Abstract
The opioid epidemic in the United States has accelerated during the COVID-19 pandemic. As of 2021, roughly a third of Americans now live in a state with a recreational cannabis law (RCL). Recent evidence indicates RCLs could be a harm reduction tool to address the opioid epidemic. Individuals may use cannabis to manage pain, as well as to relieve opioid withdrawal symptoms, though it does not directly treat opioid use disorder. It is thus unclear whether RCLs are an effective policy tool to reduce adverse opioid-related health outcomes. In this study, we examine the impact of RCLs on a key opioid-related adverse health outcome: opioid-related emergency department visit rates. We estimate event study models using nearly comprehensive emergency department data from 29 states from 2011 through 2017. We find that RCLs reduce opioid-related emergency department visit rates by roughly 7.6% for two quarters after implementation. These effects are driven by men and adults aged 25–44. These effects dissipate after six months. Our estimates indicate RCLs did not increase opioid-related emergency department visits. We conclude that, while cannabis liberalization may offer some help in curbing the opioid epidemic, it is likely not a panacea.
Keywords: Opioid use disorder, cannabis, difference in differences, emergency department, I12, I18, H7, L51
1. Introduction
The opioid epidemic in the United States has accelerated during the COVID-19 pandemic. Over 81,000 drug overdose deaths occurred between June 2019 and May 2020—the highest ever recorded in a one-year period (The Centers for Disease Control and Prevention, 2020). Meanwhile, seventeen states have legalized recreational cannabis. Over a third of the U.S. population now lives in a state with a recreational cannabis law (ProCon.Org, 2021; U.S. Census Bureau, 2021).
Recreational cannabis laws (RCLs) were not originally adopted to mitigate the opioid epidemic, though they may have the potential to reduce opioid use. Recent empirical evidence suggests cannabis is a substitute for prescription opioids in pain management (Wen et al., 2021; Shi et al., 2019; Wen & Hockenberry, 2018). In addition, there is some clinical evidence suggesting cannabis may mitigate opioid withdrawal symptoms (Wiese & Wilson-Poe, 2018). These findings are promising because RCLs, unlike medical cannabis laws (MCLs), make cannabis available to the entire population and thus have a larger impact on cannabis use (Hollingsworth, Wing, & Bradford, 2020). However, cannabis does not directly treat the symptoms of opioid use disorder, for which medications for opioid use disorder are the only clinically effective treatment.
It is thus unclear whether RCLs are an effective policy tool to reduce adverse opioid-related health outcomes. Prior studies have primarily considered the mortality effects of RCLs, and the evidence is mixed. Livingston et al. (2017) found RCLs were associated with fewer opioid-related deaths in Colorado prior to 2015, but Alcocer (2020) found no such relationship when they extended the study period to 2017. Chan, Burkhardt, and Flyr (2020) found RCLs were associated with fewer synthetic opioid-related deaths, but Shover et al. (2019) found no evidence of a relationship between RCLs and opioid-related overdose deaths. Jayawardhana and Fernandez (2021) did not find a significant association between RCLs and opioid-related emergency department visits, though they found a positive association between RCLs and opioid-related hospitalizations in some specifications.
In this study, we examine the impact of RCLs on opioid-related emergency department (ED) visits. We are the first, to our knowledge, to examine the causal effects of RCLs on this important opioid-related adverse health outcome. Estimating an event study model with nearly comprehensive state-quarter ED visit data from 29 states from 2011 through 2017, we find RCLs are associated with a roughly 7.6% decrease in opioid-related ED visits in the first two quarters after implementation. These effects are driven by men and adults aged 25–44. However, these effects dissipate after the second quarter.
2. Methods
2.1. Data
Our primary data source is the Healthcare Cost and Utilization Project (HCUP) Fast Stats database (AHRQ, 2020). These data are drawn from the HCUP Emergency Department Databases and are reported at the state-quarter level. They report our primary outcome, the number of opioid-related ED visits per 100,000 population from non-federal, non-rehabilitation hospitals. Here, ED visits include treat-and-release ED visits and those that result in an inpatient admission. The data define opioid-related ED visits as including poisoning by opioids, heroin, synthetic narcotics, and other narcotics, as well as disorders related to the misuse of opioids (e.g., opioid-induce psychotic disorders, opioid withdrawal). The data are stratified by age, income, and sex.
