Abstract
Objective:
To evaluate the accuracy and precision of cone beam computed tomography (CBCT) with regard to measurements of root length and marginal bone level in vitro and in vivo during the course of orthodontic treatment.
Materials and Methods:
Thirteen patients (aged 12–18 years) from an ongoing study and a dry skull were examined with CBCT using multiplanar reformatting for measurements of root length and marginal bone level. For in vivo evaluation of changes in root length, an index according to Malmgren et al was used, along with a modification of this method.
Results:
The in vitro mean difference between physical and radiographic measurements was 0.05 mm (SD 0.75) for root length and −0.04 mm (SD 0.54) for marginal bone level. In vivo the error was <0.35 mm for root length determinations and <0.40 mm for marginal bone level assessments.
Conclusion:
Despite changes in tooth positions, the CBCT technique yields a high level of reproducibility, enhancing its usefulness in orthodontic research.
Keywords: CBCT, Root length, Marginal bone level, Orthodontic treatment
INTRODUCTION
Orthodontically induced inflammatory root resorption (OIIRR) is an adverse effect of orthodontic treatment1 that might jeopardize an otherwise positive treatment outcome. The incidence of OIIRR among individuals having undergone orthodontic treatment differs between studies as a result of the techniques used to quantify the degree of OIIRR.2
In most studies of OIIRR intraoral radiography has been used.3 Even with efforts to obtain periodically identical radiographs,4,5 intraoral radiography has shortcomings.6–9 Follin and Lindvall10 found that in order to be observed in intraoral radiographs, the resorption has to cause a shortening of the root. Panoramic radiography has also been used to assess root shortening. This technique is sensitive to patient positioning, and even under optimal conditions the radiographs are fraught with uncertainties, particularly in the anterior jaw regions. In individuals with Angle Class II malocclusions, optimal visualization of both jaws is difficult.11
Computed tomography (CT) has become the method of choice for demanding imaging tasks. Higher costs and higher radiation doses have prevented CT from becoming a standard tool in dental imaging and, thus, in studies of OIIRR, despite its inherent capabilities. In the 1990s CBCT12 was introduced in dentistry. Dosimetric examinations have shown considerably lower doses from CBCT than from CT,13 although they vary between CBCT units and parameters used.14,15 Because of the high spatial resolution, low radiation doses, and relative affordability of this technique, it has gained widespread acceptance in dentistry16 and in orthodontics.17 The ability to provide distortion-free slice images of single roots provides excellent possibilities to study root resorption.
Our study aims to evaluate in vitro the accuracy and precision of CBCT with regard to measurements of root length and marginal bone level as well as the precision with which such measurements can be made in vivo.
MATERIALS AND METHODS
Subjects and Study Material
To evaluate accuracy and precision of root length and marginal bone level assessments in vitro we used a dry human skull. For the in vivo assessment of precision we used radiographs from patients in an ongoing study. The study comprised 13 patients, 7 boys and 6 girls (aged 12–18 years), participating in a study of root shortening and marginal bone level alterations during orthodontic treatment. All were diagnosed with a Class I malocclusion with crowding and were subjected to treatment comprising extraction of one premolar in each jaw quadrant and fixed appliances in both jaws. Informed consent from the patients' parents and ethical approval from the Ethics Committee at the Sahlgrenska Academy, University of Gothenburg, were obtained. Subjects were randomly chosen from patients having completed three radiographic examinations (baseline, 6-month, and end-point). Two teeth per subject and tooth group (first molar, premolar, canine, and lateral and central incisors) and one root from multi-rooted teeth were randomly chosen, providing representative samples of roots from all tooth groups.
For in vitro dry skull assessments five teeth were chosen from the upper right and five from the lower left quadrant as having no periodontal bone loss and normal root lengths. Incisors, canines, second premolars, and first molars were chosen, corresponding to the teeth examined in the patients.
Examination
A 60 × 60–mm volume was examined using 3D Accuitomo FPD (J. Morita Mfg Corp, Kyoto, Japan), a 360° rotation, and exposure parameters of 17.5 seconds, 75 kV, and 4-5.5 mA, based on subject size. Examinations were made so that the incisors to the first molars became contained in one volume. To mimic soft tissues the dry skull was immersed in water contained in a Plexiglas bowl, placed on a stand so that it could be positioned as would be a patient's head.
Data Processing
Primary data reconstructions were made by acquisition software (i-Dixel-3DX, 3D, Version 1.691, J Morita Mfg Corp) at the Accuitomo workstation providing axial, frontal, and sagittal views. Secondary reconstruction was then made using the i-Dixel software to obtain a slice thickness and interval of 0.5 mm. Using DICOM export axial slices were sent to PACS for later reformatting.
