Abstract
Background
Suicide attempt and opioid misuse continue to be major behavioral health challenges among American Indians and Alaska Natives (AI/AN). The aim of the study is to evaluate the mediating and moderating role that social support (SS) plays in their association among AI/AN high-school students in New Mexico (NM).
Methods
An aggregated NM Youth Resiliency and Risk Survey (NM-YRRS, 2009-2019: odd years) dataset was used. Multivariable logistic regression modeling and mediation analysis were conducted while adjusting for confounding variables.
Results
Overall, 12.0 and 14.0% of AI/AN students reported opioid misuse and suicide attempt, respectively. The adjusted odds ratio of suicide attempt in students with high SS relative to low SS who misused opioids was 0.43 (p-value = 0.007). The effect of high SS relative to low SS among males who misused opioids was more pronounced (AOR = 0.24, p-value < 0.0001) compared to females (AOR = 0.43, p-value = 0.007). Relative to low SS, high SS was protective for suicide attempt among AI/AN students who misused opioids and attended school in off-reservation (AOR = 0.42, p-value = 0.012) communities, rural communities (AOR = 0.44, p = 0.040), and in communities that are both rural and off-reservation (AOR = 0.39, p = 0.035). Overall, 23.64, and 41.05% of the association between opioid misuse, and suicide attempt was mediated and moderated by SS, respectively. The mediation effect of SS was lowest for rural, on-reservation schools.
Conclusion
More resources need to be allocated to rural on-reservation schools to enhance social support. The study highlights key insights into the significant role SS plays in promoting health and mitigating the association between opioid misuse and suicide attempt.
Introduction
American Indian and Alaska Native (AI/AN) populations have disproportionately higher suicide rates than the overall U.S. population [1, 2]. In the United States (US), suicide deaths occur mainly in midlife [3]; however, AI/AN populations experience the highest suicide rates during adolescence and young adulthood [4–6]. Suicide is the eighth leading cause of death among AI/AN across all ages and the second leading cause of death among those ages 10 – 34 in the US [7]. A national Youth Risk and Behavioral Survey (YRBS) from 1999 to 2015 reported that of all racial groups, AI/AN adolescents had the highest prevalence of lifetime and current use of every substance studied except for heroin, and reported the highest prevalence of attempted suicide, which was almost three times greater than non-Hispanic white adolescents [8]. New Mexico (NM) is among the top four states in the country for suicide deaths [9]. Suicide death rates in NM have been consistently higher than the national average [10]. In particular, the age-adjusted suicide death rate in NM is 23.2 per 100,000 compared to the national average, which was 14.0 per 100,000 in 2017 [10]. Although NM has seen an increase in suicide death in all age groups, from 1999 to 2017, the most significant increase (50%) was among youth 10 – 24 years, from 15.5 to 23.3 deaths per 100,000 [11]. In 2017, 14 and 13% of high school and middle school students in NM reported attempted suicide, respectively [12].
Research has shown that people who use opioids are thirteen times more likely to have suicide ideation [13]. A study among young adult patients admitted for suicide attempt revealed that they were more likely than the healthy control group to have misused opioids in the past year prior to hospitalization after controlling for past suicide attempt [14]. A study of high school students in the U.S. also revealed that adolescents who reported a history of heroin use had the strongest association with suicide attempts compared to peers who never used heroin [15]. In 2017, 14% of US adolescents reported misusing opioids. A more recent study from 2020 reported that adolescents who misuse opioids were 4.9 times more likely to have ever attempted suicide [16].
The opioid overdose death rate among AI/AN rose between 1999 to 2016 from 2.9 per 100,000 to 13.9 per 100,000 [17]. Other risk factors for AI/AN youth opioid misuse include feeling hopeless and sadness [18], and reporting anxiety and depression [19, 20]. Structural factors including years of injustice [21], historical colonization, and other structural determinants of health [22] have marginalized AI/AN communities in ways that affect upstream risk and protective factors and downstream health outcomes. Consequently, AI/AN youth face stark inequities to healthy development [23], and rank higher in health disparities relative to other racial and ethnic groups in the US [24]. Poverty, institutional racism, discrimination, disparities in health care access, health care delivery, and historical trauma play a significant role in the health status of AI/AN [25], including increasing risk for cancer, substance use disorders, obesity, and heart disease compared to the general population [26].
Household socioeconomic status and community traits may play a role in youth behavioral health as well. One measure of socioeconomic status is maternal education, which previous research suggests plays a critical role in suicide attempt and opioid misuse [27]. There is an increased risk for emotional and behavioral disorders among children whose mothers have low educational attainment [28]. A 26-year retrospective review of youth suicide in New Mexico revealed that if left untreated, these emotional and behavioral disorders could lead to increased risk of suicide attempt [29]. Living in a rural community is also associated with increased risks for drug use [30], as well as suicide and self-inflicted injuries [31, 32].
Among AI/AN youth, social support has been found to be a protective factor associated with decreased odds of opioid misuse and suicide attempt [12, 27, 33]. Social support is operationalized in several different ways. For the sake of this study, social support is conceptualized in terms of interpersonal and structural engagements that provide functional support for AI/AN youth. Some social network factors that can protect AI/AN youth behavioral health include a sense of belonging to one’s culture, a strong tribal or spiritual bond, an opportunity to discuss challenges with family or friends, family connectedness, and positive emotional health [34, 35]. Other protective factors include college aspirations and good academic performance [36], positive self-image [35], feeling cared about by adults [37], community factors like participation in sports and clubs [35], and enculturation [38, 39]. In addition, several studies of adolescents reported strong familial attachment [40–42], school connectedness [40, 43], and community characteristics like opportunities to serve and community support groups [44] are associated with lower probability of suicide attempt. However, some social network factors like low parental involvement in the daily activities of the youth, engaging with peers who use illicit substances, and less familial disapproval of substance use can also be risk factors for opioid misuse [19, 45, 46].
The role of social network factors in the relationship between opioid misuse and suicide attempt among AI/AN middle and high school students remains unclear. The extant literature shows that social and familial support are relevant to suicide and substance use for AI/AN adolescents [17, 47–49]. And due to the importance of family and social support, some tribes have integrated cultural support structures into clinical and behavioral therapy [17], and utilized strong family and community connections to mitigate risky health behaviors [33, 50, 51]. Yet, the extent to which social networks may operate as a protective factor modifying the association between opioid misuse and suicide attempt among AI/AN youth is notably lacking. The current study aims to estimate the mediation and moderation effect of social support on the relationship between opioid misuse and suicide attempt among AI/AN youth in New Mexico in order to better understand the role of this key protective factor in AI/AN behavioral health.
Methods
Data source and design
This is a repeated cross-sectional design with deidentified respondents who were not able to be matched between survey years. Aggregated data from 6 years (2009, 2011, 2013, 2015, 2017, and 2019) of the high school New Mexico Youth Risk and Resiliency Survey (NM-YRRS) were obtained from the New Mexico Department of Health (NM-DOH). The NM-YRRS uses a two-stage cluster sampling design to produce a representative sample of high school students in grades 9-12 [52]. However, Albuquerque Area Southwest Tribal Epidemiology Center (AASTEC) assisted in oversampling AI/AN youth to provide a more robust and representative sample of AI/AN students [52]. This study was determined to be exempt by the University of Utah Institutional Review Board (IRB #137165). AASTEC, through NM-DOH, provided the oversampled data for the study after a data-use agreement was signed. A Community Advisory Board (CAB) and AASTEC were instrumental in providing insights into the results and findings of this study. The CAB reviewed the major findings in a meeting and provided feedback on interpretations of the results presented in this study.
Measures
For consistency, only variables asked in all survey years were included in the analysis. The primary outcome of interest was a self-reported indicator (binary 0 or 1) for one or more suicide attempts in the past year. Suicide attempt was obtained by asking the question, “During the past 12 months, how many times did you actually attempt suicide,” with possible responses of zero through six or more times.
