Abstract
Introduction
One in 10 women have hypertensive disorders in pregnancy (HDP) and are at risk of adverse short- and long-term health outcomes, yet there is limited information on their postnatal health and care needs. This study aimed to look at postnatal physical and psychological morbidity in women with HDP, compared to women without HDP, and the postnatal care received in both groups.
Methods
Within a prospective cohort study, women with and without HDP were identified and recruited on the postnatal ward of 17 maternity units across England and invited to complete a short baseline questionnaire. At 3 months postpartum, women were sent a follow-up questionnaire, with reminders. The principal outcomes were the mean score at 3 months for the Edinburgh Postnatal Depression Scale (EPDS) and the EuroQol Group 5-dimension (EQ-5D) scale.
Results
One thousand eight hundred twenty-nine women agreed to participate. Of these, 1757 (96%) completed the baseline questionnaire: 769 (44%) women had HDP and 988 (56%) women did not. Despite a difference in health-related quality of life and symptoms of depression at baseline between the two groups, at 3 months postnatal, within the 653 women who completed their follow-up questionnaire (37.2% of those who completed the baseline questionnaire) there were no significant differences between the groups (median EQ-5D VAS: 85 in women with HDP, 85 in women without HDP, p = 0.99 and mean EPDS score 5.5 in women with HDP, 5.0 in women without HDP, p = 0.80). Overall levels of physical postnatal morbidity were high, with 89% reporting one or more morbidities. Approximately 9% of women were re-admitted within 3 months after birth, higher in the HDP group (13.1%) higher compared to women without HDP (5.5%; RR 2.41; 95% CI 1.44–4.05).
Conclusion
Overall levels of physical and psychological morbidity were high in this postnatal population. Although there were increased needs of women with HDP in the immediate postnatal period (compared to other women), their health assessments were similar at 3 months. This study highlights the unmet needs of women in the postnatal period, in addition to a missed opportunity to influence future pregnancies and improve the longer-term health of women and their babies.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-022-04540-2.
Keywords: Pregnancy, Hypertension, High blood pressure, Postnatal
Introduction
Hypertensive Disorders of Pregnancy (HDP) affect approximately 10% of all pregnancies [1] and include chronic hypertension (pre-existing hypertension present before 20 weeks’ gestation), gestational hypertension (hypertension presenting after 20 weeks’ gestation) and pre-eclampsia (de novo, or superimposed on chronic hypertension, with proteinuria and/or renal, hepatic or haematological dysfunction). HDP are associated with substantial maternal and perinatal morbidity and mortality [2–4], responsible for approximately 14% of maternal deaths globally [5]. There is also an increased risk of recurrence of HDP in future pregnancies [6] and increased lifetime risk of maternal cardiovascular disease [7, 8].
In the United Kingdom (UK), postnatal care aims to improve and support birth recovery and good maternal and infant physical and psychological health [9]. Most women commence postnatal care in hospital, and this continues at home or in community-based clinics with midwives and health visitors after hospital discharge. Women typically are offered a routine consultation with their family doctor (GP) at 6–8 weeks after birth. Although for many years this was primarily focused on a check of the infant, this has recently been mandated to also include a maternal health check [10]. Clinical guidance is provided for routine postnatal care for women and their infants [11] with guidance for women with HDP covered by the Hypertension in Pregnancy: diagnosis and management guideline [12].
Research to date has focused predominantly on antenatal management of HDP. The neglect of the postnatal period in the evidence base and lack of evidence of postnatal care being tailored to meet individual maternal need has been highlighted as a missed opportunity to improve wellbeing and reduce long-term adverse health outcomes for women and children [9, 13]. Although a number of large observational studies in the 1990s [14–16] highlighted extensive maternal postnatal morbidity, there has been a lack of focus in more recent years.
Given the sparsity of recent evidence on postnatal health and wellbeing, and extent to which current postnatal services reflect implementation of current guidance, this study aimed to address the postnatal morbidity at 3 months after birth for women with and without HDP, specifically including both physical and psychological conditions. We aimed to evaluate whether women with HDP experience greater postnatal physical and psychological morbidity than those without HDP, and the extent and characterisation of postnatal morbidity.
Methods
Study design and setting
In this prospective multicentre cohort study, women were recruited on the postnatal wards of 17 maternity units across England between February 2019 and March 2020. Women who were 18 years old or above and who gave birth at ≥20+ 0 weeks’ gestation were eligible. The study was registered with the ISRCTN registry (ISRCTN10809239) and approved by the London - South East Research Ethics Committee (REC reference: 18/LO/2084).
Patient and public involvement
The Participant Information Sheet and study questionnaire were reviewed by members of the ‘Hypertension in Pregnancy Patient and Public Involvement group’ established at the lead site. Feedback forms demonstrated women’s support of the study (all completed forms indicated women felt the study to be ‘very important’ and that they would likely take part if invited) and no concerns were raised about the usefulness, length or clarity of the questionnaire or Participant Information Sheet. Issues were discussed relating to potential barriers to recruitment. Feedback from these meetings led to adjustments in study design, Participant Information Sheet content, questionnaire content, and questionnaire delivery method (online was unanimously preferred over paper and postal routes).
Recruitment and data collection
Eligible women were identified using the postnatal ward list at participating maternity units. A convenience sample of these women were approached by local research midwives, based on aiming to recruit similar numbers of women who were hypertensive and normotensive. Eligible women who wished to take part in the study provided their written electronic consent.
Recruited participants were asked to complete an initial (baseline) questionnaire on the postnatal ward and a follow-up questionnaire at 12 weeks postpartum, emailed (or posted to women if they preferred). The questionnaires captured information on their obstetric and medical history, family history of obstetric complications and relevant medical conditions, demographic information, infant feeding, current physical and mental health, postnatal care received, and their plans for future pregnancies. Specific morbidities included: extreme tiredness/ exhaustion; severe headaches/ migraines; back pain; perineal wound infection; Caesarean wound infection; breastfeeding problems; leakage of urine; leakage of stool; or other problems (as provided in free text answers). Both questionnaires included validated health measures: Edinburgh Postnatal Depression Scale (EPDS) (10 questions used to detect possible postnatal depression) [17], EuroQol Group five dimension (EQ-5D) (two-page assessment of health-related quality of life, consisting of five dimensions each with levels of severity and a vertical visual analogue scale) [18, 19] and the Whooley questions (two questions used to routinely screen for maternal mental health issues during and after pregnancy in NHS maternity services) [20]. Women whose EPDS score was 13 or over (i.e., indicating a presence of possible depressive symptoms) or women who answered positively to question 10 (i.e., indicating potential self-harm or suicidal thoughts) were either flagged to their case midwife on the postnatal ward (following baseline questionnaire completion) or contacted by the central research team (on follow-up questionnaire completion). At follow-up, the central research team ensured these women were aware of the services provided by appropriate healthcare professionals (e.g., health visitor, midwife, family doctor). Following discussion with Patient and Public Involvement representatives, all women were offered the opportunity to complete follow-up, even if they had not had a live birth.
