Abstract
Metal-on-metal disease (MOMD) is a rare condition following arthroplasty and has predominantly been reported following hip and knee replacement. Isolated case reports exist with respect to MOMD following total wrist arthroplasty—however, the literature remains limited. Here, we present the history and radiographic and histopathologic features of such a case, and summarize the literature and provide management recommendations.
Keywords: Motec, wrist arthroplasty, metal-on-metal disease, metallosis, pseudotumor
Introduction
Metal-on-metal (MOM) articulations have been used in hip arthroplasty since the 1960s, with proposed advantages including diminished volumetric wear and altered component size ratios (thinner acetabular component and larger femoral heads) resulting in increased stability and range of motion. However, reports of increased revision rates, and local and systemic pathology due to metal wear particles, have led to greater caution and diminished usage in the last decade.1,2
Wrist arthroplasty design has undergone many changes since its introduction. Early iterations concentrated on low-motion, high-constraint designs; recent generations have reversed this paradigm, aiming for greater range of motion and lower constraint, reflective of the native wrist. Some prostheses allow the option of MOM articulation to diminish wear and allow greater range of motion.
Isolated case reports exist with respect to MOMD following total wrist arthroplasty—however, the literature remains limited.3-7 Here, we present the history and radiographic and histopathologic features of such a case, and summarize the literature and provide suggestions regarding management.
Case
A 57-year-old left-handed male security guard was referred to our institution following a motorcycle accident. Radiographs and computed tomography (CT) demonstrated comminuted intra-articular left distal radius and ulna fracture dislocations (Figure 1). The closed fracture was provisionally reduced in the emergency department, with definitive fixation (via dorsal and volar locking distal radial plates and Kirschner wire fixation for the ulna) performed the following day. An open carpal tunnel release was also performed at this stage due to mild median nerve paraesthesia.
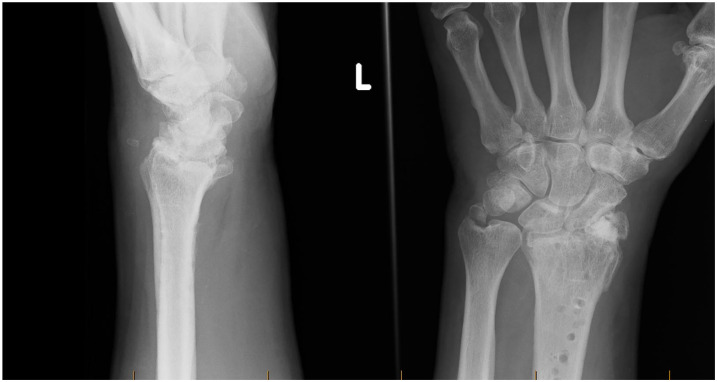
Figure 1.

Initial anteroposterior left wrist radiograph after injury demonstrating comminuted intra-articular left distal radius and ulna fracture dislocations.
The patient was immobilized in a cast for 6 weeks, given the extensively comminuted intra-articular fracture following which he received a thermoplastic splint and active movement exercises with hand therapy. All hardware was removed 3 months after the index operation due to irritation and stiffness. The patient then underwent formal hand therapy for rehabilitation; however, little improvement was noted. Six months after fixation, his range of motion was documented at 63° in the flexion-extension arc; 17° in the radioulnar deviation arc; and 145° of pronosupination. Grip strength was 8 kg on the left, compared with 42 kg on the uninjured contralateral limb. Progress radiographs revealed radiocarpal and distal radioulnar joint (DRUJ) post-traumatic arthritis (Figure 2), and the patient demonstrated progressive pain related to arc of motion.
Figure 2.
Left wrist anteroposterior and lateral radiographs performed 6 months after initial injury and following removal of distal radial plates. Note is made of progressive radiocarpal and distal radioulnar joint post-traumatic arthritis.
