Abstract
Objective:
To examine trends in mental health care use for Black and Latinx children and adolescents.
Method:
Data from the Medical Expenditure Panel Survey (MEPS) 2010 – 2017 were analyzed to assess trends among youth ages 5–17 in use and expenditures for any mental health care, outpatient mental health care, and psychotropic medication fills. Unadjusted trends for all youth and the subpopulation of youth reporting need for mental health care and disparities adjusting for need were examined.
Results:
Between 2010–2017, Black youth rates of any past year mental health care use decreased (9% to 8%) while White (13% to 15%) and Latinx youth (6% to 8%) rates increased. Among the subpopulation with need, and in regression analysis adjusting for need, we identified significant Black-White and Latinx-White disparities in any mental health care use and any outpatient mental health care use in 2010–2011 and 2016–2017, with significant worsening of Black-White disparities over time. White youth were more than twice as likely as Latinx youth to use psychotropic medications, and Latinx-White and Black-White disparities in psychotropic medication fills persisted over time. Black-White disparities existed in overall mental health expenditures (2016–2017) and outpatient mental health expenditures (2010–2011 and 2016–2017).
Conclusion:
Affordable, ubiquitous access to mental health care for Black and Latinx youth remains an elusive target. Significant disparities exist in receiving mental health care despite reforms and policies designed to increase mental health care access in the general population. Additional outreach and treatment strategies tailored to the cultural, linguistic and structural needs of youth of color are required.
Keywords: mental health care access, racial/ethnic disparities, children, mental health policy, Medical Expenditure Panel Survey
INTRODUCTION
Mental health conditions among children and adolescents (youth) can negatively impact educational and social outcomes, and lead to other health compromising behaviors.1–3 In the United States, depression, attention-deficit/hyperactivity disorder, and anxiety are the most common mental health disorders among children aged 3–17 years,4 with prevalence rates for these disorders of 3.2%, 6.8% and 7.1%, respectively.5,6 Early diagnosis and access to effective mental health care for children and their families are necessary to increase the opportunity for healthy life experiences and trajectories.
Rates of access to mental health care and disparities in access vary greatly among youth in the United States depending on the setting and type of treatment. Approximately 7.3% of youth and 20.6% of youth with elevated symptoms or clinical diagnoses receive treatment in outpatient settings.7 In studies of psychotropic medication use among children conducted in the 1990s and early 2000s, White youth were more likely to be prescribed or to endorse taking psychotropic mediation than racial/ethnic minority youth.8–10 Findings suggest that even with an indication for psychotropic medication use, Black and Latinx youth were underprescribed.10 Youth with private insurance were more likely to have been prescribed psychotropic medication.8
Across settings, racial/ethnic minority youth experience difficulties in accessing mental health care.11,12 Historically, the mental health system has failed to reach youth in the community with a need for care and has primarily focused on treatment among help-seeking individuals. The lack of mental health care access among racial/ethnic minority youth can be attributed to inadequate service availability, insurance barriers, stigma, and language barriers.13 Even among youth able to access mental health care, there is great variability by racial/ethnic group, and there can be challenges in accessing guideline concordant care or minimally adequate treatment.14
Black and Latinx children are significantly less likely to receive treatment when endorsing a need for mental health services.15,16 In an examination of youth mental health care disparity trends using the Medical Expenditure Panel Survey (MEPS), researchers found significant racial/ethnic disparities between 2002–2007.17 Black and Latinx youth reported accessing/initiating mental health care at approximately half the rate of White youth.17 Similarly in a another study using the MEPS focusing on 2006–2012, Latinx-White and Black-White disparities were identified in outpatient mental health care use among youth between 2006–2012.16 We know of no studies measuring youth mental health care disparities since that time. Our study follows up on this existing body of work, examining mental health care use disparity trends between 2010 and 2017.
Since 2012, there have been important policy developments that have had the potential to reduce youth mental health care disparities. In 2014, the Affordable Care Act created individual insurance markets (“exchanges”) with subsidized premiums and cost-sharing for families living below 400% of the federal poverty level.18,19 The ACA eliminated exclusions based on pre-existing conditions, instituted annual out-of-pocket maximums, required community rated premiums and required plans offered on the marketplace to cover ten essential health benefit categories, including pediatric well-visits and behavioral screenings.19 Moreover, the ACA extended the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 to require all insurance plans, including large-group, small-group and individual markets, to cover behavioral health services on par with medical and surgical services. The ACA also included additional resources for accountable care organizations (ACOs) and community health centers that could disproportionately affect the amount of resources/expenditures spent on the mental health care of racial/ethnic minority populations.20
Policy changes to the Children’s Health Insurance Program (CHIP) through reauthorization in 2009 also sought to improve racial/ethnic disparities by reducing the numbers of uninsured and improve quality measures for child mental health care.21,22 Along with Medicaid, CHIP insured over 42 million children in the United States. The reauthorization allocated an additional $32.8 billion in funds, expanding it to reach another 4 million children. Enrollment in Medicaid and CHIP has increased by 17 million people, decreasing the number of uninsured children in the United States between 2010 and 2017.
These policies enacted over the last decade were expected to reduce the number of uninsured youth and improve health insurance coverage of mental health care, leading to improvements in access to any mental health care, outpatient mental health care, any psychotropic medication, and mental health care expenditures given service use. We hypothesize that insurance reforms and other factors during this time-period led to increased utilization of mental health care for all racial/ethnic groups and a reduction in Black-White and Latinx-White disparities over time. Given that rates of overall youth psychotropic medication leveled off in the 2011–2014 time-period,23 and because parity laws targeted cost-sharing requirements and treatment limitations especially relevant to outpatient mental health care, we hypothesize greater increases and disparity reductions in outpatient mental health care than psychotropic medication fills.
METHOD
The Medical Expenditure Panel Survey (MEPS) is a nationally representative survey of healthcare utilization, health insurance coverage, health status and healthcare payment source completed by noninstitutionalized households in the United States. An adult member of the household, usually a parent, provided information about children under the age of 18. We used cross-sectional data from the Household Component of the MEPS to assess trends between calendar years 2010 and 2017. Data were combined into two-year periods to increase precision of the point estimates. The full-year response rate for these years was between 57.2% and 63.1%. Using survey weights developed by the Agency for the Healthcare Research and Quality,24 we weighted the sample to be nationally representative, with weighting accounting for attrition and nonresponse.
Study Cohort
Our sample consist of youth between the ages of 5–17 from the 2010–2017 MEPS that were categorized into racial/ethnic categories defined by the U.S. Census: non-Hispanic White (hereafter White; n = 16, 840), non-Hispanic Black (hereafter, Black n = 11,744) and Hispanic/Latino (hereafter Latinx; n = 22,533). Other racial/ethnic groups were not included due to small sample sizes.
Measures
Outcome variables include any mental health care use, any outpatient mental health care use, any psychotropic medication fill, and expenditures conditional on any mental health care use. Any mental health care use was considered to be one of the following events: (a) an outpatient provider visit associated with a mental health diagnosis (International Classification Disease (ICD-9) codes 291, 292 or 295–314; ICD-10 codes: F01-F99); (b) treatment coded as psychotherapy or mental health counseling; and/or (c) a psychotropic medication fill identified through the Multum Medisource Lexicon classification system. MEPS respondents report mental health diagnosis with high accuracy.25 Information reported by MEPS respondents is verified using follow-back surveys with physicians, hospitals and pharmacies.25
Covariates Representing Need for Mental Health Care
According to the IOM definition of healthcare disparities, racial/ethnic disparities in healthcare are “all differences except those due to clinical need and appropriateness and patient preferences.”26 Given the absence of measures of appropriateness and patient preferences in these data, we focus on measuring racial/ethnic differences that are not due to need for mental health care. This definition of disparities posits that the healthcare system should be evaluated on differences that are due to operation of health care systems, the legal and regulatory climate, discrimination, not differences due to the underlying clinical characteristics and demographic composition of the population at the time of treatment.26 For example, if Black youth have lower prevalence of mental illness than White youth, then it is expected that there would be lower rates of mental health care use; these prevalence-related differences should thus be removed from the disparity calculation. In contrast, differences due to other variables, such as those related to socioeconomic status (SES), insurance status, or other healthcare system characteristics should enter into the disparity calculation. These non-need differences are considered to be “unfair” or “unjust,” recognizing the compounding disadvantages of race/ethnicity, SES and discriminating legal and regulatory systems.27 For example, if Black youth have, on average, lower family income than White youth, and the healthcare system treats those with lower SES worse than those with higher SES, than the racial differences in utilization that occur via poorer treatment for those in lower SES categories should enter into the disparity calculation.