Research midwives entered additional participant data directly into the study’s secure online central database (MedSciNet, Stockholm, Sweden) extracted from the maternity records (with the participant’s consent).
Statistical analysis
Data analysis was conducted in Stata version 16 [21]. Means and frequency tables were reported and differences between the groups (women with HDP and women without HDP) examined using t-test, chi-square statistics, and median differences analysed through median tests. Differences between the groups for binary outcomes were examined using binary regression with a log link to give Risk Ratios. For the principal outcomes, we adjusted for drop-out at the 3-month timepoint by using inverse probability weightings to correct for potential imbalance in the case mix seen at enrolment. Models were not adjusted for confounders as we were interested in outcome prevalence rather than mechanisms. Adjusting for variables at enrolment could have removed consequences of pregnancy hypertension we were seeking to describe. In line with recent literature, an EPDS cut-off of 13 or more was used to identify women for further assessment for depression [22].
Free text analysis
To supplement the quantitative results and in response to initial Patient and Public Involvement work, the follow-up questionnaire included three open-ended questions. Participants were asked whether they had any comments about their health and wellbeing since having their baby; whether they had any comments about their postnatal care; and whether their perinatal experiences had changed their opinion on future pregnancies. Data were managed and analysed in NVivo 12 [23], using a thematic framework analysis. The most illustrative quotations are presented in the results section.
Results
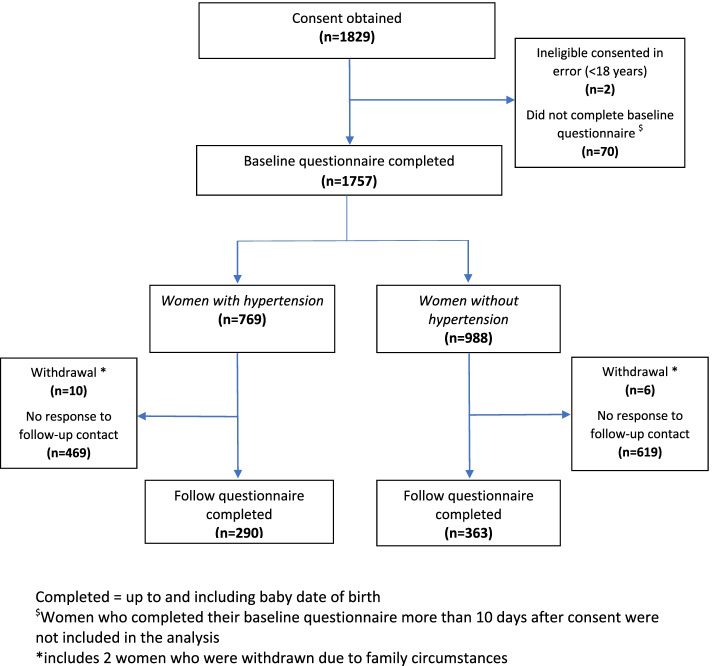
Of the 2893 eligible women approached, 1829 (63%) consented to take part. Of these, 1757 (96%) completed the baseline questionnaire (at postnatal enrolment): 769 (44%) women had HDP and 988 (56%) women did not. Follow-up questionnaires (at 12 weeks postnatal) were completed by 653 of the 1757 (37%) women: 290 of 769 women (38%) with HDP and 363 of 988 women (37%) without HDP (Fig. 1).
Fig. 1.
Flow of participants
Characteristics of the study population at postnatal enrolment are shown in Tables 1 and 2, supplementary Table 1 and supplementary Table 2; differences are noted between the two groups (women with HDP and women without HDP) in ethnicity, risk factors for hypertension, Body Mass Index, parity, multi-fetal births, intended and actual mode of birth, labour analgesia, maternal and neonatal length of inpatient postnatal stay, admission to Neonatal Unit, and proportion of small-for-gestational age infants.
Table 1.
Self-reported maternal demographics at postnatal enrolment
| Total | Hypertensive in pregnancy | Normotensive in pregnancy | Comparison/Difference | |
|---|---|---|---|---|
| Number of women (n, %) | 1757 | 769 (43.8) | 988 (56.2) | |
| Maternal age, years (mean, SD) | 32.7 (5.5) | 32.9 (5.8) | 32.6 (5.2) | 0.3538 |
| Ethnicity groupings | ||||
| Black/Black mixed | 263 (15.0) | 145 (18.9) | 118 (11.9) | < 0.0001 |
| Asian/Asian mixed | 187 (10.7) | 78 (10.1) | 109 (11.0) | |
| White | 1230 (70.0) | 508 (66.1) | 722 (73.1) | |
| Other | 75 (4.3) | 37 (4.8) | 38 (3.9) | |
| Missing | 2 (0.1) | 1 (0.1) | 1 (0.1) | |
| First baby | 1076 (61.3) | 501 (65.2) | 575 (58.2) | 0.003 |
| Singleton baby | 1712 (97.4) | 739 (96.1) | 973 (98.5) | 0.002 |
| Self-reported hypertension type(non-exclusive) | ||||
| Chronic | 84 (10.9) | Not applicable | ||
| Gestational | 240 (31.2) | |||
| Pre-eclampsia | 311 (40.4) | |||
| Eclampsia | 6 (0.8) | |||
| HELLP syndrome | 15 (2.0) | |||
| Hypertension (not specified) | 202 (26.3) | |||
| Education level beyond secondary | 1375 (78.3) | 587 (76.3) | 788 (79.8) | 0.086 |
| Currently employed (self-reported) | 1321 (75.2) | 569 (74.0) | 752 (76.1) | 0.311 |
| Living with others | 1554 (88.5) | 668 (86.9) | 886 (89.7) | 0.069 |
| Any risk factors for hypertension | 1395 (79.4) | 684 (89.0) | 711 (72.0) | < 0.0001 |
| Any mental health condition | 307 (17.5) | 149 (19.4) | 158 (16.0) | 0.064 |
| Intended mode of birth | ||||
| Spontaneous vaginal birth | 1062 (60.4) | 421 (54.8) | 641 (64.9) | |
| Elective c-section | 304 (17.3) | 117 (15.2) | 187 (18.9) | |
| Planned induction (vaginal birth) | 289 (16.5) | 157 (20.4) | 132 (13.4) | |
| Not discussed - delivered early | 24 (1.4) | 20 (2.6) | 4 (0.4) | |
| Not discussed – other | 78 (4.4) | 54 (7.0) | 24 (2.4) | |
| At initial antenatal visit | ||||
| Body mass index, kg/m2 (median, IQR) | 26 (22.5–30.7) | 27 (23.4–32.5) | 25 (22–29) | < 0.0001 |
| Current smoker | 97 (5.5) | 46 (6.0) | 51 (5.2) | 0.458 |
| Positive to either Whooley question | 124 (7.1) | 64 (8.3) | 60 (6.1) | OR 1.39 (0.97–2.02) |
| Missing | 134 (7.6) | 56 (7.3) | 78 (7.9) | |
HELLP Haemolysis, Elevated Liver enzymes, Low Platelets, OR odds ratio
Table 2.
