Abstract
This study aimed to evaluate the effectiveness of maternal and child health handbook (MCH) enhanced by mobile tools and to generate evidence informing the adoption of the program in Bangladesh. A cluster randomized controlled trial (RCT) has been implemented in Lohagora of Narail District and Dhamrai of Dhaka District. Unions of the study settings were randomly allocated in either one of three groups: (1) Intervention 1 using both mobile platform and MCH, (2) Intervention 2 using MCH alone, or (3) the Control. A total of 3,002 participants were recruited. The interventions were designed to promote two-way communications between pregnant women/their families and community health workers by an empowering approach. A total of 3,002 pregnant women were recruited. As the results, the interventions both significantly improved the utilization of CoC, although the overall proportion of CoC was relevantly low: 2.79% in the Control (95% CI: 1.37–3.54%), 6.16% in Intervention 2 (95% CI: 4.67–7.86%), and 7.89% in Intervention 1 (95% CI: 6.29–9.90%). Neonatal mortality rate with and without CoC was 5.43 per 1,000 (95% CI: 3.63–9.57 per 1,000) and 34.8 per 1,000 (95% CI: 24.3–45.4 per 1,000), respectively. Our study indicated the effectiveness of the interventions by leveraging MCH and a mobile platform to promote uptake of CoC throughout prepartum, intrapartum and postpartum/neonatal periods, potentially bringing long-lasting benefits to mothers and their offspring. The explicit approach is expected to guide policy makers to adopt MCH interventions in primary healthcare strengthening at the community level.
Trial registration: UMIN000025628 Registered June 13, 2016.
Introduction
Although Bangladesh has achieved a significant progress on reduction of maternal and child mortality during the past decades, unmet targets on delivery and utilization of maternal and neonatal healthcare services have left the issue in an agenda of Sustainable Development Goals (SDGs). The new goals of the SDGs are to reduce the maternal mortality ratio (MMR) to less than 70 per 100,000 live births and neonatal mortality ratio (NMR) to 12 per 1,000 live births by 2030 [1–3]. So far, the effectiveness of interventions for saving the lives of mothers and babies have been proven [2, 4–7], but challenges remain in health-care seeking and practices across the full continuum of maternal and child care, including the utilization of antenatal care, birth with a skilled attendant or standard facilities, emergency obstetric care in case of complications or illness for women and newborn, essential neonatal care, and postnatal visits for women and babies in resource constrained settings [8–10].
The World Health Organization (WHO) [11, 12] recommended a home-based maternal record (HMR), an effective tool to actively link pregnant women and their families to community health workers and professional hospital staffs, raise knowledge and awareness on maternal and child health, identify complications in pregnancy and labor and common illness of mothers and babies, and consequently to improve delivery and utilization of maternal and child care services [13–20]. Among antenatal notes, immunization cards, child health books and the integrated document, the maternal and child health handbook (MCH) is the most comprehensive home-based book that encompasses all the records of the continuum of care for both mothers and children, including antenatal care, labor and delivery, postpartum care, newborn and child care, immunization and family planning. The integration of the different types of records is much more effective compared to the fragmented implementation, saving both financial and human resources for the intervention [21, 22]. Besides the records, the handbook also contains guiding information on seeking care for mothers and children conveyed through ample illustrations. The recently launched WHO guideline has recommended the use of home-based records to complement facility-based records [23]. So far, its effectiveness to improve health seeking behaviors, home care practices, male involvement and communication between health professionals and women / caregivers, and feasibility has been proven by empirical epidemiological studies in various developing settings [15–20]. However, there was insufficient evidence on the type, content and implementation of home-based records (HBR), which needs to be tailored to different sociocultural and epidemiological contexts [23].
In Bangladesh, a pilot MCH project showed strong positive impact on mother’s knowledge, practices, record keeping, service utilization and empowerment of women [24, 25]. After the approval by the Government of Bangladesh, a project-based utilization of HBRs has been widely implemented by NGOs; however, the current system of HBRs is fragmented, with various types provided by different organizations. Therefore, we implemented the first cluster randomized controlled trial (RCT) to examine the effectiveness of MCH enhanced by a mobile platform in two counties of rural Bangladesh (protocol available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5902947/) [26]. The existing version of the Bangladeshi MCH designed by Bhuiyan et al. were used in the intervention. The reason for enhancing it with a mobile platform was to boost communications between pregnant women, their family and community health workers, principal healthcare providers in the rural area, and to catalyze the potential advantages of the mobile platform in knowledge dissemination, guidance and promotion of healthcare utilization [27]. We hypothesized that the proposed interventions will benefit the continuum of care and lead to better maternal and neonatal outcomes. The study aimed to assess the effectiveness of the interventions on the improvement of the target outcomes, in order to inform updates of the MCH in the context of Bangladesh and policy making for the targets of SDGs related to maternal and neonatal health.
Methods
Study settings and participants
The community-based cluster RCT (trial registration: UMIN000025628) was conducted in two upazilas (administrative regions in Bangladesh), Dhamrai in Dhaka District, Dhaka Division and Lohagora in Narail District, Khulna Division from February 2017 to August 2018. The demographic characteristics of the study sites was summarized in Supplementary file (S1 File). The study period covered the duration from the start point at which the pregnant women were identified and recruited to the end point, when the participants came through the fourth week after giving birth, or terminated the pregnancy due to miscarriage, stillbirth and neonatal / maternal mortality. The cluster, namely the unions in each Upazila, rather than the individual, was subjected to the cluster randomized sampling. These unions in the targeted study sites have homogeneous socioeconomic characteristics such as income level of household, annual birth rate, accessibility to primary healthcare, literate rate, school attendance, and hygiene conditions in household. The sampling and randomization process was briefly described in the protocol and Supplementary file (S1 File). The selected unions were randomly allocated to either 1) the intervention that combined mobile phone communication with MCH, 2) the intervention using MCH alone or 3) the control, where the proposed intervention was voluntarily implemented after the study.
The target population was pregnant women aged 15 to 49 years living in the selected settings and expected to give birth between 1 August 2017 and 31 July 2018. The eligible criteria include: i. currently having a good health status, without any maternal complication; ii. living and planning to give a birth in the study settings during the period from February 01, 2017 to August 30, 2018 and iii. willing to participate to the proposed study with agreement to the informed consent. The pregnant women were basically identified from two routes: the registration list in the upazila health complex; and field activities of the community health workers (local NGO staffs), as they have close interactions with the rural residents.
