Abstract
Background: The purpose of this article is to describe the surgical technique used by the authors and the outcome in the treatment of chronic posttraumatic instability of the distal radioulnar joint (DRUJ). Methods: A retrospective study was conducted analyzing the medical records of 11 patients with chronic posttraumatic instability of the DRUJ, treated by a foveal reattachment of the triangular fibrocartilage complex with dorsal capsular and extensor retinaculum imbrications between 2016 and 2017, with a follow-up evaluation of 1 year. Results: All patients reported pain relief and the absence of instability, returning to normal activities in 3 to 6 months. Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire ranged from 2 to 25, resulting in a mean score of 9.5. Forearm rotation averaged 89° of pronation and 85° of supination. Conclusion: Foveal reattachment of the triangular fibrocartilage complex with dorsal capsular and extensor retinaculum imbrications is an effective surgical procedure for the treatment of DRUJ chronic posttraumatic instability.
Keywords: capsuloplasty, distal radioulnar joint, posttraumatic instability
Introduction
Posttraumatic instability of the distal radioulnar joint (DRUJ) is relatively frequent in hand surgery specialists’ offices, and the biomechanical complexity makes DRUJ instability diagnosis and treatment a therapeutic challenge.1,2 The triangular fibrocartilage complex (TFCC) has an ulnar insertion in the fovea, 3 with a rich vascularization, and a good prognosis for repairing techniques.4,5 The critical stabilizers of the DRUJ are the distal radioulnar ligaments of the TFCC. The components of the complex are the triangular fibrocartilage proper (the articular disk), the meniscus homologue (the ulnocarpal meniscus), the ulnar collateral ligament, the dorsal and volar radioulnar ligament, and the sheath of the extensor carpi ulnaris.6,7 Other structures and mechanisms are considered secondary stabilizers of the DRUJ, like the dynamic tension of the extensor carpi ulnaris, the sixth extensor compartment of the wrist, the dynamic support of the pronator quadrates, and the forearm interosseous ligament.8-10
The action of DRUJ primary and secondary stabilizers is well known, but only recently is the role of the DRUJ capsule gradually being understood, especially in cases where the TFCC is damaged. 11 Some articles state that in addition to the TFCC, the joint capsule also has a critical stabilizing function;12-15 and therefore, many authors are considering the capsular imbrication as a surgical option in cases of the DRUJ posttraumatic instability.16-20
The extensor retinaculum imbrication can also be used to restore the DRUJ stability. This technique consists of making an ulnar-based retinacular flap that crosses the fifth extensor compartment to create extra-articular support similar to the anatomical course of the dorsal radioulnar ligament.21,22
The best-known treatment in the literature to correct chronic DRUJ instability is the Adams procedure 23 ; however, it is a complex procedure with large bone perforations. As well as the Adams procedure, 23 the foveal reattachment of the TFCC, the DRUJ capsular imbrication, and extensor retinaculum imbrication are established procedures for the DRUJ instability. The objective of this study was to analyze the clinical outcomes of patients with chronic posttraumatic instability of the DRUJ treated by a surgical technique that joins these 3 reconstruction concepts that are less complex and reproducible than the standard Adams procedure. 23
Material and Methods
Study Design
A retrospective study was conducted analyzing the medical records of 11 patients with chronic posttraumatic instability of the DRUJ who were treated by a foveal reattachment of the TFCC, with DRUJ dorsal capsular and extensor retinaculum imbrication between 2016 and 2017. All patients were evaluated 1 year after surgery by the same surgeon, and statistical analysis was undertaken using InStat 2.0 software and the Chi-square test. They experienced a single traumatic event, experiencing wrist pain, dorsal subluxation of the ulna, loss of grip strength, decreased range of motion (ROM), and a clicking sound when rotating the wrist. This study included 10 men and 1 woman aged 23 to 57 years (average, 42 years). The time of injury to surgery was 12 to 30 months, with a mean of 17.5 months.
On physical examination, all patients presented with dorsal instability of the DRUJ compared with the unaffected side. The anteroposterior stress test was used to diagnose the severity of the DRUJ instability before surgery, 24 and the surgical reconstruction was indicated in patients with Grades 2 and 3; in other words, only patients with radioulnar translation, without endpoint (Grade 2), or subluxation with forearm pronation (Grade 3), underwent surgical treatment (Table 1). Radiographs were essential to evaluate DRUJ widening between the distal radius and the ulnar head. Magnetic resonance imaging scans were performed in all cases with foveal avulsion of the TFCC. We do not include computed tomography for diagnosis.