Characteristics of labour, birth, and post-delivery postnatal stay at postnatal enrolment
| Totals | Hypertensive in pregnancy | Normotensive in pregnancy | Comparison/Difference | |
|---|---|---|---|---|
| Maternal outcomes: number of women (n, %) | 1757 | 769 (43.8) | 988 (56.2) | |
| Use of regional anaesthetic in labour | 1228 (69.9) | 572 (74.4) | 656 (66.4) | < 0.0001 |
| Second/third/fourth degree perineal tear or episiotomy | 668 (38.0) | 250 (32.5) | 418 (42.3) | 0.060 |
| Length of postnatal inpatient stay, days (median, IQR) | 3 (2–4) | 3 (2–5) | 2 (1–3) | < 0.0001 |
| Admission to either high dependency unit or intensive care unitb | 181(10.3) | 86 (11.2) | 95 (9.6) | 0.287 |
| Length of stay in high dependency unit or intensive care unit, days (median, IQR) | 1 (1–1) | 1 (1–2) | 1 (1–1) | < 0.0001 |
| Perinatal outcomes: number of infants | 1803 | 799 (44.3) | 1004 (55.7) | |
| Live births | 1802 (99.9) | 799 (100.0) | 1003 (99.9) | 0.372 |
| Mode of birth | ||||
| Vaginal | 657 (36.4) | 252 (31.5) | 405 (40.3) | < 0.0001 |
| Forceps | 168 (9.3) | 68 (8.5) | 100 (10.0) | |
| Ventouse | 137 (7.6) | 55 (6.9) | 82 (8.2) | |
| Pre-labour Caesarean section | 462 (25.6) | 236 (29.5) | 226 (22.5) | |
| In-labour Caesarean section | 379 (21.0) | 188 (23.5) | 191 (19.0) | |
| Gestational age at birth, weeks (mean, SD) | 38.8 (2.3) | 38.2 (2.6) | 39.4 (1.9) | < 0.0001a |
| Birthweight, kg (mean, SD) | 3.198 (0.671) | 3.010 (0.743) | 3.348 (0.565) | < 0.0001a |
| Small for Gestational Age (<10th birthweight centile) | 184 (10.2) | 177 (14.6) | 67 (6.7) | < 0.0001 |
| Length of infant inpatient stay, days (mean, SD) | 4.2 (6.7) | 5.7 (9.1) | 3.1 (3.5) | < 0.0001a |
| Baby (ies) admitted to the neonatal unit | 230 (12.8) | 155 (19.4) | 75 (7.5) | < 0.0001 |
| Length of stay in neonatal unit, days (mean, SD) | 9.7 (9.6) | 11.5 (9.9) | 5.9 (7.6) | < 0.0001a |
OR odds ratio
aAdjusted for clustering by twins
bIncludes post Caesarean section recovery
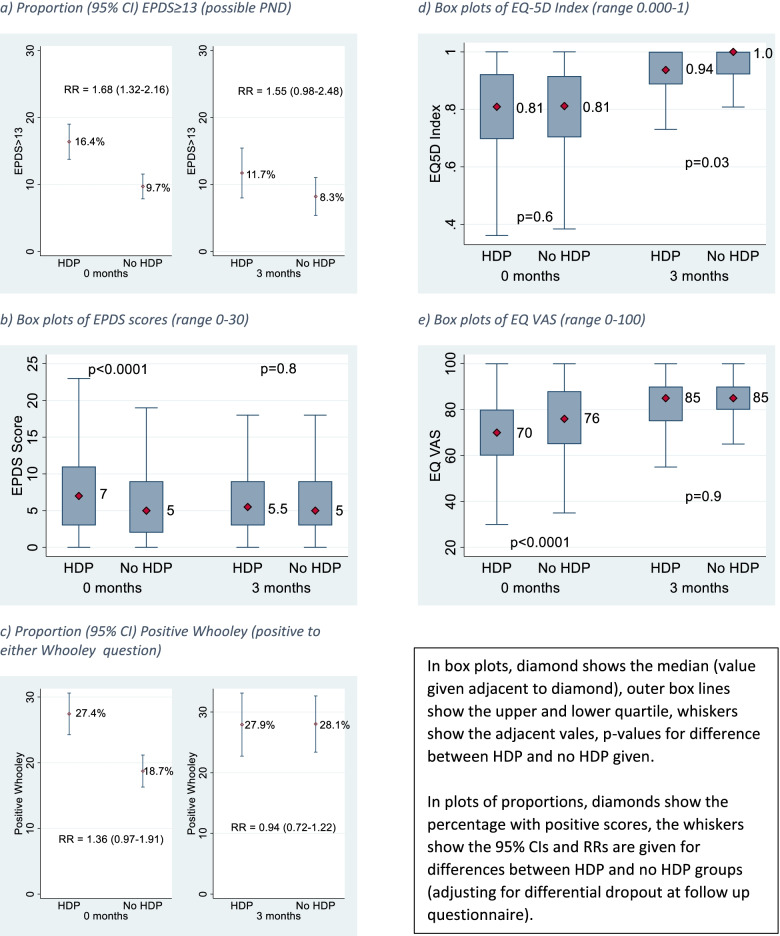
Postnatal enrolment
At postnatal enrolment, health-related quality of life, as measured by the EQ-5D Visual Analogue Scale, was lower in women with HDP compared with women without HDP (median EQ-5D VAS: 70 in women with HDP, 76 in women without HDP) but not in the EQ-5D index score between the groups (Fig. 2, supplementary Table 3). Symptoms of depression were also higher in the HDP group; for the EPDS, there was a median score of 7 (with 16.4% having scores ≥13) in women with HDP compared to a median score of 5 (with 9.7% having scores ≥13) in women without HDP (Risk Ratio 1.68; 95% CI 1.32–2.16). For the Whooley score, 27.4% of the women with HDP were positive to either question one or two compared to 18.7% of women without HDP, (RR 1.36; 95% CI 0.97–1.91) (Fig. 2, supplementary Table 3).