Workstation/Equipment
A workstation with Sectra IDS5 (Sectra Imtec AB, Linköping, Sweden) PACS Multi Planar Reconstruction was used for reformatting and viewing of axial slices. The workstation comprised a DELL computer (Optiplex 755, DELL AB, Stockholm, Sweden) with a graphic card (NVIDIA GeForce 6800 Series GPU 32-bit, Matrox MED2mp-DVI) and 20-inch flat-panel monitors. All measurements were performed on one of two monochromatic screens (OLÒRIN Medic Line ML 187D TFT-LCD, Olorin AB, Kungsbacka, Sweden) with a resolution of 1280 × 1024 pixels.
Reformatting and Measurements
Reformatting was completed so that the long axis of the tooth/root became parallel to the axes of two perpendicular, vertical image planes. This provided optimal visualization of the tooth/root in axial, coronal, and sagittal planes. Root length measurements were made along the axis of the root. The marginal bone level was assessed perpendicular to a line between the buccal and lingual cemento-enamel junction (CEJ) and the mesial and distal CEJ, respectively (Figure 1). One observer made all measurements with intervals of at least 2 days. The patient radiographs were measured twice and those of the skull five times. Direct measurements on the latter were performed after the radiographs had been taken. The bone level was marked with a thin pencil and each tooth was gently removed. The bone level and root length were measured five times using a digital caliper (Clas Ohlson, Sweden AB, resolution 0.01 mm; accuracy, ±0.03 mm for distances >100–200 mm). Measurements were taken from the CEJ to the most apical part of the bone level at the buccal, palatal/lingual, mesial, and distal aspects of the tooth. The root length was measured along the axis of the root, perpendicular to an imaginary line between the buccal and palatal/lingual CEJ.
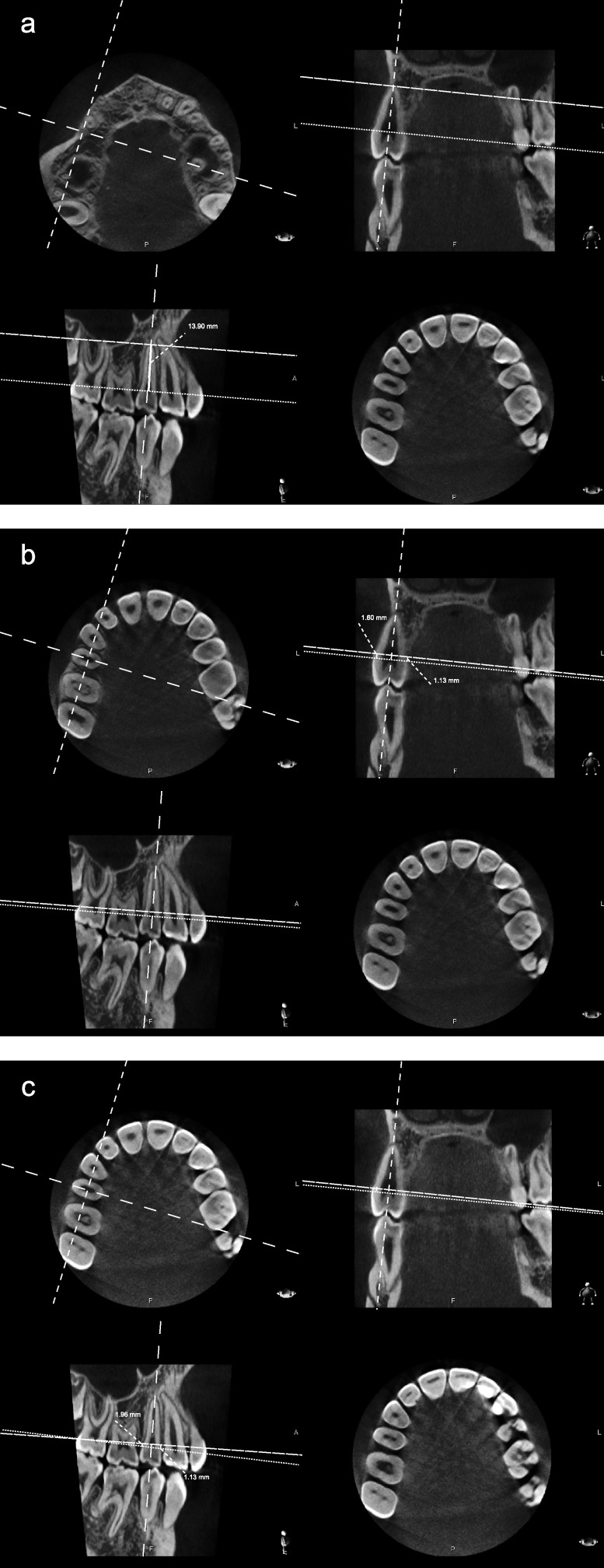
Figure 1.
