Abstract
Context: Delayed, postoperative, spine infections are rare, most commonly occurring secondary to fastidious, less virulent pathogens. The etiology may involve a distant infectious focus, not related to the index operation. Patients may present months, or even years postoperatively with pain related to mechanical implant failure, often without additional signs of systemic infection.
Findings: We present the case of a 59-year-old male who developed rapid disk degeneration and implant failure seven months following instrumented lumbar fusion surgery. The causal organism was found to be Micromonas micros, an anaerobic bacterium typically located in the oral cavity and associated with periodontal disease. The patient was found to have extensive oral caries, which were presumed to have occurred secondary to poor oral hygiene and his use of fentanyl lozenges for chronic back pain. The patient was treated with revision staged spinal surgery and long-term intravenous antibiotics.
Conclusion/clinical relevance: This case highlights an unusual etiology of delayed postoperative spinal implant failure and provides evidence for periodontal disease as a source of hematogenous seeding in postoperative spinal infections. The orthopaedist should also be aware of the potential relationship between poor oral hygiene and the use of high sugar content fentanyl lozenges in treating chronic back pain in these patients.
Keywords: Spine surgery, Implant failure, Infection, Anaerobic, Micromonas
Introduction
Infections associated with spinal surgery are not uncommon with reported incidences ranging from 2 to 20%.1,2 Early infections, generally defined as occurring within 1 month of surgery, are typically due to inoculation during the index operation and are caused by virulent microorganisms such as Staphylococcus aureus, beta-hemolytic streptococci, and aerobic Gram-negative bacilli.1 Delayed postoperative spinal infections, occurring months to years after surgery, are much more infrequent and are often culture negative or caused by more fastidious pathogens such as Cutibacterium (Propionibacterium) acnes, Staphylococcus epidermidis, and Bacillus species.1 Many of these commonly implicated organisms are also capable of biofilm formation which may make the diagnosis and treatment much more difficult. Also, the presence of a biofilm can allow late presentation of an early colonization to occur, thus making it difficult to determine the chronicity of the infection.1 These patients often present with isolated pain or mechanical failure, and often do not show systemic signs of infection such as fevers, chills, or wound drainage. We present a patient who developed rapid disk degeneration and bone-implant interface failure seven months following instrumented fusion due to delayed infection with Micromonas (Peptostreptococcus) micros, an anaerobic organism often associated with periodontal disease.3–5 To our knowledge, this represents the second reported case of delayed spinal instrumentation failure caused by M. micros, and the first in a patient without recent history of dental extraction or periodontal procedure. In addition, this case is the first to our knowledge to highlight the use of oral fentanyl lozenges for chronic pain and their role in oral decay that may lead to hematogenous spread and subsequent spinal infection.
Case report
The patient is a 59-year-old man with a history of multiple spine surgeries including L4–5 posterior lumbar interbody instrumented fusion approximately 10 years prior to presentation, intrathecal analgesic (Duramorph) pump placement for refractory low back pain, and L3–L4 laminectomy for removal of a facet cyst at L3–4. He had initial relief of pain and an acceptable clinical result with each of the procedures but his pain worsened and his right lower extremity radiculopathy recurred. This was felt to be secondary to micro-instability and the development of Meyerding grade 1 degenerative spondylolisthesis at L3–L4. He subsequently underwent removal of L4–L5 instrumentation, L2–4 posterolateral instrumented fusion with L2–4 laminectomies with re-exploration of the L3–L4 interspace (Fig. 1). He had an uneventful hospital course and was discharged home on the 5th postoperative day. Throughout his postoperative course, the patient was treated for chronic low back pain with a combination of an intrathecal morphine pump and oral analgesics. Notably, his chronic lower back pain had been maintained with transmucosal (oral) fentanyl lozenges (Actiq, Teva Pharmaceuticals, North Wales, PA, USA), in addition to his intrathecal pump for many years, leading to poor dentition and dental caries due to their high sugar content.
