Abstract
Background
Traditional fasting and no drinking schemes (fasting for 8–12 hours and no drinking for 4–6 hours) affect the metabolism of the body. The new guidelines put forward by the American Association of Anesthesiologists (fasting for 6 hours, no drinking for 2 hours) obviously reduce the time of fasting and no drinking, but the clinical efficacy and safety need to be further confirmed. In this study, a meta-analysis of randomized controlled trials (RCTs) using the new guidelines and traditional protocols was conducted to provide an evidence-based foundation for elective surgery.
Methods
The articles were searched in PubMed, EBSCO, MEDLINE, Science Direct, Cochrane Library, CNKI, China Biomedical Resources Database, Wanfang Database, Weipu, and Western Biomedical Journal Literature Database. RCTs related to fasting before surgery during the screening period were selected. Chinese and English search keywords included elective surgery, preoperative, fasting and no drinking, patient comfort, thirst, hunger, collapse, hypoglycemia, preoperative gastric volume, preoperative gastric juice pH, and intraoperative gastric volume. The RevMan 5.3 software provided by Cochrane collaboration network was used to evaluate the quality of included documents. Two professionals independently screened the literature, extracted data, and assessed the risk of bias.
Results
A total of 6 studies were included. The incidence of hunger in patients undergoing elective surgery in the experimental group and control group was significantly different [Z=3.90; relative risk (RR) =0.58; 95% confidence interval (CI): 0.44, 0.76; P<0.0001]. The incidence of thirst was significantly different between the experimental group and control group (Z=7.22; RR =0.21; 95% CI: 0.13, 0.32; P<0.00001).
Discussion
Meta-analysis results confirmed that the new guidelines can significantly reduce the hunger and thirst of patients, improve their satisfaction after surgery, and can be applied clinically.
Keywords: Elective surgery, new guidelines, no drinking and fasting, clinical effect, meta-analysis
Introduction
Fasting and drinking before elective surgery is to reduce the volume and acidity of stomach contents, prevent vomiting during anesthesia and aspiration pneumonia caused by aspiration of stomach contents, so long-term fasting and drinking before surgery is a routine clinical plan (1). For patients undergoing nerve block anesthesia, they are conscious after anesthesia. However, once nausea and vomiting are induced, there is a risk of aspiration. For patients under general anesthesia, the risk of aspiration increases. Therefore, it is necessary to implement fasting and drinking before operation (2,3).
At present, Chinese textbooks still hold the traditional view as to the time of water fasting: adult elective surgery patients should fast for 8–12 hours and should not drink 4 hours before surgery. However, it has been clinically discovered in recent years that preoperative fasting time >10 hours and no drinking time >6 hours can cause adverse reactions such as thirst, hunger, anxiety, dehydration, and hypoglycemia in patients (4-6). Therefore, the American Society of Anesthesiology (ASA) and Enhanced Recovery After Surgery (ERAS) revised the preoperative fasting guidelines in 1999 and 2012, respectively, to shorten the preoperative fasting and no drinking time (7). The new index stipulates that patients undergoing elective surgery can consume sugar-free transparent liquids such as tea, water, and juice 2 hours before surgery. Patients can also eat easily digestible foods such as milk and bread 6 hours before surgery, and can eat normally 8 hours before surgery (8-10). Anesthesiologists’ associations in many countries recommend that patients who undergo elective/limited operation can take appropriate amount of clear fluid orally 2 hours before operation. Some medical units in China also try to put this fasting scheme into practice, but the current situation of clinical application lacks evidence-based basis.
Systematic evaluation and meta-analysis are the most commonly used research methods in evidence-based medicine and are the best source of scientific evidence (11). Meta-analysis is a statistical method that combines multiple similar studies with different results from a systematic review into a quantitative indicator (12-14). A systematic review is a comprehensive collection of all relevant studies worldwide, with strict evaluation of all included studies one by one, combined analysis and evaluation of all research results, and meta-analysis when necessary. This is performed to draw a comprehensive conclusion and approach the real scientific evidence, while minimizing bias as much as possible (15-18).
The innovation of this study lies in the meta-analysis of RCTs by Cochrane systematic evaluation method through comprehensive retrieval of related studies, aiming to prove that the new guideline scheme can reduce the hunger and thirst of patients, shorten the clinical effect and safety of fasting time in clinical work, and provide sufficient evidence for clinical practice. We present the following article in accordance with the PRISMA reporting checklist (available at https://gs.amegroups.com/article/view/10.21037/gs-22-49/rc).
Methods
Article retrieval
Articles were searched in PubMed, EBSCO, MEDLINE, Science Direct, Cochrane Library, CNKI, China Biomedical Resources Database, Wanfang Database, Weipu, and Western Biomedical Journal articles database. The articles were RCTs related to fasting and no drinking before elective surgery published from the establishment of the database to May 22, 2021. Journals were manually searched to avoid omissions.
The search terms for English databases were “elective surgery”, “preoperative”, “fasting and water deprivation”, and “patients are comfortable”. The Chinese search keywords included “elective surgery”, “preoperative”, “fasting and no drinking”, and “patient comfort”.
The search terms on observation indicators for English databases were as follows: thirst, hunger, collapse, hypoglycemia, preoperative gastric volume, preoperative gastric juice pH, and intraoperative gastric volume. The Chinese search keywords were as follows: thirst, hunger, collapse, hypoglycemia, preoperative gastric volume, preoperative gastric fluid pH, postoperative insulin resistance, and intraoperative gastric volume.
Search terms and observation index search terms were freely combined to conduct multiple searches and to include more relevant reference articles. Then, search engines were adopted to track each article. Finally, the relevant researchers who published the articles were contacted to obtain the latest research progress.
