Abstract
Purpose
The aim of this study is to review our experience in treating indirect inguinal hernia in pediatric patients.
Methods
We retrospectively studied a total of 43 patients who underwent percutaneous internal ring suturing (PIRS) for indirect inguinal hernia from January 2016 to September 2018. The participants included 29 boys and 14 girls. There were cases of bilateral internal inguinal hernia (n=12), right indirect inguinal hernia (n=16), and left indirect inguinal hernia (n=15). Their mean age was 3.8±2.9 years, and mean body weight was 16 kg. Clinical features and surgical outcomes were analyzed.
Results
Mean operating time was 35 min for unilateral inguinal hernia and 40 min for bilateral inguinal hernia. There were five cases of intraoperative bleeding (12%) during needle insertion. In two cases, stress test resulted in escape of gas into the hernial sac and a second suture was inserted. The contralateral patent processus vaginalis was present in six (14% of cases) and closed. Follow-up was 6~30 months. Mean postoperative hospital stay was 1.2 days. No recurrence hernia and postoperative complications were reported.
Conclusion
Although this study investigated a small number of cases and the surgical experience was rather limited, the PIRS technique was shown to have advantages such as a short learning curve and its aid in detecting contralateral hernias. In this study, there were no reports of recurrence, metachronous inguinal hernias, and postoperative complications.
Keywords: Inguinal hernia, Pediatrics, Laparoscopy
INTRODUCTION
Inguinal hernia is one of the most common surgical disorders in pediatric patients at an incidence of approximately 0.8~4.4%.1 The only treatment method for pediatric hernias is surgical repair, and open herniorrhaphy is currently accepted as the standard procedure in Korea. However, in recent years, laparoscopy has been more frequently used for pediatric inguinal hernia surgery, and studies on laparoscopic surgery are being conducted continuously.2,3
The advantages of laparoscopic surgery are that it can be used to visualize major anatomical structures clearly and examine the contralateral patent processus vaginalis (PPV) and that it poses less risk of injury to the vas deferens or spermatic vessels. Furthermore, bilateral hernia surgery takes less time than laparoscopic surgery and requires a simpler examination for rare hernias such as inguinal or femoral hernia.4-6
Laparoscopic surgery for hernias can be divided into internal and external ligations. In the present study, we performed external ligation of indirect inguinal hernias and analyzed its clinical features and surgical outcomes.
MATERIALS AND METHODS
Fourty-three pediatric patients who underwent hernia repair in the Department of Surgery of ooo Medical Center between January 2016 and September 2018 were evaluated in terms of age, sex, body weight, laterality, operation time, intraoperative complications, postoperative complications, recurrence, metachronous hernia, and length of hospital stay through a medical record review or phone consultations.
At the time of admission, history taking, physical examination, and blood tests were performed for all the pediatric patients with hernia, and approval from the institutional review board of the hospital was obtained.
Surgical method
All surgical procedures were performed under general anesthesia, and basic intra-abdominal gas pressure was set at 10 mmHg, which was increased or decreased depending on the pediatric patient’s age or body weight. A 5-mm trocar was inserted in the umbilicus using Hasson’s technique, which permitted the use of a 5-mm camera inside the abdominal cavity. The camera was used at a field of view of 0° or 30°, and 21-G spinal needles and 4-0 Prolene sutures were used to suture the internal inguinal ring.
