Abstract
Cancer is the most common malignant tumor of the endocrine glands and comprises 1% of all malignant cancers and its incidence is still increasing. No comprehensive study summarizing the results of these studies was found. Therefore, this study aimed to determine the prevalence of thyroid cancer in Iran in a systematic review and meta-analysis. In this review, studies were extracted by searching the national and international databases of SID, MagIran, IranMedex, IranDoc, and Google Scholar, Cochrane, Embase, ScienceDirect, Scopus, PubMed, and Web of Science (WoS) from 1997 to September 2019. Simple random effects model was used for data analysis and heterogeneity of studies was investigated with I2 index. Data were analyzed using Comprehensive Meta-Analysis (version 2) software. In 28 reviewed articles, the prevalence of thyroid cancer in Iran was reported to be 3.5% with a sample size of 100,869 (95% CI: 2.7–4.4%). Regarding heterogeneity on the basis of meta-regression, there was no significant difference between the effect of the year of study (P = 0.531) and sample size (P = 0.864) and the prevalence of thyroid cancer in Iran. The results of this study indicated that the prevalence of thyroid cancer is high in Iran. Therefore, appropriate strategies should be put in place by providing feedback to hospitals in order to improve the aforementioned situation, and troubleshoot and monitor at all levels.
Keywords: Cancer, Thyroid, Prevalence, Meta-analysis
Background
Thyroid cancer is the most common form of endocrine cancers, which accounts for about 1% of malignant cancers (about 0.5% of men’s cancers and 1.5% of women’s cancers) and its incidence continues to increase [1, 2]. Thyroid cancer includes papillary (75–85%), follicular (10–20%), medullary (5%), and anaplastic (less than 5%) cancers [3].
Anaplastic thyroid cancer (ATC) is one of the most invasive types of clinical epithelial tumors and one of the most deadly human tumors. This type of cancer accounts for less than 5% of clinical thyroid cancers and more than half of all thyroid cancers with a death rate of 90% of patients, and the median survival of patients is about 6 months after diagnosis. It affects the elderly with an average age of 60 years, most of whom are women [4]. Recent advances in understanding the genetic and molecular pathogenesis of thyroid cancer have increased patients’ hope for treatment [5].
In a study conducted in the Cancer Institute of Iran, the prevalence of thyroid cancer was 76.1% of all endocrine cancers [6–9], of which 28.6% was diagnosed after metastasis [10–12]. The incidence rate of thyroid cancer has increased faster than any other malignancy in recent years, and increased incidence has been seen in both sexes and across races [13–17]. Given the influence of various factors on thyroid prevalence and the lack of general statistics on this issue throughout Iran, we decided to review the studies conducted in this area and to statistically analyze the results of these studies in order to compile an overall statistics on the prevalence of thyroid cancer in Iran and open a window into more precise planning to decrease the complications of thyroid cancer.
Methods
In this systematic review and meta-analysis, the prevalence of thyroid cancer in Iran was investigated based on the studies conducted in this area with no time limit (until September 2019). To this end, articles published in the national databases of SID, MagIran, IranMedex, and IranDoc, and international databases of Google Scholar, Cochrane, Embase, ScienceDirect, Scopus, PubMed, and Web of Science (WoS) were searched using Persian and English keywords such as Prevalence, Cancer, Thyroid, and Iran.
The criteria for selecting the studies were being observational (non-interventional studies) and full text availability. For more information, the reference section of the reviewed articles was also reviewed for access to other articles.
Selection of Studies
Initially, all articles referred to the prevalence of thyroid cancer in Iran were collected by researchers and accepted based on the inclusion and exclusion criteria. Exclusion criteria included unrelated cases, case reports, interventional studies, duplicate studies, unclear methodology, and full text unavailability. In order to reduce bias, the articles were searched independently by two researchers, and if they disagreed on an article, it was judged by the group supervisor. A total of 34 studies entered the third stage, qualitative evaluation.
Qualitative Evaluation of the Studies
The quality of the articles was evaluated based on the selected and related items of the STROBE checklist with 22 items that were measurable in this study (study design, background and literature review, place and time of study, outcome, inclusion criteria, sample size, and statistical analysis (and mentioned in the previous studies as well. Articles referring to 6 to 7 criteria were considered high-quality articles, and articles that did not mention 2 items and more than 2 items from the seven items were considered moderate- and low-methodological-quality articles, respectively [18].
