Abstract
Introduction:
Early decompression within the first 24 hours after spinal cord injury (SCI) is proposed in current guidelines. However, the possible benefits of earlier decompression are unclear. Thus, the present meta-analysis aims to investigate the existing evidence regarding the efficacy of ultra-early decompression surgery (within 12 hours after SCI) in improving patients’ neurological status.
Methods:
A search was performed in Medline, Embase, Scopus and Web of Science electronic databases, until the end of August 2021. Cohort studies and clinical trials were included in the present study. Exclusion criteria were absence of an early or late surgery group, failure to report neurological status based on the American spinal injury association impairment scale (AIS) grade, failure to perform the surgery within the first 12 hours after SCI, and duplicate reports and review articles. Two independent reviewers performed data collection, and risk of bias and certainty of evidence assessments. The outcome was reported as odds ratio (OR) and 95% confidence interval (CI).
Results:
Data from 16 articles, which studied 868 patients, were included. Compared to early or late decompression surgery, ultra-early decompression surgery significantly improves patients’ neurological status (OR = 2.25; 95% CI: 1.41 to 3.58). However, ultra-early surgery in thoracolumbar injuries is not significantly more effective than early to late surgery. Moreover, ultra-early surgery in patients with a baseline AIS A increases the chance of neurologic resolvent up to 3.86 folds (OR=3.86; 95% CI: 1.50 to 9.91). Contrastingly, ultra-early surgery does not result in significant improvement compared to early to late surgery in patients with AIS B (OR = 1.32; 95% CI: 0.51 to 3.45), AIS C (OR = 1.83; 95% CI: 0.72 to 4.64), and AIS D (OR = 0.99; 95% CI: 0.31 to 3.17).
Conclusion:
Current guidelines emphasize that spinal decompression should be performed within 24 hours after SCI, regardless of injury severity and location. However, results of the present study demonstrated that certain considerations may be taken into account when performing decompression surgery: 1) in patients with AIS A injury, decompression surgery should be performed as soon as possible, since its efficacy in neurological improvement is 3.86 folds higher in the first 12 hours after injury. 2) ultra-early decompression surgery in patients with cervical injury is more effective than in patients with thoracic or lumbar injuries. 3) postponing decompression surgery to 24 hours in SCI patients with AIS B to D does not significantly affect the neurological outcome.
Key Words: Decompression, Surgical, Spinal Cord injuries, Neurological Rehabilitation
1. Introduction:
Spinal cord injuries (SCIs) are one of the most debilitating traumas, for which there is no definitive cure. Furthermore, the risk of premature death in SCI patients is five times higher than that of healthy people. Statistics show that in 2016, about one million people suffered from SCI. as a result, SCI is responsible for a considerable proportion of the burden of trauma accidents (1).
Current therapies for SCI are surgical interventions and pharmacological treatments. Spinal decompression surgery is the most important surgical intervention within the first 24 hours after the injury (2).
Current guidelines demonstrate that surgical decompression within the first 24 hours improves six-month outcome in the patients, regardless of the level of SCI (2). Although these guidelines emphasize performing surgical decompression within the first 24 hours, the efficacy of ultra-early decompression surgery within the first 12 hours after SCI is yet to be determined. In this regard, in 2020, a meta-analysis showed that ultra-early decompression surgery can result in significant neurological improvement in SCI patients. However, the meta-analysis did not consider the severity and the location of the injury (3). Another meta-analysis depicted that ultra-early surgery within the first 8 hours, improves neurological status of the patients with complete SCI, but it is not significantly effective in patients with partial injury (4). Moreover, a meta-analysis performed in 2016 demonstrated that surgical decompression in the first 12 hours after injury may lead to a neurological improvement of up to 74%, while surgical decompression in the first 24 hours results in a neurological improvement of up to 25% (5).
Nevertheless, ultra-early decompression surgery following SCI encounters a number of challenges. As one of the most important limitations, performing the surgery within the first 8 to 12 hours is usually impossible, because of the delay in transporting the patients to medical facilities and preparing them for the surgery. However, if enough evidence supports the superiority of ultra-early decompression surgery to early decompression injury, in terms of efficacy in neurological improvement, current guidelines may be reconsidered. Yet, lack of consensus over the matter withholds a general conclusion regarding the efficacy of ultra-early decompression surgery in SCI patients. As a result, the present meta-analysis gathered existing evidence comparing the efficacy of ultra-early surgery (within 12 hours) with early (within 24 hours) and late (after 24 hours) decompression surgery. Moreover, the efficacy of ultra-early surgery in different severities of SCI was also assessed.
2. Method:
2.1 Study design
The present study is a systematic review and meta-analysis designed based on the PRISMA 2020 guidelines, performed to gather the existing evidence regarding the efficacy of ultra-early surgery (within the first 12 hours after SCI) in humans. The protocol of the present study has not been previously registered and published in its current form.
2.2 Eligibility criteria
PICO, in the current study, was defined as patients with traumatic SCI (P or patients) who underwent ultra-early decompression surgery (I or intervention). Comparison (C) was made with early (surgery within 24 hours) and late (surgery after 24 hours) decompression surgery performed on SCI patients. Finally, the evaluated outcome (O) was neurological improvement based on the American Spinal Injury Association (ASIA) impairment scale (AIS) grade. Therefore, cohort and clinical trials were selected to enter the present study. Furthermore, exclusion criteria were lack of an early or late surgery group, failure to define an exact cut-off time point as the definition of ultra-early, failure to report the neurological status of the patients based on the AIS grades, failure to perform the surgery within the first 12 hours after the injury, duplicate reports, and review articles.
2.3 Search strategy
The systematic search was performed in Medline, Embase, Scopus, and Web of Science electronic databases until the end of August 2021. Search strategy and the selected keywords for Medline database are depicted in Appendix 1. In addition to the systematic search, a manual search was conducted in google and google scholar search engines. Moreover, references of the related articles were screened to find additional articles.
