Abstract
Purpose:
To define the success rate of initial non-operative treatment for traumatic anterior shoulder instability in a defined US geographic population, describe factors that predict conversion to surgery after initial non-operative management, and describe the long-term outcomes of non-operative treatment following index traumatic anterior instability event.
Methods:
The Rochester Epidemiology Project database was utilized to identify patients –14 – 39 years of age treated for anterior shoulder instability between 1994 and 2016. Patient demographics, comorbidities, injury characteristics, and imaging were evaluated. Patients treated non-operatively for the first 6 months following index instability event were analyzed to determine long-term outcomes (recurrence rates, pain at last follow up, radiographic outcomes), success rate of continued non-operative treatment (no conversion to surgery), and factors associated with conversion to surgery (patient and injury characteristics). Survivorship free of surgery was reported with a Kaplan-Meier survival curve and Cox proportional hazard models were utilized to evaluate association of variables with conversion to surgery.
Results:
379 patients met criteria with an average follow-up of 10.2 years (range 0.53 to 25.00). Average age was 23.9, mean BMI was 26.2, and 100% of instability events were due to trauma. 79 shoulders (20.1%) ultimately failed initial non-operative treatment and progressed to surgery. At final follow-up, the rate of recurrent instability was 52.3% in the group treated definitively without surgery, and recurrence rates decreased from 92.4% to 10.1% in those who converted to surgical treatment. Factors associated with conversion to surgery included 2 or more subluxations prior to first evaluation (HR=1.82, p=0.002), 2 or more dislocations prior to first evaluation (HR=1.76, p=0.006), and recurrent instability at follow-up (HR=4.21, p<0.001).
Conclusions:
The majority of patients less than 40 years old with shoulder instability who are initially treated non-operatively for 6 months are definitively treated without surgery. Ultimately, 35% of these patients experienced recurrent dislocation after 6 months of conservative treatment and 20% ultimately underwent surgical treatment. The majority of patients that convert to surgical treatment had surgery within 12.5 years of their first instability event. Patients who experienced multiple instability events before or after consultation were more likely convert to surgery after initial non-operative management.
Level of Evidence:
Retrospective database review (Level 3).
INTRODUCTION
Anterior glenohumeral instability occurs at a rate of 23.9 per 100,000 person years, is most common in patients 15–29 years old, and occurs nearly 3 times more often in males compared to females.1 Following a first-time dislocation, the probability of a repeat event is widely variable and has been reported from 21–88% depending upon risk factors and characteristics such as age, number of dislocations, sport, occupation, and generalized ligamentous laxity to name a few.2–13 Long-term sequelae of repeated instability includes labral tears, chondral injury, glenohumeral bone loss, and arthritis.
With a wide variety of reported anterior instability recurrence rates in Level I and II studies, Wasserstein conducted a systematic review in 2016 of prospective studies analyzing non-operative treatment modalities.14 They concluded that recurrence rates following an initial dislocation event are near 21%. Factors that increase this risk include younger age (age < 30 have 6 times increased risk), male sex (2.68 times risk compared to females), and occupation with arm use above level of the chest. Greater tuberosity fractures decreased risk of recurrence. In their study, immobilization or duration, sports participation, and being a laborer had no significant effect on recurrence. Presence of a bony Bankart and/or Hill Sachs lesion was not associated with increased risk of recurrence in this study despite other reports showing increased rates of recurrence in their presence.15
Despite the previous studies mentioned, there remains a paucity of data to describe the natural history of a shoulder treated non-operatively following an index anterior instability event. More specifically, a U.S. epidemiologic-based study aimed at defining these outcomes is lacking in the current literature. Given the unique sporting and activity profiles of the U.S. population, a better understanding of shoulder instability in this group is warranted. The purpose of this study was to define the success rate of initial non-operative treatment for traumatic anterior shoulder instability in a defined US geographic population, describe factors that predict conversion to surgery after initial non-operative management, and describe the long-term outcomes of non-operative treatment following index traumatic anterior instability event.The primary variable was conversion to surgical treatment.
