Abstract
This study uses US national surveillance data to describe preimplantation genetic testing trends and outcomes between 2014 and 2018.
Preimplantation genetic testing (PGT) with in vitro fertilization (IVF) is commonly used to screen embryos for chromosome aneuploidy to prioritize embryos for transfer. However, the American Society for Reproductive Medicine states that there is “insufficient evidence to recommend routine use” of the technology1 because studies preferentially include patients with favorable prognoses and concerns exist regarding costs, risk of false-positive results, and embryo damage.2 In 2011-2012, PGT use was reported in 4.5% of all IVF cycles.3 Since then, there have been practice changes, including aneuploidy screening technology and a shift toward blastocyst-stage biopsy with delayed transfer of previously frozen embryos. We used US national surveillance data to describe PGT trends and outcomes between 2014 and 2018.
Methods
This study was reviewed and deemed exempt by the Emory University institutional review board. Data were obtained from the Society for Assisted Reproductive Technology Clinic Outcome Reporting System, estimated to include 90% of IVF cycles in the US. Cycles are entered by member clinics; data validation occurs annually for select clinics. Trends were explored using linear regression to model the number or percentage of cycles using PGT in each year against time.
Given that most transfers using PGT-screened embryos use frozen embryos, we linked originating oocyte retrievals to subsequent frozen transfers to determine cumulative live birth rate (LBR), defined as the rate of achieving 1 live birth after all fresh and frozen embryo transfers within a year of retrieval. To reduce selection bias, we used oocyte retrievals as the denominator instead of embryo transfers. We explored the association between PGT use and cumulative LBR using Mantel-Haenszel χ2 tests. This analysis was stratified by age and oocyte yield because aneuploidy rates increase with age and directly affect LBR and the decision to perform PGT is often influenced by ovarian response. Analyses were conducted using SAS On-Demand for Academics (SAS Institute Inc). Statistical significance was defined as 2-sided P < .05.
Results
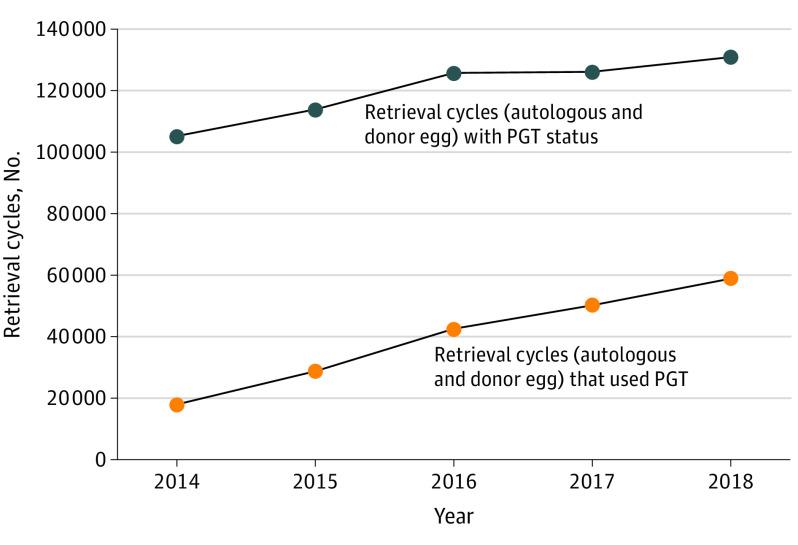
A total of 115 147 IVF cycles (16.1%) with missing PGT status were excluded from analysis; of these, 57 700 (8.0%) were canceled or yielded no embryos. The absolute number of oocyte retrieval cycles that used PGT increased from 18 059 in 2014 to 58 827 in 2018 (P < .001) (Figure 1), accounting for 17.2% of cycles in 2014 and 44.9% in 2018 (P < .001). In all years combined, PGT was used in 27.0% of autologous oocyte retrieval cycles in women younger than 35 years, 36.5% in women aged 35 to 37 years, 41.3% in women aged 38 to 40 years, 39.7% in women aged 41 to 42 years, and 29.0% in women aged 43 years or older. It was used in 28.6% of cycles using fresh donor oocytes fertilized at the time of retrieval.
Figure 1. Trends in Absolute Number of In Vitro Fertilization Retrieval Cycles and Cycles Using Preimplantation Genetic Testing (PGT), 2014-2018.
In women younger than 35 years, the cumulative LBR was 52.9% with PGT and 54.9% without PGT (P < .001). In older women, cumulative LBRs were higher in cycles that used PGT compared with cycles that did not use PGT (35-37 years: 44.0% vs 40.6%; 38-40 years: 31.4% vs 24.4%; 41-42 years: 18.1% vs 11.4%) (Figure 2A). Cumulative LBRs were significantly lower in cycles that used PGT than those that did not among women younger than 35 years, regardless of number of oocytes retrieved, but did not significantly differ by use of PGT among older women (Figure 2B).