The primary exposure variable was opioid misuse, which was obtained through combining the following two questions, “During your lifetime, how many times have you used heroin (also called smack, junk, or China White?” and “During the past 30 days, how many times did you use a painkiller to get high, like Vicodin, OxyContin (also Oxy or OC), or Percocet (also called Percs)?” Combining these two questions gave us the ability to explore the effects of overall misuse involving any non-prescribed opioid [53].
The mediator/moderator variable of interest was social support. The social support construct was developed using eight individual survey questions described in Table 1. The responses to these questions were categorized into “Not true at all or A little true,” and “Pretty much true or Very much true.” A response of “Pretty much true or Very much true” was coded as 1, indicative of positive social support, whereas a response of “Not true at all or A little true” was coded as 0, indicative of negative social support. The final composite scores were then categorized into three levels of social support. A score of three or fewer was classified as “Low Social Support,” a score of four to six was classified as “Moderate Social Support,” and a score of seven and above was categorized as “High Social Support” [27]. Rurality and reservation status were determined by high school location. Specifically, rural and urban areas were determined by population density based on predefined parameters set by the US Census Bureau in 2010, where urban areas have 50,000 or more people and urban clusters have at least 2500 but less than 50,000 people [54]. If a high school was in a census-defined urban area, it was categorized as an urban high school, and if a school was in a census-defined rural area, it was classified as a rural high school. Schools that were adjacent to a reservation or off-reservation were classified as off-reservation schools and schools on tribal lands were classified as on-reservation schools.
Table 1.
Individual social support survey questions
| 1. Parent or adult at home is interested in my school work? | |
| 2. Parent or adult at home believes I will be a success? | |
| 3. Teacher or adult at school listens to me? | |
| 4. Teacher or adult believes I will be a success? | |
| 5. Adult in the community cares about me? | |
| 6. Adult in the community tells me good job? | |
| 7. A friend my own age really cares about me? | |
| 8. When I am not at home, a parent or guardian knows where I am and who I am with? |
Other confounding variables adjusted for in the analyses include age (< 14 years, 15 years, 16 years, and ≥ 17 years), sex (male, female), year (odd years from 2009 to 2019 inclusive), grade (9th, 10th, 11th, and 12th), academic performance (high grades, poor grades), sexual identity (heterosexual/straight, gay/lesbian, bisexual, and questioning), and maternal education (<high school, high school, and college+).
Data analysis
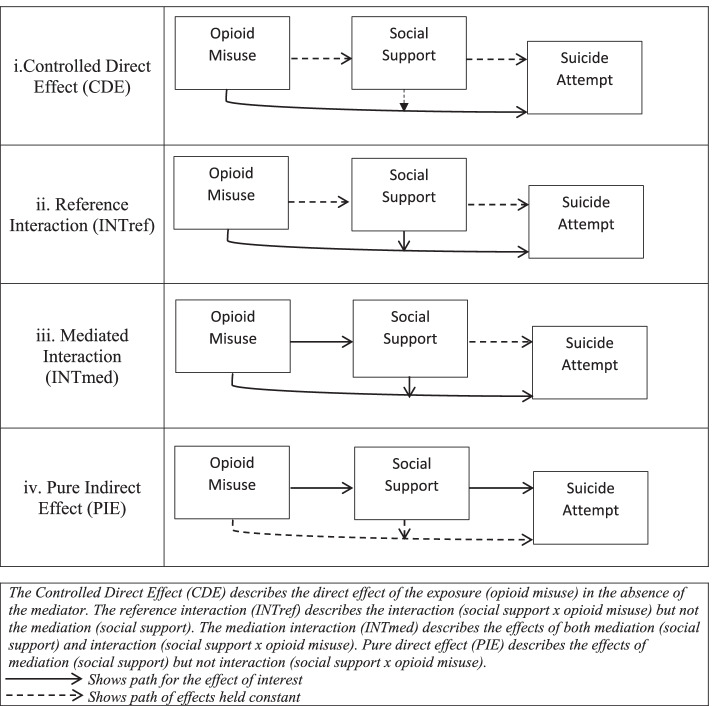
Frequencies and relative frequencies were used for descriptive statistics while accounting for the complex design of the YRRS survey. Multivariable logistic regression modeling was used to estimate the odds of suicide attempt for those who misused opioids relative to those who did not. Further, mediation analysis was employed to assess the mediation/moderation effect of social support on the association between opioid misuse and suicide attempt. In this mediation analysis, the total effect (TE) is expressed in a four-way decomposition as TE = CDE + INTref + INTmed + PIE where (i) controlled direct effect (CDE) captures the percentage of direct effect of the exposure (opioid misuse) in the absence of the mediator (social support); (ii) reference interaction (INTref) captures the percentage of interaction (social support x opioid misuse) but not mediation (social support); (iii) mediated interaction (INTmed) captures the percentage of both mediation (social support) and interaction (social support x opioid misuse); and (iv) pure indirect effect (PIE) captures the percentage of mediation (social support), but not interaction (social support x opioid misuse) [55] (Fig. 1). The mediation analysis was then stratified by sex (males and females), reservation status (attending school on- or off-reservation), rurality (attending school in a rural or urban location), and the combination between on/off reservation status and rurality (attending school in rural off-reservation, rural on-reservation, or urban off-reservation areas). All statistical analyses were performed using Stata 16.1 (StataCorp, 2019) and the SAS 9.4 system (SAS Institute Inc., Cary, NC, USA).
Fig. 1.
Risk model and the four-way decomposition of mediation and interaction analysis. This figure was inspired from Fig. 1 in Bean et al. [40]
Results
Sample characteristics
An aggregated total of 19,067 AI/AN students surveyed from 2009 through 2019 were included in the study. Out of the total participants, 12.0% reported opioid misuse. A slight majority of the students were males (50.6%), and about 28.6% were over 17 years old. Throughout the survey years, a majority of the students attended high schools in rural areas (66.0%) and in off-reservation communities (87.0%). Half (50.3%) of the students had mothers who were high school graduates, and 32.0% had college education. AI/AN students who identified as heterosexual/straight comprised 81.1% of the sample, 2.9% identified as gay or lesbian, 11.4% identified as bisexual, and 4.6% identified as questioning (Table 2). A slight majority of the students received high social support (50.9%). Except for rurality of school and sex of students, imbalance was observed in the demographic variables between those who misused opioids and those who did not (Table 2).
Table 2.
