Abstract
Objective:
To evaluate the success rate of autotransplantation of teeth in consecutive patients and to analyze factors affecting the outcome.
Materials and Methods:
The subjects consisted of 215 consecutive patients (101 women and 114 men; aged 9.1–56.4 years, median age 15.2 years [P10 = 11.4, P90 = 19.7]) who had undergone transplantation of a total of 269 teeth, all by the same surgeon. In patients with multiple transplants, only the first transplant was included, to ensure that all transplanted teeth were independent units. The transplants were recorded as unsuccessful if the tooth had been extracted or was surviving but with root resorption or ankylosis. The interval between transplantation and final follow-up was a median 4.8 years (P10 = 2.0, P90 = 5.5) for successful transplants and a median of 2.4 years (P10 = 0.4, P90 = 7.7) for unsuccessful transplants.
Results:
One-hundred seventy-five (81%) of the transplantations were recorded as successful and 40 (19%) as unsuccessful. Twenty-five teeth had been extracted and 15 had survived but did not fulfill the criteria for success.
Conclusions:
The success rate of 215 consecutively transplanted teeth was 81%. The highest success rate was for transplantation of premolars to the maxillary incisor region (100%). Complications at surgery such as difficult extraction, deviant root anatomy, or damaged root periodontium affected the outcome. During growth, a successful transplant preserves alveolar bone.
Keywords: Tooth transplantation, Follow-up, Oral surgery, Orthodontics
INTRODUCTION
Autogenous tooth transplantation is a well-established surgical treatment. Successful autotransplantation of immature mandibular third molars was reported by Fong as early as 1953.1 A method for autotransplantation of immature premolars was described in 1967 and 1974 by Slagsvold and Bjercke.2,3 High initial success rates2,4–7 and also long-term results are reported.7–10
The most common complications associated with autotransplanted teeth are ankylosis and root resorption. Many factors influence the result, such as the developmental stage of the tooth, donor type, the duration of extraoral exposure of the donor tooth during surgery, damage to the root cementum and the periodontal ligament, and the experience of the oral surgeon.10,11
The application of different criteria for success has an impact on the reported figures. The success rate is reported to be higher than 80% when the root length of the autotransplanted premolar is 50% to 75% of the normal root length at the time of the surgery.2,4,6,10,12,13 Lagerström and Kristerson14 reported maintenance of at least 70% of the final root length to be a criterion for successful outcome.
The aim of the present investigation was to evaluate the success rate of autotransplantation of teeth in a consecutive patient material and to analyze factors implicated in the outcome.
MATERIALS AND METHODS
The material was sourced from data on consecutive dental transplant patients treated by the same surgeon over a period of 15 years. Of the 218 patients, the records of three were incomplete. The material consisted of 215 patients (101 female and 114 male; aged 9.1–56.4 years, median age 15.2 years [P10 = 11.4, P90 = 19.7]) who had undergone transplantation of a total of 269 teeth. In patients with more than one transplanted tooth, only the first transplant was included to ensure that all transplanted teeth were independent units. Thus, this material comprises 215 teeth in 215 patients. The indications for treatment are presented in Table 1.
Table 1.
Indications for Autotransplantation and Number of Teeth
The same treatment protocol was followed in all cases. Examination included any necessary radiographs. Local anesthesia was used in most patients, but some younger patients (aged 9–12 years) were treated under general anesthesia. The sutures were removed 7 days after surgery. Recall examinations were scheduled for 6 and 12 months and then annually, up to 5 years postoperatively.
The surgical protocol followed the recommendations of Kristerson.6 The stage of tooth development was registered according to Moorrees et al.15 The following parameters were registered perioperatively: tooth position, condition of the follicle if present, visible damage to the periodontal ligament, whether or not the tooth was transplanted into a bony alveolus, whether or not the tooth was placed in occlusion, the type and time of fixation, how long the donor tooth was in an extraoral environment after extraction, and any complications during surgery.
