Abstract
Background: The purpose of this study was to investigate variations in radiographic metacarpal anatomy as it relates to intramedullary (IM) fixation of metacarpal fractures and to compare this anatomy with available headless screw dimensions. Methods: We radiographically analyzed posteroanterior and lateral (LAT) radiographs of 120 metacarpals across 30 patients without structural abnormalities. Primary outcomes included IM isthmus diameter, isthmus location, metacarpal cascade, and head entry point collinear with IM canal. Measurements were compared with a list of commercially available headless screws used for IM fixation. Results: The average largest isthmus diameter was in the small metacarpal (3.4 mm), followed by the index (2.8 mm), long (2.7 mm), and ring (2.7 mm) metacarpals. The average cascade angle between long and index, long and ring, and long and small metacarpals was 0°, 24°, and 27°, respectively. The appropriate head entry point ranged between 25% and 35% from the dorsal surface of the metacarpal head on a LAT view. The retrograde isthmus location of the index and long finger was 39.2 and 38.1 mm, respectively. Twenty-five screws from 7 manufacturers were analyzed with sizes ranging from 1.7 to 4.5 mm. Only 8 of 17 screws between 2.3 and 3.5 mm had a length range above 35 mm. Conclusions: Metacarpal head entry point and cascade angle can help identify the appropriate reduction with the guide pin starting point in the dorsal 25% to 35% of the metacarpal head. Surgeons should be mindful to choose the appropriate fixation system in light of the variations between metacarpal isthmus size, isthmus location, and available screw lengths.
Keywords: headless compression screws, metacarpal, intramedullary, anatomy, radiographic
Background
Metacarpal fractures are responsible for 10% of all fractures and account for 18% to 41% of hand injuries presenting to the emergency department or urgent care.1-3 Most of the hand fractures result from a fall, crush injury, or direct impact with the hand and can occur in the base, shaft, head, or neck.
Due to the variation in fracture type and pattern, different treatment options should be tailored for each injury presentation. Operative treatment is generally indicated for mal-rotated, significantly shortened, unstable, or intra-articular fractures. Indications for metacarpal fixation include multitrauma patients, severe soft-tissue injury of the hand, metacarpal bone loss, and multiple metacarpal/hand fractures.1,4 Many implant options are available for the treatment of metacarpal fractures, including Kirschner wires (K-wires), lag screws, plate and screw constructs, and wire techniques (cerclage, interosseous, and tension band fixation).4,5 More recently, the use of intramedullary headless cannulated screws (IM HCS) has gained popularity as a technique for fixation of certain types of metacarpal fractures.6,7
Considering that plain radiographs serve as the usual diagnostic modality for metacarpal fractures, we have chosen to investigate the radiographic parameters of metacarpal anatomy as it relates to IM fixation of metacarpal fractures. The purpose of this study was to assess radiographic dimensions of the index through small metacarpals and then compare those results with the dimensions of commonly available HCS for appropriate fit.
Methods
This was a retrospective study of 30 subjects (15 men and 15 women) between the ages of 18 and 60 years selected randomly from a pool of patients who presented to our clinic. Standard posteroanterior (PA) and slightly pronated lateral (LAT) radiographs of the hand were reviewed. Participants with any history of previous hand fractures and inflammatory arthritis or evidence of any hardware or bony and soft-tissue abnormalities of the hand on radiograph were excluded.
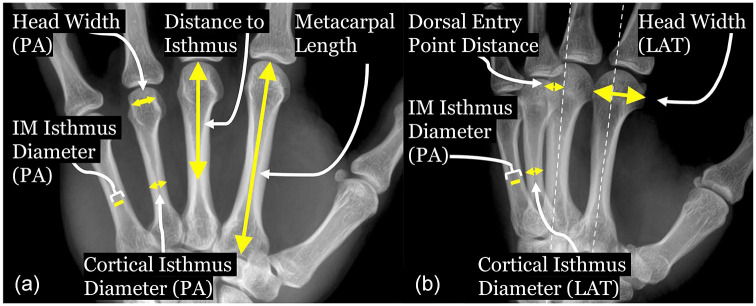
All radiographs were measured on the Sectra IDS7 (Linköping, Sweden) diagnostic imaging platform by an orthopedic surgery resident and reviewed by a fellowship-trained orthopedic hand surgeon. All measures taken within the imaging system were standardized for magnification. Measurements recorded in the PA and LAT radiographs included metacarpal length, IM isthmus diameter at the isthmus, metacarpal diameter at the isthmus (or cortical isthmus diameter), retrograde isthmus IM distance, isthmus bicortical thickness, and metacarpal head width. The isthmus bicortical thickness was calculated by subtracting the IM isthmus diameter from the cortical isthmus diameter (Figure 1). The reported isthmus bicortical thickness was reported as an average of the cortical thickness on the PA and LAT views. The projected ideal head entry point was calculated from LAT radiographs and was defined as the point at the metacarpal head that was collinear with the center of the IM canal (Figure 1). That point’s distance from the dorsal surface of the metacarpal neck was reported as a proportion of the metacarpal head width as seen on the LAT radiograph. The cross-sectional area of the metacarpal head was calculated from LAT and PA diameters at the widest portion of the head.