Inclusion and exclusion criteria of the included articles
The inclusion criteria of the articles were as follows: articles which were prospective RCTs, limited to Chinese and English only; articles in which the subjects were patients undergoing elective surgery, and the anesthesia method was general anesthesia; articles in which the intervention measures of the experimental group were preoperative fasting for 6–12 hours and no drinking for 2–3 hours, and articles in which the intervention measures of the control group were traditional fasting for 8–12 hours and no drinking for more than 4 hours; and articles whose outcome indicators included more than one of the following items: thirst, hunger, collapse, hypoglycemia, preoperative gastric volume, preoperative gastric pH, postoperative insulin resistance, and intraoperative gastric volume. The fasting interventions given to the experimental group and the control group were the same, and the key difference between the two was the length of fasting time.
Articles meeting the following criteria were excluded: articles which were non-prospective RCTs; articles which were case reports, reviews, conference abstracts, and other non-research articles; articles with children as the research subjects; articles in which the research subjects underwent non-general anesthesia; and articles whose author could not be contacted for the latest data.
Clinical outcome indicators
The clinical outcome indicators included thirst, hunger, collapse, hypoglycemia, preoperative gastric volume, preoperative gastric pH, intraoperative gastric volume, and postoperative insulin resistance.
Data extraction
Two professionals were required to use a unified Microsoft Excel spreadsheet (Microsoft, USA) to independently filter articles and extract data, and then cross-checked them. If they encountered differences, it could be resolved through discussion. The main data extracted included: general information of the articles such as title, first author, country, published journal, and publication date; basic information of the research subjects such as gender, age, and sample size; specific operation and follow-up time of intervention measures; extraction of outcome indicators such as thirst, hunger, collapse, hypoglycemia, preoperative gastric volume, preoperative gastric juice pH, postoperative insulin resistance, and intraoperative gastric volume.
Evaluation of the risk of bias
Two professionals strictly followed the five evaluation criteria of RCTs to repeatedly evaluate the risk of bias of the articles included in the study. If there were any differences, it was resolved through discussion. The evaluation criteria included whether the randomization method was correct; whether allocation concealment was strictly implemented; whether the blinding method was used; whether there was loss to follow-up; whether the number of cases and the age situation were comparable; and whether selection bias could have occurred. The two professionals evaluated the quality of the included articles with reference to the Jadad rating scale (0–5 points).
Sensitivity analysis
The impact of each study on the total combined effect size was evaluated, and the more influential studies were excluded. The random effects model (REM) and fixed effects model (FEM) were used to compare the results. According to the consistency of the results, the reliability of the combined results was analyzed and a funnel plot was used to determine whether there was publication bias.
Statistical analysis
The risk of bias evaluation chart of RevMan 5.3 software was used to evaluate the risk of bias of the included articles, and the data was sorted, filtered, and then input into the software to draw the chart. Enumeration data were measured using relative risk (RR) and its 95% confidence interval (CI), while the efficacy analysis statistics of measurement data were mean difference (MD) and its 95% CI. The heterogeneity among the articles was explored using the I2 test. When P>0.01 and I2<50%, it indicated that the heterogeneity of the included articles was small, and the FEM was used for meta-analysis. When P<0.01 and I2>50%, it indicated that the included articles showed obvious heterogeneity, and the REM was used for meta-analysis.
Results
Search results and basic information of the included articles
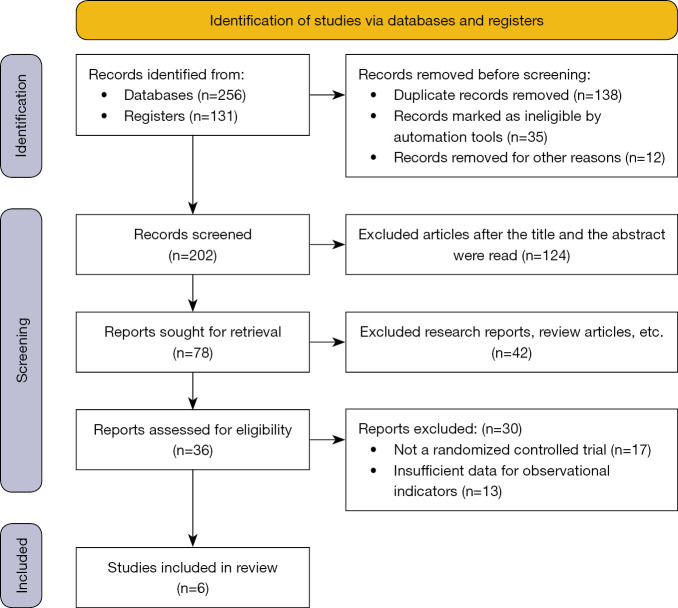
A total of 256 articles were obtained by searching the databases, 131 articles were obtained by hand-searching journals, 138 articles that were republished were eliminated, 35 articles were not qualified, and 12 articles were eliminated for other reasons. The remaining 202 articles were selected by their titles. After the abstract and title were read, 124 articles were removed, leaving 78 articles. There were 42 research reports and reviews, and 36 papers remained. After the full text was read, 17 non-RCTs were excluded, and the relevant information of the research could not be further extracted. Thirteen articles were excluded, and 6 articles were finally included in the meta-analysis (19-24). Figure 1 shows the flow chart of article retrieval.
Figure 1.
Flow chart of article retrieval.
There were 6 articles that met the inclusion criteria, including 490 patients. Among the 6 articles, the sample size ranged from 10 to 274. The 6 articles described in detail thirst, hunger, collapse, hypoglycemia, preoperative gastric volume, preoperative gastric fluid pH, postoperative insulin resistance, and intraoperative gastric volume. Table 1 shows the basic characteristics of the included articles.