After extraction, the donor tooth was stored in a cloth saturated with physiologic saline solution and transferred to the recipient site with minimum delay. Penicillin V for 7 days and rinsing with chlorhexidine twice a day were prescribed.
At follow-up, the transplanted teeth were evaluated clinically and with radiographs. Periodontal probing depth, percussion, vitality, and occlusion were registered. Where indicated, endodontic treatment was started 1 month postoperatively.
The transplants were recorded as successful if there was (1) a positive vitality response, normal periodontium, and normal root development; (2) a root-filled transplant, normal periodontium, and normal root development; or (3) a positive vitality response, normal periodontium, and arrested root development.
Transplants were recorded as unsuccessful if the tooth had been extracted. Some surviving teeth with a poor prognosis (ie, those with root resorption or ankylosis) were also recorded as unsuccessful.
The median interval between transplantation and final follow-up was median 4.8 years (P10 = 2.0, P90 = 5.5) for successful transplants and median 2.4 years (P10 = 0.4, P90 = 7.7) for unsuccessful transplants.
Statistical Analysis
The outcome was tested using logistic regression, and the level of significance was set at 5%. Minitab® statistical software (version 14) was used for the calculations.
RESULTS
Autotransplantation of one tooth was evaluated in each of 215 consecutive patients. After a median follow-up period of median 4.8 years, 175 (81%) of the transplantations were recorded as successful and 40 (19%) as unsuccessful. Of the 40 unsuccessful transplants, 25 had been extracted and 15 had survived but did not fulfill the criteria for success. These 15 surviving teeth were monitored for 2 to 12 years (median, 5.0 years; P10 = 1.4, P90 = 9.6).
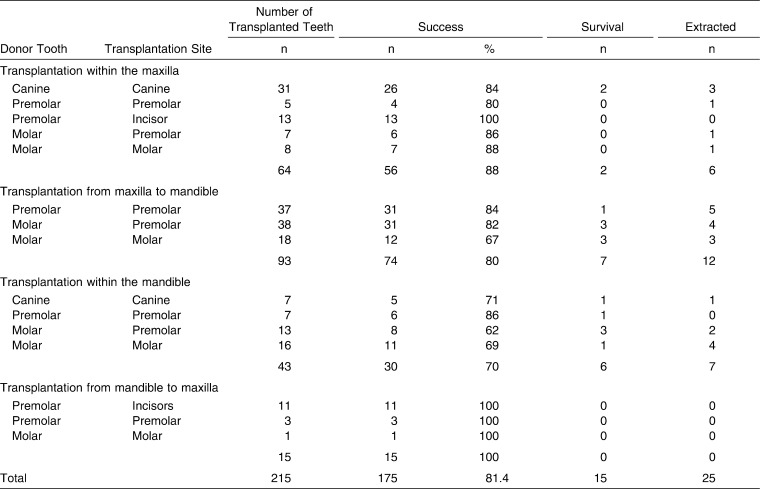
Sixty-four teeth were transplanted within the maxilla, 93 teeth from maxilla to mandible, 43 within the mandible, and 15 from mandible to maxilla (Table 2). The highest success rate was for transplantation of premolars to the maxillary incisor region. The median follow-up for these teeth was median 4.3 years (P10 = 2.8, P90 = 5.3). Thirteen maxillary and 11 mandibular premolars were transplanted to the maxillary incisor region, with 100% success (Table 2).
Table 2.
Distribution of Autotransplanted Teeth: Donor Tooth, Transplantation Site, and Success Rate
Thirty-one maxillary canines were autotransplanted from impacted to normal position in the dental arch. The success rate was 84%: three canines had to be extracted. The maxillary third molars were the most frequently used donor teeth. Seventy-one maxillary third molars were transplanted, with a success rate of 79%.