Characteristics of AI/AN youth participants (New Mexico YRRS 2009-2019)
| Total n (%1) |
AI/AN Youth with Opioid Misuse n (%2) |
AI/AN Youth with no Opioid Misuse n (%2) |
P-value | |
|---|---|---|---|---|
| Total | 19,067 (100%) | 2363 (12.0) | 16,704 (88.0) | NA |
| Mediating variable | ||||
| Social Support (SS) | ||||
| Low SS | 3258 (17.5) | 720 (22.0) | 2538 (78.0) | < 0.0001 |
| Moderate SS | 5945 (31.6) | 874 (14.5) | 5071 (85.5) | |
| High SS | 9864 (50.9) | 769 (7.3) | 9095 (92.7) | |
| Control variables | ||||
| Age (years) | ||||
| ≤ 14 | 3826 (20.8) | 361 (8.7) | 3465 (91.3) | 0.0001 |
| 15 | 4936 (26.1) | 612 (12.8) | 4324 (87.2) | |
| 16 | 4899 (24.5) | 640 (12.9) | 4259 (87.1) | |
| ≥ 17 | 5406 (28.6) | 750 (13.4) | 4656 (86.6) | |
| Sex | ||||
| Female | 9807 (49.4) | 1202 (11.8) | 8605 (88.2) | 0.3870 |
| Male | 9260 (50.6) | 1161 (12.5) | 8099 (87.5) | |
| Grade | ||||
| 9th | 5626 (29.9) | 614 (9.8) | 5012 (90.2) | 0.0039 |
| 10th | 5053 (26.7) | 631 (13.2) | 4422 (86.8) | |
| 11th | 4511 (23.0) | 618 (13.3) | 3893 (86.7) | |
| 12th | 3762 (20.4) | 473 (11.9) | 3289 (88.1) | |
| Academic performance | ||||
| High grades (A’s / B’s) | 11,577 (69.0) | 1106 (9.5) | 10,471 (90.5) | < 0.0001 |
| Poor grades (C, D, or F’s) | 5143 (31.0) | 902 (17.0) | 4241 (83.0) | |
| Maternal education level | ||||
| < High School | 2349 (18.0) | 352 (15.6) | 1997 (84.4) | 0.0001 |
| High School | 7534 (50.0) | 864 (10.9) | 6670 (89.1) | |
| ≥ College | 4437 (32.0) | 459 (10.0) | 3978 (90.0) | |
| Sexual identity | ||||
| Heterosexual | 10,633 (81.1) | 869 (8.1) | 9764 (91.9) | < 0.0001 |
| Gay/Lesbian | 353 (2.9) | 107 (29.9) | 246 (70.1) | |
| Bisexual | 1493 (11.4) | 315 (22.1) | 1178 (77.9) | |
| Questioning | 547 (4.6) | 96 (22.4) | 451 (77.6) | |
| Stratifying variables | ||||
| Reservation status of school | ||||
| On | 4066 (13.0) | 484 (10.0) | 3582 (90.0) | 0.041 |
| Off | 14,108 (87.0) | 1767 (12.0) | 12,341 (88.0) | |
| Rurality status of school | ||||
| Rural | 13,782 (66.0) | 1727 (13.0) | 12,055 (87.0) | 0.187 |
| Urban | 4392 (34.0) | 524 (11.0) | 3868 (89.0) | |
The study revealed that higher levels of social support were associated with lower levels of opioid misuse (from 22.0 to 14.5% to 7.3% among students reporting low, moderate, and high social support, respectively). In addition, we observed a higher level of opioid misuse was associated with increasing age (8.7% among those age ≤ 14 years to 13.4% among those age ≥ 17 years). AI/AN students attending off-reservation schools had a higher prevalence of opioid misuse than those on-reservation (12.0% vs. 10.0%), whereas those attending rural schools also had a higher prevalence of opioid misuse than those attending urban schools (13.0% vs. 11.0%--Table 2). A striking disproportionality of opioid misuse was detected among AI/AN students who identified as gay/lesbian (29.9%), bisexual (22.1%), and questioning (22.4%) compared to their heterosexual counterparts (8.1%).
1% = column percentage.
2% = row percentage.
Inferential statistics
In the overall sample using multivariable analysis and controlling for nine potential confounding variables, odds ratios for social support were significant in four models. AI/AN students who reported high social support and no opioid misuse had the lowest odds ratio of suicide attempts (AOR = 0.38; 95% CI: 0.27 – 0.54; p < 0.0001) compared to those with low social support. Students reporting high social support who also reported opioid misuse had significantly lower odds of suicide attempt (AOR = 0.43; 95% CI: 0.23 – 0.79; p = 0.007) compared to those with low social support (Table 3). Male AI/AN students who reported high social support and opioid misuse had a significantly lower odds ratio for suicide attempt (AOR = 0.24; 95% CI: 0.12 – 0.46; p < 0.0001) compared to those with low social support. Likewise, males who reported moderate social support and opioid misuse had a significantly lower odds ratio for suicide attempt (AOR = 0.49; 95% CI: 0.27 – 0.88; p = 0.016) compared to those with low social support. In addition, male students who reported high social support and no opioid misuse had an odds ratio of 0.21 (95% CI: 0.13 – 0.33; p < 0.0001--Table 3) for suicide attempt compared to those with low social support. Overall, no significant associations were found for students who reported moderate social support and either opioid misuse or no opioid misuse relative to those who reported low social support.
Table 3.
Adjusted odds ratios for suicide attempt and the interaction effect of Social Support and Opioid Misuse
| Overall | AOR | 95% CI | P-value |
|---|---|---|---|
| High SS vs Low SS among opioid users | 0.43 | 0.23 – 0.79 | 0.007 |
| High SS vs Low SS among non-opioid users | 0.38 | 0.27 – 0.54 | < 0.0001 |
| Moderate SS vs Low SS among opioid users | 0.89 | 0.53 – 1.50 | 0.662 |
| Moderate SS vs Low SS among Non-opioid users | 0.72 | 0.51 – 1.02 | 0.066 |
| High SS vs Moderate SS among opioid users | 0.48 | 0.29 – 0.79 | 0.004 |
| High SS vs Moderate SS among non-opioid users | 0.52 | 0.39 – 0.71 | < 0.0001 |
| Among Females | |||
| High SS vs Low SS among opioid users | 0.43 | 0.23 – 0.79 | 0.007 |
| High SS vs Low SS among non-opioid users | 0.38 | 0.27 – 0.53 | < 0.0001 |
| Moderate SS vs Low SS among opioid users | 0.89 | 0.53 – 1.50 | 0.662 |
| Moderate SS vs Low SS among Non-opioid users | 0.72 | 0.51 – 1.02 | 0.066 |
| High SS vs Moderate SS among opioid users | 0.48 | 0.29 – 0.79 | 0.004 |
| High SS vs Moderate SS among non-opioid users | 0.52 | 0.39 – 0.71 | < 0.0001 |
| Among Males | |||
| High SS vs Low SS among opioid users | 0.24 | 0.12 – 0.46 | < 0.0001 |
| High SS vs Low SS among non-opioid users | 0.21 | 0.13 – 0.33 | < 0.0001 |
| Moderate SS vs Low SS among opioid users | 0.49 | 0.27 – 0.88 | 0.016 |
| Moderate SS vs Low SS among Non-opioid users | 0.40 | 0.26 – 0.62 | < 0.0001 |
| High SS vs Moderate SS among opioid users | 0.27 | 0.15 – 0.46 | < 0.0001 |
| High SS vs Moderate SS among non-opioid users | 0.29 | 0.19 – 0.43 | < 0.0001 |
| On Reservation | |||
| High SS vs Low SS among opioid users | 0.63 | 0.12 – 3.45 | 0.589 |
| High SS vs Low SS among non-opioid users | 0.37 | 0.20 – 0.68 | 0.002 |
| Moderate SS vs Low SS among opioid users | 0.31 | 0.07 – 1.38 | 0.121 |
| Moderate SS vs Low SS among Non-opioid users | 0.41 | 0.20 – 0.86 | 0.019 |
| High SS vs Moderate SS among opioid users | 2.05 | 0.75 – 5.55 | 0.155 |
| High SS vs Moderate SS among non-opioid users | 0.90 | 0.52 – 1.56 | 0.708 |
| Off Reservation | |||
| High SS vs Low SS among opioid users | 0.42 | 0.21 – 0.82 | 0.012 |
| High SS vs Low SS among non-opioid users | 0.37 | 0.25 – 0.56 | < 0.0001 |
| Moderate SS vs Low SS among opioid users | 1.02 | 0.59 – 1.78 | 0.943 |
| Moderate SS vs Low SS among Non-opioid users | 0.75 | 0.50 – 1.12 | 0.154 |
| High SS vs Moderate SS among opioid users | 0.41 | 0.23 – 0.72 | 0.002 |
| High SS vs Moderate SS among non-opioid users | 0.50 | 0.35 – 0.71 | < 0.0001 |
| Rural high school | |||
| High SS vs Low SS among opioid users | 0.44 | 0.20– 0.96 | 0.040 |
| High SS vs Low SS among non-opioid users | 0.33 | 0.21 – 0.51 | < 0.0001 |
| Moderate SS vs Low SS among opioid users | 0.70 | 0.38 – 1.30 | 0.263 |
| Moderate SS vs Low SS among non-opioid users | 0.66 | 0.42 – 1.03 | 0.067 |
| High SS vs Moderate SS among opioid users | 0.62 | 0.34 – 1.14 | 0.125 |
| High SS vs Moderate SS among non-opioid users | 0.49 | 0.32 – 0.76 | 0.001 |
| Urban high school | |||
| High SS vs Low SS among opioid users | 0.46 | 0.18 – 1.22 | 0.119 |