To implement the IOM definition, when assessing healthcare systems, differences in utilization due to “need” factors are considered to be appropriate or allowable, and are adjusted for in regression models.27 We include measures of mental and physical health status as proxies for treatment need. Mental health status measures included the Columbia Impairment Scale (CIS) and parent-reported mental health (categorized into excellent, very good, good, fair or poor). The CIS is a parent-reported 13-item scale measuring psychological functioning and impairment in children (items are displayed in Table 1). Scores range from 0 to 52, with higher scores indicating greater impairment. The parent-administered CIS has been validated in multiethnic community samples, where it demonstrated high test-retest reliability.28 Prior studies have indicated scores > 15 on the CIS is predictive of psychological dysfunction and clinician-rated global impairment. Physical health status measures included parent-reported physical health (categorized into excellent, very good, good, fair or poor) and an indicator for an activity-limiting condition.29 We also adjusted for age (5–9, 10–13, 14–17) and sex as these demographic covariates are considered to be highly associated with treatment need.27 Indicators for survey year were also included as covariates to be adjusted for in regression models.
Table 1.
Weighted population characteristics for youth ages 5 to 17 by race/ethnicity, 2010–2017 Medical Expenditure Panel Survey (MEPS)
| N | White | White | Black | Black | Latino | Latino |
|---|---|---|---|---|---|---|
| 2010–2011 4,690 |
2016–2017 3,949 |
2010–2011 2,967 |
2016–2017 2,392 |
2010–2011 4,911 |
2016–2017 5,287 |
|
| Dependent variables | ||||||
| Any mental health care use (%) | 12.9 | 15.0 | 9.1*** | 8.0*** | 5.7*** | 7.8*** |
| Mental health expenditures given use ($) | 1704.3 | 2094.4 | 1307.6 | 2140.1 | 1309.2 | 1751.8 |
| Any outpatient mental health care use (%) | 10.2 | 13.3 | 6.4*** | 6.9*** | 4.5*** | 6.8*** |
| Outpatient mental health expenditures given use ($) | 1118.4 | 1680.1 | 716.1 | 1780.0 | 910.0 | 1401.3 |
| Any psychotropic medication use (%) | 9.1 | 7.8 | 6.8* | 4.7** | 3.2*** | 3.5*** |
| Psychotropic medication expenditures given use ($) | 1164.4 | 1144.1 | 1058.0 | 1061.8 | 1062.5 | 1199.1 |
| Need and preference | ||||||
| Age (%) | ||||||
| 5–9 | 36.7 | 35.9 | 37.3 | 38.4 | 41.6*** | 38.3 |
| 10–13 | 31.0 | 30.8 | 31.0 | 29.6 | 29.5 | 30.3 |
| 14–17 | 32.3 | 33.3 | 31.7 | 32.0 | 28.9* | 31.4 |
| Gender (%) | ||||||
| Female | 49.2 | 48.9 | 49.5 | 48.9 | 48.8 | 49.0 |
| MH status (%) | ||||||
| Excellent | 54.9 | 54.1 | 52.7 | 57.7 | 48.26** | 55.0 |
| Very good | 28.0 | 29.9 | 24.6* | 21.8*** | 29.1 | 23.5*** |
| Good | 14.7 | 13.2 | 18.2* | 17.2** | 19.7* | 19.0*** |
| Fair | 1.9 | 2.4 | 3.9*** | 2.9 | 2.5 | 2.1 |
| Poor | 0.4 | 0.4 | 0.4 | 0.5 | 0.4 | 0.3 |
| Psychological impairment (%) (age<18only) | ||||||
| Columbia impairment scale >16 | 9.9 | 7.3 | 10.8 | 7.7 | 6.9*** | 4.5*** |
| Any activity limitation (%) | 0.7 | 0.9 | 0.8 | 0.3** | 0.4 | 0.4** |
| Health status (%) | ||||||
| Excellent | 60.9 | 63.0 | 56.5* | 58.7* | 46.6*** | 55.8*** |
| Very good | 25.9 | 25.1 | 23.7 | 23.2 | 29.2* | 22.9 |
| Good | 11.3 | 10.2 | 16.5*** | 15.0*** | 19.7*** | 17.4*** |
| Fair | 1.4 | 1.5 | 2.9*** | 2.7* | 3.9*** | 3.2*** |
| Poor | 0.3 | 0.1 | 0.3 | 0.2 | 0.5 | 0.5*** |
| Socioeconomic status | ||||||
| Family income level (%) %FPL | ||||||
| <100% FPL | 10.9 | 10.4 | 34.5*** | 31.3*** | 34.0*** | 25.2*** |
| 100–125% FPL | 3.3 | 2.4 | 9.0*** | 8.6*** | 10.6*** | 8.6*** |
| 126–200% FPL | 13.9 | 12.9 | 17.1* | 17.7** | 20.8*** | 21.7*** |
| 201–400% FPL | 35.6 | 31.7 | 24.7*** | 27.4* | 24.5*** | 29.2 |
| > 400% FPL | 35.6 | 42.7 | 14.8*** | 15.2*** | 10.1*** | 15.4*** |
| Insurance status (%) | ||||||
| Private | 70.1 | 67.7 | 34.5*** | 30.8*** | 29.0*** | 32.8*** |
| Medicaid/SCHIP | 24.4 | 29.8 | 60.9*** | 66.4*** | 60.3*** | 61.8*** |
| Medicare | 0.1 | 0.02 | 0.5 | 0.1* | 0.3 | 0.1* |
| Uninsured | 5.4 | 2.5 | 4.1 | 2.7 | 10.5*** | 5.2** |
| Region (%) | ||||||
| Northeast | 18.8 | 17.1 | 16.3 | 15.5 | 11.8* | 12.0** |
| Midwest | 27.2 | 28.7 | 18.1** | 18.0*** | 10.1*** | 10.5*** |
| South | 35.2 | 35.4 | 56.9*** | 59.0*** | 35.8 | 37.6 |
| West | 18.9 | 18.8 | 8.7*** | 7.6*** | 42.4*** | 39.9*** |
Note: All comparisons between White and minority group; Calculations are weighted to be representative of the entire US population; Data: Combined yearly cross-sectional data from 2010–2017 Medical Expenditure Panel Survey (MEPS). FPL = federal poverty level; MH = mental health.
p<0.05.
p<0.01;
p<0.001.
In contrast, other “non-need” variables (e.g., SES and insurance) are not adjusted for in the disparities calculation, because they are considered to be “unfair” or “unjust” differences. Because these covariates are not adjusted for in regression models, differences in utilization due to these non-need covariates enter into the disparity calculation.27 The following variables were included in the descriptive tables describing the youth population by race/ethnicity, but not adjusted for in the disparities calculation: insurance status (private, Medicaid/SCHIP, Medicare or uninsured),30 household income in relation to the federal poverty level (FPL; <100% FPL, 100–125% FPL, 126–200% FPL, 201–400% FPL and > 400% FPL)17 and region (South, Midwest, West, Northeast).31
Analysis
First, we compared children’s outcomes and characteristics between 2010–2011 and 2016–2017, by racial/ethnic group using chi-square and t-tests for categorical and continuous variables, respectively. Second, we plotted unadjusted rates of any mental health care use by year and race/ethnicity for all youth and the subpopulation of youth with reported need for mental health care (operationalized as having a CIS score >15). Chi-square tests were used for mental health care comparisons between (2010 – 2011) and (2016 – 2017). Third, we conducted regression analyses concordant with the IOM definition of disparities,26 adjusting for mental health care need as described above. Importantly, other non-need covariates such as insurance and family income were not adjusted for when calculating racial/ethnic healthcare disparities.27,32–34
We used two-part models (TPM) to separately estimate the probability of any mental health care use and expenditures conditional on any use. This approach allows us to account for the skewness and large number of zeros in the expenditure data.35,36 In the first part of the TPM, we used logistic regression to estimate the probability of any mental health care use, where the outcome variable is dichotomous and takes on a value of 1 when expenditures are greater than zero. The second part of the TPM estimated mental health expenditures conditional on any service use using a generalized linear model with a gamma distribution and a log link function. We used the modified Park test to determine this optimal mean-variance relationship.35,36 All models were estimated using MEPS weights to reflect sample design and survey nonresponse. The primary predictor of interest in both parts of the TPM is an interaction term between race/ethnicity and time, which yields the difference in disparities over time (2010–2011 and 2016–2017). Model-based predictions of access to and expenditures of mental health care use by race/ethnicity and time-period were generated using the predictive margins command in Stata.37
Variance was estimated using bootstrap methods38 that account for the complex study design, nonresponse rate of the MEPS and standardized stratum and primary sampling unit variable across pooled years. All analyses were conducted using Stata 15.39
RESULTS
Table 1 provides unadjusted comparisons of youth characteristics by racial/ethnic group. There were significant Black-White and Latinx-White differences during the 2010–2011 and the 2016–2017 time periods, for any mental health care use, any outpatient mental health care use and psychotropic medication fill. Relative to White youth, Black and Latinx youth reported less psychological impairment and lower parent-reported mental health status ratings. Black and Latinx youth were less likely to report excellent health and more likely to report good or fair health status, relative to White youth. Black and Latinx youth were also more likely to live in the southern region of the US while Latinx youth were more likely to live in the western region.