MATERIALS AND METHODS
Following approval by the institutional review board (IRB # 16–007084-10), the Rochester Epidemiology Project (REP) database was queried to identify patients that were diagnosed with anterior shoulder instability between 1994 and 2016 who were 14 – 39 years old at presentation. This database collects healthcare information from residents of Olmsted and surrounding counties, dating back to 1966.16 Previous validation of the REP has been reported with patients in this database accurately representing the general population in the United States.16, 17 The REP is an effective means of following this cohort with glenohumeral instability. Any healthcare exposure in the defined geographic area following the initial instability event is captured and included in treatment and outcome data.
Inclusion criteria were 1) traumatic anterior glenohumeral instability or dislocation, 2) an initial trial of at least 6 months of non-operative treatment after initial evaluation, and 3) age 14–39 at the time of initial instability evaluation. Traumatic instability was defined as an instability event directly correlated with a trauma and not the result of a habitual dislocation or multidirectional instability. This was verified by reviewing the history in individual patient charts. Patients were excluded if they had posterior instability, multi-directional instability, hyperlaxity, voluntary instability, no imaging available, incomplete medical records, or had less than 6 months clinical follow-up.
All patients were followed clinically, as well as radiographically and charts were reviewed retrospectively. Relevant data points were captured including patient demographics, history of instability, physical exam findings, treatment course, and clinical and radiographic outcomes. Initial clinical evaluation was conducted by a musculoskeletal clinician, followed by subsequent clinical follow-up by either Orthopedics or the patient’s primary care physician. Radiologic examination included AP and axillary views at a minimum, and associated fractures were documented.
For those patients meeting all inclusion criteria, the rate of treatment success at final follow-up (success defined as no conversion to surgery), patient factors (gender, age, # of subluxations or dislocations at presentation, overhead sports participation, labor-intensive occupation, recurrent instability after first evaluation) and injury characteristics (Hill-Sachs or Bony Bankart on index x-ray) associated with conversion to surgery, and long-term outcomes (recurrence rates, pain at last follow up, radiographic outcomes) were evaluated. Recurrent instability was defined as any patient who presented with multiple instability events (dislocation or subluxation), or presented with one instability event and subsequently experienced an additional dislocation or subluxation in the affected shoulder.
Statistical analysis
Continuous variables were assessed for parametric assumptions using the Shapiro-Wilk test. Student t tests or Wilcoxon rank-sum tests were used to analyze continuous variables. Chi-square analysis or Fisher exact tests were used to analyze categorical variables. Continuous data was reported as means and ranges with standard deviations. Survivorship free of surgery following initial non-operative treatment was reported with a Kaplan-Meier survival curve.
A multivariate Cox proportional-hazards model was constructed to evaluate the effects of multiple variables on conversion to surgery. Individual variables were first analyzed independently using Cox proportional-hazards modeling. The variables considered for inclusion may be found in Table 1. The final model was constructed using variables with an alpha of less than 0.10 when analyzed independently and those variables deemed clinically important by the senior authors. The total number of variables included in the final model was limited so that there were at least 10 outcome events, defined as progression to surgery, per variable analyzed.18, 19
Table I:
Demographics in patients treated non-operatively for minimum of 6 months following initial instability
| Variable | Continued Non-surgical Treatment (Group A) | Converted to Surgical Treatment (Group B) | P-Value |
|---|---|---|---|
| Gender, M/F | 242/58 | 70/9 | 0.100 |
| Age, mean (range) | 24.3 (14–39) | 22.1 (14–39) | 0.017 |
| BMI, mean (range) | 26.2 (18.9–47.8) | 26.1 (19.6–47.7) | 0.860 |
| Smoking, n (%) | 57 (21.3) | 13 (17.8) | 0.516 |
| Drug use, n (%) | 25 (9.3) | 7 (9.6) | 0.946 |
| Diabetes, n (%) | 5 (1.9) | 1 (1.4) | 1 |
| NM Disease, n (%) | 0 (0) | 0 (0) | - |
| Seizure Disorder, n (%) | 4 (1.5) | 2 (2.7) | 0.612 |
| Hand Dominance (R/L/Amb) | 131/17/0 | 52/5/0 | 0.574 |
| Dislocation (R/L/Bil) | 140/158/2 | 36/41/2 | 0.341 |
| Traumatic, n (%) | 300 (100) | 79 (100) | - |
| # Instability events 1st eval | 2.1 | 2.5 | 0.115 |
| Sports Participation, n (%) | 195 (65.2) | 56 (51.9) | 0.273 |
| Laborer, n (%) | 25 (8.5) | 10 (12.7) | 0.253 |
| Arthritis on Index XR, n (%) | 3 (1.1) | 0 (0) | 1 |
| Hill Sachs on Index XR, n (%) | 78 (27.9) | 23 (31.5) | 0.539 |
| Bony Bankart on Index XR, % | 20 (7.1) | 1 (1.4) | 0.091 |
M, male; F, female; BMI, body mass index; NM, neuromuscular; R, right;
L, left; Amb, ambidextrous; Bil, bilateral; eval, evaluation; XR, x-ray
Statistical significance was defined as alpha of 0.05.
