Abstract
BACKGROUND and AIMS:
Patient-reported outcome measures (PROMs) provide a wholesome view of patient well-being. We conducted a retrospective cohort study to evaluate whether PROMs inform risk of unplanned healthcare utilization in patients with IBD.
METHODS:
We identified adult patients with IBD who completed at least two surveys in a large internet-based cohort within 1 year. We evaluated the association between baseline patient characteristics, disease activity indices, medication use, and PROMs, assessed using NIH Patient Reported Outcome Measurement Information System (PROMIS) and subsequent risk of incident hospitalization (at time of first follow-up) within 1y, and readmission within 1y (in patients with hospitalization at first follow-up), using multivariable logistic regression.
RESULTS:
Of 7902 patients with IBD (45.5y, 72% females, 63% Crohn’s disease), 1377 (17.4%) were hospitalized within 1y. Among PROMs, pain interference (adjusted OR per 5-point increase in PROMIS, 1.09; 95% CI, 1.05–1.14), but not depression, anxiety, fatigue or sleep disturbance, were predictive of higher risk of hospitalization. Prior surgery or hospitalization, symptomatic disease, biologic and corticosteroid use were also associated with higher risk of hospitalization. Of 521 patients hospitalized with IBD, 133 (25.5%) were readmitted within 1y. Anxiety and pain interference were predictive of higher risk of readmission, whereas depression was associated with lower risk of readmission.
CONCLUSIONS:
In a large internet-based cohort study, PROMs may have a modest effect on modifying risk of unplanned healthcare utilization in patients with IBD, with pain interference being most consistently associated with increased risk of hospitalization and readmission.
Keywords: patient-reported outcomes, adverse outcomes, prediction, ulcerative colitis, population health management
INTRODUCTION
The global burden and costs of Inflammatory bowel diseases (IBD) are rising.1–4 While contribution of pharmacotherapy to costs of IBD care are rising, unplanned healthcare utilization (e.g., hospitalizations and readmissions) remains a primary driver of healthcare costs in patients with IBD.5 In population-based cohorts, approximately 50–80% of patients with IBD require hospitalization within 10 years of diagnosis and these contribute a significant percentage of direct medical costs with approximately 30% of patients accounting for over 80% of total IBD-related healthcare costs.6 In a systematic review of 17 cohort studies, 18% and 26% of hospitalized patients with IBD were readmitted within 30-day and 90-day, respectively.6 Factors associated with hospitalizations are multifaceted and prior studies on predicting hospitalizations have focused on clinical- or hospital-related characteristics at time of initial admission, with limited assessment of patient-reported outcome measures (PROMs).7–10
PROMs are essential components of patient-centered research, and have increasingly been used in regulatory approval of medications in IBD.11, 12 In clinical practice, routine assessment of PROMs in chronic conditions may improve patient-provider relationship, with patients feeling more empowered in conveying physical and emotional wellbeing, and providers noting that it may help in initiating symptom-specific patient education and counselling.12–14 In an evaluation of patient reported outcomes measurement information system (PROMIS), a generic PRO measurement tool which includes anxiety, depression, fatigue, sleep disturbance, (lack of) satisfaction with social role and pain interference (self-reported consequences of pain on relevant aspects of a person’s life), Kappelman and colleagues demonstrated worse functioning in each PROMIS domain with increasing levels of IBD activity and worsening scores on quality of life domains.15 Subsequent studies have suggested a bi-directional relationship between mood disorders including depression and anxiety, and clinical disease activity and corticosteroid use in patients with IBD.9, 16–18 While claims-based studies and small single-center studies have variably suggested an association between presence of depression, anxiety and chronic pain and hospitalization, and readmissions, in patients with IBD, it remains unclear whether PROMs (without reaching thresholds for clinical diagnoses for depression or mood disorders) may inform risk of unplanned healthcare utilization in patients with IBD.7, 10, 18, 19
We sought to comprehensively understand the independent impact of PROMs, on risk of hospitalization and readmissions in patients with IBD, while simultaneously adjusting for demographic and clinical characteristics, patient-reported disease activity and use of medications. To accomplish this, we conducted a longitudinal cohort study within IBD Partners, an internet-based cohort of >15,000 patients with IBD, in a set of patients who filled out at least 2 surveys over 1 year.
METHODS
Study Population and Inclusion Criteria
We performed a retrospective cohort study within the Crohn’s and Colitis Foundation’s IBD Partners cohort. The study cohort has been described in detail previously (Supplementary Appendix).20, 21 To evaluate risk factors associated with incident hospitalization in the IBD Partners cohort (cohort 1), we included (i) adult patients with IBD recruited into IBD Partners between 2011–18, (ii) who responded to at least 2 surveys within 1y (B=Baseline, F1=1st follow-up), (iii) and responded “no” to the question regarding hospitalization within 12 months prior to the baseline survey (to identify patients with incident hospitalization between survey B and F1, and to avoid confounding by disease severity since prior hospitalization is a very strong risk factor for re-hospitalization). Subsequently, to evaluate risk and risk factors for readmission within 12m after hospitalization (cohort 2), we identified patients with self-reported hospitalization at time of F1, who responded to another survey (F2) within 1y after second survey (F1). We excluded patients who did not have follow-up within 1y after baseline survey. Figure 1 shows the study cohorts and flow.
Figure 1.