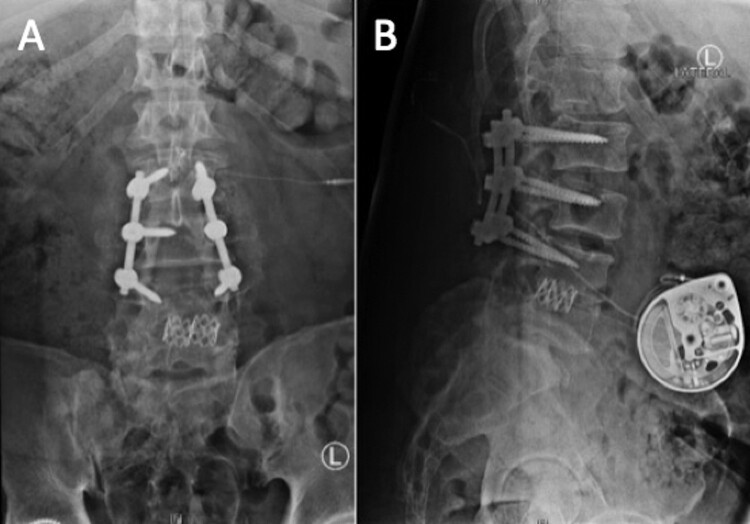
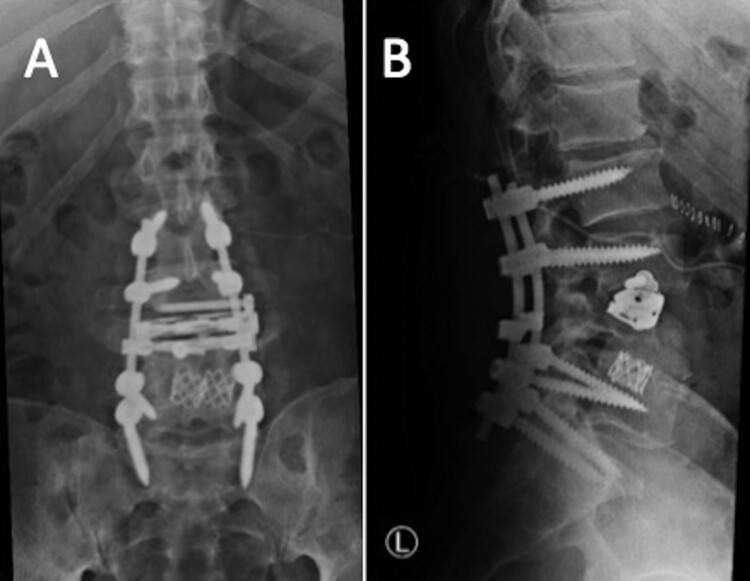
Figure 1.
(A) and (B) AP and lateral lumbar radiographs following the removal of L4–L5 instrumentation and L2–4 posterolateral instrumented fusion.
Six-week, 3-month, and 6-month follow-up visits showed appropriate healing radiographically. The patient then presented seven months post-operatively with increasing low back pain unrelieved by analgesics, including his intrathecal morphine pump. He denied any recent trauma, fevers, chills, leg pain, lower extremity weakness, or bowel or bladder dysfunction. Vital signs were within normal limits and he demonstrated no neurologic deficits on examination. Additionally, there was no erythema, drainage, or other outward signs of infection surrounding the surgical scars or the patient’s morphine pump. However, repeat radiographs revealed a new and profound collapse of the L3–4 disc space with associated spondylolisthesis and loss of fixation of the L4 pedicle screws bilaterally (Fig. 2). Laboratory evaluation revealed an elevated erythrocyte sedimentation rate of 107 mm/h, C-reactive protein of 117 mg/l, and a white blood cell count of 11,800 mm3 with 87% neutrophils.
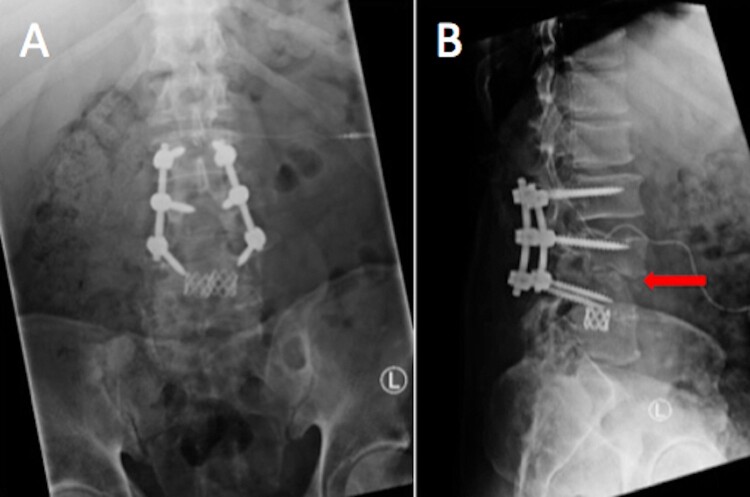
Figure 2.