RESULTS
A total of 480 patients with isolated anterior shoulder instability were initially identified (Figure 1). Of these, 101 underwent surgery in the first 6 months and were excluded from the study. The remaining 379 underwent an initial 6 month trial of non-operative treatment, met all inclusion criteria, and made up the study cohort. In these 379 patients, mean follow up was 10 years (range 0.53 to 25.0). Their demographics and injury characteristics are reported in Table 1. The entire study cohort was then further divided into patients who went on to definitive non-surgical management for their anterior shoulder instability (Group A) and patients who converted to surgical treatment greater than 6 months from their index instability event (Group B), and (Figure 1).
Figure 1:
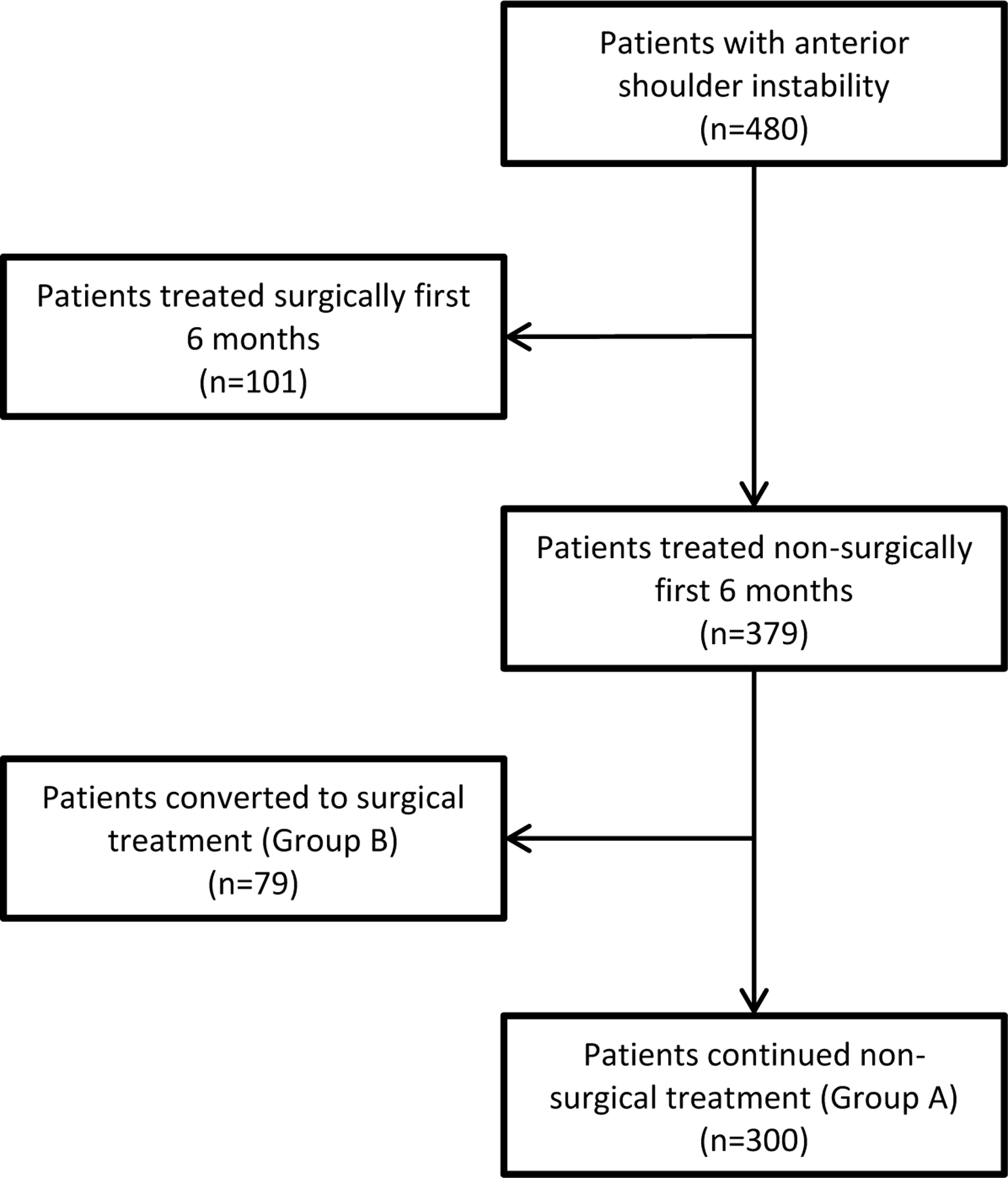
Study Flowchart.
Number of instability events on presentation and subsequent instability events are represented in Figure 2. In group A, 157 patients experienced more than one instability event before or during the study period (52.3%). In group B, 73 patients experienced multiple instability events before, or during the study period (92.4%). Following operative intervention, 7 reported an additional dislocation post-operatively and 1 reported a subluxation event with final recurrence rate of 10.1%. Combined, 230 patients in Group A and Group B experienced greater than 1 instability event before or after initial evaluation, demonstrating an overall recurrence rate of instability of 60.7. Total recurrent instability rate following initial presentation