Table 1.
Degrees of DRUJ Instability.
| Degree | Description |
|---|---|
| 0 | Normal stability |
| 1 | Laxity, steady “End Point,” no symptoms |
| 2 | Translation, without steady “End Point,” with symptoms |
| 3 | Subluxation with forearm pronation |
Note. DRUJ = distal radioulnar joint.
We use as inclusion criteria, patients with chronic posttraumatic instability of the DRUJ treated by a foveal reattachment of the TFCC, with DRUJ dorsal capsular and extensor retinaculum imbrication with 1-year minimum follow-up time. We do not use age as an inclusion or exclusion criterion. We use as exclusion criteria, radius fractures, ulnar styloid fractures, the ulnar impaction, arthritis, and rheumatoid changes of the DRUJ.
We measured forearm ROM with a standard goniometer and compared it with the contralateral wrist. We also measured individual results using the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire score translation into Brazilian Portuguese. 25
Surgical Technique
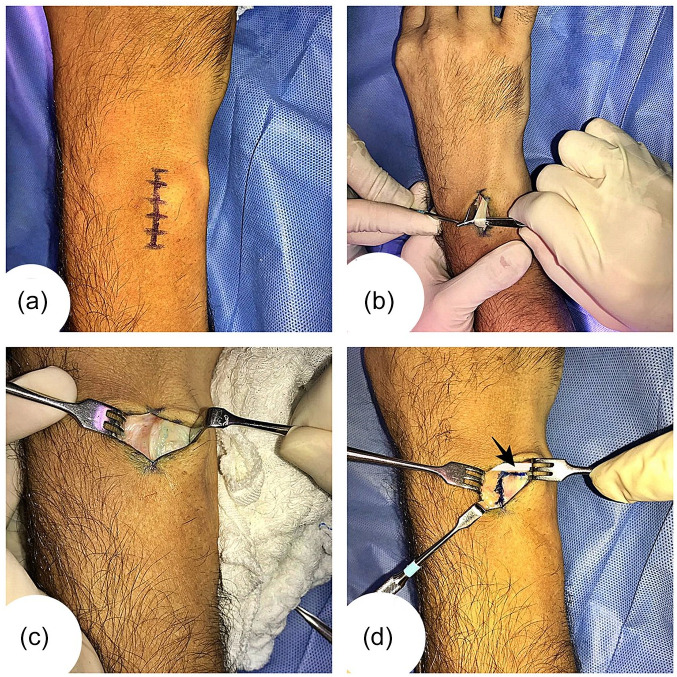
Under brachial plexus block anesthesia, the arm is placed on a hand table with the elbow extended and the forearm pronated. A longitudinal incision is created over the fifth extensor compartment at the level of the wrist (Figure 1a). The fifth extensor compartment is opened, and the extensor digiti quinti (EDQ) is retracted radially (Figure 1b and c). The dorsal joint capsule is exposed and divided with an inverted “L” incision. The transverse portion is made immediately proximal to the dorsal radioulnar ligament and the longitudinal portion over the DRUJ (Figure 1d).
Figure 1.
(a) An incision with 3 to 4 cm was made over the fifth extensor compartment of the wrist. (b) After opening the fifth extensor compartment of the wrist, the extensor digiti quinti tendon was identified. (c) Extensor digiti quinti tendon was retracted radially, and the distal radioulnar joint (DRUJ) capsule can be seen below. (d) Design of the inverted “L” shaped joint capsule incision with transverse part immediately proximal to the dorsal radioulnar ligament (black arrow) and longitudinal part over the DRUJ.