Figure 1.
Diagrammatic depiction of radiographic measurements.
Note. All measurements are referenced through the central axis of the metacarpal as depicted on lateral radiograph (b). (a) PA radiograph showing measurement of retrograde head to isthmus distance—“distance to isthmus”; head width, metacarpal length, cortical width at isthmus—“cortical isthmus diameter”; and canal width at isthmus—“IM isthmus diameter.” (b) LAT radiograph showing measurement of lateral head width, distance from dorsal surface to center of intramedullary canal—“dorsal entry point distance”; metacarpal length, cortical width at isthmus—“cortical isthmus diameter”; and canal width at isthmus—“IM isthmus diameter.” PA = posteroanterior; LAT = lateral; IM = intramedullary.
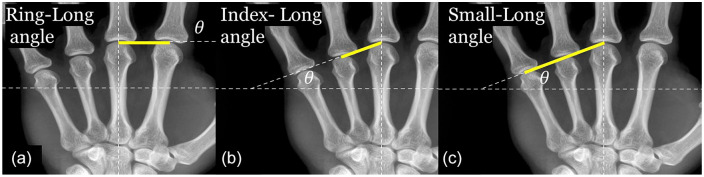
The metacarpal head cascade angle was measured on the PA view relative to a reference line—a line perpendicular to central axis of the long metacarpal placed at the distal edge of the metacarpal head. Lines were then drawn from the apex of the long metacarpal head to the apices of the index, ring, and small metacarpal heads. The measurement of the angle formed between the reference line and that extending to the other metacarpal heads was measured (Figure 2).
Figure 2.
Diagrammatic depiction of cascade angle measurements. Cascade angles referenced by the line perpendicular to the long axis of the long metacarpal: (a) index to long angle, (b) ring to long angle, and (c) small to long angle.
Sex differences were analyzed using the independent-samples t test. Differences within the same individual were analyzed using the paired-sample t test. All advanced statistical analysis was performed using SPSS Statistics 25.0 (IBM, Armonk, New York).
These measurements were then compared with 25 commercially available HCS recording the leading and trailing thread diameters and available lengths. The screws were chosen based on surgeon experience and the public availability of operative technique guides which contained the specifications of interest. We considered a screw to fit without reaming if the average screw diameter of the leading and trailing threads was less than or equal to the narrowest measured canal isthmus diameter. We also calculated the percentage of head occupied by the trailing portion of the HCS.
Results
There were 30 patients (15 men and 15 women) with an average age of 36.9 years (range, 18-60 years). There was no significant difference in age between men and women (34.5 vs 39.3 years; P < .05). The index metacarpal was the longest in length (67.3 mm), followed closely by the long metacarpal (64.9 mm) and then the ring and small metacarpals (57.1 and 52.5 mm, respectively) (Table 1). The 2-sample t test showed that men had statistically longer metacarpal bones in all 4 digits (P < .05) (Table 2). The average distance from the metacarpal head to the isthmus was longest for the index finger (39.2 mm), followed by the long (38.1 mm), ring (32.0 mm), and small fingers (28.2 mm) (Table 1 and Figure 3).
Table 1.
Anatomical Measurements.
| Radiographic Parameter | Index (n = 30) | Long (n = 30) | Ring (n = 30) | Small (n = 30) |
|---|---|---|---|---|
| PA metacarpal length | 67.3 ± 4.8 | 64.9 ± 4.5 | 57 ± 4.2 | 52.5 ± 4.2 |
| PA IM isthmus diameter | 2.9 ± 1.1 | 2.7 ± 0.8 | 2.7 ± 0.8 | 3.7 ± 0.9 |
| LAT IM isthmus diameter | 2.8 ± 1.0 | 3.2 ± 0.9 | 3.1 ± 0.9 | 3.4 ± 0.8 |
| PA isthmus distance | 39.2 ± 3.0 | 38.1 ± 2.7 | 32 ± 3.3 | 28.2 ± 3.0 |
| PA head width | 15.3 ± 1.7 | 15.8 ± 1.7 | 13.1 ± 1.5 | 12.4 ± 1.4 |
| LAT head width | 18.4 ± 2.0 | 17.4 ± 1.7 | 14.7 ± 1.6 | 13.2 ± 1.8 |
| LAT dorsal entry distance | 6.4 ± 1.3 | 5.3 ± 1.4 | 4.4 ± 0.9 | 3.8 ± 0.7 |
| LAT dorsal entry/Head width | 0.4 ± 0.05 | 0.3 ± 0.05 | 0.3 ± 0.06 | 0.3 ± 0.05 |
| Isthmus cortical thickness | 5.6 ± 0.67 | 5.2 ± 0.60 | 3.8 ± 0.49 | 3.5 ± 0.72 |
| Head cross-sectional area | 222.4 ± 45.2 | 218.6 ± 43.2 | 153 ± 32.2 | 130 ± 28.4 |
| (n = 30) | ||||
| Index to long cascade angle | 0 ± 3.2 | |||
| Ring to long cascade angle | 24 ± 3.4 | |||
| Small to long cascade angle | 26.8 ± 3.1 |
Note. Data represent mean (mm) ± SD; cascade angles are in degrees compared with the orthogonal line to long axis of long metacarpal. PA = posteroanterior; LAT = lateral; IM = Intramedullary.