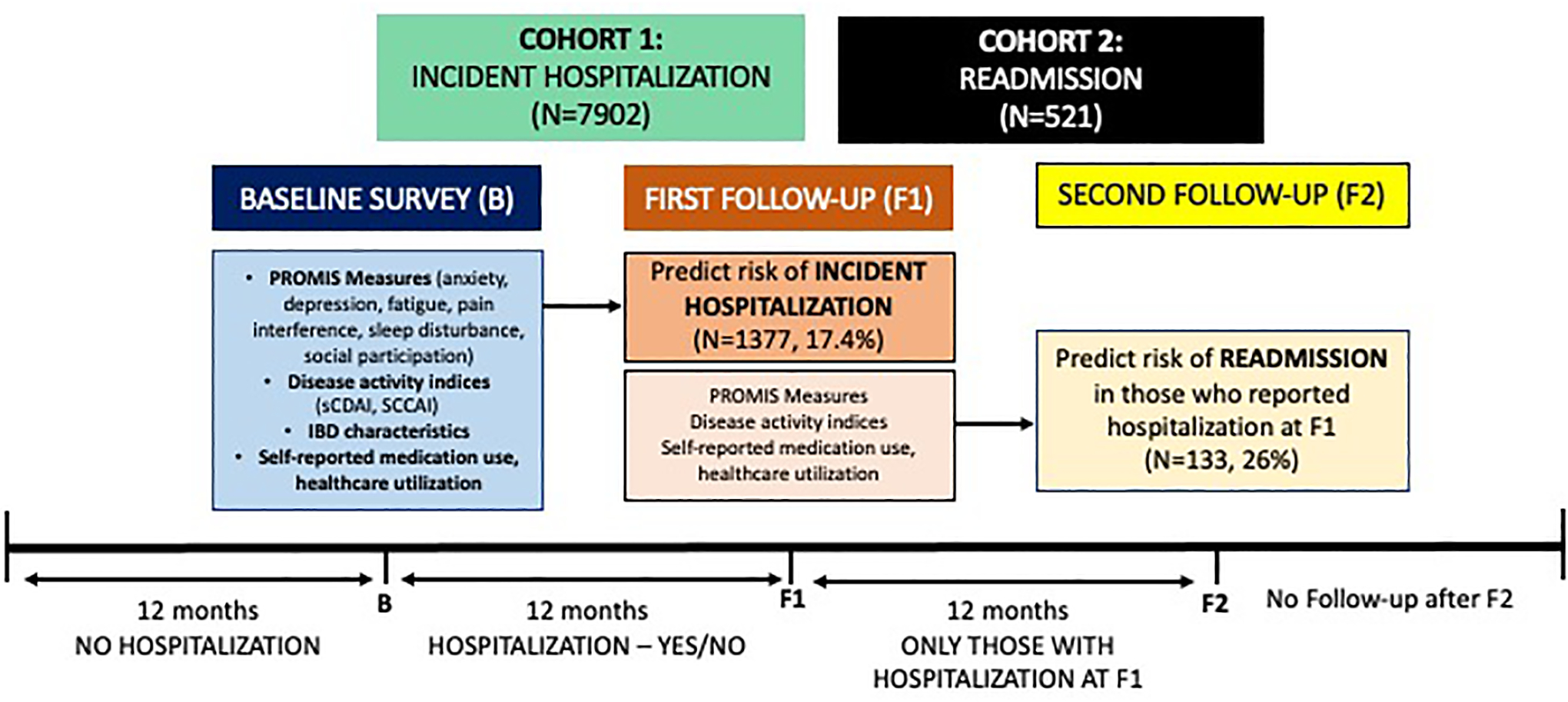
Study design and patient flow
IBD Partners’ study protocol was approved by the Institutional Review Board at the University of North Carolina, Chapel Hill, North Carolina; this secondary analysis of previously collected data was deemed exempt by the University of California San Diego Institutional Review Board.
Exposure
Cohort 1:
To evaluate the longitudinal association between PROMIS measures at baseline (B) and subsequent risk of hospitalization (F1), our primary exposure was PROMIS measures. PROMIS instruments are general (not disease-specific) measures that are valid and responsive, allow comparisons within and between conditions, and are grouped into item banks based on symptoms, function, well-being, and general health. Participants completed 4 items from each of 6 PROMIS item banks measuring individual dimensional constructs of health-related quality of life. A complete list of all PROMIS items included in this study is included in Supplementary Table 1. PROMIS items are calibrated using a T-score metric with the mean of the US general population equal to 50 and standard deviation (SD) in the general population equal to 10. Higher scores indicate more of the domain being measured, such that high scores for anxiety, depression, fatigue, sleep disturbance, and pain interference indicate poorer health, whereas high scores for satisfaction with social role indicate better health. Minimal Important Differences (MIDs), the score that is large enough to have implications for a patient’s treatment or care, has been estimated between 2–6; for our study, we classified a 5-point difference in PROMIS measures as clinically meaningful.15 Of note, these scores do not necessarily denote clinically-diagnosed depression or anxiety, but rather suggest the presence of depressive or anxiety-related symptoms affecting quality of life.
Cohort 2:
To evaluate whether PROMIS measures impact risk of readmission (F2), we evaluated PROMIS at F1.
Overall analysis focused on all patients with IBD, and subgroup analyses in patients with UC and CD were performed.
Outcome
For cohort 1, primary outcome of interest was risk of incident hospitalization (at time F1). For cohort 2, primary outcome was risk of readmission (at time F2), in subset of patients who reported hospitalization at time of F1. Though self-reported hospitalization has not specifically been validated in IBD Partners, a similar Crohn’s and Colitis Foundation initiative has demonstrated high accuracy of patient-reported IBD-related hospitalization (96%) against electronic medical record.22 Unfortunately, with self-report based on surveys at fixed time points, reasons or exact timing of hospitalization in relation to PROM assessment was not available.