In laparoscopic external ligation of inguinal hernia, the surgical procedure first proposed by Patkowski et al.4 is used, and the following procedure was used in the present study. A 21-G spinal needle was prepared with 4-0 Prolene suture inside it (Fig. 1). The end of the suture was pulled to create a loop. A 5-mm trocar was inserted through the umbilical incision, as well as a camera for inspection for an open internal inguinal ring. A 1- to 2-mm skin incision was made over the internal inguinal ring by using blade No. 11. The spinal needle with the suture was positioned through the incision (Fig. 2). After the needle was passed through half of the internal inguinal ring from 12 o’clock direction and positioned in the preperitoneal cavity, it was pushed inside the abdominal cavity in the 6 o’clock position. With caution to prevent the tip of the needle from touching the intestines, forceps were used to slide the suture further into the needle to create a big loop inside the abdominal cavity. When the loop was formed long enough inside the abdominal cavity, the needle was withdrawn carefully while ensuring that the suture loop was not pulled out. After the needle was removed from the suture completely, the needle was inserted in the internal inguinal ring in the 12 o’clock position through the same skin incision, passed through the opposite half of the internal inguinal ring, and then inserted in the abdominal cavity again. After the tip of the needle was passed through the suture loop inside the abdominal cavity, one end of the suture was slid from outside into the needle to insert it in the abdominal cavity lengthwise. With caution to prevent the slide suture from being pulled out while withdrawing the needle, two strands of the suture were pulled together to create a loop. When the loop came up, the tip of the suture inside the abdominal cavity was grasped, and the suture was pulled while checking whether the suture passed circularly around the internal inguinal ring. Then, the suture was tied off firmly outside the abdominal cavity, and whether the internal inguinal ring was closed was checked. The trocar was then removed. Vicryl 4-0 was used to close the peritoneum, muscle, and fascia. Then, Monocyn 5-0 was used to suture the skin. Finally, sterile strips were placed on the 1- to 2-mm incision in the groin (Fig. 3).
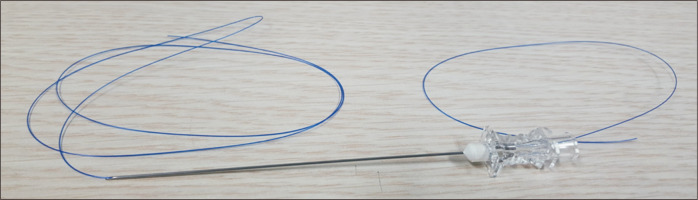
Fig. 1.
Surgical preparation. A 4-0 Prolene suture is inserted in a 21-G spinal needle.
Fig. 2.
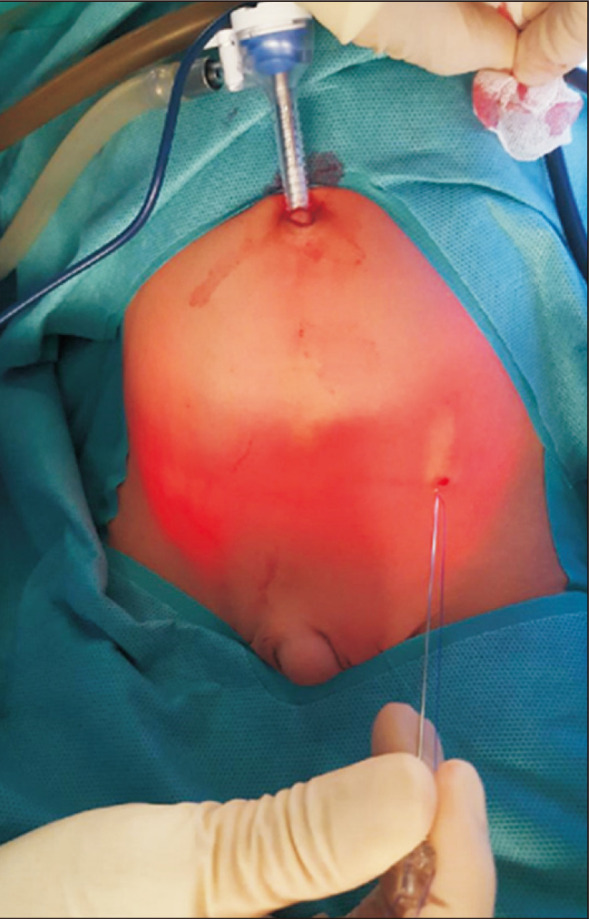
Incision and trocar insertion. A 5-mm trocar is inserted through the umbilical incision, and a 1- to 2-mm skin incision is made above the internal inguinal ring.
Fig. 3.