Table 2.
Sex Differences of Anatomical Measurements.
| Index |
Long |
Ring |
Small |
|||||
|---|---|---|---|---|---|---|---|---|
| Radiographic Parameter | Male (n = 15) | Female (n = 15) | Male (n = 15) | Female (n = 15) | Male (n = 15) | Female (n = 15) | Male (n = 15) | Female (n = 15) |
| PA metacarpal length | 69.8 ± 4.8 | 64.5 ± 3.0 * | 67 ± 4.1 | 62.6 ± 3.7 * | 58.9 ± 3.9 | 55 ± 3.4 * | 55 ± 3.4 | 49.8 ± 3.3 * |
| PA IM isthmus diameter | 3.4 ± 1.1 | 2.5 ± 0.8 * | 2.9 ± 0.9 | 2.5 ± 0.6 | 2.9 ± 0.8 | 2.4 ± 0.7 | 4 ± 0.8 | 3.6 ± 0.9 |
| LAT IM isthmus diameter | 3.3 ± 1.1 | 2.3 ± 0.7 * | 3.5 ± 1.0 | 2.9 ± 0.8 | 3.4 ± 1.0 | 2.8 ± 0.7 | 3.9 ± 0.6 | 3 ± 0.7 * |
| PA isthmus distance | 40.5 ± 2.6 | 37.8 ± 2.7 | 39.3 ± 2.7 | 36.8 ± 2.2 | 32.7 ± 2.6 | 31.3 ± 3.9 | 29.6 ± 2.7 | 26.7 ± 2.7 |
| PA head width | 16.4 ± 1.5 | 14 ± 0.8 * | 17.1 ± 1.3 | 14.5 ± 1.0 * | 14.1 ± 1.2 | 12.1 ± 1.0 * | 13.3 ± 1.1 | 11.4 ± 1.1 * |
| LAT head width | 19.5 ± 2.1 | 17.3 ± 1.1 * | 18.5 ± 1.4 | 16.2 ± 1.2 * | 15.8 ± 1.2 | 13.5 ± 1.0 * | 14.3 ± 1.7 | 11.9 ± 0.8 * |
| LAT dorsal entry distance | 7 ± 1.2 | 5.8 ± 1.1 | 6.3 ± 1.4 | 5.2 ± 1.3 | 4.4 ± 0.8 | 4.4 ± 1.1 | 3.9 ± 0.8 | 3.6 ± 0.6 |
| LAT dorsal entry/Head width | 0.4 ± 0.05 | 0.33 ± 0.05 | 0.3 ± 0.07 | 0.32 ± 0.06 | 0.28 ± 0.04 | 0.3 ± 0.06 * | 0.3 ± 0.04 | 0.3 ± 0.05 |
| Isthmus cortical thickness | 5.8 ± 0.62 | 5.4 ± 0.68 | 5.4 ± 0.65 | 4.9 ± 0.41 * | 4 ± 0.53 | 3.6 ± 0.31 * | 3.9 ± 0.65 | 3.2 ± 0.63 * |
| Head cross-sectional area | 252.5 ± 43.5 | 190.1 ± 13.6 * | 249 ± 35.1 | 186.4 ± 23.3 * | 175.8 ± 25.4 | 129 ± 17.3 * | 150.3 ± 23.1 | 108.4 ± 13.8 * |
| Male |
Female |
|||||||
| (n = 15) | (n = 15) | |||||||
| Index to long cascade angle | (−) 0.5 ± 3.1 | 0.5 ± 3.4 | ||||||
| Ring to long cascade angle | 23.8 ± 4.0 | 24.2 ± 2.6 | ||||||
| Small to long cascade angle | 25.8 ± 2.9 | 27.9 ± 3.0 | ||||||
Note. Data represent mean (mm) ± SD; cascade angles are in degrees compared with the orthogonal line to long axis of long metacarpal. PA = posteroanterior; LAT = lateral; IM = intramedullary.
P < .05.
Figure 3.