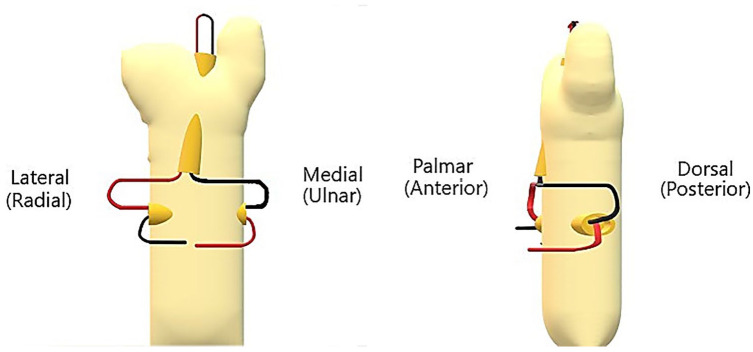
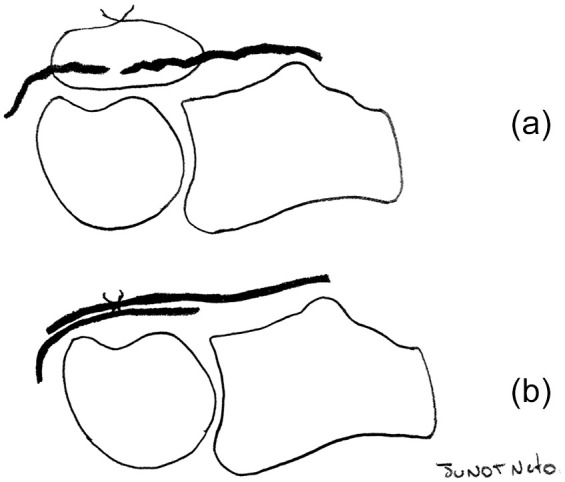
A U-shaped suture is applied on the ulnar edge of the TFCC using FiberWire number 2 (AR-7200) (Figure 2). A 2.5 mm diameter bone tunnel is made from the center of the fovea to the ulnar metaphysis, and a second bone tunnel with the same diameter is built at the ulna diaphysis with anteroposterior obliquity. The suture threads are passed first through the foveal tunnel, and then we do the same with the second tunnel in opposite directions (1 part should be moved from medial to lateral and another part from lateral to medial) (Figure 3). Two other sutures are passed through each side of the inverted “L” shaped incision with FiberWire number 2 (AR-7200).
Figure 2.
(a) Surgical image of the triangular fibrocartilage complex (TFCC) U-shaped suture technique. (b) Illustration of the U-shaped suture placed on the ulnar edge of the TFCC.
Figure 3.
Technique of bone tunnels and sutures: The first tunnel interconnecting the fovea and the ulna diaphysis.
Note. The second tunnel with anteroposterior obliquity is done from slightly dorsal-ulnar to slightly palmar-radial on the ulna diaphysis about 1 cm proximal to the first bone tunnel. The lateral (radial) stitch (red) is placed from palmar-radial to dorsal-ulnar and the medial (ulnar) stitch (black) from dorsal-ulnar to palmar-radial in the ulna diaphysis crossing the tunnel. The suture is accommodated on the palmar cortex of the ulna.
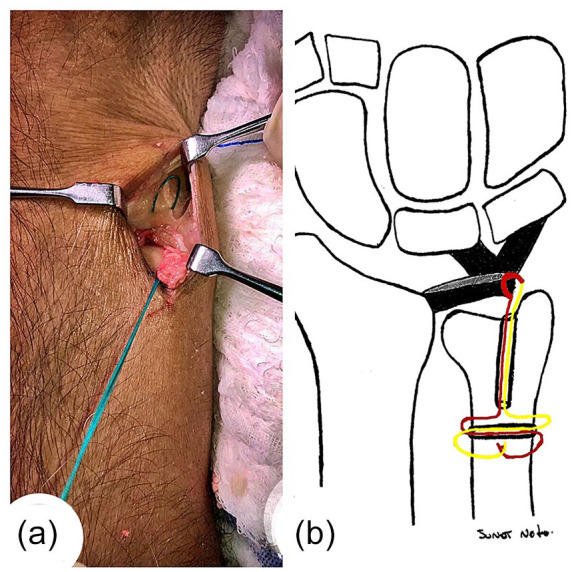
The elbow is now positioned in flexion and the forearm in supination. We reattached the TFCC to the fovea by pulling and tightened the sutures passed through the bone tunnels. The 2 stitches passed through each side of the inverted “L” shaped incision are stretched with imbrication of the joint capsule that was distended (Figure 4).
Figure 4.
(a) Illustration of the redundant joint capsule before imbrication. (b) Illustration of the redundant joint capsule after imbrication.
