Abstract
Background.
Growing literature supports the hypothesis that personality influences health outcomes. Few studies have examined the association between personality traits and key clinical manifestations in persons with multiple sclerosis (pwMS).
Objective.
To investigate whether personality traits are associated with physical function, cognition, and depression in persons with MS.
Methods.
In this cross-sectional study, we analyzed data from two cohorts (UPMC, n=365 and CUIMC, n=129). Participants completed a personality scale (assessing neuroticism, extraversion, openness, agreeableness, and conscientiousness) and validated surveys measuring physical function, cognition, and depression. Stepwise linear regressions were used to evaluate associations between personality traits and outcome measures.
Results.
Consistently across cohorts, higher extraversion was associated with better physical function, whereas higher neuroticism was associated with worse depression. In the first cohort, higher extraversion was associated with better cognition, while higher neuroticism was associated with greater risk for memory impairment in the second cohort. Relationships were independent of age and disease duration.
Conclusion.
Findings suggest a potentially protective role of extraversion, and a harmful role of neuroticism, in MS-specific patient-reported clinical outcomes. Increased understanding of the interplay between personality and health outcomes may inform risk models for physical decline, cognitive impairment, and depression in pwMS.
Keywords: multiple sclerosis, personality traits, physical function, cognition, mood
Introduction
Multiple sclerosis (MS) is a chronic neurological disease characterized by decline in physical and cognitive function and heightened risk for mood disorders. Approximately 80% of people with MS (pwMS) experience sensorimotor impairments of the upper and lower limbs,1 60% experience cognitive dysfunctions,2 and lifetime prevalence estimates of depression approach 30%.3 In addition to disease-modifying therapy (DMT), several protective factors could mitigate the deleterious effects of neurological damage on clinical manifestations in pwMS. Physical activity,4 healthy diet,5 and social support,6,7 for instance, are known to influence disease course and symptom burden. Another potential factor is personality, distilled into five measurable traits (i.e., ‘the Big Five’): neuroticism, extraversion, openness, agreeableness, and conscientiousness.8
In pwMS, low neuroticism, high extraversion, and high conscientiousness are shown to be associated with less depression and anxiety9 as well as lower levels of physical disability.10 Further, high openness and low neuroticism were identified as protective traits for memory function.11 In previous studies, however, sample sizes were small (rarely exceeding 100 participants) and comprehensive assessments of key clinical outcomes were lacking.12 Here, we investigated personality traits in relation to cognition, physical function, and mood in 494 pwMS across two cohorts. Building on prior research,12,13we hypothesized beneficial associations of low neuroticism and high openness with cognitive and non-cognitive outcomes. We further hypothesized a protective role of extraversion for better physical function, mood, and cognition, given that extroversion is the proclivity to engage in prosocial behaviors and higher social support had a beneficial role for pwMS based on our prior research.6,7,11
Methods
Participants
The study included patients from two clinic-based MS cohorts: (1) the Prospective Investigation of Multiple Sclerosis in the Three Rivers Region (PROMOTE) study, a longitudinal and clinic-based MS cohort study from the University of Pittsburgh Medical Center (UPMC), which began enrollment in January 2017; and (2) the Columbia University Irving Medical Center (CUIMC), which enrolled patients between December 2014 and August 2019. At enrollment, all participants (UPMC: n=365; CUIMC: n=129) were 18 years or older with a neurologist-confirmed MS diagnosis. Demographic and clinical histories were obtained through questionnaires and review of electronic health records data at each center (Table 1). The UPMC and CUIMC institutional review boards approved the study protocols. All participants provided written informed consent.
Table 1.