2.4 Data collection
Two independent reviewers screened titles and abstracts of the articles and gathered full texts of the related ones. Then, the gathered full texts were thoroughly studied and completely related articles were selected. Afterwards, each of the reviewers extracted required data using a checklist on the Excel program. The data included name of the first author, date of publication, country, study type and design, definition of ultra-early group, definition of late surgery group, location of injury, severity of injury based on AIS grade, definition of neurological improvement, age and gender distribution of samples, number of neurological improvements in ultra-early and late surgery, number of not-improved patients, and follow-up duration. Any disagreements were resolved through discussion with a third reviewer.
2.5 Quality assessment of included papers
Since the included studies were either cohort or clinical trials, the quality assessment of the studies were performed based on the guidelines of the National Heart, Lung, and Blood institute (NHLBI) risk of bias assessment tool (6). Moreover, risk of bias of the clinical trials was assessed using Cochrane guidelines (7). Scoring and assessing the risk of bias based on the NHLBI guidelines have been previously discussed (8).
2.6 Evaluated outcomes
The evaluated outcome was improvement of the neurological status of the patients following surgical decompression based on the AIS grades. This scale is a five-point scoring scale, covering complete sensory-motor injury (AIS A) to normal status (AIS E). The reason for selecting AIS scoring system was that even one point improvement based on this scale is considered as a clinically significant improvement and a sign of decrease in inflammation (9).
2.7 Certainty of evidence
The level of evidence was scored based on the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) criteria (10). The level of evidence of each study was scored by two independent researchers based on the existence of risk of bias, imprecision, indirectness, inconsistency, and publication bias.
2.8 Data synthesis and statistical analysis
The cut-off point used to define the ultra-early surgery varied between four to 12 hours after the injury. Since most of the previous articles defined ultra-early as eight or 12 hours after the injury, the 12 hours cut-off point was adopted as the definition of ultra-early surgery in the present study. Data were recorded as number of improved and non-improved cases in ultra-early (surgery within 12 hours), early (surgery within 24 hours), and late (surgery after 24 hours) groups. Some studies reported the outcome of surgery after 12 hours as a whole and did not discriminate early and late surgeries. Therefore, the efficacy of ultra-early decompression surgery in promoting neurological recovery was compared with early to late surgery in a pooled analysis. Furthermore, data were recorded with respect to AIS grades.
Data were entered to STATA 17.0 statistical program, and the analyses were performed using Meta command. Since the study design and the evaluated SCI severity differed between the studies, researchers in the present study adopted the random effect model analysis. Heterogeneity and publication bias were assessed using I2 test and Egger’s test, respectively.
The efficacy of ultra-early decompression surgery in promoting neurological recovery was reported as a pooled odds ratio (OR) and 95% confidence interval (CI). In addition, subgroup analyses were performed based on the injury location, injury severity, and the cut-off time point for each (early surgery and late surgery). Since age and follow-up time variations were possible confounding factors, a meta-regression was performed to evaluate the possible effects of these confounding factors.
3. Results:
3.1 Study flow and characteristics of included studies
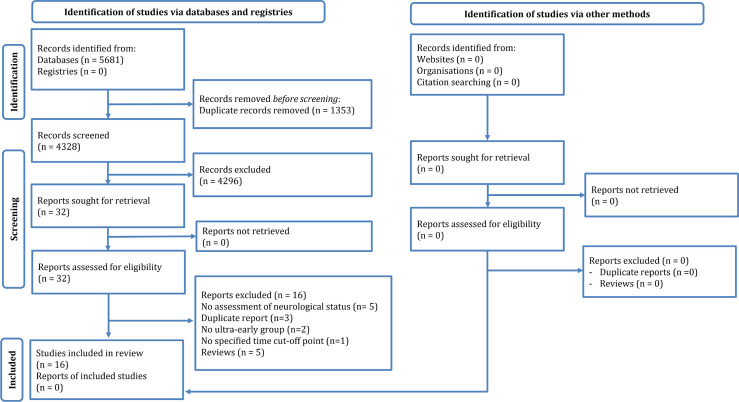
The systematic search yielded 4328 non-duplicate records. After reviewing the articles, 32 possibly related articles were selected, among which 16 studies were included in the present systematic review and meta-analysis (11-26). The reasons for exclusion were failure to evaluate neurological status based on the AIS/Frankel grade (n=5), duplicate reports (n=3), lack of an ultra-early surgery group, failure to define a distinct cut-off point for ultra-early surgery (n=1), and review articles (n=5) (Figure 1).
Figure 1.
PRISMA flow diagram of the current review
12 articles were retrospective cohorts, three studies were prospective cohort, and one study was clinical trial. The studies included data from 868 patients (429 patients in ultra-early surgery group and 439 patients in early to late surgery group). Injury location was cervical in 12 studies, thoracolumbar in two studies, and all areas of the spinal cord in two other studies. Injury severity based on the AIS grades were between A to D. Ultra-early was defined as within eight hours after SCI in eight studies and within 12 hours after SCI in five other studies. A cut-off point of four, five, and six hours after the SCI was defined as the definition of ultra-early in one study each. Early surgery (within 24 hours) was reported in five studies, and the other studies combined the data from early and late surgery and the comparison was made between the numbers from ultra-early surgery and that of the early and late surgeries, combined. Follow-up period varied between six (in nine studies) to 68 months. Recovery was defined as at least one grade improvement based on the AIS score. Table 1 shows the included data in the present study.
Table 1.
