Abstract
Background
We investigated the COVID19-related psychological impact on healthcare workers in Italy and in Italian-speaking regions of Switzerland, three weeks after its outbreak. All professional groups of public hospitals in Italy and Switzerland were asked to complete a 38 questions online survey investigating demographic, marital and working status, presence of stress symptoms and need for psychological support.
Results
Within 38 h a total of 3,038 responses were collected. The subgroup analysis identified specific categories at risk according to age, type of work and region of origin. Critical care workers, in particular females, reported an increased number of working hours, decline in confidence in the future, presence of stress symptoms and need for psychological support. Respondents reporting stress symptoms and those with children declared a higher need for psychological support.
Conclusions
The large number of participants in such a short time indicates for a high interest on topic among health-care workers. The COVID19 outbreak has been experienced as a repeated trauma for many health-care professionals, especially among female nurses' categories. Early evidence of the need of implementating short and long-term measures to mitigate impact of the emotional burden of COVID-19 pandemic are still relevant.
Keywords: COVID-19, early outbreaks, stress, healthcare workers, mental health, hospital management, trauma
Background
The Coronavirus 2019 disease (COVID-19) has been a mass casualty event (1), being stressful and intrusive by affecting daily life and putting adaptive skills to the test.
Psychologically, during the early stages of the outbreak, it has been experienced the so-called alarm stage, because of a virus that confined all of us at home (or at work, in the case of health personnel), putting social relationships, freedom, and economy at strain. Feelings of inadequacy or insufficiency are common, and one can experience a sense of being lost and confused (2). Moreover, mass media provide an incessant heavy load of information about COVID-19, that may act as a potential adding stressor to one's experience of the ongoing pandemic (3).
After the initial stun due to the unimaginable experience of the start of the COVID-19 outbreak, anxiety, irritability, and restlessness come forth. Some physical reactions can mimic the COVID-19 but are linked to somatization of stress: palpitations or difficulty in breathing (expression of sympathetic system activation), cognitive reactions like disorientation, sluggish cognitive tempo, anger, sadness and sleep problems may have appeared, as also the Diagnostic Manual of Mental Disorders suggests in relationship to Acute Stress Disorders 5th edition (DSM-5) (4–8).
It is likely that the whole population would have experienced marked stress reactions, especially on subjects suffering from psychological fragilities already before the COVID-19 outbreak (9, 10).
In this sense, attention on healthcare workers (especially doctors and nurses) has been high since the beginning (11), as they have been the first ones (and maybe the most) under both physical and psychological pressure, because of their frontline role and their major risk of becoming infected (2, 5, 11–13). However, a few studies had focused on healthcare team members other than medical professionals (eg. therapists, obstetricians, pharmacists, technical operators including ones working in the canteens, laundry etc., and others) who also had also been involved into the frontlines since the early start of the COVID-19 pandemic (11–13).
For these reasons, an immediate special task force of Italian-speaking medical specialists in the field of either mental health or emergency medicine was created to give a quick qualitative overview of the mental health status of the whole category of healthcare professionals.
The “Coping with COVID-19” (CwCOVID-19) project was developed in early March, during the first days of the COVID-19 outbreak in Italy and Swiss. The purpose of this project was to support healthcare professionals during the first critical phase of the disease management. This was conducted through a dedicated web service managed by specialists in mental health and emergency medicine and specifically dedicated to healthcare workers, available on social networks, which provided information about acute stress.
Furthermore, the project also aimed to conduct an exploratory overview of stress behaviors and coping skills of healthcare professionals during early phases of COVID-19 outbreak management among Italian-speaking regions, such as northern Italy, where the European outbreak began, and southern Switzerland, that followed a few days later.
Methods
Study Design and Participants
Cw-COVID-19 is an open project developed in the very early days of COVID-19 outbreak by experienced medical specialists, expert in the field of either mental health or emergency medicine.