Participant characteristics
| UPMC (n = 365) | CUIMC (n = 129) | Statistic, p-value | |
|---|---|---|---|
|
| |||
| Age, y, mean (SD) | 51.3 (12.8) | 45.7 (10.9) | t = 4.70, p < .001 |
| Female sex, n (%) | 299 (81.9) | 98 (76.0) | χ2= 2.14, p = .144 |
| Race, n (%) | χ2=51.56, p <.001 | ||
| Caucasian | 352 (96.4) | 38 (29.5) | |
| Black/African American | 13 (3.6) | 11 (8.5) | |
| Unknown | 80 (62) | ||
| Ethnicity, n (%) | χ2=35.59, p <.001 | ||
| Hispanic | 5 (1.4) | 9 (7) | |
| Non-Hispanic | 360 (98.6) | 51 (40.3) | |
| Unknown | 69 (52.7) | ||
| Disease course (RRMS/other) | 324/41 | 113/16 | |
| Years of education, median (IQR) | 15 (14–18) | 16 (15–18) | t = −.69, p =.487 |
| Disease duration, y, mean (SD) | 14.8 (9.7) | 10.9 (8.1) | t = 4.40, p < .001 |
| NEO-FFI, T-score, mean (SD) | |||
| Neuroticism | 48.53 (11.19) | 50.10 (11.85) | t = −.1.32, p =.189 |
| Extraversion | 46.79 (10.76) | 50.26 (11.31) | t = −.3.02, p =.003 |
| Openness | 49.13 (10.61) | 53.10 (10.75) | t = −.3.55, p < .001 |
| Agreeableness | 52.25 (10.43) | 51.82 (11.97) | t = .35, p = .726 |
| Conscientiousness | 48.87 (10.72) | 47.57 (11.84) | t = 1.13, p = .261 |
Abbreviations: SD = standard deviation, RRMS = Relapsing-Remitting Multiple Sclerosis, IQR = interquartile range, NEO-FFI = NEO Five Factor Inventory
Personality traits
Participants from both cohorts completed the NEO Five-Factor Inventory (NEO-FFI),14 a 60-item measure of the following 5 personality traits: (a) neuroticism, a maladaptive response to stress; (b) extraversion, the proclivity for being energized by social situations; (c) openness, characterized by creative thinking, sensitivity, adventuresomeness, and attentiveness to inner feelings; (d) agreeableness, characterized by high cooperation and eagerness to help others as well as attributes such as trust, altruism, and honesty; (e) conscientiousness, characterized by high impulse control, goal-oriented behavior as well as a high degree of organization and attention to details. Extroverts are excitable, outgoing, and socially expressive, while introverts (those who score low on the extroversion scale) gain their energy from solitude. Raw scores were converted to t-scores for each subscale using the values in the published manual,14 which are derived from a normative sample (mean=50, SD=10) and adjusted for sex. Higher scores in each category indicate higher expression of that trait. The NEO-FFI is widely used in clinical practice and is a validated and reliable measure of personality among patients with MS.15
Outcomes
Physical function, cognition, and depression were quantified using validated measures. Different measures were used in the two cohorts, permitting rigorous assessment of relationships between personality traits and MS outcomes.
Physical function
UPMC cohort participants completed the Patient-Reported Outcomes Measurement Information System (PROMIS) Physical Function scale (version 1.2), which was developed by the National Institutes of Health to assesses the perceived ability to perform a variety of physical activities including mobility, dexterity, neck/back function, and daily living tasks across health and disease. Response options range from 1 (unable to perform) to 5 (can perform without difficulty). Total scores are reported on the t-score metric (M = 50, SD = 10), centered on the general United States population mean with consideration for age, gender, and race/ethnicity. PROMIS is a computer adaptive test with better precision, lower skew, and less participant burden than traditional measures.16 The high sensitivity of the PROMIS enables detection of differences in physical function among pwMS with mild to moderate disability. UPMC participants also completed the Multiple Sclerosis Rating Scale-Revised (MSRS-R) and the Patient Determined Disease Steps (PDDS) survey. While MSRS-R assesses overall neurological symptom burden, PDDS provides a more specific assessment of gait impairment. The MSRS-R examines eight neurological domains (walking, upper limb function, vision, speech, swallowing, cognition, sensory, and bladder and bowel function). Each domain in MSRS-R is scored 0 to 4 with 0 indicating no neurological symptoms and 4 indicating severe disability. PDDS is highly correlated with clinician-rated Expanded Disability Status Scale (EDSS)17. The PDDS scale is based on an ordinal scale from 0 to 8 with 0 indicating no gait impairment and 8 indicating bed-bound status. To address clinically implausible fluctuations in PRO responses, the mean values for MSRS-R and PDDS scales were calculated using scores collected between January 2020 and May 2021. Outlier values that were at least 0.75 IQR above or below the population mean were removed. PDDS and MSRSR means/medians were then recalculated per participant.
In the CUIMC cohort, physical function was assessed using the EDSS and a patient-reported visual analogue scale (VAS). The EDSS evaluates the degree of neurologic impairment based on walking ability and information from other functional systems (e.g., sensory, bowel and bladder, visual). Scores range from 0 to 10, with higher scores indicating higher levels of neurological disability. The VAS assessed the intensity of sensorimotor symptoms (i.e., visual problems, pain, leg/arm numbness/weakness) from 0 (no symptoms) to 100 (worst intensity).
