Abstract
Background:
Over the past decade, medical care has shifted from institutions into home settings—particularly among persons with dementia. Yet it is unknown how home-based clinical services currently support persons with dementia, and what factors shape access.
Methods:
Using the National Health and Aging Trends Study linked to Medicare claims 2012–2017 we identified 6664 community-dwelling adults age ≥70 years enrolled in fee-for-service Medicare. Annual assessment of dementia status was determined via self-report, cognitive interview, and/or proxy assessment. Receipt of four types of home-based clinical care (home-based medical care (HBMC) (i.e., nurse practitioner, physician, or physician assistant visits), skilled home health care, podiatry visits, and other types of home-based clinical services (e.g., behavioral health)) was assessed annually. We compared age-adjusted rates of home-based clinical care by dementia status and determined sociodemographic, health, and environmental characteristics associated with utilization of home-based clinical care among persons with dementia.
Results:
Nearly half (44.4%) of persons with dementia received any home-based clinical care annually compared to only 14.4% of those without dementia. Persons with dementia received substantially more of each type of home-based clinical care than those without dementia including a 5-fold increased use of HBMC (95% CI=3.8–6.2) and double the use of skilled home health care (95% CI=2.0–2.5). In adjusted models, Hispanic/Latino persons with dementia were less likely to receive HBMC (OR= 0.32;95% CI=0.11 – 0.93). Use of HBMC, podiatry, and other home-based clinical care was significantly more likely among those living in residential care facilities, in the Northeast and in metropolitan areas.
Conclusion:
While almost half of community-dwelling persons with dementia receive home-based clinical care, there is significant variation in utilization based on race/ethnicity and environmental context. Increased understanding as to how these factors impact utilization is necessary to reduce potential inequities in healthcare delivery among the dementia population.
Keywords: Dementia, home-based medical care, home health, podiatry
Background
Growth in the prevalence of dementia1, 2 will intensify the challenges of delivering person-centered care to older adults. Persons with dementia (PWD) often have coexisting medical conditions and behavioral needs impacting quality of life and caregiver stress.3, 4 As their function declines, PWD require extensive logistical support and care coordination beyond simple assistance with daily activities.5–8 Consistent with individuals’ preference to live at home,9, 10 the locus of long-term care has shifted to the community.11 Dementia care is increasingly provided in the home setting, even at the end of life.12 More PWD with significant functional impairment and mobility issues live at home.13, 14 These numbers will likely increase given recent care challenges within nursing facilities during COVID-19.15
Leaving the home to access medical care may result in undue burden for PWD and caregivers due to challenges navigating clinical environments and accessing transportation, especially as the functional status of the PWD declines.16 Such difficulty may result in PWD foregoing routine care and instead experiencing costly and potentially unnecessary ED visits or hospitalizations after becoming acutely ill.17–19 Hospitalization may be particularly risky for PWD due to increased risk for delirium and iatrogenesis.
A range of home-based clinical services exist within the traditional fee-for-service (FFS) Medicare system that have been identified by our group.20 Most recognized and pervasive among home-based clinical services, skilled home health care (SHHC) is provided on an episodic basis by home health agencies to homebound beneficiaries who have a need for skilled services in the home (e.g., nursing, physical therapy).21 22 SHHC requires a physician referral and can be initiated in the post-acute or community setting. Other types of care include: home-based medical care (HBMC) or clinical practices that provide nurse practitioner, physician, physician assistant-led care (primary or specialist) to homebound adults;23 podiatry services; and a variety of other clinical services billed under Medicare part B including behavioral health, imaging, and lab work.
In light of the long and unpredictable course of dementia and as care preferences and policy initiatives propel the setting of dementia care from institutions to the community,24 it is imperative that we understand how dementia care is delivered at home. Such knowledge will help to expand service delivery and ensure individuals receive high quality care at the optimal time in a coordinated fashion. Existing research suggests PWD make up a significant portion of HBMC users.23 They are also more likely to utilize SHHC via community referral than patients without dementia and to utilize home health for longer periods of time.25 Yet it is unknown how much home-based clinical care in its totality is being used in dementia care, the patterns of care, or what factors are associated with the provision of home-based clinical care among PWD. Therefore, this paper aims to determine the utilization patterns of home-based clinical care received by PWD living in the community and identify factors associated with receipt of home-based clinical care among this population.
Methods
Sample
We used 2011–2016 data from the National Health and Aging Trends Study (NHATS), a nationally-representative annual longitudinal study of Medicare beneficiaries26 linked to Medicare claims 2012–2017. Inclusion criteria included age >=70 (as per NHATS weighting guidelines), known dementia status, community–dwelling status, and linkage to at least one month of fee-for-service (FFS) Medicare claims data post NHATS survey assessment for identification of home-based clinical care. Our final sample included 6664 respondents >=70 who were followed for up to 6 waves resulting in 19,396 person years of observation. Our main unit of analysis was person years (mean = 2.9 observations per individual). As a sensitivity analysis, we limited analyses to unique individuals in the 2015 NHATS cohort (n=3,801).
