is likely vastly underestimated, as it doesn’t account for deaths related to synthetic opioids or tramadol. 9 Extrapolation of the current trends in opioid use via a mathematical algorithm has predicted that the number of deaths due to opioid overdose will exceed 81 000 annually by 2025, corresponding with a nearly 150% increase over the course of 10 years. 10 Increased pressure on the medical community to curb the amount of opioid prescriptions issued to patients has resulted in an overall decline in the overall quantity of prescriptions since 2012, but the average number of days supplied continues to increase.11,12 This is particularly problematic, as studies have shown that the probability of continued opioid use at >1 year is directly related to the initial prescription supply, both in surgical and nonsurgical fields.5,6
In recent years, special attention has been given to patient education as a potential method of minimizing the risk of opioid abuse. This study shows that preoperative counseling, in the form of a multimedia presentation, can reduce the number of opioids consumed by patients following a variety of upper extremity orthopedic surgeries by over 33%. Receiving information regarding common opioid medications, the epidemic and strategies to safely manage pain allows patients to more knowledgably use their prescriptions postoperatively. The presentation was easily played for patients in the preoperative rooms after being seen by nursing staff and the surgeon. This is a time and space when patients are typically unoccupied and are interested in learning about their postoperative pain management plan. Additionally, family members or caretakers are also often present during the preoperative time and can watch the presentation along with the patient. Having well-informed family and caretakers is an important, and understudied, aspect of opioid education. Although this was not quantified in our study, understanding the impact of the presence of a family member during the counseling is a potential area of future investigation.
Previous studies in general surgery, hand surgery, and upper and lower extremity surgery have shown that receiving some degree of counseling on opioid medications reduces patient consumption by up to 50%.8,13-15 Early discontinuation of opioids was another important finding in patients receiving counseling. 14 This correlates with the results of our study, as patients who were counseled consumed significantly fewer opioid pills and stopped consuming opioid medication 2 days sooner.
A number of education modalities have been explored including opioid education handouts, informational sheets reviewed with a physician, and a combination of oral and written counseling.8,13,15,16 Online resources for patients regarding opioid use are generally available but are often written for an advanced audience and can contain conflicting information, a finding that suggests a more standardized approach to opioid education is needed in the perioperative time. 17 The multimedia presentation shown to patients in this study was developed with this in mind, explaining concepts such as “opioids” and “narcotics” at their most basic level.
In patients undergoing upper extremity orthopedic surgery, it has been shown that 13% of opioid-naïve patients will continue to fill prescriptions more than 3 months postoperatively, emphasizing the need for an effective intervention to prevent opioid misuse in this population. 17 The current study showed that patients receiving preoperative counseling on opioid use discontinued their medications earlier than patients who did not receive counseling. The sooner opioids are stopped, the less likelihood there is of continued use at 1 year, making this an important takeaway from this study. 5
It is also important to address the finding that prescriptions for opioid medications often far exceed patient consumption realities, with significant quantities of pills left over. In the current study, there were 3767 opioid pills prescribed. Of these, 1876 went unused, equating to more than 14 pills leftover per patient. When considering upper extremity orthopedic surgery, upward of two-thirds of pills go unused, a finding that was similarly substantiated in this study. 3 On average, only one-third of patients dispose of opioids once their pain is adequately controlled, a fact that is not surprising given that a mere one-fourth of patients ever receive information on how to properly dispose of unused pills.18,19 These are statistics that emphasize the need for patient counseling and improved prescribing guidelines. It has previously been suggested that opioid prescribing in upper extremity orthopedic surgery be based on the nature of the procedure and the anatomic location, following the general rule that hand surgery requires the fewest opioid pills and increasing quantities may be necessary as you move proximally toward the shoulder, a consumption pattern that was corroborated by this study. 3 Among physicians in this study, the least variation in opioid prescription quantities was seen in patients undergoing surgery on the soft tissues of the hand, including carpal tunnel release, mass excision, and trigger finger release. In these cases, almost all physicians prescribed only 5 to 10 opioids. However, there was much more variation seen in surgeries of the shoulder and elbow. Based on our study findings and other studies, we would recommend prescribing 10 to 20 opioid pills after shoulder and elbow surgeries.3,20
In terms of implementation of preoperative opioid counseling, we recommend surgeons create a prerecorded educational video that can be played on smart device, tablet, or viewed online. We have generally found that patients are more receptive to watching a video then reading educational material. Moreover, the video mechanism affords the greatest efficiency for counseling while not taking the time of the physician or any physician extenders. Moreover, it can be provided to the patient anytime including at the time of scheduling in the office, at home at their leisure, or the day of surgery in the preoperative area. In our own practice, we have placed the video on a tablet that patients watch in the preoperative area with their accompanying friends or family members. Lastly, we often incorporate additional postoperative instructions along with the opioid counseling information.