Cognition
The UPMC cohort participants completed the PROMIS Cognitive Function scale (version 2.0), assessing the frequency of cognitive difficulties experienced in the preceding 7 days in areas such as mental acuity, concentration, and memory. Several of the scale items measure executive functions, e.g., I have been able to keep track of what I am doing even if I am interrupted; My thinking has been as fast as usual. Response options range from 1 (high frequency of cognitive difficulties) to 5 (never), with higher scores indicating better cognition. The total scores are reported on the t-score metric (M = 50, SD = 10). CUIMC cohort participants completed the 13-item Everyday Memory Questionnaire-Revised (EMQ-R), a patient-reported measure of memory failure in everyday life over the preceding month.18
Depression
UPMC cohort participants completed the PROMIS Depression scale (version 1.0), assessing depressive symptoms based on cognitive and affective indicators during the preceding 7 days. Response options range from 1 (never) to 5 (always) with total scores reported on the t-score metric (M = 50, SD = 10). CUIMC cohort participants completed the 21-item Beck Depression Inventory II (BDI-II, log-transformed), assessing the existence and severity of dysphoria, anhedonia, suicidal ideation, and other common symptoms of depression (e.g., loss of appetite, irritability).19 The 4-point scale for each item ranges from 0 to 3 with higher scores indicating worse depressive symptoms. Final scores are log-transformed. Mean scores for all outcome variables are displayed in Table 2.
Table 2.
Scores for all outcome measures used in the UPMC and CUIMC cohort
| UPMC (n= 365) | |
|
| |
| PROMIS, T score, mean (SD) | |
| physical function | 42.41 (13.77) |
| cognitive function | 46.63 (13.09) |
| depression | 49.58 (10.31) |
| MSRS-R, median (IQR) | |
| walking | 2 (0–3) |
| total | 6 (3–10) |
| PDDS, median, IQR | 1 (0–4) |
|
| |
| CUIMC (n=129) | |
|
| |
| BDI-II, mean (SD) | 11.65 (10.08) |
| EMQ, mean (SD) | 28.80 (12.71) |
| VAS sensorimotor, mean (SD) | 20.51 (24.26) |
| EDSS, median, IQR | 1.5 (1–2) |
Abbreviations: PROMIS = Patient-Reported Outcomes Measurement Information System, MSRS-R = Multiple Sclerosis rating Scale -Revised, PDDS = Patient Determined Disease Steps, BDI-II = Beck Depression Inventory, EMQ = Everyday Memory Questionnaire, VAS = Visual Analog Scale, EDSS = Expanded Disability Status Scale
Statistical Analysis
Study design is shown in Figure 1. All analyses were conducted using IBM SPSS Statistics version 26. Potential confounding factors were selected a priori based on previous research (i.e., age, disease duration, education, sex, race). To avoid overfit models20 and multicollinearity, we then used an operational (correlation) approach to determine the variables that appreciably changes the association between the predictors and the outcomes (see, Supplementary Materials). Age and disease duration (i.e., time between MS diagnosis and completion of the NEO-FFI) were retained and adjusted as confounder in all analyses. For quality control, we evaluated regression-relevant assumptions, including linearity and homogeneity of error variance for ordinary least squares estimation. Partial correlations, adjusting for age and disease duration, were computed between the five personality factors and all independent variables. To assess independent contributions of personality traits to outcome measures, we performed linear regressions, with the five personality traits entered in stepwise fashion, controlling for age and disease duration. Significance levels for entry were .05 and for removal .10. We reported F-tests for comparing the proposed model to the intercept only model to indicate whether the added coefficients improved the model’s fit. Statistical significance of both p-value and overall F ratio were verified to reject the null hypothesis. All hypothesis tests were two-sided and significance threshold was set at p <.05.
Figure 1.