Covariates
To identify other potential risk factors associated with hospitalization and readmission, we abstracted data on: age at diagnosis, sex, body mass index (BMI, in kg/m2), disease duration, smoking status, ethnicity, education status, clinical disease activity, measured using short Crohn’s disease activity index (sCDAI) in patients with CD (<150 = remission)23 and simple clinical colitis activity index (SCCAI) in patients with UC (<5 = remission),24 self-reported hospitalization or surgery any time since diagnosis, as well as medications for treatment of IBD including 5-aminosalicylates, corticosteroids, immunomodulators (thiopurines or methotrexate), and biologic therapies and narcotic use. Data on self-reported IBD location and behavior was previously demonstrated to have suboptimal performance, and hence, was not considered.21
Statistical Analysis
Descriptive analysis was used to describe baseline characteristics (Supplementary Appendix). To evaluate the independent effect of PROMIS measures on hospitalization, we performed multivariable logistic regression with backward variable selection, in conjunction with clinical plausability. A p-value cut-off for inclusion into the final regression model was defined as a p<0.20 on univariate analysis of the following variables: age at diagnosis, sex, BMI, education level, smoking status, disease duration, history of hospitalization, history of bowel surgery ever, history of recent bowel surgery (in the past 12 months), clinical disease activity as a categorical variable of remission vs. active disease, current medications (e.g., narcotics, biologics, steroids, immunomodulator, and 5-ASA), and PROMIS domains (e.g., anxiety, depression, fatigue, sleep disturbance, increased participation in social events, and pain) per 5-unit change. All hypothesis testing was performed using a two-sided p-value with a statistical significance threshold <0.05. All statistical analyses were performed with Stata MP (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).
RESULTS
Risk of Hospitalization
We included 7902 adults with IBD who responded to at least 2 surveys within 1y, and reported no hospitalization in 12m preceding the baseline (B) survey (cohort 1) (Table 1, Supplementary Table 2). Of these, 72% were females, 63% were diagnosed with CD; 37% reported prior surgery, and 59% reported ever being hospitalized (>1y prior to baseline survey). Majority of patients were in remission (68% patients with CD, 75% patients with UC), 36% were treated with biologics, 17% were on corticosteroids, and 10% reported narcotic use. Of these 7902 patients, 1377 patients (17.4%) were hospitalized within 1y (reported at F1 survey) (1043/5013, 20.8% patients with CD; 334/2899, 11.6% patients with UC).
Table 1.
Baseline characteristics of all patients with IBD without recent hospitalization at time of baseline survey (B)
| Characteristics | All patients (n = 7,902) | Patients who were not hospitalized (n = 6,525) | Patients who were hospitalized (n = 1,377) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 45.5 ± 15.3 | 45.5 ± 15.2 | 45.7 ± 16.1 | 0.66 |
| Age at diagnosis (years) | 30.1 ± 13.8 | 30.5 ± 13.8 | 28.2 ± 13.4 | <0.01 |
| Women (%) | 72.2% | 71.9% | 73.8% | 0.16 |
| BMI – median (range) | 24.4 (21.7 – 28.3) | 24.5 (21.9 – 28.3) | 23.9 (21.2 – 27.9) | <0.01 |
| Disease duration (years) – median (range) | 12 (5 – 23) | 11 (5 – 22) | 13 (7 – 27) | <0.01 |
| Education (% >college) | 92.6% | 92.8% | 91.4% | 0.09 |
| • Other | 9.0% | 9.1% | 8.3% | |
| Smoking (current, % yes) | 34.0% | 34.0% | 33.7% | 0.83 |
| History of hospitalization (%) | 58.6% | 55.5% | 73.3% | <0.01 |
| History of bowel surgery (%) | 36.6% | 33.5% | 51.2% | <0.01 |
| Patients with recent bowel surgery since the last survey | 3.2% | 2.9% | 4.5% | 0.002 |
| Proportion with Crohn’s Disease | 63.4% | 60.8% | 75.7% | <0.01 |
| Disease Activity | ||||
| SCCAI (UC patients only) | 3.3 ± 2.7 | 3.1 ± 2.5 | 4.9 ± 3.5 | <0.01 |
| Clinical remission in UC patients (SCCAI 4 or less; %) | 23.7% | 26.6% | 10.0% | <0.01 |
| SCDAI (CD patients only) | 140.7 ± 92.1 | 130.4 ± 84.3 | 183.1 ± 109.2 | <0.01 |
| Clinical remission in CD patients (SCDAI 150 or less; %) | 31.9% | 33.4% | 24.6% | <0.01 |
| Current Medications | ||||
| Narcotics | 9.8% | 8.4% | 16.3% | <0.01 |
| Biologics | 36.0% | 33.9% | 46.1% | <0.01 |
| Steroids | 16.9% | 14.9% | 26.3% | <0.01 |
| Immunomodulator | 27.5% | 27.6% | 26.8% | 0.53 |
| 5-ASA | 45.2% | 47.5% | 34.1% | <0.01 |
| Healthcare Utilization | ||||
| • 3 or more times | 32.6% | 32.3% | 34.4% | |
| • 3 or more times | 40.8% | 39.6% | 46.2% | |
| PROMIS Measures | ||||
| Anxiety | 52.5 ± 9.4 | 52.3 ± 9.3 | 53.8 ± 9.7 | <0.01 |
| Depression | 50.5 ± 9.1 | 50.2 ± 9.0 | 52.1 ± 9.5 | <0.01 |
| Fatigue | 54.6 ± 10.8 | 54.0 ± 10.7 | 57.6 ± 10.9 | <0.01 |
| Sleep disturbance | 51.4 ± 8.3 | 51.0 ± 8.3 | 53.0 ± 8.4 | <0.01 |
| Participation in social roles and activities domain | 48.8 ± 9.7 | 49.4 ± 9.6 | 46.2 ± 9.9 | <0.01 |
| Pain interference | 51.7 ± 9.7 | 51.0 ± 9.5 | 54.7 ± 10.1 | <0.01 |
Risk factors for incident hospitalization
Baseline PROMIS scores across domains of anxiety, depression, fatigue, sleep disturbance, participation in social activities and pain interference (self-reported consequence of pain on social, cognitive, emotional, physical, and recreational activities) were inferior in patients who were subsequently hospitalized, as compared to patients who were not hospitalized (Table 1). Patients who were hospitalized were slightly younger at time of diagnosis, had longer disease duration, reported prior remote history of hospitalization and history of bowel surgery (ever and/or since the last survey), and were more likely to have CD, reported clinically active disease in the preceding year, and higher rates of corticosteroid, biologic and narcotic use, as compared to patients without hospitalization.