Salvage options, including wrist denervation, radioscapholunate arthrodesis, total wrist arthrodesis, and total wrist arthroplasty, were discussed with the patient. Although the DRUJ pathology was also noted, the radiocarpal joint was clinically the more symptomatic. Seven and a half months after initial fixation, the patient underwent a Motec total wrist arthroplasty (Swemac Innovation, Linköping, Sweden). Following proximal row carpectomy, the metacarpal was prepared and a 55-mm implant was inserted. The radius was then prepared for a 44-mm radial screw. Owing to wrist stiffness, a small neck was used, along with a MOM bearing surface (Figure 3).
Figure 3.
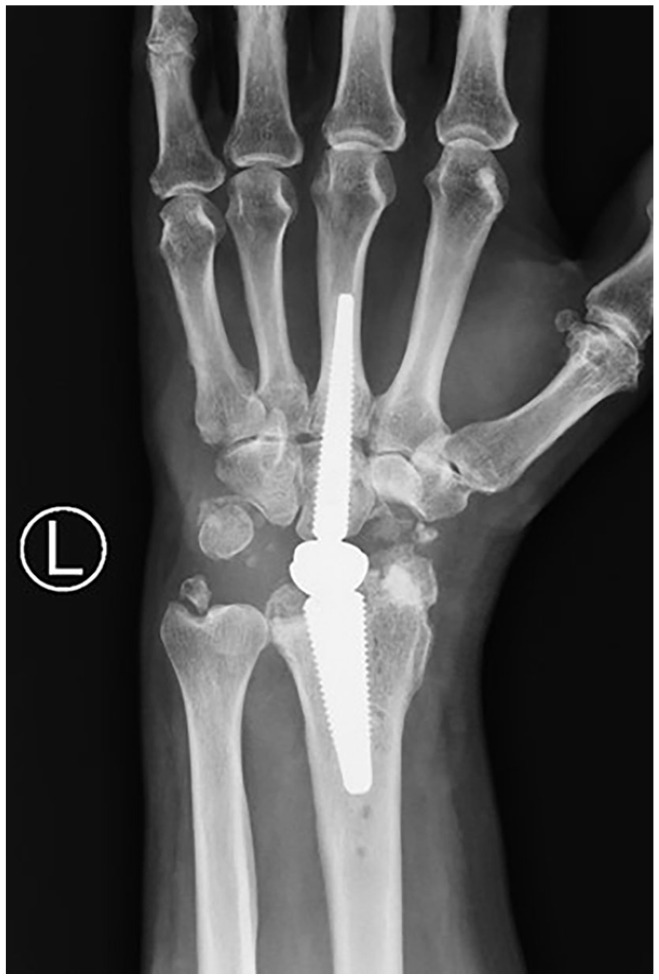
Initial anteroposterior left wrist radiograph performed postoperatively demonstrating noncemented left wrist arthroplasty components in situ.
Postoperatively, the patient was placed in a volar slab for 2 weeks, which was then converted to a thermoplastic splint. A regular hand therapy protocol was instituted. Substantial improvement in pain and range of motion was noted, with an 85° flexion-extension arc, 45° radioulnar deviation, and 134° of pronosupination achieved by 7 weeks after arthroplasty.
The postoperative course was complicated by ulna sided wrist pain thought to be related to post-traumatic DRUJ arthritis. After therapeutic and diagnostic corticosteroid injections, the patient underwent a distal ulna resection (Darrach procedure) approximately 6 and 8 months after arthroplasty, respectively. Despite this, the patient progressed well, with minimal pain, and was initially satisfied with the result of the arthroplasty, demonstrating 112° flexion-extension arc and 135° of pronosupination 1 year after arthroplasty.
However, over the next few months, the patient reported mild discomfort and recurrent dorsal wrist swelling. Serial radiographs demonstrated marked osteolysis surrounding the radial implant (Figure 4). This was confirmed on 3-dimensional imaging via CT and magnetic resonance imaging (MRI), which showed intermediate signal synovitis adjacent to the bone prosthesis interface (Figures 5 and 6). Serum cobalt levels were slightly elevated at 35 nmol/L (normal: <20 nmol/L), with normal chromium levels at 45 nmol/L. Metal-on-metal disease was suspected. The patient was counseled accordingly, with options of revision arthroplasty or arthrodesis offered. The patient was extremely satisfied with his motion and pain relief, and reluctant to undergo arthrodesis. Thus, the patient underwent a revision total wrist arthroplasty with synovectomy 16 months after initial arthroplasty.