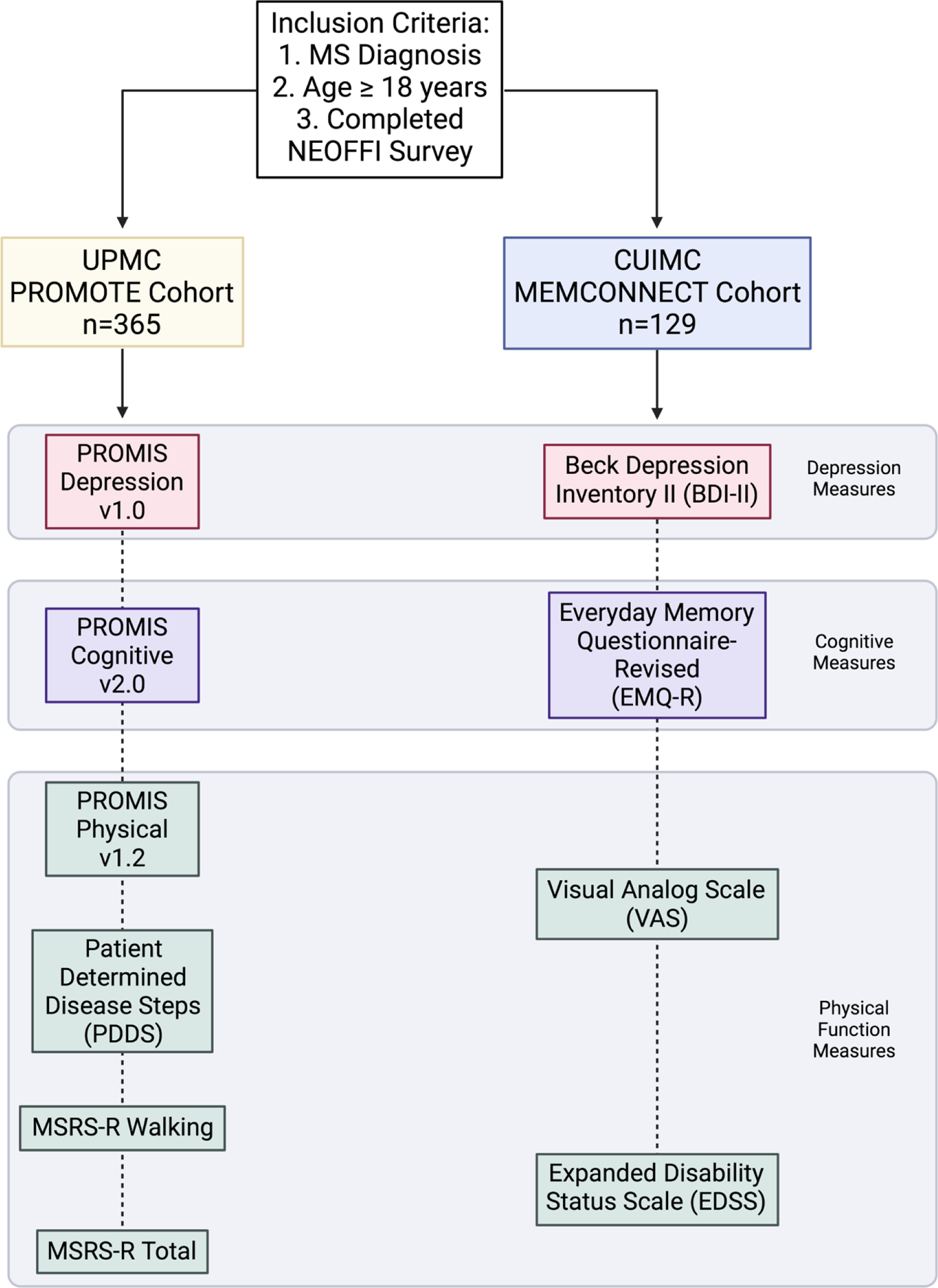
Study design
Results
The demographics of the two cohorts differed in age at enrollment and disease duration (Table 1). Mean (and standard deviation) age was 51.3 (12.8) and 45.7 (10.9) years, and mean disease duration was 14.8 (9.7) and 10.8 (8.1) years for the UPMC and CUIMC cohorts, respectively. Detailed results are displayed in Table 3.
Table 3.