On multivariable analysis, among all PROMIS domains, only pain interference was predictive of increased risk of incident hospitalization (OR per 5-unit increase in score, 1.09 [95% CI, 1.05–1.14]); higher anxiety, depression, fatigue or sleep disturbance and decreased ability to participate in social events were not predictive of risk of incident hospitalization (Table 2). Besides PROMIS domains, clinically active disease, longer disease duration, prior and recent surgery, remote hospitalization, lower BMI, and treatment with biologics and corticosteroids were independently associated with increased risk of hospitalization. We observed strong correlation between anxiety and depression (Pearson’s correlation coefficient = 0.75). Both anxiety and depression were associated with increased risk of subsequent hospitalization on univariate analysis. However, on multivariable analysis including either only anxiety or depression, no significant differences were observed (results not shown).
Table 2.
Clinical, medication, and patient-reported outcomes (at baseline survey, B) predictive of subsequent hospitalization (reported at F1) in patients with IBD
| Odds ratio (95% Confidence Interval) | |
|---|---|
| Clinical characteristics | |
| BMI | 0.97 (0.96 – 0.98) |
| Disease duration (per 1 y) | 1.01 (1.00 – 1.01) |
| History of hospitalization (%) | 1.21 (1.02 – 1.45) |
| History of bowel surgery ever (%) | 1.19 (1.00 – 1.41) |
| Recent bowel surgery since the last survey | 1.57 (1.11 – 2.24) |
| Patients in clinical remission | 0.53 (0.45 – 0.61) |
| Current Medications | |
| Biologics | 1.40 (1.22 – 1.61) |
| Steroids | 1.69 (1.44 – 1.98) |
| Immunomodulator | 0.90 (0.77 – 1.04) |
| 5-ASA | 0.80 (0.69 – 0.93) |
| PROMIS Domains (per 5 points increase in PROMIS scores) | |
| Anxiety domain | 0.97 (0.93 – 1.01) |
| Fatigue domain | 1.03 (0.99 – 1.07) |
| Increased participation in social events domain | 0.96 (0.91 – 1.00) |
| Pain interference domain | 1.09 (1.05 – 1.14) |
Backwards logistic regression model was utilized. Variables that did not make it into the final regression model did not have an odds ratio reported: age at diagnosis, sex, education, disease duration, narcotic use at baseline, depression or sleep disturbance at time of baseline survey
On subgroup analysis, in patients with CD, higher pain interference (but none of the others PROMIS domains), clinically active disease, longer disease duration, lower BMI, and use of biologics and corticosteroids were predictive of incident hospitalization (Table 3). In patients with UC, higher pain interference, higher disruption in ability to participate in social events, lower depression scores, clinically active disease, younger age, lower education level and treatment with corticosteroids were predictive of increased risk of incident hospitalization, whereas treatment with 5-aminosalicylates was associated with lower risk of hospitalization (Table 3). On sensitivity analysis of patients with IBD in clinical remission at baseline and without recent bowel surgery (no bowel surgery in preceding 12m), higher scores on pain interference (OR per 5-unit increase in score, 1.12 [95% CI, 1.05 – 1.20]) and fatigue (OR per 5-unit increase in score, 1.06 [95% CI, 1.00 – 1.13]) at baseline, and lower anxiety scores (OR per 5-unit increase in score, 0.88 [95% CI, 0.82–0.95]) were predictive of incident hospitalization.
Table 3.