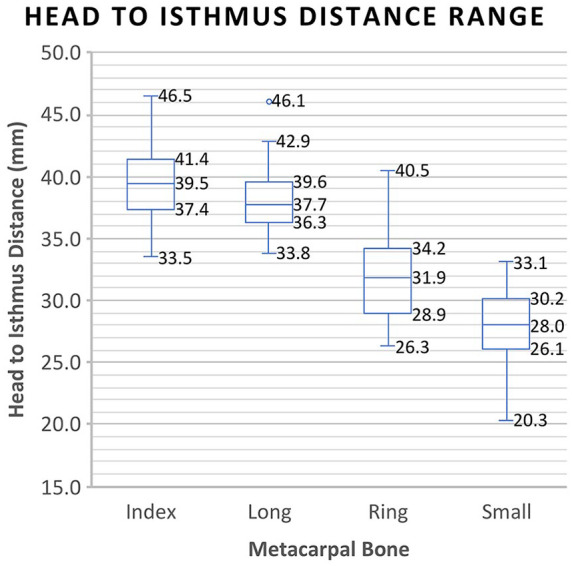
Distance from metacarpal head to isthmus (mm). Mean and interquartile ranges of the retrograde distance from the metacarpal head to the location of the isthmus in the index, long, ring, and small metacarpals.
On the PA projection, the small metacarpal has the widest isthmus canal diameter (3.7 mm), followed by the index (2.9 mm), long (2.7 mm), and ring (2.7 mm) metacarpals. On the LAT projection, the isthmus IM canal diameter was again widest for the small metacarpal (3.4 mm), followed by the long (3.2 mm), ring (3.1 mm), and index (2.8 mm) metacarpals. The paired-sample t test comparing PA and LAT isthmus canal diameter found that the long and ring metacarpals were narrower on the PA view, whereas the small metacarpal was narrower on the LAT view (P < .05) (Table 2). There was no difference in the index canal diameter at the isthmus on the PA versus LAT view (P = .248). We also found a wide range in the isthmus diameter from a minimum of 1 to 5.7 mm across all metacarpals (Figure 4).
Figure 4.
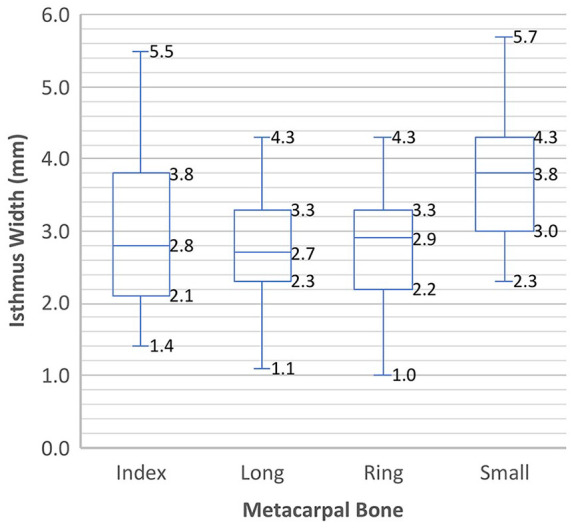
Isthmus width range (mm). Mean and interquartile ranges of the width of the isthmus on the posteroanterior view in the index, long, ring, and small metacarpals.
Isthmus bicortical thickness was greatest at the index (5.6 mm), followed by the long (5.2 mm), ring (3.8 mm), and small (3.5 mm) metacarpals (Table 1). Although the isthmus bicortical thickness at the index metacarpal was not statistically different between men and women (5.8 mm vs 5.4 mm, P = .130), men had a statistically thicker cortical bone at the isthmus in the long, ring, and small metacarpals (p < .05) (Table 2). A Pearson correlation test controlling for sex showed that the long metacarpal average thickness had a moderate negative correlation with age with an r coefficient of −0.40 and P value of .03. There was a negative correlation for the index (r = −0.26), ring (r = −0.33), and small (r = −0.13) metacarpals; however, these values are not statistically significant.
The cascade angle from index to long finger was 0°, from long to ring finger was 24°, and from long to small finger was 26.8°. There was no statistically significant difference between men and women in any of the cascade angles. The proportion of the distance of the head entry point from dorsal surface to the LAT width of the metacarpal head was 0.35, 0.33, 0.29, and 0.29 between the index, long, ring, and small metacarpals, respectively (Table 1).
Dimensions of 25 commercially available screws, appropriate for IM metacarpal fixation, from 7 manufacturers were tabulated (Table 3). The leading thread diameter ranged from 1.7 to 4.5 mm, and trailing thread diameters ranged from 2.1 to 5.8 mm. The trailing head of the available screws occupied 2.2% to 7.1% of the head cross-sectional area for the index metacarpal, 3.2% to 7.3% for the long metacarpal, 4.6% to 10.4% for the ring metacarpal, and 6.2% to 9.8% for the small metacarpal. There are a wide variety of screw lengths available with the smaller diameter screws generally manufactured in shorter lengths. The maximum length available for most of the screws was less than the average metacarpal lengths. Only 4 (Zimmer HCS 4.5, Exosmed Innate 4.0, Stryker AutoFIX 3.0, Stryker AutoFIX 4.0) of the 25 screws are produced in lengths of 50 mm or longer.