Operative procedure. (A) An open internal inguinal ring is identified. (B) The needle is inserted in the internal inguinal ring through the inguinal incision. The end of the suture is pulled through the needle to make a loop inside the abdominal cavity. (C) The tip of the needle is passed through the suture loop inside the abdominal cavity. (D) The end of the other tip of the suture is slid from outside into the needle to insert it in the abdominal cavity. (E) The needle is withdrawn, leaving the suture to pass through the loop. (F) Two strands of the suture are pulled together to hook the end of the suture and passed circularly around the internal inguinal ring. (G) The suture is tied off extraperitoneally to close the internal inguinal ring.
RESULTS
Indirect inguinal hernia repair was performed in 43 pediatric patients, including 29 boys (67%) and 14 girls (33%). Their mean age was 3.8±2.9 years and mean body weight was 16 kg. Of the 46 patients, 12 (28%) had bilateral indirect inguinal hernia; 16 (37%), right indirect inguinal hernia; and 15 (35%), left indirect inguinal hernia (Table 1). Laparoscopic surgery was performed in all the patients without conversion to open herniorrhaphy. Contralateral PPV was detected in six cases (14%) and repaired during the study period. The average operation time from skin incision to closure was 35 minutes for unilateral inguinal hernia repair and 40 minutes for bilateral repair. In two cases, gas escaped into the hernial sac because of the stress test performed during surgery, and additional suturing was performed. An additional port was inserted in three cases because of difficulty of inserting the needle in the peritoneum around the internal inguinal ring in two cases and because of gas inflation after hernia sac ligation in one case (Table 2). No complications occurred in all the patients, and the length of their postoperative hospital stay was 1.2 days (31 hours). The follow-up period ranged from 6 to 30 months, during which no recurrent or metachronous hernia was observed (Table 3).
Table 1.
Patients baseline characteristics
| N=43 | |
|---|---|
| Mean age (yr), mean±SD | 3.8±2.9 |
| ≤1 year, no. (%) | 7 (16) |
| Male, no. (%) | 29 (67) |
| Body weight (kg), mean | 16 |
| Laterality, no. (%) | |
| Right | 16 (37) |
| Left | 15 (35) |
| Bilateral | 12 (28) |
Table 2.
Clinical outcome
| N=43 | |
|---|---|
| Mean operation time (min) | |
| Unilateral repair | 35 |
| Bilateral repair | 40 |
| Intraoperative complication, no. (%) | |
| Vas deferens injury | 0 (0) |
| Spermatic vessels injury | 0 (0) |
| Incidental vessels injury | 5 (12) |
| Concomitant repair of unaware contralateral hernia, no. (%) | 6 (14) |
| Right side | 3 (7) |
| Left side | 3 (7) |
| Post op. complication, no. (%) | 0 (0) |
| Hydrocele, Wound infection, Scrotal edema, Testicular atrophy | |
| Metachronous hernia | 0 |
| Recurrence | 0 |
| Post op hospital stay, mean (days) | 1.2 |
| Length of follow-up (months) | 6~30 |
Table 3.
Additional port insertion case
| Case | Age (months) | Sex | Body weight (kg) | Laterality | Operation time (min) | Complications | Postoperative hospital stay |
|---|---|---|---|---|---|---|---|
| 1 | 49 | Boy | 14 | Bilateral | 55 | As it was confirmed that gas was escaping into the left hernial sac, a 3-mm port was inserted in RLQ, the ligated suture was cut off, and PIRS was performed again. | 1 |
| 2 | 3 | Boy | 7.5 | Right | 50 | Difficulties to get through the peritoneum resulted in bleeding, a 3-mm port was inserted additionally on the left side, and the internal ring was sutured in the purse string method. | 0 |
| 3 | 33 | Boy | 17 | Right | 25 | A 3-mm port was additionally drilled on the left side as the peritoneum could not be passed through. | 1 |
DISCUSSION
The use of laparoscopy is increasing in pediatric hernia surgery, as it reduces the incidence of metachronous hernia, takes less time, improves recovery, and has cosmetic advantages.1,7 In Korea, however, laparoscopic surgery has not been used frequently in pediatric hernia surgery, and only few studies have reported on this topic. Hence, this study reports the clinical features and surgical outcomes of laparoscopic external ligation of pediatric indirect inguinal hernias to contribute to the progress of laparoscopic surgery for pediatric hernias in Korea.