Clinical, medication, and patient-reported outcomes (at baseline survey, B) predictive of subsequent hospitalization (reported at F1) in patients with IBD, by Crohn’s disease and ulcerative colitis
| Crohn’s disease | Ulcerative Colitis | |
|---|---|---|
| Odds ratio (95% Confidence Interval) | Odds ratio (95% Confidence Interval) | |
| Clinical characteristics | ||
| Age at diagnosis (per 1 y) | - | 0.98 (0.97 – 0.99) |
| Women (%) | - | - |
| BMI | 0.97 (0.96 – 0.99) | 0.98 (0.95 – 1.00) |
| Education (% >college) | - | 0.55 (0.33 – 0.92) |
| Disease duration (per 1 y) | 1.01 (1.00 – 1.01) | - |
| History of hospitalization (%) | 1.17 (0.96 – 1.43) | 1.34 (0.98 – 1.83) |
| History of bowel surgery ever (%) | - | - |
| Recent bowel surgery since the last survey | 1.36 (0.91 – 2.03) | - |
| Patients in clinical remission | 0.52 (0.43 – 0.62) | 0.48 (0.33 – 0.68) |
| Current Medications | ||
| Narcotics | - | - |
| Biologics | 1.42 (1.21 – 1.66) | - |
| Steroids | 1.56 (1.29 – 1.88) | 2.30 (1.64 – 3.23) |
| Immunomodulator | 0.85 (0.72 – 1.01) | - |
| 5-ASA | 0.88 (0.74 – 1.05) | 0.61 (0.44 – 0.84) |
| PROMIS Domains (per 5 points increase in PROMIS scores)- | ||
| Anxiety domain | 0.96 (0.89 – 1.02) | |
| Depression domain | 1.07 (0.99 – 1.15) | 0.86 (0.77 – 0.96) |
| Fatigue domain | - | - |
| Sleep disturbance domain | - | - |
| Increased participation in social events domain | - | 0.88 (0.79 – 0.97) |
| Pain interference domain | 1.11 (1.06 – 1.17) | 1.12 (1.01 – 1.23) |
Backwards logistic regression model was utilized. Variables that did not make it into the final regression model did not have an odds ratio reported.
Risk of Readmission with 1 year
Of 1377 patients with IBD with incident hospitalization (at time of F1), 521 (38%) patients completed a second follow-up survey (F2) within 1y (75% patients with CD). Of the 521 patients, 133 patients (26%) reported readmission at time of second follow-up survey (F2).
Risk factors for readmission
PROMIS scores across domains of anxiety, depression, fatigue, sleep disturbance, participation in social activities and pain interference, at time of F1, were consistently inferior in patients who were readmitted, as compared to patients without readmission. Patients with readmission within 1y were more also likely to have active disease at time of prior survey (F1), and lower BMI (Table 4).
Table 4.
Clinical characteristics of patients with IBD with hospitalization at time of first follow-up survey (F1)
| Not readmitted since index hospitalization (n = 388) |
Readmitted after index hospitalization (n = 133) |
p-value | |
|---|---|---|---|
| Age (years) | 45.9 ± 15.8 | 43.2 ± 16.1 | 0.08 |
| Women (%) | 70.9% | 74.4% | 0.43 |
| BMI – median (range) | 23.6 (20.9 – 27.1) | 21.9 (19.3 – 26.5) | 0.01 |
| Disease duration (years) – median (range) | 14 (7 – 28) | 11 (5 – 30) | 0.16 |
| Patients with recent bowel surgery since the last survey | 31.4% | 30.1% | 0.77 |
| Proportion of Crohn’s (%) | 74.2% | 78.9% | 0.28 |
| Disease activity | |||
| SCCAI (UC patients only) | 3.8 ± 2.7 | 5.2 ± 2.9 | 0.08 |
| Clinical remission in UC patients (SCCAI 4 or less; %) | 10.6% | 5.3% | 0.08 |
| SCDAI (CD patients only) | 169.4 ± 112.5 | 229.7 ± 125.3 | <0.01 |
| Clinical remission in CD patients (SCDAI 150 or less; %) | 30.9% | 15.0% | <0.01 |
| Current Medications | |||
| Narcotics | 24.0% | 26.5% | 0.57 |
| Biologics | 43.0% | 45.5% | 0.63 |
| Steroids | 27.6% | 34.9% | 0.11 |
| Immunomodulator | 24.7% | 31.1% | 0.16 |
| 5-ASA | 35.6% | 25.8% | 0.04 |
| Healthcare Utilization | |||
| • 3 or more times | 31.5% | 37.7% | |
| • 3 or more times | 58.0% | 67.4% | |
| PROMIS Measures | |||
| Anxiety | 53.5 ± 9.8 | 56.8 ± 9.9 | 0.001 |
| Depression | 52.0 ± 9.6 | 54.6 ± 10.1 | 0.008 |
| Fatigue | 57.3 ± 11.3 | 61.7 ± 9.6 | <0.01 |
| Sleep disturbance | 52.9 ± 8.4 | 54.9 ± 8.1 | 0.01 |
| Participation in social roles and activities domain | 45.6 ± 9.7 | 41.5 ± 8.6 | <0.01 |
| Pain interference | 54.1 ± 10.4 | 58.9 ± 9.8 | <0.01 |
On multivariable analysis, among all PROMIS domains, higher anxiety was predictive of increased risk of readmission (OR per 5-unit increase in score, 1.23 [95% CI, 1.00–1.50]), whereas higher depression was associated with lower risk of readmission (Table 5). Besides PROMIS domains, clinically active disease and non-use of 5-ASA were independently predictive of increased risk of readmission. On subgroup analysis, in patients with CD, higher pain interference was the only PROMIS domain predictive of increased risk of readmission (OR per 5-unit increase in score, 1.21 [95% CI, 1.04–1.42]). In patients with UC, higher disruption in ability to participate in social events was the only PROMIS domain predictive of increased risk of readmission (OR per 5-unit increase in score, 0.22 [95% CI, 0.07–0.75]).
Table 5.