Figure 4.

Anteroposterior left wrist radiograph performed 12 months postoperatively with subsequent distal ulna resection. Progressive lucency and extensive osseous resorption adjacent to the radial cup of the Motec wrist prosthesis (arrows) and the distal radius metaphysis.
Figure 5.
Axial (a) and sagittal (b) noncontrast computed tomography of the left wrist confirming progressive osseous resorption adjacent to the distal radius stem/ball-and-socket articulation (5b, arrow) with cortical defect in the medial distal radius (5a, arrow).
Figure 6.
Noncontrast magnetic resonance imaging left wrist.
Note. (a) Coronal STIR WARP. Intermediate signal synovitis adjacent to the bone prosthesis interface (arrow), which extends to abut the margin of the distal ulna resection. (b) Coronal PD WARP. Intermediate signal synovitis extending adjacent to the ulna resection, distal radial cup, and carpus.
Intraoperative findings included significant dark discoloration of surrounding soft tissues, which were sent for histopathological analysis (Figure 7). A thorough debridement was performed with extensive synovectomy. Both the metacarpal and radial implants were deemed stable, and revision not thought necessary. The short neck was exchanged for a medium neck, and the articulation was replaced with a metal-on-PEEK interface (PEEK or polyetheretherketone being an inert and biocompatible thermoplastic polymer). Stability and range of motion on table was excellent. It was theorized that the implant was impinged in terminal extension, resulting in edge loading and accelerated wear.
Figure 7.
(a, b) Intraoperative photograph demonstrating metallosis of surrounding soft tissue adjacent to the implant. (c) Histopathology of removed synovial tissue demonstrating mild to moderate predominantly chronic inflammatory cell infiltrate. In addition, there is a histiocytic and multinucleate giant cell reaction, several of which show polarisable foreign material within their cytoplasm. Histopathological features were in keeping with the clinical history of metallosis.
Postoperatively, the patient was immobilized in a volar slab for 4 weeks in an effort to avoid the terminal extension impingement. Three months after revision wrist arthroplasty, his range of motion comprised 55° of wrist extension, 35° of wrist flexion, 60° of supination, 85° of pronation, and 15° of ulna deviation and 5° of radial deviation. Grip strength was 11 kg on the left compared with 42 kg on the uninjured contralateral limb.
Discussion
Total wrist arthroplasty has advanced significantly since its initial iterations, which were based on high-constraint devices that resulted in abnormal stresses and raised failure and complication rates. Recent generations have adopted a philosophy of lower constraint and greater range of motion, with some implants providing MOM articulations aimed at altering component size relationships and increasing stability and range of motion. The Motec total wrist arthroplasty is one such implant, based on a ball-and-socket model. It adopts the philosophy of low constraint to allow increased range of motion and offers an option to facilitate conversion to arthrodesis as a salvage procedure in case of failure. Promising early to medium-term results have led to broadening of indications and patient eligibility, with more regular implantation. 3
Although MOMD has been widely described in weight-bearing joints, its prevalence in non-weight-bearing prostheses is far less well documented, with only 4 reports (involving 7 patients) in the setting of wrist arthroplasty found in the literature.3-7 Day described carpal tunnel syndrome secondary to MOMD in a 37-year-old female patient 6 years after implantation of Universal 2 total wrist implant (Integra Life Sciences, Plainsboro, New Jersey). 4 Preoperative imaging had demonstrated osteolysis surrounding both the carpal and radial implants. Open carpal tunnel release revealed extensive soft tissue discoloration and debris, which was reported as proliferative synovitis and exuberant foreign body giant cell reaction (consistent with implant-related arthropathy) on histopathology. Taha reported on a 54-year-old male patient who complained of intermittent pain and persistent dorsal swelling 6 years after implantation of Universal 2 implant. 5 Magnetic resonance imaging and intraoperative findings revealed a pseudotumor, and revision was performed with larger implants. Similarly, Heyes documented 4 cases of metallosis causing carpal tunnel syndrome in patients who underwent wrist arthroplasty with a Universal 2 prosthesis for end-stage inflammatory arthropathy. 6 He noted that all patients who developed carpal tunnel syndrome were women, younger (40-52 years old, compared with a mean of 55 years), and possessed significantly better flexion arcs (range: 65°-75°, compared with 30°-55°) than a control group that did not develop carpal tunnel syndrome. Open carpal tunnel release again revealed discolored particulate matter, tenosynovitis, and capsular synovitis; histopathology demonstrated a florid type IV hypersensitivity reaction with metal deposition, histiocytosis, and fibrinous proliferation. One patient underwent revision for ongoing pain and osteolysis—eccentric wear was noted on the edge of the polyethylene.