Summary of included papers
| Study | Design | Ultra-early definition* | Late definition* | Injury location | Follow-up (months) | Severity | Score | Improvement definition | Mean age (years) | No. of males | No. of ultra-early | No. of late |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aarabi, 2017; USA | R-C | 12 | >12 | Cervical | 6 | A-C | AIS | at least 1 grade | 39.5 | 89 | 51 | 49 |
| Aarabi, 2020; USA | R-C | 12 | 12-24; >24 | Cervical | 6 | A-C | AIS | at least 1 grade | 46 | 60 | 32 | 40 |
| Biglari, 2016; Germany | P-C | 4 | 4 to 24 | All levels | 6 | A-C | AIS | at least 1 grade | 43.37 | 40 | 29 | 22 |
| Burke, 2019; USA | R-C | 12 | 12-24; >24 | Cervical | NR | A-C | AIS | at least 1 grade | 56.5 | 38 | 18 | 30 |
| Cengiz, 2008; Turkey | RCT | 8 | >72 | Th2-L2 | 14.5 | A-C | AIS | at least 1 grade | 41.4 | 18 | 12 | 15 |
| Dobran, 2015; Italy | P-C | 12 | 12 to 72 | Cervical | 24 | A-D | AIS | at least 1 grade | 50.2 | 44 | 27 | 30 |
| Gaebler., 1999; Austria | R-C | 8 | >8 | Thoracic-lumbar | 68 | A-D | Frankel | at least 1 grade | 32.6 | 56 | 24 | 43 |
| Grassner, 2016; Germany | R-C | 8 | >8 | Cervical | 12 | A-D | AIS | at least 1 grade | 51 | 59 | 35 | 35 |
| Jug, 2015; Slovenia | P-C | 8 | 8 to 24 | Cervical | 6 | A-C | AIS | at least 1 grade | 47.3 | 34 | 22 | 20 |
| Lee, 2018; Korea | R-C | 8 | 8 to 24 | All levels | 6 | A-C | AIS | at least 1 grade | 48 | 35 | 26 | 30 |
| Mattiassich, 2017; Austria | R-C | 5 | 5 to 24 | Cervical | 6 | A-D | AIS | at least 1 grade | 50 | 38 | 33 | 16 |
| McCarthy, 2011; Australia | R-C | 8 | >8 | Cervical | 6 | A-D | AIS | at least 1 grade | NR | 31 | 17 | 25 |
| Nagata, 2016; Japan | R-C | 6 | 6 to 11 | Cervical | 13.8 | A-B | AIS | at least 1 grade | 54 | 28 | 21 | 9 |
| Nasi, 2019; Italy | R-C | 12 | 12 to 48 | Cervical | 12 | A-D | AIS | at least 1 grade | 57.8 | 58 | 40 | 41 |
| Tsuji, 2019; Japan | R-C | 8 | >8 | Cervical | 6 | A-D | AIS | at least 1 grade | 71.8 | 35 | 10 | 23 |
| Wutte, 2020; Germany | R-C | 8 | >8 | Cervical | 12 | A-D | AIS | at least 1 grade | 48.7 | 34 | 32 | 11 |
NR: Not reported; P-C: Prospective cohort; RCT: Randomized clinical trial; R-C: Retrospective cohort; AIS: American Spinal Injury Association impairment scale.
*, hours after spinal cord injury.
3.2 Effect of ultra-early decompression injury on neurological status of SCI patients
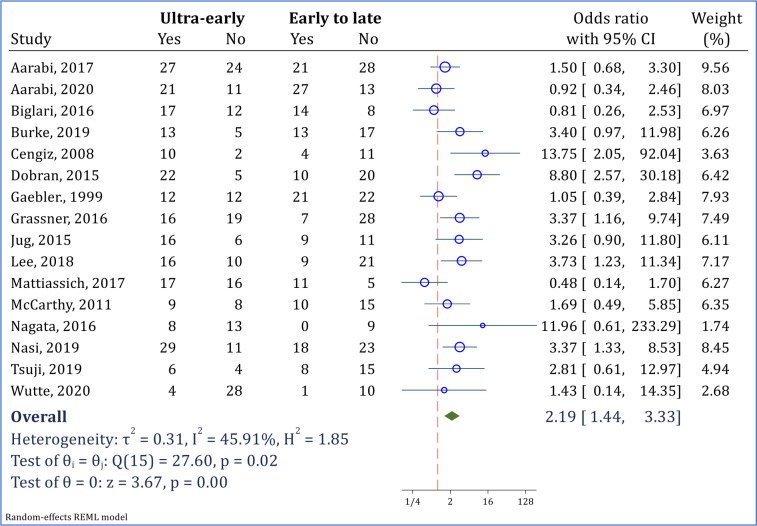
Overall pooled analysis, regardless of the injury severity, injury location, and the group selected for comparison (early or late surgery) demonstrated that the chances of recovery in patients undergoing ultra-early surgery was 2.19 times higher than that of patients undergoing decompression surgery after 12 hours after injury (OR = 2.19; 95% CI: 1.44, 3.33; I2 = 49.51%) (Figure 2).
Figure 2.
Overall pooled analysis for assessment of ultra-early surgery (< 12 hours) versus early to late surgery (>12 hours) in improvement of neurological status. Neurological improvement was defined as at least 1 grade improvement in American Spinal Injury Association impairment scale (AIS) grade
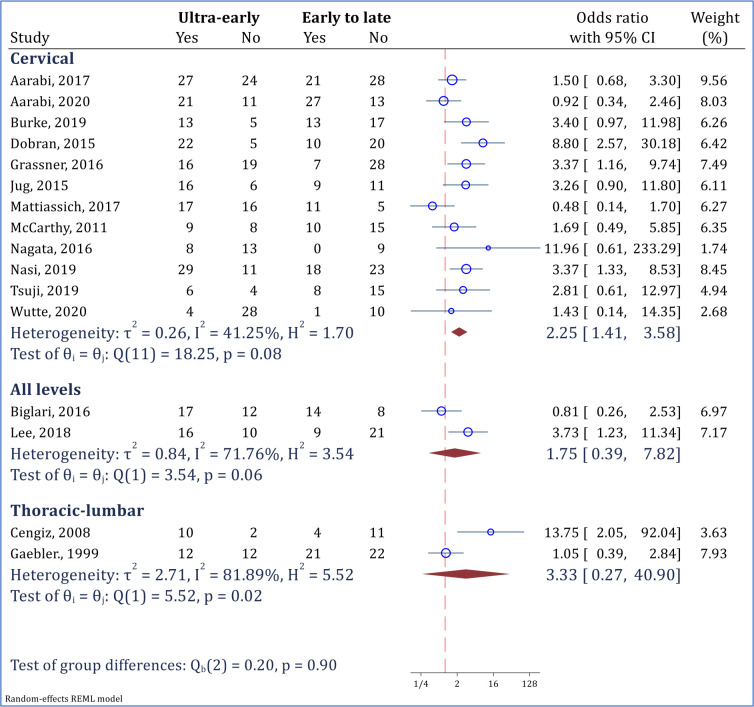
Subgroup analysis demonstrated that ultra-early surgery was significantly more effective than early to late surgery in improving neurological status of the patients experiencing a cervical injury (OR = 2.25; 95% CI: 1.41 to 3.58; I2 = 41.25%). However, ultra-early surgery did not show a significantly superior efficacy in thoracolumbar injuries, in comparison with early to late surgeries (Figure 3).