Clinical, medication, and patient-reported outcomes (at time of first follow-up survey, F1) predictive of readmission within 1y (reported at 2nd follow-up survey, F2) in patients with IBD with recent hospitalization
| Risk factors | Odds ratio (95% Confidence Interval) |
|---|---|
| Clinical characteristics | |
| Patients in clinical remission | 0.52 (0.30 – 0.90) |
| Current Medications | |
| Narcotics | 0.65 (0.38 – 1.12) |
| Immunomodulator | 1.52 (0.94 – 2.46) |
| 5-ASA | 0.60 (0.36 – 0.99) |
| PROMIS Domains (per 5 points increase in PROMIS scores) | |
| Anxiety domain | 1.23 (1.00 – 1.50) |
| Depression domain | 0.80 (0.65 – 0.98) |
| Increased participation in social events domain | 0.87 (0.74 – 1.03) |
| Pain interference domain | 1.14 (0.99 – 1.31) |
Backwards logistic regression model was utilized. Variables that did not make it into the final regression model did not have an odds ratio reported: age at diagnosis, sex, body mass index, education, disease duration, history of remote hospitalization, history of prior or recent bowel surgery, biologic or corticosteroid use at time of index hospitalization, fatigue or sleep disturbance at time of index hospitalization
DISCUSSION
While most prior studies have focused on the impact of individual PROs and mood disorders such as depression, anxiety, fatigue and sleep disturbance on clinical disease course and health-related quality of life, few studies have focused on comprehensive assessment of multiple PROs simultaneously, along with clinical and treatment characteristics, and its longitudinal impact on hospitalization and readmission in patients with IBD.7, 9, 16, 19, 25–27 In this secondary analysis of prospectively collected data on 7902 patients with IBD from an internet-based cohort, we made several key observations regarding PROMs and risk incident hospitalization and readmission. First, amongst patients with IBD without recent hospitalization, 17% report incident hospitalization, whereas in patients with recent hospitalization, 26% report readmission within 1y. Second, PROMs were only modestly predictive of risk of hospitalization, after adjusting for key disease covariates. Among PROMIS domains, pain interference was the most consistent PROM associated with increased risk of hospitalization, in patients with CD and UC, and in patients in clinical remission at baseline. Amongst patients with UC, inability to participate in social events and lower depression scores were also predictive of with increased risk of incident hospitalization. In a subset of patients with patients with UC in clinical remission without recent surgery, higher fatigue scores were predictive of incident hospitalization. We also confirmed prior observations that clinically active disease and measures of severe disease (prior and recent surgery, remote hospitalization, and treatment with biologics and corticosteroids) were predictive of increased risk of incident hospitalization within 1y. Third, in patients with recent hospitalization, higher anxiety scores and lower depression scores, besides conventional risk factors may be predictive of readmission within the next 1y. Overall, in addition to confirming previously known disease-and treatment-related risk factors predictive of unplanned healthcare utilization, we observed that PROMs, particularly pain interference, may modestly predict risk of incident hospitalization and readmission.
Prior cross-sectional and retrospective studies have identified that the prevalence of chronic pain and need for narcotic pain medications, is higher in hospitalized patients, and inadequate pain control and opioid use disorder has been variably associated with increased risk of readmission within 30–90 days.9, 25–29 We confirmed that regardless of disease phenotype and activity and narcotic use, pain interference was the most consistent PROM predictive of hospitalization and readmission. The pain interference domain of PROMIS captures the consequences of pain on relevant aspects of a person’s life and includes the extent to which pain hinders engagement with social, cognitive, emotional, physical, and recreational activities.30 Beyond physical pain, pain interference examines the psycho-socio-functional impact of pain on daily activities and hence, was able to predict subsequent hospitalization.
Our findings regarding the lack of impact of depression and anxiety on risk of interval hospitalization may appear surprising, in light of a considerable evidence which suggests that the prevalence of depression and anxiety is high in patients with IBD, and is associated with increased clinical disease activity, inferior quality of life, increased health-seeking behavior and contributes to healthcare costs in IBD.7, 9, 16, 31, 32 However, prospective cohort studies have failed to show an independent association between depression and/or anxiety and subsequent risk of hospitalization. In a prospective single-center study of 414 patients with IBD, Narula and colleagues observed that while anxiety, but not depression, was associated with poor IBD-related outcomes, no significant association was observed between baseline diagnosis of anxiety and depression and subsequent risk of IBD-related hospitalization.19 Similarly, Gracie and colleagues observed a bi-directional association between IBD disease activity and anxiety and depression. While presence of anxiety and depression was associated with increased risk of disease flare, need for corticosteroids and escalation of medical therapy, it was not associated with increased risk of hospitalization or surgery.16 This difference in findings from prospective observational studies vs. large cross-sectional or administrative claims-based analyses may be due to differences in definition of exposure and outcome of interest, and confounding by severity. While claims-based analyses and single-center retrospective studies rely on either a diagnostic claim for psychiatric diseases like depression or anxiety, or reports of depression and use of anti-depressants based on chart review, prospective observational studies like ours relied on a validated tool to examine depressive and anxiety symptoms using PROMIS, rather than a clinical diagnosis of corresponding psychiatric diseases. Moreover, by focusing on examining the prevalence of psychiatric diseases in patients at time of hospitalization, claims-based studies are confounded by disease severity and diagnostic suspicion bias and are unable to infer a temporal association between depressive and anxiety symptoms and subsequent risk of hospitalization.
Examining PROMs predictive of readmission was insightful. In these patients, anxiety was predictive of increased risk of readmission which may denote a heightened self-awareness of symptoms that resulted in prior admission, and a lower threshold to seek urgent care if unable to be accommodated proactively in ambulatory clinic. In contrast, depressive symptoms were predictive of a lower risk of readmission, which may denote psychosocial withdrawal and decreased healthcare-seeking behavior resulting in a behavior of avoiding hospitalization. Whether routine measurement of these PROMs in patients at time of hospital discharge (or during early post-discharge follow-up), along with interventions to address patients’ concerns through multi-disciplinary care may reduce readmission rates remains to be seen.
