Abstract
Background:
Resident-to-resident elder mistreatment (RREM) in nursing homes has serious physical and psychological consequences, but factors related to RREM occurrence remain unclear. This study identifies individual and environmental characteristics associated with involvement in RREM episodes.
Methods:
The design was an observational study carried out in five urban and five suburban New York state nursing homes randomly selected on the basis of size and location. The sample consisted of 2011 residents in 10 facilities; 83% of facilities and 84% of eligible residents participated. RREM and potential correlates were identified through resident interviews, staff interviews, shift coupons, observation, chart review, and accident or incident reports.
Results:
A multivariate analysis controlling for relevant covariates found that individuals involved in RREM incidents exhibit milder dementia, show behavioral symptoms, and are less functionally impaired. Although special care units (SCU) for dementia have benefits for residents, one potential hazard for SCU residents is elevated risk for RREM.
Conclusions:
Interventions to prevent and intervene in RREM incidents are greatly needed. The correlates identified in this research point to the need for targeted interventions, specifically for residents with milder impairment and with behavioral symptoms and individuals in SCUs.
Keywords: behavioral symptoms, dementia, elder mistreatment, nursing home
INTRODUCTION
It is surprising fact that nursing homes, where care is provided to the most vulnerable adults in our society, are also the site of violent interactions. Research shows that physical and verbal aggression from residents toward staff is common and comprises a significant source of stress for caregiving personnel.1 Other studies have found relatively high rates of self-reported and observed verbal and physical aggression from staff to residents.2-4 Despite this interest, limited scientific attention thus far has been paid to a potentially even more prevalent and injurious behavior in nursing homes: violence and aggression among residents, termed resident-to-resident elder mistreatment (RREM).
Existing research suggests that RREM is prevalent in nursing homes.5,6 We conducted a study7 using a standardized and validated case-finding methodology expressly developed for estimating the prevalence of RREM. This study found a 1-month prevalence of all RREM types of 20%. The most common forms were verbal aggression (9%), physical aggression (5%), other RREM (5%), and sexual mistreatment (0.6%). Several exploratory studies in other countries, including Norway,2 Portugal,8 and Australia9 show that RREM is likely a prevalent global phenomenon. RREM also has been found in one study to occur often in assisted living facilities.10
The prevalence is concerning, because research and clinical accounts have documented the adverse consequences of RREM. RREM has been linked to physical injury and mortality11-14 among long-term care residents. Negative effects on residents' psychological well-being have also been noted.15 Staff feel unprepared to intervene in RREM incidents, with resulting contributions to job stress and burnout.16 Residents’ experience of RREM has been found to cause anxiety and distress among their family members.17 In sum, the prevalence and serious consequences of RREM demand attention to prevent and treat the problem.
Intervention attempts are hampered by the lack of high-quality studies and reliable research findings on factors that predispose nursing home residents to become involved in RREM incidents.18 In an earlier article on the prevalence of RREM using this data set, we examined in an exploratory fashion whether several subgroups exhibited higher rates of RREM. Certain characteristics of nursing home subpopulations (in particular lower levels of cognitive impairment, residing on a dementia unit, and higher nurse assistant caseload) were associated with higher estimated rates of RREM. The specific aim of this article is to advance understanding of factors associated with RREM by moving beyond this simple bivariate approach, as well as exploring additional explanatory variables. This aim is important, because successful prevention programs require the identification of high-risk scenarios for RREM to which interventions can be targeted.18,19
We use data from an observational prevalence cohort study of RREM in nursing homes using a novel methodology specifically developed to identify RREM comprehensively. This study aimed to improve research on RREM by including data from resident and staff surveys, records review, and direct observation of RREM as it occurred. Given the prevalence rates established in the earlier analysis of these data noted above, understanding factors that may place an individual at risk of RREM is a high priority.
Conceptual framework for risk factors for RREM
This study is based in the social-ecological model, which has become increasingly prominent in social science and public health research.20 As we have articulated in prior work, the social-ecological approach emphasizes connections between human interactions and the larger physical and sociocultural environment.5 The social-ecological framework views nursing homes as contingent environments, in which the behavior of an individual resident is difficult to separate from the other actors in the setting. Furthermore, individual resident behaviors are contingent on the long-term care facility environment. Instead of attributing behavior to one personal or environmental factor, the social-ecological framework includes influences at multiple levels.5 Current knowledge regarding RREM suggests that multiple factors should be included when considering possible predictors. Following this framework, we examine two sets of potential risk factors: resident-level factors and environmental factors.
Resident-level factors
Cognition and behavioral symptoms.
Research suggests that cognitively impaired individuals are at greater risk of RREM.7,14,21 Specifically, the agitated and aggressive behaviors that often accompany dementia increase the risk of RREM in the nursing home setting. Multiple patients with dementia and related behavioral problems are often congregated, in particular in special care units (SCU) for dementia. This concentration creates frequent opportunities for cognitively impaired individuals to become involved in RREM incidents. Residents with dementia may injure other residents because of their behaviors, but they may also place themselves “in harm’s way” as their behaviors can be provocative to other residents (e.g., wandering, yelling, and rummaging through others’ belongings).