Measures:
Our primary measure of interest was receipt of home-based clinical care. Based on previous analysis of home-based clinical care, we used Medicare claims data to identify 4 unique categories of services: (1) HBMC (i.e. physician, physician assistant, or nurse practitioner visits), (2) podiatry visits (e.g., diabetic foot care, toenail trimming), (3) other FFS home-based clinical services (e.g., behavioral health, imaging/diagnostics), and (4) SHHC delivered in the home. We considered home to be either a private residential home or a non-nursing facility residential setting, such as an assisted living facility or group home. Based on previous work,27 we used Healthcare Common Procedure Coding System (HCPCS) codes to identify the provision of HBMC, excluding visits made by podiatrists. Podiatry services, with or without HBMC HCPCS, were determined based on a provider type code (48). All other carrier file claims that occurred in the home (place of service = home, assisted living facility, group home, custodial care facility, or residential substance abuse treatment facility) but did not meet criteria for HBMC or podiatry visits were grouped together as other FFS home based clinical care. Use of SHHC was based on any visit identified via the Medicare home health file.
Dementia status was determined at each survey wave using criteria for probable dementia established by NHATS which incorporates self-report of dementia, proxy responses to the Alzheimer’s disease (AD)-8 screening tool, and a cognitive interview that assessed memory, orientation, and function both through self-report and direct cognitive assessment conducted by NHATS.28 Based on our previous analysis of factors associated with the use of HBMC,23 we examined the following demographic, clinical and environmental characteristics: age, sex, self-reported race/ethnicity, education, Medicaid enrollment, living alone, residing in a metropolitan area, residing in a non-nursing facility residential setting (e.g., assisted living), geographic region (Northeast, Midwest, South, West), receiving help with activities of daily living (eating, bathing, toileting, dressing, walking inside, transferring in/out of bed), any hospital admission within a year after NHATS survey, and self-reported medical conditions (heart attack, stroke, cancer, heart disease, hypertension, diabetes, lung disease, depression).
Analysis:
First, we compared utilization of any home-based clinical care and each of the 4 identified types of care based on dementia status adjusting for age. We calculated age-adjusted risk ratios with 95% confidence intervals. Next, we compare use of home-based clinical care among persons with dementia by demographic, clinical and environmental factors using bivariate logistic regression models. Finally, we conducted four multivariable logistic regression models to examine factors associated with use of HBMC, podiatry, other FFS home-based clinical care, and SHHC among those with dementia. We account for multiple observations per individual though clustering in the survey command as per NHATS guidance.29
Because these findings relied on multiple observations per individual, as a sensitivity analysis we repeated analyses among unique individuals from 2015 NHATS cohort, which provided the largest sample for unique individuals as the unit of analysis. All analyses used Stata Version 16 and accounted for survey design and sampling approach.
The Johns Hopkins University Institutional Review Board (IRB) approved the National Health and Aging Trends Study (NHATS) protocol. The Icahn School of Medicine at Mount Sinai’s IRB approved the present study.
Results
Nearly half of PWD received any type of home-based clinical care (44.4%) over 12 months. PWD were significantly more likely than persons without dementia to receive any type of home-based clinical care after adjusting for age (risk ratio =2.4; 95% CI=2.2–2.6) (Figure 1). PWD were also more likely to use each type of home-based clinical care compared to persons without dementia. The largest difference in care receipt was among HBMC: 14.2% of PWD received HBMC compared to < 2% of those without dementia (risk ratio=4.9; 95% CI=3.8–6.2). Podiatry and other FFS home-based clinical care was used far more frequently among PWD (risk ratios >3.0). SHHC was used by more than one third (34.3%) of PWD compared to only 12.3% of those without dementia.