Statistical Analysis
In order to evaluate the heterogeneity of the selected studies, the Egger test at significance level of 0.05 was used to investigate the publication bias, and with regard to the high volume of samples entered into the study, the Begg and Mazumdar test at the significant level of 0.1 and its corresponding Funnel plot were also used. Sensitivity analysis was used to evaluate the effect of individual studies on the final result. Meta-regression was used to investigate the relationship between the prevalence of thyroid cancer and the year of the study and sample size. Data were analyzed using Comprehensive Meta-Analysis (version 2) software. For geographical study of the prevalence of thyroid cancer in Iran, the information extracted from the meta-analysis was entered into Arc map (ArcGIS 10.3) software and the prevalence of thyroid cancer in Iran was reported using maps drawn by the software.
Results
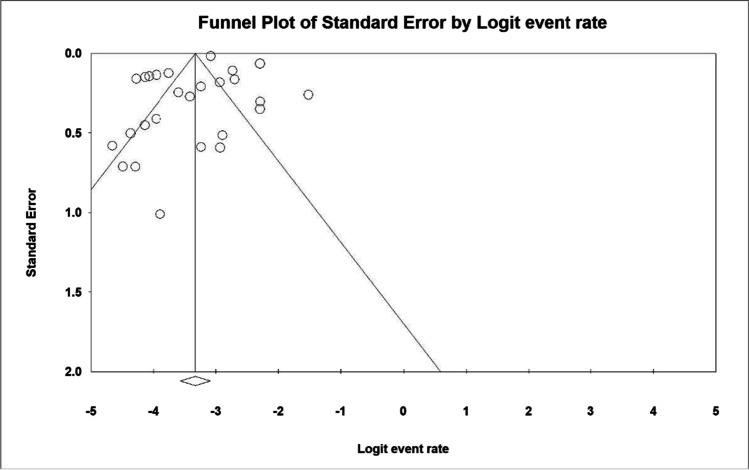
The possibility of publication bias in results was evaluated by the Funnel plot and the Egger test (Fig. 1) which showed that the dissemination bias was not statistically significant (0.256). Also, the results of the Begg and Mazumdar test at the significant level of 0.1 indicated no publication bias in the present study (P = 0.678).
Fig. 1.
Funnel plot of the results of the prevalence of thyroid cancer in Iran
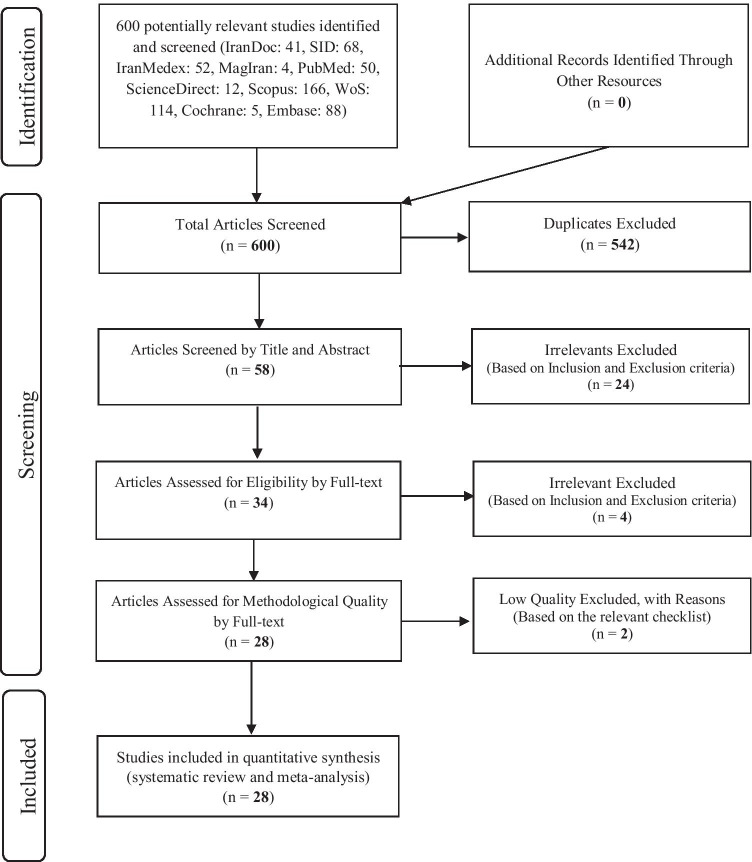
In this study, all studies regarding the prevalence of thyroid cancer in Iran were systematically reviewed according to PRISMA guidelines with no time limitation. In the initial search, 600 articles were identified that eventually 28 studies published from 1997 to September 2019 entered the final analysis (Fig. 2).
Fig. 2.