When maxillary or mandibular premolars were used as donor teeth, the success rate, regardless of recipient site, was 89%: 68 were successful and 8 failed. The loss of transplanted teeth was 13% for transplantation from maxilla to mandible. Of 93 such transplanted teeth, 12 (13%) had to be extracted. The extraction rate was 16% for transplantation within the mandible: of 43 transplanted teeth, 7 (16%) had to be extracted (Table 2).
The logistic regression model disclosed the following conditions as predictors of lower success rate (P = .001):
Complications at surgery, such as a difficult extraction, deviant root anatomy, or damaged root periodontium (P = .04; odds ratio, 1.66; 95% confidence interval, 1.02–2.72).
Recipient jaw: lower success rate for the mandible (P = .01; odds ratio, 3.05; 95% confidence interval, 1.30–7.18).
Age of the patient: the success rate for those older than 20 years was lower than for younger patients (P = .02; odds ratio, 3.17; 95% confidence interval, 1.18–8.50).
Prolonged extraoral exposure of the transplant tooth after extraction was associated with complications at surgery, but it did not enhance the predictive value for lower success.
Statistical analysis of the following remaining factors did not disclose predictive values: the condition of the follicle, which tooth was transplanted, and the presence or absence of bone alveolus at the recipient site.
DISCUSSION
Loss or aplasia of one or more teeth may be treated by various strategies such as prosthetic therapy, implants, autotransplantation, and orthodontic treatment. In adult patients in whom no further bone growth is expected, these conditions are frequently treated with bridgework and/or implant therapy. In a review about single-crown restorations on implants, a 5-year survival of 94.5% was reported. Technical complications were frequent.16 It should be remembered that an implant acts as an ankylosed tooth.17 Long-term results for resin-bonded bridges indicated an estimated 5-year survival of 87.7%. Technical complications such as debonding were frequent.18 The 10-year probability of survival for fixed partial dentures was reported to be 89.1%, while the success rate was 71.1%.19 However, in growing individuals, such treatment can impair the longitudinal, vertical, and transverse growth of the alveolar processes. Thus, in younger patients, autotransplantation is indicated and is often carried out in conjunction with orthodontic treatment.6,13,14,20
A success rate of 82% was reported by Kristerson and Lagerström7 for transplantation to the upper incisor region, and Kugelberg et al21 also achieved favorable results: 96% of immature premolars and 82% of mature premolars transplanted to the maxillary incisor region were successful 4 years after surgery. In a study by Czochrowska et al,22 it was concluded that in adolescents, transplantation of premolars may be recommended to replace missing maxillary incisors. In the present study, the best results were recorded for premolars, both maxillary and mandibular, transplanted to the maxillary incisor area: the success rate was 100%. Longer follow-up is required to determine whether transplantation of premolars should be recommended as the treatment of choice for a lost maxillary incisor in patients at an age at which the premolar roots are not fully developed. An optimal clinical outcome demands close cooperation between the orthodontist and the oral and maxillofacial surgeon.
A predictor of lower success was patient age greater than 20 years. This is consistent with the finding that the optimal time for transplantation is before final root development. The patients in the present study were treated on the assumption that root development of two-thirds three-fourths was optimal. Suzaki et al23 recently proposed that the prognosis for transplantation of teeth in adults might be improved by several months of orthodontic treatment prior to transplantation of teeth that have been in occlusion for some time.
In the present study, some palatally displaced maxillary canines were treated orthodontically before transplantation, as reported in detail in a previous study.24 This facilitated the transplantation procedure, and at the time of transplantation, the periodontal ligament was wider.
All transplantations in the present study were performed by one oral surgeon following an established protocol. This was probably important for the outcome.25
A more favorable prognosis is reported for donor teeth with incomplete root development. The position of the tooth and the extent and type of trauma during surgery are also important factors, along with extraoral exposure of the extracted tooth and endodontic treatment.6,13
There is a relationship between complicating factors at the time of surgery and prolonged extraoral exposure of the donor tooth after extraction. Complications encountered during surgery often lead to a prolonged extraoral interval. A technically more difficult tooth extraction increases the risk of damage to the periodontal ligament. This means that technical problems during surgery are associated with a lower success rate. It also highlights the importance of highly competent surgeons, with special training and experience in the field.
