Abstract
Objective: Determine the prevalence of lateral epicondylosis (LE) of the dominant elbow in manual wheelchair users based on ultrasound assessment and physical exam.
Design: Prospective, cross-sectional.
Setting: National Veteran Wheelchair Games 2018 and 2019 (event medical services).
Participants: Manual wheelchair users who attended the National Veteran Wheelchair Games (n = 87).
Interventions: Participants completed a questionnaire then underwent an ultrasound assessment and a physical exam of their dominant arm evaluating for common extensor tendinopathy (CET) or clinically LE.
Main Outcome Measure: Prevalence of CET diagnosed by ultrasound criteria was compared with other diagnostic criteria with MaNemar test for paired binary data.
Results: Forty-six percent (N = 40) of participants met diagnostic criteria for CET by ultrasound assessment and 17% (N = 15) of participants met criteria for LE based on physical exam. These values are dramatically higher than what has been reported in the able-bodied population where the prevalence is estimated to be <2%. Age and number of years of wheelchair use were significant predictors of ultrasound diagnosis of LE (P = 0.02, 95% confidence interval [CI] 1.01–1.11) and (P = 0.05, 95% CI 1.00–1.09), respectively. Association analysis based on odds ratio and CI found no association between ultrasound findings suggestive of LE with regular adaptive sport participation greater than 1.5 h per week.
Conclusion: Compared to able-bodied population, there is an increased prevalence of both CET and LE in manual wheelchair users based on either ultrasound assessment or physical exam. CET is associated with increased age and increased years using a manual wheelchair. There is no association between the diagnosis of LE and participation in adaptive sport.
Keywords: Lateral epicondylosis, Wheelchair user, Ultrasound, Adaptive sport
Introduction
Lateral epicondylosis (LE) or “tennis elbow” is a degenerative process related to the repetitive wrist and arm motions.1,2 Prior studies estimate that the prevalence of LE in the general population is about 1.3%, but the prevalence of LE is in manual wheelchair users in generally unknown.3 Biomechanically, the extensor carpi radialis brevis tendon that inserts at the lateral epicondyle is under maximal force during forearm pronation, wrist flexion and ulnar deviation.2 Widely accepted physical exam maneuvers for LE include the Cozen’s test and Mill’s test.2 A previous study validated these tests with comparisons to ultrasonographic findings suggestive of LE, concluding that Cozen’s test was effective at ruling out LE (sensitivity 84%, specificity 0%) whereas Mill’s test was an appropriate maneuver to rule-in LE (sensitivity 53%, specificity 100%).2
Previous studies in able-bodied individuals have shown tennis playing as a risk factor in LE.4 With regard to relevance for adaptive sports, which is often played at a wheelchair-level, a study by Roy et al. showed that there was no increased risk of LE observed in wheelchair tennis players as compared to non-tennis playing wheelchair users.5 A secondary finding of that study was that the duration of wheelchair use was a significant predictor of LE in manual wheelchair users, regardless of tennis playing. Manual wheelchair users are dependent on their upper extremities for mobility and other activities of daily living. Studies have shown chronic conditions of the shoulder and wrist joints related to wheelchair use, but fewer studies focus on the prevalence of elbow pain and its etiologies. Unspecified elbow pain has been reported in 33% of individuals with wheelchair use due to paraplegia.6
LE remains a clinical diagnosis, however, ultrasound evaluation of the elbow may reveal calcifications, tears, bony irregularity of the lateral epicondyle and thickening and heterogenicity of the common extensor tendon, all findings suggestive of LE.7,8 Although LE is a clinical diagnosis, ultrasound is being used to confirm this with physical exam findings. For example, a common extensor tendon thickness of 4.2 mm or greater correlates well with LE.9 Previous interobserver studies examining tendon thickness, color doppler activity and bony spurs found good to excellent reliability for all measurements.8,10 Ultrasound findings of hypoechogenicity of the extensor tendon complex and bony changes indicate increased stress of the common extensor tendon at the lateral epicondyle as seen with LE.11 A previous study in the able-bodied population found that the common extensor tendon of the dominant elbow in asymptomatic, able-bodied individuals was thicker as compared to the nondominant elbow in males as compared to females but with no age correlation.12
In this study, we hypothesized that the prevalence of LE, based on ultrasound assessment and physical exam of the dominant elbow, would be higher in manual wheelchair users than what has previously been reported in able-bodied individuals. We further hypothesized that participation in regular adaptive sports would increase the risk of LE. Finally, based on previous work by Roy et al., we hypothesized that increased years of manual wheelchair use would be associated with increased risk of ultrasound findings suggestive of LE.5
Methods
Participants
This study was a prospective, cross-sectional study conducted at the 2018 and 2019 National Veteran Wheelchair Games in Orlando, FL, and Louisville, KY, respectively. Participants were recruited throughout the duration of the games as attendees. This study was approved by the Institutional Review Board within Clement J. Zablocki Veteran Affairs Medical Center including ethical approval by the VA Privacy Office. All participants signed written informed consent prior to study participation. Inclusion criteria included age 18 years or older, male or female, were able to provide consent and use a manual wheelchair as their primary means of mobility in the community. Exclusion criteria included a history of significant trauma to the elbow, abnormal elbow anatomy, were unable to provide consent, or persons who do not use a manual wheelchair as their primary means of mobility in the community.
