Abstract
Background:
One in twenty older adults in the United States is homebound and rarely/never leaves home. Although being homebound decreases the quality of the lived experience of individuals with serious illnesses, little is known about the frequency or likelihood of transitions in or out of homebound status. The objective of this study was to characterize the probability of transitions to and from homebound status among older adults and examine the relationship between dementia status and homebound transitions.
Methods:
Using 2011–2018 data from the National Health and Aging Trends Study (NHATS), a nationally-representative longitudinal study of aging in the US, we identified 6,375 community-dwelling Medicare beneficiaries. Homebound status (independent, semi-homebound (leaving home but with difficulty or help), homebound (rarely or never leaving home), nursing home resident, dead) was assessed annually via self-report. Transition probabilities across states was assessed using a multistate Markov model.
Results:
Less than half of homebound individuals remain homebound (probability = 41.5% [95% CI: 39.2%, 43.5%]) after one year. One out of four die (24% [22.3%, 26.0%]) and there is a low probability (3.2% [2.5%, 4.1%]) of transition to a nursing home. Dementia status was associated with increased risk of progression from independence to homebound status (HR: 1.83 [1.01, 3.34]). Dementia was consistently associated with increased probabilities of transitions to death including a two-fold increased hazards of progression from homebound to death (HR: 2.18 [1.69, 2.81]). Homebound individuals with dementia have a 34.2% [25.8%, 48.1%] probability of death in 5 years, compared to 17.4% [13.7%, 24.3%] among those without dementia.
Discussion:
Dementia is associated with greater risk of transitioning across homebound states. There is a greater need to support home-based care for patients with dementia, especially as the ongoing COVID pandemic has raised concerns about the need to invest in alternative models to nursing home care.
Keywords: homebound, dementia, Markov models
Background
As the population ages, a growing number of older adults with serious illnesses, including dementia, reside in the community.1–3 As their function declines, many older adults require extensive care provided through supportive care environments and/or paid and unpaid caregiving. Our previous work using data from the National Health and Aging Trends Study (NHATS) found that a staggering one out of 20 older adults nationwide were homebound (defined as rarely or never leaving home).4 Notably, the homebound population is significantly larger than the nursing home population.5, 6 Dementia is highly prevalent among the homebound population,4, 7, 8 with estimates suggesting that more than half of the homebound population have extensive cognitive impairment coupled with associated functional challenges.
By virtue of their condition, the homebound are understudied and often “invisible” relative to care delivery and quality.9 Yet an increasing evidence base suggests there are adverse downstream consequences of becoming homebound. The homebound experience high symptom burden,10 significant functional impairment,4 have higher medication use,11 hospitalization,12, 13 and health care utilization4 than their non-homebound counterparts. Even when compared to individuals with similar demographic, functional, and clinical characteristics, the homebound have greater mortality.14, 15 Consequences of being homebound, like difficulty accessing routine medical care,4 increased depression,16 and inability to engage in valued activities,17 may contribute to these poor outcomes.
Nearly half of community-dwelling older adults are homebound in the year before death.14 Despite this, little is known about what influences transitions between being homebound, recovering, and dying, or how long community-dwelling individuals with serious illness remain homebound. Homebound status may be a dynamic state — one year after older adults were identified as newly homebound, we have found that only one-third remained homebound and only 2.2% transitioned to a nursing home.18 To date, there is limited insight into both the predictors and timing of transitions from living independently in the community to relying on others to leave home and becoming functionally homebound.
Understanding the forces that influence both recovery and death for homebound older adults can assist in the development and dissemination of appropriate medical and supportive services for homebound individuals and their families. Of particular concern is the degree to which dementia, which is highly prevalent among the homebound and nursing home populations, influences transitions between homebound states. Identifying the populations at highest risk for being persistently homebound, requiring institutionalization, or dying is a necessary step to both identify unmet needs and target supports. This information is urgently needed as we continue to address the ongoing COVID pandemic in which nursing homes are struggling financially, residents face medical risk and social isolation and there has been a clear need for the development of home and community-based services as alternative models to nursing home care.19 In this study, we leverage a prospective national cohort study that followed older adults for up to 8 years and comprehensively examine their transitions between being homebound, recovering, residing in a nursing home, or dying.
Methods
Sample
Data came from the National Health and Aging Trends Study (NHATS), a nationally-representative annual longitudinal study of Medicare beneficiaries age 65 and over.20 Among 7,609 community-dwelling older adults surveyed in 2011, 6,554 had follow up data at wave 2 and were eligible for study inclusion. Among this sample, we excluded 179 individuals (2.7%) who were missing data on homebound status or other covariates. Data are included from 6,375 initially community-dwelling individuals who are followed longitudinally up to 8 waves (2011–2018) resulting in 35,148 data points.
Measures
Our primary variables of interest were homeboundness, nursing home admission, and mortality. During each wave (approximately one year intervals), individuals (or their proxies) report ability to leave the home in the last month as follows: independent (not homebound), semi-homebound (needs help or has difficulty leaving the home), or homebound (rarely or never left the home [once per week or less]).4, 21 We chose to differentiate individuals who leave home regularly (at least twice per week) without help or difficulty (‘independent’) from those who have difficulty leaving the home or rely on others to do so (‘semi-homebound’). Thus, the semi-homebound may include individuals who may otherwise be homebound but receive help and travel frequently out of the home for medical care. While our definition of homebound is different from what is used by Medicare to estimate home health service needs,22 it is grounded in prior evidence as to the function and independence of older adults and has been widely used in research.4, 23, 24 We also determined if respondents had been admitted to a long stay nursing home or had died at each wave.