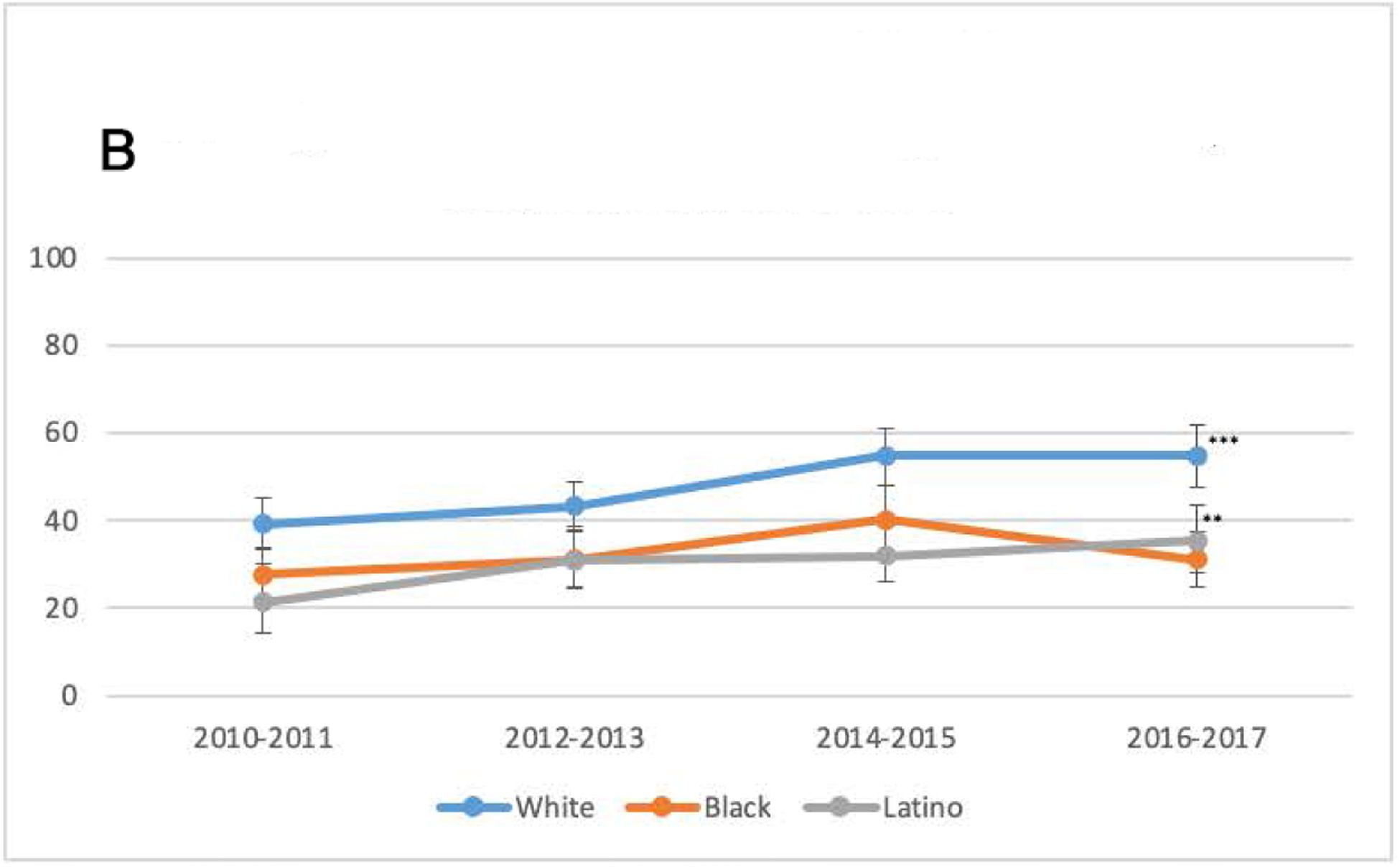
Between 2010–2017, the unadjusted rate of receiving any mental health care (Figure 1A) significantly increased for White and Latinx youth from 13% to 15% and 6% to 8%, respectively. During the same period, the unadjusted rate of receiving any outpatient mental health care (Figure 1B) significantly increased for White (10% to 13%) and Latinx (5% to 7%) youth. Rates of any psychotropic medication fills (Figure 1C) significantly decreased