Questionnaire
Each participant completed a survey on (1) demographics including age, sex, race/ethnicity, and history of elbow injury, (2) cause of injury leading to wheelchair use, (3) designation as athlete vs non-athlete based on regular adaptive sport participation defined as more than 1.5 h per week, (4) number of years as a wheelchair user, and (5) subjective elbow pain.
Ultrasound assessment
The dominant arm of each participant was examined by a Physical Medicine and Rehabilitation or Sports Medicine board-certified, ultrasound-trained physician to evaluate for (1) tendon thickening (defined as > 4 mm), (2) increased vascularity as seen by Doppler, and (3) extensor tendon hypoechogenicity. Currently, there are no standardized ultrasound criteria for the diagnosis of LE. While each ultrasound abnormality listed above may individually suggest a common extensor tendinopathy (CET), multiple internally consistent abnormalities are more convincing than isolated abnormalities, which raise the possibility of technical mishap. Therefore, a diagnosis of common extensor tendinopathy by ultrasound examination was given if there was the presence of at least two of three above-mentioned criteria.13 The examiner also assessed for the presence of calcifications at the common extensor insertion site, cortical irregularities, or presence of a common extensor tendon tear. The dominant elbow was examined using a SonoSite M-Turbo (SonoSite, Bothell, Washington) or GE LOGIQ e (GE Healthcare, Chicago, IL), both portable high-resolution ultrasound machines, using a linear transducer high-frequency probe.
Physical exam
A focused physical exam of the dominant elbow of each participant was conducted by a licensed physician assessing for tenderness to palpation at the lateral epicondyle and reproducible lateral epicondyle pain with Cozen’s test and Mill’s test. Mill’s test required the participant’s elbow to be flexed at 90 degrees, their forearm pronated, and wrist fully flexed while the examiner extended the elbow slowly. Cozen’s test was performed with the participant’s elbow fully extended and forearm pronated, and the examiner provided resistance to active wrist extension. A positive test for either maneuver included a reproduction of pain at the lateral epicondyle or within 2 cm distal to the tendon insertion site.2 For greater sensitivity and specificity of our clinical assessment, a positive diagnosis of LE was established if two of three physical exam maneuvers elicited elbow pain.13,14
Statistical analyses
The primary outcome measure was the prevalence of CET in manual wheelchair users based on ultrasound assessment or LE based on physical exam. Prevalence of CET as diagnosed by ultrasound criteria was compared with other diagnostic criteria with McNemar’s test for paired binary data. Sample proportions were reported with exact 95% binomial confidence intervals. Associations between diagnostic results and categorical variables (sex, age, race/ethnicity, regular adaptive sport participation, cause of injury, and years as a wheelchair user) were tested with Fisher’s exact test. Continuous variables such as age and years of wheelchair use were compared between patients’ groups (two groups) using Welch two-sample t-test. Group specific means were summarized by means and standard deviations (SDs); 95% confidence intervals (CIs) based on t-distributions were reported. Prevalence of LE in manual wheelchair users was compared to the prevalence in able-bodied population as defined in previous studies with a binomial test. A P-value < 0.05 was considered statistically significant.