We augment the Fast Stats data with state-level data on RCL and MCL implementation dates from the RAND-USC Schaeffer Opioid Policy Tools and Information Center (RAND-USC OPTIC, 2021), other opioid-related state policies from RAND-USC Schaeffer and the Kaiser Family Foundation, and socioeconomic characteristics primarily from the American Community Survey. See Appendix A for details.
2.2. Sample
Our sample consists of 812 state-quarters in 29 states from 2011 through 2017. We begin our study period in 2011 because the reformulation of Oxycontin in 2010 affected changes to the opioid epidemic that varied across states (Maclean, Mallatt, Ruhm, & Simon, 2020). The year 2017 is the last in which many states report Fast Stats data. To maintain a balanced panel, we limit our sample to states that were included in the HCUP Fast Stats for all quarters. Figure 1 visualizes our sample. The treatment states are California, Maine, Massachusetts, and Nevada, all of which implemented RCLs in the first quarter of 2017.
FIGURE 1.
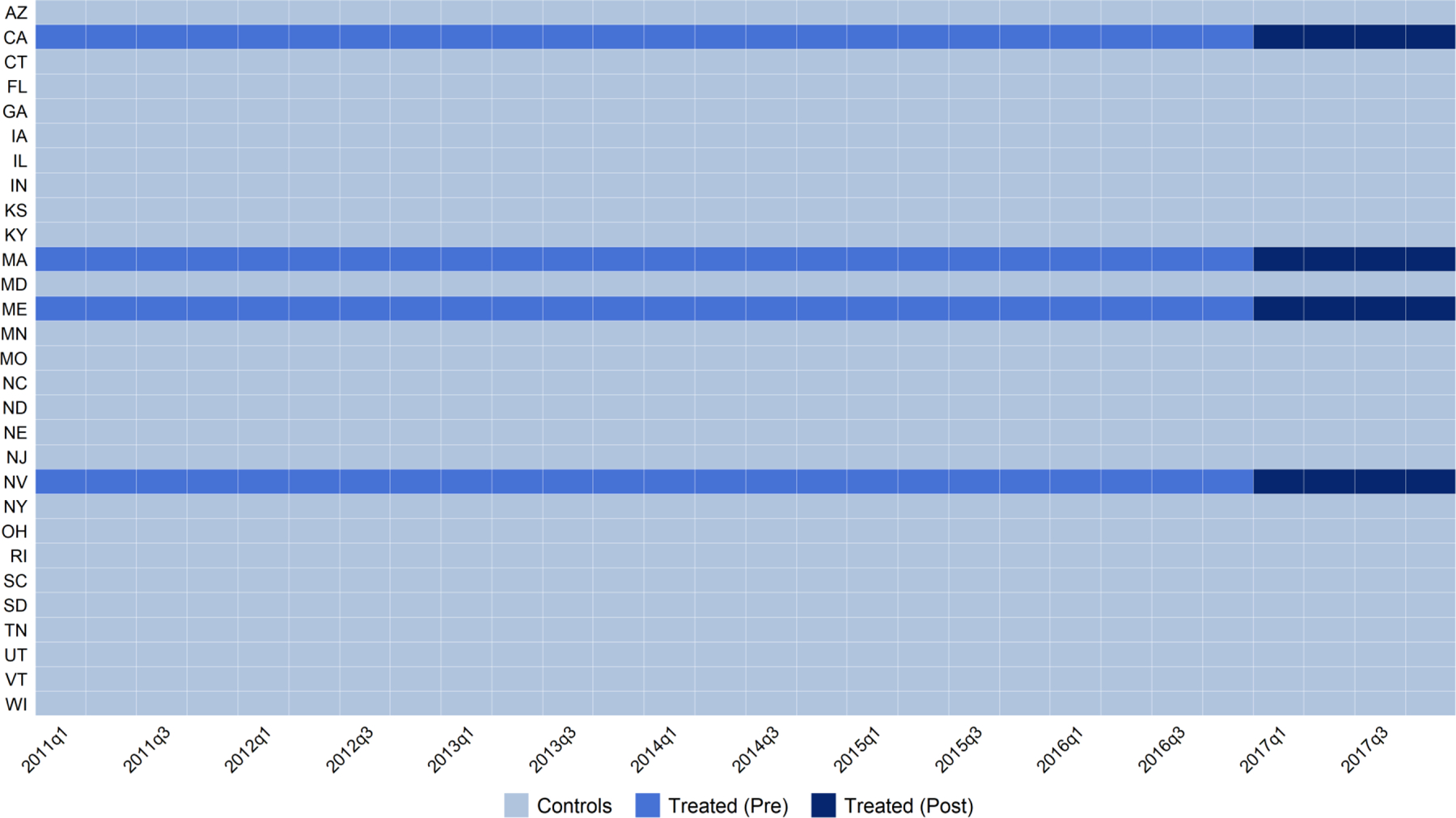
Recreational cannabis law implementation among sample states
Note. We obtained RCL implementation date data from the RAND Corporation’s Opioid Policy Tools and Information Center (RAND-USC OPTIC, 2021). We limited sample states to those that contributed to is the Agency for Health Research and Quality’s (AHRQ) Healthcare Cost and Utilization Project (HCUP) Fast Stats database (AHRQ, 2020). Our sample includes 812 state-quarters.