Our study has several strengths. This is one of the largest longitudinal studies evaluating multiple PROMs simultaneously using the validated PROMIS tool, and their predictive ability for hospitalization and readmission. However, there are several limitations which merit discussion. First, while IBD Partners has notable strengths in recruitment and retention, there is selection bias and the dataset may not be truly representative of a population of patients with IBD, including a higher percentage of female patients (>70%), Caucasian race (>90%) and higher rates of college education than national averages. Second, in our longitudinal cohort, a significant proportion of patients were lost to follow-up both at F1 and F2, since participation in the survey was voluntary, leading to response bias. Third, hospitalization was a self-reported outcome, and though it had high positive predictive value, we are unable to ascertain exact reason, or timing of hospitalization in relation to survey (or PROM measurement). Fourth, IBD Partners cohort does not include physician notes, laboratory, radiology or endoscopy data. Hence, we were unable to corroborate our findings with simultaneous assessment of clinical and endoscopic disease activity. We also do not have validated data on clinical phenotype, disease location or extent in this cohort, limiting detailed analyses of assessment of disease severity.
In summary, in a large internet-based cohort study of patients with IBD, we observed that PROMs, particularly pain interference, but not depression, anxiety, fatigue or sleep disturbance, may be modestly predictive of risk of incident hospitalization. Anxiety may be with increased risk of readmission in patients with IBD with recent hospitalization. Though PROMs in routine practice may improve patient-provider communication and coproduction of care, it is unclear whether they meaningfully inform risk of unplanned healthcare utilization.
Supplementary Material
Funding:
Dr. Nguyen is supported by NIDDK (T32DK007202) and NLM (T15LM011271). Dr. Singh is supported by NIDDK (K23DK117058) and ACG Junior Faculty Development Award. Dr. Sandborn is supported in part by the NIDDK-funded San Diego Digestive Diseases Research Center (P30 DK120515).
Disclosures:
NHN – None to declare
XZ – None to declare
MDL – Consulting fees from AbbVie, Pfizer, UCB, Salix, Valeant, Takeda, Prometheus, Janssen, and Target PharmaSolutions; research support from Takeda and Pfizer.
WJS – research grants from Abbvie, Abivax, Arena Pharmaceuticals, Boehringer Ingelheim, Celgene, Genentech, Gilead Sciences, Glaxo Smith Kline, Janssen, Lilly, Pfizer, Prometheus Biosciences, Seres Therapeutics, Shire, Takeda, Theravance Biopharma; consulting fees from Abbvie, Abivax, Admirx, Alfasigma, Alimentiv (Robarts Clinical Trials, owned by Health Academic Research Trust [HART]), Alivio Therapeutics, Allakos, Amgen, Applied Molecular Transport, Arena Pharmaceuticals, Bausch Health (Salix), Beigene, Bellatrix Pharmaceuticals, Boehringer Ingelheim, Boston Pharmaceuticals, Bristol Meyers Squibb, Celgene, Celltrion, Cellularity, Cosmo Pharmaceuticals, Escalier Biosciences, Equillium, Forbion, Genentech/Roche, Gilead Sciences, Glenmark Pharmaceuticals, Gossamer Bio, Immunic (Vital Therapies), Index Pharmaceuticals, Intact Therapeutics, Janssen, Kyverna Therapeutics, Landos Biopharma, Lilly, Oppilan Pharma, Otsuka, Pandion Therapeutics, Pfizer, Progenity, Prometheus Biosciences, Protagonists Therapeutics, Provention Bio, Reistone Biopharma, Seres Therapeutics, Shanghai Pharma Biotherapeutics, Shire, Shoreline Biosciences, Sublimity Therapeutics, Surrozen, Takeda, Theravance Biopharma, Thetis Pharmaceuticals, Tillotts Pharma, UCB, Vendata Biosciences, Ventyx Biosciences, Vimalan Biosciences, Vivelix Pharmaceuticals, Vivreon Biosciences, Zealand Pharma; and stock or stock options from Allakos, BeiGene, Gossamer Bio, Oppilan Pharma, Prometheus Biosciences, Progenity, Shoreline Biosciences, Ventyx Biosciences, Vimalan Biosciences. Spouse: Iveric Bio - consultant, stock options; Progenity - stock; Oppilan Pharma - consultant, stock options; Prometheus Biosciences - employee, stock options; Ventyx Biosciences – stock options; Vimalan Biosciences – stock optionsMDK – Consulting fees from Abbvie, Janssen, Takeda, Eli Lilly; research support from Abbvie and Janssen; stockholder Janssen
MDK - consulted for Abbvie, Janssen, Pfizer, and Takeda, is a shareholder in Johnson & Johnson, and has received research support from Abbvie and Janssen.