We further expected that residents with mild to moderate dementia will be at greater risk than persons with severe dementia. In later stages of dementia, individuals become so impaired that they are unlikely to be aggressive or to provoke aggression.7 We therefore posit that individuals involved in RREM will be less cognitively impaired than those who are not involved.
Communication.
Communication difficulties affecting residents may increase their likelihood of being involved in RREM22: Aggression and violence may ensue when residents are unable to communicate their own needs or desires or when they are unable to understand the boundaries and preferences of other residents. This pattern can entail conflicts over seating, the TV volume, or heat and light settings13; invasions of personal space, private rooms, and property7,14,23,24; and an inability to consent to or reject sexual advances.17 Therefore, we expect that communication difficulties will be positively associated with involvement in RREM.
Functional status.
Research on agitated behaviors among residents suggests a positive relationship between such behaviors and functional impairment or dependency.14,22,23,25 However, based on the nature of RREM, we propose that individuals who are less functionally impaired will be more likely to be involved in RREM incidents,7,22 because residents are most at risk if they are ambulatory and able to move into negative interactions with other residents.
Hearing and Vision.
Problems with sight and hearing could lead residents into unwanted physical contact with one another, as well as an inability to escape aggressive approaches by other residents.
Depression.
A growing number of studies have found that depression is a risk factor for aggressive actions by residents.26,27 We posit a similar relationship for RREM incidents.
Gender.
Studies show that male residents are more likely to be aggressive.11-13,21 We therefore expect that male residents will be more likely to be involved in RREM incidents.
Race.
Lachs and colleagues1 examined aggression by residents toward staff and found that African Americans were less likely to engage in these behaviors. They proposed as a possible explanation that the majority of certified nursing assistants (CNAs) in the study were from minority backgrounds. This finding may reflect a lower likelihood of aggression when the CNA–resident dyad is concordant (i.e., a resident is less likely to engage in aggression toward a staff member of the same background). Further, research has found lower rates of expression of anger by African Americans, especially among older individuals who feel less “anger privilege” and are more likely to be sanctioned when expressing anger.28 Instances of RREM may be rarer among these residents because African Americans, especially older individuals,29,30 may more often suppress feelings of anger.31-33
Age.
We expect that age will be negatively related to RREM.7,11,12 This pattern may occur because of the potential presence of younger mentally ill residents in nursing homes,34 as well as the greater likelihood that younger people are more able to move about the facility and thereby become at greater risk of RREM.
Environmental factors
Living in a SCU.
We expect that residence in a SCU will increase risk of RREM, because residents with dementia and related behavioral problems are closely congregated, creating constant contact with other potentially high-risk individuals.2,7,14,25 SCUs in this study were defined following Holmes and Teresi as “a unit that has, as residents, a majority with dementia, and is physically separated from other units, and that, in addition, displays any one of the following characteristics: self-definition as an SCU, availability of special activities and/or programming for dementia patients, or special training for staff.”35
Staffing.
We anticipated that units in which CNAs cared for fewer residents would have lower RREM rates, as staff would be more available to prevent or intervene in RREM.7,17
METHODS
Description of the study
Facility selection
Twelve nursing homes in New York state were selected at random by using a pseudo-random number generator procedure; 6 were selected from among the 21 nursing homes with 250 or more beds in an urban region, and 6 from among the 13 large nursing homes (200 or more beds) in a suburban region. Ten of the 12 facilities agreed, yielding a participation rate of 83%.7 Eighty percent of the facilities were nonprofit and 20% were proprietary; 70% of the facilities had SCUs. Of the resident sample, 16 percent lived in a SCU. As shown in Table 1, the resident populations of the facilities had a relatively large proportion of minority group residents relative to nursing homes nationally (18% African American and 15% Hispanic). The study was approved by the Weill Cornell Medicine and Cornell University Institutional Review Boards (IRB).
TABLE 1.