Figure 2 and Appendix Table A1 report unadjusted trends in log opioid-related ED visit rates over time among treatment and comparison states. Opioid-related ED visit rates increased substantially over our study period for both groups. Outcome levels are higher among the treatment group, though trends between the two groups appear to be similar. Mean opioid-related ED visits per 100,000 population were 258.1 and 261.1 in 2016 and 2017 among the comparison states, and 368.1 and 343.8 in 2016 and 2017 among the treatment states.
FIGURE 2.
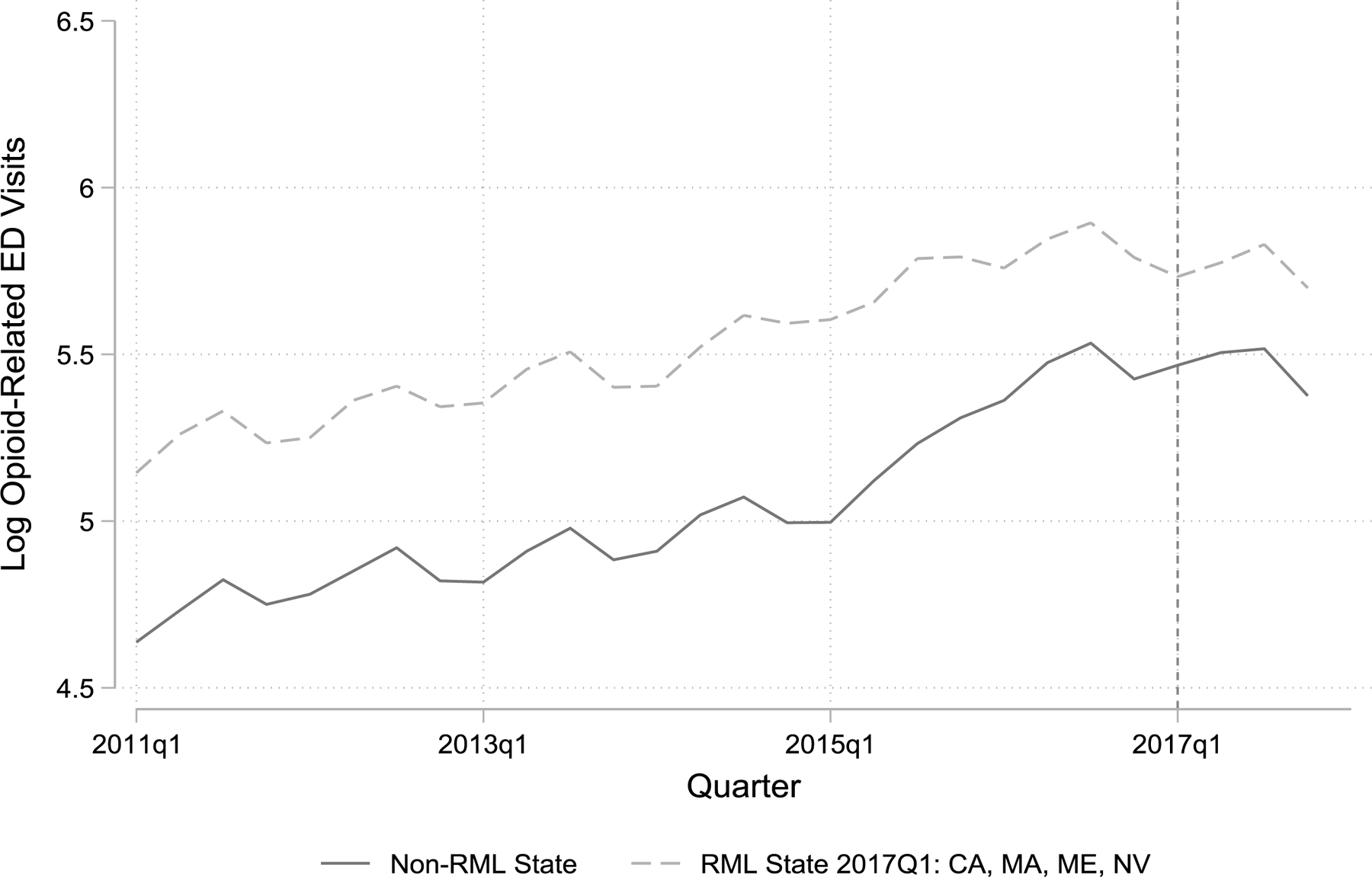
Unadjusted trends in log opioid-related ED visit rates
Note. All sample states are listed in Appendix A and are shown in Figure 1.
2.3. Empirical Strategy
We employ an event study model to estimate the causal effect of recreational cannabis laws (RCLs) on opioid-related ED visit rates. An event study model is similar to a difference-in-differences analysis, but it identifies treatment effects relative to the time period in which a policy is implemented. Several studies have found dynamic treatment effects related to cannabis legalization (e.g., Powell, Pacula, & Jacobson, 2018; Wen et al., 2021). Accordingly, we use an event study model as our baseline model to examine variation in treatment effects over time. Our baseline specification is
The outcome, ln(EDratest), is the log opioid-related ED visit rates per 100,000 population in state s in quarter t. In the summation term indexes the quarter relative to the implementation of a RCL in a treatment state—implementation occurs at j = 0—and k represents the quarter in which a RCL was implemented. We observe three periods after RCL implementation, so the summation ends with 3. We also include “leads” in the model where j < 0 to test for differential