in groups A and B was 34.6%. When the 79 patients who underwent surgery after 6 months are combined with the 101 patients who had surgery prior to 6 months of non-operative treatment, the overall conversion to surgery was 37.5% (180/480).
Figure 2:

Flowchart of instability events before and after presentation in Group A and Group B.
Median time from consultation to surgery in Group B was 16 months (range 6.1 to 214.5 months) from initial evaluation. Survival is shown in Figure 3. Of note, rate of conversion to surgery leveled off after 12.5 years. Regarding surgical techniques, arthroscopic repair was performed in 61 patients with anchors placed in 52 (65.8%), and bone block augmentation in five. 18 patients required open treatment (22.8%), and of those, 5 had anchors placed, 5 received bone block augmentation, and capsular shift occurred in 4 patients. 15 patients in this group showed evidence of cartilage injury at the time of surgery with 5 demonstrating grade 3 or 4 cartilage injury.
Figure 3:

Survivorship free of surgery (in months) after initial 6-month period of nonsurgical treatment, with loss to follow-up as competing risk
A number of factors were associated with failure of non-operative treatment and conversion to surgery and are represented in Table 2. Presence of a bony Bankart lesion on x-ray had a hazard ratio of 0.31 which was statistically significant. This would imply presence of this lesion was protective from conversion to surgery. However, patients with a bony Bankart more commonly underwent surgery prior to 6 months, skewing this result.