| High SS vs Low SS among non-opioid users | 0.48 | 0.27– 0.86 | 0.013 |
| Moderate SS vs Low SS among opioid users | 1.62 | 0.64 – 4.13 | 0.303 |
| Moderate SS vs Low SS among non-opioid users | 0.81 | 0.45 – 1.46 | 0.487 |
| High SS vs Moderate SS among opioid users | 0.28 | 0.12 – 0.66 | 0.004 |
| High SS vs Moderate SS among non-opioid users | 0.59 | 0.38 – 0.93 | 0.024 |
| Rural Off Reservation | |||
| High SS vs Low SS among opioid users | 0.39 | 0.16 – 0.93 | 0.035 |
| High SS vs Low SS among non-opioid users | 0.32 | 0.18 – 0.55 | < 0.0001 |
| Moderate SS vs Low SS among opioid users | 0.80 | 0.41 – 1.57 | 0.512 |
| Moderate SS vs Low SS among Non-opioid users | 0.74 | 0.43 – 1.24 | 0.252 |
| High SS vs Moderate SS among opioid users | 0.48 | 0.24 – 0.99 | 0.047 |
| High SS vs Moderate SS among non-opioid users | 0.43 | 0.26 – 0.71 | 0.001 |
| Rural On Reservation | |||
| High SS vs Low SS among opioid users | 0.63 | 0.12 – 3.45 | 0.589 |
| High SS vs Low SS among non-opioid users | 0.37 | 0.20 – 0.68 | 0.002 |
| Moderate SS vs Low SS among opioid users | 0.31 | 0.07 – 1.38 | 0.121 |
| Moderate SS vs Low SS among non-opioid users | 0.41 | 0.20 – 0.86 | 0.019 |
| High SS vs Moderate SS among opioid users | 2.05 | 0.75 – 5.55 | 0.155 |
| High SS vs Moderate SS among non-opioid users | 0.90 | 0.52 – 1.56 | 0.708 |
| Urban Off Reservation | |||
| High SS vs Low SS among opioid users | 0.47 | 0.18 – 1.22 | 0.119 |
| High SS vs Low SS among non-opioid users | 0.48 | 0.27 – 0.86 | 0.013 |
| Moderate SS vs Low SS among opioid users | 1.63 | 0.64 – 4.13 | 0.303 |
| Moderate SS vs Low SS among non-opioid users | 0.81 | 0.45 – 1.46 | 0.487 |
| High SS vs Moderate SS among opioid users | 0.29 | 0.12 – 0.67 | 0.004 |
| High SS vs Moderate SS among non-opioid users | 0.59 | 0.38 – 0.93 | 0.024 |
Reservation and rurality
Students who reported high social support and opioid misuse and attended school off-reservation had a significantly lower odds for suicide attempt (AOR = 0.42; 95% CI: 0.21 – 0.82; p = 0.012) relative to those who reported low social support. A similar significantly lower odds ratio for suicide attempt was found for students who reported high social support and no opioid misuse and attended school on-reservation (AOR = 0.37, 95% CI: 0.20 – 0.68; p = 0.002) compared to those with low social support, and students who reported high social support and no opioid misuse (AOR = 0.37; 95% CI: 0.25 – 0.56; p < 0.0001) compared to those with low social support (Table 3). Students reporting moderate social support and no opioid misuse and attended on-reservation schools had a lower odds ratio for suicide attempt (AOR = 0.41; 95% CI: 0.20-0.86, p = 0.019) relative to students with low social support. For students who attend off-reservation high schools, those who reported high social support and opioid misuse had a significantly lower odds ratio for suicide attempt (AOR = 0.41; 95% CI: 0.23-0.72, p = 0.002) compared to those with moderate social support; whereas students who did not report opioid misuse had an odds ratio of 0.50 (95% CI: 0.35-0.71, p < 0.0001) for suicide attempt.
Among those attending schools on-reservation, no significant associations were found for students who reported high social support and opioid misuse (AOR = 0.63, 95% CI: 0.12-3.45, p = 0.589) relative to those with low social support, students reporting moderate social support and opioid misuse (AOR = 0.31, 95% CI: 0.07-1.38, p = 0.121) compared to those reporting low social support, students who reported high social support and opioid misuse (AOR = 2.05, 95% CI: 0.75-5.55, p = 0.155) compared to those with moderate social support, and students who reported high social support and no opioid misuse (AOR = 0.90, 95% CI: 0.52-1.56, p = 0.708) compared to those with moderate social support. For students who attend off-reservation schools, we did not find significant associations for students who reported moderate social support and either misused opioids (AOR = 1.02, 955 CI: 0.59-1.78, p = 0.943), or did not misuse opioids (AOR = 0.75, 95% CI:0.50-1.12, p = 0.154) compared to those with low social support.
In rural high schools, students who reported high social support and opioid misuse had a significantly lower odds ratio for suicide attempt (AOR = 0.44, 95% CI: 0.20-0.96, p = 0.040), and those who did not report opioid misuse also had a significantly lower odds ratio for suicide attempts (AOR = 0.00, 95% CI: 0.21-0.51, p < 0.0001) compared to those with low social support. Students who reported high social support and no opioid misuse had a significantly lower odds ratio for suicide attempt (AOR = 0.49, 95% CI: 0.32-0.76, p = 0.001) relative to those with moderate social support. In urban high schools, students who reported high social support and no opioid misuse had an odds ratio of 0.48 (95% CI: 0.27-0.86, p = 0.013) for suicide attempt compared to those with low social support. Comparing high social support and moderate social support, students who reported opioid misuse had a significantly lower odds for suicide attempt (AOR = 0.28, 95% CI: 0.12-0.66, p = 0.004), and students who did not report opioid misuse had a significantly lower odds of suicide attempt (AOR = 0.59, 95% CI: 0.38-0.93, p = 0.024).
No significant associations were found for students in rural high schools who reported moderate social support and either opioid misuse or not compared to low social support, and students who reported high social support and opioid misuse compared to moderate social support (Table 3). For students in urban high schools, we also found no significant associations for students who reported high social support and opioid misuse compared to low social support, students who reported moderate social support and either opioid misuse or not compared to those with low social support (Table 3).
Rural off reservation, rural on reservation, and urban off reservation
Students in rural off-reservation schools who reported high social support and either opioid misuse (AOR = 0.39, 95% CI: 0.19-0.93, p = 0.035) or no opioid misuse also had a significantly lower odds ratio for suicide attempt (AOR = 0.32, 95% CI: 0.18-0.55, p < 0.001) compared to those with low social support. In addition, a borderline significantly lower odds for suicide attempt (AOR = 0.48, 95% CI: 0.24-0.99, p = 0.047) was found for students who reported high social support and opioid misuse compared to those with moderate social support. Students who reported high social support and no opioid misuse had a significantly lower odds ratio of 0.43 for suicide attempt (95% CI: 0.26-0.71, p = 0.001) compared to those with moderate social support. In rural on-reservation schools, students who reported high social support and no opioid misuse had a significantly lower odds ratio for suicide attempt (AOR = 0.37, 95% CI: 0.20-0.68, p = 0.002) compared to those with low social support. Likewise, students who reported moderate social support and no opioid misuse also had a significantly lower odds ratio for suicide attempts (AOR = 0.41, 95% CI: 0.20-0.86, p = 0.019) relative to those with low social support. For students in urban off-reservation schools, those who reported high social support and no opioid misuse had a significantly lower odds ratio for suicide attempt (AOR = 0.48, 95% CI: 0.27-0.86, p = 0.013) compared to those with low social support. Comparing high and moderate social support, students who reported opioid misuse and no opioid misuse had a significantly lower odds for suicide attempt (AOR = 0.29, 95% CI: 0.12-0.67, p = 0.004; AOR = 0.59, 95% CI: 0.38-0.93, p = 0.024, respectively).