pre-trends between treatment and comparison states. The reference category is j = −1. The furthest lead, j = −5, serves as a catch-all term for pre-treatment periods where j ≤ −5. Polst is a vector of state-quarter policy indicators including: a medical cannabis law; a mandatory prescription drug monitoring program; Medicaid expansion; a good Samaritan law; a Naloxone access law. Demst is a vector of state-year socioeconomic variables including: the poverty rate; median household income; the unemployment rate; community hospital beds per 1,000 population. We also include state and quarter fixed effects θs and τt. We cluster the error term, ϵst, at the state level. See Appendix A for further details.
Our identifying assumption is that opioid-related ED visit rates would have trended similarly in states that legalized recreational cannabis in the absence of legalization. We lend support to this assumption by testing whether the lead coefficients are statistically different from zero.
3. Results
3.1. Baseline Results
We present the results from our baseline model in Figure 3 and Appendix Table A2. Relative to mean opioid-related ED visits per 100,000 population of 265.9 in the quarter prior to treatment (2016Q4), we find that RCLs are associated with 7.8% (95% CI = −13.6 to −2.0) and 7.7% (95% CI = −13.8 to −1.5) decreases in opioid-related ED visit rates in the first two quarters following implementation. However, these effects dissipate in the third and fourth quarters following implementation, when RCLs are associated with insignificant 3.0% (95% CI = −9.8 to 3.7) and 2.4% (95% CI = −9.5 to 4.8) decreases. Overall, RCLs are associated with a marginally significant 5.2% (95% CI = −10.7 to 0.2, P = 0.06) decrease in opioid-related ED visit rates over the study period.
FIGURE 3.