Between 14th and 16th March 2020, hospital workers of different public hospitals in Switzerland and Italy were asked to complete an online survey regarding the early psychological impact of the COVID-19 outbreak on daily life, at the time point when the virus mainly widespread in northern Italy, Iran and China, but hadn't assumed extensive dissemination in Switzerland yet. Participants were invited to answer the questionnaire via social media (either Facebook®, Instagram®, or WhatsApp®) and agreed voluntarily to the questionnaire being fulfilled. Voluntary participation was stimulated through the social networks (public posts visible on social networks' profiles of the authors or on open channels and groups, and by word of mouth) to collect data from a large and motivated sample.
All data were anonymized, so that, according to the European and Swiss legislation, no informed consent or institutional review board approval was needed. The study was conducted according with the Declaration of Helsinki.
All subjects' categories working in the hospital teams were included, such as physicians, nurses, therapists, obstetricians, pharmacists, technical operators including ones working in the canteens, laundry etc.. and others.
The Coping With COVID-19 (CwCOVID-19) Questionnaire
The Coping with COVID-19 (CwCOVID-19) questionnaire (see Supplementary Material available online) was built on Google Forms (https://www.google.com/forms/about/).
It consisted of 38 items, investigating demographic, social, and working status (gender, age, civil status, the total number of households and of family members aged >65-year-old, years worked in the hospital, type of profession, department, changes in working schedules since the beginning of the outbreak. A few items on previous medical or psychological fragilities have been also explored, such as presence of chronic diseases, alcohol drinking, drugs consumption, smoking status and number of cigarettes per-day, social media use, history of anxiety and medical therapy). Moreover, positive coping attitudes have also been asked (such as time spent doing hobbies or physical activity). Inspiring to the DSM-5, acute stress symptoms have been investigated (eating behavior changes, new symptoms occurring in the last three weeks, number of hours spent to get information and to speak about COVID-19, detachment from family due to the confinement, stress behaviors in children, change in physical contacts). Moreover, need for psychological support (actual perception of the need for qualified psychological support and overall trust in the future) was asked. We decided to not use previously validated scales to catch behaviors and psychological changes associated with the peculiar emergency situation, as explorative surveys have been a method already adopted for other research about pandemics (9–11).
The (closed) form is available at the following link:
Statistical Methods
All anonymized data were collected on an Excel database (Microsoft Excel® 2019) and analyzed.
The exploratory analysis was performed taking into consideration the non-probability nature of the sample, based on unrestricted, self-selected survey, as indicated by Fricker (14).
Statistical analysis was performed using the open-source packages “Pandas,” “NumPy,” “SciPy,” “Seaborn,” and “PyMC” for Mac Os X versions 0.23.0, 11.1.3, 1.1.0, 0.8.1, and 2.3.6, respectively.
Categorical variables are represented either as numbers and percentages in brackets or as medians with interquartile ranges. Continuous variables are listed with means and standard deviations. The Shapiro–Wilk test was performed to evaluate the distribution of the variables.
Our analysis was based on highly Confidence Intervals (CI) of parameter estimates (*). Statistical significance was considered achieved whenever CI would be non-overlapping. To compare proportions in different sub-populations, we performed a Bayesian estimation of the parameter distribution for a Bernoulli stochastic variable using a non-informative uniform prior. The posterior was then plotted to have a graphical overview, and credible intervals were computed by assessing the highest density interval (HDI) at 95%. Only as a reference, whenever two proportions had to be compared, we used also a two-tail P test computation based on classic proportion comparison using chi-square. Statistical significance was considered p < 0.05. All MCMC runs were checked for adequacy based on Raftery-Lewis diagnostics and by visually inspecting Z score plots. MCMC runs were for 40,000 iterations with a 5,000-iteration burn-in (15). Reasonably low effect size of a sample size greater than 2,500 was considered adequate (16).
Results
From 14th March 2020, 8.52 p.m. to 16th March 2020, 10.45 a.m., over 38 h, 3,038 hospital workers completed the survey. The percentage of completed surveys was 97.3% as 79 subjects did not answer one or more questions. All the variables had a skewed distribution.