Demographics and resident characteristics for the total sample and by determination of RREM status during the 1-month prevalence period (N = 2011)
| Total (N =2011) |
No (n = 1604) |
Yes (n = 407) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | M/(%) | SD | N | M/(%) | SD | N | M/(%) | SD | p | |
| Demographics | ||||||||||
| Age (years) | 2011 | 84.1 | (10.4) | 1604 | 84.5 | (10.3) | 407 | 82.9 | (10.8) | 0.007 |
| Education (years) | 1648 | 12.1 | (3.8) | 1288 | 12.0 | (3.9) | 360 | 12.4 | (3.5) | 0.061 |
| Female, n (%) | 1458 | (72.5) | 1174 | (73.2) | 284 | (69.8) | 0.172 | |||
| White, n (%) | 1367 | (68.0) | 1063 | (66.3) | 304 | (74.7) | 0.001 | |||
| African American, n (%) | 367 | (18.2) | 321 | (20.0) | 46 | (11.3) | <0.001 | |||
| Hispanic, n (%) | 297 | (14.8) | 231 | (14.4) | 66 | (16.2) | 0.361 | |||
| Married, n (%) | 252 | (12.9) | 201 | (12.9) | 51 | (13.0) | 0.951 | |||
| Never married, n (%) | 318 | (16.3) | 254 | (16.3) | 64 | (16.4) | 0.987 | |||
| State: suburban, n (%) | 549 | (27.3) | 451 | (28.1) | 98 | (24.1) | 0.099 | |||
| State: urban, n (%) | 1462 | (72.7) | 1153 | (71.9) | 309 | (75.9) | ||||
| Environment | ||||||||||
| SCU: no, n (%) | 1683 | (83.7) | 1371 | (85.5) | 312 | (76.7) | <0.001 | |||
| SCU: yes, n (%) | 328 | (16.3) | 233 | (14.5) | 95 | (23.3) | ||||
| Residents assigned to CNA | 2011 | 8.2 | (2.6) | 1604 | 8.1 | (2.5) | 407 | 8.7 | (2.9) | <0.001 |
| Resident characteristics | ||||||||||
| Depression (FTQ response) | 1576 | 8.4 | (6.3) | 1221 | 8.1 | (6.1) | 355 | 9.6 | (6.8) | <0.001 |
| Cognitive impairment (CAREDIAG) | 1973 | 7.7 | (4.8) | 1571 | 8.1 | (4.9) | 402 | 6.3 | (4.2) | <0.001 |
| Functional impairment (PADL total) | 1734 | 11.5 | (14.0) | 1373 | 12.6 | (14.3) | 361 | 7.6 | (12.2) | <0.001 |
| Behavioral symptoms (Barrett Behavior Index) | 1966 | 9.0 | (7.5) | 1565 | 8.2 | (6.9) | 401 | 12.2 | (8.8) | <0.001 |
| Expressive communication scale | 1718 | 0.4 | (0.8) | 1344 | 0.4 | (0.8) | 374 | 0.3 | (0.6) | <0.001 |
| Receptive communication scale | 1664 | 0.2 | (0.4) | 1293 | 0.2 | (0.4) | 371 | 0.2 | (0.4) | 0.424 |
| Speech communication scale | 1725 | 0.5 | (1.0) | 1349 | 0.6 | (1.0) | 376 | 0.3 | (0.7) | <0.001 |
| Total communication scale | 1721 | 1.2 | (1.9) | 1346 | 1.2 | (2.0) | 375 | 0.8 | (1.5) | <0.001 |
| Global rating of vision | 1313 | 0.9 | (1.1) | 994 | 0.9 | (1.1) | 319 | 0.9 | (1.1) | 0.371 |
| Global rating of hearing | 1596 | 0.6 | (0.8) | 1231 | 0.6 | (0.8) | 365 | 0.6 | (0.9) | 0.857 |
Note: CNA = certified nursing assistant; FTQ = Feeling Tone Questionnaire, CAREDIAG = Comprehensive Assessment and Referral Evaluation Diagnostic Cognitive Disorder Scale; PADL = Performance Activities of Daily Living. All scales and indices are in the disordered or impaired direction, with higher scores indicative of more disorder or impairment. Comparisons conducted by t-tests for continuous variables and likelihood ratio χ2 tests for binary and categorical variables.
Exclusion/inclusion criteria
All long-stay residents except those on hospice care were invited to participate. For residents who were unable to complete the consent process (due to, e.g., cognitive impairment, language barrier, health impairment), consent was sought by designated proxies (families or legal guardians). Residents unable to respond (due to language other than English or Spanish, or impairment) were excluded from resident level measures; chart review, staff informant, and observational measures were performed on those whose families provided proxy consent.
Response rate
Excluding residents who were not available, expired, or were discharged prior to enrollment in the denominator; the overall response rate was 86.5% (1462 enrolled/1691 eligible) for the urban sample and 78.2% (549 enrolled/702 eligible) for the suburban sample. There were a total of 334 resident and family refusals (201 urban; 133 suburban). Letters requesting proxy consent were sent to 483 (400 urban; 83 suburban) key contacts (usually family members) for residents who were unable for provide consent. There were 34 refusals (8.5%) in the urban sample and 5 (6%) in the suburban sample. There were 1024 (50.9%) eligible for the extended self-report RREM interview based on their performance on a cognitive screen, and 962 (962 completed/1024 eligible = 93.95%) completed some (n = 14) or all (n = 948) of the RREM interview.
Assessment of RREM
RREM status was operationalized in this research as negative and aggressive physical, sexual, or verbal interactions between two or more long-term care residents that in a community setting would likely be construed as unwelcome and have high potential to cause physical or psychological distress in the recipient. It is often difficult to determine a “perpetrator” and “victim” in RREM, given problems in determining intent among residents with dementia and the fact that many incidents appear to have mutual involvement.5 Therefore, positive cases were individuals involved in an incident of RREM, regardless of which resident may have incited it.
RREM status was assessed using multiple methodologies: (1) structured interviews with residents and staff that asked about 22 forms of physical, verbal, or sexual events in a one-month period and also during the past year; (2) shift reporting coupons completed by staff upon observation of an event, (3) direct observation by research staff members, (4) chart review, and (5) review of incident or accident reports. Data were collected between July 2009 and June 2013. A classification of RREM status was made through an exhaustive adjudication process that included expert review of multiple sources of data and case conferencing. Full details on the adjudication process are available elsewhere.7 The analyses were performed using both the 1-month prevalence estimates of RREM as well as the annual prevalence estimates.