(A) and (B) AP and lateral lumbar radiographs upon presentation, demonstrating collapse of the L3–4 disc space (arrow) with associated spondylolisthesis and loss of fixation of the L4 pedicle screws bilaterally.
Advanced outpatient imaging was ordered and the patient was prescribed a lumbosacral orthosis to provide temporary stability while further imaging was obtained. However, he was subsequently admitted to the hospital 48 h after this visit with new complaints of positional urinary incontinence while in the upright position and uncontrolled pain. Further imaging done on an urgent basis with magnetic resonance imaging (MRI) and computed tomography (CT) of the lumbar spine revealed fluid in the disc space and surrounding bone marrow edema suggestive of diskitis and osteomyelitis at the L3–4 level with loss of fixation and lucencies surrounding the L4 pedicle screws, in addition to a 1 × 1 cm right psoas abscess (Figs. 3 and 4). The following day, he underwent revision of posterior instrumentation and posterior spinal fusion from L2-S1 with iliac instrumentation followed by staged anterior column debridement, evacuation of the psoas abscess and cage placement from a direct lateral interbody approach to L3–L4 during the same admission (Fig. 5). Blood cultures on admission and four-out-of-five intraoperative spinal cultures grew M. micros. Upon further questioning, the patient related he had recently been evaluated for dental disease, but denied recent dental procedures or extractions. Dental consultation found extensive periodontal disease with decaying dentition and gingivitis, but no abscesses. The remainder of the patient’s hospital course was uncomplicated. He had a peripherally inserted central catheter placed and was discharged with a 6 week course of intravenous ertapenem 1 g daily, followed by 6 weeks of oral amoxicillin-clavulanic acid 875/125 mg every 12 h. His ESR and CRP both normalized with therapy. On outpatient follow up, the patient has mild persistent lower back pain but is neurologically intact and has regained bowel and bladder function. Imaging studies at the patient’s one-year follow up demonstrated a broken left S1 screw with otherwise intact hardware on radiographs and fusion at L3–4 and L4–5 on CT scan (Fig. 6). A slight lucency was noted around the left L2 screw, however this remained stable upon repeat CT performed 21 months post-surgery with no further signs of loosening. He was referred to an oral surgeon for extraction of multiple decayed teeth. He remains on suppressive oral amoxicillin 500 mg daily.
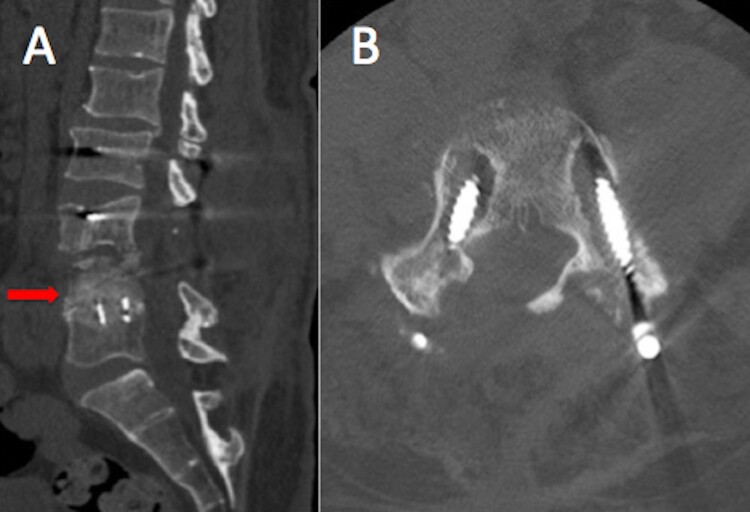
Figure 3.