Pediatric inguinal hernia repair using open herniorrhaphy requires an accurate understanding of the procedure, has a difficulty in checking anatomical structures due to the narrow surgical field of view, and involves a delicate operation to avoid damage to the vas deferens and blood vessels. The advantages of laparoscopic surgery, however, are that it makes observation of major anatomical structures easier and reduces damage to the vas deferens and blood vessels by minimizing handling it.8
Laparoscopic surgery involves internal and external ligations. In internal ligations, operating inside an infant’s small abdominal cavity is difficult and requires enough experience and skill to suture the internal inguinal ring properly. Patkowski introduced the percutaneous internal ring suturing (PIRS) to minimize complications from intra-abdominal suturing more easily. Since its introduction, PIRS has been adapted in various ways and used broadly for pediatric inguinal hernia surgery, and its outcomes have been widely reported.3 PIRS is a surgical technique that is easier to learn than intra-abdominal suturing, takes less operation time, and is comparable with intra-abdominal suturing with respect to the risk of complications or recurrences.1
The recurrence rate after pediatric inguinal hernia surgery was 0~6% after open herniorrhaph, 0~15.5% after laparoscopic surgery, and recurrences occurred mostly within 1 year after surgery.1,7,9,10 In this study, none of the patients had a recurrence during the follow-up period.
The average operation time in the present study was 35 minutes for unilateral hernias and 40 minutes for bilateral hernias, confirming the shorter operation time in PIRS than in the 25 cases of open herniorrhaphy performed for inguinal hernias in the same hospital by same surgeon between January 2014 and January 2016 (Table 4). As no wound infections or damage to the vas deferens or spermatic vessels was observed and no recurrence or complications occurred during the follow-up, we suggest that this surgical method can be applied easily and safely. PIRS has the same advantages of other laparoscopic surgery. An advantage of laparoscopic surgery is that it allows checking for and repair of undetected contralateral hernia at the same time, thereby reducing the incidence of metachronous hernias. A previous study reported that the incidence of metachronous hernias was 3.6~12% after open herniorrhaphy and 0~0.9% after laparoscopic surgery.11,12 As for the causes, Miyake et al. described possibilities that (1) the contralateral PPV is blocked or covered due to peritoneal wrinkles when intra-abdominal air is present or (2) an acquired hernia or intra-abdominal air overinflates the PPV like a parachute, contributing to a contralateral hernia.13 Sumida et al. highlighted that an irregular orifice may cause metachronous hernias and that close observation and checking of the contralateral PPV are important.14 The present study confirmed that 3 (6%) of the patients had a medical history of open herniorrhaphy for contralateral inguinal hernia and that 6 (12%) had contralateral PPV during surgery. While opinions vary on whether observation of the contralateral PPV is necessary during laparoscopic surgery, ligation takes a short time and has a low incidence of complications.15,16 Hence, in the present study, all cases were ligated regardless of diameter or length, and no metachronous hernia was reported during the follow-up period.
Table 4.