for Black youth from 7% to 5% and remained steady for White and Latinx youth.
Figure 1. Mental Health Care Differences by Race/Ethnicity, 2010–2017.
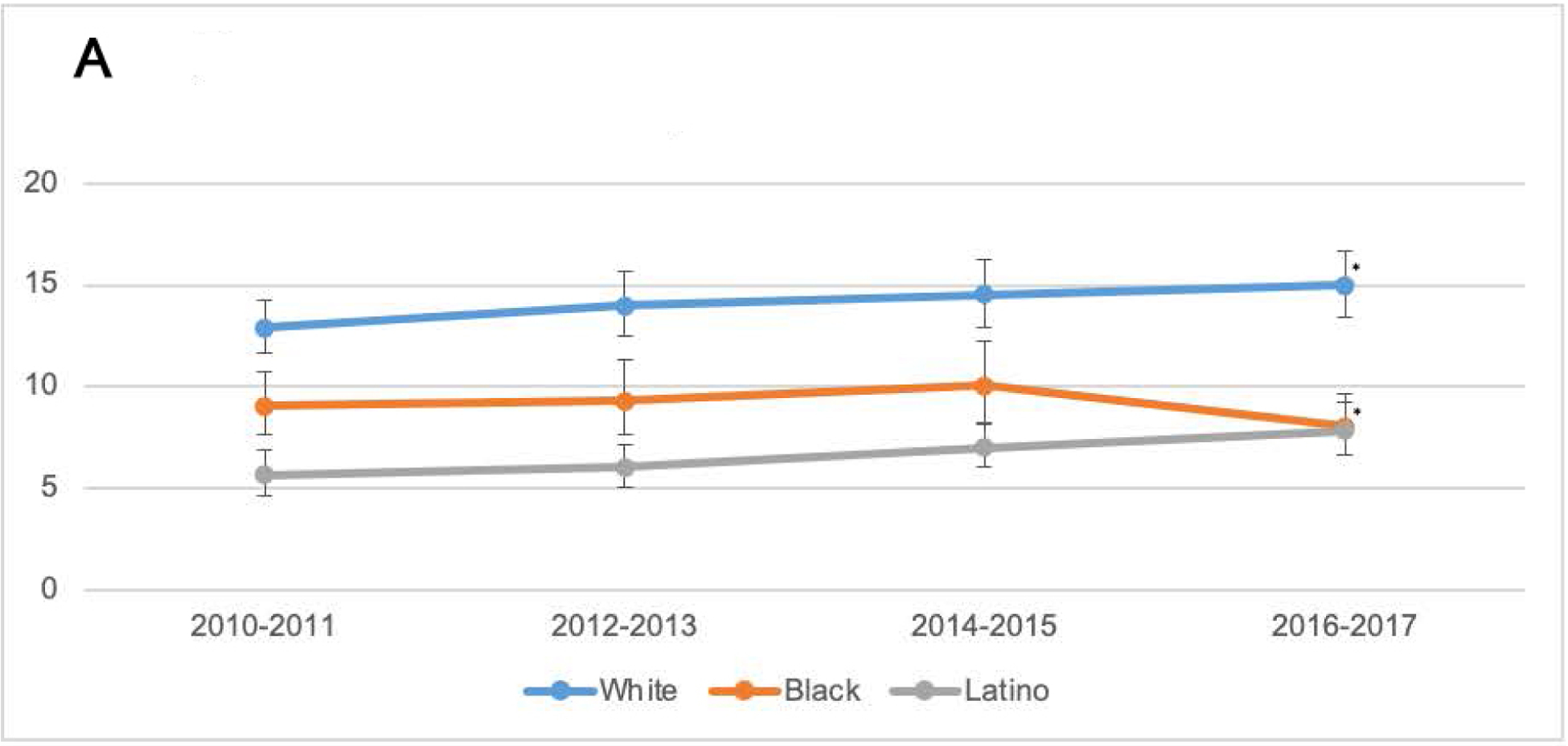
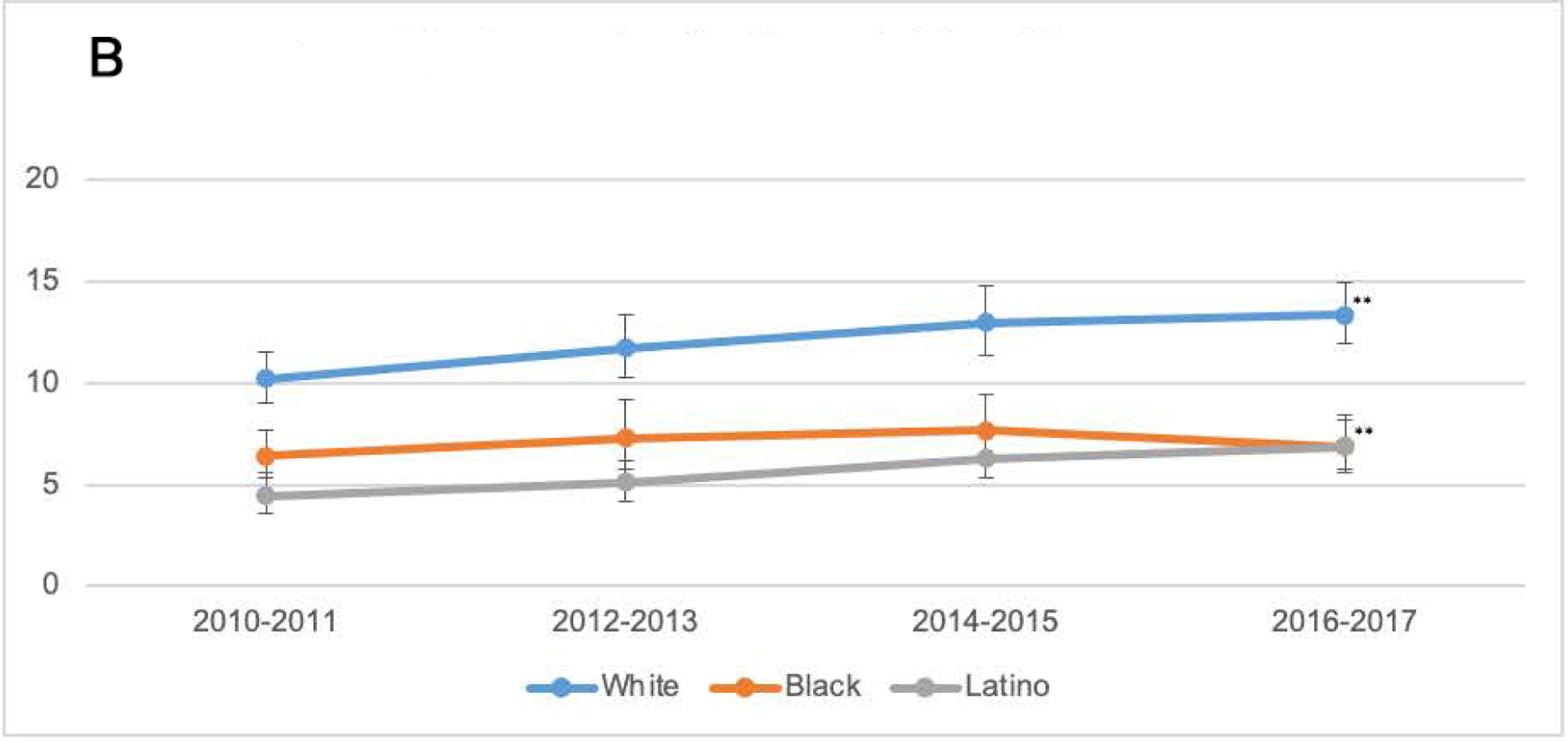
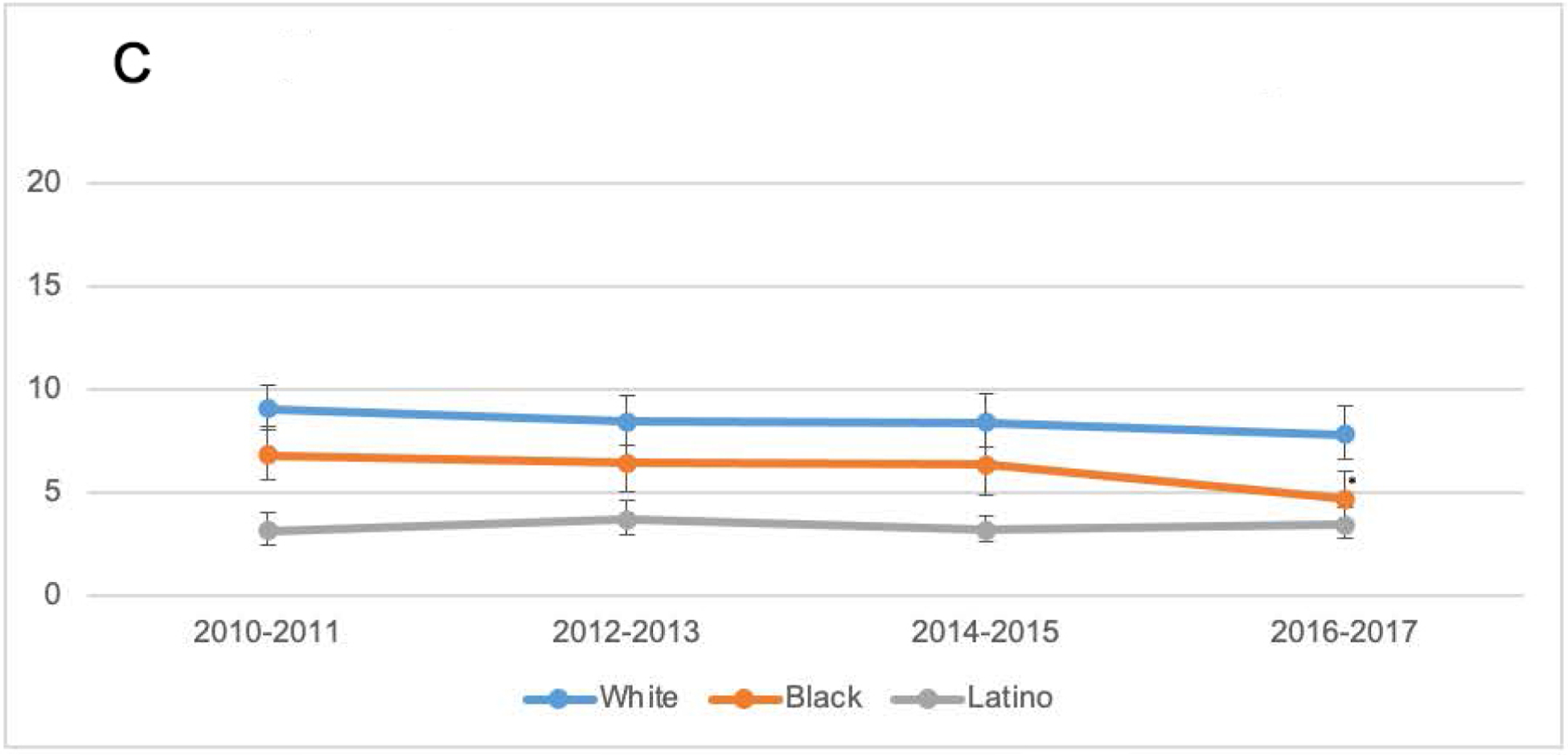
Note: A) any mental health care use by race/ethnicity, 2010 – 2017. B) any outpatient mental health care use by race/ethnicity, 2010 – 2017. C) any psychotropic medication use by race/ethnicity, 2010 – 2017.