The study also included healthcare providers at the community. We also included health professionals in each upazila as required. A total of 3,002 participants were finally recruited, including 998 for the intervention 1, 1,001 for the intervention 2 and 1,003 for the control. Table 1 summarizes the participants in the study settings. Details of study design and sampling issues were described in our published protocol [26].
Table 1. Study settings and allocation.
| Lohagora Upazila | Dhamrai Upazila | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Union No. | Control | Intervention 1 | Internation 2 | Total | Union No. | Control | Intervention 1 | Internation 2 | Total |
| 1 | 0 | 0 | 113 | 113 | 13 | 0 | 103 | 0 | 103 |
| 2 | 109 | 0 | 0 | 109 | 14 | 0 | 0 | 86 | 86 |
| 3 | 0 | 0 | 126 | 126 | 15 | 0 | 74 | 0 | 74 |
| 4 | 0 | 0 | 79 | 79 | 16 | 87 | 0 | 0 | 87 |
| 5 | 0 | 0 | 190 | 190 | 17 | 71 | 0 | 0 | 71 |
| 6 | 0 | 222 | 0 | 222 | 18 | 0 | 0 | 107 | 107 |
| 7 | 141 | 0 | 0 | 141 | 19 | 0 | 0 | 81 | 81 |
| 8 | 78 | 0 | 0 | 78 | 20 | 92 | 0 | 0 | 92 |
| 9 | 96 | 0 | 0 | 96 | 21 | 0 | 88 | 0 | 88 |
| 10 | 0 | 126 | 0 | 126 | 22 | 0 | 0 | 109 | 109 |
| 11 | 76 | 0 | 0 | 76 | 23 | 0 | 156 | 0 | 156 |
| 12 | 0 | 144 | 0 | 144 | 24 | 76 | 0 | 0 | 76 |
| 25 | 84 | 0 | 0 | 84 | |||||
| 26 | 0 | 0 | 110 | 110 | |||||
| 27 | 0 | 85 | 0 | 85 | |||||
| 28 | 93 | 0 | 0 | 93 | |||||
| Total | 500 | 492 | 508 | 1,500 | Total | 503 | 506 | 493 | 1,502 |
The interventions
The two interventions were designed to promote two-way communications between pregnant women/their families and CHWs by an empowering approach. The intervention 1 applied mobile platform, including text and / or audio messages and phone calls if necessary, which were combined with MCH, while the intervention 2 utilized MCH alone. Contents of MCH encompassed the general profile of pregnant mother, menstrual history and history of previous pregnancy (if any), records of health education and consulting, records of conditions/health status, healthcare utilization and clinical results during pregnancy, delivery and postnatal/neonatal period, as well as information on common complications and signs of danger, on health seeking for mothers and babies, and on daily care and nutrition. In the two interventions, MCH was distributed to each participant at the point of recruitment. Every two months the enrolled pregnant women and their families and CHWs were organized for a community meeting, where health education, consulting/advice and anthropometric measurements were provided to accompany the discussions on seeking health services for mothers and babies and the application of MCH. Additionally in Intervention 1, besides MCH and community meetings, user-friendly mobile messages were developed and sent according to the gestational age (GA), including reminders of antenatal and postnatal care visits and facility-based delivery, list of locations of skilled birth attendants and hospitals, GA-specific health issues, daily care and nutrition during pregnancy, intake of iron tablet and folic acid, support from husband and families during pregnancy and lactating period, signs of danger, signs of labor, and postnatal/neonatal care. Audio messages and phone call were also used for follow-up and consulting/advice, as necessary. For those participants in households without mobile phones, the community staffs made regular visits to their home according to their GA to provide equivalent information.
The primary study target was the pregnant women, and their families (husbands, mother-in-law and / or mothers) were also invited to participate to the interventions, as they were substantially involved in daily home-based care during and after pregnancy, as well as seeking and utilization of healthcare services during pregnancy, childbirth and neonatal period in the study settings. By leveraging the community network, pregnant women and their families were organized for health education / health promotion activities, and a linkage with the community health workers were established to provide advice and referral when necessary. Through the network built, the interventions also closely involved communications among health care providers at different levels: for example, those healthcare staffs at the community were able to provide supports and advice and refer those with maternal complications to health professionals at the upper-level facilities (Upazila and District), and health professionals at the referral level were able to provide necessary guidance and training as well. The study procedure was briefly described in the protocol and Supplementary file (S1 File).
The expected outcomes
The expected outcomes were neonatal death, fetal death (stillbirth/miscarriage), preterm birth, low birthweight, maternal pregnancy complications and referral, antenatal care visits for at least one time (ANC1), antenatal care visits for at least four times (ANC4), antenatal care visits for at least six times (ANC6), facility-based delivery (FBD), mode of delivery, utilization of postnatal/neonatal care (PNC), and the experience of health education. The definition of neonatal deaths followed the standard employed by WHO, that is, death within the first 28 days of life. By referring Bangladesh Demographic and Health Survey (BDHS) 2014, neonatal deaths and fetal deaths were determined from the complete birth history from mothers and recorded by our trained staffs [28]. The continuum of care (COC) for mothers and babies in the study referred to healthcare services during pregnancy, at birth and after birth, and the variable was then created by combining ANC4, FBD and PNC.
Data analysis
For data analysis, univariate analysis was first performed to explore the characteristics of variables. In the comparison of each variable, the equality of covariates of the three groups at baseline was examined by a stratification. To examine the effect of the interventions on the targeted outcomes, we carried out multivariate logistic regressions. We considered potential correlations in the participants from the same unions. Then, generalized estimation equations (GEE) with an independent correlation structure were performed. The covariates were adjusted by using ratio residuals for each cluster obtained from the logistic regression models. For the fixed effect and the mixed effect of the cluster, namely the unions, we also performed generalized linear mixed models (GLMM) for comparison, in which the union ID was subject to the randomization. Risk ratios (RR) and their 95% confidence interval (CI) were calculated for the targeted outcomes in the intervention groups compared to the control group, after controlling demographic and socioeconomic factors of the pregnant women, such as age, education, household income, and those related to healthcare accessibility. Data analysis was performed using Stata 15.0.
Ethical consideration
The study was approved by the ethical committee of Bangladesh Medical Research Council (BMRC), Bangladesh. After stipulating the objectives, procedures, risks, benefits, confidentiality and voluntary both verbally and literally, the pregnant women who were willing to participate were asked for a signature in the informed consent form. For those unable to read and write, their substitutes (basically their families, relatives or neighbors) were asked to sign on the form on behalf. Additionally, for those aged below 18 years, their guardians were asked to accompany with, and then sign on behalf of them for the informed content. These consent procedures as described were approved by the ethical committee.