Baseline characteristics according to the surgical method
| Variable | Laparoscopic (2016.01~2018.09) n=43 | Open (2014.01~2016.01) n=25 | p |
|---|---|---|---|
| Mean age, (months) | 45.8±34.8 | 43.0±31.2 | 0.743 |
| Female, no. (%) | 25 (58) | 6 (24) | 0.006 |
| Bilateral presentation, no. (%) | 12 (28) | 2 (8) | 0.050 |
| Hospital day, median (range) | 2 (1~3) | 2 (1~3) | 0.183 |
| Operation time (minute), median (range) | 35 (10~75) | 45 (25~100) | 0.012 |
| Intraoperative complications, no. (%) | 5 (11) | 0 (0) | 0.077 |
Other non-spermatic vessels were pricked, leading to complications in 12% of the cases, which were resolved by external compression or spontaneously (Table 5). No additional surgery was required, and no postoperative complications were observed. Two patients had additional suturing due to the gas escaped into the hernial sac, which was resolved by resuturing or additional suturing. As PIRS mostly uses only one port for camera or another one for assist forcep, it has excellent cosmetic results but pricked blood vessels or incomplete purse strings have been reported. One-puncture technique and saline hydrodissection have been introduced as part of an effort to reduce the incidence of the aforementioned complications. In the one-puncture technique, an insertion is made in the same area when suturing the internal inguinal ring to prevent other tissues from being sutured unnecessarily and to reduce recurrence. The present study also performed saline injection to prevent incidental vessel pricking later in the procedure and make it easier to enter between the peritoneum and vessels. While it helped avoid injury to the spermatic vessels or vas deferens at the bottom of the internal inguinal ring, it inflated the peritoneum on the left and right sides and visually interfered with the internal inguinal ring in some cases when saline was not accurately injected. Basic intra-abdominal pressure during surgery was set as 10 mmHg and fluctuated depending on the patient’s body weight and abdominal cavity size. Increasing gas pressure by 2 mmHg to widen the internal inguinal ring was helpful when suturing the internal inguinal ring. As the infants were small, it was easier for the surgeon to stand on the side opposite to the hernia to use the right hand while performing the procedure. Checking whether an infant has urinated before surgery is necessary because an inflated bladder restricts the field of view because of the infant’s small abdominal cavity. A further option would be to tilt the bed and move the intestines to the opposite side when the internal inguinal ring is visually obstructed.
Table 5.
Incidental vessel injury case
| Case | Age (months) | Sex | Body weight (kg) | Laterality | Operation time (min) | Complications | Postoperative hospital stay |
|---|---|---|---|---|---|---|---|
| 1 | 8 | Girl | 9.4 | Right | 50 | Hematoma due to femoral vein injury | 1 |
| 2 | 49 | Boy | 16 | Left | 30 | Abdominal wall vessel injury during needle insertion | 1 |
| 3 | 33 | Boy | 14 | Right | 45 | Inferior epigastric vessel injury while closing an internal opening | 1 |
| 4 | 132 | Boy | 34 | Right | 30 | Abdominal wall vessel injury during needle insertion | 1 |
| 5 | 3 | Boy | 7.5 | Right | 50 | Peritoneum vessel injury during needle insertion | 0 |
Limitations
The present study has some limitations, including the small number of patients and the fact that the surgical procedures were performed at a single center by the same surgeon. Moreover, the evaluation of recurrent and metachronous hernias was limited because the follow-up period was not long enough.
CONCLUSION
Percutaneous internal ring suturing can be applied easily and safely in pediatric indirect inguinal hernias, as its associated recurrence and postoperative complication rates are low. Furthermore, as it has another advantage of detecting and treating previously undetected contralateral hernias, more studies must be conducted in Korea to widen the application of this surgical method.
ACKNOWLEDGMENTS
None.
Footnotes
AUTHORS’ CONTRIBUTIONS
Conceptualization: YJK. Formal analysis: CHK. Methodology: CHK, YJK. Writing-original draft: CHK, YJK. Writing-review and editing: YJK, KTK.
CONFLICT OF INTEREST
None.
FUNDING
None.