Table 1. Basic characteristics and scale scores of the included articles.
| First author | Year of publication | Number of cases (n) | Experimental group (n) | Control group (n) | Intervention (experimental group vs. control group) | Outcome indicators |
|---|---|---|---|---|---|---|
| Dock-Nascimento (19) | 2012 | 24 | 12 | 12 | Fasting for 8 hours, oral carbohydrate 200 mL 2 hours before surgery vs. fasting and drinking for 8 hours | Postoperative insulin resistance |
| Faria (20) | 2009 | 21 | 11 | 10 | Fasting for 8 hours, oral carbohydrate 200 mL 2 hours before surgery vs. fasting and drinking for 8 hours | Postoperative insulin resistance |
| Itou (21) | 2012 | 274 | 135 | 139 | Fasting for 12 hours, oral carbohydrate 500 mL 2 hours before surgery vs. fasting and drinking for 12 hours | Hunger, thirst, anxiety, nausea, vomiting, gastric fluid volume, gastric fluid pH |
| Järvelä (22) | 2008 | 101 | 50 | 51 | Fasting for 12 hours, oral carbohydrate 400 mL 2 hours before surgery vs. fasting and drinking for 12 hours | Nausea, vomiting |
| Singh (23) | 2015 | 10 | 5 | 5 | Fasting for 8 hours, oral carbohydrate 200 mL 2 hours before surgery vs. fasting and drinking for 8 hours | Postoperative insulin resistance |
| Yildiz (24) | 2013 | 60 | 30 | 30 | Fasting for 8 hours, oral carbohydrate 200 mL 2–3 hours before surgery vs. fasting and drinking for 8 hours | Weakness, thirst, fasting, malaise, fatigue, nausea, concentration difficulty, gastric volume, gastric fluid pH |
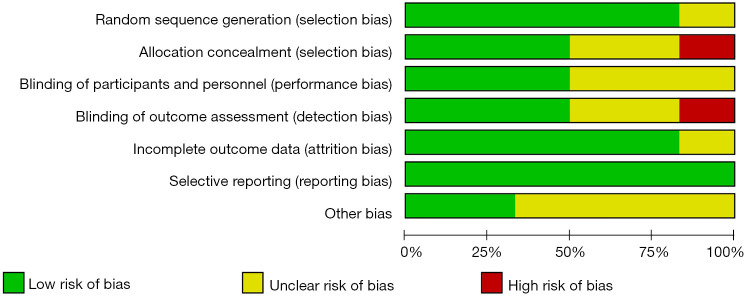
Risk of bias evaluation results of the included articles
Figure 2 shows the risk of bias evaluation results of the included articles drawn by RevMan 5.3 software. Figure 3 is a summary diagram of the bias risk of the articles. Among the 6 RCTs in this study, 3 RCTs (20,21,24) described allocation concealment in detail, 5 articles (19,20,22-24) described the random allocation method, and 3 articles (19,20,23) use blinding.
Figure 2.
Risk of bias evaluation results of the included articles.
Figure 3.
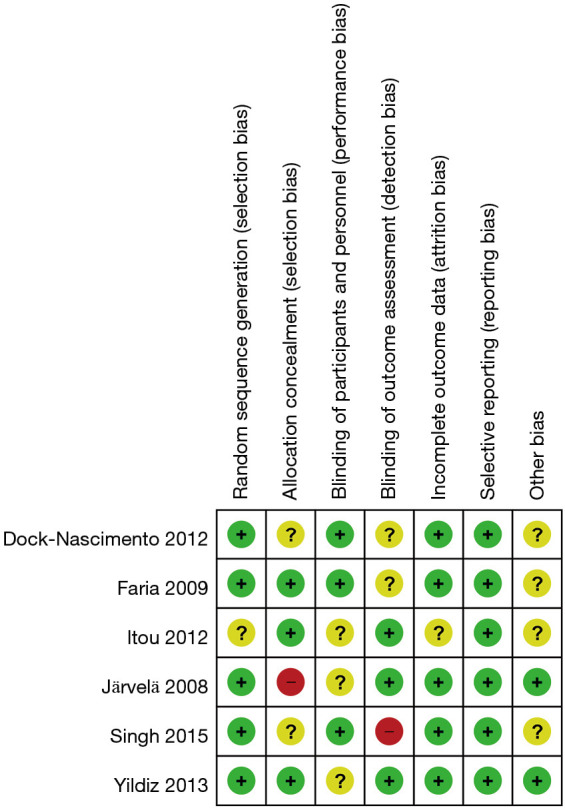
Summary of the risk of bias evaluation of the articles. “+”: low risk; “-”: high risk; “?”: unclear.
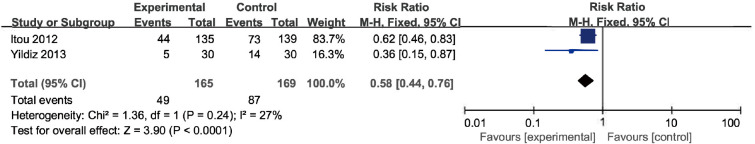
The effects of the two schemes on the incidence of hunger in elective surgery patients
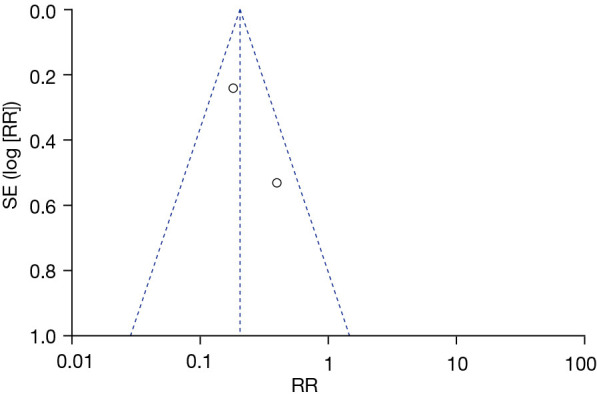
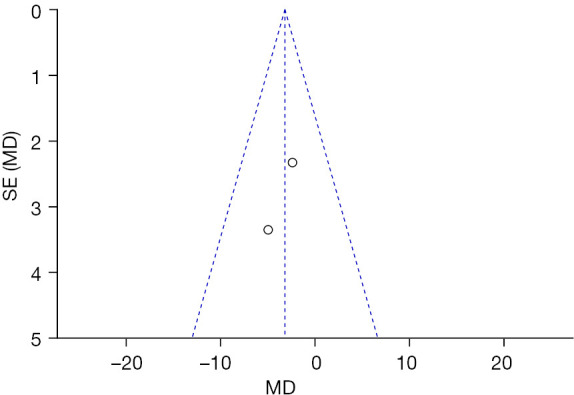
A total of 2 articles (21,24) analyzed the effects of the two programs on the incidence of hunger in elective surgery patients and their RR. Figure 4 is a forest plot of the effect of the two schemes on the incidence of hunger in elective surgery patients using the REM. The 2 articles used binary variables to describe hunger incidence in elective surgery patients. The overall heterogeneity test was performed, and the results revealed chi-square (Chi2) =1.36, degree of freedom (df) =1, and I2=27%<50%, so there was no heterogeneity among the articles. The horizontal line of the 95% CI of all articles was to the left of the invalid vertical line. The analysis results using FEM suggested that the experimental group was significantly different compared with the control group (Z=3.90; RR =0.58; 95% CI: 0.44, 0.76; P<0.0001). Figure 5 is a funnel plot of the incidence of hunger in elective surgery patients with the two schemes. The circles of the included articles were concentrated near the midline and were basically symmetrical, indicating that the accuracy of the included articles was relatively high and there was no obvious publication bias. These findings showed that elective surgery patients receiving the fasting and no drinking scheme based on the new protocol guidelines have a significantly reduced incidence of hunger.