(A) Sagittal computed tomography (CT) cut of the lumbar spine demonstrating complete collapse of the L3–4 disk space (arrow). (B) Axial CT cut at the L4 level demonstrating loss of pedicle screw fixation with lucency surrounding the L4 pedicle screws.
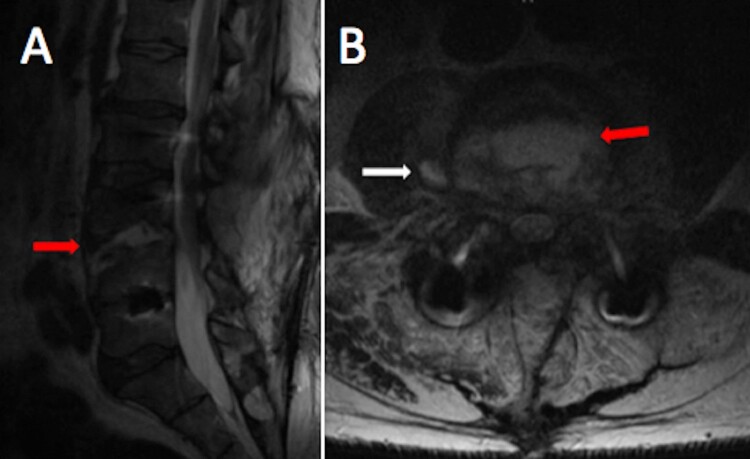
Figure 4.
(A) Sagittal T2 weighted magnetic resonance imaging (MRI) cut of the lumbar spine demonstrating fluid in the L3–4 disc space (arrow) and surrounding bone marrow edema. (B) Axial T2 weighted MRI cut at the level of the L4 superior endplate demonstrating bone marrow edema (thick arrow) and right psoas abscess (thin arrow).
Figure 5.
(A) and (B) AP and lateral lumbar radiographs following revision posterior instrumentation and fusion from L2-S1 with iliac instrumentation as well as staged anterior column debridement and L3–4 direct lateral interbody cage placement.
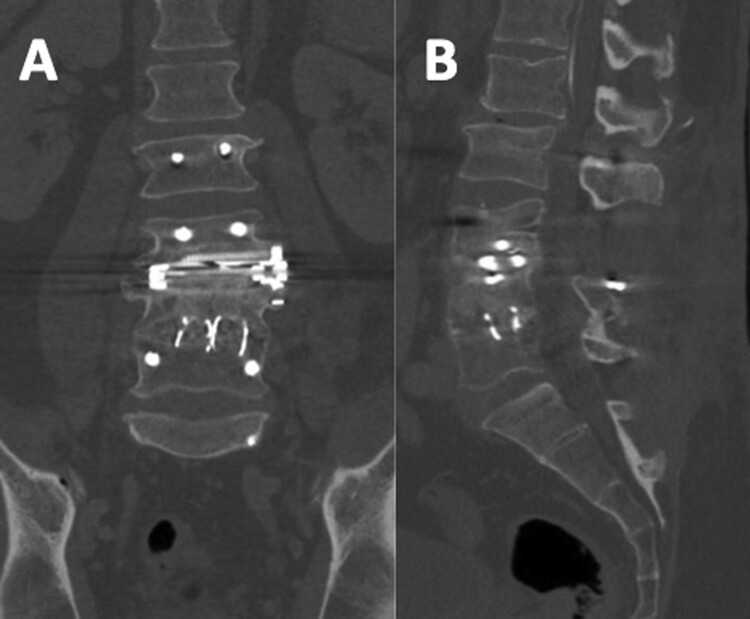
Figure 6.
(A) and (B) Coronal and sagittal CT cuts of the lumbar spine demonstrating fusion at L3–4 and L4–5. Note: Slight lucency surrounding the left L2 screw remained stable with follow-up imaging.