Results
Demographic and maternal characteristics of the participants
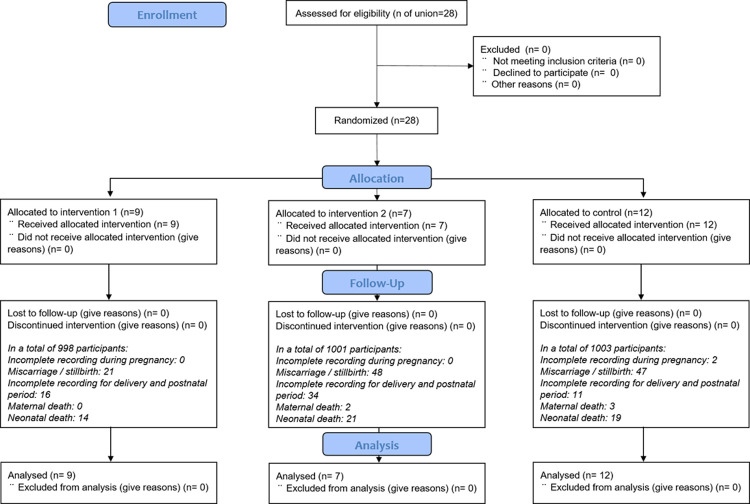
Fig 1 summarized participant flow. The details of demographic and maternal characteristics of the participants were all listed in Supplementary file (S1 File). The average age of the participants was 23.53 years (SD: 4.67 years). The average gestation age at birth and birth weight was 37.4 weeks (SD: 1.8 weeks) and 2,841.24 g (SD: 439.64 g), respectively. The proportion of those live birth who undertook cesarean section was as high as 50.81%. Socio-demographical characteristics did not significantly differ between the intervention groups and the study settings at baseline.
Fig 1. Participant flow diagram.
Mortality and morbidities
Tables 2 and 3 generated results from univariate and multivariate analyses to examine effects of the interventions on the expected outcomes. Among the overall participants, there were 5 maternal deaths, 116 fetal deaths (miscarriage/stillbirth) and 54 neonatal deaths reported in the study settings. Neonatal mortality rate (NMR) was 27.8 per 1,000 (95% CI: 19.7–36.0 per 1,000), 28.2 per 1,000 (95% CI: 10.5–45.8 per 1,000), and 34.8 per 1,000 (95% CI: 17.6–52.1 per 1,000) in Intervention 1, Intervention 2 and control group, respectively, while no significant difference in the three groups was identified. The factors independently affecting neonatal survival included referral of complications during pregnancy and delivery, multiple birth, congenital malformation, maternal status and COC. NMR among those having received COC and the counterparts was 5.43 per 1,000 (95% CI: 3.63–9.57 per 1,000) and 34.8 per 1,000 (95% CI: 24.3–45.4 per 1,000), respectively.
Table 2. Univariate analysis for effects of the interventions on the expected outcomes.
| Odds Ratio | 95% CI | ||
|---|---|---|---|
| Antenatal care > = 1 | MCH+mobile vs. control | 1.199 | 1.142–1.259 |
| MCH only vs. control | 1.116 | 1.060–1.176 | |
| interventions vs. control | 1.158 | 1.106–1.212 | |
| Antenatal care > = 4 | MCH+mobile vs. control | 2.344 | 1.733–3.170 |
| MCH only vs. control | 2.233 | 1.648–3.027 | |
| intervention vs. control | 2.289 | 1.728–3.030 | |
| Antenatal care > = 6 | MCH+mobile vs. control | 2.344 | 1.127–4.876 |
| MCH only vs. control | 3.509 | 1.751–7.031 | |
| intervention vs. control | 2.927 | 1.505–5.692 | |
| Postnatal care> = 1 | MCH+mobile vs. control | 1.169 | 1.052–1.300 |
| MCH only vs. control | 1.125 | 1.010–1.252 | |
| intervention vs. control | 1.147 | 1.044–1.260 | |
| Facility of delivery | MCH+mobile vs. control | 1.144 | 1.064–1.230 |
| MCH only vs. control | 1.137 | 1.057–1.223 | |
| intervention vs. control | 1.141 | 1.069–1.217 | |
| Referral of complication in pregnancy and childbirth | MCH+mobile vs. control | 1.025 | 0.999–1.051 |
| MCH only vs. control | 1.014 | 0.987–1.042 | |
| intervention vs. control | 1.019 | 0.995–1.044 | |
| Survival status of mother | MCH+mobile vs. control | 1.003 | 0.999–1.007 |
| MCH only vs. control | 1.001 | 0.996–1.006 | |
| intervention vs. control | 1.002 | 0.998–1.006 | |
| Survival status of the newborn | MCH+mobile vs. control | 1.006 | 0.994–1.018 |
| MCH only vs. control | 0.997 | 0.984–1.011 | |
| intervention vs. control | 1.002 | 0.991–1.013 | |
| Low birthweight | MCH+mobile vs. control | 0.879 | 0.699–1.107 |
| MCH only vs. control | 0.869 | 0.690–1.095 | |
| intervention vs. control | 0.874 | 0.718–1.064 | |
| Continuum of care | MCH+mobile vs. control | 4.735 | 3.080–7.279 |
| MCH only vs. control | 3.382 | 2.164–5.286 | |
| intervention vs. control | 4.069 | 2.683–6.171 |
Table 3. Multivariate analysis (GEE) for effects of the interventions on the expected outcomes.