Measures of resident-level factors
Cognition
The main cognitive screening measure used in this study is part of the INCARE, the Care CAREDIAG (Comprehensive Assessment and Referral Evaluation Diagnostic Cognitive Disorder Scale), an interviewer-administered questionnaire for residents.36,37 Note that the CAREDIAG has been studied using several advanced psychometric models, including analyses of its relationship to dementia diagnosis.38 This scale was used to assess cognitive status because it has been found to be more culturally fair than others.39,40 The Cronbach’s alpha coefficient estimate for this sample was 0.88 at baseline; it was scored in the cognitively impaired direction.
Behavioral symptoms
The Nurse/CNA Informant Interview, which includes the short version of the Barrett Behavior Index,41 was used. The short version (31 items), adapted for CNAs, was used by staff to rate resident’s behavior. Typical items include “Wanders during the day”; “Repetitive questioning”; “Argumentative”; “Demanding”; and “Disrupts other’s activities.” Items are rated in terms of frequency of occurrence: “Not at all”; “Sometimes (1–4 times per week)”; and “Often (5+ times per week).” In an urban nursing home sample, the Cronbach’s alpha estimate was in the 0.80s, and in the 0.60s in a rural nursing home sample.41,42 This scale had a Cronbach’s alpha estimate of 0.87 for this sample at baseline.
Communication
Communication was measured by the research assistants’ ratings of specific items based on their observation of the respondent during the interview. These items are a part of the INCARE assessment instrument. Types of communication rated were expressive (5 items), receptive (4 items), and speech (6 items). A total communication score was created using all of the items.37 All items were rated on whether or not the condition was present. Ordinal alpha estimates for this sample were 0.77 for expressive communication, 0.70 for receptive, 0.79 for speech, and 0.89 for total communication; the scales and subscales were scored in the impaired direction. Due to collinearity, the speech scale was retained in the multivariate analyses.
Functional status
The performance activities of daily living (PADL)43 (Cronbach’s alpha estimate typically in the 0.90s)44 is a 27-item scale that measures an individual’s lack of ability to perform certain activities of daily living independently. This scale was scored in the functionally impaired direction. Respondents are assessed for their ability to perform various upper and lower body movement tasks associated with eating, dressing and grooming, such as putting on a sweater, buttoning and unbuttoning a sweater, guiding a spoon to the mouth, combing hair. Performance times are recorded, and items are rated as to whether the task was performed with or without cueing, or could not be performed at all. The Cronbach’s alpha estimate coefficient for this sample was 0.94 at baseline.
Depression
The feeling tone questionnaire (FTQ) was developed for use in a cross-national study of institutionalized persons. The measure contains 16 questions asked directly of the resident. Typical items are “Are you feeling well?”; “Are you feeling happy today?”; “Do you feel lonely?” Each item is coded “yes,” “no,” or “equivocal (sometimes, it depends),” and affect was rated using a 5-point continuum from 1—“laughs, praises, enthusiastic, emphatically positive” to 5—“extreme negative—cries, groans, curses, is emphatically negative.” Three scales are scored: response, affect, and total. The FTQ has been used among numerous samples of nursing home residents, in which reliabilities were in the 0.90s.45 The FTQ response scale Cronbach’s alpha estimate at baseline for this sample was 0.79. The measure, used in the multivariate analyses, was scored in the direction of negative affect.
Hearing and vision
Hearing and vision were assessed by the research assistants’ global ratings, based on their observation of the respondent during the interview. These items are a part of the INCARE.
Measures for environmental factors
Living in special care unit
The resident lived in a SCU designated by the facility as dedicated to those with cognitive impairment (usually Alzheimer’s disease). The intent of these units was to provide specialized care for those with cognitive and often behavioral disorders
Staffing
Staffing levels were measured directly by counting the number of residents assigned to each CNA. A list of assigned residents for all daytime shift CNAs was obtained from each facility. We were thus able to count the number of residents for which each CNA interviewed was providing care. The staffing data were collected primarily from CNAs working during the week on the day shift. This approach is reasonable, given that RREM is much more likely when residents are active in the nursing home.
Statistical procedures
SPSS 2746 was used to conduct analyses. Bivariate analyses were conducted to examine the association of study variables with the RREM classification, using t tests for continuous variables and likelihood ratio χ2 tests for binary variables. The Complex Samples Logistic Regression procedure was used for the multivariate analyses adjusting for clustering within unit and CNA. The EM algorithm was used to model missing data. Selection of covariates was based on theoretical and statistical significance at the bivariate level. Collinearity diagnostics were performed, and variables were excluded from the final model either because of collinearity or nonsignificance at the bivariate level. Robustness of the model was tested by alternatively removing and including variables with collinearity. Not all of the communication variables could be entered into the model at once because of collinearity. The scales were entered individually into the model. Sensitivity analysis was performed including vision and hearing variables in the model.
RESULTS
Sample
The mean age of participants was 84 years (SD = 10.4); most were female (72.5%), and White (68%), with a mean education of 12 years (SD = 3.8). Four-hundred and seven participants (20%) had been involved in an RREM incident during the one-month prevalence period and 507 (25.2%) during the annual period (see Table 1).