Dementia status was determined using criteria for probable dementia established by NHATS which incorporated self-report of dementia, proxy responses to the Alzheimer’s disease (AD)-8 screening tool, and a cognitive interview that assessed memory, orientation, and function both self-report and direct cognitive assessment conducted by NHATS.25 Based on our previous cross-sectional analysis of factors associated with homebound status,4 we also examined the following covariates: age (over 85), sex, education (High School education and greater), marital status, the presence of 2 or more self-reported comorbidities (heart attack, stroke, cancer, hip fracture, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, depression, and anxiety), impairment with Activities of Daily Living (ADL) (receives help with none vs >=1 ADL), and race/ethnicity (non-Hispanic White vs other racial/ethnic categories). Dementia, age, ADL impairment, and comorbidities were recorded at each timepoint; other covariates were recorded at baseline.
Analysis
We first characterize the transition probabilities between homeboundness states over time, using an unadjusted continuous time homogenous Markov model (Figure 1).22–23 We examine five states: independent, semi-homebound, homebound, residing in nursing home, and deceased. We denote the possible paths by an arrow. Not every path from each state is possible; death is an absorbing state indicating that no paths can go out from that state. Further, temporary nursing home stays shorter than one year were disregarded (<1% of sample); these individuals were reclassified based on their pre-nursing home state.
Figure 1: Graphical representation of five-state Markov model for homeboundess progression.
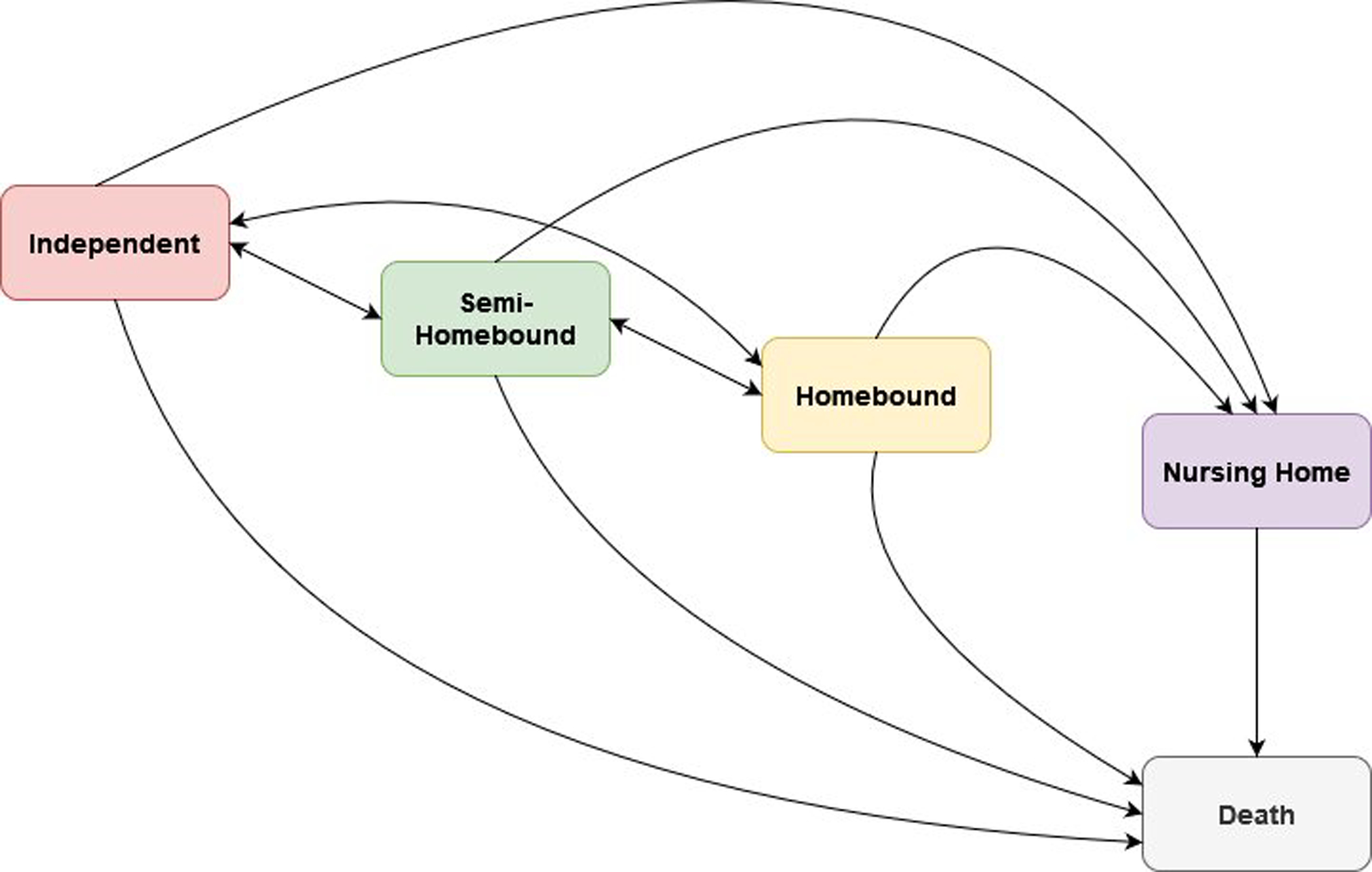
Underlying 5-state model for examining homeboundness progression among NHATs participants, 2011–2018. Model allows for bi-directional transitions between non-homebound, semi-homebound, and homebound states. The nursing home state can only progress to death; the model does not allow progression from nursing home back to community-dwelling states. Death is the absorbing state. Individuals may remain in their existing states.