Figure 1: Use of Medicare-funded home-based clinical care among PWD.
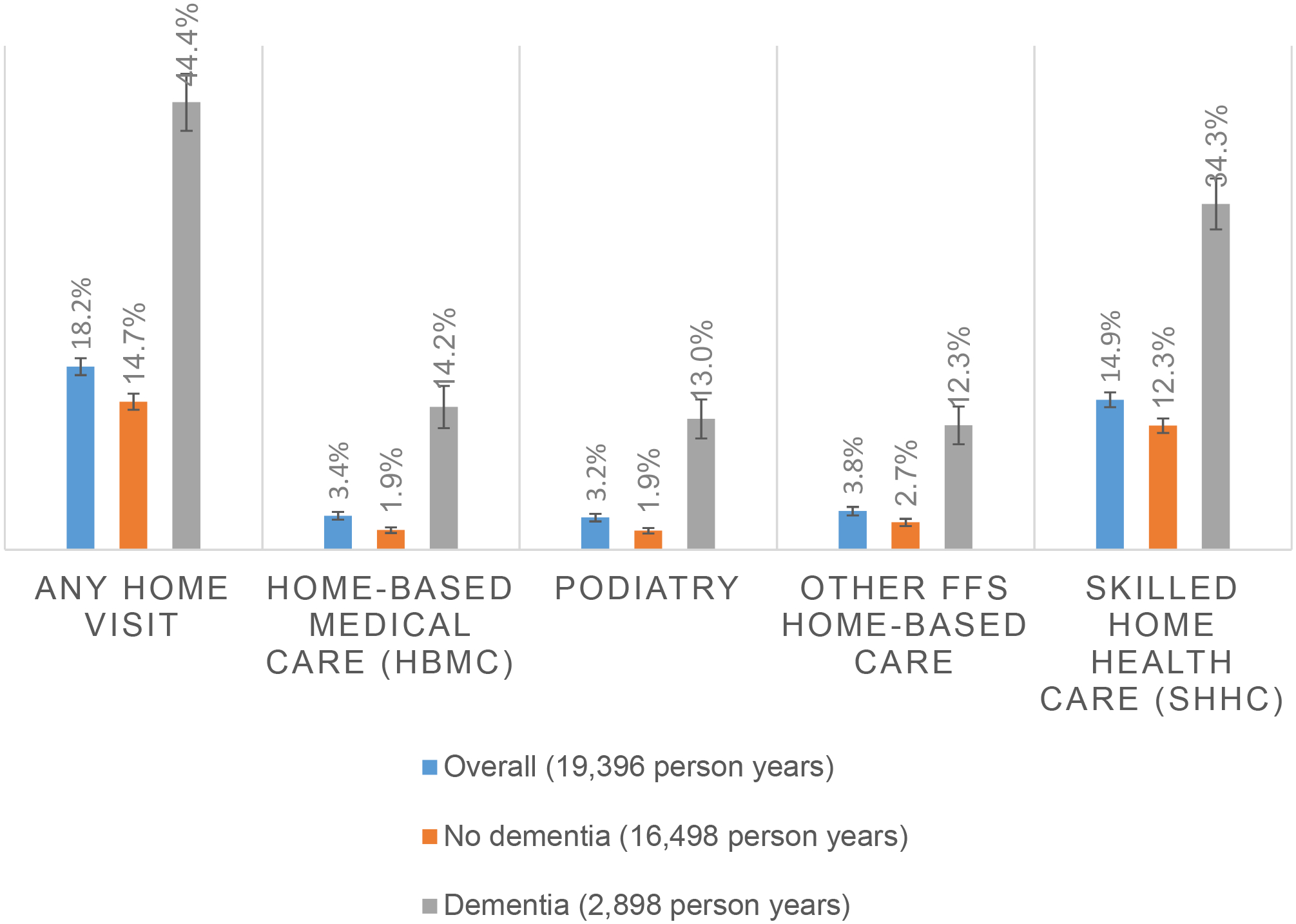
All estimates are age-adjusted and adjusted for survey weights
Among those with dementia, use of home-based clinical care varied based on sociodemographic and clinical factors and the environmental context. As shown in Table 1, all home-based clinical services were more frequently used by females, with significant differences for HBMC (68.5% female among HBMC users vs. 56.3% among non-users). There was also significantly less use of HBMC and podiatry among Hispanic/Latino NHATS participants. Not surprisingly, all home-based clinical services were used more frequently by those with more ADL impairment and by those who experienced hospitalizations during the measurement period. PWD living in non-nursing home residential facilities (e.g., assisted living) and those living in metropolitan areas were far more likely to use HBMC, podiatry and others FFS services, as were those who live alone. There was regional variation in use of HBMC, podiatry, and other FFS-home based care. There were not differences in race/ethnicity, residential setting and region between those who received SHHC vs. those who did not.
Table 1.
Characteristics associated with receipt of home-based clinical care among community-dwelling persons with dementia
| Overall (2898 person years) | HBMC (395 person years) | Podiatry (345 person years) | Other FFS home-based clinical care (359 person years) | SHHC (1052 person years) | |
|---|---|---|---|---|---|
| Demographics | |||||
| Race/ethnicity | |||||
| White, Non-Hispanic | 74.5% | 79.6% | 82.8% | 75.4% | 75.5% |
| Black, Non-Hispanic | 10.9% | 12.8% | 10.3% | 13.4% | 12.8% |
| Other, Non-Hispanic | 5.1% | NR | NR | NR | 2.9% |
| Hispanic/Latino | 9.5% | NR* | NR* | NR | 8.8% |
| Female | 58.0% | 68.5%* | 63.3% | 65.9% | 60.6% |
| Age | |||||
| <75 | 13.1% | 10.5% | 6.5% | 10.2% | 11.0% |
| 75–79 | 16.9% | 8.6% | 9.1% | 12.1% | 15.9% |
| 80–84 | 24.6% | 19.2% | 21.4% | 22.3% | 24.5% |
| 85+ | 45.3% | 61.7% | 63.0%* | 55.3% | 48.6% |
| Education: >=High school | 61.5% | 68.1% | 76.3%* | 65.4% | 62.5% |
| Income below poverty | 42.0% | 40.3% | 37.7% | 49.2% | 43.4% |
| Medicaid | 27.8% | 29.9% | 28.2% | 37.0%* | 29.9% |
| Clinical | |||||
| self-reported chronic condition count (Mean) | 2.0 | 2.1 | 2.0 | 2.2* | 2.2* |
| Charlson comorbidity index (Mean) | 2.1 | 2.4* | 2.4* | 2.5* | 2.7* |
| Number of ADL impairments | |||||
| 0 | 31.3% | 20.7%* | 21.6% | 16.8%* | 19.9%* |
| 1–2 | 33.0% | 34.5%* | 32.0% | 37.7%* | 35.0%* |
| 3+ | 35.7% | 44.9%* | 46.4%* | 45.4%* | 45.1%* |
| Any hospital admission 12 months after survey | 36.3% | 48.9%* | 47.6%* | 55.0%* | 60.4%* |
| Environmental | |||||
| Residential Care, excl. NH | 20.5% | 52.2%* | 61.8%* | 42.8%* | 23.0% |
| Lives alone | 35.4% | 57.5%* | 60.1%* | 49.8%* | 35.4% |
| Lives in metropolitan area | 83.8% | 92.9%* | 94.3%* | 92.0%* | 85.1% |
| Region | |||||
| Northeast | 17.8% | 26.4% | 27.4% | 28.2% | 19.5% |
| Midwest | 17.2% | 17.0% | 22.0% | 15.0%* | 17.5% |
| South | 44.4% | 42.8%* | 32.8%* | 41.4%* | 47.2% |
| West | 20.6% | 13.7%* | 17.8%* | 15.4%* | 15.8%* |
| Year of NHATS interview | |||||
| 2011 | 18.5% | 14.3% | 15.8% | 13.9% | 17.3% |
| 2012 | 17.0% | 17.7%* | 16.3% | 15.4% | 17.4% |
| 2013 | 16.8% | 16.8% | 13.5% | 17.5%* | 15.6% |
| 2014 | 16.3% | 18.9%* | 17.0% | 15.9% | 15.1% |
| 2015 | 15.3% | 15.9% | 20.2%* | 18.4%* | 17.5%* |
| 2016 | 16.0% | 16.3% | 17.1% | 18.8% | 17.1% |
Repeat observations per individuals; all estimates survey weighted; NR = not reportable per NHATS/CMS guidelines; Referent category = white race, age <75, 0 ADLs, Northeast region, 2011 Year of NHATS interview; HBMC= Home based medical care; SHHC= Skilled home healthcare; self-reported chronic condition count rabged from 0–8 based on the following medical conditions: heart attack, stroke, cancer, heart disease, hypertension, diabetes, lung disease, depression; Charlson Comorbidity Index determined based on 6 months claims prior to NHATS interview;