Multivariate analysis
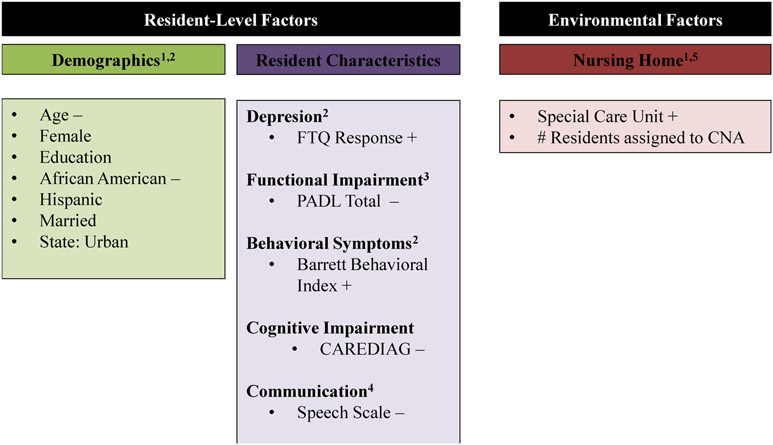
The significant correlates based on a logistic regression predicting RREM (involvement) during the 1-month prevalence period were age (estimate = −0.02; p = 0.014); depression (FTQ response, estimate = 0.03; p = 0.006), behavioral symptoms (Barrett Behavior Index, estimate = 0.07, p < 0.001), race (African American) (estimate = −0.45, p = 0.018); cognitive impairment (CAREDIAG, estimate = −0.07, p < 0.001), functional impairment (PADL total, estimate = −0.02, p = 0.009), residence in SCUs (estimate = 0.56, p = 0.002), and the speech communication scale (estimate = −0.16, p = 0.037). Figure 1 includes the findings from the multivariate analysis
FIGURE 1.
Factors considered in association with RREM involvement.
1 = facility records, 2 = resident, 3 = staff, 4 = research assistant observation, 5 = TESS-NH
Individuals involved in RREM were significantly: younger, had higher levels of depression, exhibited more behavioral symptoms, were less likely to be African American, had lower levels of cognitive impairment, and lower levels of functional impairment. Additionally, residents engaging in RREM were more likely to reside in SCUs. Staffing level approached significance at the multivariate level; the greater the number of residents assigned to a CNA (indicative of lower front-line staffing), the greater the rate of RREM (estimate = 0.05, p = 0.074) (see Table 2).
TABLE 2.
Logistic regression prediction RREM determination status for the total sample (N = 2011)
| One-month prevalence (n = 407) |
Annual prevalence (n = 503) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI for EXP(B) |
95% CI for EXP(B) |
|||||||||||
| Variable | Estimate | SE | p | Exp. (estimate) | Lower | Upper | Estimate | SE | p | Exp. (estimate) | Lower | Upper |
| Intercept | −0.94 | 0.51 | 0.065 | 0.389 | 0.14 | 1.06 | −0.36 | 0.47 | 0.435 | 0.695 | 0.28 | 1.74 |
| # Residents assigned to CNA | 0.05 | 0.03 | 0.074 | 1.047 | 1.00 | 1.10 | 0.06 | 0.03 | 0.028 | 1.060 | 1.01 | 1.12 |
| Urban | 0.22 | 0.15 | 0.158 | 1.242 | 0.92 | 1.68 | −0.14 | 0.15 | 0.354 | 0.867 | 0.64 | 1.17 |
| SCU | 0.56 | 0.18 | 0.002 | 1.742 | 1.23 | 2.47 | 0.63 | 0.18 | <0.001 | 1.876 | 1.31 | 2.69 |
| Age | −0.02 | 0.01 | 0.014 | 0.986 | 0.97 | 1.00 | −0.02 | 0.01 | 0.003 | 0.984 | 0.97 | 1.00 |
| Female | −0.04 | 0.14 | 0.748 | 0.957 | 0.73 | 1.25 | −0.03 | 0.14 | 0.805 | 0.967 | 0.74 | 1.27 |
| African American | −0.45 | 0.19 | 0.018 | 0.641 | 0.44 | 0.93 | −0.32 | 0.17 | 0.062 | 0.725 | 0.52 | 1.02 |
| Hispanic | 0.09 | 0.18 | 0.618 | 1.092 | 0.77 | 1.54 | 0.04 | 0.17 | 0.796 | 1.045 | 0.75 | 1.46 |
| Married | 0.08 | 0.19 | 0.690 | 1.080 | 0.74 | 1.58 | −0.03 | 0.18 | 0.859 | 0.968 | 0.68 | 1.38 |
| Depression (FTQ response) | 0.03 | 0.01 | 0.006 | 1.028 | 1.01 | 1.05 | 0.03 | 0.01 | 0.005 | 1.027 | 1.01 | 1.05 |
| Cognitive impairment (CAREDIAG) | −0.07 | 0.02 | <0.001 | 0.932 | 0.90 | 0.97 | −0.07 | 0.02 | <0.001 | 0.937 | 0.91 | 0.97 |
| Functional impairment (PADL total) | −0.02 | 0.01 | 0.009 | 0.985 | 0.97 | 1.00 | −0.02 | 0.01 | 0.005 | 0.985 | 0.97 | 1.00 |
| Behavioral symptoms (Barrett Behavior Index) | 0.07 | 0.01 | <0.001 | 1.074 | 1.06 | 1.09 | 0.07 | 0.01 | <0.001 | 1.067 | 1.05 | 1.08 |
| Speech communication scale | −0.16 | 0.08 | 0.037 | 0.854 | 0.74 | 0.99 | −0.12 | 0.07 | 0.075 | 0.889 | 0.78 | 1.01 |
Note: All scales and indices are in the disordered or impaired direction. SPSS 27 Complex Samples Logistic Regression used in all analyses adjusting for clustering within unit and CNA. CNA = certified nursing assistant, FTQ = Feeling Tone uestionnaire, CAREDIAG = Comprehensive Assessment and Referral Evaluation Diagnostic Cognitive Disorder Scale, PADL = Performance Activities of Daily Living.