Fig. 2.
Mental and physical health scores in women with and without hypertensive disorders of pregnancy, at 0 months (n = 769 with HDP; n = 988 with no HDP) and 3 months (n = 290 with HDP; n = 363 with no HDP) postnatally. a Proportion (95% CI) EPDS≥13 (possible PND). b Box plots of EPDS scores (range 0–30). c Proportion (95% CI) Positive Whooley (positive to either Whooley question). d Box plots of EQ-5D Index (range 0.000–1). e Box plots of EQ VAS (range 0–100)
Three month postnatal physical and mental wellbeing
At 3 months postnatal, there was no evidence of a significant difference between the groups in physical and mental health scores, including the mean Edinburgh Postnatal Depression Scale score (p = 0.80), median EQ-5D quality of life scale score (p = 0.99), the Whooley responses (RR 0.94; 95% CI 0.72–1.22) and most physical morbidities (Fig. 2; Table 3).
Table 3.
Main primary and secondary outcomes at 3 months postnatal
| Totals | Hypertensive in pregnancy | Normotensive in pregnancy | Comparison/difference | |
|---|---|---|---|---|
| Number of women | 653 | 290 (44.4) | 363 (55.6) | |
| EPDS score ≥ 13 | 64 (9.8) | 34 (11.7) | 30 (8.3) | OR 1.47 (0.88–2.47) |
| EPDS total score (mean, SD) | 6.2 (4.6) | 6.3 (4.8) | 6.1 (4.5) | 0.617 |
| Positive to either Whooley Q1 or Q2 | 183 (28.0) | 81 (27.9) | 102 (28.1) | OR 0.99 (0.70–1.40) |
| EQ-5D index score (mean, SD) | 0.935 (0.088) | 0.926 (0.093) | 0.943 (0.084) | 0.0222 |
| EQ-5D VAS score (0–100) | 82.8 (13.3) | 82.2 (13.5) | 83.2 (13.1) | 0.3557 |
| Any reported morbidity at 3 months postnatal | 582 (89.1) | 260 (89.7) | 322 (88.7) | OR 1.17 (0.49–2.77) |
| Women with any morbidity who consulted a health care professional | 378 (57.9) | 171 (59.0) | 207 (57.0) | OR 1.19 (0.50–2.86) |
| Morbidities reported: | ||||
| Extreme tiredness/ exhaustion | 252(38.6) | 120 (41.4) | 132 (36.4) | OR 1.23 (0.90–1.69) |
| Severe headaches/ migraines | 100 (15.3) | 55 (19.0) | 45 (12.4) | OR 1.65 (1.07–2.53) |
| Back pain | 357 (54.7) | 168 (57.9) | 189 (52.1) | OR 1.26 (0.92–1.72) |
| Perineal wound infection | 36 (5.5) | 18 (6.2) | 18 (5.0) | OR 1.33 (0.67–2.63) |
| Caesarean wound infection | 61 (9.3) | 33 (11.4) | 28 (7.7) | OR 1.22 (0.70–2.14) |
| Breastfeeding problems | 298 (45.6) | 120 (41.4) | 178 (49.0) | OR 0.69 (0.50–0.96) |
| Leakage of urine | 189 (29.0) | 83 (28.6) | 106 (29.2) | OR 0.97 (0.69–1.36) |
| Leakage of stool | 26 (4.0) | 10 (3.5) | 16 (4.4) | OR 0.77 (0.35–1.73) |
| Other problems | 161 (24.7) | 73 (25.2) | 88 (24.2) | OR 1.05 (0.73–1.50) |
EPDS Edinburgh Postnatal Depression Scale, EQ-5D VAS EuroQol Group five dimension visual analogue scale, OR odds ratio
Overall levels of physical postnatal morbidity were high, with 89% reporting one or more morbidities since birth, with back pain (55%) and breastfeeding problems (46%) most commonly reported (Table 3). Rates of responses to ‘ever breastfed’ or ‘currently breastfeeding’ at 3 months were similar in both groups. For breastfeeding, 90% reported having ever breastfed and 52% were currently breastfeeding (Table 4, supplementary Table 4).
Table 4.