Discussion
Delayed postoperative spinal infections are relatively rare, and are often caused by less virulent and more fastidious organisms. C. acnes and S. epidermidis are the organisms most commonly implicated as the cause of these late infections.1 In this case, M. micros was isolated from the blood and operative tissue cultures and was considered the causative pathogen, presumably from an intraoral source. M. micros, formerly known as Peptostreptococcus micros and recently re-classified as Parvomonas micra, is an anaerobic gram-positive coccus that constitutes part of the normal flora of the human oral cavity, gastrointestinal, and genital tracts.6 M. micros is typically associated with periodontal disease and infections in the oral cavity.3–5 However, bacteremia, often following periodontal procedures such as tooth extractions,7,8 has been shown to cause infections in other areas of the body including sites of orthopedic implants such as prosthetic joints.9–11 Patients undergoing such procedures should therefore be closely monitored both with routine postoperative imaging as well as clinically to assess for any warning signs of infection.
Initial workup in the setting of suspected spinal infections should include plain radiographs as well as laboratory markers such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). These values, which are elevated in 90% or more of spinal infections, however, are relatively non-specific.12 Further imaging should include CT to assess osseous integrity as well as MRI to evaluate the disc space, neural elements, and extent of infection.12 In a clinically stable patient, empiric antibiotics may be withheld until operative cultures are obtained. No consensus exists with regards to the exact timing of surgery in the setting of infection, however one should proceed expediently in the case of sepsis due to overwhelming infection or in the case of acute neurologic compression. Current standard of care dictates that suspected cauda equina syndrome should be decompressed within 48 h to decrease the likelihood of permanent neurologic damage.13 In this case, the patient was initially neurologically and hemodynamically stable. He then, however, presented with acute loss of bowel and bladder function several days later, which prompted urgent surgical intervention for decompression and stabilization. Another option in this case would have been to treat the patient with implant removal, debridement, long-term antibiotics, and an external orthosis. However, given the extent of the infection and concerns for significant spinal instability following disc space debridement in a patient that had already developed a spondylolisthesis and bony erosive changes, the addition of instrumentation and an interbody implant was felt to better provide adequate stability to eradicate the infection and promote arthrodesis.
Spinal infections due to anaerobic pathogens are rarely reported. M. micros has been established through multiple case reports as a causative organism in spinal osteomyelitis and diskitis.6,14–18 However, these cases involve individuals without a history of spine surgery and instrumentation. Cases of delayed postoperative infection with M. micros in the setting of orthopaedic total joint implants are reported,9–11 however to our knowledge, only one case of a spinal hardware infection caused by M. micros has been reported in the literature.14 In the latter case, and in many of the periprosthetic joint infections caused by M. micros, a recent periodontal procedure was implicated as the precipitating event in bacterial seeding. In this case, the patient’s intrathecal morphine infusion pump was also considered as a potential source of infection. Nevertheless, it was felt to be unlikely given the anaerobic nature of the pathogen (Micromonas micros), which is strongly associated with the oral cavity, as well as the lack of drainage, erythema, or other signs of infection surrounding the morphine pump.
Our patient was found to have severe dental and periodontal disease, but denied any history of dental procedures or extractions. The patient did report excessive use of fentanyl lozenges since his last operation as an adjunct to help control his chronic low back pain. He temporally related the dental decay and periodontal disease to use of the lozenges. The high sugar content of the lozenges, combined with poor oral hygiene, was the most likely the mechanism for his condition. Other authors have published reports of the risk of development of dental caries with the use of fentanyl lozenges.19–21 The lozenges contain hydrated dextrates equivalent to approximately 2 g of glucose per lozenge. A mixture of a low pH environment in the oral cavity with fermentable carbohydrates and reduced salivary flow associated with opioids is theorized to promote rapid progression of dental caries. It is important to note, as this is a retrospective report, that the patient’s oral hygiene cannot be definitively established as the cause of the Micromonas infection. However, given the species that was isolated on intraoperative cultures, the patient’s significant dental findings as well as the association of this organism to the oral cavity, this is the most plausible theory.
Bacteremia caused by dental procedures and periodontal disease is extensively addressed in the adult reconstructive literature22,23 and the guidelines put forth by the American Academy of Orthopaedic Surgeons (AAOS).7 However, there remains a paucity of literature concerning the potential association between periodontal bacteremia and spinal infections. Studies have shown an incidence of bacteremia in up to 65% of patients undergoing dental extractions.7 Despite a lack of conclusive evidence to support the association between poor oral hygiene and prosthetic joint infections, many surgeons still require patients to be free of active dental infections prior to undergoing a joint reconstructive procedure. Likewise, there is no high-quality evidence to support or refute routine oral antibiotics prior to dental procedures following spinal instrumentation. While progression of the patient’s periodontal disease was thought to have precipitated the spinal infection in this case, the possibility of early colonization during the index operation with subsequent delayed presentation cannot be ruled out.