Figure 3.
Subgroup analysis for assessment of ultra-early surgery (< 12 hours) versus early to late surgery (>12 hours) in improvement of neurological status based on the level of injury. Neurological improvement was defined as at least 1 grade improvement in American Spinal Injury Association impairment scale (AIS) grade
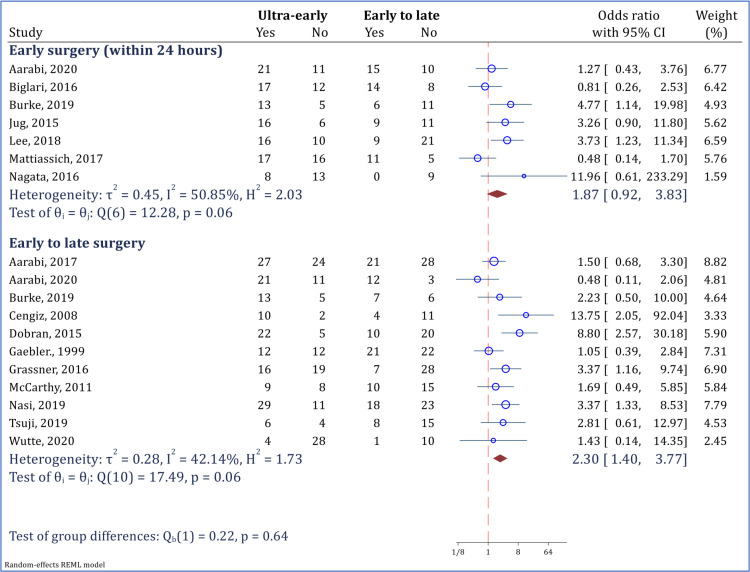
It is noteworthy that ultra-early surgery is not more effective than early surgery (within 24 hours after SCI), and the observed neurological status recovery was similar in both surgeries. (OR = 1.87; 95% CI: 0.92 to 3.83; I2 = 50.85%). However, the observed efficacy of ultra-early surgery in neurological recovery was significantly higher than that of early to late surgery (OR = 2.30; 95% CI: 1.40 to 3.77; I2 = 42.14%) (Figure 4).
Figure 4.
comparison of ultra-early surgery (< 12 hours) and early to late surgery (including surgery within 24 hours and afterwards) in improvement of neurological status. Neurological improvement was defined as at least 1 grade improvement in American Spinal Injury Association impairment scale (AIS) grade
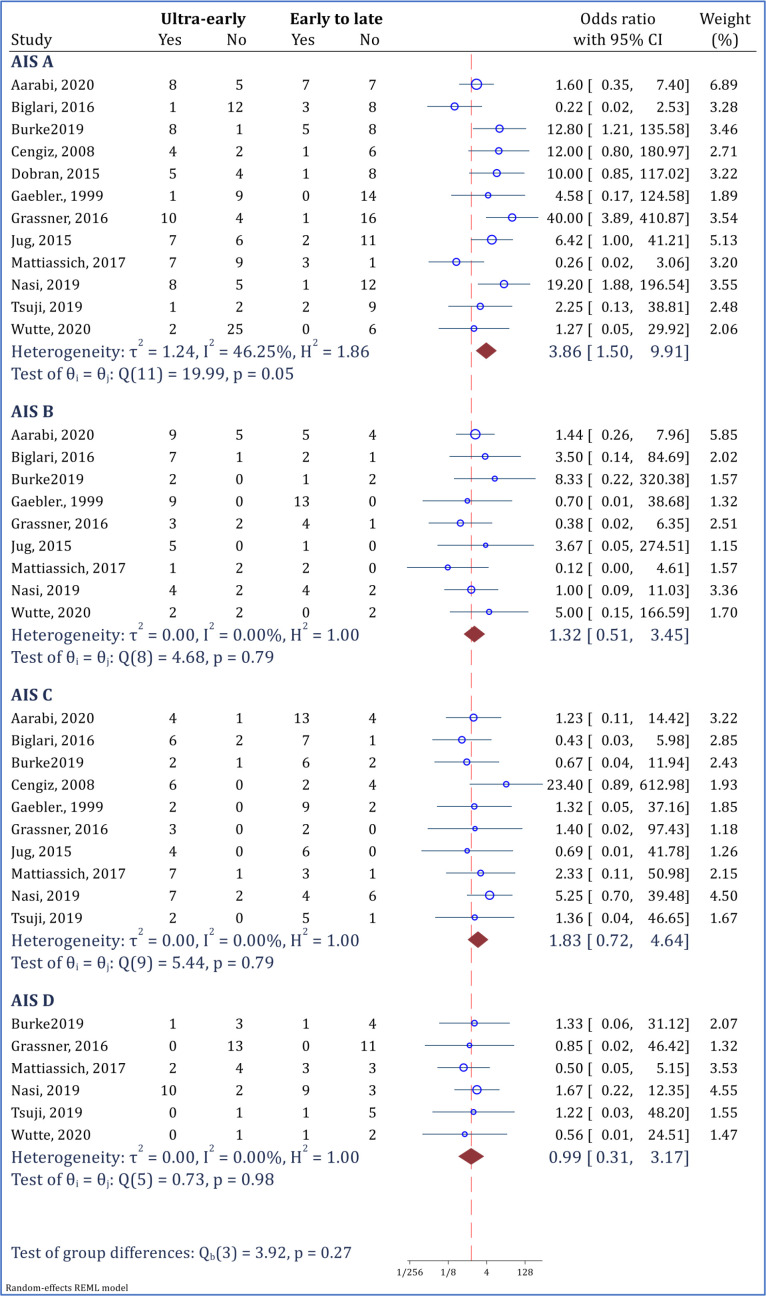
3.3 Effect of ultra-early decompression surgery on neurological status based on baseline AIS score
As a sensitivity analysis, the efficacy of ultra-early decompression surgery based on the baseline AIS score was evaluated. The results demonstrated that ultra-early surgery in patients with a baseline AIS of A can increase the chances of neurological recovery up to 3.86 times (OR = 3.86; 95% CI: 1.50 to 9.91; I2 = 46.25%). Nevertheless, ultra-early surgery was not significantly more effective than early to late surgery in patients with AIS B (OR = 1.32; 95% CI: 0.51 to 3.45; I2 = 0.00%), AIS C (OR = 1.83; 95% CI: 0.72 to 4.64; I2 = 0.00%), and AIS D (OR = 0.99; 95% CI: 0.31 to 3.17; I2 = 0.00%) (Figure 5).