Measurement procedure for assessment of root length and marginal bone level by means of reformatted images in axial, sagittal, and coronal planes. (a) Root length—measurement from a reference line between buccal and palatal cemento-enamel junction (CEJ) to apex. The levels of CEJ and root apex were assessed using a combination of axial, sagittal, and coronal images. (b) Buccal and palatal/lingual bone levels—measurement in frontal and/or axial views from a reference line at CEJ, according to Figure 1a, to the buccal and palatal/lingual marginal bone crest, respectively. (c) Mesial and distal bone levels—measurement from a reference line at CEJ to the mesial and distal marginal bone crest, respectively. An adjusted axial view was used to determine the level of the reference line between the mesial and distal CEJ.
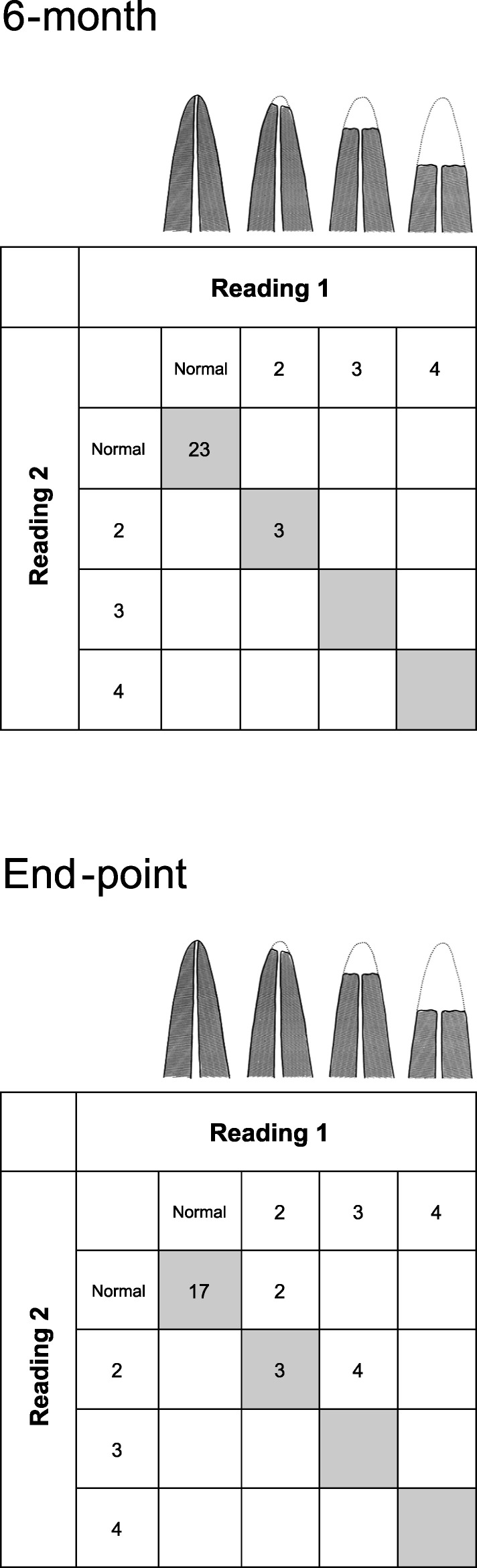
Index
For in vivo assessments of root length we also used an index by Malmgren et al.18 The index (Figure 2) comprises four scores, thus: 1 = irregular root contour, 2 = root resorption apically amounting to <2 mm (minor resorption), 3 = root resorption from 2 mm to ⅓ of the original root length (severe resorption), and 4 = root resorption >⅓ of the original root length (extreme resorption). Score 1 was excluded because irregular root contour was noted at teeth already at baseline (ie, before the start of treatment). To describe a surface resorption of the buccal, palatal/lingual, mesial, or distal part of the apex that did not result in root shortening a modification of the index was used (Figure 3).
Figure 2.