Postnatal care at 3 months postnatal and opinions on future pregnancies (self-reported)
| Totals | Hypertensive in pregnancy | Normotensive in pregnancy | Comparison/ difference | |
|---|---|---|---|---|
| Number of women | 653 | 290 (44.4) | 363 (55.6) | |
| Breastfeeding | ||||
| Ever breastfeed baby | 586 (89.7) | 261 (90.0) | 325 (89.5) | OR 1.05 (0.63–1.75) |
| First feed breastmilk (of those who ever breastfed) | 540 (92.2) | 231 (88.5) | 309 (95.2) | OR 0.40 (0.21–0.75) |
| Currently feeding breastmilk (of those who ever breastfed) | 305 (52.1) | 129 (49.4) | 176 (54.2) | OR 0.83 (0.60–1.15) |
| BP measured in hospital | 619 (94.8) | 274 (94.5) | 345 (95.0) | |
| Frequency of BP measured in hospital (where measured) | ||||
| Less than once a day | 33 (5.3) | 7 (2.6) | 26 (7.5) | < 0.0001 |
| Approximately once a day | 115 (18.6) | 23 (8.4) | 92 (26.7) | |
| More than once a day | 460 (74.3) | 240 (87.6) | 220 (63.8) | |
| Other | 11 (1.8) | 4 (1.5) | 7 (2.0) | |
| BP medication taken between birth and 6 weeks postnatal | 208 (31.9) | 194 (66.9) | 14 (3.9) | OR 54.17 (20.0–97.80) |
| One or more postnatal visits at: | ||||
| Home | 505 (77.3) | 236 (81.4) | 269 (74.1) | OR 1.70 (1.14–2.52) |
| Hospital/ clinic | 215 (32.9) | 104 (35.9) | 111 (30.6) | OR 1.30 (0.94–1.81) |
| GP | 466 (71.4) | 222 (76.6) | 244 (67.2) | OR 1.73 (1.20–2.48) |
| Median (IQR) number of postnatal visits (of women visited) at: | ||||
| Home | 2 (2–3) | 3 (2–2) | 3 (4–2) | 0.174 |
| Hospital/ clinic | 2 (3–1) | 2 (3–1) | 1 (2–1) | 0.553 |
| GP | 1 (2–1) | 2 (3–1) | 1 (2–1) | < 0.0001 |
| BP never measured at postnatal visits (of women visited) at: | ||||
| Home | 196 (38.8) | 56 (23.7) | 140 (52.0) | < 0.0001 |
| Hospital/ clinic | 77 (35.8) | 24 (23.1) | 53 (47.8) | < 0.0001 |
| GP | 90 (19.3) | 23 (10.4) | 67 (27.5) | < 0.0001 |
| Readmitted to hospital | 58 (8.9) | 38 (13.1) | 20 (5.5) | OR 2.6 (1.49–4.64) |
| Readmitted to hospital due to BP | 28 (4.3) | 24 (8.3) | 4 (1.1) | OR 8.10 (2.78–23.62) |
| Attendance at GP postnatal check | 584 (89.4) | 258 (89.0) | 326 (89.8) | OR 1.06 (0.61–1.84) |
| BP measured at GP postnatal check (of those attending) | 459 (78.6) | 214 (83.0) | 245 (75.2) | OR 1.61 (1.07–2.42) |
| Any self-monitoring of BP since birth | 154 (23.6) | 125 (43.1) | 29 (8.0) | OR 9.03 (5.78–14.12) |
| Regular self-monitoring of BP since birth | 79 (12.1) | 72 (24.8) | 7 (1.9) | OR 16.80 (7.59–37.16) |
| Excellent/Very Good/Good opinion of postnatal care | 548 (83.9) | 232 (80.0) | 316 (87.1) | OR 0.63 (0.40–0.98) |
| Women likely to consider having a future pregnancy | 421 (64.5) | 192 (66.2) | 229 (63.1) | OR 1.19 (0.86–1.66) |
| Women currently pregnant | 3 (0.5) | 2 (0.7) | 1 (0.3) | OR 2.54 (0.23–28.19) |
| Women who have changed their family plans | 206 (31.6) | 107 (36.9) | 99 (27.3) | OR 1.59 (1.14–2.23) |
BP blood pressure, GP general practitioner, OR odds ratio
Although temporal trends are visible in Fig. 2, the number of women completing the follow-up questionnaire at 3 months postnatal was substantially smaller (653 women) than the group completing the baseline questionnaire (1751 women).
Analysis of free-text responses (106 from women with HDP, 116 from women with no HDP; Table 5) regarding health and wellbeing in the postnatal period identified both physical and mental health as common themes in both groups: “I was a little disappointed to have to seek help myself in issues with my mental health. I do believe it was due to how I was spoken to and treated by the healthcare professionals…. Now I have sought help myself, I feel much better and enjoying motherhood” (woman with HDP). Another theme that developed was around the support available: “After the regular appointments in pregnancy, you feel rather abandoned after birth” (woman with no HDP).
Table 5.
Thematic framework analysis of free-text open-ended questions
| Themes | Total | Hypertensive in pregnancy | Normotensive in pregnancy |
|---|---|---|---|
| Aspects of recent maternity care that have influenced decision-making around future pregnancies | |||
| Number of women responding | 206 | 107 (51.9) | 99 (48.1) |
| 1. Caesarean section | 21 (10.2) | 16 (15.0) | 5 (5.1) |
| 2. Content with care received | 24 (11.7) | 15 (14.0) | 9 (9.1) |
| 3. Induction of labour | 3 (1.5) | 0 (0.0) | 3 (3.0) |
| 4. Hypertensive disorders of pregnancy | 25 (12.1) | 25 (23.4) | 0 (0.0) |
| 5. Lessons for the future (advocating, change in care, preparedness) | 37 (18.0) | 21 (19.6) | 16 (16.2) |
| 6. Put off by experience/postnatal care | 29 (14.1) | 13 (12.1) | 16 (16.2) |
| Highlighted aspects of postnatal health and well-being | |||
| Number of women responding | 222 | 106 (47.7) | 116 (52.3) |
| 1. Blood pressure and postnatal care | 36 (16.2) | 36 (34.0) | 0 (0.0) |
| 2. Breastfeeding | 10 (4.5) | 0 (0.0) | 10 (8.6) |
| 3. Mental health | 26 (11.7) | 13 (12.3) | 13 (11.2) |
| 4. Physical health | 29 (13.1) | 13 (12.3) | 16 (13.8) |
| 5. Support (including by health care professionals) | 19 (8.6) | 12 (11.3) | 7 (6.0) |
| Views on postnatal care | |||
| Number of women responding | 272 | 129 (47.4) | 143 (52.6) |
| 1. Breastfeeding | 29 (10.7) | 11 (8.5) | 18 (12.6) |
| 2. GP/community care | 72 (26.5) | 39 (30.2) | 33 (23.1) |
| 3. Hospital care | 9 (3.3) | 0 (0.0) | 9 (6.3) |
| 4. Lack of information | 20 (7.4) | 16 (12.4) | 4 (2.8) |
| 5. Postnatal ward | 66 (24.3) | 37 (28.7) | 29 (20.3) |
GP general practitioner
Self-reported postnatal care
Significant differences between the groups in self-reported postnatal care were seen in blood pressure evaluations and medication use in and out of hospital (Table 4, supplementary Table 5). Approximately 9% of women were readmitted to hospital within 3 months postnatally, with re-admission in women with HDP higher (RR 2.41; 95% CI 1.44–4.05) compared with women without, including for blood pressure concerns (RR 7.71; 95% CI 2.69–22.12). One in four women self-monitored their blood pressure postnatally; 43% of women with HDP had ever measured their BP postnatally (compared to 8% of women without HDP; RR 5.47; 95% CI 3.77–7.94) and 25% of women with HDP regularly measured their BP (compared to 2% of women without HDP).