This model characterizes the likelihood that someone who was homebound at any single wave (wave W) enters into a non-homebound status during the next wave (wave W+1). If an individual is lost to follow-up (e.g., is no longer in the sample but did not die), they can still contribute information to the model for the transitions that we did observe.26
Multistate Markov models assume that transitions across homebound states is a memoryless process; that is, transitions depend on the current state and not on the history of previous states. We implemented two empirical tests to explore whether this Markov assumption is likely to be supported (see Supplementary Materials for details).25,26
We then investigated the association between dementia status and homeboundness transitions, adding covariates (age, sex, education, comorbidities, race/ethnicity, ADLs and marital status) to the model described above. Age, comorbidities, ADLs and dementia status were included as time-varying covariates. Transition-specific hazard ratios and 95% confidence intervals were estimated to determine how dementia status and other covariates are associated with risk of transition across homeboundness states (e.g., from independent to semi-homebound). A hazard ratio greater than 1 indicates dementia status is associated with an increased risk of the transition. A significance level of 0.05 was used to identify factors significantly associated with transition probabilities between homebound states.
Finally, we used our adjusted model to estimate probabilities of homeboundness transitions among participants with and without dementia during any wave. We estimate the probability that someone with dementia, who is currently in one state (e.g., homebound), will transition to another state (e.g., nursing home) after 1 wave and in 5 waves, and contrast this to the transition probability for an individual without dementia. We generated 95% confidence intervals by taking 1000 draws from a multivariate normal distribution of the model’s estimates, as described in detail elsewhere.27 Data management was performed using Stata, version 16.. Analyses used the “msm: Multi-state Markov model” version 1.6.727 and “markovchain” version 0.8.628 R packages in R Studio, version 1.2.5042.
The Johns Hopkins University Institutional Review Board (IRB) approved the National Health and Aging Trends Study (NHATS) protocol. The Icahn School of Medicine at Mount Sinai’s Institutional Review Board (IRB) approved the present study.
Results:
Our sample included 6,375 community-dwelling individuals (homebound, semi-homebound or independent) at wave 1 (2011; Table 1). Individuals were followed up to 8 waves (2018) and on average, completed 5.5 waves before death or loss to follow up. The homebound were older (average age =83.9 years), predominantly female (74.7%) and had more comorbidities and disability than semi-homebound or independent individuals (Table 1). Nearly half of homebound respondents at wave 1 (51.1%) had dementia.
Table 1:
Wave 1 Characteristics by Homebound Status
| Independent (n=4750) |
Semi-Homebound (n=1147) |
Homebound (n=466) |
|
|---|---|---|---|
| Mean age | 76.6 | 80.6 | 83.9 |
| Age 85+ | 15.6 | 34.0 | 51.5 |
| Female | 54.0 | 68.5 | 74.7 |
| White Non-Hispanic | 72.6 | 62.8 | 55.4 |
| Black Non-Hispanic | 19.9 | 26.0 | 29.4 |
| Other race/ethnicity | 2.7 | 2.5 | 3.0 |
| Hispanic | 4.7 | 8.4 | 12.0 |
| >=High School Education | 77.8 | 62.4 | 51.5 |
| Married | 52.9 | 33.5 | 24.3 |
| Has Medicaid | 11.5 | 25.1 | 37.6 |
| Self-reported health=fair/poor | 19.5 | 51.2 | 63.7 |
| Help with 1+ ADL | 6.2 | 48.4 | 74.0 |
| Help with 1+ IADL | 10.6 | 63.0 | 85.8 |
| 2 or more self-reported comorbidities | 97.4 | 94.9 | 91.4 |
| Probable dementia | 6.3 | 26.5 | 51.1 |
| Lives in assisted living | 0.3 | 3.5 | 9.7 |
| Has family/unpaid caregiver | 75.6 | 88.1 | 92.7 |
| Lives in metropolitan area | 80.6 | 81.5 | 84.1 |
| Region: northeast | 17.8 | 17.6 | 18.0 |
| midwest | 23.9 | 20.8 | 23.8 |
| south | 38.3 | 42.5 | 41.6 |
| west | 20.0 | 19.2 | 16.5 |
| Died within one year | 2.9 | 10.4 | 24.3 |
Summary statistics for the community-dwelling NHATs sample. Comparisons between homebound states used t-tests or chi-square analyses; 2 or more comorbidities (heart attack, stroke, cancer, hip fracture,, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, depression, and anxiety); ADL= Activity of Daily Living; IADL=Instrumental Activity of Daily Living.
Unadjusted Markov Model
Figure 2 depicts the probability transition matrix for the unadjusted Markov model. Associated frequency table can be found in the supplementary table (Supplementary Table 1). Participants who are currently homebound are most likely to remain homebound (transition probability = 41.5%, 95% CI: 39.2%, 43.5%) or die by the next wave (24%, 95% CI = 22.3%, 26.0%). There is a moderate probability of improvement in homebound status in the next wave (becoming independent [11%, 95% CI = 10.1%, 12.9%] or semi-homebound [20%, 95% CI = 18.3%, 21.9%). Although the probability of transitioning from homebound to nursing home status is relatively low (3.2%, 95% CI = 2.5%, 4.1%), next-wave nursing home status is more likely for homebound individuals than semi-homebound [2.0%, 95% CI = 1.7%, 2.5%] or independent [0.34%, 95% CI = 0.29%, 0.45%] individuals. Participants who are currently independent are unlikely to become homebound in the next wave (transition probability = 2.2%, 95% CI = 2.0%, 2.5%) and are far more likely to remain independent (84.5%, 95% CI = 84.0%, 84.9%]) or transition to semi-homebound status (9.7%, 95% CI = 9.3%, 10.1%). An individual who is semi-homebound is more likely to remain semi-homebound (46.8% [95% CI = 45.4%, 48.1%]) or become independent (26.5% [95% CI = 25.3%, 27.6%]), than become homebound (12.6% [95% CI = 11.7%, 13.5%]) or die (12.0% [95% CI = 11.3%, 13.0%]) at the next wave. The complete probability transition matrix with 95% confidence intervals is available in Supplementary Table 2.
Figure 2: Transition probabilities by homebound status (2011–2018).