Flow diagram of study selection
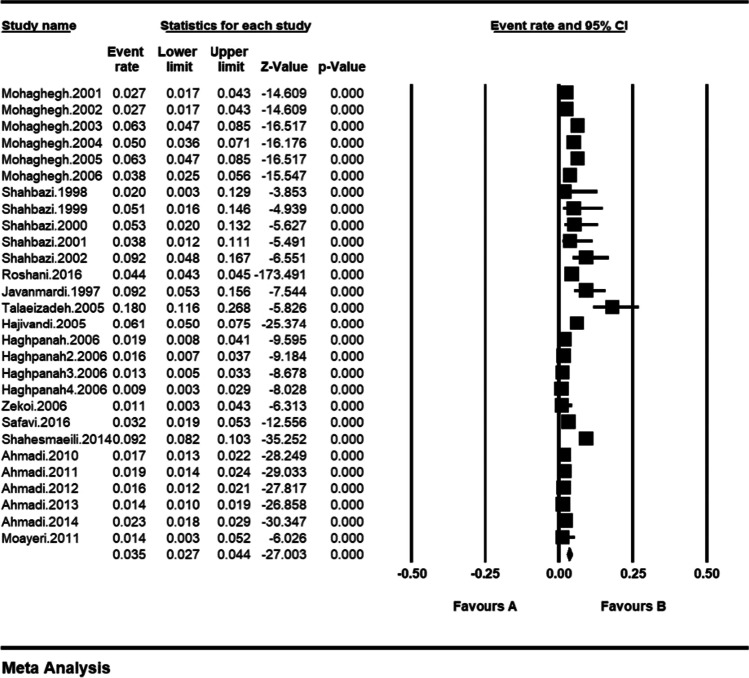
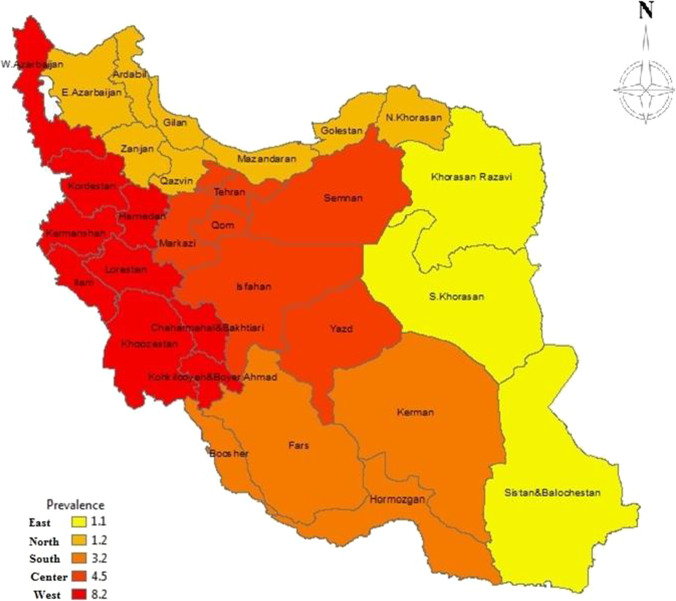
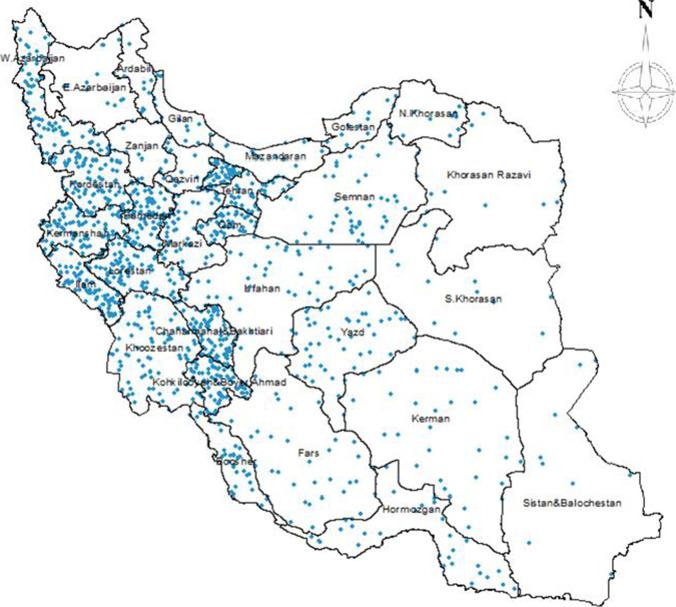
Based on the results of the (I2: 94.4) test and due to the heterogeneity of the selected studies, the random effects model was used to combine the studies and for the joint prevalence estimation. The total sample size was 100,869 individuals with the mean age of sample in each study. The specifications of the selected articles are presented in Table 1. The lowest and highest sample sizes were related to the studies by Shahbazi et al. (50 individuals) [22] and Roshani et al. (75,500 individuals) [25], respectively, and the highest and lowest prevalence of thyroid cancer in Iran were associated with the studies by Talaeizadeh et al. [27] and Haghpanah et al. [29], respectively. According to the results of this study, the overall prevalence of thyroid cancer in Iran was 3.5% (95% CI: 2.7–4.4%) (Fig. 3). Prevalence of thyroid cancer in Iran was reported based on different geographical areas in Iran and according to the Geographical Information System (GIS) (Fig. 4) and by hot dots in different provinces (Fig. 5). Accordingly, it reports a higher prevalence of thyroid cancer in the West as well as in central Iran.