Figure 5.
Effectiveness of ultra-early surgery (< 12 hours) in improvement of neurological status based on baseline American Spinal Injury Association impairment scale (AIS) grade. Neurological improvement was defined as at least 1 grade improvement in AIS grade
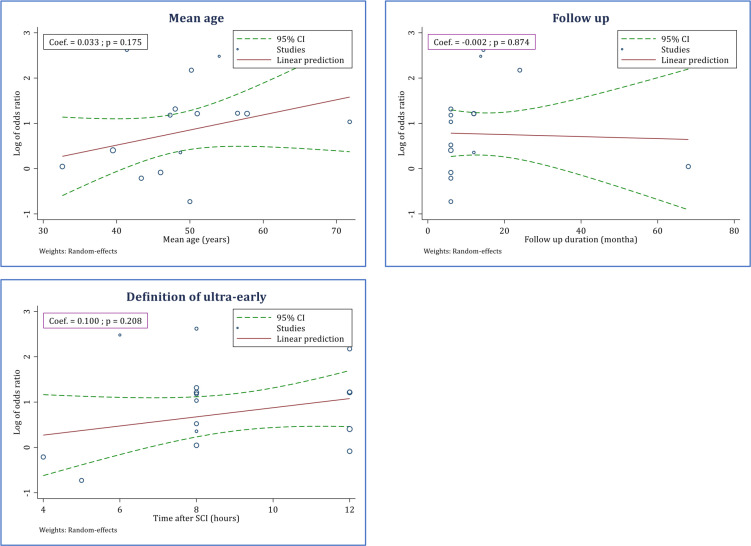
3.4 Meta-regression
Since the mean age and follow-up period were diverse among the studies, a meta-regression was performed with respect to the two variables. The meta-regression demonstrated that the mean age of patients at the time of SCI (meta-regression coefficient = 0.033; p = 0.175) and follow-up time (meta-regression coefficient = -0.002; p = 0.874) were not associated with the efficacy of ultra-early decompression surgery in promoting neurological recovery. Moreover, the meta-regression depicted that ultra-early decompression surgery within the first 12 hours is as effective as when it is performed earlier (meta-regression coefficient = 0.100; p = 0.208) (Figure 6).
Figure 6.
Effectiveness of ultra-early surgery (< 12 hours) in improvement of neurological status based on mean age of patients, follow-up duration, and timing of surgery
3.5 Risk of bias assessment
15 cohorts and one clinical trial were included in the present study. Risk of bias of the one clinical trial was low. Moreover, risk of bias assessment of the cohort studies based on NHLBI tool showed that in terms of sufficiency of time frame, the status could not be determined in two studies (signaling question 7). Furthermore, judgment regarding rate of loss to follow-up was not possible in five studies (signaling question 13). Based on the presence of these two fatal errors among the studies, the overall risk of bias in the five studies was scored as high. Also, some risk of bias was found in eight studies, since blinding status and sample size justification were not provided. Risk of bias was considered low in two studies (Table 2).
Table 2.
Risk of bias assessment of included studies
| Study | Q1 | Q2 | Q3* | Q4 | Q5 | Q6* | Q7* | Q8 | Q9 | Q10 | Q11* | Q12 | Q13* | Q14 | Overall |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort studies according to NHLBI tool | |||||||||||||||
| Arabi, 2017 | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | Yes | NA | Yes | NR | CD | NA | High risk |
| Arabi, 2020 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | NR | CD | NA | High risk |
| Biglari, 2016 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | NR | CD | NA | High risk |
| Burke, 2019 | Yes | Yes | Yes | Yes | NR | Yes | CD | Yes | Yes | NA | Yes | NR | CD | NA | High risk |
| Dobran, 2015 | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | Yes | NA | Yes | NR | Yes | NA | Some concern |
| Gaebler., 1999 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | NR | Yes | NA | Some concern |
| Grassner, 2016 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | NR | Yes | NA | Some concern |
| Jug, 2015 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | NA | Low risk |
| Lee, 2018 | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | Yes | NA | Yes | NR | Yes | NA | Some concern |
| Mattiassich, 2017 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | NR | Yes | NA | Some concern |
| McCarthy, 2011 | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | Yes | NA | Yes | NR | Yes | NA | Some concern |
| Nagata, 2016 | Yes | Yes | Yes | Yes | NR | Yes | Yes | No | Yes | NA | Yes | NR | CD | NA | High risk |
| Nasi, 2019 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | NR | Yes | NA | Some concern |
| Tsuji, 2019 | Yes | Yes | Yes | Yes | NR | Yes | CD | Yes | Yes | NA | Yes | NR | Yes | NA | High risk |
| Wutte, 2020 | Yes | Yes | Yes | Yes | NR | Yes | Yes | Yes | Yes | NA | Yes | Yes | Yes | NA | Low risk |
| D1 | D2 | D3 | D4 | D5 | |||||||||||
| Clinical trial according Cochrane risk of bias assessment tool | |||||||||||||||
| Cengiz, 2008 | Low | Low | Low | Low | Low | -- | -- | -- | -- | -- | -- | -- | -- | -- | Low risk |
Q: Signaling question; D: Domain; NR: Not reported; NA: Not applicable; CD: Cannot determine.