| RR | 95% CI | p | ||
|---|---|---|---|---|
| Antenatal care> = 1 | ||||
| MCH+mobile | 1.848 | 1.617 | 2.111 | 0.000 |
| MCH only | 1.450 | 1.276 | 1.649 | 0.000 |
| Control | ref. | |||
| maternal age | 0.954 | 0.894 | 1.018 | 0.157 |
| maternal education | 0.998 | 0.960 | 1.039 | 0.937 |
| household income | 1.000 | 1.000 | 1.000 | 0.002 |
| primiparous pregnancy | 1.053 | 0.915 | 1.211 | 0.473 |
| distance to the nearest facility | 0.990 | 0.952 | 1.029 | 0.607 |
| knowledge on healthcare seeking | 1.551 | 1.364 | 1.763 | 0.000 |
| Antenatal care> = 4 | ||||
| MCH+mobile | 1.573 | 1.325 | 1.869 | 0.000 |
| MCH only | 1.537 | 1.293 | 1.827 | 0.000 |
| Control | ref. | |||
| maternal age | 0.999 | 0.924 | 1.080 | 0.980 |
| maternal education | 1.073 | 1.023 | 1.125 | 0.004 |
| household income | 1.000 | 1.000 | 1.000 | 0.021 |
| primiparous pregnancy | 1.011 | 0.857 | 1.192 | 0.895 |
| distance to the nearest facility | 1.041 | 0.994 | 1.090 | 0.088 |
| knowledge on healthcare seeking | 0.992 | 0.884 | 1.112 | 0.887 |
| Antenatal care> = 6 | ||||
| MCH+mobile | 1.806 | 1.324 | 2.465 | 0.000 |
| MCH only | 1.446 | 1.047 | 1.996 | 0.025 |
| Control | ref. | |||
| maternal age | 1.103 | 0.972 | 1.252 | 0.130 |
| maternal education | 1.128 | 1.044 | 1.218 | 0.002 |
| household income | 1.000 | 1.000 | 1.000 | 0.001 |
| primiparous pregnancy | 0.924 | 0.703 | 1.214 | 0.571 |
| distance to the nearest facility | 1.095 | 1.014 | 1.183 | 0.020 |
| knowledge on healthcare seeking | 0.973 | 0.794 | 1.192 | 0.788 |
| Postnatal care > = 1 | ||||
| MCH+mobile | 1.358 | 1.185 | 1.555 | 0.000 |
| MCH only | 1.280 | 1.117 | 1.465 | 0.000 |
| Control | ref. | |||
| maternal age | 0.984 | 0.922 | 1.052 | 0.642 |
| maternal education | 1.040 | 0.999 | 1.084 | 0.058 |
| household income | 1.000 | 1.000 | 1.000 | 0.000 |
| primiparous pregnancy | 0.889 | 0.773 | 1.022 | 0.098 |
| distance to the nearest facility | 1.010 | 0.971 | 1.050 | 0.621 |
| knowledge on newborn care | 1.820 | 1.661 | 1.996 | 0.000 |
| baby’s sex | 0.981 | 0.881 | 1.092 | 0.728 |
| singleton or multiple birth | 0.818 | 0.423 | 1.579 | 0.549 |
| malformation | 0.790 | 0.388 | 1.610 | 0.516 |
| low birthweight | 0.827 | 0.702 | 0.973 | 0.022 |
| perceived health status of baby | 2.436 | 2.194 | 2.704 | 0.000 |
| Facility delivery | ||||
| MCH+mobile | 1.280 | 1.087 | 1.508 | 0.003 |
| MCH only | 0.946 | 0.798 | 1.122 | 0.524 |
| Control | ref. | |||
| maternal age | 1.010 | 0.930 | 1.098 | 0.811 |
| maternal education | 1.151 | 1.094 | 1.212 | 0.000 |
| household income | 1.000 | 1.000 | 1.000 | 0.017 |
| primiparous pregnancy | 0.849 | 0.711 | 1.013 | 0.069 |
| distance to the nearest facility | 1.021 | 0.973 | 1.071 | 0.394 |
| antenatal care > = 4 times | 2.995 | 2.294 | 3.911 | 0.000 |
| complications during delivery | 0.060 | 0.048 | 0.074 | 0.000 |
| singleton or multiple birth | 0.955 | 0.409 | 2.229 | 0.915 |
| preterm | 1.652 | 1.419 | 1.923 | 0.000 |
| knowledge on complications / danger signs | 1.048 | 0.902 | 1.219 | 0.538 |
| knowledge on delivery | 1.289 | 1.101 | 1.510 | 0.002 |
| Referral for complications | ||||
| MCH+mobile | 1.821 | 1.106 | 2.999 | 0.018 |
| MCH only | 1.500 | 0.945 | 2.381 | 0.086 |
| Control | ref. | |||
| maternal age | 0.967 | 0.768 | 1.218 | 0.776 |
| maternal education | 1.215 | 1.042 | 1.417 | 0.013 |
| household income | 1.000 | 1.000 | 1.000 | 0.883 |
| primiparous pregnancy | 1.017 | 0.609 | 1.697 | 0.950 |
| distance to the nearest facility | 0.980 | 0.854 | 1.125 | 0.776 |
| antenatal care > = 4 times | 0.592 | 0.382 | 0.917 | 0.019 |
| knowledge on complications / danger signs | 1.128 | 0.813 | 1.565 | 0.470 |
| knowledge on healthcare seeking | 1.011 | 0.749 | 1.364 | 0.945 |
| singleton or multiple birth | 3.071 | 1.303 | 7.238 | 0.010 |
| preterm | 1.252 | 0.713 | 2.198 | 0.434 |
| Maternal survival | ||||
| MCH+mobile | 1.000 | |||
| MCH only | 1.438 | 0.698 | 2.964 | 0.325 |
| Control | ref. | |||
| maternal age | 0.758 | 0.503 | 1.140 | 0.183 |
| maternal education | 0.840 | 0.652 | 1.082 | 0.178 |
| household income | 1.000 | 1.000 | 1.000 | 0.425 |
| primiparous pregnancy | 1.461 | 0.587 | 3.637 | 0.415 |
| distance to the nearest facility | 1.042 | 0.800 | 1.358 | 0.761 |
| antenatal care > = 4 times | 1.000 | |||
| complications during delivery | 1.000 | |||
| singleton or multiple birth | 1.000 | |||
| preterm | 0.950 | 0.399 | 2.259 | 0.907 |
| knowledge on complications / danger signs | 0.871 | 0.523 | 1.451 | 0.597 |
| knowledge on guiding delivery | 0.771 | 0.465 | 1.278 | 0.313 |
| Neonate survival | ||||
| MCH+mobile | 1.139 | 0.725 | 1.789 | 0.573 |
| MCH only | 1.131 | 0.725 | 1.765 | 0.588 |
| Control | ref. | |||
| maternal age | 1.415 | 1.123 | 1.783 | 0.003 |
| maternal education | 1.047 | 0.933 | 1.174 | 0.436 |
| household income | 1.000 | 1.000 | 1.000 | 0.409 |
| primiparous pregnancy | 0.753 | 0.442 | 1.284 | 0.297 |
| knowledge on daily care | 1.306 | 0.277 | 6.164 | 0.736 |
| knowledge on healthcare seeking | 0.920 | 0.455 | 1.862 | 0.817 |
| knowledge on complications / danger signs | 1.605 | 0.713 | 3.608 | 0.253 |
| knowledge on delivery | 1.173 | 0.552 | 2.494 | 0.679 |
| knowledge on newborn care | 1.254 | 0.659 | 2.385 | 0.491 |
| referral of complication during delivery | 0.483 | 0.234 | 0.996 | 0.049 |
| singleton or multiple birth | 0.274 | 0.092 | 0.811 | 0.019 |