Results
Eighty-seven participants completed the questionnaire and examinations. The average age of the individuals was 56 ± 12years (Table 1). Types of injuries included spinal cord injuries (n = 58; 67%), lower-extremity amputation (n = 19; 22%), and “other” (which included multiple sclerosis, other neurological condition or traumatic brain injury) (n = 9; 10%) (Table 2). The average time using a manual wheelchair was 16 ± 13 years (Table 2). Eight participants did not disclose race/ethnicity, one participant did not disclose injury type and ten participants did not provide a number of years as a wheelchair user. Self-reported elbow pain of the dominant side at the time of the study was reported in 25% of participants (N = 22). Seventy-three percent of participants (N = 62) indicated that they participate in adaptive sports regularly (defined as more than 1.5 h a week) (Table 2).
Table 1. Demographics of participants.
| Characteristic | Total N = 87 |
|---|---|
| Age | |
| Mean (SD) | 56 ± 12 years |
| Median | 58 |
| Sex | |
| Male | 78 males (90%) |
| Female | 9 females (10%) |
| Race/ethnicity | |
| Caucasian | N = 49 (56%) |
| African American | N = 16 (18%) |
| Latino | N = 10 (11%) |
| Asian | N = 3 (3%) |
| Undisclosed | N = 9 (10%) |
Table 2. Characteristics of participants based on questionnaire.
| Characteristic | Total |
|---|---|
| Dominant elbow | |
| Right | N = 71 (82%) |
| Left | N = 16 (18%) |
| Type of injury | |
| Spinal cord injury | N = 58 (67%) |
| Lower extremity amputee | N = 19 (22%) |
| Neurological | N = 9 (10%) |
| Years a wheelchair user | |
| Mean (SD) | 16 ± 13 years |
| Median | 13 |
| Adaptive sport | |
| Athlete | 62 (73%) |
| Non-athlete | 23 (27%) |
| History of elbow injury | |
| Yes | 28 (33%) |
| No | 58 (67%) |
| Elbow Pain | |
| Yes | 22 (26%) |
| No | 64 (74%) |
Prevalence of ultrasound diagnosis of common extensor tendinopathy (CET) among wheelchair users was compared to estimated prevalence in the general population (1.3% using physical exam criteria).3 Forty-six percent (N = 40) of participants met diagnostic criteria for CET via ultrasound assessment by meeting two of three diagnostic