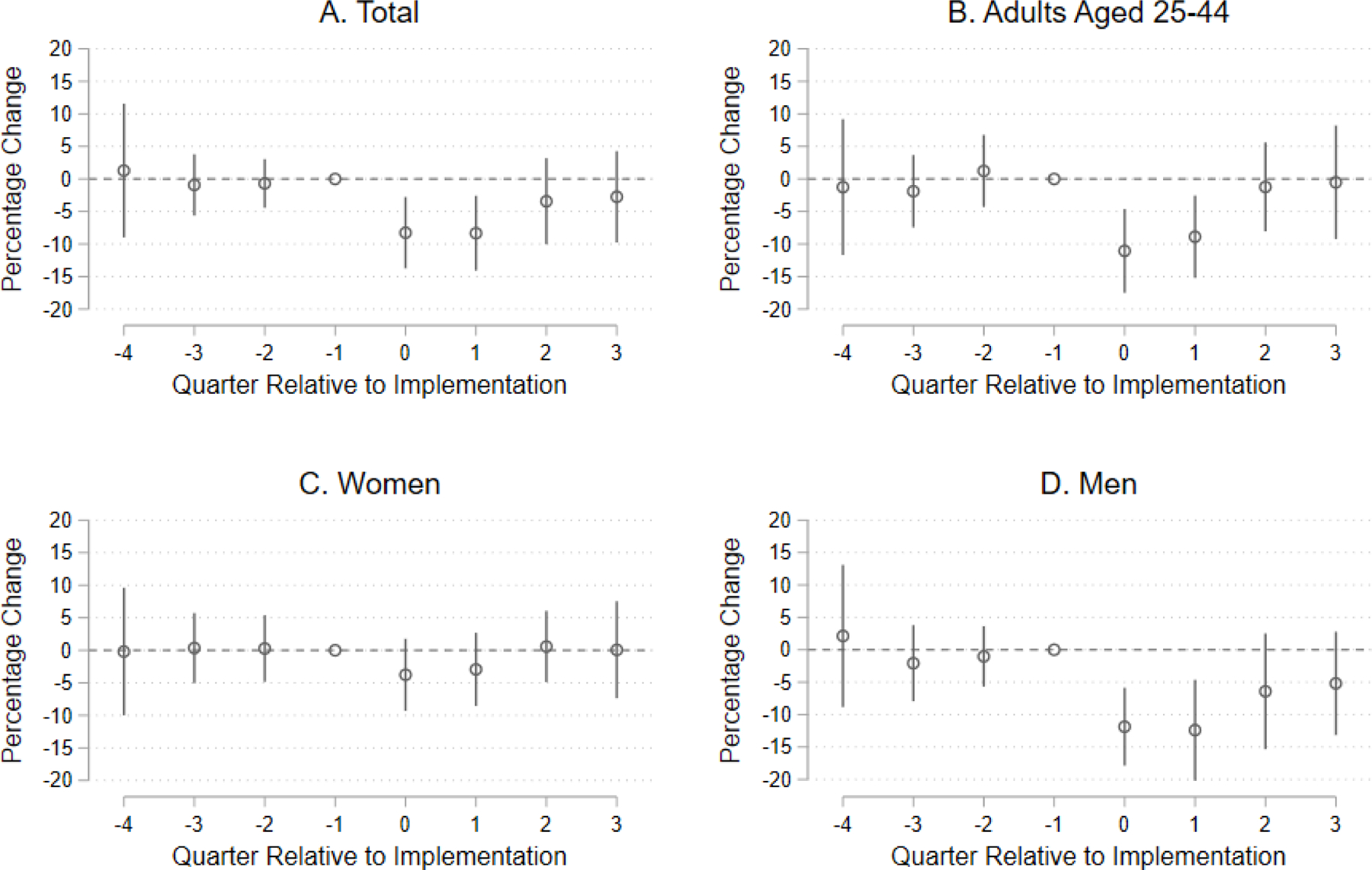
Event study estimates of recreational cannabis laws’ effect on the number of opioid-related emergency department visits per 100,000 population
Note. Point estimates correspond to the baseline model described in Section 2.3 and Appendix A. Exact point estimates are provided in Table 2. Coefficients are retransformed to represent percentage changes in rates, and standard errors are calculated using the delta method. Coefficients and standard errors are listed in Appendix Tables A1 and A2.