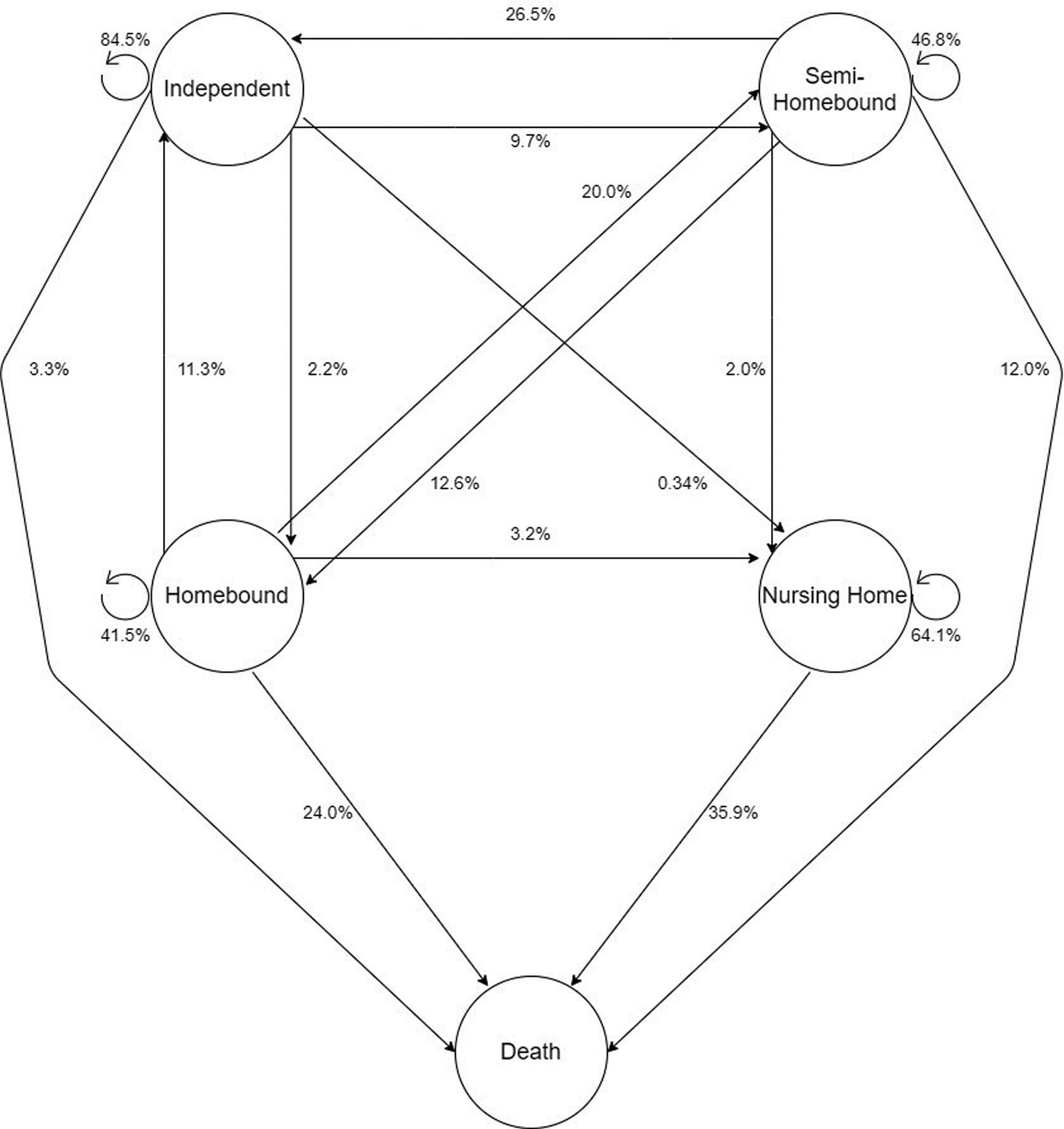
Transition probabilities for next wave status for the 5-state Markov model, unadjusted for covariates. The circular arrows indicate the probability of remaining in the same state in the next wave.
Adjusted Markov model
Transition-specific hazard ratios (HRs) for the multivariate Markov model, which examine the associations among dementia status and other covariates and each possible transition, are given in Table 2. Dementia was associated with increased risk of progression from independence to semi-homebound (HR: 1.69 [1.42, 2.02]), and independence to homebound (HR: 1.83 [1.01, 3.34]). Dementia was also significantly associated with increased hazards of progression from homebound to death (HR: 1.93 [1.49, 2.50]). Similarly, patients with dementia had increased risk of progression from semi-homebound to homebound (HR: 1.70 [1.38, 2.11]), and semi-homebound to death (HR: 1.62 [1.23, 2.15]) (See Supplementary Table 3).