Table 1.
Characteristic of included studies, prevalence of thyroid cancer
| Author, year, reference | Mean age (years) | City | Sample size | Sample size (male) | Sample size (female) | Prevalence % | Prevalence (male) | Prevalence (female) | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Moayeri, 2001, [19] | 10.9 | Tehran | 148 | 92 | 56 | 1.4 | - | - | High |
| Safavi, 2016, [20] | 45 | Tehran | 438 | - | - | 3.2 | - | - | High |
| Zekoi, 2006, [21] | 47.5 | Khorasan | 180 | 108 | 72 | 1.1 | - | - | Medium |
| Shahbazi, 1998, [22] | 51.14 | Shahrekord | 50 | - | - | 2.0 | - | - | High |
| Shahbazi, 1999, [22] | - | Shahrekord | 59 | - | - | 5.1 | - | - | High |
| Shahbazi, 2000, [22] | - | Shahrekord | 76 | - | - | 5.3 | - | - | High |
| Shahbazi, 2001, [22] | - | Shahrekord | 79 | - | - | 3.8 | - | - | High |
| Shahbazi, 2002, [22] | - | Shahrekord | 98 | - | - | 9.2 | - | - | High |
| Mohaghegh, 2006, [23] | - | Markazi | 634 | 375 | 259 | 3.8 | 4 | 20 | High |
| Mohaghegh, 2005, [23] | 57.3 | Markazi | 634 | 375 | 259 | 6.3 | 10 | 30 | High |
| Mohaghegh, 2004, [23] | - | Markazi | 634 | 375 | 259 | 5.0 | 8 | 24 | High |
| Mohaghegh, 2003, [23] | - | Markazi | 634 | 375 | 259 | 6.3 | 14 | 26 | High |
| Mohaghegh, 2002, [23] | - | Markazi | 634 | 375 | 259 | 2.7 | 4 | 13 | High |
| Mohaghegh, 2001, [23] | 60.9 | Markazi | 634 | 375 | 259 | 2.7 | 4 | 13 | High |
| Shahesmaeili, 2014, [24] | 60 | Kerman | 2838 | 1544 | 1294 | 9.2 | 142 | 119 | High |
| Roshani, 2016, [25] | 68 | Iranian elderly | 75,500 | 40,241 | 35,259 | 4.4 | - | - | Medium |
| [26] | - | Kashan | 130 | 112 | 18 | 9.2 | 2 | 10 | High |
| Talaeizadeh, 2005, [27] | - | Ahvaz | 100 | 8 | 92 | 18 | - | - | High |
| Hajivandi, 2005, [28] | - | Bushehr | 1503 | 646 | 857 | 6.1 | 48 | 44 | Medium |
| Haghpanah1, 2006, [29] | - | Kerman | 319 | 167 | 152 | 1.9 | 2 | 4 | High |
| Haghpanah2, 2006, [29] | - | Mazandaran | 319 | 167 | 152 | 1.6 | 2 | 3 | High |
| Haghpanah3, 2006, [29] | - | Gilan | 319 | 167 | 152 | 1.3 | 1 | 3 | High |
| Haghpanah4, 2006, [29] | - | Golestan | 319 | 167 | 152 | 0.9 | 1 | 2 | High |
| Ahmadi, 2010, [30] | - | Southwest | 2918 | 1735 | 1183 | 1.7 | - | - | High |
| Ahmadi, 2011, [30] | - | Southwest | 2918 | 1735 | 1183 | 1.9 | - | - | High |
| Ahmadi, 2012, [30] | - | Southwest | 2918 | 1735 | 1183 | 1.6 | - | - | High |
| Ahmadi, 2013, [30] | - | Southwest | 2918 | 1735 | 1183 | 1.4 | - | - | High |
| Ahmadi, 2014, [30] | - | Southwest | 2918 | 1735 | 1183 | 2.3 | - | - | High |
Fig. 3.