If the transplanted tooth develops root resorption, this usually occurs within the first year after surgery.6 Splitting osteotomy of the alveolar process has a negative influence on pulpal revascularization and also seems to exert a negative effect on postoperative root growth of transplanted immature third molars.26
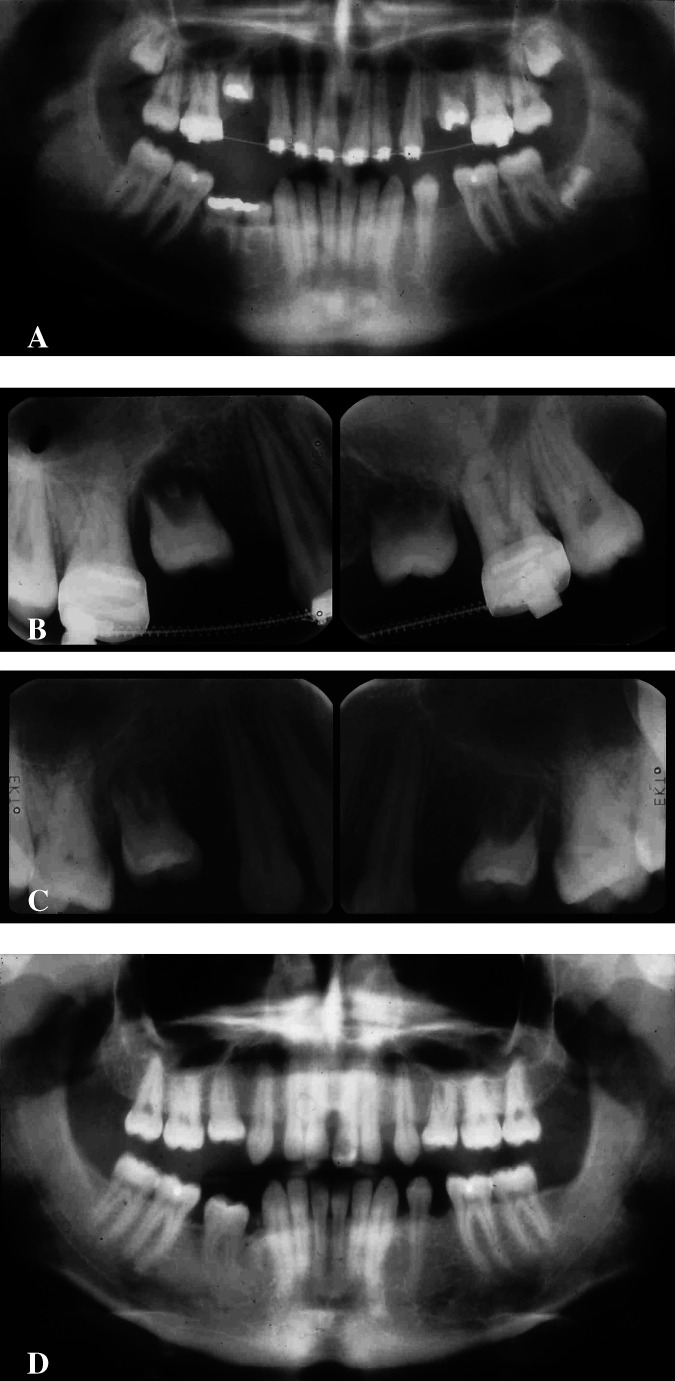
Adequate mesiodistal and vertical space is required at the recipient site. In the present study, the teeth were most frequently transplanted to recipient sites that lacked buccal and lingual alveolar bone, as illustrated in Figure 1B,C. The presence of the right tissue in the right place at the right time provides conditions for favorable growth. The major priority was to avoid damage to the periodontal ligament of the donor tooth. Normal mobility was achieved within 3 months and corresponded with radiographic evidence of bone formation.