Data for A) and B): Youth ages 5–17 (n= 51,117) from the 2010–2017 Medical Expenditure Panel Survey (MEPS). Any mental health care use is defined as an outpatient provider visit associated with a mental health diagnosis (International Classification Disease (ICD-9) codes 291, 292 or 295–314; ICD-10 codes: F01-F99) or treatment coded as psychotherapy or mental health counseling or a psychotropic medication fill identified through the Multum Medisource Lexicon classification system. The statistical comparison is between the first and last point on the x-axis (2010–11 vs 2016–17). Data for C): Youth ages 5–17 (n= 51,117) from the 2010–2017 Medical Expenditure Panel Survey (MEPS). Any psychotropic medication fill was identified through the Multum Medisource Lexicon classification system. The statistical comparison is between the first and last point on the x-axis (2010–11 vs 2016–17).
*p<0.05; **p<0.01.
When looking at a sub-group of youth with reported need for mental health care (Figures 2A - 2C), between 2010–2017, rates of any mental health care and any outpatient mental health care significantly increased by more than 10 percentage-points for White (12% and 16%, respectively) and Latinx (13% and 14%, respectively) youth. There were no significant changes among racial/ethnic groups in rates of psychotropic medication fills.
Figure 2. Mental Health Care Differences by Race/Ethnicity Among Youth With Need, 2010–2017.
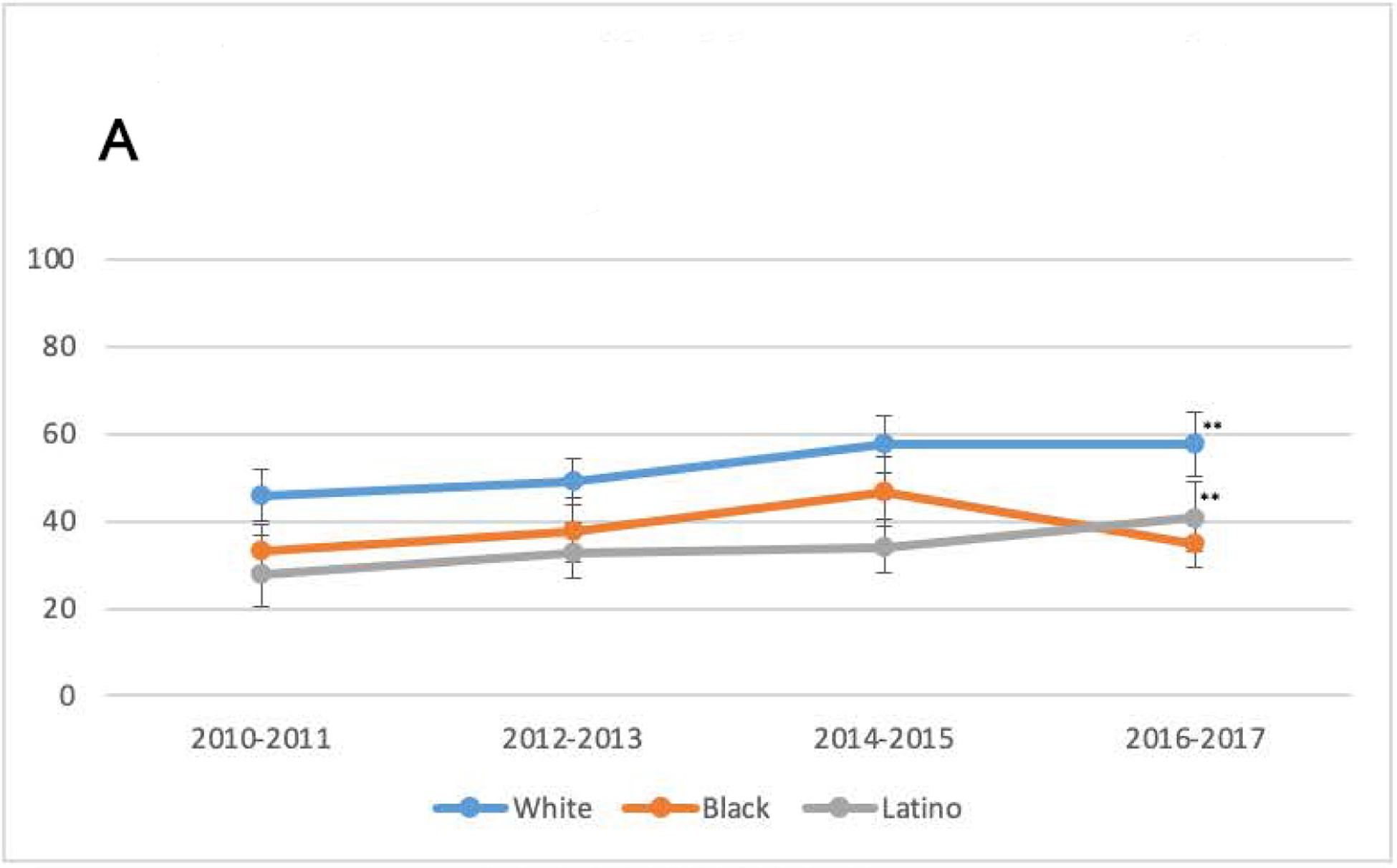
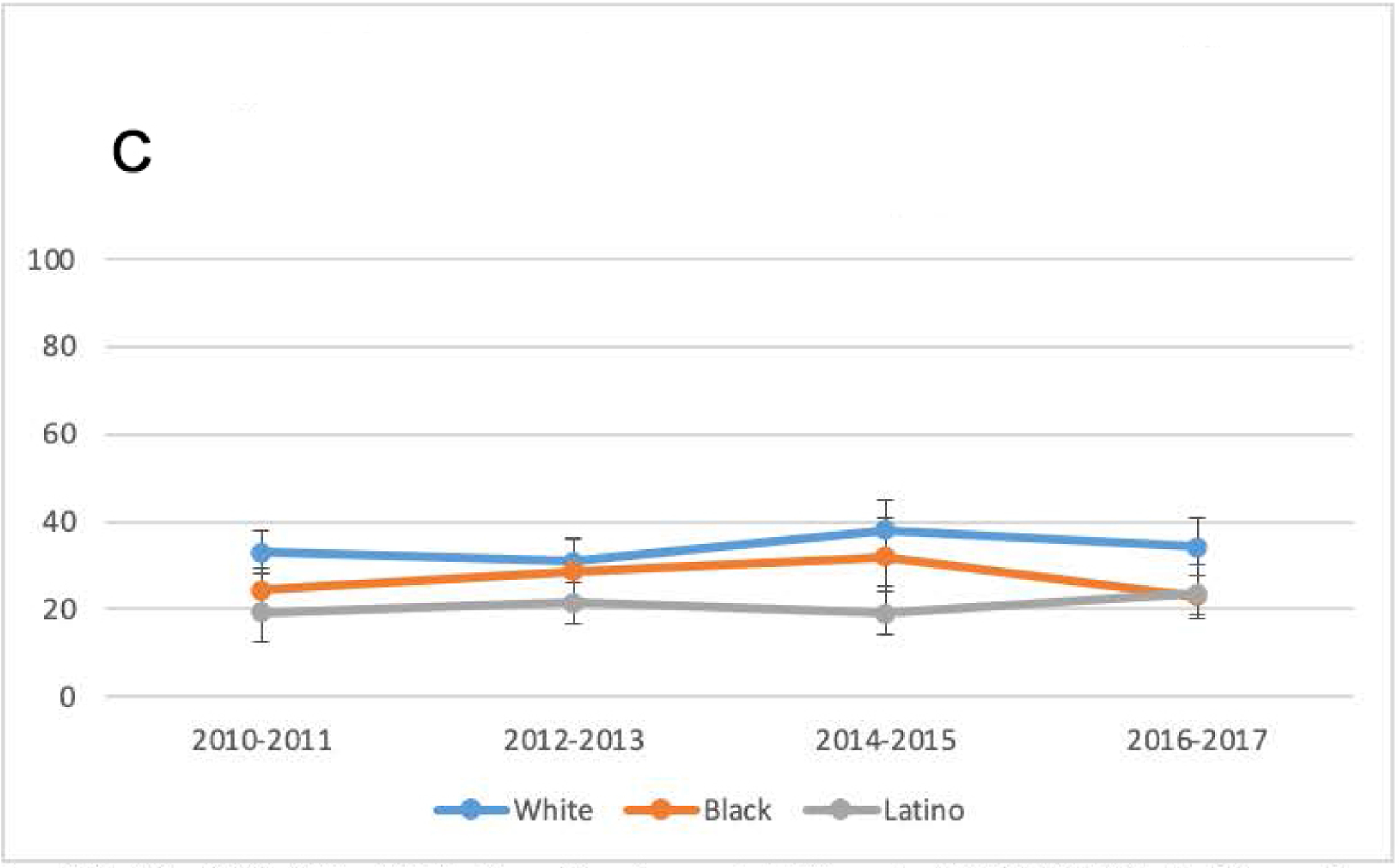
Note: A) Any mental health care use among youths with a need for mental health care by race/ethnicity, 2010 – 2017. B) any outpatient mental health care use among youths with a need for mental health care by race/ethnicity, 2010 – 2017. C) any psychotropic medication use among youths with a need for mental health care by race/ethnicity 2010 – 2017.