| malformation | 9.023 | 3.551 | 22.927 | 0.000 |
| baby’s sex | 0.820 | 0.573 | 1.174 | 0.278 |
| low birthweight | 0.755 | 0.364 | 1.567 | 0.451 |
| preterm | 0.929 | 0.643 | 1.343 | 0.695 |
| maternal survival | 0.265 | 0.075 | 0.934 | 0.039 |
| cesarean section | 0.725 | 0.453 | 1.159 | 0.179 |
| continuum of care | 0.273 | 0.118 | 0.630 | 0.002 |
| Low birthweight | ||||
| MCH+mobile | 0.877 | 0.731 | 1.051 | 0.156 |
| MCH only | 0.857 | 0.698 | 1.051 | 0.138 |
| Control | ref. | |||
| maternal age | 0.961 | 0.893 | 1.034 | 0.289 |
| maternal education | 0.961 | 0.916 | 1.009 | 0.108 |
| household income | 1.000 | 1.000 | 1.000 | 0.512 |
| primiparous pregnancy or not | 0.952 | 0.782 | 1.158 | 0.620 |
| antenatal care > = 4 times | 1.056 | 0.925 | 1.207 | 0.419 |
| delivery at hospital | 1.136 | 0.903 | 1.429 | 0.275 |
| baby’s sex | 1.040 | 0.908 | 1.191 | 0.572 |
| singleton or multiple birth | 0.478 | 0.282 | 0.808 | 0.006 |
| preterm | 1.111 | 0.991 | 1.245 | 0.071 |
| complications during delivery | 1.035 | 0.856 | 1.252 | 0.720 |
| Continuum of care | ||||
| MCH+mobile | 2.197 | 1.743 | 2.769 | 0.000 |
| MCH only | 1.701 | 1.340 | 2.159 | 0.000 |
| Control | ref. | |||
| maternal age | 1.006 | 0.918 | 1.104 | 0.891 |
| maternal education | 1.067 | 1.008 | 1.130 | 0.025 |
| household income | 1.000 | 1.000 | 1.000 | 0.018 |
| primiparous pregnancy or not | 0.980 | 0.806 | 1.192 | 0.841 |
| distance to the nearest facility | 1.026 | 0.971 | 1.083 | 0.361 |
| knowledge on healthcare seeking | 0.991 | 0.873 | 1.124 | 0.886 |
| preterm | 1.133 | 1.069 | 1.201 | 0.000 |
| complications during delivery | 0.577 | 0.492 | 0.676 | 0.000 |
Healthcare seeking during pregnancy, at birth and after birth
During pregnancy, participants in Intervention 1, Intervention 2 and control group went to 2.01 times (SD: 1.40 times), 1.97 times (SD: 1.49 times), and 1.48 times (SD: 1.29 times) of ANC on average, respectively. Table 4 summarized the major outcomes as predicted. The indicator of COC in Intervention 1, Intervention 2 and control group was 11.88% (95% CI: 9.91% - 13.85%), 7.80% (95% CI: 6.16% - 9.43%), and 2.79% (95% CI: 1.56% - 4.01%), respectively. Compared to the control group, the proportions of ANC1, ANC4, ANC6, and PNC were higher in the two intervention groups, and FBD and referral for complications during pregnancy were better in Intervention 1.
Table 4. The expected outcomes as predicted by multivariate analysis (GEE).
| % | 95% CI | ||
|---|---|---|---|
| Antenatal care> = 1 | 77.38 | 75.86 | 78.90 |
| MCH+mobile | 84.79 | 82.57 | 87.01 |
| MCH only | 78.54 | 75.98 | 81.09 |
| Control | 66.56 | 63.31 | 69.82 |
| Antenatal care> = 4 | 11.06 | 9.90 | 12.22 |
| MCH+mobile | 13.36 | 11.24 | 15.49 |
| MCH only | 12.86 | 10.77 | 14.96 |
| Control | 5.96 | 4.32 | 7.61 |
| Antenatal care> = 6 | 2.46 | 1.89 | 3.03 |
| MCH+mobile | 3.83 | 2.62 | 5.03 |
| MCH only | 2.36 | 1.43 | 3.30 |
| Control | 0.98 | 0.32 | 1.65 |
| Postnatal care > = 1 | 42.36 | 40.73 | 43.99 |
| MCH+mobile | 45.66 | 42.86 | 48.46 |
| MCH only | 43.82 | 41.07 | 46.57 |
| Control | 36.37 | 33.38 | 39.36 |
| Facility delivery | 61.23 | 59.99 | 62.47 |
| MCH+mobile | 64.50 | 62.34 | 66.65 |
| MCH only | 59.89 | 57.76 | 62.02 |
| Control | 58.90 | 56.75 | 61.05 |
| Referral for complications | 98.24 | 97.49 | 98.99 |
| MCH+mobile | 99.01 | 98.13 | 99.90 |
| MCH only | 98.44 | 97.31 | 99.57 |
| Control | 96.26 | 93.80 | 98.73 |
| Neonate survival | 97.23 | 98.04 | 96.42 |
| MCH+mobile | 96.96 | 98.83 | 95.10 |
| MCH only | 97.44 | 98.38 | 96.50 |
| Control | 97.23 | 98.80 | 95.65 |
| Low birthweight | 12.75 | 11.52 | 13.97 |
| MCH+mobile | 11.98 | 9.93 | 14.02 |
| MCH only | 11.52 | 9.46 | 13.59 |
| Control | 14.79 | 12.49 | 17.08 |
| Continuum of care | 8.03 | 7.04 | 9.03 |
| MCH+mobile | 11.88 | 9.91 | 13.85 |
| MCH only | 7.80 | 6.16 | 9.43 |
| Control | 2.79 | 1.56 | 4.01 |
Experience of health education
In the two intervention groups, all participants reported that health education was provided during pregnancy, while in the control group, there 36.5% participants reported no relevant experience. Regarding the (potential) usefulness of MCH for knowledge dissemination for mothers and babies, 99.9% and 81.2% of participants in the intervention and the control group, respectively, had a positive attitude.
Discussion
To our knowledge, this study is the first cluster randomized controlled trial to assess the effect of the MCH program enhanced by mobile platform This is also the first cluster randomized design for HBR to improve COC for mothers and babies in Bangladesh. Our findings indicated that the application of MCH improved uptake of multiple healthcare services, including antenatal care and postnatal/neonatal care, among rural pregnant women. The interventions increased ANC visits by using MCH and combining MCH and mobile platform, respectively. Although the overall proportion of at least four visits of ANC as recommended was relevantly low in the study settings, the figure in the two intervention groups, especially in the combined intervention, were better. A similar tendency was also observed in PNC. The combined intervention further improved facility-based delivery and utilization of healthcare facility for complications during pregnancy and delivery. The multilevel GEE models identified statistical significance of these intervention effects, after adjusting potential confounders.