Results for the annual prevalence period were consistent with the 1-month period with a few exceptions. The number of residents assigned to each CNA was not significant for the 1-month prevalence but is significant for the annual prevalence (p = 0.074 and p = 0.028, respectively). Being African American was significant for the 1-month prevalence but is not significant for the annual prevalence (p = 0.018 and p = 0.062, respectively). Speech was significant for the one-month prevalence but is not significant for the annual prevalence (p = 0.037 and p = 0.075, respectively) (see Table 2). In sensitivity analysis, the inclusion of vision and hearing yielded consistent results with the 1-month analysis. The vision and hearing variables contained a fair amount of missing data and were not significant.
DISCUSSION
The present study provides a detailed profile of etiological factors for RREM in nursing homes. Confirming some earlier research, and conforming with expected relationships, the characteristics of individuals involved in RREM are those who exhibit milder dementia, show behavioral symptoms, and have a lower level of functional impairment. This profile is consistent with clinical impressions of RREM, given that some of its manifestations necessarily involve physical ability, such as wandering or engaging in physical aggression. Conversely, the research found that certain factors appear to protect against RREM involvement, in particular high levels of physical and cognitive impairment. Further, SCU residence is associated with elevated risk for RREM at the individual level. It is possible that such elevated risk may be mitigated at the facility level by reduced risk for other residents not in the SCU. Future research could examine whether concentration of RREM-prone individuals in an SCU serves as a protective factor for other residents.
This study has several limitations that point to directions for future research. First, the data are cross-sectional; thus, inferences are limited. However, we examined both monthly and annual prevalence periods and found similar results in terms of the associations of variables with RREM. Second, we are unable to analyze differences between individuals involved in a single versus multiple RREM incidents. Clinical accounts47 suggest that some individuals may be involved disproportionately in multiple RREM incidents; future research should explore this potential phenomenon and its implications for intervention. Third, our social-ecological model suggests that it would be useful to study variation among nursing homes regarding RREM occurrence. Future studies should be conducted involving sufficient numbers of nursing homes to examine such variation.
The findings have implications for nursing home staff, from nurses involved in the care planning process to CNAs engaged in the direct provision of care. It is generally recommended that nursing homes “staff to acuity”; that is, allocate direct care staff based on the need for ADL assistance and requirements for skilled care. Such a strategy, however, could risk systematically relegating those residents at the highest risk for RREM to lower levels of staffing, as our study found that residents with lower levels of functional impairment and cognitive impairment are at the greatest risk. Guidelines are needed for how nursing homes should incorporate RREM risk into their staffing models, which are increasingly predicated on the need for ADL assistance. Further research on RREM is also required to refine the profile of individuals likely to become involved in RREM incidents, which can inform screening tools to identify high-risk residents on admission. Finally, evidence-based training programs for staff have rarely been developed48; designing and testing interventions to prevent RREM are a high priority.
Key points
Predictors of RREM can be identified using a systematic case-finding methodology.
Most at-risk are residents with less severe functional and cognitive impairment who exhibit behavioral symptoms.
Targeted intervention for high-risk nursing home residents is greatly needed to reduce RREM.
Why does this paper matter?
RREM causes significant preventable injury and suffering to nursing home residents and is a major source of stress to staff and family members. Interventions can be targeted based on understanding factors associated with RREM.
Funding information
This project was supported by the following grants: National Institute on Aging (R01AG057389; RO1AG014299); National Institute of Justice (FYO 42USC3721); New York State Department of Health Dementia Grant Program (contract # C-022657). Karl Pillemer acknowledges support from an Edward R. Roybal Center Grant from the National Institute on Aging (P30AG022845).
Jeanne Teresi and Mildred Ramirez were supported in part by the Columbia University Alzheimer’s Disease Resource Center for Minority Aging Research, National Institute on Aging, P30AG059303.
SPONSOR’S ROLE
The funding sources were not involved in the design or conduct of the study, its analyses, or the decision to submit the manuscript for publication.
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to report.