Comparing moderate social support and low social support for students at rural off- reservation schools, no significant associations were found for students who reported either opioid misuse or no opioid misuse (Table 3). For rural schools on reservations, no significant association was found for students who reported high social support and opioid misuse compared to those with low social support. Comparing moderate social support and low social support, no significant association for suicide attempt was found for students who reported opioid misuse. There were no significant associations for students who reported high social support and opioid misuse, and students who reported high social support and no opioid misuse relative to those who reported moderate social support (Table 3). In urban schools off-reservation, no significant association was found for students who reported high social support and opioid misuse relative to low social support. We also found no significant associations when comparing moderate social support and low social support among students who reported opioid misuse and no opioid misuse (Table 3).
Mediation analysis
Overall, the controlled direct effect (CDE) of opioid misuse on suicide attempt, in the absence of social support was 53.77% (95% CI: 51.01-56.54; p < 0.0001). About 24 % (23.64%) of the association between opioid misuse and suicide attempt (PIE: pure indirect effect) was mediated by social support (95% CI: 21.68 – 25.60; p < 0.0001), and about 41.05% of the association was due to the moderation effect of social support and opioid misuse (95% CI: 38.64 – 43.46; p < 0.0001) (Table 4).
Table 4.
Mediation Analysis for social support on the association between opioid misuse and suicide attempt
| Residency | Opioid Misuse | Social Support | Prevalence of Suicide Attempt (%) | Controlled Direct Effect (CDE): Due Neither to Mediation nor Interaction | Reference Interaction (INTref): Due to Interaction Only | Mediated Interaction (INTmed): Due to Mediation and Interaction | Pure Indirect Effect (PIE): Due to Mediation Only |
|---|---|---|---|---|---|---|---|
| Percent (95% CI) P-value | Percent (95% CI) P-value | Percent (95% CI) P-value | Percent (95% CI) P-value | ||||
| Overall | Yes | low SS | 50.12 | 53.77 (51.01-56.54) p < 0.0001 | 41.05 (38.64-43.46) p < 0.0001 | −18.46 (−19.97--16.95) p < 0.0001 | 23.64 (21.68-25.60) p < 0.0001 |
| Moderate SS | 38.65 | ||||||
| High SS | 23.42 | ||||||
| No | low SS | 18.04 | |||||
| Moderate SS | 11.45 | ||||||
| High SS | 7.42 | ||||||
| Rural on reservation | Yes | low SS | 49.1 | 72.38 (66.14-78.63) p < 0.0001 | 24.12 (18.69-29.56) p < 0.0001 | −13.20 (−16.56- -9.83) p < 0.0001 | 16.69 (12.38-21.00) p < 0.0001 |
| Moderate SS | 34.01 | ||||||
| High SS | 30.25 | ||||||
| No | low SS | 17.31 | |||||
| Moderate SS | 10.37 | ||||||
| High SS | 7.73 | ||||||
| Rural off reservation | Yes | low SS | 51.44 | 43.43 (39.83-47.02) p < 0.0001 | 49.52 (46.47-52.57) p < 0.0001 | −21.25 (−23.43- -19.06) p < 0.0001 | 28.30 (25.33-31.27) p < 0.0001 |
| Moderate SS | 35.14 | ||||||
| High SS | 20.93 | ||||||
| No | low SS | 20.01 | |||||
| Moderate SS | 12.53 | ||||||
| High SS | 6.55 | ||||||
| Urban off reservation | Yes | low SS | 46.79 | 60.36 (54.50-66.21) p < 0.0001 | 36.30 (30.95-41.66) p < 0.0001 | −15.88 (−18.68- -13.08) p < 0.0001 | 19.22 (15.79-22.65) p < 0.0001 |
| Moderate SS | 46.5 | ||||||
| High SS | 25.66 | ||||||
| No | low SS | 15.6 | |||||
| Moderate SS | 9.5 | ||||||
| High SS | 8.17 |
However, restricting the analysis to AI/AN youth who attend rural on-reservation schools, the CDE of opioid misuse on suicide attempt, with no social support was 72.38% (95% CI: 66.14 – 78.63; p < 0.0001). The interaction effect of opioid misuse and social support made up 24.12% (95% CI: 18.69 – 29.56; p < 0.0001) of the total association with suicide attempt whereas mediation made up only 16.69% (95% CI: 12.38 – 21.00; p < 0.0001) of the total association (Table 4).
For students who attended rural off-reservations schools, the effects of opioid misuse on suicide attempt in the absence of social support (CDE) was 43.43% (95% CI: 39.83 – 47.02; p < 0.0001). The interaction effect of opioid misuse and social support contributed about 49.52% (95% CI: 46.47 – 52.57; p < 0.0001) of the total association with suicide attempt whereas the mediation through social support contributed 28.30% (95% CI: 25.33 – 31.27; p < 0.0001).
For students who attended urban off-reservation high schools, the effects of opioid misuse on suicide attempt (CDE) were 60.36% (95% CI: 54.50 – 66.21; p < 0.0001); however, the interaction effect of opioid misuse and social support made up 36.30% (95% CI: 30.95 – 35.66; p < 0.0001) of the total association with suicide attempt (Table 4). The pure indirect effect (PIE) of social support on the association between opioid misuse and suicide attempt was 19.22% (95% CI: 15.79 – 22.65; p < 0.0001).
Discussion
The primary objective of this study was to examine how social support mediates the association between opioid misuse and suicide attempt among AI/AN youth in New Mexico. We found that high social support is broadly protective for suicide attempt, as it is associated with reduction in this risk among AI/AN youth who misuse opioids, as well as those who do not. But the risk reduction was greater among those who did not misuse opioids. This finding is consistent with prior research [33, 35, 46, 51, 56]. Strong familial support, cultural ties, and other social support, such as school personnel have been identified as significant resilience factors in AI/AN communities [18, 27, 46, 51, 53, 57], and some tribes are leveraging these areas as alternatives to interventions that only use clinical and behavioral therapy and to mitigate behavioral health risk [17, 33, 50]. This strengths-based analysis highlights how social connections with family, teachers, friends, and other mentors are key resources in AI/AN communities that improve youth health and should be integrated into behavioral health initiatives targeting youth suicide and substance use interventions.
Whereas our study revealed relatively lower mediation effect of social support on the association between opioid misuse and suicide attempt, the moderation effect of social support and opioid misuse on suicide attempt was relatively more pronounced. The mediation role of social support in the association between opioid misuse and suicide attempt was more profound among AI/AN male youth compared to females. While there was no significant sex difference in opioid misuse among New Mexico AI/AN students in these data, our analysis suggests that social support appears to have different effects. Possible explanations are gender role differences within AI/AN communities in New Mexico. In some communities, male youth may have significant expectations to learn and perpetuate cultural values and traditions and to take up leadership roles. As such, male AI/AN youth may especially benefit from social support as a way to manage community expectations as they learn to fulfill tribal gender roles [58].