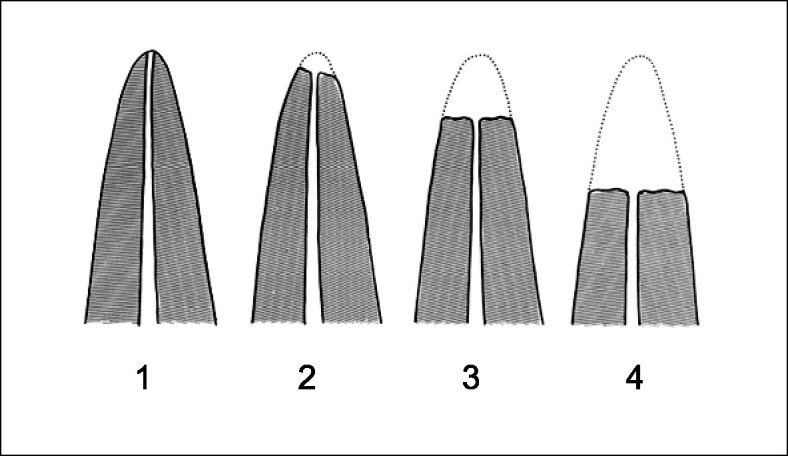
Index according to Malmgren et al.18 1 indicates irregular root contour; 2, minor resorption; 3, severe resorption; and 4, extreme resorption.
Figure 3.
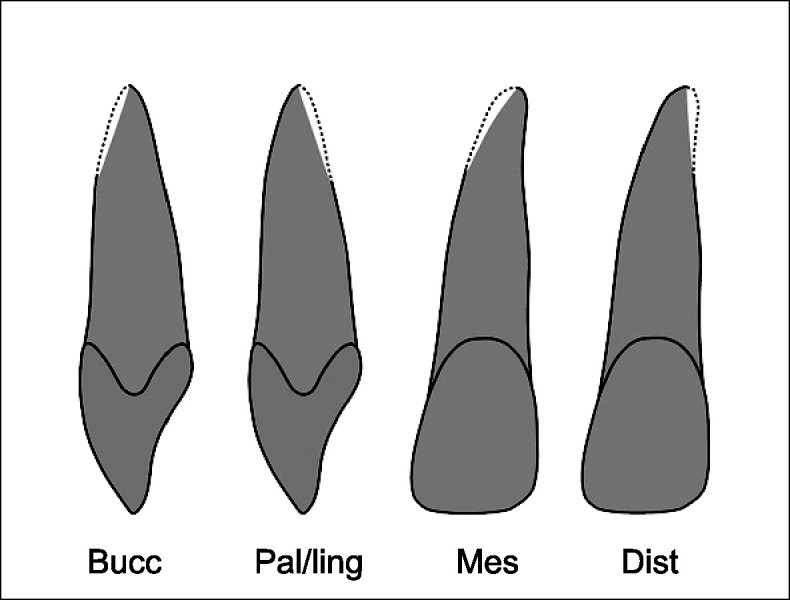
Modified index for describing slanted surface resorptions at buccal, palatal/lingual, and mesial and distal surfaces at the root apex.
Statistics
For in vitro root length measurements we used descriptive statistics presenting mean values and standard deviations for the direct physical measurements vs those from radiographs. For comparisons between direct and radiographic marginal bone level measurements we studied their mean deviations from zero and associated standard deviations. The Student's paired t-test was used for significance testing, with P < .05 as the cutoff value. The measurement error of in vivo assessments of root length and bone level from radiographs was calculated from duplicate determinations using the formula s = √∑d2/2n, according to Dahlberg,19 where d = difference between duplicate determinations and n = number of determinations. To evaluate differences between reading 1 and 2 of baseline, 6-month, and end-point examinations, the Student's paired t-test was used, and results were considered significant at P < .05. Intraexaminer reliability using index scores was evaluated using Kappa statistics. All analyses were performed using SPSS (version 15.0; SPSS Inc, Chicago, Ill).