criteria: (1) tendon thickening, (2) increased vascularity, and (3) hypoechogenicity. Paired analysis revealed an association between CET and the presence of calcifications (P < 0.005). Seventeen percent (N = 15) of participants met criteria for LE based on physical exam. Based on our findings, there was an increased rate of CET by ultrasound assessment, as compared to LE by physical exam (Tables 3 and 4).
Table 3. Number of participants with or without ultrasound findings suggestive of LE.
| Ultrasound | (+) Present | (−) Not present |
|---|---|---|
| Tendon thickening (>4 mm) | 57 | 30 |
| Increased vascularity | 10 | 77 |
| Hypoechoic | 50 | 37 |
Table 4. Number of participants with or without positive exam maneuvers clinically suggestive of LE.
| Physical exam | (+) Positive | (−) Negative |
|---|---|---|
| Tender to palpation | 20 | 67 |
| Cozen’s test | 13 | 74 |
| Mill’s test | 13 | 74 |
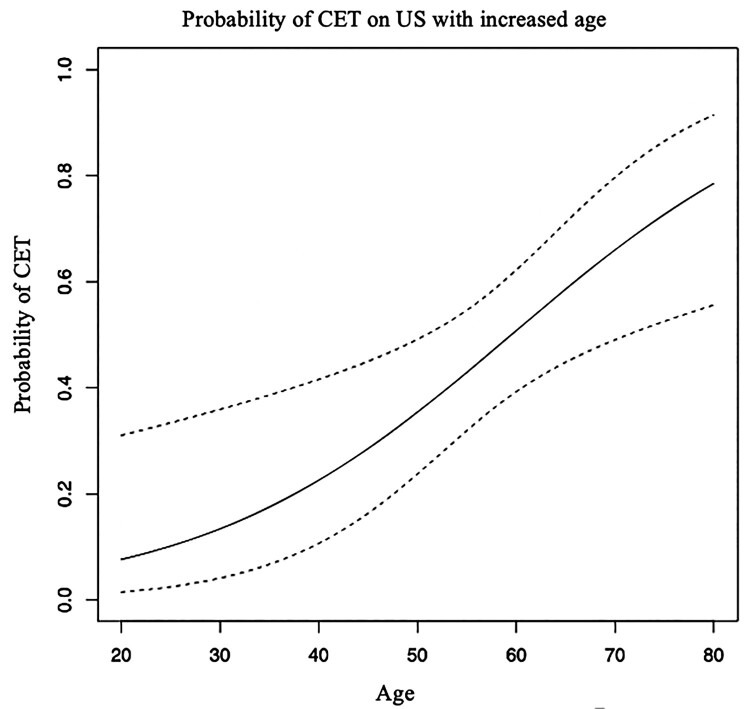
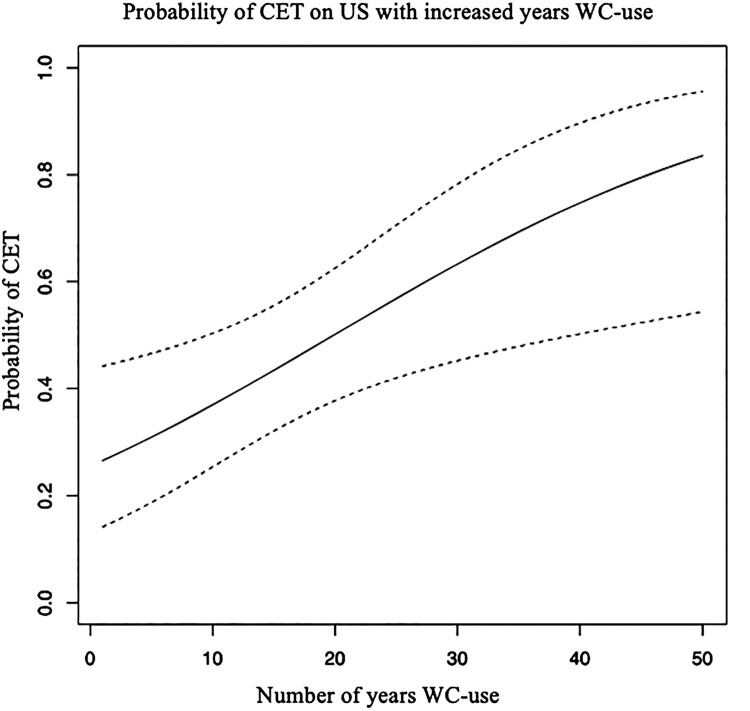
Using logistic regression models, increased age and number years of wheelchair use were significant predictors for ultrasound findings suggestive of LE (Figs. 1 and 2). Mean age for participants with ultrasound findings of CET was 61 years (SD 10.4) and mean age without ultrasound diagnosis of CET was 52.5 years (SD 12.6). Age was a significant predictor of ultrasound findings suggestive of LE, odds ratio 1.01 per year (P = 0.02, 95% CI 1.01–1.11) (Fig. 1). Number of years of wheelchair use was also a significant predictor of ultrasound findings suggestive of LE, (P = 0.05, 95% CI 1.00-1.09) (Fig. 2). Odds ratio for ultrasound findings of CET as a result of number of years of wheelchair use was 1.009 per year of wheelchair use. There was a mean duration of 21 years (SD 14) of wheelchair use for those with ultrasound findings suggestive of LE as compared to mean duration of 12 years (SD 10) for those without ultrasound findings.
Figure 1.
Predicted probability for diagnosis of LE in manual wheelchair users as adjusted by age.
Figure 2.
Predicted probability for diagnosis of LE in manual wheelchair users as adjusted by number of years using a manual wheelchair.