Moreover, our study revealed that high social support compared to low social support was more impactful among AI/AN youth who attended schools off-reservation in reducing the risk of suicide attempt for students who misused opioids. Compared to students attending schools in reservation communities, social support had a greater impact on AI/AN youth attending schools outside of the reservation, which may be because they might have adopted some other cultural experiences in addition to the native culture. There is evidence that AI/AN adolescents who have bicultural competence have significantly less hopelessness feelings [59]. More research is needed in this area. In addition, attending off-reservation schools might also grant students access to other healthcare services and other social support systems which might not be available in on-reservation schools. This is more reflective in a study that measured the academic achievement of American Indians and identified some gaps in the academic performance of AI/AN on-reservation compared to those off-reservation [60]. Furthermore, there are more tribal specific dimensions of social support like clan relationships and participating in tribal rituals that might not have been captured using the survey instrument.
Students attending -off-reservation rural schools also demonstrated greater benefit from high social support on the relationship between opioid misuse and suicide attempt than those who attended urban schools. This may be due in part to trends shown in previous research suggesting students who attend urban schools and have high social support still have higher odds of suicide attempt than their counterparts who attend rural schools [27]. While enhancing social support in urban off reservation schools is needed, the highest attention should be for rural on reservation schools.
Increasing social support is critical to improving AI/AN youth behavioral health challenges. Parents or guardians of AI/AN youth should be heavily involved in the day -to-day activities of the youth under their care. This may include engagement with their academic, recreational, and other social activities, which help to create strong positive relationships. Such positive familial environments mediate the negative impact of suicide attempts, and opioid misuse [33, 51]. Schools could also play a critical role in mitigating the risk for suicide attempts and opioid misuse by establishing teen health centers in schools with an on-site mental health counselor, and incorporating behavioral health skills development into the curricula [5], such as teaching students first aid skills for suicide prevention through role-play and group discussions [61]. At the community level, AI/AN elders could collaborate with schools to visit classrooms and help youth connect with their culture, traditions and heritage through elder taught lessons [62], and also connect students to tribal ceremonies [63]. It is imperative that cultural awareness be incorporated into social support programs. Local service providers could coordinate their efforts in data collection and combining local data repository to form a larger dataset across AI/AN communities. This approach would help augment evidence-based research for culturally based suicide prevention and other behavioral health programs [64].
Past studies have highlighted the importance of different levels of social support in adolescent behavioral health [43, 65–67]. Interpersonal levels like individual self-esteem or self-efficacy, positive mood or good emotional health protect AI/AN youth from suicide attempts and other related behavioral health issues [49, 66]. In addition, attention should also be given to other levels of social support such as the societal, and community levels [35]. Exploring the intersection of multiple levels of social support for AI/AN youth has the potential to strengthen intervention programs in ways that not only prevent deaths, but also create environments where youth can thrive [43, 67].
This study has limitations related to the data used for the analysis. First, the study relied on self-reported information and may be subject to recall bias. The self-reported data are not able to measure students who died by suicide, only those who attempted suicide without completing. Second, due to the cross-sectional design of the data, inference about the temporality of the association is not possible; hence we do not imply causation. These data only include students enrolled in school. By 12th grade, youth who were misusing opioids may have dropped out or been expelled from school. In addition, the survey measurements were not validated for AI/AN youth and may not account for important cultural considerations in how social support is perceived and valued. To the best of our knowledge, this is the first study to examine the mediation and moderation effects of social support on the association between opioid misuse and suicide attempt among AI/AN youth in New Mexico. This is a key contribution to behavioral health research in AI/AN communities in the Southwest because it highlights the role community members play in mitigating risk. While many studies highlight the risk for substance use and suicide among AI/AN populations, this study provides estimates of the significant role community resiliency factors play in promoting health.
Future studies should explore the use of culturally validated instruments for measuring substance use, suicide attempts and social support. Moreover, survey respondents were not able to be matched across waves of data collection. A longitudinal study to measure the effectiveness of social support as a mediator of the association between opioid misuse and suicide attempt is highly needed.
Conclusion
Social support mediates the association between opioid misuse, and suicide attempt. High social support relative to low social support was associated with the reduction in the risk of suicide attempt among males, and females who misuse opioids. Among students who misused opioids, high social support relative to low social support was associated with the reduction in the risk of suicide attempt for students who attended high school in off reservation, and rural communities. The mediation effects of social support on the association between opioid misuse and suicide was least among students in rural on-reservation communities. More resources need to be allocated to rural on-reservation communities to enhance social support programs.
Acknowledgements
We thank Dan Green, MPH, New Mexico Department of Health, and the Albuquerque Area Southwest Tribal Epidemiology Center (AASTEC) for providing the AI/AN oversampled NMYRRS data. We also thank the community advisory board for their feedback and expertise on indigenous culture and public health issues related to substance use and suicide with the AI/AN community in New Mexico.
Authors’ contributions
Conceptualization, F.Q.; methodology, F.Q.; formal analysis, F.Q. and D.O.A.; writing—original draft preparation, D.O.A.; writing—review and editing, F.Q., D.O.A., E.F.M., K.E., K.L.V., R.H., and T.P.S.; All authors read and approved the manuscript.
Funding
This work was supported by the National Institutes of Health [3R61DA049382-02S2, 2020]/ National Institute of Neurological Disorders and Stroke (NINDS)]: The moderation effect of social support networks on the relationship between opioid use and suicide attempts among Native American youth in New Mexico.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to restrictions by the New Mexico Department of Health (NMDOH), and the Albuquerque Area Southwest Tribal Epidemiology Center (AASTEC); the providers of the AI/AN oversampled NMYRRS data. Data can be accessed by signing a data sharing agreement with NMDOH and AASTEC (Dr. Kevin English: https://www.aastec.net/; kenglish@aaihb.org).
Declarations
Ethics approval and consent to participate
This study was determined to be exempt by the University of Utah Institutional Review Board (IRB #137165). All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
K.L.V. has a financial conflict of interest management plan through the UNM due to providing consultation and training of evidence-based treatments for addiction for fee. The remaining authors declare that they have no conflicts of interest with respect to the authorship and/or publication of this paper.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Center for Mental Health Services. (2017). Suicide Clusters within American Indian and Alaska Native Communities: A review of the literature and recommendations. [Online] Available: https://store.samhsa.gov/system/files/sma17-5050.pdf
- 2.Centers for Disease Control and Prevention. Suicides among American Indian/Alaska natives — National Violent Death Reporting System. States. 2018;18:2003–14.
- 3.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 112(49):15078–83. 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed]
- 4.SPRC. American Indian and Alaska Natives Populations. https://sprc.org/scope/racial-ethnic-disparities/american-indian-alaska-native-populations (Accessed Jan 2022).
- 5.Hamilton SM, Rolf KA. Suicide in adolescent American Indians: preventative social work programs. Child Adolesc Soc Work J. 2010;27(4):283–290. doi: 10.1007/s10560-010-0204-y. [DOI] [Google Scholar]
- 6.Burrage RL, Gone JP, Momper SL. Urban American Indian community perspectives on resources and challenges for youth suicide prevention. Am J Community Psychol. 2016;58(1-2):136–149. doi: 10.1002/ajcp.12080. [DOI] [PubMed] [Google Scholar]
- 7.CDC. suicide: facts at a glance. Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/pdf/suicide-datasheet-a.pdf (Accessed 2 Mar 2020).
- 8.A. M. Subica, L. T. Wu. Substance use and suicide in Pacific islander, American Indian, and multiracial youth. Am J Prev Med. 2018;54(6):795-805. 10.1016/j.amepre.2018.02.003. [DOI] [PMC free article] [PubMed]
- 9.CDC. Suicide Mortality by State. Centers fo Disease Control and Prevention. https://www.cdc.gov/nchs/pressroom/sosmap/suicide-mortality/suicide.htm (Accessed 18 Mar 2020).
- 10.N. M. D. o. Health. Health Indicator Report of Suicide Death. https://ibis.health.state.nm.us/indicator/view/SuicDeath.Year.NM_US.html (Accessed 12 Nov 2020).