Table II:
Multivariate Cox proportional hazards model of factors associated with conversion to surgery after initial 6 months of non-operative management
| Variable | Hazard Ratio | Confidence Interval | P-Value |
|---|---|---|---|
| Gender, male | 1.12 | 0.71–1.77 | 0.616 |
| Age < 22 | 1.00 | 0.97–1.02 | 0.817 |
| 2 or more Subluxations 1st eval | 1.82 | 1.24–2.66 | 0.002 |
| 2 or more Dislocations 1st eval | 1.76 | 1.18–2.60 | 0.006 |
| Overhead Sports Participation | 1.09 | 0.63–1.89 | 0.767 |
| Laborer | 1.63 | 0.90–2.76 | 0.101 |
| Recurrent Instability after 1st eval | 4.21 | 2.89–6.24 | <0.001 |
| Hill Sachs on Index XR, % | 1.15 | 0.75–1.73 | 0.515 |
| Bony Bankart on Index XR, % | 0.31 | 0.07–0.83 | 0.017 |
M, male; F, female; XR, x-ray;
Bold values indicate p < 0.05
Pain levels were reported by 152 non-operative patients (Group A), with 97 reporting no pain (63.8%), mild in 45 (29.8%), moderate in 10 (6.6%), and severe in 0 patients at final follow up. The surgical conversion group (Group B) had 72 patients with pain scores available at final follow-up and 61 reported no pain (84.7%), 10 with mild pain (13.9%), moderate pain in 5 (2.9%), and 1 patient with severe pain (1.4%). Pain levels were implied from clinic notes as there was no standardized reporting method. Final radiographs were available for 150 patients at mean follow-up of 46.3 months. 19 patients (12.7%) demonstrated evidence of glenohumeral arthritis with 131 showing no degenerative changes in the glenohumeral joint. Of patients with glenohumeral arthritis, 7 reported continued dislocations and 8 had converted to surgery (Group B).
Outcomes were analyzed based upon the number of instability events at the time of presentation. The rate of recurrent instability, conversion to surgery, pain at final follow-up, and development of glenohumeral arthritis was evaluated and is represented in Table 3.
Table III:
Outcomes based on # of instability events at time of presentation
| Instability events at presentation | Recurrent instabilitya | Conversion to Surgeryb | Pain (any severity)c | Osteoarthritisd |
|---|---|---|---|---|
| 1 | 32.3% (71/220) | 18.6% (41/220) | 29.1% (41/141) | 9.0% (8/89) |
| 2–3 | 36.1% (30/83) | 22.9% (19/83) | 26.7% (12/45) | 25.0% (7/28) |
| >3 | 39.5% (30/76) | 25.0% (19/76) | 34.2% (13/38) | 12.1% (4/33) |
| p-value | 0.494 | 0.437 | 0.800 | 0.110 |
Chi-square test. Data reported as % of group (number of patients/total included).
All 379 patients included
224 patients with pain documented were included in analysis
150 patients with post-operative x rays were included in analysis
DISCUSSION
In patients 14–39 years of age with anterior shoulder instability treated non-operatively for a minimum of 6 months, over half experienced at least one additional instability event and 1 in 5 patients ultimately underwent surgical treatment for instability. After an initial 6 month period of non-operative treatment, approximately 1 in 5 patients treated definitively with non-operative treatment experienced continued instability at final follow-up. Factors associated with conversion to surgery included: 2 or more subluxations prior to first evaluation, 2 or more dislocations prior to first evaluation, and recurrent instability at follow-up. For patients receiving surgical treatment, there was a substantial decrease in instability (76% reduction), even if it was performed in a delayed fashion.