Table 2:
Hazards ratios of dementia and key covariates on transitional probabilities across homebound states
| From Independent (I) | From Homebound (HB) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| I->SHB | I->HB | I->NH | I->D | HB->I | HB->SHB | HB->NH | HB->D | NH->D | |
| Probable Dementia | 1.69 (1.42–2.02) | 1.83 (1.01–3.34) | NA | 1.52 (1.00–2.31) | 0.43 (0.15–1.21) | 0.91 (0.68–1.22) | 0.66 (0.34–1.30) | 1.93 (1.49–2.50) | 1.42 (0.92–2.21) |
| Age 85+ | 1.72 (1.53–1.94) | 2.14 (1.45–3.17) | 1.14 (0.41–3.18) | 2.91 (2.34–3.63) | 0.28 (0.15–0.51) | 0.87 (0.67–1.12) | 2.56 (1.25–5.26) | 1.36 (1.07–1.72) | 2.01 (1.36–2.96) |
| Female | 1.14 (1.01–1.28) | 1.09 (0.71–1.69) | 1.77 (0.43–7.22) | 0.48 (0.38–0.60) | 0.77 (0.47–1.24) | 0.99 (0.74–1.34) | 0.77 (0.39–1.55) | 0.60 (0.47–0.76) | 0.75 (0.48–1.16) |
| High school education or greater | 0.80 (0.71–0.91) | 0.54 (0.36–0.80) | 2.20 (0.68–7.09) | 0.64 (0.50–0.81) | 1.33 (0.82–2.16) | 0.86 (0.68–1.10) | 0.61 (0.33–1.12) | 1.30 (1.03–1.64) | 1.17 (0.82–1.64) |
| White | 0.80 (0.71–0.91) | 0.82 (0.54–1.22) | 4.07 (1.07–15.54) | 1.11 (0.87–1.43) | 2.23 (1.21–4.10) | 0.74 (0.57–0.97) | 3.24 (1.44–7.32) | 1.42 (1.12–1.81) | 1.63 (1.08–2.47) |
| 2+ Comor-bidities | 2.48 (2.00–3.07) | 0.75 (0.45–1.26) | 0.92 (0.28–3.05) | 2.00 (1.44–2.75) | 0.39 (0.20–0.76) | 0.72 (0.41–1.28) | 0.66 (0.24–1.83) | 1.13 (0.59–2.18) | 1.78 (0.73–4.31) |
| Married | 0.83 (0.73–0.94) | 0.57 (0.34–0.96) | 0.32 (0.03–3.37) | 0.66 (0.52–0.84) | 1.06 (0.61–1.69) | 1.01 (0.75–1.35) | 1.63 (0.83–3.21) | 0.89 (0.68–1.15) | 1.88 (1.18–2.99) |
| ADL Impair | 2.65 (2.29–3.06) | 2.29 (1.28–4.10) | 1.44 (0.23–8.92) | 1.50 (0.97–2.33) | 0.28 (0.15–0.52) | 0.85 (0.63–1.16) | 1.05 (0.54–2.05) | 1.70 (1.23–2.34) | 1.34 (0.47–3.83) |
Multivariate, five-state Markov model adjusted for age, gender, education, race/ethnicity, 2 or more comorbidities (heart attack, stroke, cancer, hip fracture, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, depression, and anxiety), marital status and probable dementia. Hazard ratios (HRs) and corresponding 95% CIs are presented. Significant HR are bolded. HB= homebound; SHB= semi-homebound; I = independent; D= death; NH= nursing home
Older age (HR: 1.72 [1.53, 1.94]), >=2 comorbidities (HR: 2.48 [2.00, 3.07]) and ADL impairment (HR: 2.65 [2.29, 3.06]) were risk factors for progression from independence to semi-homebound, while higher education (HR: 0.80 [0.71, 0.91]), being non-Hispanic White (HR: 0.80 [0.71, 0.91]) and being married at baseline (HR: 0.83 [0.73, 0.94]) was protective against progression from independence to semi-homebound. Similarly, the risk of progression from independence to homebound was increased for participants of older age (HR: 2.14 [1.45, 3.17]) and with ADL (HR: 2.29 [1.28, 4.10]) but decreased for participants who had higher education (HR: 0.54, 0.36, 0.80]) or were married (HR: 0.57 [0.34, 0.96]).
While transitions to nursing home are rare among the homebound, we found that older (HR: 2.56 [1.25, 5.26]) and non-Hispanic White adults (HR: 3.24 [1.44, 7.32]) are at greater risk than younger adults or adults of other races and ethnicities. Additionally, older age (HR: 1.36 [1.07, 1.72]), non-Hispanic White race (HR: 1.42 [1.12, 1.81]), ADL impairment (HR: 1.70 [1.23, 2.34]) and being male (HR: 0.60 [0.47, 0.76] for females) were significantly associated with increased hazards of progression from homebound to death.
Transition Probabilities for Respondents with and without Dementia at Baseline
We examined differences in probabilities of transitioning between different states over shorter and longer follow-up periods (1 wave and 5 waves, respectively) for respondents with and without dementia (Figure 3). After adjusting for demographic and clinical characteristics, dementia is consistently associated with increased probabilities of next-wave transitions to death or nursing home status among the homebound and declining states among the semi-homebound (i.e., homebound status, death or nursing home). Respondents with dementia were twice as likely to transition from independence to semi-homebound status at the next wave than respondents without dementia (8.9% [7.3%, 11.2%] vs. 5.2% [4.3%, 6.3%]). Differences in transition probabilities among respondents with and without dementia diverge further as we examine transitions over a longer period. Homebound respondents with dementia have a 34.2% [25.8%, 48.1%] probability of death in 5 waves, compared to 17.4% [13.7%, 24.3%] among homebound respondents without dementia. The probabilities and 95% confidence intervals for Figure 3 are provided in Supplementary Table 4.
Figure 3: Predicted probabilities of progression from community-dwelling states.