RESULTS
In Vitro Assessments
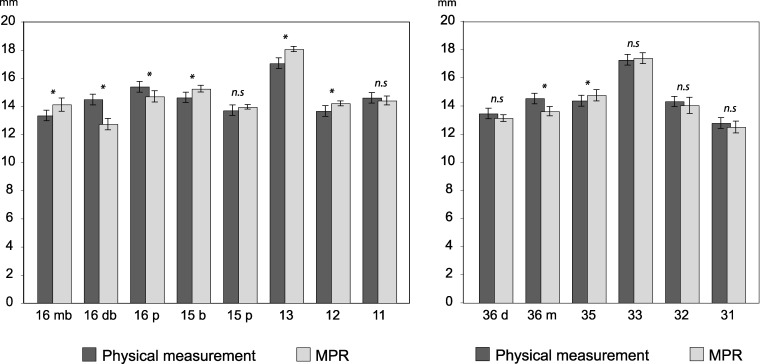
Root length and marginal bone level measurements are shown in Figures 4 and 5. The mean difference in length determinations between physical and radiographic measurements was 0.05 mm (SD 0.75; range, −1.01 mm to 1.74 mm). For some roots a significant difference at the P < .05 level was found (Figure 4). The mean difference between physical and radiographic measurements of the marginal bone levels was −0.04 mm (SD 0.54; range, −1.53 mm to 1.92 mm). A significant difference at the P < .05 level was found for some of the teeth/surfaces investigated (Figure 5).
Figure 4.
Mean values and standard deviations of in vitro root length measures obtained by direct physical and radiographic means. * indicates a significant difference at P < .05.
Figure 5.
Mean differences and standard deviations between physical and radiographic in vitro bone level measurements. * indicates a significant difference at P < .05.
In Vivo Assessments
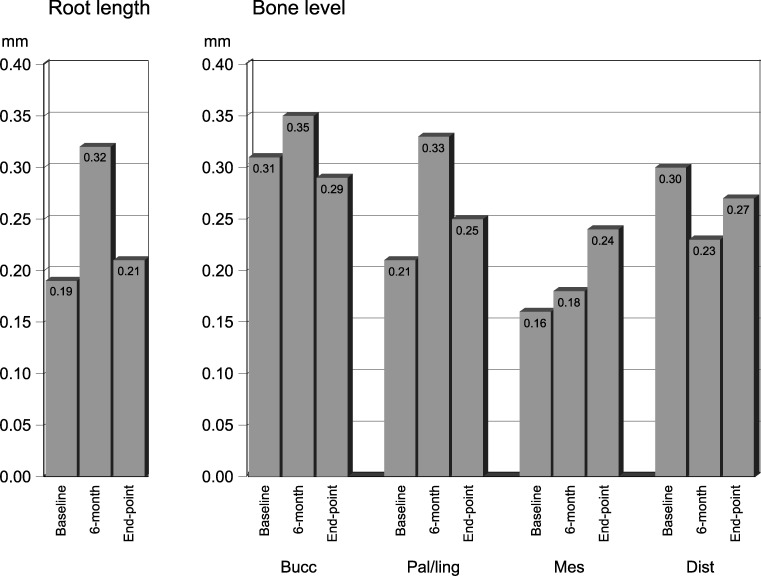
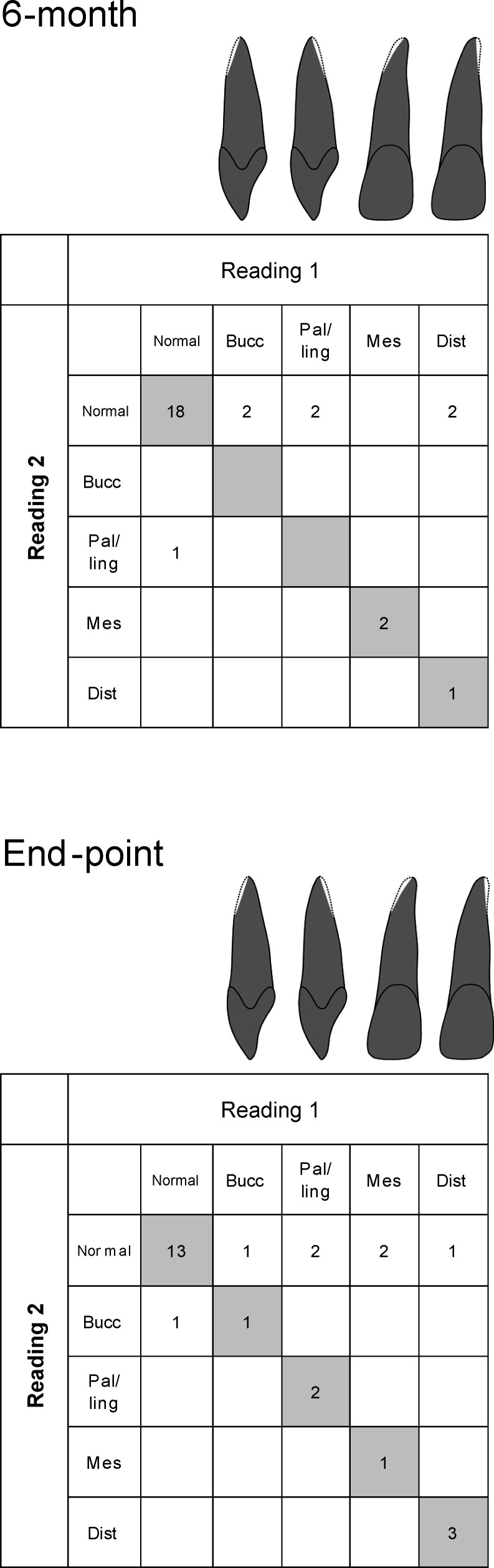
Precision of root length and bone level assessments for radiographic examinations at baseline, 6-month, and end-point are shown in Figure 6. The error for root length and bone level measurements was <0.35 mm and <0.40 mm, respectively, and statistically insignificant (P > .05). Intraexaminer reliability for assessment of root length/resorption and apical surface resorption was done using the index by Malmgren et al18 at 6-month and end-point examinations, as shown in Figures 7 and 8. The Kappa-value was 1.0 for the 6-month examination and 0.77 for the end-point examination. Using the modified index it was 0.75 for the 6-month and 0.78 for the end-point examinations, respectively.