Table 3.
Screw Specifications (mm).
| Implant | Leading thread diameter, mm | Trailing thread diameter, mm | Cross-sectional area of trailing head, mm2 | Length, mm | |
|---|---|---|---|---|---|
| Acumed Acutrak Micro a | 2.5 | 2.8 | 6.2 | 8 | 20 |
| Acumed Acutrak Mini a | 3.5 | 3.6 | 10.2 | 16 | 30 |
| Acumed Acutrak Standard a | 4.0 | 4.1 | 13.2 | 16 | 34 |
| Acumed Acutrak Fusion a | 2.0 | 2.5 | 4.9 | 14 | 24 |
| Zimmer Mini Herbert b | 2.5 | 3.2 | 8.0 | 14 | 24 |
| Zimmer Herbert 3.0 b | 3.0 | 3.9 | 11.9 | 12 | 30 |
| Zimmer HCS 4.5 b | 4.5 | 5.8 | 26.4 | 25 | 100 |
| Exosmed Innate 4.0 c | 4.0 | 4.5 | 15.9 | 35 | 75 |
| Depuy Synthes HCS 2.4 (ST) d | 2.4 | 3.1 | 7.5 | 9 | 40 |
| Depuy Synthes HCS 2.4 (LT) d | 2.4 | 3.1 | 7.5 | 17 | 40 |
| Depuy Synthes HCS 3.0 (ST) d | 3.0 | 3.5 | 9.6 | 10 | 40 |
| Depuy Synthes HCS 3.0 (LT) d | 3.0 | 3.5 | 9.6 | 10 | 40 |
| Depuy Synthes HCS 4.5 d | 4.5 | 5.0 | 19.6 | 16 | 40 |
| Stryker AutoFIX 2.0 e | 2.0 | 3.0 | 7.1 | 10 | 30 |
| Stryker AutoFIX 2.5 e | 2.5 | 3.3 | 8.5 | 10 | 30 |
| Stryker AutoFIX 3.0 e | 3.0 | 4.0 | 12.6 | 12 | 60 |
| Stryker AutoFIX 4.0 e | 4.0 | 5.2 | 21.2 | 20 | 50 |
| Stryker Fixos 2.5 e | 2.5 | 3.4 | 9.1 | 10 | 30 |
| Stryker Fixos 3.5 e | 3.5 | 4.2 | 13.8 | 14 | 24 |
| Skeletal Dynamics Reduct 2.5 f | 2.6 | 3.2 | 8.0 | 10 | 30 |
| Skeletal Dynamics Reduct 3.5 f | 3.4 | 4.0 | 12.6 | 10 | 30 |
| TriMed Cannulated Screw 1.7 g | 1.7 | 2.4 | 4.5 | 8 | 14 |
| TriMed Cannulated Screw 2.3 g | 2.3 | 3.0 | 7.1 | 10 | 28 |
| TriMed Cannulated Screw 3.0 g | 3.0 | 4.0 | 12.6 | 10 | 36 |
| TriMed Cannulated Screw 3.5 g | 3.5 | 4.5 | 15.9 | 20 | 45 |
| Range | 1.7-4.5 | 2.1-5.8 | 3.5-26.4 | 8-100 | |
Acumed (Hillsboro, Oregon).
Zimmer (Warsaw, Indiana).
Exosmed (Aliso Viejo, California).
Depuy Synthes (Raynham, Massachusetts).
Stryker (Kalamazoo, Michigan).
Skeletal Dynamics (Miami, Florida).
TriMed, Inc (Valencia, California).
Discussion
Several options for fixation of metacarpal shaft and neck fractures are available, such as lag screws, plate fixation, K-wire pinning, and IM HCS fixation. Intramedullary pinning using K-wires can be performed antegrade with bouquet-shaped technique or via a retrograde technique. In addition, K-wires can be used to pin adjacent metacarpals together for increased points of stabilization. 1 The K-wire fixation using a bouquet technique has remained a popular treatment choice due to its ease of application and minimal soft-tissue violation.4,8 However, there are inherent downsides to this technique. The K-wires are typically left external to the skin for later removal and pose a risk for pin site infection. In addition, K-wires tether soft-tissue structures which can interfere with attempts to regain early digital motion. 4 Plate fixation and screw fixation are often necessary for stabilizing comminuted fractures. While plate fixation allows early mobilization, the soft-tissue dissection required can risk avascular necrosis, soft-tissue adhesions, and joint stiffness.9,10 Antegrade IM wire fixation is another treatment method that has shown good results in terms of range of motion, dash scores, pain, and operative time.8,11-14 Complications associated with this technique are K-wire migration and distal perforation of the metacarpal head.8,14,15 This form of fixation, however, does not provide truly rigid fixation and has shown biomechanical stiffness compared with crossed K-wires.6,16,17 These constructs may need longer duration of immobilization when compared with IM screw fixation; however, this should be further studied. 8
The IM HCS fixation minimizes several of these risks. The procedure is performed using a limited-open or percutaneous retrograde approach through the dorsal aspect of the metacarpal head avoiding soft-tissue dissection required for screw and plate fixation. The screw diameter can be sized to fit within the canal with or without reaming.4,18 As the hardware is buried in the bone, there is less risk for soft-tissue adhesions. Finally, the IM HCS construct is typically strong enough to permit immediate range of motion exercises, typically not possible with K-wire fixation. Few complications have been reported in the literature. In a systematic review of HCS fixation for metacarpal fractures, Beck et al 19 found no serious complications reported—9 minor complications including 4 cases of hardware removal in asymptomatic patients for suspected intra-articular screw penetration, screw migration, and 2 at patients’ request.