- 11.NM-DOH. Health Indicator Report of Suicide Death. https://ibis.health.state.nm.us/indicator/view/SuicDeath.Year.Age.html (Accessed 3 Mar 2020).
- 12.AASTEC, suicide among American Indian youth in New Mexico. ed: Albuquerque area southwest tribal epidemiology Center, 2017.
- 13.Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies, (in eng). Drug Alcohol Depend. 76:S11–9. 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed]
- 14.Marengo L, et al. Opioid use as a proximal risk factor for suicidal behavior in young adults. Suicide Life Threat Behav. 2021. 10.1111/sltb.12806. [DOI] [PMC free article] [PubMed]
- 15.S. S. Wong, B. Zhou, D. Goebert, and E. S. Hishinuma. The risk of adolescent suicide across patterns of drug use: a nationally representative study of high school students in the United States from 1999 to 2009. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1611-1620. 10.1007/s00127-013-0721-z. [DOI] [PubMed]
- 16.Bhatia D, Mikulich-Gilbertson SK, Sakai JT. Prescription Opioid Misuse and Risky Adolescent Behavior. Pediatrics. 2020;145(2). 10.1542/peds.2019-2470. [DOI] [PubMed]
- 17.R. T. Tipps, G. T. Buzzard, J. A. McDougall. The opioid epidemic in Indian country. J Law Med Ethics. 2018;46(2):422-436. 10.1177/1073110518782950 [DOI] [PubMed]
- 18.Manzo K, Tiesman H, Stewart J, Hobbs GR, Knox SS. A comparison of risk factors associated with suicide ideation/attempts in American Indian and white youth in Montana. Arch Suicide Res. 2015;19(1):89–102. doi: 10.1080/13811118.2013.840254. [DOI] [PubMed] [Google Scholar]
- 19.Vaughn MG, Fu Q, Perron BE, Wu LT. Risk profiles among adolescent nonmedical opioid users in the United States. Addict Behav. 2012;37(8):974–977. doi: 10.1016/j.addbeh.2012.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beauvais F, Jumper-Thurman P, Burnside M. The changing patterns of drug use among American Indian students over the past 30 years, (in eng) Am Indian Alsk Native Ment Health Res. 2008;15(2):15–24. doi: 10.5820/aian.1502.2008.15. [DOI] [PubMed] [Google Scholar]
- 21.Greenfield BL, Venner KL. Review of substance use disorder treatment research in Indian country: future directions to strive toward health equity. Am J Drug Alcohol Abuse. 2012;38(5):483–492. doi: 10.3109/00952990.2012.702170. [DOI] [PubMed] [Google Scholar]
- 22.M. C. Skewes and A. W. Blume. Understanding the link between racial trauma and substance use among American Indians. Am Psychol. 2019;74(1):88-100. 10.1037/amp0000331. [DOI] [PMC free article] [PubMed]
- 23.Guttmannova K, et al. Assessment of risk and protection in native American youth: steps toward conducting culturally relevant, sustainable prevention in Indian country. J Community Psychol. 2017;45(3):346–362. doi: 10.1002/jcop.21852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heart MY, Chase J, Elkins J, Altschul DB. Historical trauma among indigenous peoples of the Americas: concepts, research, and clinical considerations. J Psychoactive Drugs. 2011;43(4):282–290. doi: 10.1080/02791072.2011.628913. [DOI] [PubMed] [Google Scholar]
- 25.W. E. Hartmann, D. C. Wendt, R. L. Burrage, A. Pomerville, J. P. Gone. American Indian historical trauma: anticolonial prescriptions for healing, resilience, and survivance. Am Psychol. 2019;74(1):6-19. 10.1037/amp0000326. [DOI] [PMC free article] [PubMed]
- 26.Cromer KJ, Wofford L, Wyant DK. Barriers to healthcare access facing American Indian and Alaska natives in rural America. J Community Health Nurs. 2019;36(4):165–187. doi: 10.1080/07370016.2019.1665320. [DOI] [PubMed] [Google Scholar]
- 27.Bush A, Qeadan F. Social Support and Its Effects on Attempted Suicide Among American Indian/Alaska Native Youth in New Mexico. Arch Suicide Res. 2019:1–23. 10.1080/13811118.2019.1577779. [DOI] [PubMed]
- 28.McLeod JD, Nonnemaker JM. Poverty and child emotional and behavioral problems: racial/ethnic differences in processes and effects. J Health Soc Behav. 2000;41(2):137–161. doi: 10.2307/2676302. [DOI] [Google Scholar]
- 29.V. D. Singh and S. L. Lathrop. Youth suicide in New Mexico: a 26-year retrospective review, (in eng). J Forensic Sci. 2008; 53(3):703-708. 10.1111/j.1556-4029.2008.00721.x. [DOI] [PubMed]
- 30.Thomas N, van de Ven K, Mulrooney KJD. The impact of rurality on opioid-related harms: a systematic review of qualitative research. Int J Drug Policy. 2020;85:102607. doi: 10.1016/j.drugpo.2019.11.015. [DOI] [PubMed] [Google Scholar]
- 31.Fontanella CA, et al. Widening rural-urban disparities in youth suicides, United States, 1996-2010. JAMA Pediatr. 2015;169(5):466–473. doi: 10.1001/jamapediatrics.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.G. K. Singh, R. E. Azuine, M. Siahpush, M. D. Kogan. All-cause and cause-specific mortality among US youth: socioeconomic and rural-urban disparities and international patterns. J Urban Health. 2013;90(3):388-405. 10.1007/s11524-012-9744-0. [DOI] [PMC free article] [PubMed]
- 33.M. Yu and A. R. Stiffman. Positive family relationships and religious affiliation as mediators between negative environment and illicit drug symptoms in American Indian adolescents, (in eng). Addict Behav. 2010;35(7):694-699. 10.1016/j.addbeh.2010.03.005. [DOI] [PubMed]
- 34.J. Allen, L. Wexler, and S. Rasmus. Protective factors as a unifying framework for strength-based intervention and culturally responsive American Indian and Alaska native suicide prevention. Prev Sci. 2022;23(1):59-72. 10.1007/s11121-021-01265-0. [DOI] [PubMed]
- 35.M. Henson, S. Sabo, A. Trujillo, and N. Teufel-Shone. Identifying protective factors to promote health in American Indian and Alaska native adolescents: a literature review. J Prim Prev. 2017;38(1-2):5-26. 10.1007/s10935-016-0455-2. [DOI] [PMC free article] [PubMed]
- 36.Osilla KC, Lonczak HS, Mail PD, Larimer ME, Marlatt GA. Regular tobacco use among American Indian and Alaska native adolescents: an examination of protective mechanisms, (in eng) J Ethn Subst Abus. 2007;6(3-4):143–153. doi: 10.1300/J233v06n03_06. [DOI] [PubMed] [Google Scholar]
- 37.Barney DD. Risk and Protective Factors for Depression and Health Outcomes in American Indian and Alaska Native Adolescents. Wicazo Sa Review. 2001. [Online]. Available: http://www.jstor.org.ezproxy.lib.utah.edu/stable/1409451;16(1):135–50. 10.1353/wic.2001.0001.