Few studies exist describing the general outcomes of non-operative management. Hovelius et. al followed a Swedish cohort of 257 patients aged 12–40 following anterior shoulder instability treated non-operatively and reported outcomes at 25 years.20 43% of their patients experienced no repeat instability and an additional 7% had only one repeat event. Interestingly, recurrence leveled off at 5 years. 27% had undergone surgery for repeat instability at 25 years and 7.9% experienced continued instability at final follow-up. Wasserstein et al. also evaluated the recurrence rate of instability after non-surgical management of anterior shoulder dislocator in a systematic review.14 Their pooled rate of instability recurrence was in line with the current study. Male sex and younger age predicted higher rates of instability recurrence and in this cohort recurrence approached 80%. Tuberosity fractures however, greatly decreased the risk of recurrent instability. Robinson et. al reported that 86.7% of patients with recurrent instability had recurrent events within 2 years of their initial instability event.8
Non-operative treatment protocols typically consist of a brief period of immobilization, activity modification, and physical therapy. Several Level 1 studies have evaluated the impact of operative treatment on recurrent instability compared to non-operative treatment.21–24 Bottoni and Kirkley showed decreased dislocation rates in their arthroscopic Bankart repair cohorts compared to non-operative management.19, 20 Kirkley showed a clinical improvement based upon the Western Ontario Shoulder Index (WOSI) in their surgical group compared to non-operative management.22 Wintzell et. al evaluated arthroscopic lavage versus non-operative treatment in primary anterior instability patient’s and found that lavaging the joint to relieve the hemarthrosis and allow soft tissue healing decreased instability from 60 to 20%.23, 25 Finally, Jakobsen et al. evaluated open surgical treatment of Bankart lesions versus non-operative treatment and found that at 2 years, recurrence was 56% in the non-operative group and 3% in their surgical group.24 They also reported 72% of the surgical group had good or excellent surgical outcomes based on the Oxford self-assessment score compared to unsatisfactory results in 75% of the conservative group due to recurrence of instability, pain, and/or stiffness.
Hovelius et. al presented results with their 25 year follow-up experience in patients following their index anterior instability event and reported 27% of patients were treated surgically at final follow-up.20 Surgery was required more commonly in young patients compared to the older cohort (40% of patients aged 12–22 required surgery for repeat instability, compared to 14% aged 30–40). Their rate of conversion to surgery is similar to this study. Barlow et. al evaluated early surgical treatment following the primary instability event compared to surgical intervention in a delayed fashion after recurrent anterior instability.26 Overall, they found no difference in instability recurrence or outcome measures following acute or delayed stabilization.
In our study population, factors associated with conversion to surgery after initial non-operative management include 2 or more subluxations prior to first evaluation, 2 or more dislocations prior to first evaluation,and recurrent instability at follow-up. In practice, recurrent instability is a common indication for surgery. Wasserstein et. al identified male gender and age less than 20 associated with increased odds of instability recurrence with decreased age being the strongest predictor.14 They also noted that a greater tuberosity fracture decreases the onset of recurrence by 3.8 times. In their study, there was no significant difference in the onset of recurrence in the setting of Hill-Sachs lesions, immobilization position or duration, athletic participation, or labor intensive occupation.
If surgical treatment is indicated, there are both arthroscopic and open surgical options. Balg et. al developed the instability severity index score (ISIS) to guide patient selection for arthroscopic versus open shoulder stabilization.15 This score takes into account patient age, level and type of sport, shoulder hyperlaxity, size and location of Hill-Sachs, and loss of glenoid contour. We did not include glenoid bone loss or the ISIS score in this study.
At final follow-up, greater than 90% of patients from the present study reported no or mild pain in the involved shoulder in those treated by continued non-operative measures or surgically. Similarly, greater than 98% of the patients in the cohort that converted to surgery reported no or mild pain in the affected shoulder. The previously mentioned study by Hovelius et. al reported Disabilities of the Arm, Shoulder, and Hand scores in their patients.20 They reported that at final follow-up, scores were similar in those with no recurrent instability that stabilized over time, to patients that underwent surgical stabilization. Jakobsen et. al reported on both an operatively and non-operatively treated cohort of patients in a level 1 study with 10 years of follow-up.24 They described 75% unsatisfactory results in their non-operative cohort based upon recurrence, instability, or pain and stiffness at final follow-up. The majority of the outcomes deemed unsatisfactory were due to recurrent instability and they reported rates of recurrent instability similar to the current study.
Glenohumeral arthritis was apparent in 12.7% of the current study cohort on final follow up x-rays. Buscayret reported a similar incidence of glenohumeral arthritis in a large cohort treated surgically for anterior shoulder instability.27 They demonstrated higher rates of glenohumeral arthritis in patients with increased number of dislocations, older age at initial dislocation, older age at surgery, and longer follow-up. Hovelius et. al reported radiographic outcomes in their cohort with a higher overall rate of arthropathy at 56%. 28Their higher rate was likely due to longer follow-up. Risk factors for the development of arthropathy included older age at index dislocation, recurrent instability, high energy sports, and alcohol abuse. Shoulders that did not experience recurrent instability, or that stabilized over time had lower rates of arthropathy.