Figure 4.
Forest plot of FEM analysis results for the incidence of hunger in elective surgery patients. CI, confidence interval; Chi2, chi-square; df, degree of freedom; FEM, fixed effects model.
Figure 5.
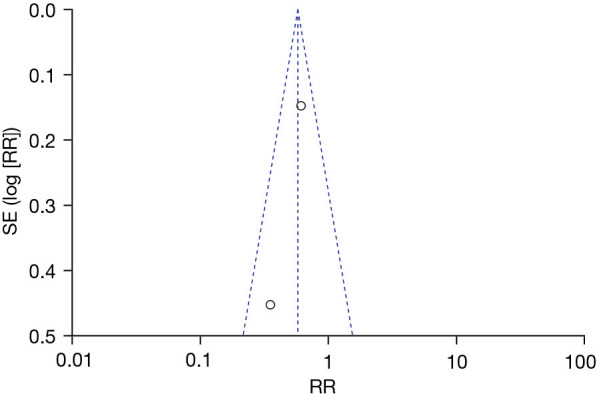
Funnel plot of the incidence of hunger in elective surgery patients. SE, standard error; RR, relative risk.
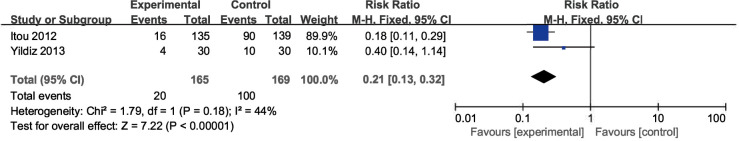
The effects of the two schemes on the incidence of thirst in elective surgery patients
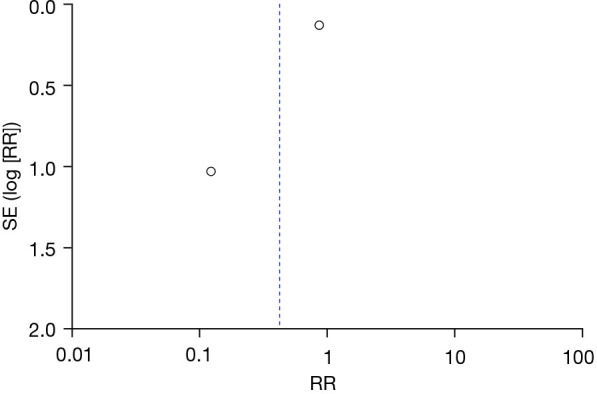
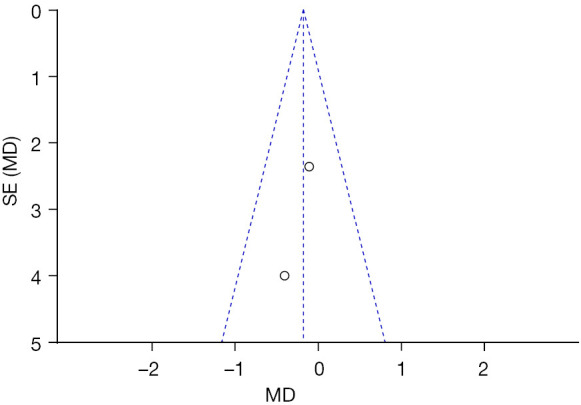
A total of 2 articles (21,24) analyzed the incidence and RR of thirst in elective surgery patients. Figure 6 is a forest plot of the FEM analysis results on thirst incidence in elective surgery patients. The 2 articles used binary variables to describe the incidence of thirst in elective surgery patients. There were 334 cases in total, including 165 cases in the experimental group and 169 cases in the control group. The overall heterogeneity test was performed, and it was found that Chi2=1.79, df=1, I2=44%<50%, and P=0.18, so there was no heterogeneity in the articles. The FEM analysis results suggested that the experimental group was significantly different compared with the control group (Z=7.22; RR =0.21; 95% CI: 0.13, 0.32; P<0.00001). Figure 7 is a funnel plot of the incidence of thirst in elective surgery patients. It can be concluded that the circles are near the midline, and therefore there was no publication bias. These findings showed that elective surgery patients receiving the fasting and no drinking scheme based on the new protocol guidelines have a significantly reduced incidence of thirst.
Figure 6.
Forest plot of FEM analysis results of the incidence of thirst in elective surgery patients. CI, confidence interval; Chi2, chi-square; df, degree of freedom; FEM, fixed effects model.
Figure 7.
Funnel plot of the incidence of thirst in elective surgery patients. SE, standard error; RR, relative risk.