p<.05 compares those who receive vs those who did not receive each service type using bivariate logistic regression analysis
In adjusted logistic regression models (Table 2), the Hispanic/Latino population was significantly less likely to use HBMC than non-Hispanic Whites (OR =0.28; 95% CI=0.10–0.80). This population also tended to use less podiatry and other home-based clinical services, although differences were not significant. Podiatry services were far more likely to be used by older PWD (OR=3.35 age 85+ vs <75). PWD with Medicaid used more podiatry and other in-home services. Hospitalizations and functional impairment were significant drivers of all services. Living in residential facilities and metropolitan areas were significant drivers of HBMC, podiatry and other FFS care. Similarly, regional variation was evident for receipt of HBMC, podiatry and other FFS home-based care. For example, there was far less use of HBMC in the South (OR=0.54; 95% CI=0.29 – 1.00) and West (OR =0.34; 95% CI=0.16–0.75) compared to the Northeast. The use of SHHC among PWD, on the other hand, was not associated with environment including region other than less use in the West relative to the Northeast (OR=0.63; 95%CI=0.41–1.00). Results from multivariable analyses were not substantively different when accounting for missingness of covariates (10.5% of dementia sample) using previous wave Medicaid status and multiple imputation in Stata (See Supplementary Table S1) although some findings were no longer statistically significant.
Table 2:
Factors associated with utilization of HBMC, podiatry, other FFS home-based clinical care, and home health care among community-dwelling persons with dementia
| HBMC | Podiatry | Other FFS home-based clinical care | SHHC | |
|---|---|---|---|---|
| Race/Ethnicity | ||||
| Black, Non-Hispanic | 1.35 (0.78 – 2.34) |
1.36 (0.78 – 2.40) |
1.38 (0.83 – 2.29) |
1.16 (0.84 – 1.61) |
| Hispanic/Latino | 0.28 (0.10 – 0.80) |
0.27 (0.07 – 1.12) |
0.67 (0.28 – 1.59) |
0.97 (0.60 – 1.55) |
| Female | 1.52 (0.97 – 2.41) |
0.83 (0.53 – 1.30) |
1.24 (0.81 – 1.89) |
1.09 (0.83 – 1.43) |
| Age | ||||
| 75–79 | 0.64 (0.22 – 1.88) |
1.92 (0.72 – 5.11) |
1.12 (0.42 – 2.97) |
1.24 (0.74 – 2.09) |
| 80–84 | 0.81 (0.30 – 2.17) |
2.71 (1.06 – 6.93) |
1.31 (0.51 – 3.34) |
1.59 (0.96 – 2.61) |
| 85+ | 1.3 (0.52 – 3.24) |
3.35 (1.37 – 8.18) |
1.32 (0.55 – 3.17) |
1.36 (0.85 – 2.19) |
| Education: >=High school | 1.00 (0.57 – 1.76) |
1.74 (1.05 – 2.89) |
1.27 (0.75 – 2.17) |
1.22 (0.91 – 1.63) |
| Has Medicaid | 1.36 (0.76 – 2.44) |
1.70 (0.96 – 3.03) |
2.01 (1.16 – 3.47) |
1.43 (1.02 – 2.01) |
| Count of self-reported chronic conditions | 1.09 (0.96 – 1.23) |
1.03 (0.91 – 1.16) |
1.07 (0.95 – 1.20) |
1.08 (0.998 – 1.18) |
| Number of ADL impairments | ||||
| 1–2 | 1.31 (0.81 – 2.12) |
1.15 (0.68 – 1.93) |
2.19 (1.32 – 3.63) |
1.85 (1.37 – 2.51) |
| 3+ | 1.82 (1.15 – 2.87) |
2.11 (1.26 – 3.55) |
2.64 (1.59 – 4.39) |
2.43 (1.82 – 3.26) |
| Any hospital admission 12 months after survey | 1.46 (1.04 – 2.04) |
1.41 (0.97 – 2.04) |
1.93 (1.42 – 2.63) |
4.73 (3.78 – 5.91) |
| Residential care, excl. NH | 4.58 (2.81 – 7.49) |
8.12 (4.67 – 14.11) |
2.80 (1.69 – 4.64) |
1.13 (0.77 – 1.66) |
| Lives alone | 1.10 (0.69 – 1.75) |
0.88 (0.51 – 1.51) |
0.99 (0.63 – 1.54) |
0.81 (0.59 – 1.10) |
| Lives in metropolitan area | 2.48 (1.21 – 5.10) |
3.96 (1.92 – 8.15) |
2.07 (1.07 – 4.00) |
1.1 (0.78 – 1.56) |
| Region | ||||
| Midwest | 0.53 (0.26 – 1.07) |
0.95 (0.49 – 1.85) |
0.47 (0.24 – 0.94) |
0.99 (0.64 – 1.52) |
| South | 0.54 (0.29 – 1.00) |
0.41 (0.23 – 0.75) |
0.55 (0.31 – 0.96) |
1.12 (0.79 – 1.59) |
| West | 0.34 (0.16 – 0.75) |
0.52 (0.26 – 1.02) |
0.45 (0.21 – 0.94) |
0.63 (0.41 – 0.99) |
| Year of NHATS interview | 1.02 (0.93 – 1.12) |
1.04 (0.94 – 1.15) |
1.06 (0.96 – 1.16) |
1.04 (0.97 – 1.11) |
Referent category = white race, age <75, <HS education, no Medicaid, 0 ADLs, Northeast region; adjusted for survey year; due to very small cell size, other race category was set to missing; HBMC= Home based medical care; SHHC= Skilled home healthcare