Prevalence of thyroid cancer and 95% confidence interval in Iran. The midpoint of each line segment shows the prevalence of thyroid cancer in each study, and the diamond figure shows the prevalence of thyroid cancer in Iran for the all studies
Fig. 4.
Overall prevalence o of thyroid cancer in Iran based on ArcGIS 10.3 by geographical areas (the figure was drawn by the software and was not extracted from another source)
Fig. 5.
Overall prevalence of thyroid cancer in Iran based on the Arc Map by using hot dots (the figure was drawn by the software and was not extracted from another source)
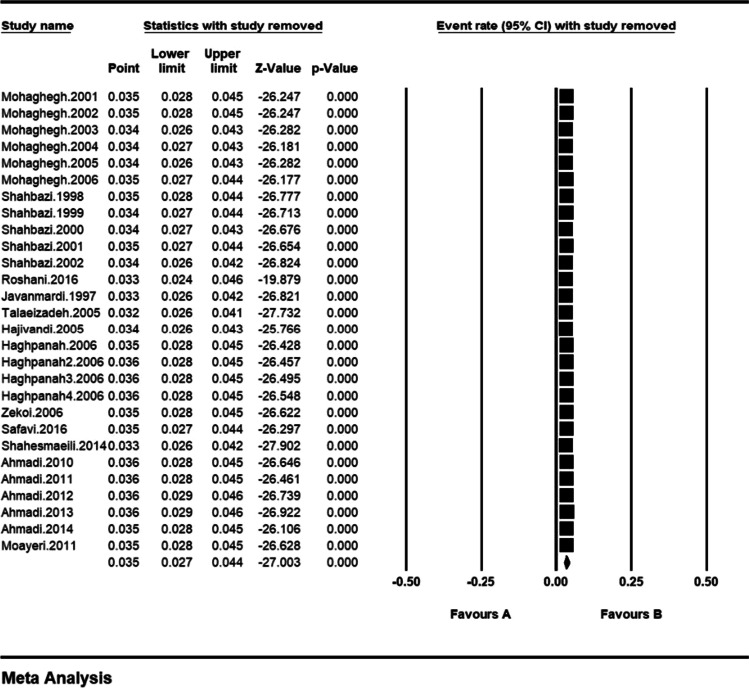
Sensitivity analysis was performed based on Fig. 4 to ensure the stability of the study results, and after removing any of the results of the included studies, the overall result of meta-analysis did not change (Fig. 6).
Fig. 6.
Results of sensitivity analysis
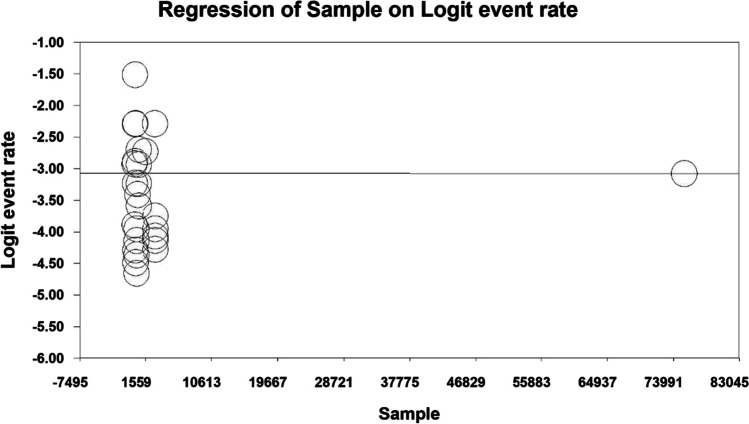
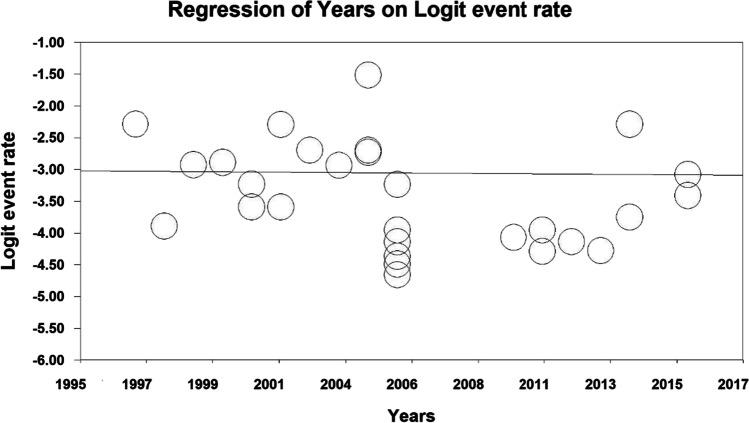
The relationship between the year of study (P = 0.531) and sample size (P = 0.864) and the prevalence of thyroid cancer in Iran was evaluated using meta-regression. There was no significant difference between the prevalence of thyroid cancer and the two abovementioned items (Figs. 7 and 8).