Figure 2. Cumulative Live Birth Rates per Oocyte Retrieval With and Without Use of Preimplantation Genetic Testing (PGT).

A, The numbers of live births/oocyte retrievals were as follows: age <35 years: without PGT, 71 514 live births/130 285 retrievals; with PGT, 21 618/40 863; age 35-37 years: without PGT, 24 992/61 595; with PGT, 13 051/29 647; age 38-40 years: without PGT, 13 058/53 465; with PGT, 10 151/32 329; age 42-42 years: without PGT, 3117/27 421; with PGT, 2920/16 160; age >43 years: without PGT, 804/24 202; with PGT: 676/8957. B, The numbers of live births/oocyte retrievals were as follows for <10 oocytes: age <35 years: without PGT: 14 612/38 768; with PGT: 2719/7653; age 35-37 years: without PGT: 8093/28 891; with PGT: 2521/8678; age 38-40 years: without PGT: 5410/32 421; with PGT: 2499/12 471; age 41-42 years: without PGT: 1529/19 549; with PGT: 835/7302; age ≥43 years: without PGT, 394/19 641; with PGT: 226/4848. The numbers of live births/oocyte retrievals were as follows for 10-20 oocytes: age <35 years: without PGT, 36 897/62 214; with PGT, 10 483/19 913; age 35-37 years: without PGT, 12 326/25 094; with PGT: 6618/14 371; age 38-40 years: without PGT, 5968/17 365; with PGT, 5211/14 782; age 41-42 years: without PGT, 1310/6842; with PGT, 1413/6784; age ≥43 years: without PGT, 314/3977; with PGT, 307/3236. The numbers of live births/oocyte retrievals were as follows for >20 oocytes: age <35 years: without PGT, 20 005/29 303; with PGT, 8416/13 297; age 35-37 years: without PGT, 4573/7610; with PGT, 3912/6598; age 38-40 years: without PGT, 1680/3679; with PGT, 2441/5076; age 41-42 years: without PGT: 278/1030; with PGT, 672/2074; age ≥43 years: without PGT, 96/584; with PGT: 143/873.
aP < .001.
bP = .001 to P < .05.
cP ≥ .05.
Discussion
From 2014 to 2018, PGT use increased significantly in the absolute number and percentage of retrieval cycles, accounting for nearly half of all cycles in 2018. These trends could reflect increasing use of IVF among older women4 at higher risk of aneuploidy or reports of higher LBRs in PGT cycles per transfer in patients with good prognosis.1,5
The high use of PGT in young women is inconsistent with their relatively low rates of aneuploidy. In addition, the cumulative LBR was lower for women younger than 35 years who used PGT vs those who did not. Data from a 2019 study6 showed no improvements in cumulative LBRs for women younger than 35 years. PGT was used relatively more often for women older than 35 years and in IVF cycles with higher numbers of oocytes retrieved, and the LBRs were higher for those who used PGT than for those who did not; aneuploidy screening may be more helpful among older women with high risk of aneuploidy.
Study limitations include potential data entry errors and missing PGT status data. However, surveillance data are validated annually. Given the broad use of PGT, further examination of its utility and risks among specific patient populations is warranted.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Associate Editor.
References
- 1.Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology; Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology . The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109(3):429-436. doi: 10.1016/j.fertnstert.2018.01.002 [DOI] [PubMed] [Google Scholar]
- 2.Paulson RJ. Hidden in plain sight: the overstated benefits and underestimated losses of potential implantations associated with advertised PGT-A success rates. Hum Reprod. 2020;35(3):490-493. doi: 10.1093/humrep/dez280 [DOI] [PubMed] [Google Scholar]
- 3.Chang J, Boulet SL, Jeng G, Flowers L, Kissin DM. Outcomes of in vitro fertilization with preimplantation genetic diagnosis: an analysis of the United States Assisted Reproductive Technology Surveillance Data, 2011-2012. Fertil Steril. 2016;105(2):394-400. doi: 10.1016/j.fertnstert.2015.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hipp H, Crawford S, Kawwass JF, et al. National trends and outcomes of autologous in vitro fertilization cycles among women ages 40 years and older. J Assist Reprod Genet. 2017;34(7):885-894. doi: 10.1007/s10815-017-0926-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scott RT Jr, Upham KM, Forman EJ, et al. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril. 2013;100(3):697-703. doi: 10.1016/j.fertnstert.2013.04.035 [DOI] [PubMed] [Google Scholar]
- 6.Munné S, Kaplan B, Frattarelli JL, et al. ; STAR Study Group . Preimplantation genetic testing for aneuploidy versus morphology as selection criteria for single frozen-thawed embryo transfer in good-prognosis patients: a multicenter randomized clinical trial. Fertil Steril. 2019;112(6):1071-1079.e7. doi: 10.1016/j.fertnstert.2019.07.1346 [DOI] [PubMed] [Google Scholar]