Sample Characteristics
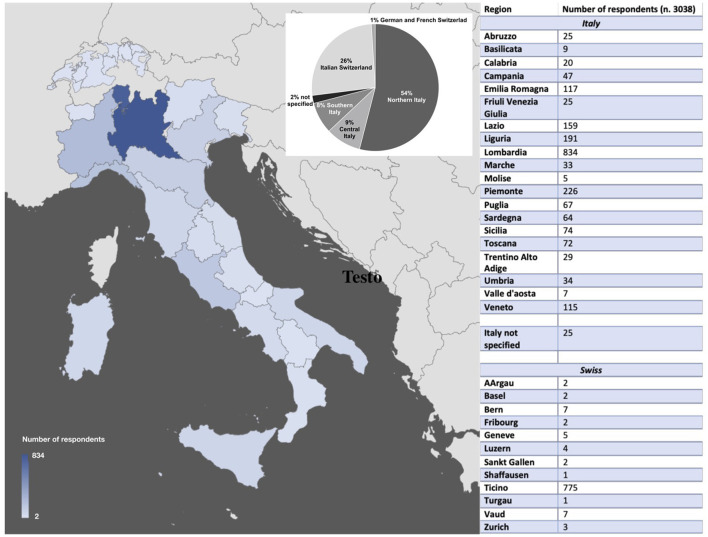
Most of our respondents were physicians, female, aged 26–36. Details on age, gender, regions of origin, and working characteristics are reported in Table 1 and Figure 1.
Table 1.
Demographic, social and work characteristics.
| N | % | ||
|---|---|---|---|
| Country | Italy | 2,176 | 71.6 |
| Switzerland | 804 | 26.4 | |
| Not specified | 58 | 2.0 | |
| Sex | Female | 2,229 | 73.7 |
| Male | 795 | 26.3 | |
| Not specified | 14 | 0.4 | |
| Age (year-old) | 18–25 | 114 | 3.8 |
| 26–35 | 1,035 | 34.1 | |
| 36–45 | 996 | 32.8 | |
| 46–55 | 617 | 20.3 | |
| 56–65 | 253 | 8.3 | |
| Over 65 | 23 | 0.8 | |
| Not specified | 0 | 0 | |
| Kind of job in hospital | Physicians | 1,600 | 53.3 |
| Nurses | 550 | 18.3 | |
| Radiology, intermediate care technicians | 441 | 14.7 | |
| Ambulance services | 87 | 2.9 | |
| Obstetricians | 60 | 2.0 | |
| Administrative | 49 | 1.6 | |
| Technical services | 30 | 1.0 | |
| Hospitality services | 13 | 0.4 | |
| Pharmacy | 7 | 0.2 | |
| Other hospital services | 167 | 5.6 | |
| Civil status | Married | 1,313 | 43.3 |
| Single | 837 | 27.6 | |
| Stable relationship | 672 | 22.2 | |
| Divorced | 172 | 5.7 | |
| Widowed | 25 | 0.8 | |
| Civil Partnership | 13 | 0.4 | |
| Not specified | 6 | 0.1 | |
| Family (number of | 1 | 615 | 20.3 |
| members) | 2 | 769 | 25.4 |
| 3 | 700 | 23.1 | |
| 4 | 663 | 21.9 | |
| 5 | 184 | 6.1 | |
| >5 | 97 | 3.2 | |
| Children <18-year-old | 0 | 1,734 | 57.3 |
| in household | 1 or more | 1,304 | 42.7 |
| Elderly >65-year-old in | 0 | 2,422 | 80.0 |
| household | 1 or more | 616 | 20.0 |
| Years of work in | 0–1 years | 207 | 6.8 |
| hospital | 2–5 years | 623 | 20.5 |
| 5–0 years | 634 | 20.9 | |
| 10–20 years | 858 | 28.3 | |
| 20–30 years | 478 | 15.8 | |
| >30 years | 233 | 7.6 | |
| Not specified | 7 | 0.2 | |
| Physical activity | Once a day | 180 | 5.9 |
| 4-5 times a week | 185 | 6.1 | |
| 2-3 times a week | 855 | 20.3 | |
| Once a week | 439 | 14.5 | |
| Less than once a week | 295 | 9.7 | |
| None at all | 1,081 | 35.6 | |
| Increased number of | No | 2,110 | 70.0 |
| working hours | Up to 10 h | 673 | 22.3 |
| Up to 20 h | 161 | 5.3 | |
| Up to 30 h | 40 | 1.3 | |
| >30 h | 30 | 1.0 |
Characteristics are expressed as absolute value and percentage.