Women’s opinion of their postnatal care was generally high with 84% of all women reporting ‘excellent’, ‘very good’, or ‘good’ care (Table 4, supplementary Table 5).
Analysis of free-text responses (129 from women with HDP, 143 from women without HDP, Table 5) regarding postnatal care identified postnatal ward care as a theme: “The hospital care postnatal was good but felt that the ward was understaffed, especially in regard to support for infant feeding” (woman with no HDP). Primary care and community care were another theme: some women reported positive experiences with family doctors, but several felt that the 6-week postnatal check felt rushed or brief: “I think the check I had at my GP [primary care/family physician] after 6 weeks was not really thorough and when I tried to book an appointment afterwards because I have had pain I couldn’t get one until 3 weeks after and then it was cancelled the day before without giving me a new appointment” (woman with HDP). A third theme was breastfeeding, with references to support both in hospital and in the community: “I feel if the NHS wants to push breastfeeding as the best option for babies and mothers, they need to provide much more aftercare support” (woman with no HDP). The final theme was a lack of or conflicting information, particularly in the HDP group: “I wish I had more information on the impact that high blood pressure can have on my future health and potential pregnancies” (woman with HDP).
On being asked about plans for future pregnancies, 37% of women with HDP had changed their family plans following birth, compared with 27% in women without HDP) (Table 4, supplementary Table 5). This was reflected in free-text responses (107 from women with HDP, 99 from women with no HDP, Table 5): “I’m now scared to become pregnant again, I always wanted more than one child now I’m worried and l will develop pre-eclampsia again” (woman with HDP). In both groups, women also talked more generally about how aspects of their experiences made them less likely to consider becoming pregnant again, but there were also positive comments about lessons for the future. “I would be more aware of postnatal problems. But more aware now that even a not so positive birth is still amazing when you have your baby” (woman with no HDP).
An analysis of maternal demographics, characteristics of birth, and study-specific outcomes captured at postnatal enrolment by responder status (with women defined as ‘responders’ if they had completed the follow-up questionnaire at 3 months postnatal) is shown in supplementary Tables 6, 7 and 8. Whilst the groups are similar in many characteristics, responding participants were more likely (than non-responders) to be of White ethnicity, educated to beyond secondary school level, and to have given birth to their first baby.
Discussion
In this prospective cohort study of women with and without HDP, we found overall postnatal physical and psychological morbidity at 3 months postpartum to be high, with around 90% of the entire cohort reporting some postnatal morbidity at 3 months after birth. There were significant differences in postnatal physical and mental health scores between women with and without HDP in the immediate postnatal period, but these differences converged by 3 months. Screening for symptoms of postnatal depression, using the Whooley questions, showed that at initial antenatal visit, one in fourteen women screened positively (this was higher in women with HDP compared with women without HDP); however, at immediately postnatal nearly one in four women screened positively (significantly higher in women with HDP compared with women without HDP) and then nearly a third of women at 12 weeks postnatal (with no significant differences between the groups). Approximately one in 10 women in this study were readmitted to hospital within the first 3 months after birth, with post birth infections the most commonly reported reason. Approximately 1 in 20 were readmitted due to their blood pressure. Women with HDP were more likely to be readmitted compared to women without, particularly with blood pressure as the reason for admission. In around a quarter of postnatal visits in women with HDP, and around half of visits in women without HDP, women did not have their blood pressure measured. Women with HDP were more likely to change their future pregnancy plans. Some statistically significant differences in outcomes are likely to be under the threshold of a minimally important clinical difference for this population group, such as differences in median EQ-5D visual analogue scale scores. Our sensitivity analysis found that characteristics associated with responder status were in line with other literature. Any significant differences in characteristics by response status were not substantial enough to have invalidated our study findings.
Strengths of this study include the large sample size of diverse women, across a number of maternity units across England (representative of the wider pregnancy population), contributing to the generalisability of the findings in similar health-care settings. The study included women with and without HDP as well as addressing women’s physical and mental co-morbidities together. Further, the study used electronic consent and primarily electronic data capture, a mode of capture appropriate for this population. Ninety-nine percent of women between 16 and 44 years old report ‘daily’ or ‘almost daily’ use of the internet, and 98% report using their mobile phone and smartphone as the most popular device to access the internet on the go [24].
Limitations of the study include the convenience sampling of eligible women identified on the postnatal ward at participating maternity units and therefore there may have been some selection bias in the study population. The study had lower than anticipated retention rates at 3 months postnatal (37% response rate). Although the study team employed strategies to reduce loss to follow-up and used a diverse range of contact options for questionnaire completion reminders, most women did not complete the 3-month follow-up questionnaire. Although smaller studies undertaken by a single dedicated researcher may have higher completion rates, this study was intentionally designed as a large multicentre cohort study. The completion rate is likely to reflect the many competing demands during a woman’s postnatal period and the impact of this on research in the postnatal period, using this methodology, needs to be considered.
A recent review of postnatal mental health following HDP [25] concluded that women with HDP may be at increased risk of developing postpartum depression, anxiety, and post-traumatic stress disorder. Included within this review, Chen et al [26] reported a substantially higher prevalence of postnatal depression than our study, at 27% of 90 women with pre-eclampsia. This discrepancy may be explained by the differences in timing of postnatal data capture (6 weeks compared with 12 weeks) and the EPDS cut-off used (10 or higher compared with 13 or higher). Mautner et al [27] reported similar mean EPDS scores in the immediate postnatal period (EPDS mean 7.83 for women with HDP); however, at 3–4 months postpartum these scores were much lower (EPDS mean 3.67) than we report, a difference that may be explained by the small sample size of 18 women with hypertensive disorders in the study. Notably in our study we had a much larger sample size across a more diverse population, such that we are better able to interpret our findings.
The prevalence of HDP is expected to rise with increasing numbers of pregnant women presenting with risk factors, including older maternal age and obesity [12]. Despite changes in maternal characteristics or case-mix with more complex births, the length of inpatient postnatal stay in the UK is shortening. A study comparing postnatal stay in 92 countries (10 low-income, 42 middle-income and 40 high-income countries) reported that the UK had the shortest mean length of stay for singleton, vaginal births amongst high-income countries [28]. In addition to decline in duration of inpatient stay in UK settings, there has been a reduction in midwifery community-based contacts, likely to reflect reduced healthcare resources rather than maternal need or preference. The implications and impact of reduced postnatal care for both the woman and infant are currently unknown. The most recent UK Confidential Enquiry into Maternal Deaths and Morbidity [29] highlighted that pregnant and postnatal women are still dying from the complications of severe hypertension and the report recommendations reiterate the importance of controlling blood pressure in pregnancy and postpartum.