One important limitation of this study is the use of patient-reported opioid consumption as one of the primary outcome measurements. It is possible that patients over- or underestimated their true utilization, despite blinding participants to the study question. Additionally, data collection was done at the first postoperative visit, 14 days after surgery, but it is possible that patients may have taken more of their prescription beyond this date for continued pain, which is not accounted for in this data. Further investigation into the long-term impact of patient education on chronic opioid consumption following upper extremity surgery is warranted, as well as the optimum method of delivering this information. Additionally, with increasing awareness surrounding the opioid epidemic, it is possible that both arms of the study are now more aware of the dangers of opioid medications despite randomization to receiving counseling.
Ultimately, this study shows that patients undergoing elective upper extremity orthopedic surgery consumed significantly fewer opioids if they received preoperative counseling in the form of a multimedia presentation. This suggests that there is a role for patient education in the preoperative period in order to decrease opioid misuse in the future.
Footnotes
Author’s Note: Nothing material or monetary was received by any of the authors in the execution of this study and the subsequent production of this manuscript.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. 5 Informed consent was obtained from all patients for being included in the study.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Asif M. Ilyas  https://orcid.org/0000-0002-5636-9873
https://orcid.org/0000-0002-5636-9873
References
- 1. Kolodny A, Courtwright D, Hwang C, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559-574. [DOI] [PubMed] [Google Scholar]
- 2. Bartels K, Mayes L, Dingmann C, et al. Opioid use and storage patterns by patients after hospital discharge following surgery. PLoS ONE. 2016;11(1):e0147972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kim N, Matzon JL, Abboudi J, et al. A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Joint Surg Am. 2016;98(20):e89. [DOI] [PubMed] [Google Scholar]
- 4. Brat G, Agniel D, Beam A, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ. 2018;360:j5790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Harbaugh C, Lee J, Hu H, et al. Persistent opioid use among pediatric patients after surgery. Pediatrics. 2018;141(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhu W, Chernew ME, Sherry TB, et al. Initial opioid prescriptions among U.S. commercially insured patients, 2012–2017. N Engl J Med. 2019;380(11):1043-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Losby J, Hyatt J, Kanter M, et al. Safer and more appropriate opioid prescribing: a large healthcare system’s comprehensive approach. J Eval Clin Pract. 2017;23(6):1173-1179. [DOI] [PubMed] [Google Scholar]
- 8. Alter T, Ilyas AM. A prospective randomized study analyzing preoperative opioid counseling in pain management after carpal tunnel release surgery. J Hand Surg Am. 2017;42(10):810-815. [DOI] [PubMed] [Google Scholar]
- 9. Wide-ranging online data for epidemiologic research (WONDER) . Atlanta, GA: CDC, National Center for Health Statistics; 2016. http://wonder.cdc.gov. Accessed April 10, 2020. [Google Scholar]
- 10. Chen Q, Larochelle M, Weaver D, et al. Prevention of prescription opioid misuse and projected overdose deaths in the United States. JAMA Netw Open. 2019;2(2):e187621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. 2018 annual surveillance report of drug—related risks and outcomes—United States. Surveillance special report. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillance-report.pdf. Published August 31, 2018. Accessed May 12, 2019. [Google Scholar]
- 12. Dart R, Surratt H, Cicero T, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241-248. [DOI] [PubMed] [Google Scholar]
- 13. Hartford L, Van Koughnett JAM, Murphy PB, et al. Standardization of outpatient procedure (stop) narcotics: a prospective non-inferiority study to reduce opioid use in outpatient general surgical procedures. J Am Coll Surg. 2019;228(1):81-88. [DOI] [PubMed] [Google Scholar]
- 14. Syed U, Aleem A, Wowkanech C, et al. Neer Award 2018: the effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: a prospective, randomized clinical trial. J Shoulder Elbow Surg. 2018;27(6):962-967. [DOI] [PubMed] [Google Scholar]
- 15. Yajnik M, Hill J, Hunter O, et al. Patient education and engagement in postoperative pain management decreases opioid use following knee replacement surgery. Patient Educ Couns. 2019;102(2):383-387. [DOI] [PubMed] [Google Scholar]
- 16. Dwyer C, Soong M, Hunter A, et al. Prospective evaluation of an opioid reduction protocol in hand surgery. J Hand Surg Am. 2018;43(6):516-522. [DOI] [PubMed] [Google Scholar]
- 17. Johnson S, Chung K, Zhong L, et al. Risk of prolonged opioid use among opioid-naïve patients following common hand surgery procedures. J Hand Surg. 2016;41(10):947-957.e3. [DOI] [PubMed] [Google Scholar]
- 18. Buffington DE, Lozicki A, Alfieri T, et al. Understanding factors that contribute to the disposal of unused opioid medication. J Pain Res. 2019;12:725-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kumar G, Jaremko K, Kou A, et al. Quality of patient education materials on safe opioid management in the acute perioperative period: what do patients find online? Pain Med. 2020;21:171-175. [DOI] [PubMed] [Google Scholar]
- 20. Adalbert JR, Ilyas AM. Implementing prescribing guidelines for upper extremity orthopedic procedures: a prospective analysis of postoperative opioid consumption and satisfaction [published online ahead of print August 23, 2019]. Hand. doi: 10.1177/1558944719867122. [DOI] [PMC free article] [PubMed] [Google Scholar]