Figure 1.
A boy aged 16 years with agenesis of seven premolars, infraocclusion of the maxillary second primary molars and mandibular right first and second primary molars, germs of the third molars. After pre-operative orthodontic treatment to correct the teeth and straighten the maxillary first molars, age 16 years, 7 months. (A) Three and a half months later, 1 week after transplantation of maxillary third molars with initial root development. (B) Eight months later. (C) At the final check-up, 5 years after transplantation, the left third molar has also been transplanted, to the mandibular right premolar region. However, the right maxillary transplant ended up in an infraoccluded position. (D). Note: A, severe infraocclusion of the deciduous molars; B, lack of bone at the recipient site; and C, bone development.
Akiyama et al27 conducted a clinical and radiographic study of the relationship between the macroscopic condition of the root surface of donor teeth and the clinical prognosis after transplantation and found no noteworthy difference between areas with exposed cementum and those with an intact periodontal ligament. Replacement root resorption was observed in teeth with cementum injury.
Early endodontic treatment has been proposed to prevent passage of degradation products and toxins from nonvital pulp tissue into the surrounding tissues through the apical foramen, accessory canals, or dentinal tubules. Endodontic treatment may thus facilitate arrest of the resorption process. In a study by Andreasen et al,28 premolars with complete root formation, treated endodontically 4 weeks after transplantation, had a 5-year survival rate of 98%.
A follow-up study of 194 patients by Kallu et al29 reported a lower success rate for canines and molars than for premolars: it was suggested that poorer accessibility increased the risk of damage to canines and molars. The reported overall success rate was 68%, but the success rate for premolars was 87%. The findings in the present study are similar: the overall success rate was 81%, whereas separate assessment of premolars disclosed a higher success rate of 90%. In the present study, extracted teeth as well as surviving teeth with a poor prognosis (ankylosis, root resorption) were registered as unsuccessful.
In a study with a follow-up of 2.5 to 22 years, autotransplantation of premolars to premolar sites only in 32 orthodontic patients had a success rate of 92%.5 Another study of 28 transplanted premolars in 24 patients reported 100% success 4 to 14 years posttreatment.30 Lundberg and Isaksson12 recommended that immature donor teeth should be placed in infraocclusion and mature donor teeth in occlusion or slight infraocclusion: this recommendation was followed in the present study. In a study of 80 patients by Josefsson et al31 using the same success criteria as in the present study, 110 teeth were transplanted to the lower second premolar site. After 4 years, the success rate was 92% for teeth with incomplete root formation and 82% for those with complete root formation.
CONCLUSIONS
The fate of 215 teeth transplanted in consecutive patients was monitored for a median of 4.8 years (P10 = 2.0, P90 = 5.5): a success rate of 81% was recorded.
Factors with a negative impact on the prognosis were difficult extraction, deviant root anatomy, or damaged periodontium of the donor teeth.
For the 24 maxillary and mandibular premolars transplanted to the maxillary incisor region, the success rate was very high.