We proceed by testing for differential trends in treatment states prior to RCL implementation. The lead terms also are displayed in Figure 3. We do not find that the lead terms included in our event study model (i.e., a year prior to RCL implementation) are jointly significant (F = 0.31, P = 0.82). We do note the lead term for 5+ quarters is significant (Appendix Table A1). As shown in Figure 2, this lead term appears to capture a historical level difference between RCL and non-RCL states prior to 2016.
We re-estimate our baseline models for socioeconomic sub-groups. The results suggest our findings are driven by men and, to a lesser extent, adults aged 25–44. Men and adults aged 25–44 experience 11.5% (95% CI = −17.9 to −5.0) and 10.6% (95% CI = −17.3 to −4.0) reductions in opioid-related ED visits in the first quarter of RCL implementation, respectively. These effects also dissipate over time, though the overall result is significant for men (beta = −8.6%, 95% CI = −15.4 to −1.8). Results for adults aged 25–44, men, and women are shown in Figure 3; results for all sub-groups are shown in Appendix Table A3. Only the results for men withstand a Bonferroni adjustment for multiple hypothesis testing, so we interpret the other results with caution.
3.2. Robustness Checks
We conduct a series of robustness checks that support a causal interpretation of our findings. First, we test whether our results are driven by a particular state by iteratively excluding treatment states from our analysis (Appendix Table A4). Doing so has a negligible effect on our findings. Second, we re-estimate our baseline model with HCUP Fast Stats data dating back to 2006 to test whether our findings are sensitive to the chosen study period. After adding state-year linear time trends to our model to account for the dynamics of the first and second waves of the opioid epidemic, we find that our results are robust (see Appendix Table A5).
4. Discussion
We provide novel evidence of the effects of RCLs on a key opioid-related adverse health event, opioid-related ED visits. We find RCLs reduce opioid-related ED visits by roughly 7.6% for two quarters after RCL implementation. These effects are driven by men and adults aged 25–44, which is consistent with prior literature finding that men and young adults account for the majority of persons using cannabis (Kerr, Lui, & Ye, 2018), and that men’s health outcomes may be more responsive to cannabis legalization (Anderson, Rees, & Sabia, 2014). Our overall findings and those for young adults and men dissipate in magnitude and are no longer significant in the third and fourth quarters. Only the results for men are significant when we aggregate the four post-treatment quarters. Still, the upper bounds of the confidence intervals for our aggregated results allow us to rule out that RCLs affected any meaningful increase in opioid-related ED visit rates (i.e., greater than 0.2%). We also are able to rule out any increase in opioid-related ED visits for men. Broadly, our findings are consistent with Jayawardhana and Fernandez (2021), who also did not find an association between RCLs and opioid-related ED visits. Our findings also are consistent with studies that have not found an association between RCLs and mortality (Alcocer, 2020; Shover et al., 2019).
Our results indicate that RCLs may only affect a temporary reduction in opioid-related ED visits. Cannabis legalization may increase cannabis use for pain relief, acting as a substitute for opioids (Wen and Hockenberry 2018). However, cannabis is not a clinically effective treatment for opioid use disorder. Persons with opioid use disorder may attempt to use cannabis after the passage of a RCL, find that it is not a sufficient substitute, and then increase use of closer substitutes, including illicit opioids, such as heroin or fentanyl. While cannabis liberalization may offer some help in curbing the opioid crisis, our results suggest that it is not a panacea.
We note three limitations. First, we are unable to distinguish ED visits related to different types of opioids (e.g., heroin, fentanyl vs. prescription opioids) and diagnoses (e.g., opioid use disorder vs. overdose) because the HCUP Fast Stats data are not stratified as such. Second, our sample excludes four states with RCLs—Alaska, Colorado, Oregon, and Washington—that are not consistently present in the HCUP Fast Stats data during the sample period. Third, RCLs may have different effects in other states and over longer time periods. Future research should continue to explore the relationships between RCLs and opioid-related health outcomes in newly legalizing states, over longer treatment periods, for different populations, and for different health outcomes.
Supplementary Material
Acknowledgments:
The authors are grateful to David Bradford and Alex Hollingsworth for their helpful feedback in developing this manuscript.
Funding Sources:
Drake acknowledges support from the National Institute on Drug Abuse under award number K01D1051761.
Footnotes
Conflict of Interest Statements: The authors have no conflicts of interest to disclose.