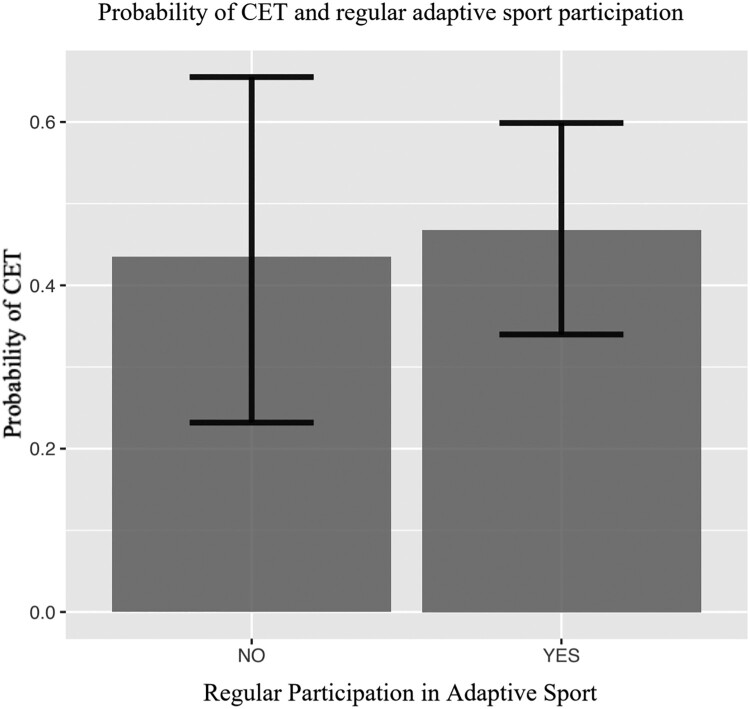
Association analysis based on odds ratio and confidence interval found no association between ultrasound diagnosis of common extensor tendinopathy and various demographic information including sex, race/ethnicity, prior history of an elbow injury, regular adaptive sport participation (Fig. 3), or injury type (comparing spinal cord injury, amputee and “other” which included multiple sclerosis, other neurological condition or traumatic brain injury).
Figure 3.
Probability of positive ultrasound findings suggestive of LE in adaptive sport athletes who participate in regular sport vs. non-athletes. There was no difference noted between groups.
Discussion
The novel findings in our study are three-fold. First, the prevalence of LE in manual wheelchair users was dramatically higher than published norms in able-bodied individuals. Based on the physical exam alone, the prevalence of LE was 17% among manual wheelchair users. The prevalence of ultrasound-abnormalities (increased tendon thickness >4 mm, tendon hypoechogenicity, and hypervascularity) as seen in LE was 46% among manual wheelchair users. While these ultrasound findings suggest LE in a symptomatic individual, this likely represents an asymptomatic common extensor tendinopathy in an individual with no symptoms of elbow pain.12 Although LE remains a clinical diagnosis based on presentation and symptoms, both of these prevalence values are in stark comparison to able-bodied individuals, where the prevalence of LE has been cited to be approximately 1.3% of the general population.3 Second, this study found that increased age and number of years using a wheelchair placed individuals at higher risk of acquiring common extensor tendinopathy (Figs. 1 and 2). Finally, we found no association between the presence of common extensor tendinopathy and regular adaptive sport participation defined as more than 1.5 h a week (Fig. 3).
It is expected that acute elbow pain at the lateral epicondyle would present with clinical symptoms such as swelling, pain, and positive exam maneuvers. LE as a tendinopathy is defined as a degenerative, overuse condition and would likely have abnormal structural findings as seen with an ultrasound assessment, as a result of repetitive damage and repair to the area.14 The sensitivities and specificities for ultrasound findings of LE for abnormalities including increased vascularity, bony irregularities, and tendon thickening are considered for chronic conditions.11
Surveillance and early intervention of musculoskeletal conditions in the upper extremity among manual wheelchair users may halt progressive symptoms that could negatively affect a manual wheelchair user’s level of independence or social and emotional well-being. Utilizing an ultrasound for diagnostic purposes of the elbow is an easy, quick and accessible tool to use in the clinic setting, although requires proper operator skill and experience. A diagnostic ultrasound assessment used in conjunction with a standard physical exam would be the ideal evaluation, however, a physical exam alone could still provide valuable information. Based on these findings, it is recommended to have a high degree of suspicion for LE in manual wheelchair users with elbow pain and early intervention for injury prevention is warranted. The biomechanics of wheelchair use is exceptionally important when treating musculoskeletal injuries of the upper extremities in this population. As an overuse condition, the development of LE may be related to wheelchair mobility and transfers. This study did not investigate which activities worsened clinical symptoms but should be considered with the clinical evaluation of elbow pain. There is evidence that with proper training of wheelchair transfer and propulsion techniques, the biomechanics of the upper extremity, including force through the elbow, can be favorably altered.15,16 Personalized training on proper transfer techniques may significantly reduce the range of motion and force reductions of the elbow during transfers, reducing elbow pain and other conditions such as ulnar neuropathy.16 Optimal seat position of a manual wheelchair may also minimize stress on the upper extremities by maintaining protective elbow angles during wheelchair propulsion.17 Most literature on manual wheelchair biomechanics focuses on the shoulder joint, but the loading of all the upper extremity joints are highly correlated to each other with manual wheelchair propulsion and transfers.16 If needed in the treatment of LE, further conservative management usually includes nonsteroidal anti-inflammatory drugs, orthotics (counter-force bracing), and therapy focusing on eccentric exercises.13 If conservative management fails to improve symptoms, a number of minimally invasive procedures may be considered such as tenotomy and injections with corticosteroid or platelet-rich plasma.1,13 Surgical repair is performed in about 2–4% of all cases in the general population.1,18
Previous studies show high sensitivity but low specificity with a correlation of ultrasonographic findings of the common extensor tendon and symptomatic LE.19 Ultrasound assessment is perhaps more sensitive to pathological changes that are known to occur with symptomatic LE and arguably, with a vulnerable population such as manual wheelchair users, it may be advised to closely monitor those with abnormal ultrasonographic findings to suggest a tendinopathy to prevent progression to a chronic condition (LE). Given no association between the ultrasound-diagnosis of common extensor tendinopathy and pain or positive physical exam maneuvers in this study, it would be interesting to study asymptomatic individuals with ultrasound diagnosis of common extensor tendinopathy longitudinally to determine if they later develop clinical symptoms of LE.