Relationships of personality traits to outcome variables
| MSRS-R walking | PROMIS cognition | PROMIS depression | ||||||||||
|
|
||||||||||||
| UPMC (n=365) | Ba | 95%CI | βb | p c | B | 95%CI | β | p | B | 95%CI | β | p |
|
| ||||||||||||
| Age | .092 | [−.017,.201] | .100 | .099 | −.172 | [−.361,.018] | −.107 | .075 | −.051 | [−.164,.063] | −.055 | .379 |
| Disease duration | −.068 | [−.215−.080] | −.055 | .367 | −.021 | [−.264,.221] | −.010 | .862 | .106 | [−.044,.256] | .087 | .164 |
| Neuroticism | .185 | [.047, 3.24] | .171 | .009 | ||||||||
| Extraversion | −.204 | [−.333, −.076] | −.186 | .002 | .266 | [.045, .487] | .139 | .018 | ||||
| Openness | ||||||||||||
| Agreeableness | .158 | [.014, .303] | .141 | .032 | ||||||||
| Conscientiousness | ||||||||||||
|
| ||||||||||||
| VAS sensorimotor | Self-reported Memory (EMQ) | BDI-II | ||||||||||
|
|
||||||||||||
| CUIMC (n=129) | B | 95%CI | β | p | B | 95%CI | β | p | B | 95%CI | β | p |
|
| ||||||||||||
| Age | .336 | [−.169, .868] | .144 | .212 | −.067 | [−.302, .167] | −.059 | .572 | .013 | [−.112, .139] | .016 | .835 |
| Disease duration | −.040 | [−.775, .695] | −.013 | .914 | .010 | [−.290, 309] | .007 | .959 | .070 | [−.093, .234] | .066 | .394 |
| Neuroticism | .294 | [3.110, 3.478] | .303 | .002 | .398 | [.290, .507] | .558 | < .001 | ||||
| Extraversion | −.767 | [−.128, .259] | −.312 | .004 | −.196 | [−.311, −.081] | −.255 | < .001 | ||||
| Openness | ||||||||||||
| Agreeableness | ||||||||||||
| Conscientiousness | ||||||||||||
Note. In a first step, age and disease duration are entered as predictor variables; subsequently, personality traits were entered in stepwise fashion. Table displays regression coefficients of predictors selected to be included in the final model based on statistical significance.
represents unstandardized regression weights
represents standardized regression weights; standardization based on z-scores with mean = 0 and standard deviation =1.
Adjusted for potential confounders: age and disease duration via linear regression as described in Methods.
Physical function
In both cohorts, we found a positive correlation between extraversion and physical function. In the UPMC cohort, higher extraversion was associated with less impaired walking function (MSRS-R walking subscale score, lower score indicating better neurological function β = −0.186, 95% CI [−0.33, −0.08], p = .002), accounting for an additional 31% of variance (R2 = 0.31) in walking abilities. None of the personality traits were associated with the PROMIS physical or PDDS scores. In the CUIMC cohort, higher extraversion was associated with less severe sensorimotor symptoms (VAS, rp = −0.285, p = .013), a finding that was confirmed when NEO scores for all personality traits were entered into a stepwise linear regression. Controlling for age and disease duration, the only personality factor maintained in the model was extraversion (β =−0.312, 95% CI [−1.28, −.2.60], p = .004), F(3,84) = 3.747, p=.014, explaining 9% of the variance in sensorimotor function (R2adjusted = 0.09). None of the personality traits were associated with EDSS scores.
Cognition
Controlling for age and disease duration, higher extraversion was associated with higher PROMIS cognition scores, i.e., better subjective cognitive function (rp = 0.137, p =.026) in UPMC participants. When entered into stepwise linear regression, the only personality factor maintained in the model was extraversion (β=0.139, 95% CI [0.05, 0.49], p = .018), F(4,285) = 2.965, p = .029, explaining 16% of the variance in cognition. In the CUIMC cohort, partial correlations showed that higher neuroticism scores were associated with higher frequency of memory dysfunction (EMQ, rp = 0.320, p < .005). Neuroticism was maintained in our regression model (β=0.303, 95% CI [0.11, 0.48], p = .002), F(3,105) = 3.992, p=.010, explaining 75% of the variance in self-reported memory function.
Depression
In both cohorts, we found significant associations of neuroticism with depressive symptoms. In the UPMC cohort, higher neuroticism was associated with higher PROMIS depression scores (rp = 0.138, p =.025), when controlling for age and disease duration. Neuroticism entered the regression model in step 1 (β =0.171, 95% CI [0.047, 0.324], p = .009), with agreeableness entering in step 2 (β =0.141, 95% CI [0.014, 0.303], p = .022), i.e., higher agreeableness was associated with greater depressive symptoms. The overall model was significant, F(4,264) = 2.405, p=.029, and both variables account for 25% of the variance in depression scores (neuroticism alone accounts for 12%). In the CUIMC cohort, higher extraversion was associated with lower depression scores (BDI-II, rp = −0.405, p < .001). In stepwise linear regression, neuroticism entered the model in step 1 (β =0.613, 95% CI [0.29, 0.51], p < .001), and extroversion in step 2 (β = −0.255, 95% CI [−0.31, −0.08], p < .001), indicating that higher neuroticism and lower extraversion were associated higher depression scores. The overall model was significant, F(4,111) = 24.24, p <.001, with personality traits accounting for 45% of the variance in BDI-II depression scores.