The authors also emphasize the importance of the extensor retinaculum imbrication. The extensor retinaculum flap was created by detaching it from the joint capsule and adjacent structures to facilitate the imbrication. The ulnar flap of the retinaculum is sutured with 2 FiberWire number 2 (AR-7200), and the EDQ is prepared for transposition from dorsal to the retinaculum flap. The extensor retinaculum imbrication confers significant additional stability that is readily perceived by an intraoperative anteroposterior stress test, right after the retinaculum imbrication. At the end of the surgical procedure, the forearm is placed in a sugar tong splint with forearm supination for 6 weeks.
Results
One year after the surgical procedure, all patients reported pain relief and the absence of instability. DASH questionnaire ranged from 2 to 25, resulting in a mean score of 9.5. Forearm rotation averaged 89° of pronation (100% of the opposite side) and 85° of supination (100% of the opposite side). All patients improved the stress test to grade zero. The return to normal activities happened from 3 to 6 months (Table 2).
Table 2.
Outcome Measurements.
| Age | Sex | Time from injury to surgery | DASH score before surgery | Return to work | DASH score after surgery | ROM (%) | Stress test |
|---|---|---|---|---|---|---|---|
| 25 | Male | 14 months | 57 | 3 months | 3 | 100 | Normal |
| 30 | Male | 14 months | 62 | 3 months | 2 | 100 | Normal |
| 23 | Male | 12 months | 79 | 2 months | 3 | 100 | Normal |
| 46 | Male | 15 months | 85 | 4 months | 13 | 100 | Normal |
| 45 | Male | 12 months | 72 | 3 months | 5 | 100 | Normal |
| 57 | Female | 30 months | 87 | 6 months | 24 | 100 | Normal |
| 55 | Male | 13 months | 59 | 3 months | 5 | 100 | Normal |
| 40 | Male | 17 months | 64 | 3 months | 5 | 100 | Normal |
| 33 | Male | 26 months | 83 | 6 months | 25 | 100 | Normal |
| 55 | Male | 19 months | 76 | 4 months | 5 | 100 | Normal |
| 54 | Male | 21 months | 83 | 5 months | 15 | 100 | Normal |
Note. DASH= Disabilities of the Arm, Shoulder and Hand; ROM = range of motion.
We had in our series, 3 patients who used to practice semi-professional tennis before the trauma and could return to play tennis at the same level or higher, before the first year of postoperative follow-up.
There were mild complications: 3 patients reported local pain for a few months after the splint release, 4 patients reported paresthesia in the dorsal-ulnar region of the hand for a few weeks, and 3 patients noticed the ulna head region was slightly protruding; however, none of these patients had complaints about this.
Discussion
Adams and Berger 26 state that the first surgical option in cases of DRUJ chronic posttraumatic instability should be the late repair of the TFCC; however, a reconstructive procedure would be indicated if TFCC is irrepairable. 27 We agree with this statement; however, it is worth noting that in our case series, the TFCC was repairable even after 18 months of injury.
Many articles and books describe several types of surgical reconstruction procedures for the treatment of DRUJ posttraumatic instability. Adams 23 described a technique of DRUJ stabilization through autologous free graft reconstruction of the palmaris longus tendon. In this technique, it is necessary to perform dorsal and palmar approaches with more significant surgical dissection for graft removal, and bone perforations must be large enough to accommodate the tendon graft.
Although we were able to reattach the TFCC, we obtained the best stability of the DRUJ after the dorsal capsular and extensor retinaculum imbrications. Gofton et al 28 compared the dorsal capsular imbrication and 3 other types of surgical reconstruction for the treatment of DRUJ instability, concluding that the Adams reconstruction, 23 the modified Fulkerson-Watson reconstruction, 29 and the Bowers reconstructions 30 significantly improved the stability, but stated that the capsular imbrication was the repair technique that most resembles the DRUJ kinematics. Manz et al, 16 Kouwenhoven et al, 17 Ahrens et al, 18 Unglaub et al 19 and Spies et al, 20 published their case series of DRUJ posttraumatic instability that was treated by a dorsal joint capsule imbrication with excellent results. This technique has become our main surgical option for the treatment of DRUJ chronic posttraumatic instability, because it is relatively simple, easily reproducible, without the need for grafting and large bone perforations, as well as multiple incisions. We had concerns about an irreparable TFCC, but in all cases, it was always repairable even after 18 months of trauma. Alternatively, it is noteworthy that the authors consider it feasible to perform the reattachment of the TFCC with a bone anchor.