REFERENCES
- 1.Lachs MS, Rosen T, Teresi JA, et al. Verbal and physical aggression directed at nursing home staff by residents. J Gen Intern Med. 2013;28:660–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Botngård A, Eide AH, Mosqueda L, Blekken L, Malmedal W. Factors associated with staff- to-resident abuse in Norwegian nursing homes: a cross-sectional exploratory study. BMC Health Serv Res. 2021;21:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castle NG. Nurse aides’ reports of resident abuse in nursing homes. J Appl Gerontol. 2012a;31:402–422. [Google Scholar]
- 4.Pillemer KA, Moore DW. Abuse of patients in nursing homes: findings from a survey of staff. Gerontologist. 1989; 29:314–320. [DOI] [PubMed] [Google Scholar]
- 5.Pillemer K, Chen EK, Van Haitsma KS, et al. Resident-to-resident aggression in nursing homes: results from a qualitative event reconstruction study. Gerontologist. 2011;52:24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woolford MH, Stacpoole SJ, Clinnick L. Resident-to-resident elder mistreatment in residential aged care services: a systematic review of event frequency, type, resident characteristics, and history. J Am Med Dir Assoc. 2021;22:1678–1691.e6. [DOI] [PubMed] [Google Scholar]
- 7.Lachs MS, Teresi JA, Ramirez M, et al. The prevalence of resident-to-resident elder mistreatment in nursing homes. Ann Intern Med. 2016;165:229–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferreira J, Tavares J, Sousa L. Resident-to-resident elder mistreatment (R-REM): a study in residential structures for elderly people (ERI) in Portugal. J Elder Abuse Negl. 2019;31:66–76. [DOI] [PubMed] [Google Scholar]
- 9.Joyce CM. Prevalence and nature of resident-to-resident abuse incidents in Australian residential aged care. Australas J Ageing. 2020;39:269–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gimm G, Chowdhury S, Castle N. Resident aggression and abuse in assisted living. J Appl Gerontol. 2018;37(8):947–964. [DOI] [PubMed] [Google Scholar]
- 11.Caspi E The circumstances surrounding the death of 105 elders as a result of resident-to-resident incidents in dementia in long-term care homes. J Elder Abuse Neglect. 2018;30:284–308. [DOI] [PubMed] [Google Scholar]
- 12.Murphy B, Bugeja L, Pilgrim J, Ibrahim JE. Deaths from resident-to-resident aggression in Australian nursing homes. J Am Geriatr Soc. 2017;65:2603–2609. [DOI] [PubMed] [Google Scholar]
- 13.Rosen T, Pillemer KA, Lachs MS. Resident-to-resident aggression in long-term care facilities: an understudied problem. Aggress Violent Behav. 2008;13:77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shinoda-Tagawa T, Leonard R, Pontikas J, McDonough JE, Allen D, Dreyer PI. Resident-to-resident violent incidents in nursing homes. J Am Med Assoc. 2004;291:591–598. [DOI] [PubMed] [Google Scholar]
- 15.Trompetter H, Scholte R, Westerhof G. Resident-to-resident relational aggression and subjective well-being in assisted living facilities. Aging Ment Health. 2011;15:59–67. [DOI] [PubMed] [Google Scholar]
- 16.Rosen T, Lachs MS, Teresi J, Eimicke J, Van Haitsma K, Pillemer K. Staff-reported strategies for prevention and management of resident-to-resident elder mistreatment in long-term care facilities. J Elder Abuse Negl. 2016;28:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baumbusch J, Puurveen G, Phinne A, Beaton MD, Leblanc ME. Family members’ experiences and management of resident-to-resident abuse in long-term residential care. J Elder Abuse Neglect. 2018;20:385–401. [DOI] [PubMed] [Google Scholar]
- 18.McDonald L, Sheppard C, Hitzig SL, Spalter T, Mathur A, Mukhi JS. Resident-to-resident abuse: a scoping review. Can J Aging. 2015;34:215–236. [DOI] [PubMed] [Google Scholar]
- 19.Abner EK, Teaster PB, Mendiondo MS, et al. Victim, allegation, and investigation characteristics associated with substantiated reports of sexual abuse of adults in residential care settings. J Interpers Violence. 2019;34:3995–4019. [DOI] [PubMed] [Google Scholar]
- 20.Wold B, Mittelmark MB. Health-promotion research over three decades: the social-ecological model and challenges in implementation of interventions. Scand J Public Health. 2018;46:20–26. [DOI] [PubMed] [Google Scholar]
- 21.Voyer P, Verreault R, Azizah GM, Desrosiers J, Champoux M, Bedard A. Prevalence of physical and verbal aggressive behaviours and associated factors among older adults in long-term care facilities. BMC Geriatr. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrah N, Murphy BJ, Ibrahim JE, et al. Resident-to-resident physical aggression leading to injury in nursing homes: a systematic review. Age Ageing. 2015;44:356–364. [DOI] [PubMed] [Google Scholar]
- 23.Snellgrove S, Beck C, Green A, McSweeney JC. Resident-to-resident violence triggers in nursing homes. Clin Nurs Res. 2013;22:461–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bridges-Parlet S, Knopman D, Thompson T. A descriptive study of physically aggressive behavior in dementia by direct observation. J Am Geriatr Soc. 1994;42(2):192–197. [DOI] [PubMed] [Google Scholar]