*, Any concern in these questions were considered as fetal error.
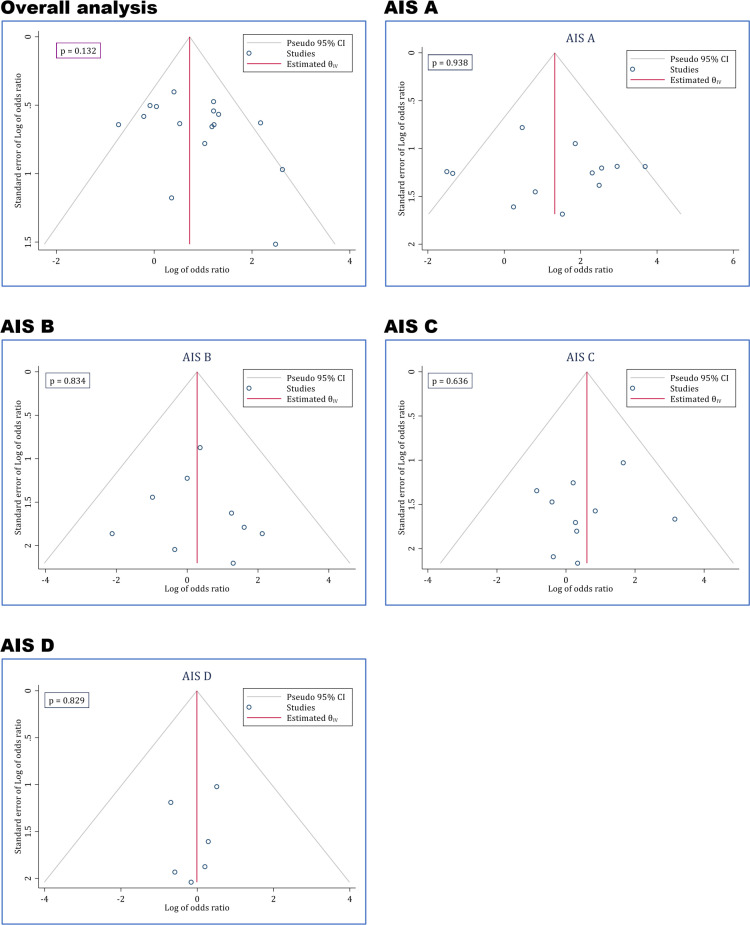
3.6 Publication bias
Egger’s test showed no evidence of publication bias among the studies. As depicted in Figure 7, no publication bias existed in the evaluation of the efficacy of ultra-early decompression in improvement of neurological status overall and in various AIS grades.
Figure 7.
Publication bias assessment of included studies based on AIS grade. AIS: American Spinal Injury Association (ASIA) impairment scale grade
3.7 Certainty of evidence
According to the GRADE’s protocol, the overall level of evidence is low in observational studies. Since there is a possible risk of bias in the present study, one point was deducted from the GRADE score in all outcomes. However, due to the existence of a large magnitude of effect and possible plausible confounders, which increase the confidence of findings, the overall level of evidence was increased and became moderate. Table 3 provides details of our judgments regarding the certainty of evidence.
Table 3.
Level of evidence by outcome
| Outcome | Sample size | Risk of bias | Imprecision |
Inconsistency
(I 2 range) |
Indirectness | Publication bias | Judgment and level of evidence | Level of evidence |
|---|---|---|---|---|---|---|---|---|
| Overall neurological status | 868 | Serious | Not serious | Not serious | Not serious | Not serious | Rated down 1 point:
|
Moderate . ⊖⊕⊕ |
| Neurological status based on location of injury | 868 | Serious | Not serious | Not serious | Not serious | Not serious | Rated down 1 point:
|
Moderate . ⊖⊕⊕ |
| Neurological status based on definition of late surgery | 868 | Serious | Not serious | Not serious | Not serious | Not serious | Rated down 1 point:
|
Moderate . ⊖⊕⊕ |
| Neurological status based on severity of injury | 640 | Serious | Not serious | Not serious | Not serious | Not serious | Rated down 1 point:
|
Moderate . ⊖⊕⊕ |
*, Since most of the studies had assessed cervical spinal cord patients, the authors decided that there are possible plausible confounders, which increase the confidence of findings.
**, Since late group compromise surgery after 12 hours (rather than 24 hours) in the most included studies, the authors decided that there are possible plausible confounders, which increase the confidence of findings.
4. Discussion:
Moderate level of evidence demonstrated that ultra-early decompression surgery within the first 12 hours after SCI may improve neurological recovery in patients with cervical SCI with an AIS grade of A. The analyses showed that in comparison with early to late surgery, the ultra-early surgery does not result in a significantly higher efficacy in other severities of SCI (AIS B to D).
Although conflicting results were reported in different studies regarding the prognostic effects of baseline AIS score on the treatment success of spinal decompression surgery (27-30), results of the present study showed that in comparison with early and late surgery, ultra-early surgical decompression can promote neurological recovery in AIS A patients. In these patients, whom are encountered with complete sensory-motor injury, the spinal cord is experiencing devastating pressure. As result, promptly eliminating this pressure may prevent further secondary injuries responsible for a considerable amount of damage following SCI. Hence, this may be the reason behind the observed efficacy of ultra-early early surgery only in AIS A patients. Accordingly, researchers of the present study recommend that ultra-early decompression surgery be performed as soon as possible in patients with complete sensory-motor injury.