Figure 1.
Participants' regions.
Seventy percent of respondents declared not to have any additional work due to the COVID-19 emergency. Among respondents who answered to have to work more, 59 were ambulance personnel, 38 nurses, 36% administrative personnel, and 30% physicians. Dividing for department, 60 of workers in the intensive care units, 50 of anesthesiologists, 50 of the staff in the emergency departments, and 46% of general practitioners declared to work more than normal.
Risk Categories Among Healthcare Workers, Based on Working Experience
Respondents working in hospitals in the last 20–30 years had the highest percentage of increased number of working hours. By grouping working categories in critical care (intensive care unit, emergency department, anesthesiology, ambulance service), surgery (otorhinolaryngology, neurosurgery, orthopedics, cardiac surgery, urology, gynecology), and general practitioners, surgery resulted to be the group that had to reduce the most the number of working hours (C.I. 25.0–31.7%), whereas the other two groups had to work more (C.I 44.7–52.3% for critical care and 40.8–54.8% for general practitioners). On the contrary, 2,256 (76.4%) subjects did not have to reduce their working hours because of COVID-19 emergency, while 308 (10.4%) had to reduce the work up to ten hours per week, 92 (3.1%) up to 20 h per week, 121 (4.1%) up to 30 h per week. One-hundred and fifty (5.1%) respondents had to be quarantined and 24 (0.8%) reported getting infected with the virus. Twenty-three percent of physicians declared to have to work less than normal. As expected, respondents working in southern Italy (C.I. 16.6–22.8%), where the COVID-19 did not spread yet, declared to work less than their counterparts in northern Italy (C.I. 31.1–35.6%) and Switzerland (C.I. 33.5–48.4%).
Pre-existing Risk Factors for Developing Stress Symptoms Among Healthcare Workers
Almost a half of our sample (1,538 respondents, 50.6%) declared to have a chronic health problem, of whom roughly a quarter (348 subjects, 22.6%) experienced a worsening in their chronic health condition. Appearing of new symptoms were reported by 969 individuals (31.9%) and, more specifically, 285 (9.4%) experienced palpitations, 276 (9.1%) respiratory symptoms, 124 (4.1%) pain, and 285 (9.4%) other symptoms.
Stress Symptoms
Details are reported in Table 2. problems were the category at higher risk to suffer from sleep disturbances (accuracy 82.9%).
Table 2.
Stress symptoms.
| N | % | ||
|---|---|---|---|
| Sleeping | Sleep less than usual | 1,203 | 39.6 |
| Sleep the same number of hours but they feel less rested | 953 | 31.4 | |
| No change | 678 | 22.3 | |
| Sleep more than usual | 172 | 5.7 | |
| Sleep the same number of hours but they feel more rested | 30 | 1.0 | |
| Eating | No change | 1,164 | 38.4 |
| More than usual | 715 | 23.6 | |
| Less than usual | 529 | 17.4 | |
| Same quantity of food, but healthier | 223 | 7.3 | |
| Same quantity but more unhealthy food | 402 | 13.3 | |
| Smoking | Never smoked | 1,820 | 59.9 |
| Started before the last three weeks | 652 | 21.5 | |
| Quitted before the last three weeks | 487 | 16.1 | |
| Started in the last three weeks | 27 | 0.9 | |
| Quitted smoking in the last three weeks | 41 | 1.4 |
Characteristics are expressed as absolute value and percentage.