Fig. 7.
Meta-regression of the relationship between the sample size and the prevalence of thyroid cancer in Iran
Fig. 8.
Meta-regression of the relationship between the year of study and the prevalence of thyroid cancer in Iran
Discussion
According to studies conducted in Southwest Asian countries, the prevalence of thyroid cancer is reported to be 1.1 to 3.5% in men and 2.6 to 12.1% in women [31]. Given the incidence rate of 3.5% in this study, it seems that our country is located in the middle of the areas with maximum prevalence and minimum prevalence.
Thyroid cancer is of medium importance but is recognized as the second most common cancer in women in Southwest Asia countries. Since there is no population-based thyroid cancer screening program in most Asian countries, most patients have advanced thyroid cancer. Most Asian countries are low- and middle-income countries with limited access to effective care. Due to late diagnosis and inadequate access to care, survival of people with thyroid cancer in Asia is lower than in Western countries. Improvement of thyroid cancer in most Asian countries remains a challenge that can be addressed by the cooperation of various sectors, including public and private sectors [31].
In our study, thyroid cancer was less prevalent in individuals under 14 years of age [19], and the highest prevalence of thyroid cancer was associated with Talaeizadeh et al.’s study with an average age of 45 years [27]. In most studies in Iran, the mean age for both sexes is included in the age group of 50–40 years [20–22 and 27]. In a study carried out by Larijani et al. (1998–2001) in all provinces of Iran, the highest incidence rate was in the age group of 45–55 years for women and 55–65 years for men, and the incidence rate had increased in both sexes after 65 years of age [31–33]. In Saudi Arabia, the highest incidence rate of thyroid cancer was reported in women aged 30–39 years, which is significantly different from the results of the present study [32].
The National Cancer Registry System of Iran, the site for collecting and analyzing cancer information, is the center for disease management and it receives data on cancer patients through the city and province health centers. In recent years, the National Cancer Registry System in Iran has faced many difficulties in collecting information and data from cancer patients, such that the center for disease management in those years has not been able to provide accurate statistics on the incidence of cancer in the country. But the cancer registry has worked well in recent years and believes that on average, up to 80% of cancers in the country are registered today. The data recorded in the Hospital-based Cancer Registry system of Iran are incomplete and more limited to individual characteristics and tumor identification. Therefore, it is recommended to conduct necessary research in order to provide a proper registration system so that with the use of more accurate and complete information, more effective steps can be taken to better understand the disease, to identify the factors affecting the disease, and to reduce the mortality [33].
Conclusion
The results of this study showed that the prevalence of thyroid cancer in Iran is high. Therefore, appropriate strategies should be put in place by providing feedback to hospitals in order to improve the aforementioned situation, and troubleshoot and monitor at all levels.
Acknowledgements
The authors thank the Student Research Committee, Kermanshah University of Medical Sciences.
Abbreviations
- SID
Scientific Information Database
- STROBE
Strengthening the Reporting of Observational Studies in Epidemiology for cross-sectional Study
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
Author Contribution
MK and NS contributed to the design and MM to statistical analysis and participated in most of the study steps. MK and MM prepared the manuscript. MK and MM assisted in designing the study, and helped in the interpretation of the study. All authors have read and approved the content of the manuscript.
Funding
By deputy of research and technology, Kermanshah University of Medical Sciences (980794). The deputy of research and technology, Kermanshah University of Medical Sciences, had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of Data and Materials
Datasets are available through the corresponding author upon reasonable request.
Declarations
Ethics Approval and Consent to Participate
Ethics approval was received from the Ethics Committee of deputy of research and technology, Kermanshah University of Medical Sciences. Reference Number: IR.KUMS.REC.1398.856.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nader Salari, Email: n_s_514@yahoo.com.
Mohsen Kazeminia, Email: mohsenkaz221@gmail.com.
Masoud Mohammadi, Email: Masoud.mohammadi1989@yahoo.com.