REFERENCES
- 1.Fong C. C. Transplantation of the third molar. Oral Surg Oral Med Oral Pathol. 1953;6:917–926. doi: 10.1016/0898-1221(53)90129-1. [DOI] [PubMed] [Google Scholar]
- 2.Slagsvold O, Bjercke B. Autotransplantation of premolars with partly formed roots. Am J Orthod. 1974;66:355–366. doi: 10.1016/0002-9416(74)90046-3. [DOI] [PubMed] [Google Scholar]
- 3.Slagsvold O, Bjercke B. Autotransplantation of premolarer. Göteborg. Tandläkare Sällskapsartikelserie. 1967;351:45–85. [Google Scholar]
- 4.Andreasen J. O, Paulsen H. U, Yu Z, Schwartz O. A long-term study of 370 autotransplanted premolars. Part I, II, III. Eur J Orthod. 1990;12:3–37. doi: 10.1093/ejo/12.1.25. [DOI] [PubMed] [Google Scholar]
- 5.Jonsson T, Sigurdsson T. J. Autotransplantation of premolars to premolar sites: a long-term follow-up study of 40 consecutive patients. Am J Orthod Dentofacial Orthop. 2004;125:668–675. doi: 10.1016/j.ajodo.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Kristerson L. Autotransplantation of Teeth Influence of Different Factors on Periodontal and Pulpal Healing. Stockholm-Halmstad: [thesis]. Stockholm, Sweden: Karolinska Institute; 1985. [Google Scholar]
- 7.Kristerson L, Lagerström L. Autotransplantation of teeth in cases with agenesis or traumatic loss of maxillary incisors. Eur J Orthod. 1991;13:486–492. doi: 10.1093/ejo/13.6.486. [DOI] [PubMed] [Google Scholar]
- 8.Nethander G. Autogenous free tooth transplantation with a two-stage operation technique. Swed Dent J (suppl) 2003;161:1–51. [PubMed] [Google Scholar]
- 9.Czochrowska E. M, Stenvik A, Bjercke B, Zachrisson B. U. Outcome of tooth transplantation: survival and success rates 17–41 years posttreatment. Am J Orthod Dentofacial Orthop. 2002;121:110–119. doi: 10.1067/mod.2002.119979. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz O, Bergmann P, Klausen B. Resorption of autotransplanted human teeth: a retrospective study of 291 transplantations over a period of 25 years. Int Endod J. 1985;18:119–131. doi: 10.1111/j.1365-2591.1985.tb00428.x. [DOI] [PubMed] [Google Scholar]
- 11.Ahlberg K, Bystedt H, Eliasson S, Odenrick L. Long-term evaluation of autotransplanted maxillary canines with completed root formation. Acta Odontol Scand. 1983;41:23–31. doi: 10.3109/00016358309162300. [DOI] [PubMed] [Google Scholar]
- 12.Lundberg T, Isaksson S. A clinical follow-up study of 278 autotransplanted teeth. Br J Oral Maxillofac Surg. 1996;34:181–185. doi: 10.1016/s0266-4356(96)90374-5. [DOI] [PubMed] [Google Scholar]
- 13.Slagsvold O, Bjercke B. Applicability of autotransplantation in cases of missing upper anterior teeth. Am J Orthod. 1978;74:410–421. doi: 10.1016/0002-9416(78)90063-5. [DOI] [PubMed] [Google Scholar]
- 14.Lagerström L, Kristerson L. Influence of orthodontic treatment on root development of autotransplanted premolars. Am J Orthod. 1986;89:146–150. doi: 10.1016/0002-9416(86)90091-6. [DOI] [PubMed] [Google Scholar]
- 15.Moorrees C. F. A, Fanning E. A, Hunt E. E. J. Age variation of formation stages for ten permanent teeth. J Dent Res. 1963;42:1490–1502. doi: 10.1177/00220345630420062701. [DOI] [PubMed] [Google Scholar]
- 16.Jung R. E, Pjetursson B. E, Glauser R, Zembic A, Zwahlen M, Lang N. P. A systematic review of the 5-year survival and complication rates of implant-supported single crowns. Clin Oral Implants Res. 2008;19:119–130. doi: 10.1111/j.1600-0501.2007.01453.x. [DOI] [PubMed] [Google Scholar]