A 2009–2010 postnatal care survey of first-time mothers conducted by the National Childbirth Trust (n = 1260) documented differing standards of postnatal care and provision as a key issue. This report highlighted women’s lack of involvement in their postnatal care planning and understaffing of postnatal wards (42% of women said there were ‘sometimes or never’ enough midwives to provide them with the care and support on the hospital postnatal ward). In the first month after birth, women highlighted lack of emotional support (61% of women), insufficient physical care (50% of women), inadequate information and advice provided (59% of women) and insufficient support or conflicting advice on infant feeding (55% of women) [30]. This is further supported by one of the key findings of the 2019 Care Quality Commission maternity services survey (n = 17,151) which indicated a poorer experience of postnatal care compared with antenatal and intrapartum care, a finding which is in line with previous years [31]. Although not directly comparable with our study, these findings complement our results with the high level of postnatal morbidity reported by women. A 2013 Royal College of Midwives audit of midwives’ views (n = 2349) reported challenges around the provision of postnatal care, citing organisational pressures as the most influential factor in determining the number of postnatal contacts [32].
Our study highlights this ongoing unmet need in the postnatal period as identified by women, with a missed opportunity for intervention in this period to influence future pregnancies and cardiovascular health, the need to unite physical and mental health, and the challenges of undertaking studies involving postnatal women. Notably around 10% of women reported not attending their postnatal check at 6–8 weeks after birth, highlighting an important gap for these women. Although we found that electronic delivery of study information and questionnaires was acceptable and feasible, in line with other studies [33, 34], this does not overcome the difficulties of reaching women at this time.
Given the study findings, future research should further explore models of postnatal care (contacts and content) starting from initial antenatal visit, how women’s pregnancy health history and plans for care going forward are better communicated to primary care teams and ensuring that women are provided with information around risks, with the opportunity for questions to be addressed about their future health, including future pregnancies. These research recommendations complement a number of the top 10 prioritised research questions documented by the James Lind Alliance priority setting partnership on Hypertension in Pregnancy, including ‘How can we provide better support for women with pregnancy hypertension and their families?’, in which research questions were prioritised by women with lived experience of pregnancy hypertension and healthcare professionals [35]. Despite a recent major policy review of maternity care in England [13] and a specific recommendation in the NHS Long-Term Plan to improve perinatal pelvic floor health [36], much more work is needed to address the gaps in the provision of postnatal care to better meet maternal health needs.
In summary, this study usefully highlights the ongoing current gaps in clinical care and research needs for women with HDP in the postnatal period. If these gaps are to be addressed, review of postnatal policy and research funding priorities are urgently needed.
Supplementary Information
Additional file 1: Supplementary Table 1. Maternal demographics at postnatal enrolment. Supplementary Table 2. Labour, birth, and postnatal characteristics at postnatal enrolment. Supplementary Table 3. Study specific postnatal enrolment baseline characteristics. Supplementary Table 4. Primary and main secondary outcomes at 3 months postnatal. Supplementary Table 5. Postnatal care at 3 months postnatal and opinions on future pregnancies (self-reported). Supplementary Table 6. Maternal demographics at postnatal enrolment by responder status. Supplementary Table 7. Characteristics of labour, birth and post-delivery postnatal stay at postnatal enrolment by responder status. Supplementary Table 8. Study specific outcomes at postnatal enrolment by responder status.
Acknowledgements
We would like to thank all the participating women and site research midwives for their contribution to the study.
BPiPP study group: Elizabeth Bailey, Susan Barnes, Lucy Boustred, Catherine Chmiel, Katherine Clark, Sarah Collins, Alice Lewin, Pippa Nightingale, Chidera Onyeagor, Abby Rand, Gina Short, Sophia Stone, Hayley Tarft and Bonnie Trinder.
Abbreviations
- HDP
Hypertensive Disorders of Pregnancy
- EPDS
Edinburgh Postnatal Depression Scale
- EQ-5D
EuroQol Group five-dimension scale
Authors’ contributions
DB, LCC and DCA were involved in the conception of the study. DCA, SM and LB made a substantial contribution to the running of the study. DCA, LB and PTS did the statistical analysis. DCA, LB and LCC wrote the manuscript with substantial contributions from all other authors when reviewing and revising the manuscript. All authors reviewed, contributed to, and approved the final version of the manuscript.
Funding
This study was funded by Professor Lucy Chappell’s National Institute for Health Research (NIHR) Research Professorship (PR-2014-05-019) and NIHR Applied Research Collaboration South London. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funding bodies had no input into the study design, analysis, write up or interpretation of the study findings.
Availability of data and materials
The dataset generated during the current study will be available to appropriate academic parties on request from the Chief Investigator (LCC) in accordance with the data sharing policies of King’s College London.
Declarations
Ethics approval and consent to participate
Study methods were carried out in accordance with relevant guidelines and regulations. Ethical approval was obtained from the London - South East Research Ethics Committee (REC reference: 18/LO/2084) prior to recruitment. Written informed electronic consent was obtained from all participating women.
Consent for publication
Not applicable (no single identifiable patient).
Competing interests
The authors declare that they have no competing interests.