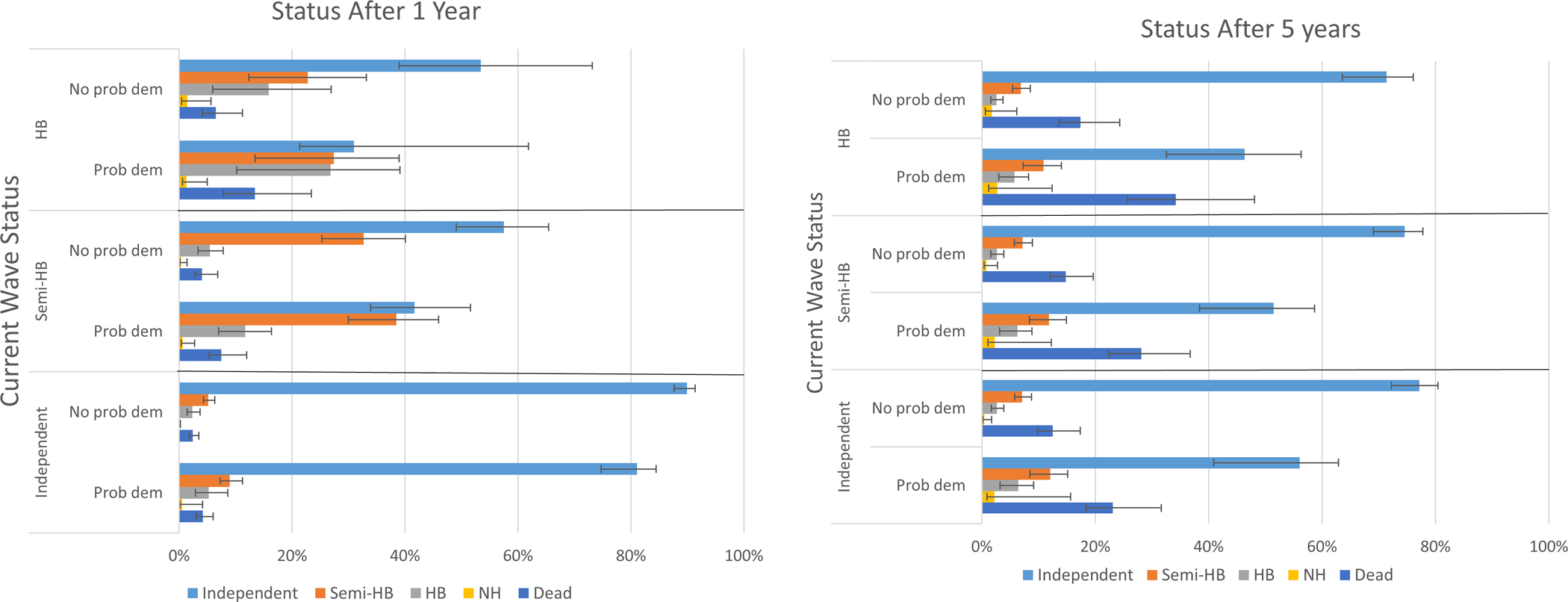
Based on multivariate five-state Markov model, for patients with and without probable dementia, for 1-year and 5-year durations.
Discussion
Using data from a prospective, nationally representative sample of older adults, we characterized the transitions between homebound states over time. To our knowledge, our study is the first to do this. A significant portion of older adults who are homebound are likely to remain homebound or die within the next year. Transitions to nursing home residence are rare among all groups, but are higher among homebound individuals than among semi-homebound or independent individuals. Moreover, we see that dementia status is associated with increased risk of decline across states including twice the likelihood of dying once homebound or even semi-homebound. We also find that social and economic factors (race and education) are associated with different probabilities of transitions across states after controlling for presence of dementia and other comorbidities.
Although homebound and semi-homebound adults are most likely to remain in their current state or decline over time, decline is not inevitable — improvement is possible from homebound status. This is the case for community dwelling older adults with and without dementia. Consistent with other research18 these results suggest that homebound status does not necessarily follow a clear declining gradient over time and reengagement with the community may be possible. Thus we need to better understand who improves over time and why, especially if factors may be modifiable.
Our results reveal that dementia is highly prevalent among those who are homebound and associated with further decline in independence or death, relative to homebound individuals without dementia. These findings demonstrate need for targeted services for people with dementia who are homebound. In particular, home-based primary care may be particularly important for patients with dementia, yet current availability remains low.29 Consistent with cultural differences regarding family support and use of nursing homes,30 we find that non-Hispanic White race is associated with a far greater risk of transitions to nursing home status than other racial/ethnic categories combined. Similarly, these findings are consistent with data that shows Black and Hispanic white adults are most likely to be homebound, especially following the onset of COVID-19.31 Our findings about education, in conjunction with our previous research on income,21 calls for greater attention to the role of socioeconomic factors as predictors of homebound status and disability among older adults. Lack of social and financial resources may not only increase vulnerability to the diseases, impairments, and disabilities that lead to becoming homebound, but may also limit ability to accommodate or overcome these disabilities. Interventions that solely target health-related risk factors will likely not prevent homebound status or additional decline for many older adults. Further work is necessary to examine the multiple pathways by which socioeconomic factors are associated with homebound status, including the role of systemic racism over the lifecourse.32
In concert with preferences to remain at home, the locus of long-term care (LTC) is shifting away from costly nursing homes to the community.33 Most individuals with dementia are able to live at home.34, 35 Although low overall, the risk of transition to long-term nursing home stay is higher among the homebound than from other groups. It is critical that we ensure that home and community-based services are designed so that people, including those with dementia, can remain safely in their homes, especially given recent concerns regarding financial viability of nursing homes during COVID.36 The development of a wide variety of community-based programs to support dementia is underway and promising.37–39 Increased availability of in-home modifications40 which have reduced functional decline and costs may be successful models for improving homebound status.
There are several limitations to this study. Although the NHATS allows us to follow a nationally-representative cohort, it surveys annually. We are therefore missing changes in homebound status between NHATS surveys, including brief episodes of being homebound such as seasonal patterns or weeks of being homebound after a musculoskeletal injury or fall. We are also unable to determine reason for homebound status. NHATS also makes use of proxy reporting (12.1% in our dataset). While we used a time-homogenous MSM model here, alternate approaches such as estimating a time-inhomogeneous MSM model could also be used, which allows for the probability of moving between states to also depend on the elapsed follow-up time.27 We examined associations among transition probabilities and dementia, other comorbidities, and sociodemographic factors, but we did not have data on dementia behaviors, disease severity, nor did we examine the role of factors such as degree of assistance from family caregiver, residence in assisted living or receipt of home care services. We also did not have comprehensive data on hospice use for all time points for the whole sample. The role of home care services and social supports in homebound transitions is left for future work. We did not use survey weights in implementing the multi-state Markov model, as software to do so is not readily available. Finally, small sample size precluded more nuanced examination of the relationship between race and homebound transitions. Despite these limitations, these data represent the most comprehensive examination to date on changes in homebound status over time among older Medicare beneficiaries.