Our results with the DASH score after using the foveal reattachment of the TFCC, with DRUJ dorsal capsular and extensor retinaculum imbrications, had an average of 9.5. Manz et al 16 used only capsular imbrication and had a DASH score average of 14. Seo et al 31 used the Adams procedure and had a DASH score average of 10.5. El-Haj et al 32 used the retinaculum imbrication and had a DASH score average of 13.39. The comparison between the results of the most commonly used procedures for chronic posttraumatic instability of the DRUJ published in the literature leads the authors to believe that the combination of foveal reattachment of the TFCC with DRUJ dorsal capsular and extensor retinaculum imbrications has excellent results with minor complications. This work has limitations because it is a retrospective study, with a low number of patients and without a control group.
Conclusion
Foveal reattachment of the TFCC with DRUJ dorsal capsular and extensor retinaculum imbrications is an effective surgical procedure for the treatment of DRUJ chronic posttraumatic instability.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the committee responsible for (institutional and national) human experimentation and with the Helsinki Declaration of 1975, revised in 2008.
Statement of Informed Consent: Informed consent was obtained when necessary
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Junot H. S. Neto  https://orcid.org/0000-0001-9258-0708
https://orcid.org/0000-0001-9258-0708
References
- 1. Stuart PR, Berger RA, Linscheid RL, et al. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg Am. 2000;25(4):689-699. [DOI] [PubMed] [Google Scholar]
- 2. Kleinman WB. Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg Am. 2007;32(7):1086-1106. [DOI] [PubMed] [Google Scholar]
- 3. af Ekenstam F, Hagert CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg. 1985;19(1):17-25. [DOI] [PubMed] [Google Scholar]
- 4. Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg Am. 1991;16(6):1101-1105. [DOI] [PubMed] [Google Scholar]
- 5. Thiru RG, Ferlic DC, Clayton ML, et al. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg Am. 1986;11(2):258-263. [DOI] [PubMed] [Google Scholar]
- 6. Schuind F, An KN, Berglund L, et al. The distal radioulnar ligaments: a biomechanical study. J Hand Surg Am. 1991;16(6):1106-1114. [DOI] [PubMed] [Google Scholar]
- 7. Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist–anatomy and function. J Hand Surg Am. 1981;6(2):153-162. [DOI] [PubMed] [Google Scholar]
- 8. Spinner M, Kaplan EB. Extender carpi ulnaris. Its relation to the stability of the distal radio-ulnar joint. Clin Orthop Relat Res. 1970;68:124-129. [PubMed] [Google Scholar]
- 9. Ruby LK, Ferenz CC, Dell PC. The pronator quadratus interposition transfer: an adjunct to resection arthroplasty of the distal radioulnar joint. J Hand Surg Am. 1996;21(1):60-65. [DOI] [PubMed] [Google Scholar]
- 10. Hotchkiss RN, An KN, Sowa DT, et al. An anatomic and mechanical study of the interosseous membrane of the forearm: pathomechanics of proximal migration of the radius. J Hand Surg Am. 1989;14(2):256-261. [DOI] [PubMed] [Google Scholar]
- 11. Kleinman WB, Graham TJ. The distal radioulnar joint capsule: clinical anatomy and role in posttraumatic limitation of forearm rotation. J Hand Surg Am. 1998;23(4):588-599. [DOI] [PubMed] [Google Scholar]
- 12. Haugstvedt JR, Berger RA, Berglund LJ, et al. An analysis of the constraint properties of the distal radioulnar ligament attachments to the ulna. J Hand Surg Am. 2002;27(1):61-67. [DOI] [PubMed] [Google Scholar]
- 13. Shaw JA, Bruno A, Paul EM. Ulnar styloid fixation in the treatment of posttraumatic instability of the radioulnar joint: a biomechanical study with clinical correlation. J Hand Surg Am. 1990;15(5):712-720. [DOI] [PubMed] [Google Scholar]