Although there is fair to excellent consistency among examiners specifically regarding the measurement of the common extensor tendon, it is worth mentioning that ultrasound assessment is highly dependent on variables such as operator experience, equipment, and stage of pathology.20 It is likely best practice to combine clinical judgement with a physical exam while supplementing use of diagnostic ultrasound for management of LE.
Given the high prevalence of upper extremity pain symptoms in manual wheelchair users, we wanted to investigate whether regular participation in adaptive sport increases the risk of LE. This study considered a participant an “athlete” if they indicated regular participation in adaptive sports, defined as participation in any sports more than 1.5 h a week. It is worth noting that although participants in this study were recruited at a national-level adaptive sport event, several attendees do not participate in adaptive sport regularly. A threshold of 1.5 h per week of adaptive sport participation was chosen based on physical activity guidelines for the spinal cord injury population from 2018 that recommends at least 20 min of moderate to vigorous intensity aerobic activity twice a week with strength-training exercises twice a week, or for cardiometabolic health benefits 30 min of moderate to vigorous intensity aerobic exercise 3 times per week is recommended.21 Based on these guidelines, 1.5 h of adaptive sport per week would identify individuals who meet recommended SCI guidelines for physical activity. Unfortunately, individuals with spinal cord injury are a physically inactive population, with nearly 49% of individuals with a spinal cord injury reporting no physical activity.22–24 Similarly, another study found that 54% of adults with physical disabilities do not participate in any physical activity.25 In our study, 27% of our participants do not meet standard physical activity guidelines for the SCI population despite recruitment at a national sporting event. Based on the prevalence of common extensor tendinopathy among “athletes” and “non-athletes”, our results indicated there was no increased risk of CET association with regular participation in adaptive sport. A pilot study by Roy et al., investigating the risk of LE among wheelchair users who play tennis, found a similar finding that there was no increased risk of LE associated with tennis playing among manual wheelchair users. This is reassuring, as there are known benefits for organized sports for individuals with a disability through adaptive sport opportunities. These include physical and psychological benefits such as increased strength and balance, mood regulation, maintenance of healthy weight, social engagement and enhancing emotional well-being through adaptive sport.26,27
Limitations/Future directions
Each ultrasound assessment was performed by one of three ultrasound-trained physicians with previous ultrasound experience. The intrarater and interrater reliability of diagnosis of LE were not assessed in this study. Recruitment of participants was limited to the National Veteran Wheelchair Games which has prior screening protocol for eligible participants. This may have led to a selection bias of more active and independent manual wheelchair users compared to the non-active wheelchair user. All participants disclosed that they use manual wheelchairs as their primary means of mobility, but with varying amounts of wheelchair use leading to differences in upper extremity reliance for mobility (i.e. amount of wheelchair use for complete paraplegia vs lower extremity amputation). Recall bias was a limitation due to participants self-reporting on the questionnaire. This study did not obtain information regarding participant occupation status or type and volume of sport participation but may be an area for further investigations. Further research is recommended to determine if the amount and type of physical activity influence musculoskeletal conditions such as LE. Furthermore, this study did not determine the duration of any clinical symptoms related to the elbow to differentiate between an acute or chronic condition as it pertains to ultrasound findings. Only the dominant elbow was assessed in this study, but there is no previously published data as to whether the dominant or non-dominant elbow is more prone to overuse injuries in manual wheelchair users.