- 25.Sloane PD, Mitchell CM, Preisser JS, Phillips C, Commander C, Burker E. Environmental correlates of resident agitation in Alzheimer’s disease special care units. J Am Geriatr Soc. 1998;46:862–869. [DOI] [PubMed] [Google Scholar]
- 26.Menon AS, Gruber-Baldini AL, Hebel JR, et al. Relationship between aggressive behaviors and depression among nursing home residents with dementia. Int J Geriatr Psychiatry. 2001;16(2):129–146. [DOI] [PubMed] [Google Scholar]
- 27.Thériault ÉR, Grant A. Depression and aggressive behaviour in continuing care: how cognitive impairment might not explain the whole story. J Long-Term Care. 2020;0:1–12. [Google Scholar]
- 28.Collins PH. Black Sexual Politics: African Americans, Gender, and the New Racism. Routledge; 2004. [DOI] [PubMed] [Google Scholar]
- 29.Magee W, Louie P. Did the difference between Black and White Americans in anger-out decrease during the first decade of the twenty-first century? Race Soc Probl. 2016;8:256–270. [Google Scholar]
- 30.Peters RM. Racism and hypertension among African Americans. West J Nurs Res. 2004;26:612–631. [DOI] [PubMed] [Google Scholar]
- 31.Mabry JB, Kiecolt KJ. Anger in Black and White: race, alienation, and anger. J Health Soc Behav. 2005;46:85–101. [DOI] [PubMed] [Google Scholar]
- 32.Magai C, Kerns MD, Gillespie M, Huang B. Anger experience and anger inhibition in sub-populations of African American and European American older adults and relation to circulatory disease. J Health Psychol. 2003;8:413–432. [DOI] [PubMed] [Google Scholar]
- 33.Wilkins A ‘Not out to start a revolution’: race, gender, and emotional restraint among Black university men. J Contemp Ethnography. 2012;41:34–65. [Google Scholar]
- 34.Jervis LL. An imperfect refuge: life in an “old folk’s home” for younger residents with psychiatric disorders. Soc Sci Med. 2002;2002(54):79–91. [DOI] [PubMed] [Google Scholar]
- 35.Holmes D, Teresi J. Characteristics of special care units in the north-east five state survey: implications of different definitional criteria. Alzheimer’s Dis Assoc Disord. 1994;8:S97–S105. [PubMed] [Google Scholar]
- 36.Gurland B, Kuriansky J, Sharpe L, Simon R, Stiller P, Birkett P. The comprehensive assessment and referral evaluation (CARE)—rationale, development and reliability. Int J Aging Hum Dev. 1977;8(1):9–42. [DOI] [PubMed] [Google Scholar]
- 37.Golden RR Teresi JA, Gurland BJ. Development of indicator scales for the comprehensive assessment and referral evaluation (CARE) interview schedule. J Gerontol. 1984;39(2):138–146. [DOI] [PubMed] [Google Scholar]
- 38.Teresi JA, Kleinman M, Ocepek-Welikson K, et al. Applications of item response theory to the examination of the psychometric properties and differential item functioning of the CARE dementia diagnostic scale among samples of Latino, African-American and White non-Latino elderly. Res Aging. 2000;22:738–773. [Google Scholar]
- 39.Ramirez M, Teresi JA, Holmes D, Gurland BJ, Lantigua R. Differential item functioning (DIF) and the mini-mental state examination (MMSE): overview, sample and issues of translation. Med Care. 2006;44:S95–S106. [DOI] [PubMed] [Google Scholar]
- 40.Teresi JA. Commentary: scaling the mini-mental state examination using item response theory. J Clin Epidemiol. 2007;60:256–259. [DOI] [PubMed] [Google Scholar]
- 41.Barrett VW. A Study of Disturbing Behavior in Mentally Impaired Elderly. Doctoral dissertation. Columbia University; 1988. [Google Scholar]
- 42.Teresi J, Holmes D, Benenson E, et al. A primary care nursing model in long-term care facilities: evaluation of impact on affect, behavior, and socialization. Gerontologist. 1993;33:667–674. [DOI] [PubMed] [Google Scholar]
- 43.Kuriansky J, Gurland B. The performance test of activities of daily living. Int J Aging Human Develop. 1976;7:343–352. [DOI] [PubMed] [Google Scholar]
- 44.Petkova E, Teresi J. Some statistical issues in the analyses of data from longitudinal, intervention studies of elderly chronic care populations. J Psychosom Res. 2002;64:531–547. [DOI] [PubMed] [Google Scholar]
- 45.Teresi JA, Ocepek-Welikson K, Toner JA, et al. Methodological issues in measuring subjective well-being and quality-of-life: applications to assessment of affect in older, chronically and cognitively impaired, ethnically diverse groups using the feeling tone questionnaire. Appl Res Qual Life. 2017;12:251–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.IBM Corp. IBM SPSS Statistics for Windows, Version 27.0. IBM Corp; 2020. [Google Scholar]
- 47.Resnick B, Galik E, McPherson R, Boltz M, Van Haitsma K, Kolanowski A. Gender differences in disease, function, and behavioral symptoms in residents with dementia. West J Nurs Res. 2021; [Epub before print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Teresi JA, Ramirez M, Ellis J, et al. A staff intervention targeting resident-to-resident elder mistreatment (R-REM) in long-term care increased staff knowledge, recognition and reporting: results from a cluster randomized trial. Int J Nurs Stud. 2013;50:644–656. [DOI] [PMC free article] [PubMed] [Google Scholar]