Notably, our research allows for gradations in degree of homeboundness by considering ‘semi-homebound’ status. Not all semi-homebound individuals become homebound. In fact, we find than an individual who is semi-homebound is more likely to remain semi-homebound or become independent than become homebound at the next wave. Future work may consider alternative or more nuanced homebound gradations when considering transitions over time.
Our research demonstrates that being homebound is a far more dynamic state than previously appreciated and highlights the increased likelihood of decline in independence over time among individuals with dementia. It is critical that clinicians, health services researchers, and policy makers ensure that supportive services meet the fluctuating needs of older adults to help them remain safely and comfortably in the community for longer.
Supplementary Material
Key points:
One quarter of the homebound die within 1 year.
Homebound individuals with dementia have increased risk of transitions to death or long-stay nursing homes, compared to homebound individuals without dementia
Why does this paper matter?
First study to characterize how US older adults transition across homebound states.
Acknowledgements
Funding
The National Health and Aging Trends Study (NHATS) is sponsored by the National Institute on Aging (grant number NIA U01AG032947) and is conducted at the Johns Hopkins University. This study was supported by National Institute on Aging P30AG028741, R01AG060967 (Dr. Ornstein), K24AG062785 (Dr. Kelley), and K76AG064427 (Dr. Ankuda).
Sponsor’s Role
Funders played no role in the study’s design, analysis, and preparation of the article. This paper does not reflect the views of the U.S. Department of Veterans Affairs or the U.S. government.
Footnotes
Conflicts of Interest
No conflicts of interest to report
Supplementary material
REFERENCES
- 1.Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. May 7 2013;80(19):1778–83. doi: 10.1212/WNL.0b013e31828726f5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimer’s & dementia : the journal of the Alzheimer’s Association. Jan 2013;9(1):63–75. e2. doi: 10.1016/j.jalz.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 3.Langa KM, Larson EB, Crimmins EM, et al. A Comparison of the Prevalence of Dementia in the United States in 2000 and 2012. JAMA internal medicine. Jan 1 2017;177(1):51–58. doi: 10.1001/jamainternmed.2016.6807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ornstein KA, Leff B, Covinsky KE, et al. Epidemiology of the Homebound Population in the United States. JAMA internal medicine. Jul 2015;175(7):1180–6. doi: 10.1001/jamainternmed.2015.1849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Long-Term Care Providers and Services Users in the United States: Data From the National Study of Long-Term Care Providers, 2013–2014 (Centers for Disease Control; ) (2016). [PubMed] [Google Scholar]
- 6.Services DoHaH, ed. Nursing Home Data Compendium. 2015 edition ed. CMS; 2015. Accessed 1/20/18. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/nursinghomedatacompendium_508-2015.pdf [Google Scholar]
- 7.Ornstein K, hernandez C, DeCherrie LV, Soriano T. The Mount Sinai Visiting Doctors Program: Meeting the needs of the urban homebound population. Journal of Long Term Home Health Care. 2011;12(4):159–163. NOT IN FILE. [DOI] [PubMed] [Google Scholar]
- 8.Reckrey JM, Soriano TA, Hernandez CR, et al. The Team Approach to Home-Based Primary Care: Restructuring Care to Meet Individual, Program, and System Needs. J Am Geriatr Soc. Jan 30 2015;doi: 10.1111/jgs.13196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leff B, Carlson CM, Saliba D, Ritchie C. The invisible homebound: setting quality-of-care standards for home-based primary and palliative care. Health affairs. Jan 1 2015;34(1):21–9. doi: 10.1377/hlthaff.2014.1008 [DOI] [PubMed] [Google Scholar]
- 10.Wajnberg A, Ornstein K, Zhang M, Smith KL, Soriano T. Symptom burden in chronically ill homebound individuals. J Am Geriatr Soc. Jan 2013;61(1):126–31. doi: 10.1111/jgs.12038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kronish IM, Federman AD, Morrison RS, Boal J. Medication utilization in an urban homebound population. JGerontol A BiolSciMedSci. 2006;61(4):411–415. NOT IN FILE. [DOI] [PubMed] [Google Scholar]
- 12.Desai NR, Smith KL, Boal J. The positive financial contribution of home-based primary care programs: the case of the Mount Sinai Visiting Doctors. JAmGeriatrSoc. 2008;56(4):744–749. NOT IN FILE. [DOI] [PubMed] [Google Scholar]
- 13.Negron-Blanco L, de Pedro-Cuesta J, Almazan J, Rodriguez-Blazquez C, Franco E, Damian J. Prevalence of and factors associated with homebound status among adults in urban and rural Spanish populations. Jul 15 2016;16:574. doi: 10.1186/s12889-016-3270-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soones T, Federman A, Leff B, Siu AL, Ornstein K. Two-Year Mortality in Homebound Older Adults: An Analysis of the National Health and Aging Trends Study. J Am Geriatr Soc. Jan 2017;65(1):123–129. doi: 10.1111/jgs.14467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jacobs JM, Hammerman-Rozenberg A, Stessman J. Frequency of Leaving the House and Mortality from Age 70 to 95. J Am Geriatr Soc. Nov 22 2017;doi: 10.1111/jgs.15148 [DOI] [PubMed] [Google Scholar]