Although none of the aforementioned cases involved MOM articulations, both Day and Heyes hypothesized that component malposition and excessive range of motion may result in accelerated type 2 wear (between an articulating and nonarticulating surface), and recommended caution when considering wrist arthroplasty in high-demand, young patients with retained range of motion. Only 1 prior case has been documented involving a MOM articulation. Karjalainen described severe pain and functional deterioration in a 55-year-old man, commencing 6 months after Motec arthroplasty. 7 The wrist extension-flexion arc was maintained at 130°. By 18 months after arthroplasty, lysis and a periprosthetic foreign body was noted on radiographs, with MRI revealing a pseudotumor. Cobalt and chromium ion levels were elevated to 11.0 and 4.3 ppb, respectively. Revision to a metal-on-PEEK articulation resulted in resolution of symptoms and functional improvement.
Adverse local tissue reaction (ALTR) is the collective term used to categorize the reactive tissue inflammatory changes occurring as a response to metal wear products. 8 Metallosis is a subtype of local tissue reaction and refers to prosthetic loosening or fibrosis secondary to metal corrosion and wear—as such, it is primarily a surgical diagnosis. Imaging evaluation of ALTR plays a central role in prompt diagnosis and subsequent operative intervention aimed at reducing secondary soft tissue destruction.
Plain film radiography and CT imaging may demonstrate abnormal prosthetic alignment with associated erosion, periprosthetic foreign body, prosthetic loosening, and bony osteolysis in more advanced stages. The presence of radiodense metallic debris visible on plain film imaging has been associated with moderate to severe intraoperative grading of metallosis. 8 Previous studies suggest that more than half of the surgically proven cases of metallosis demonstrate no retrospective diagnostic features on plain film radiography. In addition to playing a role in potential aspiration or biopsy of lesions, ultrasound may be used to detect the sequelae of metallosis, such as echogenic fluid collections, pathologic tendon conditions, or bursitis.
Magnetic resonance imaging with metal artifact reduction sequences is the gold standard for both the diagnosis of ALTR and the associated follow-up, allowing detailed anatomical assessment of the tissue-implant interface, periprosthetic bone, and soft tissues.9,10 Magnetic resonance imaging has superior sensitivity than plain radiography and CT in the diagnosis and subsequent grading of ALTR, the characterization of pseudotumor or soft tissue lesions, and the evaluation of secondary muscular atrophy.2,9 Magnetic resonance imaging findings can include expansion of the pseudocapsule with homogeneity of the high signal intensity fluid. The synovial pattern can subsequently progress to a mixed solid-cystic appearance with associated debris resembling pseudotumors. Disruption of the pseudocapsule is commonly seen.9,10 Magnetic resonance imaging can also help to demonstrate imaging features more suggestive of localized infection including perisynovial edema, synovitis, and the presence of a joint effusion. Early hypertrophic soft tissue reaction, extracapsular collections, and subsequent bony destruction may also be appreciated.