Our patient’s case highlights an unusual etiology of a delayed postoperative spinal infection causing implant failure and necessitating anterior and posterior revision surgery. There is a high prevalence of chronic back pain in patients undergoing spinal surgery, specifically instrumented spinal fusion,24,25 and fentanyl lozenges may be used as adjunct opioid analgesia in these patients. This case provides further evidence for periodontal disease as a potential source for postoperative spinal infection. Clinicians should therefore inquire about recent dental work as well as oral hygiene in patients presenting with delayed postoperative infections and consider anaerobic pathogens as potential causes. Anaerobic coverage should be included when treating these infections empirically. Chronic pain patients who are being considered for instrumented spinal fusion should be queried about use of fentanyl lozenges. Referral for dental evaluation may be a prudent component of the preoperative assessment in selected cases.
Disclaimer statements
Contributors None.
Funding None.
Conflict of interest Authors have no conflict of interests to declare.
References
- 1.Kasliwal MK, Tan LA, Traynelis VC.. Infection with spinal instrumentation: review of pathogenesis, diagnosis, prevention, and management. Surg Neurol Int. 2013;4(Suppl 5):S392–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olsen MA, Nepple JJ, Riew KD, Lenke LG, Bridwell KH, Mayfield J, et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am. 2008;90(1):62–69. doi: 10.2106/JBJS.F.01515 [DOI] [PubMed] [Google Scholar]
- 3.Sundqvist G. Associations between microbial species in dental root canal infections. Oral Microbiol Immunol. 1992;7(5):257–62. doi: 10.1111/j.1399-302X.1992.tb00584.x [DOI] [PubMed] [Google Scholar]
- 4.Dahlén G, Leonhardt A.. A new checkerboard panel for testing bacterial markers in periodontal disease. Oral Microbiol Immunol. 2006;21(1):6–11. doi: 10.1111/j.1399-302X.2005.00243.x [DOI] [PubMed] [Google Scholar]
- 5.Haffajee AD, Socransky SS.. Microbial etiological agents of destructive periodontal diseases. Periodontol 2000. 1994;5:78–111. doi: 10.1111/j.1600-0757.1994.tb00020.x [DOI] [PubMed] [Google Scholar]
- 6.Uemura H, Hayakawa K, Shimada K, Tojo M, Nagamatsu M, Miyoshi-Akiyama T, et al. Parvimonas micra as a causative organism of spondylodiscitis: a report of two cases and a literature review. Int J Infect Dis. 2014;23:53–55. doi: 10.1016/j.ijid.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 7.Watters W, Rethman MP, Hanson NB, Abt E, Anderson PA, Carroll KC, et al. Prevention of orthopaedic implant infection in patients undergoing dental procedures. J Am Acad Orthop Surg. 2013;21(3):180–9. doi: 10.5435/JAAOS-21-03-180 [DOI] [PubMed] [Google Scholar]
- 8.Otten JE, Pelz K, Christmann G.. Anaerobic bacteremia following tooth extraction and removal of osteosynthesis plates. J. Oral Maxillofac Surg. 1987;45:477–80. doi: 10.1016/S0278-2391(87)80005-8 [DOI] [PubMed] [Google Scholar]
- 9.Riesbeck K, Sanzén L.. Destructive knee joint infection caused by Peptostreptococcus micros: importance of early microbiological diagnosis. J Clin Microbiol. 1999;37(8):2737–9. doi: 10.1128/JCM.37.8.2737-2739.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartz H, Nonnenmacher C, Bollmann C, Kuhl M, Zimmermann S, Heeg K, et al. Micromonas (Peptostreptococcus) micros: unusual case of prosthetic joint infection associated with dental procedures. Int J Med Microbiol. 2005;294(7):465–70. doi: 10.1016/j.ijmm.2004.10.001 [DOI] [PubMed] [Google Scholar]