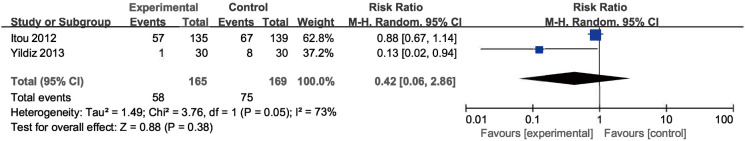
The effects of the two schemes on the anxiety of elective surgery patients
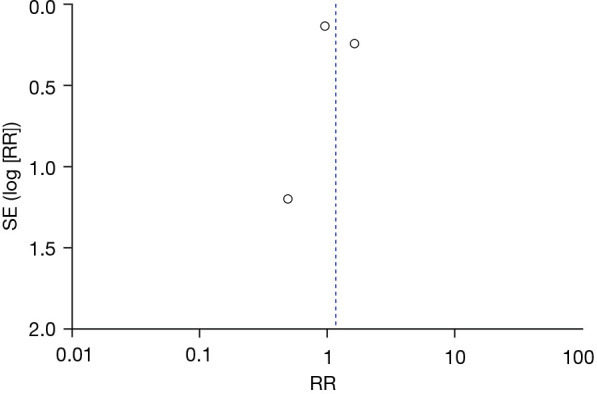
A total of 2 articles (21,24) analyzed the incidence and RR of anxiety in elective surgery patients. Figure 8 is a forest plot of the FEM analysis results on the degree of anxiety in elective surgery patients. The 2 articles used binary variables to describe the degree of anxiety in elective surgery patients. There were 334 cases in total, including 165 cases in the experimental group and 169 cases in the control group. The overall heterogeneity test was performed, and it was found that Chi2=3.76, df=1, I2=73%>50%, and P=0.05, so there was heterogeneity in the articles. The FEM analysis results suggested that the experimental group was not significantly different compared with the control group (Z=0.88; RR =0.42; 95% CI: 0.06, 2.86; P=0.38). Figure 9 is a funnel plot of the degree of anxiety in elective surgery patients. It can be seen that the circles are near the midline and basically symmetrical, indicating that there was no publication bias. These findings showed that elective surgery patients receiving the fasting and no drinking scheme based on the new protocol guidelines have significantly reduced anxiety.
Figure 8.
Forest plot of REM analysis results on anxiety in elective surgery patients. CI, confidence interval; Chi2, chi-square; df, degree of freedom; REM, random effects model.
Figure 9.
Funnel plot of anxiety in elective surgery patients. SE, standard error; RR, relative risk.
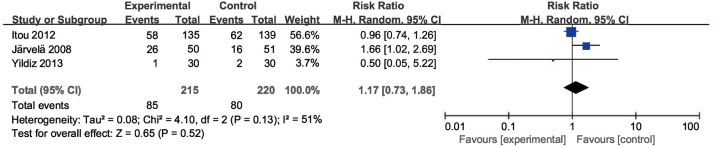
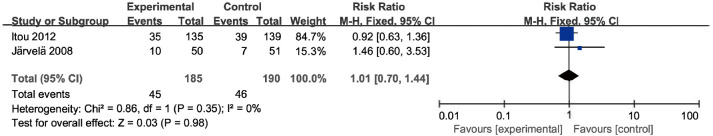
The effects of the two schemes on the incidence of nausea and vomiting in elective surgery patients
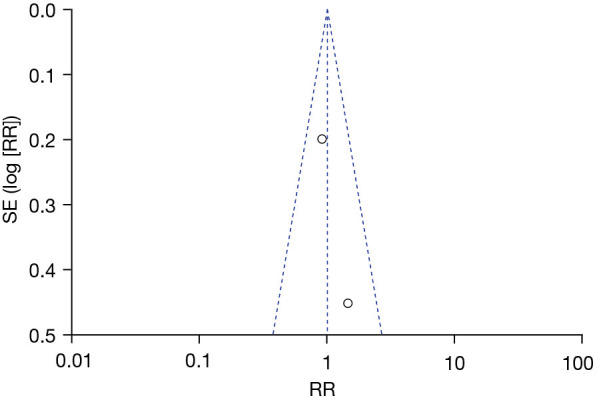
A total of 3 articles (21,22,24) analyzed the incidence of nausea and vomiting in elective surgery patients. Figures 10,11 are forest plots of the FEM analysis results for the incidence of nausea and vomiting, respectively. The 3 articles used binary variables to describe the incidence of nausea and vomiting in elective surgery patients. There were 435 cases in total, including 215 cases in the experimental group and 220 cases in the control group. The overall heterogeneity test was performed, and it was found that Chi2=4.10, df=2, I2=51%>50%, and P=0.13 for nausea; and Chi2=0.86, df=1, I2=0%<50%, and P=0.35 for vomiting, so there was no heterogeneity among the articles. The FEM analysis results showed that the difference between the experimental group and the control group was not statistically significant (nausea: Z=0.65, RR =1.17, 95% CI: 0.73, 1.86, P=0.52; vomiting: Z=0.03, RR =1.01, 95% CI: 0.70, 1.44, P=0.98). Figures 12,13 show the funnel plots of nausea and vomiting, respectively. It can be seen that the circles are concentrated near the midline and are roughly symmetrical, indicating that there was no publication bias. These findings showed that elective surgery patients receiving the fasting and no drinking scheme based on the new protocol guidelines do not have a reduced incidence of nausea and vomiting.
Figure 10.
The forest plot of the REM analysis results for the incidence of nausea. CI, confidence interval; Chi2, chi-square; df, degree of freedom; REM, random effects model.
Figure 11.
The forest plot of the FEM analysis results for the incidence of vomiting. CI, confidence interval; Chi2, chi-square; df, degree of freedom; FEM, fixed effects model.
Figure 12.
The funnel plot of nausea. SE, standard error; RR, relative risk.
Figure 13.
The funnel plot of vomiting. SE, standard error; RR, relative risk.