Our case is the second description of MOMD resulting from MOM articulation in the setting of wrist arthroplasty in the literature, as well as the second in a ball-and-socket type prosthesis. Commonalities between all cases include a high range of motion and the relatively young age of patients. It seems that low levels of constraint may not be the panacea for wrist arthroplasty in all patients. We would recommend caution in performing wrist arthroplasty in young patients with a retained range of motion and advise against MOM articulations in all patients.
Patients who are demonstrating potential signs of MOMD should be investigated by thorough history and examination, as well as radiographic and hematologic investigations. Plain radiographs and CT imaging (assessing for component malposition and osteolysis or debris) should be followed by metal artifact reduction MRI to judge the presence of effusion, pseudotumors, and other soft tissue reactions. Serum erythrocyte sedimentation rate, C-reactive protein, and metal ions (cobalt and chromium) should be measured and compared against norms. The decision to explant the prosthesis should be based on the complete clinical picture, and not a single result. Asymptomatic patients with MOM articulations should be routinely reviewed clinically, radiographically, and hematologically.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects performed by any of the authors.
Statement of Informed Consent: Informed patient consent was obtained prior to the completion of this case report.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Christopher J. Rothe  https://orcid.org/0000-0002-8768-3179
https://orcid.org/0000-0002-8768-3179
Brahman S. Sivakumar  https://orcid.org/0000-0003-0890-2132
https://orcid.org/0000-0003-0890-2132
David J. Graham  https://orcid.org/0000-0003-3421-822X
https://orcid.org/0000-0003-3421-822X
References
- 1. Cooper HJ, Urban RM, Wixson RL, et al. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am. 2013;95(10):865-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Heffernan E, Alkubaidan F, Nielsen T, et al. The imaging appearances of metallosis. Skeletal Radiol. 2007;37(1):59-62. doi: 10.1007/s00256-007-0362-y. [DOI] [PubMed] [Google Scholar]
- 3. Giwa L, Siddiqui A, Packer G. Motec wrist arthroplasty: 4 years of promising results. J Hand Surg Asian Pac Vol. 2018;23(3):364-368. [DOI] [PubMed] [Google Scholar]
- 4. Day CS, Lee AH, Ahmed I. Acute carpal tunnel secondary to metallosis after total wrist arthroplasty. J Hand Surg Eur Vol. 2013;38(1):80-81. [DOI] [PubMed] [Google Scholar]
- 5. Taha R, Roushdi I, Williams C. Pseudotumour secondary to metallosis following total wrist arthroplasty. J Hand Surg Eur Vol. 2015;40(9):995-996. [DOI] [PubMed] [Google Scholar]
- 6. Heyes GJ, Julian HS, Mawhinney I. Metallosis and carpal tunnel syndrome following total wrist arthroplasty. J Hand Surg Eur Vol. 2018;43(4):448-450. [DOI] [PubMed] [Google Scholar]
- 7. Karjalainen T, Pamilo K, Reito A. Implant failure after Motec wrist joint prosthesis due to failure of ball and socket-type articulation—two patients with adverse reaction to metal debris and polyether ether KETONE. J Hand Surg Am. 2018;43(11):1044.e1-1044.e4. doi: 10.1016/j.jhsa.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 8. Duggan P, Burke C, Saha S, et al. Current literature and imaging techniques of aseptic lymphocyte-dominated vasculitis-associated lesions (ALVAL). Clin Radiol. 2013;68(11):1089-1096. doi: 10.1016/j.crad.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 9. Fritz J, Lurie B, Miller T, et al. MR imaging of hip arthroplasty implants. Radiographics. 2014;34(4):E106-E132. doi: 10.1148/rg.344140010. [DOI] [PubMed] [Google Scholar]
- 10. Talbot B, Weinberg E. MR imaging with metal-suppression sequences for evaluation of total joint arthroplasty. Radiographics. 2016;36(1):209-225. doi: 10.1148/rg.2016150075. [DOI] [PubMed] [Google Scholar]