Footnotes
Names listed under Acknowledgements for inclusion as collaborators.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 2011;25(4):391–403. doi: 10.1016/j.bpobgyn.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301. doi: 10.1136/bmj.g2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buchbinder A, Sibai BM, Caritis S, Macpherson C, Hauth J, Lindheimer MD, et al. Adverse perinatal outcomes are significantly higher in severe gestational hypertension than in mild preeclampsia. Am J Obstet Gynecol. 2002;186(1):66–71. doi: 10.1067/mob.2002.120080. [DOI] [PubMed] [Google Scholar]
- 4.Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376(9741):631–644. doi: 10.1016/S0140-6736(10)60279-6. [DOI] [PubMed] [Google Scholar]
- 5.Say L, Chou D, Gemmill A, Tuncalp O, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–e333. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 6.van Oostwaard MF, Langenveld J, Schuit E, Papatsonis DN, Brown MA, Byaruhanga RN, et al. Recurrence of hypertensive disorders of pregnancy: an individual patient data metaanalysis. Am J Obstet Gynecol. 2015;212(5):624.e1–624.17. doi: 10.1016/j.ajog.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Brown MC, Best KE, Pearce MS, Waugh J, Robson SC, Bell R. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28(1):1–19. doi: 10.1007/s10654-013-9762-6. [DOI] [PubMed] [Google Scholar]
- 8.Leon LJ, McCarthy FP, Direk K, Gonzalez-Izquierdo A, Prieto-Merino D, Casas JP, et al. Preeclampsia and Cardiovascular Disease in a Large UK Pregnancy Cohort of Linked Electronic Health Records: A CALIBER Study. Circulation. 2019;140(13):1050–1060. doi: 10.1161/CIRCULATIONAHA.118.038080. [DOI] [PubMed] [Google Scholar]
- 9.Bick D, MacArthur C, Knight M, Adams C, Nelson-Piercy C, Shakespeare J. Post-pregnancy care: missed opportunities in the reproductive years. In: Annual report of the chief medical officer, 2014, the health of the 51%: women: London: Department of Health; 2015. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/595439/CMO_annual_report_2014.pdf.
- 10.NHS England . Update to the GP contract agreement 2020/21 - 2023/24. 2020. [Google Scholar]
- 11.National Institute for Health and Care Excellence . Postnatal care up to 8 weeks after birth. 2006. [PubMed] [Google Scholar]
- 12.National Institute for Health and Care Excellence . Hypertension in pregnancy: diagnosis and management. London: National Institute for Health and Care Excellence; 2019. [PubMed] [Google Scholar]
- 13.National Maternity Review . BETTER BIRTHS: Improving outcomes of maternity services in England - A Five Year Forward View for maternity care. 2016. [Google Scholar]
- 14.Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998;105(2):156–161. doi: 10.1111/j.1471-0528.1998.tb10045.x. [DOI] [PubMed] [Google Scholar]
- 15.Glazener CM, Abdalla M, Stroud P, Naji S, Templeton A, Russell IT. Postnatal maternal morbidity: extent, causes, prevention and treatment. Br J Obstet Gynaecol. 1995;102(4):282–287. doi: 10.1111/j.1471-0528.1995.tb09132.x. [DOI] [PubMed] [Google Scholar]
- 16.MacArthur C, Lewis M, Knox E. Health after childbirth. London: HM Stationery Office; 1991. [DOI] [PubMed] [Google Scholar]
- 17.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 18.Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ. 2018;27(1):7–22. doi: 10.1002/hec.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual Life Res. 2011;20(10):1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12(7):439–445. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.StataCorp. Stata statistical software: release 16. College Station: StataCorp LLC; 2019. [Google Scholar]
- 22.Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ. 2020;371:m4022. doi: 10.1136/bmj.m4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.QSR International . NVivo qualitative data analysis software, version 12. 2018. [Google Scholar]
- 24.Office for National Statistics . Internet access – households and individuals, Great Britain: 2019. 2019. [Google Scholar]
- 25.Roberts L, Davis GK, Homer CSE. Depression, Anxiety, and post-traumatic stress disorder following a hypertensive disorder of pregnancy: a narrative literature Review. Front Cardiovasc Med. 2019;6:147. doi: 10.3389/fcvm.2019.00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen L, Wang X, Ding Q, Shan N, Qi H. Development of postpartum depression in pregnant women with preeclampsia: a retrospective study. Biomed Res Int. 2019;2019:9601476. doi: 10.1155/2019/9601476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mautner E, Greimel E, Trutnovsky G, Daghofer F, Egger JW, Lang U. Quality of life outcomes in pregnancy and postpartum complicated by hypertensive disorders, gestational diabetes, and preterm birth. J Psychosom Obstet Gynaecol. 2009;30(4):231–237. doi: 10.3109/01674820903254757. [DOI] [PubMed] [Google Scholar]
- 28.Campbell OM, Cegolon L, Macleod D, Benova L. Length of stay after childbirth in 92 countries and associated factors in 30 low- and middle-income countries: compilation of reported data and a cross-sectional analysis from nationally representative surveys. PLoS Med. 2016;13(3):e1001972. doi: 10.1371/journal.pmed.1001972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knight M, Bunch K, Tuffnell D, Shakespeare J, Kotnis R, Kenyon S, et al. Saving lives, improving mothers’ care lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2016–18. 2020. [Google Scholar]
- 30.NCT . Left to your own devices: The postnatal care experiences of 1260 first-time mothers. 2010. [Google Scholar]
- 31.Care Quality Commission . Maternity services survey 2019. 2020. [Google Scholar]
- 32.Royal College Of Midwives . Audit of practice in postnatal care. 2015. [Google Scholar]
- 33.Phillippi JC, Doersam JK, Neal JL, Roumie CL. Electronic informed consent to facilitate recruitment of pregnant women into research. J Obstet Gynecol Neonatal Nurs. 2018;47(4):529–534. doi: 10.1016/j.jogn.2018.04.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Skelton E, Drey N, Rutherford M, Ayers S, Malamateniou C. Electronic consenting for conducting research remotely: a review of current practice and key recommendations for using e-consenting. Int J Med Inform. 2020;143:104271. doi: 10.1016/j.ijmedinf.2020.104271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ho A, Webster L, Bowen L, Creighton F, Findlay S, Gale C, et al. Research priorities for pregnancy hypertension: a UK priority setting partnership with the James Lind Alliance. BMJ Open. 2020;10(7):e036347. doi: 10.1136/bmjopen-2019-036347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.NHS England 2019. The NHS Long Term Plan. 2019. Downloaded from: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table 1. Maternal demographics at postnatal enrolment. Supplementary Table 2. Labour, birth, and postnatal characteristics at postnatal enrolment. Supplementary Table 3. Study specific postnatal enrolment baseline characteristics. Supplementary Table 4. Primary and main secondary outcomes at 3 months postnatal. Supplementary Table 5. Postnatal care at 3 months postnatal and opinions on future pregnancies (self-reported). Supplementary Table 6. Maternal demographics at postnatal enrolment by responder status. Supplementary Table 7. Characteristics of labour, birth and post-delivery postnatal stay at postnatal enrolment by responder status. Supplementary Table 8. Study specific outcomes at postnatal enrolment by responder status.
Data Availability Statement
The dataset generated during the current study will be available to appropriate academic parties on request from the Chief Investigator (LCC) in accordance with the data sharing policies of King’s College London.