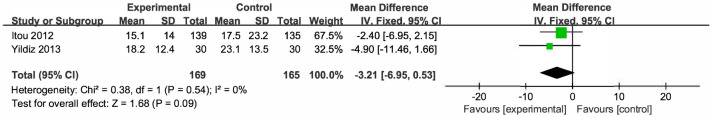
The effects of the two schemes on the amount of gastric contents in elective surgery patients
A total of 2 articles (21,24) analyzed the amount of gastric contents in elective surgery patients. Figure 14 is a forest plot of the FEM analysis results of gastric contents in elective surgery patients. The 2 articles used continuous variables to describe the gastric contents of elective surgery patients. There were 334 cases in total, including 169 cases in the experimental group and 165 cases in the control group. The overall heterogeneity test showed Chi2=0.38, df=1, I2=0%<50%, and P=0.54, so there was no heterogeneity among the included articles. The FEM analysis results illustrated that the difference between the experimental group and the control group was not statistically significant (Z=1.68; MD =−3.21; 95% CI: −6.95, 0.53; P=0.09). Figure 15 is a funnel plot of the amount of gastric contents of elective surgery patients. It can be concluded that the circles are near the midline and are roughly symmetrical, indicating that there was no publication bias. These findings showed that elective surgery patients receiving the fasting and no drinking scheme based on the new protocol guidelines do not have an increased amount of gastric contents.
Figure 14.
The forest plot of the FEM analysis results of gastric contents in elective surgery patients. SD, standard deviation; CI, confidence interval; Chi2, chi-square; df, degree of freedom; FEM, fixed effects model.
Figure 15.
The funnel plot of gastric contents in elective surgery patients. SE, standard error; MD, mean difference.
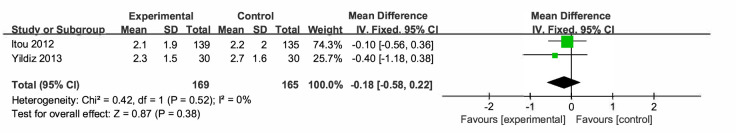
The effects of the two schemes on the gastric pH of elective surgery patients
A total of 2 articles (21,24) analyzed the gastric pH value in elective surgery patients. Figure 16 is a forest plot of the FEM analysis results of the gastric pH of elective surgery patients. The 2 articles used continuous variables to describe the gastric pH values of elective surgery patients. There were a total of 334 cases, including 169 cases in the experimental group and 165 cases in the control group. The overall heterogeneity test showed Chi2=0.42, df=1, I2=0%<50%, and P=0.52, so there was no heterogeneity among the articles. The FEM analysis results proved that the difference between the two groups was not statistically significant (Z=0.87; MD =−0.18; 95% CI: −0.58, 0.22; P=0.38). Figure 17 is a funnel plot of gastric pH in elective surgery patients. It can be concluded that the circles are near the midline and are roughly symmetrical, indicating that there was no publication bias. These findings indicate that the fasting and no drinking scheme based on the new protocol guidelines would not affect the gastric pH values of patients undergoing elective surgery.
Figure 16.
The forest plot of FEM analysis results of gastric pH values of elective surgery patients. SD, standard deviation; CI, confidence interval; Chi2, chi-square; df, degree of freedom; FEM, fixed effects model.
Figure 17.
The funnel plot of the gastric pH values of elective surgery patients. SE, standard error; MD, mean difference.
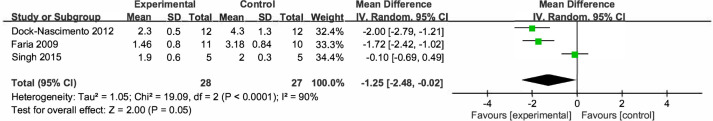
The effects of the two schemes on postoperative insulin resistance in elective surgery patients
A total of 3 articles (19,20,23) analyzed postoperative insulin resistance in elective surgery patients. Figure 18 is a forest plot of the REM analysis results of postoperative insulin resistance in elective surgery patients. The 3 articles used continuous variables to describe the postoperative insulin resistance of elective surgery patients. There were a total of 55 cases, including 28 cases in the experimental group and 27 cases in the control group. The overall heterogeneity test showed Chi2=19.09, df=2, I2=90%>50%, and P<0.0001, so there was heterogeneity among the articles. The REM analysis results proved that the difference between the two groups was not statistically significant (Z=2.00; MD =−1.25; 95% CI: −2.48, −0.02; P=0.05). Figure 19 is a funnel plot of the postoperative insulin resistance of elective surgery patients. It can be concluded that the circles are near the midline and are roughly symmetrical, so there was no publication bias. These findings demonstrate that the fasting and no drinking scheme based on the new protocol guidelines would not affect the postoperative insulin resistance of patients undergoing elective surgery.
Figure 18.
The forest plot of REM analysis results of postoperative insulin resistance of elective surgery patients. SD, standard deviation; CI, confidence interval; Chi2, chi-square; df, degree of freedom; REM, random effects model.
Figure 19.
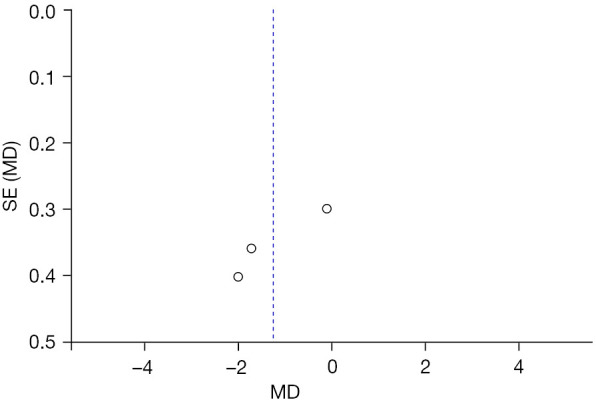
The funnel plot of the postoperative insulin resistance of elective surgery patients. SE, standard error; MD, mean difference.
Discussion
The purpose of conventional no drinking and fasting before elective surgery is to fully empty the stomach to prevent aspiration pneumonia caused by aspiration of stomach contents during anesthesia. The traditional no drinking and fasting program is long, and patients are prone to adverse complications (25). Most national associations of anesthesiologists recommend that patients undergoing elective surgery can consume clear liquid food 2 hours before surgery. A number of RCTs worldwide have confirmed the effectiveness and safety of the fasting and no drinking regimen, but there is a lack of scientific evidence to support its application (26).