Discussion
In this cross-sectional study of 494 adults with MS from two geographically and demographically distinct cohorts, we found that personality traits were associated with physical function, cognition, and depression. While patterns of relationships differed between cohorts, there were important consistencies. In both cohorts, higher extraversion correlated with better physical function, while higher neuroticism correlated with greater depression symptoms. Higher extraversion was also associated with better overall subjective cognition in the first cohort, while higher neuroticism was associated with worse subjective memory function in the second cohort. Relationships were independent of age and disease duration (factors identified as possible confounding variables). Overall, findings suggest a protective role of extraversion and a harmful role of neuroticism with respect to clinically relevant patient-reported outcomes in pwMS.
In the general population, personality traits are associated with physical function. Extraversion, for instance, has been consistently linked to walking performance and muscle strength in adults,21,22 possibly through its relationship with health-promoting behaviors such as physical activity.23 Interestingly, a prior study showed a significant negative correlation between extraversion and rater-determined EDSS scores in cognitively preserved MS patients.24 Comparatively little is known about the influence of personality on patient-reported physical function in pwMS. A prior study showed that functional disability was greater in pwMS exhibiting lower novelty seeking behavior and reward dependence, tendencies strongly linked to lower extraversion.25
In this study, higher extraversion was associated not only with better physical function but also with better self-reported cognitive function. In healthy adults, extraversion and openness to experience correlate with cognitive function, including memory26 and language abilities.27 Similarly, greater openness and extraversion may potentially protect against cognitive decline in later age.28 In the context of the theory of cognitive reserve,29 extraverts are postulated to engage in more socially and intellectually stimulating activities, which in turn lead to enhanced cognitive outcomes.30 The few studies that have examined the relationship between personality and cognition in pwMS reported inconsistent findings. Higher openness and lower neuroticism were associated with better memory performance,31 a finding partially confirmed by the current observation of an inverse relationship between neuroticism and self-reported memory function in our second cohort. Other studies described associations of cognitive dysfunction with high neuroticism and low conscientiousness,32 while a recent review suggested that low levels of extraversion, agreeableness, and conscientiousness together with high neuroticism negatively affect cognitive performance and mood.12 Important methodological variability across studies (e.g., self-reported versus informant-reported personality, exclusion of personality factors, and limited cognitive battery) might account for differences in results. Further, sample sizes in prior studies were often modest. Additional studies are warranted to clarify possible mechanisms underlying the interplay of personality traits with physical and cognitive function. For instance, engagement in leisure activities, perceived social support, educational attainment, improvement in socioeconomic status, and brain reserve (i.e., total maximal lifetime brain volume) may serve as mediating factors in the protective versus harmful role of personality traits in pwMS.
Finally, our study revealed positive relationships of neuroticism with depression in both cohorts, consistent with previous research.9 High neuroticism, encompassing an increased tendency to experience negative affect and psychological distress, presents as a potent risk factor for psychopathology (especially depression and anxiety) in healthy adults.33 The underlying mechanism of the associations between neuroticism and mood disorders are only beginning to emerge. For instance, genetic risk factors for neuroticism and major depression are closely related.34 Understanding the role of neuroticism in the development and maintenance of mood disorders is crucial given the higher prevalence of depressive symptoms in pwMS when compared to individuals with other neurological conditions.35 Moreover, understanding the interplay of neuroticism and resilience may yield valuable insights that could translate into behavior interventions.
Our study has two key strengths. First, the study results are largely consistent and confirmatory using data from nearly 500 pwMS across two geographically distinct academic MS centers with different demographic and clinical features, bolstering generalizability of our findings. Second, the study included a broad collection of diverse but validated outcome measures, enabling a rigorous assessment of physical function, cognition, and depression within the study population. Importantly, the overall findings were largely consistent in direction of associations across cohorts despite the use of different surveys to measure the same constructs. To our knowledge, this is the largest study to date that investigated the interplay between personality traits and a wide range of clinically relevant outcomes in MS.
Our study also has limitations. First, we could not draw causal conclusions given the cross-sectional design. While future longitudinal studies will be more informative, the current study has clinical relevance insofar as it reveals patterns to inform testable hypotheses for future research. Second, all of our outcomes were self-report measures that have been validated for use in MS. While we maintain that patient self-report offers valuable insight into function, there remains an opportunity for future studies utilizing objective measures of physical and cognitive function to bolster and extend these findings. In particular, employing comprehensive cognitive batteries that encompass domains including executive function, language, and memory, will provide insights into targeted relationships of personality traits to cognition. Third, our two cohorts differ in size and patient characteristics. The UPMC cohort was older and had longer average disease duration than the CUIMC cohort. The CUIMC cohort was smaller and potentially underpowered to detect some of the observed relationships, which might explain some of the results. Importantly, the overall findings were largely consistent despite small differences.