Our study aimed to radiographically assess index through small metacarpal radiographic parameters as they relate to the sizing of a headless compression screw for IM metacarpal fixation. The results highlighted many differences between the digits and were able to reproduce findings from several cadaveric and radiographic studies.22-24 Our study has contributed additional metacarpal parameters pertinent to the application of IM HCS fixation, including metacarpal isthmus diameter, isthmus bicortical thickness, appropriate distal entry point, and metacarpal cascade angles, to help understand metacarpal alignment.
Previous studies specific for HCS reported ranges from 2.2 to 4.0 mm diameter and 26 to 50 mm length.7,19,20,25-30 Del Piñal et al 7 recommended using 3-mm diameter screws in the index, long, and ring metacarpal fractures while using a 4-mm screw in the small metacarpal. This study is consistent with these sizes and further elucidates the limits in screw lengths available for IM fixation.
Several metacarpal isthmus characteristics need to be considered for IM HCS fixation, including isthmus location and diameter. The screw diameter must be appropriate to fit through the isthmus, and possibly engage the cortex, without causing iatrogenic fracture or incarceration from size mismatch. This can be done with a reamed technique or by simply sizing the screw to fit appropriately in the isthmus. Finally, screw length is important for determining what will reach within the isthmus and potentially beyond the isthmus. Comparing our compiled list of screws with the metacarpal isthmus diameters and locations shows that screw sizes between 2.4 and 4.0 mm can roughly account for the average size of the canal at the isthmus that would allow engagement of the screw threads. The isthmus location of the index and long fingers is 39.2 and 38.1 mm respectively; however, 11 of 19 screws had sets of this size under 40 mm of maximum length. There is a potential deficit in screw size for fracture of the index and long metacarpals.
Another isthmus consideration is the tolerance of this area for IM reaming as it relates to cortical thickness at the isthmus. It is not known how much reaming the metacarpal can tolerate before risking iatrogenic fracture, but unlike other larger tubular bones that are reamed for IM fixation such as the femur or tibia, there is much less tolerance for overreaming. The average isthmus bicortical thickness was 5.7, 5.2, 3.8, and 3.5 mm for the index, long, ring, and small metacarpals, respectively. Men also had greater cortical thickness compared with women in the long, ring, and small metacarpals. These results would indicate that the small and ring metacarpals would be less tolerant to reaming, particularly in female patients. However, further studies are needed to fully describe this theoretical risk.
Alignment of the metacarpals, and specifically metacarpal shortening with fracture, can be evaluated with the cascade angle and can be useful for assessing reduction or overshortening. There were no sex differences between men and women. The distal apex of the index and long metacarpals is at the same level based on an index long cascade angle of 0°. The average angle between the long and ring metacarpals is 24.0° versus 26.8° in the long and small metacarpals. Thus, as a rough estimate, one can assume that index, ring, and small metacarpal head apices are relatively collinear. These angular relationships can be used to approximate the amount of shortening of a metacarpal fracture. For example, in a ring finger metacarpal injury, a line from the apex of the long to small metacarpal head should align with the ring metacarpal head. The metacarpal head distance from this tangent line is an estimate of shortening. Furthermore, this aids in evaluating restoration of length and the quality of the reduction radiographically. This is especially important when reducing a fracture with comminution where the metacarpal bone is unstable in length. Intramedullary headless cannulated screws have a relative contraindication within this setting.
The projected optimal head entry point is the point collinear with the IM canal and ranged between 29% and 35% of the metacarpal head width measured from the dorsal cortex seen on the LAT view. As a general guideline, centering the distal entry point at the dorsal one-third of the metacarpal head should produce appropriate metacarpal head and shaft fragment alignment and proper trajectory to the isthmus. Furthermore, biasing the distal entry point to the dorsal one-third of the articular surface of the metacarpal head places the reamer hole in a more forgiving area of the articular surface as noted by ten Berg et al 18 who found that such placement avoided engaging the center of the articular base of the proximal phalanx in the more clinically relevant sagittal arc of motion.