References
- 1.Livolsi VA. Papillary thyroid carcinoma: an update. Mod Pathol. 2011;24:1–9. doi: 10.1038/modpathol.2010.129. [DOI] [PubMed] [Google Scholar]
- 2.Schweppe RE. Thyroid cancer cell lines: critical models to study thyroid cancer biology and new therapeutic targets. Front Endocrinol. 2012;3:81. doi: 10.3389/fendo.2012.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li M, Milas M, Nasr C, Brainard JA, Khan MJ, Burkey BB, Scharpf J. Anaplastic thyroid cancer in young patients: a contemporary review. Am J Otolaryngol. 2013;34(6):636–640. doi: 10.1016/j.amjoto.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Hundahl SA, Fleming ID, Fremgen AM, Menck HR. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the US, 1985–1995. Cancer: Interdisciplinary International Journal of the American Cancer Society. 1998;83(12):2638–2648. doi: 10.1002/(SICI)1097-0142(19981215)83:12<2638::AID-CNCR31>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 5.Nagaiah G, Hossain A, Mooney CJ, Parmentier J, Remick SC (2011) Anaplastic thyroid cancer: a review of epidemiology, pathogenesis, and treatment. J Oncol 2011:542358 [DOI] [PMC free article] [PubMed]
- 6.Deandrea M, Gallone G, Veglio M, Balsamo A, Grassi A, Sapelli S, Rossi C, Nasi R, Porcellana V, Varvello G. Thyroid cancer histotype changes as observed in a major general hospital in a 21-year period. J Endocrinol Invest. 1997;20(2):52–58. doi: 10.1007/BF03347976. [DOI] [PubMed] [Google Scholar]
- 7.Reynolds P, Elkin EP, Layefsky ME, Lee GM. Cancer in California school employees, 1988–1992. Am J Ind Med. 1999;36(2):271–278. doi: 10.1002/(SICI)1097-0274(199908)36:2<271::AID-AJIM6>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 8.Coard K. The pathology of thyroid neoplasms at the University Hospital of the West Indies. A 10-year analysis. The West Indian medical journal. 1997;46(3):80–82. [PubMed] [Google Scholar]
- 9.Verkooijen HM, Fioretta G, Pache J-C, Franceschi S, Raymond L, Schubert H, Bouchardy C. Diagnostic changes as a reason for the increase in papillary thyroid cancer incidence in Geneva. Switzerland Cancer Causes & Control. 2003;14(1):13–17. doi: 10.1023/A:1022593923603. [DOI] [PubMed] [Google Scholar]
- 10.Bacher-Stier C, Riccabona G, Tötsch M, Kemmler G, Oberaigner W, Moncayo R. Incidence and clinical characteristics of thyroid carcinoma after iodine prophylaxis in an endemic goiter country. Thyroid. 1997;7(5):733–741. doi: 10.1089/thy.1997.7.733. [DOI] [PubMed] [Google Scholar]
- 11.Haghpanah V, Soliemanpour B, Heshmat R, Mosavi-Jarrahi AR, Tavangar SM, Malekzadeh R, Larijani B (2006) Endocrine cancer in Iran: based on cancer registry system. Indian J Cancer 43(2):80–85 [DOI] [PubMed]
- 12.Larijani B, Aghakhani S, Khajeh-Dini H, Baradar-Jalili R. Clinico-pathological features of thyroid cancer as observed in five referral hospitals in Iran. Acta Oncol. 2003;42(4):334–337. doi: 10.1080/02841860310001547. [DOI] [PubMed] [Google Scholar]
- 13.Ries LAG, Melbert D, Krapcho M, Mariotto A, Miller BA, Feuer EJ, et al (2007) SEER Cancer Statistics Review, 1975-2004, National Cancer Institute. Bethesda, MD. https://seer.cancer.gov/csr/1975_2004/, based on November 2006 SEER data submission, posted to the SEER web site
- 14.Kohler BA, Ward E, McCarthy BJ, et al. Annual report to the nation on the status of cancer, 1975–2007, featuring tumors of the brain and other nervous system. J Natl Cancer Inst. 2011;103:714. doi: 10.1093/jnci/djr077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen AY, Jemal A, Ward EM. Increasing incidence of differentiated thyroid cancer in the United States, 1988–2005. Cancer: Interdisciplinary International Journal of the American Cancer Society. 2009;115(16):3801–3807. doi: 10.1002/cncr.24416. [DOI] [PubMed] [Google Scholar]
- 16.Enewold L, Zhu K, Ron E, Marrogi AJ, Stojadinovic A, Peoples GE, Devesa SS. Rising thyroid cancer incidence in the United States by demographic and tumor characteristics, 1980–2005. Cancer Epidemiology and Prevention Biomarkers. 2009;18(3):784–791. doi: 10.1158/1055-9965.EPI-08-0960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khoshnevis N, Ahmadizar F, Alizadeh M, Akbari ME (2012) Nutritional assessment of cancer patients in Tehran, Iran. Asian Pac J Cancer Prev 13(4):1621–1626 [DOI] [PubMed]