Current treatment guidelines emphasize that decompression injury be performed within the first 24 hours, regardless of the injury severity and location. However, current evidences suggest that when performing decompression surgery, certain consideration may be taken into account. These considerations include: 1) in patients with AIS A injury, decompression injury may/should be performed as soon as possible, as it can enhance the chance of neurological recovery to up to 3.86 times. 2) ultra-early decompression surgery is more effective in cervical SCI patients compared to thoracic and lumbar SCI patients. 3) delaying decompression surgery until 24 hours in patients with AIS B to D SCI does not significantly affect the final neurological outcome. 4) different cut-off points were defined for ultra-early decompression injury among the studies, ranging from four to 12 hours. Meta-regression demonstrated that performing ultra-early decompression surgery within a time frame of 12 hours after the injury is as effective as when performed within sooner time points. Therefore, a 12-hour time window after SCI maybe considered as an appropriate definition of performing ultra-early surgery. This definition can promote the possibility of performing ultra-early surgery.
One of the limitations of the present study was the small number of the articles evaluating the results of decompression surgery in thoracic and lumbar spine injuries. Only two studies researched the effects of ultra-early decompression surgery in these patients, which may deduct the power of the performed analyses. As a result, it is recommended that future studies be performed evaluating the effects of ultra-early decompression surgery in patients with lumbar and thoracic SCIs. another limitation of the current study was that only one clinical trial was included. In addition, due to the observational nature of the included studies and the analyses being uncontrolled for possible confounding factors, further clinical trials are encouraged to be performed to overcome the existing limitations.
5. Conclusion:
The present meta-analysis, performed on 15 cohorts and one clinical trial, demonstrated that ultra-early decompression surgery within the first 12 hours following SCI in patients with an AIS A injury and/or a cervical SCI may be more effective than surgeries performed after the first 12 hours following SCI in promoting neurological recovery. The efficacy of the ultra-early intervention in lumbar and thoracic injuries or less severe injuries (AIS B to D) was not proven in the present study; therefore, further clinical trials are needed in this regard.
6. Declarations:
6.1 Acknowledgments
None.
6.2 Authors’ contributions
Study Design: MY, RJK
Data gathering: MY, BH, RKO, AMN
Analysis: MY
Interpretation of results: RJL, RK, RKO
Drafting: MY, AMN
Critically revised: All authors
6.3 Funding and supports
None
6.4 Conflict of Interest
There are no conflicts of interest
References
- 1.James SL, Theadom A, Ellenbogen RG, Bannick MS, Montjoy-Venning W, Lucchesi LR, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Neurology. 2019;18(1):56–87. doi: 10.1016/S1474-4422(18)30415-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fehlings MG, Tetreault LA, Wilson JR, Aarabi B, Anderson P, Arnold PM, et al. A Clinical Practice Guideline for the Management of Patients With Acute Spinal Cord Injury and Central Cord Syndrome: Recommendations on the Timing (≤24 Hours Versus >24 Hours) of Decompressive Surgery. Global Spine Journal. 2017;7(3):195s–202s. doi: 10.1177/2192568217706367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hsieh YL, Tay J, Hsu SH, Chen WT, Fang YD, Liew CQ, et al. Early versus Late Surgical Decompression for Traumatic Spinal Cord Injury on Neurological Recovery: A Systematic Review and Meta-Analysis. Journal of Neurotrauma.38(21):2927–36. doi: 10.1089/neu.2021.0102. [DOI] [PubMed] [Google Scholar]
- 4.Ma Y, Zhu Y, Zhang B, Wu Y, Liu X, Zhu Q. The Impact of Urgent (<8 Hours) Decompression on Neurologic Recovery in Traumatic Spinal Cord Injury: A Meta-Analysis. World Neurosurgery. 2020;140:e185–e94. doi: 10.1016/j.wneu.2020.04.230. [DOI] [PubMed] [Google Scholar]
- 5.Yousefifard M, Rahimi-Movaghar V, Baikpour M, Ghelichkhani P, Hosseini M, Jafari A, et al. Early versus late spinal decompression surgery in treatment of traumatic spinal cord injuries; a systematic review and meta-analysis. Emergency. 2017;5(1) [PMC free article] [PubMed] [Google Scholar]
- 6.National Heart L, and Blood Institute (NHLBI) Quality Assessment Tool for Observational Case-Control Studies USA: National Library of Medicine. 2014. [Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 7.Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. Cochrane handbook for systematic reviews of interventions. . 2019:205–28. [Google Scholar]
- 8.Yousefifard M, Toloui A, Ahmadzadeh K, Gubari MIM, Neishaboori AM, Amraei F, et al. Risk Factors for Road Traffic Injury-Related Mortality in Iran; a Systematic Review and Meta-Analysis. Archives of Acadic Emergency Medicine. 2021;9(1):e61. doi: 10.22037/aaem.v9i1.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pneumaticos SG, Triantafyllopoulos GK, Lasanianos NG. American spinal injury association-ASIA-impairment scale for neurological deficit. Trauma and Orthopaedic Classifications. Springer; 2015. pp. 227–8. [Google Scholar]