In summary, our study highlights personality traits, in particular extraversion and neuroticism, as significant factors associated with differential physical function, cognition, and mood in pwMS. Future longitudinal studies are necessary to identify biopsychological mechanisms and/or neural substrates that underlie relationships between personality traits and clinical outcomes in MS. Better understanding of personality as a risk or protective factor in MS supports the inclusion of personality in predictive models of disease outcomes to ultimately inform the development of behavioral interventions targeting personality as a factor related to health outcomes in MS.
Supplementary Material
Highlights:
Higher extraversion is associated with better subjective physical and cognitive function
Higher neuroticism is associated with worse depression
Extraversion may be a protective personality trait for persons with multiple sclerosis
Neuroticism may be a risk factor for clinically relevant outcomes in MS
Study Funding:
Funding for this study was provided by the National Multiple Sclerosis Society (MB-1605-08706) and the National Institutes of Health (NINDS, R25 NS088248) to Victoria M. Leavitt.
Footnotes
The Authors declare that there is no conflict of interest.
Financial Disclosures
Anne Kever – Reports no disclosures relevant to this work.
Elizabeth L. Walker – Reports no disclosures relevant to this work.
Claire S. Riley - Reports no disclosures relevant to this work.
Rock A. Heyman – Reports no disclosures relevant to this work.
Zongqi Xia – Reports no disclosures relevant to this work.
Victoria M. Leavitt – Reports no disclosures relevant to this work.
CRediT author statement
Anne Kever: Data curation, Writing- Original draft preparation, Formal Analysis, Writing- Reviewing and Editing
Elizabeth L. Walker: Data curation, Writing- Original draft preparation
Claire S. Riley: Resources, Writing- Reviewing and Editing
Rock A. Heyman: Resources, Writing- Reviewing and Editing
Zongqi Xia: Conceptualization, Methodology, Writing- Reviewing and Editing, Supervision
Victoria M. Leavitt: Conceptualization, Methodology, Writing- Reviewing and Editing, Supervision
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Souza A, Kelleher A, Cooper R, et al. Multiple sclerosis and mobility-related assistive technology: Systematic review of literature. J Rehabil Res Dev 2010; 47: 213. [DOI] [PubMed] [Google Scholar]
- 2.Sumowski JF, Benedict R, Enzinger C, et al. Cognition in multiple sclerosis: State of the field and priorities for the future. Neurology 2018; 90: 278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marrie RA, Reingold S, Cohen J, et al. The incidence and prevalence of psychiatric disorders in multiple sclerosis: A systematic review. Mult Scler J 2015; 21: 305–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leavitt VM, Cirnigliaro C, Cohen A, et al. Aerobic exercise increases hippocampal volume and improves memory in multiple sclerosis: Preliminary findings. Neurocase 2014; 20: 695–697. [DOI] [PubMed] [Google Scholar]
- 5.Katz Sand I. The Role of Diet in Multiple Sclerosis: Mechanistic Connections and Current Evidence. Curr Nutr Rep 2018; 7: 150–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kever A, Buyukturkoglu K, Riley CS, et al. Social support is linked to mental health, quality of life, and motor function in multiple sclerosis. J Neurol Epub ahead of print 3 January 2021. DOI: 10.1007/s00415-020-10330-7. [DOI] [PubMed] [Google Scholar]
- 7.Kever A, Buyukturkoglu K, Levin SN, et al. Associations of social network structure with cognition and amygdala volume in multiple sclerosis: An exploratory investigation. Mult Scler J 2021; 135245852110183. [DOI] [PubMed] [Google Scholar]
- 8.McCrae RR. The five-factor model and its assessment in clinical settings. J Assess Online Ser 1991; 57: 399–314. [DOI] [PubMed] [Google Scholar]
- 9.Bruce JM, Lynch SG. Personality traits in multiple sclerosis: Association with mood and anxiety disorders. J Psychosom Res 2011; 70: 479–485. [DOI] [PubMed] [Google Scholar]
- 10.Estrada-López M, Reguera-García MM, Pérez Rivera FJ, et al. Physical disability and personality traits in multiple sclerosis. Mult Scler Relat Disord 2020; 37: 101465. [DOI] [PubMed] [Google Scholar]
- 11.Levin SN, Riley CS, Dhand A, et al. Association of social network structure and physical function in patients with multiple sclerosis. Neurology 2020; 95: e1565–e1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maggio MG, Cuzzola MF, Latella D, et al. How personality traits affect functional outcomes in patients with multiple sclerosis: A scoping review on a poorly understood topic. Mult Scler Relat Disord 2020; 46: 102560. [DOI] [PubMed] [Google Scholar]
- 13.Roy S, Drake AS, Eizaguirre MB. Trait neuroticism, extraversion, and conscientiousness in multiple sclerosis: link to cognitive impairment? Mult Scler J 2018; 24: 205–213. [DOI] [PubMed] [Google Scholar]
- 14.Costa PT, McCrae RR. Professional manual for the NEO PI-R and NEO-FFI.