Eight RCTs were included in this study, of which 4 RCTs described allocation concealment in detail, 3 described the random allocation method, and 1 article did not use blinding. The traditional no drinking and fasting program reduces the gastric contents of patients and reduces the risk of intraoperative anesthesia (27). However, fasting from food and water for too long before surgery will produce a series of adverse reactions that affect the safety and effectiveness of the surgery (the most common occurrences are hunger, thirst, abnormal metabolic function, and digestive tract reactions). It can also increase the chance of reflux after anesthesia, which not only reduces the comfort of the patient during the perioperative period, but can even lead to the postponement or cancellation of the operation (28). The ASA and ERAS revised the preoperative fasting guidelines to shorten the preoperative fasting and no drinking time. The meta-analysis results showed that compared with the traditional fasting and no drinking regimen, the new guidelines were beneficial to patients in improving hunger (Z=3.90; RR =0.58; 95% CI: 0.44, 0.76; P<0.0001) and thirst (Z=7.22; RR =0.21; 95% CI: 0.13, 0.32; P<0.00001). The survey data showed that patients had a longer preoperative fasting and no drinking time, which was longer in clinical practice than in the guidelines, directly relating to the operation implementation and postoperative recovery of patients. Prolonged fasting and no drinking can cause thirst and hunger, and sympathetic nervous system excitement caused by hunger can cause irritability and anxiety in patients. Such results were similar to the research results of Napolitano et al. [2021] (29). In addition, shortening the time of elective surgery fasting and no drinking will not increase the gastric contents and the pH value of gastric juices of patients, and will not increase the risk of aspiration. Therefore, compared with the traditional preoperative fasting and no drinking regimen which is too long, shortening the fasting and no drinking time of elective surgery patients will not affect the safety of the surgery, and can improve the satisfaction and comfort of patients and their families during the perioperative period. In addition, this scheme is safe and applicable in clinical treatment.
For patients, surgery, no matter how big or small, will cause a certain degree of trauma. Prolonged fasting and no drinking can lead to imbalances in the internal environment of patients, which mainly manifests as decreased insulin secretion and increased growth hormone and glucagon levels, leading to imbalances in the glucose metabolism of the body. In addition, patients develop insulin resistance after surgery. If fasting for a long time before surgery can easily aggravate postoperative insulin resistance, this can reduce the body’s anti-infection ability and interfere with tissue repair and incision healing.
The experimental group included in the articles in this study consumed different drinks (such as water, tea, fruit juice, and glucose) before the no drinking regimen, and there may be some clinical heterogeneity. However, the results of this study showed that it was feasible to shorten the preoperative fasting and no drinking time of elective surgery patients, which can greatly improve the satisfaction of patients, family members, and medical staff, and can be promoted and used in clinical practice.
Conclusions
Articles on elective surgery using the traditional fasting and no drinking guidelines and the new fasting and no drinking guidelines were screened for systematic review and meta-analysis. We aimed to explore the clinical effect and safety of the new fasting and no drinking program for elective surgery patients. Meta-analysis results confirmed that the new program can effectively reduce the hunger and thirst of patients, improve their satisfaction after surgery, and can be applied clinically. The shortcomings of this study were that there were few RCTs included, and the outcome indicators of the articles were not completely consistent. In future studies, the sample size should be expanded and unified indicators should be included for in-depth exploration. In short, preoperative fasting and no drinking is used for clinical medicine, general anesthesia, and medical care. In the future, multidisciplinary cooperation and exploration should be carried out to promote communication and collaboration in various fields. In-depth research should also be carried out on the determination of fasting and drinking time, and regular training on the new guidelines should be provided to medical staff. Furthermore, health education for patients and their families may help to promote the implementation of the fasting and no drinking regimen according to the new guidelines.
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://gs.amegroups.com/article/view/10.21037/gs-22-49/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://gs.amegroups.com/article/view/10.21037/gs-22-49/coif). The authors have no conflicts of interest to declare.
(English Language Editor: C. Betlazar-Maseh)
References
- 1.Cheng Z, Yang QQ, Zhu P, et al. Transesophageal Echocardiographic Measurements of the Superior Vena Cava for Predicting Fluid Responsiveness in Patients Undergoing Invasive Positive Pressure Ventilation. J Ultrasound Med 2019;38:1519-25. 10.1002/jum.14839 [DOI] [PubMed] [Google Scholar]
- 2.Agarwal A, Chari P, Singh H. Fluid deprivation before operation. The effect of a small drink. Anaesthesia 1989;44:632-4. 10.1111/j.1365-2044.1989.tb13581.x [DOI] [PubMed] [Google Scholar]
- 3.Brown CS, Albright J, Henke PK, et al. Modeling the elective vascular surgery recovery after coronavirus disease 2019: Implications for moving forward. J Vasc Surg 2021;73:1876-1880.e1. 10.1016/j.jvs.2020.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kruzik N. Benefits of preoperative education for adult elective surgery patients. AORN J 2009;90:381-7. 10.1016/j.aorn.2009.06.022 [DOI] [PubMed] [Google Scholar]