- 11.Stoll T, Stucki G, Brühlmann P, Vogt M, Gschwend N, Michel BA.. Infection of a total knee joint prosthesis by peptostreptococcus micros and propionibacterium acnes in an elderly RA patient: implant salvage with long-term antibiotics and needle aspiration/irrigation. Clin Rheumatol. 1996;15(4):399–402. doi: 10.1007/BF02230366 [DOI] [PubMed] [Google Scholar]
- 12.Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP.. Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine. 2000;25(12):1515–22. doi: 10.1097/00007632-200006150-00010 [DOI] [PubMed] [Google Scholar]
- 13.An HS, Seldomridge JA.. Spinal infections: diagnostic tests and imaging studies. Clin Orthop Relat Res. 2006;443:27–33. doi: 10.1097/01.blo.0000203452.36522.97 [DOI] [PubMed] [Google Scholar]
- 14.George IA, Pande A, Parsaei S.. Delayed infection with Parvimonas micra following spinal instrumentation. Anaerobe. 2015;35(Pt B):102–4. doi: 10.1016/j.anaerobe.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 15.Frat JP, Godet C, Grollier G, Blanc JL, Robert R.. Cervical spinal epidural abscess and meningitis due to Prevotella oris and Peptostreptococcus micros after retropharyngeal surgery. Intensive Care Med. 2004;30(8):1695. doi: 10.1007/s00134-004-2265-x [DOI] [PubMed] [Google Scholar]
- 16.Bielecki DK, Sartoris D, Resnick D, Van lom K, Fierer J, Haghighi P.. Intraosseous and intradiscal gas in association with spinal infection: report of three cases. AJR Am J Roentgenol. 1986;147(1):83–86. doi: 10.2214/ajr.147.1.83 [DOI] [PubMed] [Google Scholar]
- 17.Leder KS, Barlam TF.. A case of paraspinal abscess and diskitis due to Peptostreptococcus micros. Clin Infect Dis. 2000;30(3):622–3. doi: 10.1086/313735 [DOI] [PubMed] [Google Scholar]
- 18.Papasian CJ, Mcgregor DH, Hodges GR, Kennedy J.. Peptostreptococcal vertebral osteomyelitis. J Clin Microbiol. 1986;24(4):633–5. doi: 10.1128/jcm.24.4.633-635.1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mandel L, Carunchio MJ.. Rampant caries from oral transmucosal fentanyl citrate lozenge abuse. J American Dental Assoc. 2011;142(4):406–9. doi: 10.14219/jada.archive.2011.0195 [DOI] [PubMed] [Google Scholar]
- 20.Wynn RL. The sugar-loaded fentanyl lollipop (Actiq) and the risk for tooth decay. Gen Dent. 2011;59(3):168–70. [PubMed] [Google Scholar]
- 21.Sharma V, Miah M, Cameron M.. Lozenge risks. Br Dental J. 2012;213:199. doi: 10.1038/sj.bdj.2012.788 [DOI] [PubMed] [Google Scholar]
- 22.Laporte DM, Waldman BJ, Mont MA, Hungerford DS.. Infections associated with dental procedures in total hip arthroplasty. J Bone Joint Surg Br. 1999;81-B(1):56–59. doi: 10.1302/0301-620X.81B1.0810056 [DOI] [PubMed] [Google Scholar]
- 23.Waldman BJ, Mont MA, Hungerford DS.. Total knee arthroplasty infections associated with dental procedures. Clin Orthop Relat Res. 1997;343:164–72. doi: 10.1097/00003086-199710000-00027 [DOI] [PubMed] [Google Scholar]
- 24.Mirza SK, Deyo RA.. Systematic review of randomized trials comparing lumbar fusion surgery to nonoperative care for treatment of chronic back pain. Spine. 2007;32(7):816–23. doi: 10.1097/01.brs.0000259225.37454.38 [DOI] [PubMed] [Google Scholar]
- 25.Phillips FM, Slosar PJ, Youssef JA, Andersson G, Papatheofanis F.. Lumbar spine fusion for chronic low back pain due to degenerative disc disease: a systematic review. Spine. 2013;38(7):E409–22. doi: 10.1097/BRS.0b013e3182877f11 [DOI] [PubMed] [Google Scholar]