Figure 6.
Precision of radiographic in vivo assessments of root length and bone level at baseline, 6-month, and end-point examinations.
Figure 7.
Intraobserver agreement between readings 1 and 2 at 6-month and end-point examinations using an index by Malmgren et al.18
Figure 8.
Intraobserver agreement between readings 1 and 2 at 6-month and end-point examinations using a modified index for description of slanted surface resorption.
DISCUSSION
New methods in management and care need to be evaluated before being clinically applied. Fryback and Thornbury20 described a hierarchy of levels at which a method can be evaluated. At lower levels technical efficacy, such as resolution and diagnostic accuracy, can be evaluated. At the highest level the efficacy from a societal point of view is evaluated. Our study concerns lower levels of this hierarchy, but it must be pointed out that a method with poor efficacy on a lower level may have no value at higher ones. It is noteworthy that what we describe is the assessment of a method that may be valuable as an aid when evaluating a clinical procedure.
That orthodontic treatment may induce root resorption is known, but as a result of the absence of good methods to study its extent, in-depth scientific studies are scarce. It is for this reason that an evaluation, albeit on a low level, of a new method that can visualize parts of teeth and roots needs to be done.
The in vitro comparison of root length between direct and radiographic measurements showed statistically significant mean differences for some roots. Although the largest difference was 1.74 mm, 50% of them were below 0.5 mm. Recent studies21–25 of the linear accuracy of CBCT radiographs of dry skulls report mean differences between physical and radiographic measurements in the range of 0.07–0.26 mm. The larger mean differences we found at specific roots might be explained by difficulties in reproducing the direct measurements, as a result of anatomical conditions, rather than by inconsistencies in the multiplanar reconstructions.
The marginal bone level assessments also showed significant mean differences between direct physical and radiographic measurements for some teeth and surfaces. A major factor influencing the assessments, especially the direct ones, might be related to identification of the CEJ, which in dried teeth can be less well demarcated. Also, use of a pencil to mark the bony crest on the root surface may have induced errors. Mol and Balsundaram26 report a mean difference between CBCT and physical measurements of 1.27 mm (SD 1.43) when quantifying periodontal bone defects in vitro. Others27,28 have reported differences ranging from 0.19 mm to 0.41 mm. In contrast, using a measuring object with inserted metal balls to investigate accuracy and precision of tomograms, Lund et al29 showed a mean difference between physical and radiographic measurements that in some cases was less than the voxel size (0.125 mm). Hence, anatomical structures are likely to be more difficult to unequivocally define than are artificial ones.
In the clinical part of our study the largest measurement error (0.32 mm) for root length assessment was found at the 6-month examination. This might be explained by an initial remodeling of the root apex, which would make it more diffuse and harder to identify. The precision of bone level assessment at buccal and palatal/lingual surfaces also showed the largest measurement error at the 6-month examination. Artifacts due to metallic orthodontic brackets, wires, and bands may have influenced the identification of the CEJ.30
The intraobserver agreement when using the index of Malmgren et al18 was high for the examination at the 6-month mark, which can be explained by the large number of unaffected roots. At the end-point examination the agreement was somewhat lower, probably as a consequence of a higher frequency of apical remodeling. In contrast, the intraobserver agreement regarding surface resorption at the root apex was lower at both the 6-month and end-point examinations. These changes may occur as an early response to tooth movements. Being subtle, they can be more difficult to identify. However, the intraobserver agreement for the modified index was still high.