As a sensitivity analysis, we repeated analyses limiting to the 2015 NHATS population. Our findings regarding higher use of home-based clinical care in dementia were consistent (e.g., 49.6% PWD received any home-based clinical care). Although limited sample size precluded the application of a regression model, we found similar predictors of individual types of home-based clinical care within the dementia population (See Supplementary Tables S2–3).
Discussion
Our study, the first to examine the provision of home-based clinical care among PWD nationally, finds that nearly half of PWD living in the community receive Medicare-funded home-based clinical care each year. Higher use among PWD compared to those without dementia is evident across all 4 types of home-based clinical care assessed: HBMC, podiatry, other FFS clinical services (e.g., behavioral health, imaging/diagnostics) and SHHC. We also find that home-based clinical care use among PWD is highly variable with variation due to environmental and demographic factors.
There is significantly less HBMC and other FFS home-based clinical care provided to Hispanic/Latino PWD. This is problematic given that they are the fastest growing subpopulation among the aging homebound population30 and are less likely to receive institutional care.31 Limited use in this population may have to do with availability and use of interpreters, care referral patterns, delay in start of care, caregiving environment, and preferences and suitability of the home for home-based clinical care, although this needs to be further evaluated.32 Moreover, our study and others find that Hispanic/Latino older adults are less likely to live in residential facilities such as assisted livings33 where there is far greater use of HBMC, podiatry, and other home-based clinical services. More research and larger sample sizes will be needed to adequately study needs of the aging Hispanic/Latino population in the US.
SHHC use, on the other hand, appears more ubiquitous geographically, although we do find less use in the western region, as others have observed.34 SHHC and nursing home care have been components of post-acute care since Medicare was established and therefore have more established infrastructures across the country.35 While SHHC use appears to be driven more by clinical need, more work is necessary to better understand whether SHHC is as readily accessible through community referrals as compared to only the post-acute setting. While Medicare allows for both forms of SHHC, PWD appear to use community-initiated services at higher rates.25
Our study uncovered a spectrum of home-based clinical services currently used by PWD. While SHHC was most commonly used (34.3%), in-home podiatry care was accessed by 13% of PWD per year. While podiatry interventions have been evaluated to reduce falls,36 more research is needed to examine how home-based podiatry services, in particular, may benefit PWD, as well as other older adults with multimorbidity. While there are many types of home-based clinical services and procedures reimbursed via FFS Medicare that could potentially be provided to PWD, most are in practice rare. For example, in-home behavioral health services are currently provided to <1% PWD, although they may be especially beneficial for the management of behavioral symptoms among PWD.
The high use of home-based clinical care by PWD is, in many respects, not surprising given the challenges PWD and their caregivers face in accessing traditional ambulatory care services.16 Arranging transportation and navigating unfamiliar clinical environments for PWD is challenging, especially in the context of declining function and onset of behavioral symptoms. Home-based clinical care is well-suited to address this need. Care in the home offers a number of advantages, including working closely with the family and paid caregiving team, as well as allowing clinicians to identify safety and environmental needs for PWD (e.g., assessment of falls risk).37, 38 Moreover, proactive preventive care and caregiver support may reduce likelihood for hospitalizations.