REFERENCES
- 1).Esposito C, St Peter SD, Escolino M, Juang D, Settimi A, Holcomb GW, 3rd Laparoscopic versus open inguinal hernia repair in pediatric patients: a systematic review. J Laparoendosc Adv Surg Tech A. 2014;24:811–818. doi: 10.1089/lap.2014.0194. [DOI] [PubMed] [Google Scholar]
- 2).Han SR, Kim HJ, Kim NH, et al. Inguinal hernia surgery in Korea: nationwide data from 2007-2015. Ann Surg Treat Res. 2019;97:41–47. doi: 10.4174/astr.2019.97.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Dreuning K, Maat S, Twisk J, van Heurn E, Derikx J. Laparoscopic versus open pediatric inguinal hernia repair: state-of-the-art comparison and future perspectives from a meta-analysis. Surg Endosc. 2019;33:3177–3191. doi: 10.1007/s00464-019-06960-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Patkowski D, Czernik J, Chrzan R, Jaworski W, Apoznanski W. Percutaneous internal ring suturing: a simple minimally invasive technique for inguinal hernia repair in children. J Laparoendosc Adv Surg Tech A. 2006;16:513–517. doi: 10.1089/lap.2006.16.513. [DOI] [PubMed] [Google Scholar]
- 5).Parelkar SV, Oak S, Gupta R, et al. Laparoscopic inguinal hernia repair in the pediatric age group--experience with 437 children. J Pediatr Surg. 2010;45:789–792. doi: 10.1016/j.jpedsurg.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 6).Giseke S, Glass M, Tapadar P, Matthyssens L, Philippe P. A true laparoscopic herniotomy in children: evaluation of long-term outcome. J Laparoendosc Adv Surg Tech A. 2010;20:191–194. doi: 10.1089/lap.2009.0069. [DOI] [PubMed] [Google Scholar]
- 7).Yang C, Zhang H, Pu J, Mei H, Zheng L, Tong Q. Laparoscopic vs open herniorrhaphy in the management of pediatric inguinal hernia: a systemic review and meta-analysis. J Pediatr Surg. 2011;46:1824–1834. doi: 10.1016/j.jpedsurg.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 8).Shalaby R, Ismail M, Samaha A, et al. Laparoscopic inguinal hernia repair; experience with 874 children. J Pediatr Surg. 2014;49:460–464. doi: 10.1016/j.jpedsurg.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 9).Xiang B, Jin S, Zhong L, Li F, Jiang X, Xu Z. Reasons for Recurrence After the Laparoscopic Repair of Indirect Inguinal Hernia in Children. J Laparoendosc Adv Surg Tech A. 2015;25:681–683. doi: 10.1089/lap.2014.0401. [DOI] [PubMed] [Google Scholar]
- 10).Taylor K, Sonderman KA, Wolf LL, et al. Hernia recurrence following inguinal hernia repair in children. J Pediatr Surg. 2018;53:2214–2218. doi: 10.1016/j.jpedsurg.2018.03.021. [DOI] [PubMed] [Google Scholar]
- 11).Hamad MA, Osman MA, Abdelhamed M. Laparoscopic-assisted percutaneous internal ring ligation in children. Ann Pediatr Surg. 2011;7:66–69. doi: 10.1097/01.XPS.0000396410.14046.a7. [DOI] [Google Scholar]
- 12).Tam YH, Wong YS, Pang KK, et al. Unexpected metachronous hernia development in children following laparoscopic unilateral hernia repair with negative evaluation for contralateral patent processus vaginalis. J Laparoendosc Adv Surg Tech A. 2013;23:287–290. doi: 10.1089/lap.2012.0365. [DOI] [PubMed] [Google Scholar]
- 13).Miyake H, Fukumoto K, Yamoto M, et al. Risk factors for recurrence and contralateral inguinal hernia after laparoscopic percutaneous extraperitoneal closure for pediatric inguinal hernia. J Pediatr Surg. 2017;52:317–321. doi: 10.1016/j.jpedsurg.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 14).Sumida W, Watanabe Y, Takasu H, Oshima K, Komatsuzaki N. Effects of insistent screening for contralateral patent processus vaginalis in laparoscopic percutaneous extraperitoneal closure to prevent metachronous contralateral onset of pediatric inguinal hernia. Surg Today. 2016;46:569–574. doi: 10.1007/s00595-015-1199-y. [DOI] [PubMed] [Google Scholar]
- 15).International Pediatric Endosurgery Group. IPEG Guidelines for Inguinal Hernia and Hydrocele. J Laparoendosc Adv Surg Tech A. 2010;20:x–xiv. doi: 10.1089/lap.2010.9998. [DOI] [PubMed] [Google Scholar]
- 16).Chong AJ, Fevrier HB, Herrinton LJ. Long-term follow-up of pediatric open and laparoscopic inguinal hernia repair. J Pediatr Surg. 2019;54:2138–2144. doi: 10.1016/j.jpedsurg.2019.01.064. [DOI] [PubMed] [Google Scholar]