Intraoral radiography still is the number one choice for root length assessments during orthodontic treatment.3 Despite efforts to obtain periodically identical radiographs, the technique has fundamental shortcomings as a result of the irradiation geometry in particular.8,9 The CBCT technique for assessment of root length and bone level during orthodontic treatment has many advantages over intraoral radiography. It makes it possible to create scenes similar to previous ones despite changes that may have occurred during treatment. It also displays buccal and palatal/lingual marginal bone not visible in intraoral radiographs.31
Today many CBCT machines are on the market, and more are likely to come. It must be noted that they differ with respect to, for example, geometric resolution, which may influence both measurement accuracy and precision. Also, when larger volumes are examined, as may often be the case in orthodontics, geometric resolution will decrease. Thus, the results we present are valid for the machine we have used or others with similar geometric resolution. The reason we have used a CBCT unit yielding high geometric resolution is that it will be used to study the effects of orthodontic treatment with respect to root shortening and marginal bone level changes. A disadvantage of the CBCT technique is that the radiation dose is higher than that of intraoral radiography.15 This leads to special considerations regarding treatment follow-ups and controls, especially in healthy young individuals, such as those undergoing orthodontic treatment. Efforts must be made to follow the ALARA (As Low As Reasonably Achievable) principle.32 Despite that, the CBCT technique is a valuable instrument in orthodontic research.
CONCLUSIONS
Cone beam computed tomography performed with a machine providing high-resolution images combined with multiplanar reconstructions provides a method for both accurate and precise assessment of root shortening and bone level changes during orthodontic treatment.
Despite changes in tooth positions, cone beam computed tomography generally yields a high level of reproducibility, thus enhancing its usefulness in orthodontic research.
REFERENCES
- 1.Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part I: The basic science aspects. Angle Orthod. 2002;72:175–179. doi: 10.1043/0003-3219(2002)072<0175:OIIRRP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:138–146. doi: 10.1016/S0889-5406(05)81763-9. [DOI] [PubMed] [Google Scholar]
- 3.Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part II: The clinical aspects. Angle Orthod. 2002;72:180–184. doi: 10.1043/0003-3219(2002)072<0180:OIIRRP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Brezniak N, Goren S, Zoizner R, Dinbar A, Arad A, Wasserstein A, Heller M. The use of an individual jig in measuring tooth length changes. Angle Orthod. 2004;74:780–785. doi: 10.1043/0003-3219(2004)074<0780:TUOAIJ>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Gegler A, Fontanella V. In vitro evaluation of a method for obtaining periapical radiographs for diagnosis of external apical root resorption. Eur J Orthod. 2008;30:315–319. doi: 10.1093/ejo/cjm125. [DOI] [PubMed] [Google Scholar]
- 6.Brezniak N, Goren S, Zoizner R, Dinbar A, Arad A, Wasserstein A, Heller M. A comparison of three methods to accurately measure root length. Angle Orthod. 2004;74:786–791. doi: 10.1043/0003-3219(2004)074<0786:ACOTMT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Brezniak N, Goren S, Zoizner R, Shochat T, Dinbar A, Wasserstein A, Heller M. The accuracy of the cementoenamel junction identification on periapical films. Angle Orthod. 2004;74:496–500. doi: 10.1043/0003-3219(2004)074<0496:TAOTCJ>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Katona T. R. Flaws in root resorption assessment algorithms: role of tooth shape. Am J Orthod Dentofacial Orthop. 2006;130:698, e19–e27. doi: 10.1016/j.ajodo.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 9.Katona T. R. The flaws in tooth root resorption assessment algorithms: the role of source position. Dentomaxillofac Radiol. 2007;36:311–316. doi: 10.1259/dmfr/52061649. [DOI] [PubMed] [Google Scholar]
- 10.Follin M. E, Lindvall A. M. Detection of lingual root resorptions in the intraoral radiographs. An experimental study. Swed Dent J. 2005;29:35–42. [PubMed] [Google Scholar]