Yet more than half of PWD are not accessing home-based clinical care. A key driver of the underutilization of HBMC, podiatry, and other FFS clinical care by PWD in the community is likely due to limited availability of these services. A key driver of lack of ubiquity of non-SHHC home-based clinical services is the challenge of creating a financially sustainable model for home -based clinical care within a FFS system. Currently, reimbursement for care of patients with complex chronic illness and functional impairments may be inadequate, especially given travel time required for home-based services. Far higher rates of HBMC among those living in residential facilities (e.g., assisted living) and in metropolitan areas likely reflect the fact that favorable geographic factors create operational efficiencies and opportunities to improve the financial sustainability of HBMC practices. This is consistent with literature reporting a dearth of HBMC practices in rural areas.27 Also of note, there are existing workforce shortages in geriatric care further challenging provision of specialty home-based and dementia care.39 In order to address the high need of care in the home and inadequate services currently available, new models of care will be required that more effectively leverages interprofessional care and still assures skills and competence in dementia and home-based care.40
This study had several potential limitations. Dementia status and other variables were determined annually via survey and may not reflect possible fluctuations in these characteristics between intervals. In addition, claims data were available only for FFS Medicare beneficiaries. While our results do not include HBMC that occurs under Medicare Advantage, a 2020 analysis of HBMC in the Medicare Advantage population found similar HBMC utilization estimates.41 More work is necessary to examine use of home-based clinical care within Medicare Advantage. Additionally, this study does not include data on Medicaid-funded home-based clinical care or acute home-based medical services such as hospital at home or paramedicine, which fall outside of the scope of this study. We did not include home-based hospice care in this analysis given the unique prognosis-dependent nature of hospice. (Overall use of home-based clinical care among PWD further increases to 47.9% when we include hospice.) While we used a general indicator of receipt of any SHHC, future analyses will examine type, timing and duration of SHHC relative to hospitalization and receipt of other home-based clinical services. Additionally, we defined use of other home-based clinical care as >=1 encounter per one-year period which may represent more episodic care delivery rather than longitudinal home-based care. However, we did not see significant differences in utilization patterns when we restricted analyses to multiple HBMC visits (data not shown). Future research will examine longitudinal patterns of home visits including variation by visit type (e.g., annual wellness visit).
Despite these limitations our work provides critical information on an essential healthcare delivery mechanism for a growing yet underserved population. Nearly half of community-dwelling Medicare beneficiaries with dementia receive home-based clinical care each year. Access was strongly driven by regional and residential factors, indicating that the pool of individuals who may benefit from home-based clinical care may be greater than those who receive it. This gap in access to home-based clinical care is especially crucial in the context of how COVID-19 has changed concerns over safety in institutional settings and may further drive care from nursing facilities into the home. Equitable access to high quality home-based clinical care will require ensuring adequate payment mechanisms for in-home care providers.
Supplementary Material
Table S1. Factors associated with utilization of HBMC, podiatry, other FFS home-based clinical care, and home health care among community-dwelling persons with dementia (with imputation of Medicaid status and education).
Table S2. Utilization of home-based clinical services among persons living with and without dementia in the community, 2015 (n=3801).
Table S3. Characteristics associated with receipt of home-based clinical services among community-dwelling persons with dementia, 2015.
Key Points.
Almost half of persons with dementia receive some type of Medicare-funded home-based clinical care annually including home-based medical care, podiatry services, and skilled home health care.
Use of services among persons with dementia vary significantly based on sociodemographic factors (e.g., race/ethnicity) and environmental setting (e.g., region, urbanicity).
Why does this matter?
As dementia care shifts into the home for longer periods, it is critical that high quality Medicare-funded home-based clinical care of all kinds have the capacity to reach persons in the community living with dementia.
Acknowledgments
The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (grant number NIA U01AG032947) and is conducted at the Johns Hopkins University. This study was supported by National Institute on Aging P01AG066605 (Drs. Ornstein and Ritchie), K76AG064427 (Dr. Ankuda), K23AG066930 (Dr. Reckrey), K24AG062785 (Dr. Kelley), and P30AG028741.
Sponsor’s Role:
Funders played no role in the study’s design, analysis, and preparation of the article.
Funding:
Funding for this study was provided by NIA U01AG032947, P01AG066605, K76AG064427, K23AG066930, K24AG062785, and P30AG028741.
Footnotes
Conflicts of Interest: The authors have no conflicts.