In the current study, outcomes were also analyzed based upon number of instability events at the time presentation. The primary finding of this analysis was that increased number of instability events at presentation was not associated with increased rates of recurrent instability at subsequent follow-up. We did not find a statistically significant association between number of instability events at presentation and conversion to surgery, pain severity, or eventual development of osteoarthritis.
Limitations
There are several limitations to the present study that merit discussion. This study was performed in a retrospective manner, and therefore we were limited to the data available in the medical records. Because this is a defined population based study, it includes a number of different treating physicians/surgeons and treatment protocols were not standardized across providers. The wide variety of surgical techniques complicates the reporting of recurrence rates following surgery, and techniques have changed significantly since 1966 when patients were first included in this study. Also, MRI was not routinely used in follow-up, we do not report patient reported outcomes, and radiographs were not reviewed beyond their associated radiology report. Finally, this study did not include patients who were treated surgically within 6 months after their first instability event. Patients were more likely to be treated with early surgical intervention if they were young and presented after multiple instability events, had bone loss on presentation, or if they participated in higher sports activity level, leading to potential selection bias. Due to this,the findings may be less applicable to patients with more severe pathology or who are at the highest risk for repeat instability and elect to receive early surgical treatment.
CONCLUSION
The majority of patients less than 40 years old with shoulder instability who are initially treated non-operatively for 6 months are definitively treated without surgery. Ultimately, 35% of these patients experienced recurrent dislocation after 6 months of conservative treatment and 20% ultimately underwent surgical treatment. The majority of patients that convert to surgical treatment have surgery within 12.5 years of their first instability event. Patients who experienced multiple instability events before or after consultation were more likely convert to surgery after initial non-operative management.
Acknowledgments
The authors would like to acknowledge the support from the Foderaro/Quattrone Musculoskeletal-Orthopaedic Surgery Research Innovation Fund. Additionally, this study used the resources of the Rochester Epidemiology Project (REP) medical records-linkage system, which is supported by the National Institute on Aging (NIA; AG 058738), by the Mayo Clinic Research Committee, and by fees paid annually by REP users. The content of this article is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health (NIH) or the Mayo Clinic.
Footnotes
Primary Location where this investigation was performed: Mayo Clinic, Rochester, MN
REFERENCES
- 1.Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am 2010;92:542–549. [DOI] [PubMed] [Google Scholar]
- 2.Leroux T, Wasserstein D, Veillette C, et al. Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med 2014;42:442–450. [DOI] [PubMed] [Google Scholar]
- 3.Kralinger FS, Golser K, Wischatta R, Wambacher M, Sperner G. Predicting recurrence after primary anterior shoulder dislocation. Am J Sports Med 2002;30:116–120. [DOI] [PubMed] [Google Scholar]
- 4.Sachs RA, Lin D, Stone ML, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg Am 2007;89:1665–1674. [DOI] [PubMed] [Google Scholar]
- 5.Henry JH, Genung JA. Natural history of glenohumeral dislocation--revisited. Am J Sports Med 1982;10:135–137. [DOI] [PubMed] [Google Scholar]
- 6.Hoelen MA, Burgers AM, Rozing PM. Prognosis of primary anterior shoulder dislocation in young adults. Arch Orthop Trauma Surg 1990;110:51–54. [DOI] [PubMed] [Google Scholar]