Data for A): Youth ages 5–17 from the 2010–2017 Medical Expenditure Panel Survey (MEPS). Any mental health care use is defined as an outpatient provider visit associated with a mental health diagnosis (International Classification Disease (ICD-9) codes 291, 292 or 295–314; ICD-10 codes: F01-F99) or treatment coded as psychotherapy or mental health counseling or a psychotropic medication fill identified through the Multum Medisource Lexicon classification system. The statistical comparison is between the first and last point on the x-axis (2010–11 vs 2016–17). Data for B): Youth ages 5–17 from the 2010–2017 Medical Expenditure Panel Survey (MEPS). Any outpatient mental health care use defined as an outpatient provider visit associated with a mental health diagnosis (International Classification Disease (ICD-9) codes 291, 292 or 295–314; ICD-10 codes: F01-F99) or treatment coded as psychotherapy or mental health counseling. The statistical comparison is between the first and last point on the x-axis (2010–11 vs 2016–17). Data for C): Youth ages 5–17 from the 2010–2017 Medical Expenditure Panel Survey (MEPS). Any psychotropic medication fill was identified through the Multum Medisource Lexicon classification system. The statistical comparison is between the first and last point on the x-axis (2010–11 vs 2016–17).
**p<0.01; ***p<0.001.
Results from our IOM-concordant analysis (Table 2), show that there were Black-White and Latinx-White disparities in both 2010–2011 and 2016–2017 periods for any mental health care use and any outpatient mental health care use. Concerning any psychotropic medication fill, there were Latinx-White disparities for both time-periods and Black-White disparities during the 2016–2017 period. Black-White disparities in any mental health care use and any outpatient mental health care use were significantly exacerbated between 2010–2011 and 2016–2017. All other differences in access disparities over time were non-significant. Among youth with any service use, we identified Black-White disparities in overall mental health care expenditures (2016–2017) and outpatient mental health care expenditures (2010–2011 and 2016–2017). There were no significant differences in Latinx-White disparities for any expenditure outcome at any period. Disparity trends were non-significant for all expenditure measures.
Table 2.
Racial-ethnic disparities in mental health care service use and expenditures among youth (5–17), 2010–2017 Medical Expenditure Panel Survey
| Any mental health care use | SE | Any outpatient mental health care use | SE | Any psychotropic medication use | SE | |
|---|---|---|---|---|---|---|
| Black-White | ||||||
| 2010–2011 | −1.3 | 0.4 | −1.6 | 0.5 | −0.3 | 0.4 |
| 2016–2017 | −3.8 | 0.6 | −3.7 | 0.6 | −1.5 | 0.4 |
| Difference in disparity | −2.5 | 0.8 | −2.1 | 0.8 | −1.1 | 0.6 |
| Latino-White | ||||||
| 2010–2011 | −4.4 | 0.4 | −2.9 | 0.4 | −3.7 | 0.3 |
| 2016–2017 | −4.0 | 0.5 | −3.6 | 0.5 | −2.6 | 0.3 |
| Difference in disparity | 0.4 | 0.70 | −0.7 | 0.60 | 1.1 | 0.50 |
| Mental health expenditures given any use | SE | Outpatient mental health expenditures given any use | SE | Psychotropic medication expenditures given any use | SE | |
| Black-White | ||||||
| 2010–2011 | −87.5 | 110.3 | −239.4 | 71.7 | 25.1 | 147.7 |
| 2016–2017 | −373.1 | 218.5 | −442.1 | 184.4 | 32.3 | 176.0 |
| Difference in disparity | −285.6 | 237.1 | −202.7 | 199.1 | 7.1 | 231.3 |
| Latino-White | ||||||
| 2010–2011 | −243.1 | 113.2 | 80.0 | 99.6 | −223.1 | 197.4 |
| 2016–2017 | −153.2 | 217.5 | 26.0 | 276.2 | −252.6 | 276.4 |
| Difference in disparity | 89.8 | 228.46 | −54.0 | 284.56 | −29.5 | 355.0 |
Bold numbers indicate significance at p<0.05; Standard errors were calculated using balanced repeated replication methods; Results were adjusted for need variables based on the IOM definition: parent-reported mental health and physical health status, Columbia impairment scale, activity limitation, age, and sex
DISCUSSION
Affordable, ubiquitous access to mental health care for youth in need of treatment remains an elusive target in the United States. Using the Medical Expenditure Panel Survey (MEPS), a nationally representative survey of healthcare utilization, we examined trends in mental healthcare utilization among children ages 5–17. In agreement with our hypotheses, overall mental health care use increased between 2010–2011 and 2016–2017, most notably for outpatient mental health care. Increases in overall and outpatient mental health treatment were identified for White and Latinx youth and among the sub-group of youth reporting need for mental health care. Contrary to our hypothesis, Black-White and Latinx-White disparities did not diminish over time. In fact, in analyses adjusting for need, Black-White and Latinx-White disparities in mental health care persisted over time, and in the case of Black-White disparities in any mental health care use and any outpatient mental health care use, these disparities actually worsened over time. For those that did access mental health care, Black-White disparities existed in outpatient mental health care expenditures and these disparities persisted over time.
Enactment of Medicaid and CHIP reforms and parity laws during this time period did not reduce disparities in mental health care use as expected, extending the concerning exacerbation of access disparities seen in analyses of 2006–2012 MEPS data.16,17 Continued expansion of Medicaid and SCHIP eligibility in states with large populations of youth of color could help to reduce disparities. While approximately 50% of children with a mental health disorder have not received care from a mental health professional in the U.S.,40 the rate of unmet need is greater than 53% in 12 Southern and Midwestern states, with rates as high as 72% in North Carolina.40
Similar to a prior study we identified that psychotropic medication use leveled off between 2010 and 2017 for White and Latinx youth, but decreased among Black youth. The benefits of parity laws targeting cost-sharing requirements and treatment limitations appear to not have extended to gains in psychotropic medication use. Future study assessing racial/ethnic differences in factors underlying prescription trends (e.g., changes in utilization management of psychotropic medications, family preferences for medications) would help to better understand these results.
Taken together, these findings suggest that insurance coverage reforms may be necessary but are not sufficient to reduce disparities in access to mental health care for youth in the United States. Three additional areas of reform should be considered to improve access to mental health care for Black and Latinx children. First, efforts should be made to decrease discrimination across the patient care experience (from setting the appointment, to treatment at the front desk, to the patient-provider interaction).41,42 Patient experience of healthcare discrimination have a significant negative impact on subsequent decisions about accessing mental health care. The historical context of racial discrimination and injustice in the United States impacts health and has shaped the mental health care system.43 Mis-treatment, mistrust and inequities have created barriers in the opportunity for Black and Latinx communities to engage with confidence and a sense of safety in the existing, traditional models of psychotropic medication and outpatient mental health care.44–46 Training for providers and administration on the impact of discrimination and existing system-level structure barriers is needed.