- 18.Vandenbroucke JP, VON Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explantion and elaboration. Epidemiology. 2007;18(6):805–35. doi: 10.1097/EDE.0b013e3181577511. [DOI] [PubMed] [Google Scholar]
- 19.Moayeri H, Oloomi Z, Sambo SA (2011) A cross-sectional study to determine the prevalence of calcium metabolic disorder in malignant childhood cancers in patients admitted to the pediatric ward of Vali-Asr Hospital. Acta Medica Iranica 49(12):818–823 [PubMed]
- 20.Safavi A, Azizi F, Jafari R, Chaibakhsh S, Safavi AA. Thyroid cancer epidemiology in Iran: a time trend study. Asian Pac J Cancer Prev. 2016;17(1):407–412. doi: 10.7314/APJCP.2016.17.1.407. [DOI] [PubMed] [Google Scholar]
- 21.Zekoi SR, Mousavi Z, Rezaei H, Mehrabi M. Prevalence of benign and malignant thyroid masses following childhood head and neck radiotherapy in Khorasan province, Iranian Journal of Endocrinology and Metabolism, Shahid Beheshti University of Medical Sciences. Year. 2006;4(3):161–164. [Google Scholar]
- 22.Shahbazi D, Azar DA. Prevalence of radiation-related cancers in Chaharmahal va Bakhtiari province over a 5 year period. Shahrekord Medical University the period. 2004;6(1):7–13. [Google Scholar]
- 23.Mohaghegh F, Hamta A, Shariatzadeh SMA. Survey of common cancers in Markazi province and their system of registration in 2001–2005 years compared to national statistics, Arak University of Medical Sciences Journal. Eleventh year, Number. 2006;2:84–93. [Google Scholar]
- 24.Shahesmaeili A, Malekpour Afshar R, Sadeghi A, Bazrafshan A. Cancer incidence in Kerman Province, Southeast of Iran: report of an ongoing population-based cancer registry, 2014. Asian Pac J Cancer Prev. 2018;19(6):1533–1541. doi: 10.22034/APJCP.2018.19.6.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roshani Z, Kamrani AAA, Shati M, Sahaf R. Prevalence of types of cancers in the elderly covered by insurance of the Islamic Republic of Iran Broadcasting Company in 2015 - Comparison with younger groups. Asian Pac J Cancer Prev. 2016;17:269–273. doi: 10.7314/APJCP.2016.17.S3.269. [DOI] [PubMed] [Google Scholar]
- 26.Javanmardi M (1997) Thyroid carcinoma in patients with goiter treated by surgery at Kashan Naghavi Hospital Year 1983- 1989, Kashan University of Medical Sciences and Health Services. 1(2):55–60
- 27.Talaeizadeh AH, Sarmast MH (2005) Prevalence and type of malignancy in thyroid nodules in patients referred to Imam Khomeini Hospital in Ahvaz Year 1991-2000, Ahvaz University of Medical Sciences. 10(38):87–93
- 28.Hajivandi A, Mohammadi A, Aezadi A. Ultrasound prevalence of thyroid nodules in people aged 15–65 referred to Fatemeh Zahra Hospital in Bushehr Year 2005. Bushehr University of Medical Science. 2005;11:87–94. [Google Scholar]
- 29.Haghpanah V, Solaimanpour B, Heshmat R, Tavangar S M. (2006). Endocrine cancers in four provinces of Iran, Journal of Sabzevar School of Medical Sciences. the period. 13(4): 190–195.
- 30.Ahmadi A, Salehi F, Ahmadimirghaed Z. Cancer trends in a province of Southwest of Iran, 2003–2016. Journal of Research in Medical Sciences. 2018;23(1):80–89. doi: 10.4103/jrms.JRMS_68_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salim EI, Moore MA, Bener A, Habib OS, Seif-Eldin I, Sobue T. Cancer epidemiology in South-West Asia-past, present and future. Asian Pac J Cancer Prev. 2010;11(Suppl 2):33–48. [PubMed] [Google Scholar]
- 32.Hussain F, Iqbal S, Mehmood A, Bazarbashi S, ElHassan T, Chaudhri N. Incidence of thyroid cancer in the Kingdom of Saudi Arabia, 2000–2010. Hematol Oncol Stem Cell Ther. 2013;6(2):58–64. doi: 10.1016/j.hemonc.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Larijani B, Mohagheghi MA, Bastanhagh MH, Mosavi-Jarrahi AR, Haghpanah V, Tavangar SM, Bandarian F, Khaleghian N. Primary thyroid malignancies in Tehran. Iran Medical principles and practice. 2005;14(6):396–400. doi: 10.1159/000088112. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Datasets are available through the corresponding author upon reasonable request.