References
- Agency for Health Research and Quality. (2020). HCUP Fast Stats. Retrieved September 1, 2020, from https://www.hcup-us.ahrq.gov/faststats/landing.jsp
- Alcocer JJ (2020). Exploring the effect of Colorado’s recreational marijuana policy on opioid overdose rates. Public Health, 185, 8–14. 10.1016/j.puhe.2020.04.007 [DOI] [PubMed] [Google Scholar]
- Anderson DM, Rees DI, & Sabia JJ (2014). Medical marijuana laws and suicides by gender and age. American Journal of Public Health, 104(12), 2369–2376. 10.2105/AJPH.2013.301612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan NW, Burkhardt J, & Flyr M (2020). The Effects of Recreational Marijuana Legalization and Dispensing on Opioid Mortality. Economic Inquiry, 58(2), 589–606. 10.1111/ecin.12819 [DOI] [Google Scholar]
- Hollingsworth A, Wing C, & Bradford A (2020). Comparative Effects of Recreational and Medical Marijuana Laws On Drug Use Among Adults and Adolescents. SocArXiv Papers. 10.31235/osf.io/drx9f [DOI] [Google Scholar]
- Jayawardhana J, & Fernandez JM (2021). S. Health Services Research, 1–11. 10.1111/1475-6773.13632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Lui C, & Ye Y (2018). Trends and age, period and cohort effects for marijuana use prevalence in the 1984–2015 US National Alcohol Surveys. Addiction, 113(3), 473–481. 10.1111/add.14031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston MD, Barnett TE, Delcher C, & Wagenaar AC (2017). Recreational cannabis legalization and opioid-related deaths in Colorado, 2000–2015. American Journal of Public Health, 107(11), 1827–1829. 10.2105/AJPH.2017.304059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclean JC, Mallatt J, Ruhm CJ, & Simon K (2020). Review of Economic Studies on the Opioid Crisis. NBER Working Paper, 28067. Retrieved from http://www.nber.org/papers/w28067
- Powell D, Pacula RL, & Jacobson M (2018). Do medical marijuana laws reduce addictions and deaths related to pain killers? Journal of Health Economics, 58, 29–42. 10.1016/j.jhealeco.2017.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ProCon.Org. (2021). Legal Recreational Marijuana States and DC. Retrieved May 4, 2021, from https://marijuana.procon.org/legal-recreational-marijuana-states-and-dc/
- RAND-USC OPTIC. (2021). OPTIC-Vetted Policy Data Sets. Retrieved February 10, 2021, from https://www.rand.org/health-care/centers/optic/resources/datasets.html
- Saloner B, & Karthikeyan S (2015). Changes in Substance Abuse Treatment Use Among Individuals With Opioid Use Disorders in the United States, 2004–2013. JAMA, 314(14), 1515–1517. [DOI] [PubMed] [Google Scholar]
- Shi Y, Liang D, Bao Y, An R, Wallace MS, & Grant I (2019). Recreational marijuana legalization and prescription opioids received by Medicaid enrollees. Drug and Alcohol Dependence, 194(October 2018), 13–19. 10.1016/j.drugalcdep.2018.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shover CL, Davis CS, Gordon SC, & Humphreys K (2019). Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proceedings of the National Academy of Sciences of the United States of America, 116(26), 12624–12626. 10.1073/pnas.1903434116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Centers for Disease Control and Prevention. (2020). Overdose Deaths Accelerating During COVID-19. Retrieved February 11, 2021, from https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
- U.S. Census Bureau. (2021). State Population Totals and Components of Change: 2010–2019. Retrieved May 4, 2021, from https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-total.html
- Wen H, & Hockenberry JM (2018). Association of medical and adult-use marijuana laws with opioid prescribing for medicaid enrollees. JAMA Internal Medicine, 178(5), 673–679. 10.1001/jamainternmed.2018.1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen J, Wen H, Butler JS, & Talbert JC (2021). The impact of medical and recreational marijuana laws on opioid prescribing in employer-sponsored health insurance. Health Economics. 10.1002/hec.4237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiese B, & Wilson-Poe AR (2018). Emerging evidence for cannabis’ role in opioid use disorder. Cannabis and Cannabinoid Research, 3(1), 179–189. 10.1089/can.2018.0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