- 11.Leach H. A, Ireland A. J, Whaites E. J. Radiographic diagnosis of root resorption in relation to orthodontics. Br Dent J. 2001;190:16–22. doi: 10.1038/sj.bdj.4800870. [DOI] [PubMed] [Google Scholar]
- 12.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol. 1999;28:245–248. doi: 10.1038/sj/dmfr/4600448. [DOI] [PubMed] [Google Scholar]
- 13.Tsiklakis K, Donta C, Gavala S, Karayianni K, Kamenopoulou V, Hourdakis C. J. Dose reduction in maxillofacial imaging using low dose cone beam CT. Eur J Radiol. 2005;56:413–417. doi: 10.1016/j.ejrad.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 14.Lofthag-Hansen S, Thilander-Klang A, Ekestubbe A, Helmrot E, Gröndahl K. Calculating effective dose on a cone beam computed tomography device: 3D Accuitomo and 3D Accuitomo FPD. Dentomaxillofac Radiol. 2008;37:72–79. doi: 10.1259/dmfr/60375385. [DOI] [PubMed] [Google Scholar]
- 15.Ludlow J. B, Davies-Ludlow L. E, Brooks S. L, Howerton W. B. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–226. doi: 10.1259/dmfr/14340323. [DOI] [PubMed] [Google Scholar]
- 16.Suomalainen A, Salo A, Robinson S, Peltola J. The 3DX multi image micro-CT device in clinical dental practice. Dentomaxillofac Radiol. 2007;36:80–85. doi: 10.1259/dmfr/30358216. [DOI] [PubMed] [Google Scholar]
- 17.Kau C. H, Richmond S, Palomo J. M, Hans M. G. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 18.Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod. 1982;82:487–491. doi: 10.1016/0002-9416(82)90317-7. [DOI] [PubMed] [Google Scholar]
- 19.Dahlberg G. Statistical Methods for Medical and Biological Students. New York, NY: Interscience Publications; 1940. pp. 122–132. [Google Scholar]
- 20.Fryback D. G, Thornbury J. R. The efficacy of diagnostic imaging. Med Decis Making. 1991;11:88–94. doi: 10.1177/0272989X9101100203. [DOI] [PubMed] [Google Scholar]
- 21.Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using limited cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2004;19:228–231. [PubMed] [Google Scholar]
- 22.Loubele M, Maes F, Schutyser F, Marchal G, Jacobs R, Suetens P. Assessment of bone segmentation quality of cone-beam CT versus multislice spiral CT: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:225–234. doi: 10.1016/j.tripleo.2005.10.039. [DOI] [PubMed] [Google Scholar]
- 23.Mischkowski R. A, Pulsfort R, Ritter L, Neugebauer J, Brochhagen H. G, Keeve E, Zöller J. Geometric accuracy of a newly developed cone-beam device for maxillofacial imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:551–559. doi: 10.1016/j.tripleo.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 24.Pinsky H. M, Dyda S, Pinsky R. W, Misch K. A, Sarment D. P. Accuracy of three-dimensional measurements using cone-beam CT. Dentomaxillofac Radiol. 2006;35:410–416. doi: 10.1259/dmfr/20987648. [DOI] [PubMed] [Google Scholar]
- 25.Stratemann S. A, Huang J. C, Maki K, Miller A. J, Hatcher D. C. Comparison of cone beam computed tomography imaging with physical measures. Dentomaxillofac Radiol. 2008;37:80–93. doi: 10.1259/dmfr/31349994. [DOI] [PubMed] [Google Scholar]
- 26.Mol A, Balasundaram A. In vitro cone beam computed tomography imaging of periodontal bone. Dentomaxillofac Radiol. 2008;37:319–324. doi: 10.1259/dmfr/26475758. [DOI] [PubMed] [Google Scholar]
- 27.Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: an in vitro study on native pig and human mandibles. J Periodontol. 2005;76:665–673. doi: 10.1902/jop.2005.76.5.665. [DOI] [PubMed] [Google Scholar]
- 28.Misch K. A, Yi E. S, Sarment D. P. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–1266. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 29.Lund H, Gröndahl K, Gröndahl H-G. Accuracy and precision of linear measurements in cone beam computed tomography Accuitomo tomograms obtained with different reconstruction techniques. Dentomaxillofac Radiol. 2009;38:379–386. doi: 10.1259/dmfr/15022357. [DOI] [PubMed] [Google Scholar]
- 30.Sanders M. A, Hoyjberg C, Chu C. B, Leggitt V. L, Kim J. S. Common orthodontic appliances cause artifacts that degrade the diagnostic quality of CBCT images. J Calif Dent Assoc. 2007;35:850–857. [PubMed] [Google Scholar]
- 31.Vandenberghe B, Jacobs R, Yang J. Diagnostic validity (or acuity) of 2D CCD versus 3D CBCT-images for assessing periodontal breakdown. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:395–401. doi: 10.1016/j.tripleo.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 32.Brooks S. L. CBCT dosimetry: orthodontic considerations. Semin Orthod. 2009;15:14–18. [Google Scholar]