Conclusion
Compared to previously published meta-analysis with able-bodied individuals, there is a dramatic increase in structural abnormalities that the authors believe may lead to LE in manual wheelchair users. Increased age and increased number of years of wheelchair use were both significant predictors of increased prevalence of common extensor tendinopathy. Participation in adaptive sport did not increase risk of LE. Ultrasound evaluation of the lateral epicondyle in manual wheelchair users can be used to better assess the population most at risk of developing symptomatic LE.
Acknowledgements
We thank Dr. Matt Durand and Rachel Minkin (Medical College of Wisconsin) for their guidance and also acknowledge Dr. Vivian Roy (Shirley Ryan AbilityLab) as her original research helped create this study.
Disclaimer statements
Contributors None
Funding The funding was provided by the Research Administration Committee (RAC) in the Department of Physical Medicine and Rehabilitation at the Medical College of Wisconsin.
Conflicts of interest Authors have no conflict of interests to declare.
References
- 1.Degen RM, Conti MS, Camp CL, Altchek DW, Dines JS, Werner BC.. Epidemiology and disease burden of lateral epicondylitis in the USA: analysis of 85,318 patients. HSS J 2018;14(1):9–14. doi: 10.1007/s11420-017-9559-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saroja G, Leo A, venkata sai P.. Diagnostic accuracy of provocative tests in lateral epicondylitis. Int J Physiother Res 2014;2:815–23. doi: 10.16965/ijpr.2014.699 [DOI] [Google Scholar]
- 3.Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M.. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol 2006;164(11):1065–74. doi: 10.1093/aje/kwj325 [DOI] [PubMed] [Google Scholar]
- 4.Kitai E, Itay S, Ruder A, Engel J, Modan M.. An epidemiological study of lateral epicondylitis (tennis elbow) in amateur male players. Ann Chir Main 1986;5(2):113–21. doi: 10.1016/S0753-9053(86)80023-0 [DOI] [PubMed] [Google Scholar]
- 5.Roy V, Lee L, Uihlein M, Roy I, Lee K.. Ultrasonographic comparison of the lateral epicondyle in wheelchair-user (and able-bodied) tennis players: a pilot study. J Spinal Cord Med 2019: 1–8. doi: 10.1080/10790268.2019.1603898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kentar Y, et al. Prevalence of upper extremity pain in a population of people with paraplegia. Spinal Cord 2018;56(7):695–703. doi: 10.1038/s41393-018-0062-6 [DOI] [PubMed] [Google Scholar]
- 7.Maffulli N, Regine R, Carrillo F, Capasso G, Minelli S.. Tennis elbow: an ultrasonographic study in tennis players. Br J Sports Med 1990;24(3):151–5. doi: 10.1136/bjsm.24.3.151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teggeler M, Schmitz M, Fink A, Jansen JA, Pisters MF.. Reliability and agreement of ultrasonographic thickness measurements of the common lateral extensors of the elbow. Ultrasound Med Biol 2015;41(6):1592–8. doi: 10.1016/j.ultrasmedbio.2015.01.018 [DOI] [PubMed] [Google Scholar]
- 9.Lee MH, Cha JG, Jin W, Kim BS, Park JS, Lee HK, Hong HS.. Utility of sonographic measurement of the common tensor tendon in patients with lateral epicondylitis. AJR Am J Roentgenol 2011;196(6):1363–7. doi: 10.2214/AJR.10.5769 [DOI] [PubMed] [Google Scholar]
- 10.Krogh TP, Fredberg U, Christensen R, Stengaard-Pedersen K, Ellingsen T.. Ultrasonographic assessment of tendon thickness, Doppler activity and bony spurs of the elbow in patients with lateral epicondylitis and healthy subjects: a reliability and agreement study. Ultraschall Med 2013;34(5):468–74. doi: 10.1055/s-0033-1335951 [DOI] [PubMed] [Google Scholar]