- 14. Watanabe H, Berger RA, An KN, et al. Stability of the distal radioulnar joint contributed by the joint capsule. J Hand Surg Am. 2004;29(6):1114-1120. [DOI] [PubMed] [Google Scholar]
- 15. Marangoz S, Leblebicioğlu G. Stability of the distal radioulnar joint contributed by the joint capsule. J Hand Surg Am. 2005;30(4):868-869. [DOI] [PubMed] [Google Scholar]
- 16. Manz S, Wolf MB, Leclère FM, et al. Capsular imbrication for posttraumatic instability of the distal radioulnar joint. J Hand Surg Am. 2011;36(7):1170-1175. [DOI] [PubMed] [Google Scholar]
- 17. Kouwenhoven ST, de Jong T, Koch AR. Dorsal capsuloplasty for dorsal instability of the distal ulna. J Wrist Surg. 2013;2(2):168-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ahrens C, Unglaub F, Bruckner T, et al. Midterm functional outcome after dorsal capsular imbrication for posttraumatic instability of the distal radioulnar joint. Arch Orthop Trauma Surg. 2014;134(11):1633-1639. [DOI] [PubMed] [Google Scholar]
- 19. Unglaub F, Manz S, Bruckner T, et al. [Dorsal capsular imbrication for dorsal instability of the distal radioulnar joint]. Oper Orthop Traumatol. 2013;25(6):609-614. [DOI] [PubMed] [Google Scholar]
- 20. Spies CK, Hahn P, Unglaub F. Comments on: dorsal capsuloplasty for dorsal instability of the distal ulna (J Wrist Surg 2013;2(2):168-175). J Wrist Surg. 2014;3(2):155-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gupta RK, Singh H, Sandhu VP. Stabilisation of the distal radioulnar joint with a double-breasted slip of the extensor retinaculum. J Bone Joint Surg Br. 2008;90(2):200-202. [DOI] [PubMed] [Google Scholar]
- 22. Dy CJ, Ouellette EA, Makowski AL. Extensor retinaculum capsulorrhaphy for ulnocarpal and distal radioulnar instability: the Herbert sling. Tech Hand Up Extrem Surg. 2009;13(1):19-22. [DOI] [PubMed] [Google Scholar]
- 23. Adams BD. Anatomic reconstruction of the distal radioulnar ligaments for DRUJ instability. Tech Hand Up Extrem Surg. 2000;4(3):154-160. [DOI] [PubMed] [Google Scholar]
- 24. Lester B, Halbrecht J, Levy IM, et al. “Press test” for office diagnosis of triangular fibrocartilage complex tears of the wrist. Ann Plast Surg. 1995;35(1):41-45. [DOI] [PubMed] [Google Scholar]
- 25. Orfale AG, Araújo PM, Ferraz MB, et al. Translation into Brazilian Portuguese, cultural adaptation and evaluation of the reliability of the Disabilities of the Arm, Shoulder and Hand Questionnaire. Braz J Med Biol Res. 2005;38(2):293-302. [DOI] [PubMed] [Google Scholar]
- 26. Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg Am. 2002;27(2):243-251. [DOI] [PubMed] [Google Scholar]
- 27. Adams BD, Samani JE, Holley KA. Triangular fibrocartilage injury: a laboratory model. J Hand Surg Am. 1996;21(2):189-193. [DOI] [PubMed] [Google Scholar]
- 28. Gofton WT, Gordon KD, Dunning CE, et al. Comparison of distal radioulnar joint reconstructions using an active joint motion simulator. J Hand Surg Am. 2005;30(4):733-742. [DOI] [PubMed] [Google Scholar]
- 29. Fulkerson JP, Watson HK. Congenital anterior subluxation of the distal ulna: a case report. Clin Orthop Relat Res. 1978(131):179-182. [PubMed] [Google Scholar]
- 30. Bowers WH. Instability of the distal radioulnar articulation. Hand Clin. 1991;7(2):311-327. [PubMed] [Google Scholar]
- 31. Seo KN, Park MJ, Kang HJ. Anatomic reconstruction of the distal radioulnar ligament for posttraumatic distal radioulnar joint instability. Clin Orthop Surg. 2009;1(3):138-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. El-Haj M, Baughman C, Thirkannad SM. A technique for treating dorsal instability of the distal radioulnar joint. Tech Hand Up Extrem Surg. 2017;21(2):67-70. [DOI] [PubMed] [Google Scholar]