Fixation within the cancellous bone of the distal metacarpal metaphysis and head is improved with a larger diameter screw. However, this consideration needs to be weighed against minimizing articular surface damage to accommodate the screw diameter. The percentage volume occupied by the trailing end of the 2.4- and 3-mm screws within the metacarpal head has been measured as a mean of 4% of subchondral volume by others with quantitative computed tomographic analysis. 14 Our results showed a similar small percentage of area projected to be occupied by the trailing end of the IM HCS in the metacarpal head cross section, ranging from 3.2% to 10% of the metacarpal head cross section. When this size defect is in the dorsal segment of the head, this is likely to be clinically insignificant as shown by Ruchelsman et al. 30
This study has its limitations. First, there are inherent limitations in assessing 3-dimensional anatomy based solely on 2-dimensional plain radiographs. While all images were stored and measured using the same software, there is a possibility that the images were magnified and subsequently not adjusted. Second, we used the slight oblique radiographic view as an approximation for a lateral film so that we could better visualize each individual metacarpal. Our study was based on subjects with normal bone morphology, so our conclusion may not be applicable to patients with bony abnormalities or arthritic distortion. Such situations may require different screw design and sizes. 31 Our study assumes that the best fit for screws is in the isthmus; however, there is no study showing this is true nor does it show that an isthmus fitting screw improves patients’ outcomes. Furthermore, with the reamed technique, the effective length of the isthmus is increased, making a precise isthmus location less helpful. Finally, our study evaluated 7 manufacturers’ commercially available HCS regarding screw lengths and diameters. This is not a completely exhaustive list of all available commercial screw options and was limited to screws with publicly available technique guides that displayed all specifications of interest. We did not analyze differences in screw shape, thread characteristics (pitch, partially thread, fully threaded), and screw material, which could affect application and strength.
This study demonstrates that although there are differences between sexes and between metacarpals within the same individuals, there are also several radiographic landmarks that are relatively consistent, such as distal entry point and cascade angle, which can be used to approximate screw placement and fracture reduction. Surgeons should be mindful of the anatomical variations, specifically the thinner isthmus cortical thickness in the small and ring fingers, especially in women, as well as the capacious nature of the small metacarpal isthmus space, especially in men. The index and long metacarpal bones may not have screws appropriately sized in width and length for the isthmus that are long enough to reach, so preoperative planning with the appropriate system is necessary. Given that the index and long metacarpals have relatively thick cortices at the isthmus, reaming to widen the isthmus may help accommodate a larger, longer screw. Future modifications to HCS design that accounts for the parameters explored in this study may improve the application of this technique for certain metacarpal fractures.
Footnotes
Disclosure: Nothing material or monetary was received by any of the authors in the execution of this study and the subsequent production of this manuscript.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Michael Okoli  https://orcid.org/0000-0003-4775-9367
https://orcid.org/0000-0003-4775-9367
References
- 1. Cotterell I, Richard M. Metacarpal and phalangeal fractures in athletes. Clin Sports Med. 2015;34(1):69-98. doi: 10.1016/S0278-5919(05)70098-3. [DOI] [PubMed] [Google Scholar]
- 2. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908-915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 3. Nakashian MN, Pointer L, Owens BD, et al. Incidence of metacarpal fractures in the US population. Hand. 2012;7(4):426-430. doi: 10.1007/s11552-012-9442-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kollitz KM, Hammert WC, Vedder NB, et al. Metacarpal fractures: treatment and complications. Hand. 2014;9(1):16-23. doi: 10.1007/s11552-013-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kozin SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal fractures and phalangeal shaft fractures. J Am Acad Orthop Surg. 2000;8(2):111-121. [DOI] [PubMed] [Google Scholar]
- 6. Avery DM, Klinge S, Dyrna F, et al. Headless compression screw versus Kirschner wire fixation for metacarpal neck fractures: a biomechanical study. J Hand Surg Am. 2017;42(5):392.e1-392.e6. doi: 10.1016/j.jhsa.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 7. del Piñal F, Moraleda E, Rúas JS, et al. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am. 2015;40(4):692-700. doi: 10.1016/j.jhsa.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 8. Padegimas EM, Warrender WJ, Jones CM, et al. Metacarpal neck fractures: a review of surgical indications and techniques. Arch Trauma Res. 2016;5(3):e32933. doi: 10.5812/atr.32933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Buchler U, Fischer T. Use of a minicondylar plate for metacarpal and phalangeal periarticular injuries. Clin Orthop Relat Res. 1987(214):53-58. [PubMed] [Google Scholar]