- 11.Dones VC 3rd, Grimmer K, Thoirs K, Suarez CG, Luker J.. The diagnostic validity of musculoskeletal ultrasound in lateral epicondylalgia: a systematic review. BMC Med Imaging 2014;14:10. doi: 10.1186/1471-2342-14-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krogh TP, Fredberg U, Ammitzbol C, Ellingsen T.. Ultrasonographic characteristics of the common extensor tendon of the elbow in asymptomatic individuals: thickness, color Doppler activity, and bony spurs. Orthop J Sports Med 2017;5(5). 2325967117704186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N.. Lateral epicondylitis. Bone Joint J 2013;95-B(9):1158–64. doi: 10.1302/0301-620X.95B9.29285 [DOI] [PubMed] [Google Scholar]
- 14.Buchanan BK, Varacallo M.. Tennis elbow (lateral epicondylitis). In: Statpearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. Available from https://www.ncbi.nlm.nih.gov/books/NBK431092/ [PubMed] [Google Scholar]
- 15.van der Woude LHV, Veeger HEJ, Dallmeijer AJ, Janssen TWJ, Rozendaal LA.. Biomechanics and physiology in active manual wheelchair propulsion. In adapted form, published as Woude et al. [1]. Med Eng Phys. 2001;23(10):713–33. [DOI] [PubMed]
- 16.Tsai CY, Boninger ML, Hastings J, Cooper RA, Rice L, Koontz AM.. Immediate biomechanical implications of transfer component skills training on independent wheelchair transfers. Arch Phys Med Rehabil 2016;97(10):1785–92. doi: 10.1016/j.apmr.2016.03.009 [DOI] [PubMed] [Google Scholar]
- 17.Slowik JS, Neptune RR.. A theoretical analysis of the influence of wheelchair seat position on upper extremity demand. Clin Biomech 2013;28(4):378–85. doi: 10.1016/j.clinbiomech.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 18.Sanders TL, Maradit Kremers H, Bryan AJ, Ransom JE, Morrey BF.. Health care utilization and direct medical costs of tennis elbow: a population-based study. Sports Health 2016;8(4):355–8. doi: 10.1177/1941738116650389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levin D, Nazarian LN, Miller TT, O'Kane PL, Feld RI, Parker L, McShane JM.. Lateral epicondylitis of the elbow: US findings. Radiology 2005;237(1):230–4. doi: 10.1148/radiol.2371040784 [DOI] [PubMed] [Google Scholar]
- 20.Latham SK, Smith TO.. The diagnostic test accuracy of ultrasound for the detection of lateral epicondylitis: a systematic review and meta-analysis. Orthop Traumatol Surg Res 2014;100(3):281–6. doi: 10.1016/j.otsr.2014.01.006 [DOI] [PubMed] [Google Scholar]
- 21.Martin Ginis KA, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord 2018;56(4):308–21. doi: 10.1038/s41393-017-0017-3 [DOI] [PubMed] [Google Scholar]
- 22.wRocchi M, Routhier F, Latimer-Cheung AE, Ginis KAM, Noreau L, Sweet SN.. Are adults with spinal cord injury meeting the spinal cord injury-specific physical activity guidelines? A look at a sample from a Canadian province. Spinal Cord 2017;55(5):454–9. doi: 10.1038/sc.2016.181 [DOI] [PubMed] [Google Scholar]
- 23.Martin Ginis KA, Jorgensen S, Stapleton J.. Exercise and sport for persons with spinal cord injury. Pm r 2012;4(11):894–900. doi: 10.1016/j.pmrj.2012.08.006 [DOI] [PubMed] [Google Scholar]
- 24.Anneken V, Hanssen-Doose A, Hirschfeld S, Scheuer T, Thietje R.. Influence of physical exercise on quality of life in individuals with spinal cord injury. Spinal Cord 2010;48(5):393–9. doi: 10.1038/sc.2009.137 [DOI] [PubMed] [Google Scholar]
- 25.Diaz R, Miller EK, Kraus E, Fredericson M.. Impact of adaptive sports participation on quality of life. Sports Med Arthrosc Rev 2019;27(2):73–82. doi: 10.1097/JSA.0000000000000242 [DOI] [PubMed] [Google Scholar]
- 26.Lape EC, Katz JN, Losina E, Kerman HM, Gedman MA, Blauwet CA.. Participant-reported benefits of Involvement in an adaptive sports program: a qualitative study. PM R 2018;10(5):507–15. doi: 10.1016/j.pmrj.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin Ginis KA, Ma JK, Latimer-Cheung AE, Rimmer JH.. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol Rev 2016;10(4):478–94. doi: 10.1080/17437199.2016.1198240 [DOI] [PubMed] [Google Scholar]