Compared to the monitoring data of UNICEF which targeted the overall population during the study period in Bangladesh [29], our study which targeted pregnant women living in rural areas identified higher NMR of 29.7 per 1,000 (95% CI: 21.6–37.8 per 1,000). Although the estimated figure was lower in the two intervention groups, no statistical significance on the immediate efforts to reduce mortality and morbidities was identified. A possible reason for this could be the calculation of the study sample size was based on an NMR of 24.4 per 1,000 (derived from the final MDG report), while the indicator has been substantially reduced since then. We also acknowledged that unlike obstetric care practices, MCH does not have an immediate life-saving effect and that the universal access to good-quality obstetric and neonatal healthcare plays a key role in reducing NMR based on the success observed in Bangladesh and other developing settings [30, 31]. On the other hand, consistent with the findings of a systematic review, [32] our analysis confirmed that a crucial determinant in reducing NMR was COC; both interventions showed a significant improvement. This suggests that MCH has a potential to improve neonatal survival through the promotion of utilization of COC for mothers and the newborn.
In our study, MCH brought upon several benefits, such as health education, promotion of daily care awareness and practices, involvement of husband and family members and boosting communication between pregnant women and healthcare providers, especially CHWs, leading to better healthcare utilization during pregnancy, at birth and after birth. This was compatible to previous studies on MCH [16–20]. The interventions involved primary healthcare at the community as an inevitable aspect. In the intervention settings, and the local residents, including pregnant women and their families, were organized and networked, and community meetings aiming to strengthen participatory learning and action on preventive and care-seeking behaviors were also implemented regularly. Similar empowerment practices have proven to be effective in improving key behaviors and neonatal survival outcomes, although its mechanism may depend on local practices, capabilities and the responsiveness of health services [33]. In our study, during this empowerment process, MCH or MCH combined with the mobile platform were the key instruments. CHWs were mobilized to reinforce the linkage, deliver knowledge and primary care, organize the community meeting and bridge pregnant women and healthcare facilities, in order to accomplish the proposed interventions. To this end, the results suggested that MCH can be a useful tool to strengthen primary healthcare delivery in rural Bangladesh. The interventions largely filled the gap of health education during pregnancy and routine primary healthcare at the community level, and the (potential) usefulness of these interventions were definitely recognized among most participants.
Compared to MCH alone, the combined intervention achieved better utilization of COC, especially in terms of facility-based delivery and care seeking for complications during pregnancy and delivery. What works for this intervention were likely to be effective contacts and more frequent interactions between pregnant women and CHWs, such as sharing information and advising daily home-based care, together with seeking relevant healthcare based on individual needs and requirement. Text and voice messages complemented MCH in knowledge dissemination and deepening the understanding of the key contents of MCH. The high mobile coverage and the low costs in the study settings facilitated the intervention. The results added relevant evidence on the effectiveness of mHealth on improvement of maternal and neonatal outcomes and related care seeking by the high-quality study design, which were of lack in low- and middle-income countries [34], and suggested the value to apply these effective tools in primary healthcare at the community level.
Our study revealed the latest status of universal health coverage for mothers and neonates in rural Bangladesh. The uptake of ANC4 among rural pregnant women living in the study settings was considerably lower than that of the overall population identified by BDHS 2014 [35, 36], but was comparable to that of community-based studies conducted in a rural area [37, 38]. This can be explained by a substantial rural-urban gap in the uptake of maternal healthcare services [39]. Contrary to the stagnant progress in ANC uptake, our results suggested a fairly progressive uptake of PNC and FBD compared to previous surveys and estimates [40, 41]. The overall low uptake of these maternal and neonatal services suggested a big room for improvement through strengthening primary healthcare as the frontline of health system [42], particularly in rural areas.
The incidence of cesarean section (CS) identified in our study was much higher compared to that in BDHS 2014 [43], and largely exceeded the optimal rate ranging from 5% to 20% [44], while we did not identify the significant impact of undertaking CS on neonatal mortality reduction. Although it is a life-saving measure in obstetric care, a high level of CS indicates a substantial proportion of the practice without medical indication, leading to wasting of scarce healthcare resources and a high health and economic burden, especially in low- and middle-income countries [45–47]. The mechanism of the high-level CS tended to be complicated, mixing motivations of both the supply and demand sides, and the decision of the mothers and their family may largely be affected by doctors due to poorly informed healthcare needs [43, 48]. Our results suggested that this alarming phenomenon is emerging in not only urban areas, but also in rural areas recently, and an intervention by applying MCH and mobile platform had the potential to reduce the misuse. The emerging issues on CS in MCH for implementing health promotion/health education programs at community level are expected to be covered.
In interpreting these major findings, several issues should be carefully considered. The enrollment of the target pregnant women relied on self-report and local registration. Because of the variation in identifying pregnancy among the participants, gestational age at enrollment was diversified, causing differences in the participation duration. Moreover, our study was likely to be inevitably contaminated somehow, because the interventions and the outcomes cannot be masked, and there had been some previous NGO-driven health promotion campaigns and activities targeting the rural community in the study settings. However, there was no differences regarding these factors across the study settings and groups. Finally, because of the limited follow-up duration, our study did not observe the outcomes posterior to the neonatal period, potentially missing the overall effects of the target tools on maternal and child health.
Conclusions
In conclusion, our study indicated the effectiveness of the interventions by leveraging MCH and a mobile platform to promote uptake of COC throughout prepartum, intrapartum and postpartum/neonatal periods, potentially bringing long-lasting benefits to mothers and their offspring. These tools coordinated the interactions of pregnant women, their families and CHWs and their active engagement in primary healthcare at the community level, potentially contributing to better health outcomes. It is worth including these tools in primary healthcare to achieve universal health coverage for mothers and babies in rural Bangladesh.
Supporting information
(DOC)
(DOCX)
(DOCX)
Acknowledgments
The field study was conducted and coordinated by Bridge of Community Development Foundation (BCDF), a local NGO in Bangladesh. We would like to acknowledge of the field staffs who are fully involved in this study and contributed to the successful implementation. We also thank Dr. Julian Tang, for his linguistic edition of the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was granted by Japan Society of the Promotion of Sciences (16H06241) and Research grant of Ministry of Health, Labour and Welfare (Japan) (No, 20ba2001). The funder had no role in design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.General Economics Division, Planning Commission of Government of the People’s Republic of Bangladesh, UNDP Bangladesh. Millennium Development Goals Bangladesh Country Report 2013. 2014.