References
- 1.Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. May 7 2013;80(19):1778–83. doi: 10.1212/WNL.0b013e31828726f5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alzheimer’s Association. 2019 ALZHEIMER’S DISEASE FACTS AND FIGURES. Alzheimer’s Dement. 2019;15(3):321–387. [Google Scholar]
- 3.Kelley AS. Defining “serious illness”. Journal of palliative medicine. Sep 2014;17(9):985. doi: 10.1089/jpm.2014.0164 [DOI] [PubMed] [Google Scholar]
- 4.Kelley AS, Covinsky KE, Gorges RJ, et al. Identifying Older Adults with Serious Illness: A Critical Step toward Improving the Value of Health Care. Health Serv Res. Feb 2017;52(1):113–131. doi: 10.1111/1475-6773.12479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholzel-Dorenbos CJ, Meeuwsen EJ, Olde Rikkert MG. Integrating unmet needs into dementia health-related quality of life research and care: Introduction of the Hierarchy Model of Needs in Dementia. Aging & mental health. Jan 2010;14(1):113–9. doi: 10.1080/13607860903046495 [DOI] [PubMed] [Google Scholar]
- 6.Fortinsky RH. Health care triads and dementia care: Integrative framework and future directions. Aging & mental health. May 2001;5(sup1):35–48. doi: 10.1080/713649999 [DOI] [PubMed] [Google Scholar]
- 7.Fortinsky RH, Downs M. Optimizing person-centered transitions in the dementia journey: a comparison of national dementia strategies. Health Aff (Millwood). Apr 2014;33(4):566–73. doi: 10.1377/hlthaff.2013.1304 [DOI] [PubMed] [Google Scholar]
- 8.Austrom MG, Boustani M, LaMantia MA. Ongoing Medical Management to Maximize Health and Well-being for Persons Living With Dementia. Gerontologist. Jan 18 2018;58(suppl_1):S48–S57. doi: 10.1093/geront/gnx147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolff JL, Kasper JD, Shore AD. Long-term care preferences among older adults: a moving target? Journal of aging & social policy. 2008;20(2):182–200. [DOI] [PubMed] [Google Scholar]
- 10.Gillsjo C, Schwartz-Barcott D, von Post I. Home: the place the older adult cannot imagine living without. BMC geriatrics. Mar 17 2011;11:10. doi: 10.1186/1471-2318-11-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eiken S, Burwell B, Sredl K. An examination of the woodwork effect using national medicaid long-term services and supports data. Journal of aging & social policy. 2013;25(2):134–45. doi: 10.1080/08959420.2013.766054 [DOI] [PubMed] [Google Scholar]
- 12.Aldridge MD, Bradley EH. Epidemiology And Patterns Of Care At The End Of Life: Rising Complexity, Shifts In Care Patterns And Sites Of Death. Health Aff (Millwood). Jul 1 2017;36(7):1175–1183. doi: 10.1377/hlthaff.2017.0182 [DOI] [PubMed] [Google Scholar]
- 13.Mitchell SL, Black BS, Ersek M, et al. Advanced dementia: state of the art and priorities for the next decade. Annals of internal medicine. Jan 3 2012;156(1 Pt 1):45–51. doi: 10.7326/0003-4819-156-1-201201030-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harrison KL, Ritchie CS, Patel K, et al. Care Settings and Clinical Characteristics of Older Adults with Moderately Severe Dementia. J Am Geriatr Soc. Sep 2019;67(9):1907–1912. doi: 10.1111/jgs.16054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ouslander JG, Grabowski DC. COVID-19 in Nursing Homes: Calming the Perfect Storm. J Am Geriatr Soc. Oct 2020;68(10):2153–2162. doi: 10.1111/jgs.16784 [DOI] [PubMed] [Google Scholar]
- 16.Samus QM, Black BS, Bovenkamp D, et al. Home is where the future is: The BrightFocus Foundation consensus panel on dementia care. Alzheimer’s & dementia : the journal of the Alzheimer’s Association. Jan 2018;14(1):104–114. doi: 10.1016/j.jalz.2017.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Desai NR, Smith KL, Boal J. The positive financial contribution of home-based primary care programs: the case of the Mount Sinai Visiting Doctors. J Am Geriatr Soc. Apr 2008;56(4):744–9. NOT IN FILE. doi: 10.1111/j.1532-5415.2007.01641.x [DOI] [PubMed] [Google Scholar]
- 18.Aldridge MD, kelley AS. Epidemiology of serious illness and high utilization of health care. Institute of Medicine Dying in America: improving quality and honoring individual preferences near the end of life. National Academies Press; 2014:397–438. [PubMed] [Google Scholar]
- 19.Musich S, Wang SS, Hawkins K, Yeh CS. Homebound older adults: Prevalence, characteristics, health care utilization and quality of care. Geriatric nursing (New York, NY). Nov-Dec 2015;36(6):445–50. doi: 10.1016/j.gerinurse.2015.06.013 [DOI] [PubMed] [Google Scholar]
- 20.Ankuda CK, Ornstein KA, Leff B, Kinosian B, Brody AA, Ritchie CS. Defining a taxonomy of Medicare-funded home-based clinical care using claims data. 2021;under review [DOI] [PMC free article] [PubMed]
- 21.Ritchie CS, Leff B. Population Health and Tailored Medical Care in the Home: the Roles of Home-Based Primary Care and Home-Based Palliative Care. Journal of pain and symptom management. Mar 2018;55(3):1041–1046. doi: 10.1016/j.jpainsymman.2017.10.003 [DOI] [PubMed] [Google Scholar]
- 22.Medicare Payment Advisory Commission. Medicare Payment Policy: Report to the Congress. medpac; 2019:chap 19. Accessed 4/1/19. http://medpac.gov/docs/default-source/reports/mar19_medpac_entirereport_sec.pdf?sfvrsn=0