SS – research grants from AbbVie, Janssen
Guarantor of Article:
Dr. Siddharth Singh had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol 2020;5:17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 2018;390:2769–2778. [DOI] [PubMed] [Google Scholar]
- 3.Park KT, Ehrlich OG, Allen JI, et al. The Cost of Inflammatory Bowel Disease: An Initiative From the Crohn’s & Colitis Foundation. Inflamm Bowel Dis 2020;26:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology 2019;156:254–272 e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dieleman JL, Cao J, Chapin A, et al. US Health Care Spending by Payer and Health Condition, 1996–2016. JAMA 2020;323:863–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen NH, Khera R, Ohno-Machado L, et al. Annual Burden and Costs of Hospitalization for High-Need, High-Cost Patients With Chronic Gastrointestinal and Liver Diseases. Clin Gastroenterol Hepatol 2018;16:1284–1292 e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnes EL, Kochar B, Long MD, et al. Modifiable Risk Factors for Hospital Readmission Among Patients with Inflammatory Bowel Disease in a Nationwide Database. Inflamm Bowel Dis 2017;23:875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen NH, Koola J, Dulai PS, et al. Rate of Risk Factors for and Interventions to Reduce Hospital Readmission in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Limsrivilai J, Stidham RW, Govani SM, et al. Factors That Predict High Health Care Utilization and Costs for Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol 2017;15:385–392 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waljee AK, Lipson R, Wiitala WL, et al. Predicting Hospitalization and Outpatient Corticosteroid Use in Inflammatory Bowel Disease Patients Using Machine Learning. Inflamm Bowel Dis 2017;24:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Snyder CF, Jensen RE, Segal JB, et al. Patient-reported outcomes (PROs): putting the patient perspective in patient-centered outcomes research. Med Care 2013;51:S73–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen ER, Melmed GY. Making a Case for Patient-Reported Outcomes in Clinical Inflammatory Bowel Disease Practice. Clin Gastroenterol Hepatol 2018;16:603–607. [DOI] [PubMed] [Google Scholar]
- 13.Singh S PROMises Made, PROMises To Be Kept: Patient-Reported Outcome Measures in Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol 2018;16:624–626. [DOI] [PubMed] [Google Scholar]
- 14.Verma M, Stites S, Navarro V. Bringing Assessment of Patient-Reported Outcomes to Hepatology Practice. Clin Gastroenterol Hepatol 2018;16:447–448. [DOI] [PubMed] [Google Scholar]
- 15.Kappelman MD, Long MD, Martin C, et al. Evaluation of the patient-reported outcomes measurement information system in a large cohort of patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol 2014;12:1315–23 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gracie DJ, Guthrie EA, Hamlin PJ, et al. Bi-directionality of Brain-Gut Interactions in Patients With Inflammatory Bowel Disease. Gastroenterology 2018;154:1635–1646 e3. [DOI] [PubMed] [Google Scholar]
- 17.Gracie DJ, Williams CJ, Sood R, et al. Poor Correlation Between Clinical Disease Activity and Mucosal Inflammation, and the Role of Psychological Comorbidity, in Inflammatory Bowel Disease. Am J Gastroenterol 2016;111:541–51. [DOI] [PubMed] [Google Scholar]
- 18.Kochar B, Barnes EL, Long MD, et al. Depression Is Associated With More Aggressive Inflammatory Bowel Disease. Am J Gastroenterol 2018;113:80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Narula N, Pinto-Sanchez MI, Calo NC, et al. Anxiety But Not Depression Predicts Poor Outcomes in Inflammatory Bowel Disease. Inflamm Bowel Dis 2019;25:1255–1261. [DOI] [PubMed] [Google Scholar]
- 20.Long MD, Kappelman MD, Martin CF, et al. Development of an internet-based cohort of patients with inflammatory bowel diseases (CCFA Partners): methodology and initial results. Inflamm Bowel Dis 2012;18:2099–106. [DOI] [PubMed] [Google Scholar]
- 21.Randell RL, Long MD, Cook SF, et al. Validation of an internet-based cohort of inflammatory bowel disease (CCFA partners). Inflamm Bowel Dis 2014;20:541–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Deen WK PD, Kwon MH, Blissett G, Crate DJ, Oberai R, Shah SA, Hwang C, Weaver SA, Siegel CA, Melmed GY. Validating Patient Reported Utilization in the IBD Qorus Learning Health System. Gastroenterology 2019;156:S11. [Google Scholar]
- 23.Thia K, Faubion WA Jr., Loftus EV Jr., et al. Short CDAI: development and validation of a shortened and simplified Crohn’s disease activity index. Inflamm Bowel Dis 2011;17:105–11. [DOI] [PubMed] [Google Scholar]
- 24.Jowett SL, Seal CJ, Phillips E, et al. Defining relapse of ulcerative colitis using a symptom-based activity index. Scand J Gastroenterol 2003;38:164–71. [DOI] [PubMed] [Google Scholar]
- 25.Allegretti JR, Borges L, Lucci M, et al. Risk Factors for Rehospitalization Within 90 Days in Patients with Inflammatory Bowel Disease. Inflammatory Bowel Diseases 2015;21:2583–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hazratjee N, Agito M, Lopez R, et al. Hospital readmissions in patients with inflammatory bowel disease. American Journal of Gastroenterology 2013;108:1024–32. [DOI] [PubMed] [Google Scholar]
- 27.Tinsley A, Naymagon S, Mathers B, et al. Early readmission in patients hospitalized for ulcerative colitis: incidence and risk factors. Scandinavian Journal of Gastroenterology 2015;50:1103–9. [DOI] [PubMed] [Google Scholar]
- 28.Feuerstein JD, Martinez-Vazquez M, Belkin E, et al. 30 day readmissions rate and predictors of readmission in hospitalized patients with ulcerative colitis. Gastroenterology 2014;1):S-375. [Google Scholar]
- 29.Rizk M, Boules M, Michael M, et al. Creation of a novel prospectively based inflammatory bowel disease readmission index. American Journal of Gastroenterology 2016;111:S265–S266. [Google Scholar]
- 30.Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain 2010;150:173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alexakis C, Kumar S, Saxena S, et al. Systematic review with meta-analysis: the impact of a depressive state on disease course in adult inflammatory bowel disease. Aliment Pharmacol Ther 2017;46:225–235. [DOI] [PubMed] [Google Scholar]
- 32.Szigethy E, Murphy SM, Ehrlich OG, et al. Mental Health Costs of Inflammatory Bowel Diseases. Inflamm Bowel Dis 2020. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