- 2.El Arifeen S, Hill K, Ahsan KZ, Jamil K, Nahar Q, Streatfield PK. Maternal mortality in Bangladesh: A countdown to 2015 country case study. The Lancet. 2014; 384 (9951): 1366–74. doi: 10.1016/S0140-6736(14)60955-7 [DOI] [PubMed] [Google Scholar]
- 3.Sustainable Development Goals. Goal 3: Ensure healthy lives and promote well-being for all at all ages. Available at: http://www.un.org/sustainabledevelopment/health/ (Accessed on August 14, 2020)
- 4.Lassi ZS, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. The Cochrane Database of Systematic Reviews. 2015; 3: CD007754. doi: 10.1002/14651858.CD007754.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perry HB, Rassekh BM, Gupta S, Wilhelm J, Freeman PA. Comprehensive review of the evidence regarding the effectiveness of community-based primary healthcare in improving maternal, neonatal and child health: 1. Rationale, methods and database description. Journal of Global Health. 2017; 7(1): 010901. doi: 10.7189/jogh.07.010901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies and stillbirths, and at what cost? Lancet. 2014; 384 (9940): 347–70. doi: 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 7.Van den Broek N. Happy Mother’s Day? Maternal and neonatal mortality and morbidity in low- and middle-income countries. International Health. 2019; 11(5): 353–357. doi: 10.1093/inthealth/ihz058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. Working with individuals, families and communities to improve maternal and newborn health. 2010. Available at: http://www.who.int/maternal_child_adolescent/documents/who_fch_rhr_0311/en/ (Accessed on August 14, 2020)
- 9.Smith HJ, Portela AG, Maston C. Improving implementation of health promotion interventions for maternal and newborn health. BMC Pregnancy Childbirth 2017; 17: 280. doi: 10.1186/s12884-017-1450-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mbuagbaw L, Medley N, Darzi AJ, Richardson M, HabibaGarga K, Ongolo-Zogo P. Health system and community level interventions for improving antenatal care coverage and health outcomes. The Cochrane Database Syst Rev 2015; 12: CD010994. doi: 10.1002/14651858.CD010994.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Home-based maternal records: guidelines for development, adaptation and evaluation. Geneva: WHO. 2018. Available at: https://www.who.int/maternal_child_adolescent/documents/home-based-records-guidelines/en/ (Accessed on August 14, 2020) [Google Scholar]
- 12.Shah PM, Selwyn BJ, Shah K, Kumar V. Evaluation of the home-based maternal record: A WHO collaborative study. Bull World Health Organ 1993; 71 (5): 535–48. [PMC free article] [PubMed] [Google Scholar]
- 13.Turner KE, Fuller S. Patient-held maternal and/or child health records: Meeting the information needs of patients and healthcare providers in developing countries? Online J Public Health Inform 2011; 3 (2): ojphi.v3i2.3631. doi: 10.5210/ojphi.v3i2.3631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Takayanagi K, Iwasaki S, Yoshinaka Y. The role of the Maternal and Child Health Handbook system in reducing perinatal mortality in Japan. Clin Perform Qual Healthcare. 1992; 1: 29–33. [PubMed] [Google Scholar]
- 15.Hagiwara A, Ueyama M, Ramlawi A, Sawada Y. Is the Maternal and Child Health Handbook effective in improving health-related behavior? Evidence from Palestine. J Public Health Pol. 2012; 34: 31–45. doi: 10.1057/jphp.2012.56 [DOI] [PubMed] [Google Scholar]
- 16.Kaneko K, Niyonkuru J, Juma N, Mbonabuca T, Osaki K, Aoyama A. Effectiveness of the maternal and child health handbook in Burundi for increasing notification of birth at health facilities and postnatal care uptake. Glob Health Action 2017; 10: 1297604. doi: 10.1080/16549716.2017.1297604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Osaki K, Kosen S, Indriasih E, Pritasari K, Hattori T. Factors affecting the utilization of maternal, newborn and child health services in Indonesia: the role of the maternal and child health handbook. Public health 2015; 129: 582–586. doi: 10.1016/j.puhe.2015.01.001 [DOI] [PubMed] [Google Scholar]
- 18.Yanagisawa S, Soyano A, Igarashi H, Ura M, Nakamura Y. Effect of a maternal and child health handbook on maternal knowledge and behavior: a community-based controlled trial in rural Cambodia. Health Policy Plan 2015; 30: 1184–92. doi: 10.1093/heapol/czu133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osaki K, Hattori S, Toda A, Mulati E, Hermawan L, Pritasari K, et al. Maternal and child health handbook use for maternal and child care: A cluster randomized controlled study in rural Java, Indonesia. Journal of Public Health. 2019; 41: 170–182. doi: 10.1093/pubmed/fdx175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mori R, Yonemoto N, Noma H, Ochirbat T, Barber E, Soyolgerel G, et al. The maternal and child health handbook in Mongolia: a cluster-randomized controlled trial. PLoS One. 2015; 10: e0119772. doi: 10.1371/journal.pone.0119772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aiga H, Huy TKP, Nguyen VD. Cost savings through implementation of an integrated home-based record: A case study in Vietnam. Public Health 2018; 156: 124–31. doi: 10.1016/j.puhe.2017.12.018 [DOI] [PubMed] [Google Scholar]
- 22.Aiga H, Nguyen VD, Nguyen CD, Nguyen TTT, Nguyen LTP. Fragmented implementation of maternal and child health home-based records in Vietnam: need for integration. Glob Health Action 2016; 9: 10. doi: 10.3402/gha.v9.29924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. WHO recommendations on home-based records for maternal, newborn and child health. Available at: https://apps.who.int/iris/bitstream/handle/10665/274277/9789241550352-eng.pdf (Accessed on August 14, 2020) [PubMed]
- 24.Shafi UB, Nakamura Y, Nahid A. Study on the development and assessment of maternal and child health (MCH) handbook in Bangladesh. Journal of Public Health and Development 2006; 4: 45–60. [Google Scholar]
- 25.Shafi UB. Development, field testing and potential benefits of a maternal and child health (MCH) handbook in Bangladesh. Journal of International Health 2009; 24: 73–76. [Google Scholar]
- 26.Tobe RG, Haque SE, Ikegami K, Mori R. Mobile-health tool to improve maternal and neonatal healthcare in Bangladesh: A cluster randomized controlled trial. BMC Pregnancy Childbirth. 2018; 18: 102. doi: 10.1186/s12884-018-1714-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sondaal SF, Browne JL, Amoakoh-Coleman M, Borgstein A, Miltenburg AS, Verwijs M, et al. Assessing the effect of mHealth interventions in improving maternal and neonatal care in low- and middle-income countries: A systematic review. PLoS One. 216; 11: e0154664. doi: 10.1371/journal.pone.0154664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akter T, Dawson A, Sibbritt D. Changes in neonatal mortality and newborn health-care practices: descriptive data from the Bangladesh Demographic and Health Surveys 2011 and 2014. Who South East Asia J Public Health. 2018; 7: 43–50. doi: 10.4103/2224-3151.228427 [DOI] [PubMed] [Google Scholar]
- 29.United Nations Children’s Fund (UNICEF). Key demographic indicators of Bangladesh, neonatal mortality rate. https://data.unicef.org/country/bgd/ (Accessed on August 14, 2020).