- 23.Reckrey JM, Yang M, Kinosian B, et al. Receipt Of Home-Based Medical Care Among Older Beneficiaries Enrolled In Fee-For-Service Medicare. Health Aff (Millwood). Aug 2020;39(8):1289–1296. doi: 10.1377/hlthaff.2019.01537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Department of Health and Human Services. The National Plan to Address Alzheimer’s Disease: 2018 update. Accessed april 1, 2019, https://aspe.hhs.gov/national-plans-address-alzheimers-disease
- 25.Ankuda CK, Leff B, Ritchie CS, et al. Implications of 2020 Skilled Home Healthcare Payment Reform for Persons with Dementia. J Am Geriatr Soc. Oct 2020;68(10):2303–2309. doi: 10.1111/jgs.16654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freedman VA, Kasper JD. Cohort Profile: The National Health and Aging Trends Study (NHATS). Int J Epidemiol. Aug 1 2019;48(4):1044–1045g. doi: 10.1093/ije/dyz109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yao N, Ritchie C, Camacho F, Leff B. Geographic Concentration Of Home-Based Medical Care Providers. Health Aff (Millwood). Aug 1 2016;35(8):1404–9. doi: 10.1377/hlthaff.2015.1437 [DOI] [PubMed] [Google Scholar]
- 28.Kasper JD, Freedman VA, Spillman B. Classification of Persons by Dementia Status in the National Health and Aging Trends Study. Technical Paper #5. 2013. May be accessed at www.nhats.org
- 29.Freedman VA, Hu M, DeMatteis J, Kasper JD. Accounting for Sample Design in NHATS and NSOC Analyses: Frequently Asked Questions. NHATS Technical Paper #23. Johns Hopkins University School of Public Health. Accessed 6/1/2021, https://nhats.org/sites/default/files/2021-01/Accounting_for_the_NHATS_NSOC_Design_in_Analyses_FAQ_1.pdf
- 30.Ankuda CK, Leff B, Ritchie CS, Siu AL, Ornstein KA. Association of the COVID-19 Pandemic With the Prevalence of Homebound Older Adults in the United States, 2011–2020. JAMA internal medicine. 2021;doi: 10.1001/jamainternmed.2021.4456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gorges RJ, Sanghavi P, Konetzka RT. A National Examination Of Long-Term Care Setting, Outcomes, And Disparities Among Elderly Dual Eligibles. Health Aff (Millwood). Jul 2019;38(7):1110–1118. doi: 10.1377/hlthaff.2018.05409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Song J, Zolnoori M, McDonald MV, et al. Factors Associated with Timing of the Start-of-Care Nursing Visits in Home Health Care. Journal of the American Medical Directors Association. Apr 9 2021;doi: 10.1016/j.jamda.2021.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aldridge MD, Ornstein KA, McKendrick K, Moreno J, Reckrey JM, Li L. Trends In Residential Setting And Hospice Use At The End Of Life For Medicare Decedents. Health Aff (Millwood). Jun 2020;39(6):1060–1064. doi: 10.1377/hlthaff.2019.01549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang Y, Leifheit-Limson EC, Fine J, et al. National Trends and Geographic Variation in Availability of Home Health Care: 2002–2015. J Am Geriatr Soc. Jul 2017;65(7):1434–1440. doi: 10.1111/jgs.14811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benjamin AE. An historical perspective on home care policy. The Milbank quarterly. 1993;71(1):129–66. [PubMed] [Google Scholar]
- 36.Wylie G, Torrens C, Campbell P, et al. Podiatry interventions to prevent falls in older people: a systematic review and meta-analysis. Age and ageing. May 1 2019;48(3):327–336. doi: 10.1093/ageing/afy189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Callahan CM, Boustani M, Sachs GA, Hendrie HC. Integrating care for older adults with cognitive impairment. Current Alzheimer research. Aug 2009;6(4):368–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Olsan TH, Shore B, Coleman PD. A clinical microsystem model to evaluate the quality of primary care for homebound older adults. Journal of the American Medical Directors Association. Jun 2009;10(5):304–13. doi: 10.1016/j.jamda.2009.02.003 [DOI] [PubMed] [Google Scholar]
- 39.Flaherty E, Bartels SJ. Addressing the Community-Based Geriatric Healthcare Workforce Shortage by Leveraging the Potential of Interprofessional Teams. J Am Geriatr Soc. May 2019;67(S2):S400–s408. doi: 10.1111/jgs.15924 [DOI] [PubMed] [Google Scholar]
- 40.Ritchie CS, Leff B, Garrigues SK, Perissinotto C, Sheehan OC, Harrison KL. A Quality of Care Framework for Home-Based Medical Care. Journal of the American Medical Directors Association. Oct 2018;19(10):818–823. doi: 10.1016/j.jamda.2018.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harrison KL, Leff B, Altan A, Dunning S, Patterson CR, Ritchie CS. What’s Happening at Home: A Claims-based Approach to Better Understand Home Clinical Care Received by Older Adults. Med Care. Apr 2020;58(4):360–367. doi: 10.1097/MLR.0000000000001267 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Factors associated with utilization of HBMC, podiatry, other FFS home-based clinical care, and home health care among community-dwelling persons with dementia (with imputation of Medicaid status and education).
Table S2. Utilization of home-based clinical services among persons living with and without dementia in the community, 2015 (n=3801).
Table S3. Characteristics associated with receipt of home-based clinical services among community-dwelling persons with dementia, 2015.