- 10.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1 Introduction—GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology. 2011;64(4):383–94. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 11.Aarabi B, Sansur CA, Ibrahimi DM, Simard JM, Hersh DS, Le E, et al. Intramedullary Lesion Length on Postoperative Magnetic Resonance Imaging is a Strong Predictor of ASIA Impairment Scale Grade Conversion Following Decompressive Surgery in Cervical Spinal Cord Injury. Neurosurgery. 2017;80(4):610–20. doi: 10.1093/neuros/nyw053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aarabi B, Akhtar-Danesh N, Chryssikos T, Shanmuganathan K, Schwartzbauer GT, Simard JM, et al. Efficacy of Ultra-Early (< 12 h), Early (12-24 h), and Late (>24-138 h) Surgery with Magnetic Resonance Imaging-Confirmed Decompression in American Spinal Injury Association Impairment Scale Grades A, B, and C Cervical Spinal Cord Injury. Journal of Neurotrauma. 2020;37(3):448–57. doi: 10.1089/neu.2019.6606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Biglari B, Child C, Yildirim TM, Swing T, Reitzel T, Moghaddam A. Does surgical treatment within 4 hours after trauma have an influence on neurological remission in patients with acute spinal cord injury? Therapeutics and Clinical Risk Management. 2016;12:1339–46. doi: 10.2147/TCRM.S108856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burke JF, Yue JK, Ngwenya LB, Winkler EA, Talbott JF, Pan JZ, et al. Ultra-Early (<12 Hours) Surgery Correlates With Higher Rate of American Spinal Injury Association Impairment Scale Conversion After Cervical Spinal Cord Injury. Neurosurgery. 2019;85(2):199–203. doi: 10.1093/neuros/nyy537. [DOI] [PubMed] [Google Scholar]
- 15.Cengiz SL, Kalkan E, Bayir A, Ilik K, Basefer A. Timing of thoracolomber spine stabilization in trauma patients; impact on neurological outcome and clinical course A real prospective (rct) randomized controlled study. Archives of Orthopaedic and Trauma Surgery. 2008;128(9):959–66. doi: 10.1007/s00402-007-0518-1. [DOI] [PubMed] [Google Scholar]
- 16.Dobran M, Iacoangeli M, Nocchi N, Di Rienzo A, di Somma LG, Nasi D, et al. Surgical treatment of cervical spine trauma: Our experience and results. Asian Journal of Neurosurgery. 2015;10(3):207–11. doi: 10.4103/1793-5482.161192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gaebler C, Maier R, Kutscha-Lissberg F, Mrkonjic L, Vècsei V. Results of spinal cord decompression and thoracolumbar pedicle stabilisation in relation to the time of operation. Spinal Cord. 1999;37(1):33–9. doi: 10.1038/sj.sc.3100765. [DOI] [PubMed] [Google Scholar]
- 18.Grassner L, Wutte C, Klein B, Mach O, Riesner S, Panzer S, et al. Early decompression (< 8 h) after traumatic cervical spinal cord injury improves functional outcome as assessed by spinal cord independence measure after one year. Journal of Neurotrauma. 2016;33(18):1658–66. doi: 10.1089/neu.2015.4325. [DOI] [PubMed] [Google Scholar]
- 19.Jug M, Kejžar N, Vesel M, Al Mawed S, Dobravec M, Herman S, et al. Neurological Recovery after Traumatic Cervical Spinal Cord Injury Is Superior if Surgical Decompression and Instrumented Fusion Are Performed within 8 Hours versus 8 to 24 Hours after Injury: A Single Center Experience. Journal of Neurotrauma. 2015;32(18):1385–92. doi: 10.1089/neu.2014.3767. [DOI] [PubMed] [Google Scholar]
- 20.Lee DY, Park YJ, Song SY, Hwang SC, Kim KT, Kim DH. The Importance of Early Surgical Decompression for Acute Traumatic Spinal Cord Injury. Clinics in Orthopedic Surgery. 2018;10(4):448–54. doi: 10.4055/cios.2018.10.4.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mattiassich G, Gollwitzer M, Gaderer F, Blocher M, Osti M, Lill M, et al. Functional Outcomes in Individuals Undergoing Very Early (< 5 h) and Early (5-24 h) Surgical Decompression in Traumatic Cervical Spinal Cord Injury: Analysis of Neurological Improvement from the Austrian Spinal Cord Injury Study. Journal of Neurotrauma. 2017;34(24):3362–71. doi: 10.1089/neu.2017.5132. [DOI] [PubMed] [Google Scholar]
- 22.McCarthy MJ, Gatehouse S, Steel M, Goss B, Williams R. The influence of the energy of trauma, the timing of decompression, and the impact of grade of SCI on outcome. Evidence-Based Spine-Care Journal. 2011;2(2):11–7. doi: 10.1055/s-0030-1267100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nagata K, Inokuchi K, Chikuda H, Ishii K, Kobayashi A, Kanai H, et al. Early versus delayed reduction of cervical spine dislocation with complete motor paralysis: a multicenter study. European Spine Journal. 2017;26(4):1272–6. doi: 10.1007/s00586-017-5004-z. [DOI] [PubMed] [Google Scholar]
- 24.Nasi D, Ruscelli P, Gladi M, Mancini F, Iacoangeli M, Dobran M. Ultra-early surgery in complete cervical spinal cord injury improves neurological recovery: A single-center retrospective study. Surgical Neurology International. 2019;10:207. doi: 10.25259/SNI_485_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tsuji O, Suda K, Takahata M, Matsumoto-Harmon S, Komatsu M, Menjo Y, et al. Early surgical intervention may facilitate recovery of cervical spinal cord injury in DISH. Journal of Orthopaedic Surgery (Hong Kong). 2019;27(1):2309499019834783. doi: 10.1177/2309499019834783. [DOI] [PubMed] [Google Scholar]
- 26.Wutte C, Becker J, Klein B, Mach O, Panzer S, Stuby FM, et al. Early Decompression (<8 Hours) Improves Functional Bladder Outcome and Mobility After Traumatic Thoracic Spinal Cord Injury. World Neurosurgery. 2020;134:e847–e54. doi: 10.1016/j.wneu.2019.11.015. [DOI] [PubMed] [Google Scholar]
- 27.Park JH, Kim JH, Roh SW, Rhim SC, Jeon SR. Prognostic factor analysis after surgical decompression and stabilization for cervical spinal-cord injury. British Journal of Neurosurgery. 2017;31(2):194–8. doi: 10.1080/02688697.2016.1247781. [DOI] [PubMed] [Google Scholar]
- 28.Kawano O, Maeda T, Sakai H, Masuda M, Morishita Y, Hayashi T, et al. Significance of the neurological level of injury as a prognostic predictor for motor complete cervical spinal cord injury patients. The Journal of Spinal Cord Medicine. 2021:1–7. doi: 10.1080/10790268.2021.1903139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khorasanizadeh M, Yousefifard M, Eskian M, Lu Y, Chalangari M, Harrop JS, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. Journal of Neurosurgery: Spine. 2019;30(5):683–99. doi: 10.3171/2018.10.SPINE18802. [DOI] [PubMed] [Google Scholar]
- 30.Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M. Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Frontiers in Human Neuroscience. 2014;8:141. doi: 10.3389/fnhum.2014.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]