- 5.Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg 2013;37:259-84. 10.1007/s00268-012-1772-0 [DOI] [PubMed] [Google Scholar]
- 6.Khan RMA, Hajibandeh S, Hajibandeh S. Early elective versus delayed elective surgery in acute recurrent diverticulitis: A systematic review and meta-analysis. Int J Surg 2017;46:92-101. 10.1016/j.ijsu.2017.08.583 [DOI] [PubMed] [Google Scholar]
- 7.Henderson A, Henderson S. Provision of a surgeon's performance data for people considering elective surgery. Cochrane Database Syst Rev 2015;(2):CD006327. 10.1002/14651858.CD006327.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toh JWT, Phan K, Hitos K, et al. Association of Mechanical Bowel Preparation and Oral Antibiotics Before Elective Colorectal Surgery With Surgical Site Infection: A Network Meta-analysis. JAMA Netw Open 2018;1:e183226. 10.1001/jamanetworkopen.2018.3226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Habermann EB. Are Opioids Overprescribed Following Elective Surgery? Adv Surg 2018;52:247-56. 10.1016/j.yasu.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 10.Galyfos G, Sigala F, Bazigos G, et al. Weekend effect among patients undergoing elective vascular surgery. J Vasc Surg 2019;70:2038-45. 10.1016/j.jvs.2019.03.020 [DOI] [PubMed] [Google Scholar]
- 11.Turunen E, Miettinen M, Setälä L, et al. Elective Surgery Cancellations During the Time Between Scheduling and Operation. J Perianesth Nurs 2019;34:97-107. 10.1016/j.jopan.2017.09.014 [DOI] [PubMed] [Google Scholar]
- 12.Dias JD, Sauaia A, Achneck HE, et al. Thromboelastography-guided therapy improves patient blood management and certain clinical outcomes in elective cardiac and liver surgery and emergency resuscitation: A systematic review and analysis. J Thromb Haemost 2019;17:984-94. 10.1111/jth.14447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orange ST, Northgraves MJ, Marshall P, et al. Exercise prehabilitation in elective intra-cavity surgery: A role within the ERAS pathway? A narrative review. Int J Surg 2018;56:328-33. 10.1016/j.ijsu.2018.04.054 [DOI] [PubMed] [Google Scholar]
- 14.Alverdy JC, Hyman N, Gilbert J. Re-examining causes of surgical site infections following elective surgery in the era of asepsis. Lancet Infect Dis 2020;20:e38-43. 10.1016/S1473-3099(19)30756-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levy N, Selwyn DA, Lobo DN. Turning 'waiting lists' for elective surgery into 'preparation lists'. Br J Anaesth 2021;126:1-5. 10.1016/j.bja.2020.08.021 [DOI] [PubMed] [Google Scholar]
- 16.Biondi A, Santullo F, Fico V, et al. Long-term Outcomes of Elective Surgery for Diverticular Disease: A Call for Standardization. J Clin Gastroenterol 2016;50 Suppl 1:S77-9. 10.1097/MCG.0000000000000599 [DOI] [PubMed] [Google Scholar]
- 17.Carmichael H, Moore A, Steward L, et al. Disparities in Emergency Versus Elective Surgery: Comparing Measures of Neighborhood Social Vulnerability. J Surg Res 2020;256:397-403. 10.1016/j.jss.2020.07.002 [DOI] [PubMed] [Google Scholar]
- 18.Sparreboom CL, Lambrichts DPV, Menon AG, et al. Outcomes After Elective Colorectal Surgery by 2 Surgeons Versus 1 Surgeon in a Low-Volume Hospital. Surg Innov 2019;26:753-9. 10.1177/1553350619868109 [DOI] [PubMed] [Google Scholar]
- 19.Dock-Nascimento DB, de Aguilar-Nascimento JE, Magalhaes Faria MS, et al. Evaluation of the effects of a preoperative 2-hour fast with maltodextrine and glutamine on insulin resistance, acute-phase response, nitrogen balance, and serum glutathione after laparoscopic cholecystectomy: a controlled randomized trial. JPEN J Parenter Enteral Nutr 2012;36:43-52. 10.1177/0148607111422719 [DOI] [PubMed] [Google Scholar]
- 20.Faria MS, de Aguilar-Nascimento JE, Pimenta OS, et al. Preoperative fasting of 2 hours minimizes insulin resistance and organic response to trauma after video-cholecystectomy: a randomized, controlled, clinical trial. World J Surg 2009;33:1158-64. 10.1007/s00268-009-0010-x [DOI] [PubMed] [Google Scholar]
- 21.Itou K, Fukuyama T, Sasabuchi Y, et al. Safety and efficacy of oral rehydration therapy until 2 h before surgery: a multicenter randomized controlled trial. J Anesth 2012;26:20-7. 10.1007/s00540-011-1261-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Järvelä K, Maaranen P, Sisto T. Pre-operative oral carbohydrate treatment before coronary artery bypass surgery. Acta Anaesthesiol Scand 2008;52:793-7. 10.1111/j.1399-6576.2008.01660.x [DOI] [PubMed] [Google Scholar]
- 23.Singh M, Chaudhary M, Vashistha A, et al. Evaluation of effects of a preoperative 2-hour fast with glutamine and carbohydrate rich drink on insulin resistance in maxillofacial surgery. J Oral Biol Craniofac Res 2015;5:34-9. 10.1016/j.jobcr.2015.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yildiz H, Gunal SE, Yilmaz G, et al. Oral carbohydrate supplementation reduces preoperative discomfort in laparoscopic cholecystectomy. J Invest Surg 2013;26:89-95. 10.3109/08941939.2012.699998 [DOI] [PubMed] [Google Scholar]
- 25.Dwyer T, Henry PD, Cholvisudhi P, et al. Neurological Complications Related to Elective Orthopedic Surgery: Part 1: Common Shoulder and Elbow Procedures. Reg Anesth Pain Med 2015;40:431-42. 10.1097/AAP.0000000000000178 [DOI] [PubMed] [Google Scholar]
- 26.Noba L, Wakefield A. Are carbohydrate drinks more effective than preoperative fasting: A systematic review of randomised controlled trials. J Clin Nurs 2019;28:3096-116. 10.1111/jocn.14919 [DOI] [PubMed] [Google Scholar]
- 27.Feuerstein JD, Curran T, Alosilla M, et al. Mortality Is Rare Following Elective and Non-elective Surgery for Ulcerative Colitis, but Mild Postoperative Complications Are Common. Dig Dis Sci 2018;63:713-22. 10.1007/s10620-018-4922-x [DOI] [PubMed] [Google Scholar]
- 28.Ducey A, Nikoo S. Formats of responsibility: elective surgery in the era of evidence-based medicine. Sociol Health Illn 2018;40:494-507. 10.1111/1467-9566.12659 [DOI] [PubMed] [Google Scholar]
- 29.Napolitano MA, Sparks AD, Randall JA, et al. Elective surgery for diverticular disease in U.S. veterans: A VASQIP study of national trends and outcomes from 2004 to 2018. Am J Surg 2021;221:1042-9. 10.1016/j.amjsurg.2020.08.050 [DOI] [PubMed] [Google Scholar]