Second, more intervention is needed to improve the cultural competence of mental health providers and to expanding the mental healthcare workforce to include more providers of color. The lack of cultural competence of mental health providers is another potential driver of disparities as providers’ failure to understand the values and priorities of youth and their family members are associated with poor retention in mental health care.47,48 This may in part explain the finding that Black youth that did access treatment had lower overall treatment expenditures than White youth. Expanding cultural competence training beyond individual targets (e.g., the provider) to creating value-based payment reforms that hold provider organizations and health plans accountable for reaching disparities reduction or cultural competence metrics is an additional solution.49,50
Lastly, existing traditional mental health services systems may not be meeting the needs of youth of color and may continue to need adaptation and examination. Future research should explore non-traditional mental health care models that engage additional levels of clinical providers. For example, engaging community health worker, peer support and youth peer support service models have not been fully explored as a potential pathway to reducing disparities in access.51–54 Leveraging new models of meeting with patients that overcome obstacles of transportation and conflicts with school and job responsibilities should also be explored. Telehealth has been used widely and covered by most insurance plans during the COVID-19 pandemic. Future researchers should investigate the impact of this change in modality of treatment on disparities in mental health care. Telepsychiatry represents an opportunity for improving access to treatment (e.g., by reducing the transportation, time off employment, and child care needed for parents to take their child to a visit) but also new barriers such as unreliable three-way video call interpretation, youth privacy, lack of access to internet-enabled devices (e.g., computer, tablet, or smartphone) and reliable internet connectivity/subscription.
In the advent of the recent acute awareness of the national and deleterious impact of racism in the United States, exacerbated by the disproportionate impact of the COVID-19 pandemic on Black and Latinx communities, the need for mental health care has greatly increased. The COVID-19 pandemic has generated non-traditional formats (e.g., insurance-covered telehealth). Taking the opportunity to further expand the existing mental health system and accompanying policies that reach beyond the status quo is required to address persistent disparities in access and utilization of mental health care, especially for Black youth.
The present findings should be considered in the context of several limitations. First, these data do not allow for the differentiation of mental health service overuse or underuse in access and expenditure analyses. Regression models adjust for mental health status but do not rule out the possibility that disparities are driven by overuse of White youth. Second, we do not have information on the ethnic diversity of the youth represented in this data (e.g., for Black and Latinx families). Third, we did not include a measure of patient preference in our analysis, which is to be adjusted for according to the IOM definition of healthcare disparity. However, fully informed preferences are difficult to elicit and may be influenced by prior experiences of discrimination.44 Fourth, not all school-based mental health services are captured in the MEPS dataset. It is likely that these missing data lead to an undercount of mental health care use. However, it is likely to bias our disparity estimates downward as school-based mental health care racial/ethnic disparities have shown to be persistent and pervasive in school-based settings.55 Lastly, our sample consists of noninstitutionalized U.S youth and does not include those in juvenile detention centers or in group homes (e.g. residential child-care communities).
There is an abundance of existing literature identifying disparities and challenges in access to and utilization of mental health care for Black and Latinx communities. However, this study suggests that existing policy changes regarding insurance coverage and access for mental health care has not yielded the impact anticipated in decreasing or eliminating these disparities. Our findings show that, despite significant insurance reforms between 2012 and 2017, there continues to be challenges and barriers to providing equitable and accessible mental health care to Black and Latinx youth in the United States.
Acknowledgments
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health (Grant No. P50 MH126283), principal investigators Benjamin Lê Cook and Philip Wang.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Rodgers, Flores, Lê Cook, Mr. Bassey, and Ms. Augenblick have reported no biomedical financial interests or potential conflicts of interest.
References
- 1.Erskine HE, Moffitt TE, Copeland WE, et al. A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol Med. 2015;45(7):1551–1563.doi: 10.1017/S0033291714002888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glied S, Cuellar AE. Trends and issues in child and adolescent mental health. Health affairs. 2003;22(5):39–50. doi: 10.1377/htlthaff.22.5.39 [DOI] [PubMed] [Google Scholar]
- 3.Alegria M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child and Adolescent Psychiatric Clinics. 2010;19(4):759–774. doi.org/ 10.1016/j.chc.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olfson M, Blanco C, Wang S, Laje G, Correll CU. National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry. 2014;71(1):81–90. doi: 10.1001/jamapsychiatry.2013.3074. [DOI] [PubMed] [Google Scholar]
- 5.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and Treatment of Depression, Anxiety, and Conduct Problems in US Children. The Journal of Pediatrics. 2019;206:256–267.e253. doi.org/10/1016/j.jpeds.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Center for Disease Control and Prevention. Mental Health Surveillance Among Children United States, 2005 – 2011. Morbidity and Mortality Weekly Report. 2013;62:1–40.23302815 [Google Scholar]
- 7.Duong MT, Bruns EJ, Lee K, et al. Rates of Mental Health Service Utilization by Children and Adolescents in Schools and Other Common Service Settings: A Systematic Review and Meta-Analysis. Administration and Policy in Mental Health and Mental Health Services Research. 2021;48(3):420–439. doi: 10.1007/s10488-020-01080-9. [DOI] [PubMed] [Google Scholar]
- 8.Chirdkiatgumchai V, Xiao H, Fredstrom BK, et al. National trends in psychotropic medication use in young children: 1994–2009. Pediatrics. 2013;132(4):615–623. doi: 10.1542/pedis.2013-1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jonas B, Gu Q, Albertorio-Diaz J. Psychotropic Medication use among adolescents: United States, 2005 – 2010. NCHS Data Brief. 2013;(135): 1–8. [PubMed] [Google Scholar]
- 10.Cook BL, Carson NJ, Kafali EN, et al. Examining psychotropic medication use among youth in the U.S. by race/ehnicity and psychological impairment. General Hospital Psychiatry. 2017;45:32–39. doi.org/ 10.1016/j-genhosppsych.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simon AE, Pastor PN, Reuben CA, Huang LN, Goldstrom ID. Use of Mental Health Services by Children Ages Six to 11 With Emotional or Behavioral Difficulties. Psychiatric Services. 2015;66(9):930–937. doi: 10.1176/appi.ps.201400342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Costello EJ, He JP, Sampson NA, Kessler RC, Merikangas KR. Services for adolescents with psychiatric disorders: 12-Month data From the National Comorbidity Survey -Adolescent. Psychiatric Services. 2014;65(3):359–366. doi: 10.1176/appi.ps.201100518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cook BL, Hou SS-Y, Lee-Tauler SY, Progovac AM, Samson F, Sanchez MJ. A Review of Mental Health and Mental Health Care Disparities Research: 2011–2014. Medical Care Research and Review. 2019;76(6):683–710. doi: 10.1177/1077558718780592. [DOI] [PubMed] [Google Scholar]
- 14.Saloner B, Carson N, Cook BL. Episodes of Mental Health Treatment Among a Nationally Representative Sample of Children and Adolescents. Medical Care Research and Review. 2014;71(3):261–279. doi: 10.1177/1077558713518347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cummings JR, Ji X, Lally C, Druss BG. Racial and Ethnic Differences in Minimally Adequate Depression Care Among Medicaid-Enrolled Youth. Journal of the American Academy of Child & Adolescent Psychiatry. 2019;58(1):128–138. doi: 10.1016/j.jaac.2018.04.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marrast L, Himmelstein DU, Woolhandler S. Racial and Ethnic Disparities in Mental Health Care for Children and Young Adults: A National Study. Int J Health Serv. 2016;46(4):810–824. doi: 10.1177/0020731416662736 [DOI] [PubMed] [Google Scholar]
- 17.Cook BL, Barry CL, Busch SH. Racial/Ethnic Disparity Trends in Children’s Mental Health Care Access and Expenditures from 2002 to 2007. Health Services Research. 2013;48(1):129–149. doi.org/ 10.1111/j.1475-6773.2012.01439.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.HealthCare.gov. Federal Poverty Level (FPL). https://www.healthcare.gov/glossary/federal-poverty-level-fpl/. Published 2021. Accessed2021.