- 38.Mmari KN, Blum RW, Teufel-Shone N. What Increases Risk and Protection for Delinquent Behaviors Among American Indian Youth?:Findings from Three Tribal Communities. Youth Soc. 2010;41(3):382–413. doi: 10.1177/0044118x09333645. [DOI] [Google Scholar]
- 39.Whitbeck LB, Hoyt DR, Stubben JD, LaFromboise T. Traditional Culture and Academic Success among American Indian Children in the Upper Midwest. J Am Indian Educ. 2001;40(2):48–60. [Google Scholar]
- 40.Carter M, McGee R, Taylor B, Williams S. Health outcomes in adolescence: associations with family, friends and school engagement. J Adolesc. 2007;30(1):51–62. doi: 10.1016/j.adolescence.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 41.Maimon D, Browning CR, Brooks-Gunn J. Collective efficacy, family attachment, and urban adolescent suicide attempts. J Health Soc Behav. 2010;51(3):307–324. doi: 10.1177/0022146510377878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Logan JE, Crosby AE, Hamburger ME. Suicidal ideation, friendships with delinquents, social and parental connectedness, and differential associations by sex: findings among high-risk pre/early adolescent population, (in eng) Crisis. 2011;32(6):299–309. doi: 10.1027/0227-5910/a000091. [DOI] [PubMed] [Google Scholar]
- 43.Standley CJ, Foster-Fishman P. Intersectionality, social support, and youth suicidality: a socioecological approach to prevention. Suicide Life Threat Behav. 2021;51(2):203–211. doi: 10.1111/sltb.12695. [DOI] [PubMed] [Google Scholar]
- 44.Allen J, Mohatt GV, Fok CC, Henry D, Burkett R. A protective factors model for alcohol abuse and suicide prevention among Alaska native youth, (in eng) Am J Community Psychol. 2014;54(1-2):125–139. doi: 10.1007/s10464-014-9661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baldwin JA, Brown BG, Wayment HA, Nez RA, Brelsford KM. Culture and context: buffering the relationship between stressful life events and risky behaviors in American Indian youth, (in eng) Subst Use Misuse. 2011;46(11):1380–1394. doi: 10.3109/10826084.2011.592432. [DOI] [PubMed] [Google Scholar]
- 46.Nalven T, Spillane NS, Schick MR. Risk and protective factors for opioid misuse in American Indian adolescents. Drug Alcohol Depend. 2020;206:107736. doi: 10.1016/j.drugalcdep.2019.107736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oetzel J, Duran B, Jiang Y, Lucero J. Social support and social undermining as correlates for alcohol, drug, and mental disorders in American Indian women presenting for primary care at an Indian Health Service hospital, (in eng) J Health Commun. 2007;12(2):187–206. doi: 10.1080/10810730601152771. [DOI] [PubMed] [Google Scholar]
- 48.P. Pokhrel, P. Fagan, K. Cassel, D. R. Trinidad, J. K. Kaholokula, and T. A. Herzog. Social network characteristics, social support, and cigarette smoking among Asian/Pacific islander young adults, (in eng). Am J Community Psychol. 2016;57(3-4):353-365. 10.1002/ajcp.12063. [DOI] [PMC free article] [PubMed]
- 49.Mackin J, Perkins T, Furrer C. The power of protection: a population-based comparison of native and non-native youth suicide attempters, (in eng) Am Indian Alsk Native Ment Health Res. 2012;19(2):20–54. doi: 10.5820/aian.1902.2012.20. [DOI] [PubMed] [Google Scholar]
- 50.Ayunerak P, Alstrom D, Moses C, Charlie J, Sr, Rasmus SM. Yup'ik culture and context in Southwest Alaska: community member perspectives of tradition, social change, and prevention, (in eng) Am J Community Psychol. 2014;54(1-2):91–99. doi: 10.1007/s10464-014-9652-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stiffman AR, Brown E, Freedenthal S, House L, Ostmann E, Yu MS. American Indian youth: personal, familial, and environmental strengths. J Child Fam Stud. 2007;16(3):331–346. doi: 10.1007/s10826-006-9089-y. [DOI] [Google Scholar]
- 52.Agyemang DO, et al. A trend analysis of the prevalence of opioid misuse, social support, and suicide attempt among American Indian/Alaska native high school students in New Mexico: 2009-2019 Youth risk resiliency survey (YRRS). BMC Public Health. 22(1, Feb 21 2022):370. 10.1186/s12889-022-12764-2. [DOI] [PMC free article] [PubMed]
- 53.Qeadan F, et al. Associations between opioid misuse and social relationship factors among American Indian, Alaska Native, and Native Hawaiian college students in the U.S. Drug Alcohol Depend. 2021;222:108667. doi: 10.1016/j.drugalcdep.2021.108667. [DOI] [PubMed] [Google Scholar]
- 54.U. C. Bureau. 2010 Census Urban and Rural Classification and Urban Area Criteria. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html Accessed 03/03, 2022, DOI: 10.4088/PCC.21cr03043.
- 55.T. J. VanderWeele. A unification of mediation and interaction: a 4-way decomposition. Epidemiol. 2014;25(5):749-761. 10.1097/EDE.0000000000000121. [DOI] [PMC free article] [PubMed]
- 56.C. Rees, A. Freng, L. T. Winfree, Jr. The native American adolescent: social network structure and perceptions of alcohol induced social problems. J Youth Adolesc. 2014;43(3):405-425. 10.1007/s10964-013-0018-2. [DOI] [PubMed]
- 57.Kelley A, Witzel M, Fatupaito B. Preventing substance use in American Indian youth: the Case for social support and community connections, (in eng) Subst Use Misuse. 2019;54(5):787–795. doi: 10.1080/10826084.2018.1536724. [DOI] [PubMed] [Google Scholar]
- 58.Shears J, Bubar R, Hall RC. Understanding fathering among urban native American men. Adv Soc Work. 2011;12(2):201–217. doi: 10.18060/468. [DOI] [Google Scholar]
- 59.K. Albright and T. D. Lafromboise. Hopelessness among white- and Indian-identified American Indian adolescents. Cult Divers Ethn Minor Psychol. 2010;16(3):437-442. 10.1037/a0019887. [DOI] [PubMed]
- 60.Fischer S, Stoddard C. The academic achievement of American Indians. Econ Educ Rev. 2013;36:135–152. doi: 10.1016/j.econedurev.2013.05.005. [DOI] [Google Scholar]
- 61.Pham TV, et al. Suicide interventions for American Indian and Alaska native populations: a systematic review of outcomes. SSM - Mental Health. 2021;1. 10.1016/j.ssmmh.2021.100029.
- 62.M. Cwik et al. Let our apache heritage and culture live on forever and teach the young ones": development of the Elders' resilience curriculum, an upstream suicide prevention approach for American Indian youth, (in eng). Am J Community Psychol. 2019;64(1-2): 137-145. 10.1002/ajcp.12351. [DOI] [PubMed]
- 63.Muehlenkamp JJ, Marrone S, Gray JS, Brown DL. A college suicide prevention model for American Indian students. Prof Psychol Res Pract. 2009;40(2):134–140. doi: 10.1037/a0013253. [DOI] [Google Scholar]
- 64.Puneet Chawla S, Sarah K. Culturally appropriate evaluation of tribally based suicide prevention programs: a review of current approaches. Wicazo Sa Review. 2012;27(2):99–127. doi: 10.5749/wicazosareview.27.2.0099. [DOI] [Google Scholar]
- 65.S. D. Golden and J. A. Earp. Social ecological approaches to individuals and their contexts: twenty years of health education & behavior health promotion interventions. Health Educ Behav. 2012;39(3):364-372. 10.1177/1090198111418634. [DOI] [PubMed]
- 66.Perkins DF, Hartless G. An ecological risk-factor examination of suicide ideation and behavior of adolescents. J Adolesc Res. 2002;17(1):3–26. doi: 10.1177/0743558402171001. [DOI] [Google Scholar]
- 67.Standley CJ. Expanding our paradigms: intersectional and socioecological approaches to suicide prevention. Death Stud. 2022;46(1):224–232. doi: 10.1080/07481187.2020.1725934. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to restrictions by the New Mexico Department of Health (NMDOH), and the Albuquerque Area Southwest Tribal Epidemiology Center (AASTEC); the providers of the AI/AN oversampled NMYRRS data. Data can be accessed by signing a data sharing agreement with NMDOH and AASTEC (Dr. Kevin English: https://www.aastec.net/; kenglish@aaihb.org).