- 7.Mc LH, Cavallaro WU. Primary anterior dislocation of the shoulder. Am J Surg 1950;80:615–621; passim. [DOI] [PubMed] [Google Scholar]
- 8.Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am 2006;88:2326–2336. [DOI] [PubMed] [Google Scholar]
- 9.Rowe CR, Sakellarides HT. Factors related to recurrences of anterior dislocations of the shoulder. Clin Orthop 1961;20:40–48. [PubMed] [Google Scholar]
- 10.Safran O, Milgrom C, Radeva-Petrova DR, Jaber S, Finestone A. Accuracy of the anterior apprehension test as a predictor of risk for redislocation after a first traumatic shoulder dislocation. Am J Sports Med 2010;38:972–975. [DOI] [PubMed] [Google Scholar]
- 11.Salomonsson B, von Heine A, Dahlborn M, et al. Bony Bankart is a positive predictive factor after primary shoulder dislocation. Knee Surg Sports Traumatol Arthrosc 2010;18:1425–1431. [DOI] [PubMed] [Google Scholar]
- 12.Simonet WT, Cofield RH. Prognosis in anterior shoulder dislocation. Am J Sports Med 1984;12:19–24. [DOI] [PubMed] [Google Scholar]
- 13.Vermeiren J, Handelberg F, Casteleyn PP, Opdecam P. The rate of recurrence of traumatic anterior dislocation of the shoulder. A study of 154 cases and a review of the literature. Int Orthop 1993;17:337–341. [DOI] [PubMed] [Google Scholar]
- 14.Wasserstein DN, Sheth U, Colbenson K, et al. The True Recurrence Rate and Factors Predicting Recurrent Instability After Nonsurgical Management of Traumatic Primary Anterior Shoulder Dislocation: A Systematic Review. Arthroscopy 2016;32:2616–2625. [DOI] [PubMed] [Google Scholar]
- 15.Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470–1477. [DOI] [PubMed] [Google Scholar]
- 16.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol 2012;41:1614–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol 2011;173:1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Concato J, Peduzzi P, Holford TR, Feinstein AR. Importance of events per independent variable in proportional hazards analysis. I. Background, goals, and general strategy. J Clin Epidemiol 1995;48:1495–1501. [DOI] [PubMed] [Google Scholar]
- 19.Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol 1995;48:1503–1510. [DOI] [PubMed] [Google Scholar]
- 20.Hovelius L, Olofsson A, Sandstrom B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. a prospective twenty-five-year follow-up. J Bone Joint Surg Am 2008;90:945–952. [DOI] [PubMed] [Google Scholar]
- 21.Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med 2002;30:576–580. [DOI] [PubMed] [Google Scholar]
- 22.Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy 2005;21:55–63. [DOI] [PubMed] [Google Scholar]
- 23.Wintzell G, Haglund-Akerlind Y, Nowak J, Larsson S. Arthroscopic lavage compared with nonoperative treatment for traumatic primary anterior shoulder dislocation: a 2-year follow-up of a prospective randomized study. J Shoulder Elbow Surg 1999;8:399–402. [DOI] [PubMed] [Google Scholar]
- 24.Jakobsen BW, Johannsen HV, Suder P, Sojbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy 2007;23:118–123. [DOI] [PubMed] [Google Scholar]
- 25.Wintzell G, Hovelius L, Wikblad L, Saebo M, Larsson S. Arthroscopic lavage speeds reduction in effusion in the glenohumeral joint after primary anterior shoulder dislocation: a controlled randomized ultrasound study. Knee Surg Sports Traumatol Arthrosc 2000;8:56–60. [DOI] [PubMed] [Google Scholar]
- 26.Barlow JD, Grosel T, Higgins J, Everhart JS, Magnussen RA. Surgical treatment outcomes after primary vs recurrent anterior shoulder instability. J Clin Orthop Trauma 2019;10:222–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buscayret F, Edwards TB, Szabo I, Adeleine P, Coudane H, Walch G. Glenohumeral arthrosis in anterior instability before and after surgical treatment: incidence and contributing factors. Am J Sports Med 2004;32:1165–1172. [DOI] [PubMed] [Google Scholar]
- 28.Hovelius L, Saeboe M. Neer Award 2008: Arthropathy after primary anterior shoulder dislocation−-223 shoulders prospectively followed up for twenty-five years. J Shoulder Elbow Surg 2009;18:339–347. [DOI] [PubMed] [Google Scholar]