- 16.Xiang X, An R, Oh H. The Bidirectional Relationship Between Depressive Symptoms and Homebound Status Among Older Adults. The journals of gerontology Series B, Psychological sciences and social sciences. Jan 25 2018;doi: 10.1093/geronb/gbx180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szanton SL, Roberts L, Leff B, et al. Home but still engaged: participation in social activities among the homebound. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. Aug 2016;25(8):1913–20. doi: 10.1007/s11136-016-1245-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ankuda CK, Husain M, Bollens-Lund E, et al. The dynamics of being homebound over time: A prospective study of Medicare beneficiaries, 2012–2018. J Am Geriatr Soc. Mar 8 2021;doi: 10.1111/jgs.17086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ouslander JG, Grabowski DC. COVID-19 in Nursing Homes: Calming the Perfect Storm. J Am Geriatr Soc. Oct 2020;68(10):2153–2162. doi: 10.1111/jgs.16784 [DOI] [PubMed] [Google Scholar]
- 20.Freedman VA, Kasper JD. Cohort Profile: The National Health and Aging Trends Study (NHATS). Int J Epidemiol. Aug 1 2019;48(4):1044–1045g. doi: 10.1093/ije/dyz109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ornstein KA, Garrido MM, Bollens-Lund E, et al. The Association Between Income and Incident Homebound Status Among Older Medicare Beneficiaries. Journal of the American Geriatrics Society. Aug 10 2020;doi: 10.1111/jgs.16715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Medicare.gov: home health services. CMS. Accessed 3/17/21, 2021. https://www.medicare.gov/coverage/home-health-services [Google Scholar]
- 23.Ornstein KA, Garrido MM, Bollens-Lund E, et al. Estimation of the Incident Homebound Population in the US Among Older Medicare Beneficiaries, 2012 to 2018. JAMA internal medicine. Jul 1 2020;180(7):1022–1025. doi: 10.1001/jamainternmed.2020.1636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tucher EL, Keeney T, Cohen AJ, Thomas KS. Conceptualizing Food Insecurity Among Older Adults: Development of a Summary Indicator in the National Health and Aging Trends Study. The journals of gerontology Series B, Psychological sciences and social sciences. Oct 1 2020;doi: 10.1093/geronb/gbaa147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kasper JD, Freedman VA, Spillman B. Classification of Persons by Dementia Status in the National Health and Aging Trends Study. Technical Paper #5. 2013. May be accessed at www.nhats.org
- 26.Abner EL, Charnigo RJ, Kryscio RJ. Markov chains and semi-Markov models in time-to-event analysis. J Biom Biostat. 2013;Suppl 1(e001):19522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jackson C Multi-state models for panel data: The msm package for R. Journal of Statistical Software. 2011;38(8):1–28. doi: 10.18637/jss.v038.i08 [DOI] [Google Scholar]
- 28.markovchain: Easy handling discrete time Markov chains. R CRAN; 2021. https://cran.r-project.org/web/packages/markovchain/index.html [Google Scholar]
- 29.Reckrey JM, Yang M, Kinosian B, et al. Receipt Of Home-Based Medical Care Among Older Beneficiaries Enrolled In Fee-For-Service Medicare. Health Aff (Millwood). Aug 2020;39(8):1289–1296. doi: 10.1377/hlthaff.2019.01537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomeer MB, Mudrazija S, Angel JL. How do race and Hispanic ethnicity affect nursing home admission? Evidence from the Health and Retirement Study. The journals of gerontology Series B, Psychological sciences and social sciences. Jul 2015;70(4):628–38. doi: 10.1093/geronb/gbu114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ankuda CK, Leff B, Ritchie CS, Siu AL, Ornstein KA. Association of the COVID-19 Pandemic With the Prevalence of Homebound Older Adults in the United States, 2011–2020. JAMA internal medicine. 2021;doi: 10.1001/jamainternmed.2021.4456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kawachi I, Kennedy BP. Income inequality and health: pathways and mechanisms. Health Serv Res. Apr 1999;34(1 Pt 2):215–27. [PMC free article] [PubMed] [Google Scholar]
- 33.Eiken S, Burwell B, Sredl K. An examination of the woodwork effect using national medicaid long-term services and supports data. Journal of aging & social policy. 2013;25(2):134–45. doi: 10.1080/08959420.2013.766054 [DOI] [PubMed] [Google Scholar]
- 34.Wolff JL, Kasper JD, Shore AD. Long-term care preferences among older adults: a moving target? Journal of aging & social policy. 2008;20(2):182–200. [DOI] [PubMed] [Google Scholar]
- 35.Gillsjo C, Schwartz-Barcott D, von Post I. Home: the place the older adult cannot imagine living without. BMC geriatrics. Mar 17 2011;11:10. doi: 10.1186/1471-2318-11-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kilgore ML, Grabowski DC, Morrisey MA, Ritchie CS, Yun H, Locher JL. The effects of the Balanced Budget Act of 1997 on home health and hospice in older adult cancer patients. Med Care. Mar 2009;47(3):279–85. doi: 10.1097/MLR.0b013e3181893c77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaye HS. Toward a model long-term services and supports system: state policy elements. Gerontologist. Oct 2014;54(5):754–61. doi: 10.1093/geront/gnu013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kaye HS, Harrington C, LaPlante MP. Long-term care: who gets it, who provides it, who pays, and how much? Health affairs. Jan-Feb 2010;29(1):11–21. doi: 10.1377/hlthaff.2009.0535 [DOI] [PubMed] [Google Scholar]
- 39.Lustbader D, Mudra M, Romano C, et al. The Impact of a Home-Based Palliative Care Program in an Accountable Care Organization. Journal of palliative medicine. Aug 30 2016;doi: 10.1089/jpm.2016.0265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Szanton SL, Xue QL, Leff B, et al. Effect of a Biobehavioral Environmental Approach on Disability Among Low-Income Older Adults: A Randomized Clinical Trial. JAMA internal medicine. Jan 7 2019;doi: 10.1001/jamainternmed.2018.6026 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