- 17.Thilander B, Ödman J, Lekholm U. Orthodontic aspects of the use of oral implants in adolescents: a 10-year follow-up study. Eur J Orthod. 2001;23:715–731. doi: 10.1093/ejo/23.6.715. [DOI] [PubMed] [Google Scholar]
- 18.Pjetursson B. E, Tan W. C, Tan K, Brägger U, Zwahlen M, Lang N. P. A systematic review of the survival and complication rates of resin-bonded bridges after an observation period of at least 5 years. Clin Oral Implants Res. 2008;19:131–141. doi: 10.1111/j.1600-0501.2007.01527.x. [DOI] [PubMed] [Google Scholar]
- 19.Tan K, Pjetursson B. E, Lang N. P, Chan E. S. Y. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004;15:654–666. doi: 10.1111/j.1600-0501.2004.01119.x. [DOI] [PubMed] [Google Scholar]
- 20.Nordenram Å. Autotransplantation of teeth: a clinical and experimental investigation. Acta Odont Scand. 1963;21(suppl 33):7–76. [PubMed] [Google Scholar]
- 21.Kugelberg R, Tegsjö U, Malmgren O. Autotransplantation of 45 teeth to the upper incisor region in adolescents. Swed Dent J. 1994;18:165–172. [PubMed] [Google Scholar]
- 22.Czochrowska E. M, Stenvik A, Album B, Zachrisson B. U. Autotransplantation of premolars to replace maxillary incisors: a comparison with natural incisors. Am J Orthod Dentofacial Orthop. 2000;118:592–600. doi: 10.1067/mod.2000.110521. [DOI] [PubMed] [Google Scholar]
- 23.Suzaki Y, Matsumoto Y, Kanno Z, Soma K. Preapplication of orthodontic forces to the donor teeth affects periodontal healing of transplanted teeth. Angle Orthod. 2008;78:495–501. doi: 10.2319/020207-51.1. [DOI] [PubMed] [Google Scholar]
- 24.Berglund L, Kurol J, Kvint S. Orthodontic pre-treatment prior to autotransplantation of palatally impacted maxillary canines: case reports on a new approach. Eur J Orthod. 1996;18:449–456. doi: 10.1093/ejo/18.5.449. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz O, Bergmann P, Klausen B. Autotransplantation of human teeth: a life-table analysis of prognostic factors. Int J Oral Surg. 1985;14:245–258. doi: 10.1016/s0300-9785(85)80036-3. [DOI] [PubMed] [Google Scholar]
- 26.Bauss O, Zonios I, Engelke W. Effect of additional surgical procedures on root development of transplanted immature third molars. Int J Oral Maxillofac Surg. 2008;37:730–735. doi: 10.1016/j.ijom.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Akiyama Y, Fukuda H, Mashimoto K. A clinical and radiographic study of 25 autotransplanted third molars. J Oral Rehab. 1998;25:640–644. doi: 10.1046/j.1365-2842.1998.00215.x. [DOI] [PubMed] [Google Scholar]
- 28.Andreasen J. O, Paulsen H. U, Yu Z, Bayer T, Schwartz O. A long-term study of 370 autotransplanted premolars. Part II. Tooth survival and pulp healing subsequent to transplantation. Eur J Orthod. 1990;12:14–24. doi: 10.1093/ejo/12.1.14. [DOI] [PubMed] [Google Scholar]
- 29.Kallu R, Vinckier F, Politis C, Mwalili S, Willems G. Tooth transplantations: a descriptive retrospective study. Int J Oral Maxillofac Surg. 2005;34:745–755. doi: 10.1016/j.ijom.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 30.Tanaka T, Deguchi T, Kageyama T, Kanomi R, Inoue M, Foong K. W. Autotransplantation of 28 premolar donor teeth in 24 orthodontic patients. Angle Orthod. 2008;78:12–19. doi: 10.2319/120706-495.1. [DOI] [PubMed] [Google Scholar]
- 31.Josefsson E, Brattstrom V, Tegsjo U, Valerius-Olsson H. Treatment of lower second premolar agenesis by autotransplantation: four-year evaluation of eighty patients. Acta Odontol Scand. 1999;57:111–115. doi: 10.1080/000163599429002. [DOI] [PubMed] [Google Scholar]