- 15.Schwartz ES, Chapman BP, Duberstein PR, et al. The NEO-FFI in Multiple Sclerosis: Internal Consistency, Factorial Validity, and Correspondence Between Self and Informant Reports. Assessment 2011; 18: 39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Senders A, Hanes D, Bourdette D, et al. Reducing survey burden: feasibility and validity of PROMIS measures in multiple sclerosis. Mult Scler J 2014; 20: 1102–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983; 33: 1444–1444. [DOI] [PubMed] [Google Scholar]
- 18.Royle J, Lincoln NB. The Everyday Memory Questionnaire – revised: Development of a 13-item scale. Disabil Rehabil 2008; 30: 114–121. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y-P, Gorenstein C. Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Rev Bras Psiquiatr 2013; 35: 416–431. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Z. Too much covariates in a multivariable model may cause the problem of overfitting. J Thorac Dis; 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kekäläinen T, Terracciano A, Sipilä S, et al. Personality traits and physical functioning: a cross-sectional multimethod facet-level analysis. Eur Rev Aging Phys Act 2020; 17: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stephan Y, Sutin AR, Bovier-Lapierre G, et al. Personality and Walking Speed Across Adulthood: Prospective Evidence From Five Samples. Soc Psychol Personal Sci 2018; 9: 773–780. [Google Scholar]
- 23.Rhodes RE, Smith NEI. Personality correlates of physical activity: a review and meta-analysis. Br J Sports Med 2006; 40: 958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gioia MC, Cerasa A, Valentino P, et al. Neurofunctional correlates of personality traits in relapsing-remitting multiple sclerosis: An fMRI study. Brain Cogn 2009; 71: 320–327. [DOI] [PubMed] [Google Scholar]
- 25.Gazioglu S, Cakmak VA, Ozkorumak E, et al. Personality Traits of Patients With Multiple Sclerosis and Their Relationship With Clinical Characteristics. J Nerv Ment Dis 2014; 202: 408–411. [DOI] [PubMed] [Google Scholar]
- 26.Rogalski E, Gefen T, Mao Q, et al. Cognitive trajectories and spectrum of neuropathology in S uper A gers: The first 10 cases. Hippocampus 2019; 29: 458–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sutin AR, Stephan Y, Damian RI, et al. Five-factor model personality traits and verbal fluency in 10 cohorts. Psychol Aging 2019; 34: 362–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curtis RG, Windsor TD, Soubelet A. The relationship between Big-5 personality traits and cognitive ability in older adults – a review. Aging Neuropsychol Cogn 2015; 22: 42–71. [DOI] [PubMed] [Google Scholar]
- 29.Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc 2002; 8: 448–460. [PubMed] [Google Scholar]
- 30.Hertzog C, Kramer AF, Wilson RS, et al. Enrichment Effects on Adult Cognitive Development: Can the Functional Capacity of Older Adults Be Preserved and Enhanced? Psychol Sci Public Interest 2008; 9: 1–65. [DOI] [PubMed] [Google Scholar]
- 31.Leavitt VM, Buyukturkoglu K, Inglese M, et al. Protective Personality Traits: High Openness and Low Neuroticism Linked to Better Memory in Multiple Sclerosis. Mult Scler J 2017; 23: 1786–1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akbar N. Self-assessment of Cognition in Multiple Sclerosis: The Role of Personality and Anxiety. 2011; 24: 7. [DOI] [PubMed] [Google Scholar]
- 33.Kendler KS, Kuhn J, Prescott CA. The Interrelationship of Neuroticism, Sex, and Stressful Life Events in the Prediction of Episodes of Major Depression. Am J Psychiatry 2004; 161: 631–636. [DOI] [PubMed] [Google Scholar]
- 34.Fanous A, Gardner CO, Prescott CA, et al. Neuroticism, major depression and gender: a population-based twin study. Psychol Med 2002; 32: 719–728. [DOI] [PubMed] [Google Scholar]
- 35.Siegert RJ. Depression in multiple sclerosis: a review. J Neurol Neurosurg Psychiatry 2005; 76: 469–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