- 30.Rubayet S, Shahidullah M, Hossain A, Corbett E, Moran AC, Mannan I, et al. Newborn survival in Bangladesh: A decade of change and future implications. Health Policy and Planning. 2012; 27: iii40–iii56. doi: 10.1093/heapol/czs044 [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization. Newborns: Reducing mortality (fact sheets). Available at: https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality (Accessed on August 14, 2020).
- 32.Kikuchi K, Ansah EK, Okawa S, Enuameh Y, Yasuoka J, Nanishi K, et al. Effective linkages of continuum of care for improving neonatal, perinatal and maternal mortality: A systematic review and meta-analysis. PLoS One. 2015; 10: e0139288. doi: 10.1371/journal.pone.0139288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seward N, Neuman M, Colbourn T, Osrin D, Lewycka S, Azad K, et al. Effects of women’s groups practicing participatory learning and action on preventive and care-seeking behaviors to reduce neonatal mortality: A meta-analysis of cluster-randomized trial. PLoS Med. 2017; 14: e1002467. doi: 10.1371/journal.pmed.1002467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Amoakoh-Coleman M, Borgstein AB, Sondaal SF, Grobbee DE, Miltenburg AS, et al. Effectiveness of mHealth interventions targeting healthcare workers to improve pregnancy outcomes in low- and middle-income countries: A systematic review. J Med Internet Res. 2016; 18: e226. doi: 10.2196/jmir.5533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chanda SK, Ahammed B, Howlader MH, Ashikuzzaman M, Shovo T, Hossain MT. Factors associating different antenatal care contacts of women: A cross-sectional analysis of Bangladesh demographic and health survey 2014 data. PLoS One. 2020; 15: e0232257. doi: 10.1371/journal.pone.0232257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhowmik J, Biswas RK, Woldegiorgis M. Antenatal care and skilled birth attendance in Bangladesh are influenced by female education and family affordability: BDHS 2014. Public Health. 2019; 170: 113–121. doi: 10.1016/j.puhe.2019.02.027 [DOI] [PubMed] [Google Scholar]
- 37.Shahjahan M, Chowdhury HA, Al-Hadhrami AY, Harun GD. Antenatal and postnatal care practices among mothers in rural Bangladesh: A community based cross-sectional study. Midwifery. 2017; 52: 42–48. doi: 10.1016/j.midw.2017.05.011 [DOI] [PubMed] [Google Scholar]
- 38.Siddique AB, Perkins J, Mazumder T, Haider MR, Banik G, Tahsina T, et al. Antenatal care in rural Bangladesh: Gaps in adequate coverage and content. PLoS One. 2018; 13: e0205149. doi: 10.1371/journal.pone.0205149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pulok MH, Sabah MN, Uddin J, Enemark U. Progress in the utilization of antenatal and delivery care services in Bangladesh: Where does the equity gap lie? BMC Pregnancy Childbirth. 2016; 16: 200. doi: 10.1186/s12884-016-0970-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rahman MS, Rahman MM, Gilmour S, Swe KT, Abe SK, Shibuya K. Trends in, and projections of indicators of universal health coverage in Bangladesh, 1995–2030: A Bayesian analysis of population-based household data. Lancet Global Health. 2018; 6: e84–e94. doi: 10.1016/S2214-109X(17)30413-8 [DOI] [PubMed] [Google Scholar]
- 41.Rahman S, Choudhury AA, Khanam R, Moin SMI, Ahmed S, Begum N, et al. Effect of a package of integrated demand- and supply-side interventions on facility delivery rates in rural Bangladesh: Implications for large-scale programs. PLoS One 2017; 12: e0186182. doi: 10.1371/journal.pone.0186182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.United States Agency of International Development. Effective coverage of facility delivery in Bangladesh, Haiti, Malawi, Nepal, Senegal and Tanzania. DHS analytical studies 65. Available at: https://www.dhsprogram.com/pubs/pdf/AS65/AS65.pdf (Accessed on August 14, 2020). [DOI] [PMC free article] [PubMed]
- 43.Rahman MM, Haider MR, Moinuddin M, Rahman AE, Ahmed S, Khan MM. Determinants of cesarean section in Bangladesh: Cross-sectional analysis of Bangladesh demographic and health survey 2014 data. PLoS One. 2018; 13: e0202879. doi: 10.1371/journal.pone.0202879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Molina G, Weiser TG, Lipsitz SR, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA 2015; 314: 2263–2270. doi: 10.1001/jama.2015.15553 [DOI] [PubMed] [Google Scholar]
- 45.Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. World Health Organization Global Survey on Maternal and Perinatal Health Research Group Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet 2010; 375: 490–499. doi: 10.1016/S0140-6736(09)61870-5 [DOI] [PubMed] [Google Scholar]
- 46.Haider MR, Rahman MM, Moinuddin M, Rahman AE, Ahmed S, Khan MM. Ever-increasing cesarean section and its economic burden in Bangladesh. PLoS One. 2018; 13: e0208623. doi: 10.1371/journal.pone.0208623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marshall NE, Fu R, Guise JM. Impact of multiple cesarean deliveries on maternal morbidity: A systematic review. American Journal of Obstetrics and Gynecology. 2011; 205: 262.e1-8. doi: 10.1016/j.ajog.2011.06.035 [DOI] [PubMed] [Google Scholar]
- 48.Long Q, Kingdon C, Yang F, Renecle MD, Jahanfar S, Bohren MA, et al. Prevalence of and reasons for women’s, family members’, and health professionals’ preferences for cesarean section in China: A mixed-methods systematic review. PLoS Med. 2018; 15: e1002672. doi: 10.1371/journal.pmed.1002672 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.