- 10. Facca S, Ramdhian R, Pelissier A, et al. Fifth metacarpal neck fracture fixation: locking plate versus K-wire? Orthop Traumatol Surg Res. 2010;96(5):506-512. doi: 10.1016/j.otsr.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 11. Corkum JP, Davison PG, Lalonde DH. Systematic review of the best evidence in intramedullary fixation for metacarpal fractures. Hand. 2013;8(3):253-260. doi: 10.1007/s11552-013-9531-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhang B, Hu P, Yu K-L, et al. Comparison of AO titanium locking plate and screw fixation versus anterograde intramedullary fixation for isolated unstable metacarpal and phalangeal fractures. Orthop Surg. 2016;8(3):316-322. doi: 10.1111/os.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mirza A, Mirza J, Healy C, et al. Radiographic and clinical assessment of intramedullary nail fixation for the treatment of unstable metacarpal fractures. Hand. 2018;13(2):184-189. doi: 10.1177/1558944717695747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ozer K, Gillani S, Williams A, et al. Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. J Hand Surg Am. 2008;33(10):1724-1731. doi: 10.1016/j.jhsa.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 15. Balaram AK, Bednar MS. Complications after the fractures of metacarpal and phalanges. Hand Clin. 2010;26(2):169-177. doi: 10.1016/j.hcl.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 16. Curtis BD, Fajolu O, Ruff ME, et al. Fixation of metacarpal shaft fractures: biomechanical comparison of intramedullary nail crossed K-wires and plate-screw constructs. Orthop Surg. 2015;7(3):256-260. doi: 10.1111/os.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Beutel BG, Ayalon O, Kennedy OD, et al. Crossed K-wires versus intramedullary headless screw fixation of unstable metacarpal neck fractures: a biomechanical study. Iowa Orthop J. 2018;38:153-157. [PMC free article] [PubMed] [Google Scholar]
- 18. ten Berg PW, Mudgal CS, Leibman MI, et al. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg Am. 2013;38(2):322-330. doi: 10.1016/j.jhsa.2012.09.029. [DOI] [PubMed] [Google Scholar]
- 19. Beck CM, Horesh E, Taub PJ. Intramedullary screw fixation of metacarpal fractures results in excellent functional outcomes: a literature review. Plast Reconstr Surg. 2019;143(4):1111-1118. doi: 10.1097/PRS.0000000000005478. [DOI] [PubMed] [Google Scholar]
- 20. Jann D, Calcagni M, Giovanoli P, et al. Retrograde fixation of metacarpal fractures with intramedullary cannulated headless compression screws. Hand Surg Rehabil. 2018;37(2):99-103. doi: 10.1016/j.hansur.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 21. Lee J-K, Jo Y-G, Kim J-W, et al. Open reduction and internal fixation for intraarticular fracture of metacarpal head. Orthopade. 2017;46(7):617-624. doi: 10.1007/s00132-017-3392-8. [DOI] [PubMed] [Google Scholar]
- 22. McFadden D, Bracht MS. Sex and race differences in the relative lengths of metacarpals and metatarsals in human skeletons. Early Hum Dev. 2009;85(2):117-124. doi: 10.1016/j.earlhumdev.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. El Morsi DA, Al Hawary AA. Sex determination by the length of metacarpals and phalanges: X-ray study on Egyptian population. J Forensic Leg Med. 2013;20(1):6-13. doi: 10.1016/j.jflm.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 24. Manolis SK, Eliopoulos C, Koilias CG, et al. Sex determination using metacarpal biometric data from the Athens collection. Forensic Sci Int. 2009;193(1-3):130.e1-130.e6. doi: 10.1016/j.forsciint.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 25. Couceiro J, Ayala H, Sanchez M, et al. Intramedullary screws versus Kirschner wires for metacarpal fixation, functional, and patient-related outcomes. Surg J. 2018;4(1):e29-e33. doi: 10.1055/s-0038-1637002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Romo-Rodriguez R, Arroyo-Berezowsky C. [Minimal invasive osteosynthesis with cannulated screws in metacarpal fractures]. Acta Ortop Mex. 2017;31(2):75-81. [PubMed] [Google Scholar]
- 27. Tobert DG, Klausmeyer M, Mudgal CS. Intramedullary fixation of metacarpal fractures using headless compression screws. J Hand Microsurg. 2016;8(3):134-139. doi: 10.1055/s-0036-1593390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Doarn MC, Nydick JA, Williams BD, et al. Retrograde headless intramedullary screw fixation for displaced fifth metacarpal neck and shaft fractures: short term results. Hand. 2015;10(2):314-318. doi: 10.1007/s11552-014-9620-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. 2010;35(8):1260-1263. doi: 10.1016/j.jhsa.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 30. Ruchelsman DE, Puri S, Feinberg-Zadek N, et al. Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg Am. 2014;39(12):2390-2395. doi: 10.1016/j.jhsa.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 31. Morrell NT, Weiss APC. Silicone metacarpophalangeal arthroplasty for osteoarthritis: long-term results. J Hand Surg Am. 2018;43(3):229-233. doi: 10.1016/j.jhsa.2017.10.010. [DOI] [PubMed] [Google Scholar]