- 19.Cheng TL, Wise PH, Halfon N. Promise and Perils of the Affordable Care Act for Children. JAMA. 2014;311(17):1733–1734.doi: 10.1001/jama.2014.930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas KC, Shartzer A, Kurth NK, Hall JP. Impact of ACA Health Reforms for People With Mental Health Conditions. Psychiatr Serv. 2018;69(2):231–234. doi.org/ 10.1176/appi/ps.201700044 [DOI] [PubMed] [Google Scholar]
- 21.Dougherty D, Schiff J, Mangione-Smith R. The Children’s Health Insurance Program Reauthorization Act Quality Measures Initiatives: Moving Forward to Improve Measurement, Care, and Child and Adolescent Outcomes. Academic Pediatrics. 2011;11(3, Supplement):S1–S10. doi: 10.1016/j.acap.2011.02.009 [DOI] [PubMed] [Google Scholar]
- 22.Zima BT, Murphy JM, Scholle SH, et al. National Quality Measures for Child Mental Health Care: Background, Progress, and Next Steps. Pediatrics. 2013;131(Supplement 1):S38–S49. doi: 10.1542/peds.2012-1427e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hales CM, Kit BK, Gu Q, Ogden CL. Trends in Prescription Medication Use Among Children and Adolescents—United States, 1999–2014. JAMA. 2018;319(19):2009–2020. doi: 10.1001/jama.2018.5690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality. https://www.meps.ahrq.gov/mepsweb/data_stats/download_data_files_detail.jsp?cboPufNumber=HC-201. Published 2019. [DOI] [PubMed]
- 25.Machlin S, Cohen J, Elixhauser A, Beauregard K, Steiner C. Sensitivity of Household Reported Medical Conditions in the Medical Expenditure Panel Survey. Medical Care. 2009;47(6):618–625.doi: 10.1097/MLR.0b013e318195fa79 [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine (US) Committee on Understanding and Eliminating Racail and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US);2003. [PubMed] [Google Scholar]
- 27.Cook BL, McGuire TG, Zaslavsky, Alan M. Measuring Racial/Ethnic Disparities in Health Care: Methods and Practical Issues. Health Services Research. 2012;47(3 Pt 2):1232–1254.doi: 10.1111/j.1475-6773.2012.01387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bird HR, Andrews H, Schwab-Stone M, et al. Global measures of impairment for epidemiologic and clinical use with children and adolescents. International Journal of Methods in Psychiatric Research. 1996;6(4):295–307. [Google Scholar]
- 29.McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: a meta-analysis. Journal of Developmental & Behavioral Pediatrics. 2001;22(6):430–439. [DOI] [PubMed] [Google Scholar]
- 30.Stevens J, Harman JS, Kelleher KJ. Race/ethnicity and insurance status as factors associated with ADHD treatment patterns. Journal of Child & Adolescent Psychopharmacology. 2005;15(1):88–96. doi.org/ 10.1089/cap.2005.15.88 [DOI] [PubMed] [Google Scholar]
- 31.Kataoka SH, Zhang L, Wells KB. Unmet Need for Mental Health Care Among U.S. Children: Variation by Ethnicity and Insurance Status. American Journal of Psychiatry. 2002;159(9):1548–1555. doi: 10.1176/appi.ajp.159.9.1548 [DOI] [PubMed] [Google Scholar]
- 32.McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care. Health Services Research. 2006;41(5):1979–2005. doi: 10.1111/j.1475-6773.2006.00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cook BL, McGuire TG, Zuvekas SH. Measuring Trends in Racial/Ethnic Health Care Disparities. Medical Care Research and Review. 2009;66(1):23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cook BL, McGuire TG, Lock K, Zaslavsky AM. Comparing methods of racial and ethnic disparities measurement across different settings of mental health care. Health services research. 2010;45(3):825–847. doi: 10.1111/j.1475-6773.2010.01100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deb P, Norton EC. Modeling Health Care Expenditures and Use. Annual Review of Public Health. 2018;39(1):489–505. doi.org/ 10.1146/annurev-publhealth-040617-013517. [DOI] [PubMed] [Google Scholar]
- 36.Wooldridge JM. Econometric analysis of cross section and panel data. MIT press; 2010. [Google Scholar]
- 37.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. [DOI] [PubMed] [Google Scholar]
- 38.Efron B, Tibshirani R. Bootstrap Methods for Standard Errors, Confidence Intervals, and Other Measures of Statistical Accuracy. Statistical Science. 1986;1(1):54–75. [Google Scholar]
- 39.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StatCorp LP; 2017. [Google Scholar]
- 40.Whitney DG, Peterson MD. US National and State-Level Prevalence of Mental Health Disorders and Disparities of Mental Health Care Use in Children. JAMA Pediatrics. 2019;173(4):389–391. doi: 10.1001/jamapediatrics.2018.5399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Progovac AM, Cortés DE, Chambers V, et al. Understanding the Role of Past Health Care Discrimination in Help-Seeking and Shared Decision-Making for Depression Treatment Preferences. Qualitative Health Research. 2020;30(12):1833–1850. doi: 10.1177/1049732320937663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sonik RA, Creedon TB, Progovac AM, et al. Depression treatment preferences by race/ethnicity and gender and associations between past healthcare discrimination experiences and present preferences in a nationally representative sample. Social Science & Medicine. 2020:112939. doi.org/ 10.1016/j.socscimed.2020.112939 [DOI] [PubMed] [Google Scholar]
- 43.Hausmann LRM, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and health status in a racially diverse sample. Medical care. 2008;46(9):905–914. doi: 10.1097/MLR.0b013e3181792562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alang SM. Mental health care among blacks in America: Confronting racism and constructing solutions. Health Services Research. 2019;54(2):346–355. doi: 10.1111/1475-6773.13115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annual review of public health. 2019;40:105–125. doi: 10.1146/annurev-pubhealth-040218-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams DR, Lawrence JA, Davis BA, Vu C. Understanding how discrimination can affect health. Health Services Research. 2019;54:1374–1388. doi.org/ 10.111/1475-6773.13222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Butler AM, Rodgers CRR. Developing a Policy Brief on Child Mental Health Disparities to Promote Strategies for Advancing Equity among Racial/Ethnic Minority Youth. Ethn Dis. 2019;29(Suppl 2):421–426. doi: 10.18865/ed.29.S2.421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valdez CR, Rodgers CRR, Gudiño OG, et al. Translating research to support practitioners in addressing disparities in child and adolescent mental health and services in the United States. Cultural Diversity and Ethnic Minority Psychology. 2019;25(1):126–135. doi.org/ 10.1037/cdp0000257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fung K, Lo H-T, Srivastava R, Andermann L. Organizational cultural competence consultation to a mental health institution. Transcultural psychiatry. 2012;49(2):165–184. doi.org/ 10.1177/1363461512439740 [DOI] [PubMed] [Google Scholar]
- 50.Schouler-Ocak M, Graef-Calliess IT, Tarricone I, Qureshi A, Kastrup MC, Bhugra D. EPA guidance on cultural competence training. European Psychiatry. 2015;30(3):431–440. doi: 10.1016/j.eurpsy.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 51.Bellamy C, Schmutte T, Davidson L. An update on the growing evidence base for peer support. Mental Health and Social Inclusion. 2017. [Google Scholar]
- 52.Gagne CA, Finch WL, Myrick KJ, Davis LM. Peer workers in the behavioral and integrated health workforce: opportunities and future directions. American journal of preventive medicine. 2018;54(6):S258–S266. doi.org/ 10.1016/j.amepre.2018.03.010 [DOI] [PubMed] [Google Scholar]
- 53.Gopalan G, Lee SJ, Harris R, Acri MC, Munson MR. Utilization of peers in services for youth with emotional and behavioral challenges: A scoping review. Journal of adolescence. 2017;55:88–115.doi: 10.1016/j.adolescence.2016.12.011 [DOI] [PubMed] [Google Scholar]
- 54.Barnett ML, Gonzalez A, Miranda J, Chavira DA, Lau AS. Mobilizing community health workers to address mental health disparities for underserved populations: A systematic review. Administration and Policy in Mental Health and Mental Health Services Research. 2018;45(2):195–211. doi: 10.1007/s10488-017-0815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Locke J, KangYi CD, Pellecchia M, Marcus S, Hadley T, Mandell DS. Ethnic disparities in schoolbased behavioral health service use for children with psychiatric disorders. Journal of School Health. 2017;87(1):47–54. doi: 10.1111/josh.12469 [DOI] [PMC free article] [PubMed] [Google Scholar]