Eating habits changed in 1,869 (61.5%) hospital workers and 679 (22.3%) declared to be active smokers. Among them, 268 subjects (39.5%) had to increase the number of cigarettes (cigars, e-cigarettes, etc.) smoked per day in the last 3 weeks. One-thousand-six-hundred-fifty-seven respondents (55.1%) stated to drink alcohol occasionally or regularly. Among them, 57 (3.4%) started in the last 3 weeks and 255 (15.3%) declared that their consumption had increased in the last 3 weeks. The vast majority of respondents said that they never used drugs (2,756, 91.1%), whereas 129 quitted before the last 3 weeks (4.2%) and three (0.1%) within the last 3 weeks.
Regarding the item investigating time spent on searching information about COVID-19, 654 respondents (21.1%) declared less than an hour per day, 1112 (36.7%) between one and 2 h, 1,094 (36.1%) more than 2 h per day, and 173 (5.7%) did not look at such information. Nearly half of our sample (1,369 subjects, 45.1%) reported talking about the COVID-19 outbreak with family, friends and colleagues for more than two hours per day, 1,116 (36.8%) between one and 2 h, 505 (16.7%) for less than an hour and 44 (1.4%) did not spend time speaking about COVID-19.
Among respondents with children, 451 (26.0%) reported excessive crying or unusual irritation, 308 (17.7%) noticed a behavioral regression, 186 (10.7%) noticed unusual headaches or other unexplained pain sensations, 752 (43.3%) reported anxiety and concern about the COVID-19 outbreak.
Physical activity was reduced in 1,428 (47.0%) subjects in the last 3 weeks, while 125 (6.3%) said they could increase it. The physical contacts diminished in 2,875 subjects (94.9%), increased in 12 (0.4%), and did not change in 143 (4.7%). As opposed to physical contacts, virtual contacts increased for 1,960 individuals (64.6%), diminished for 175 subjects (5.8%), and did not change for 898 (29.6%). Hobbies and other activities undertaken for pleasure or relaxation diminished for 1,908 persons (63%), increased for 260 persons (8.6%), and did not change for 862 (28.4%). A statistically significant correlation was found between an increased number of working hours and stress symptoms such as eating less or more, sleeping less or not feeling relaxed, drinking or smoking more.
One thousand two hundred and eighty-four respondents (42.4%) declared they are separated from their family because of COVID-19.
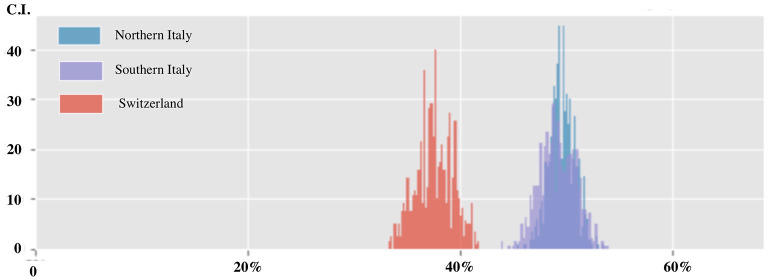
Need for Psychological Support and Confidence in the Future
In the last 3 weeks, 706 respondents perceived to need specialized psychological support (23.3%). Confidence in the future was diminished for 1,404 persons (46.3%), increased for 246 subjects (8.1%), and did not change for 1,384 (45.6%). Individuals feeling the need of professional psychological support were more often female (C.I. 24.8–28.3 vs. 13.0–17.1% for females and males, respectively), in a couple (C.I. 23.7–27.4%) or subjects reporting stress symptoms (Figure 2). Long-career workers (C.I. 7.1–15.0%) and ambulance services (C.I. 7.5–20.8%) expressed less often the need for psychological support. As reported in Figure 3, different professional categories expressed different psychological support need. Subjects stating increased confidence in the future were more often males (C.I 5.4–11.6% vs. 9.2–30.2% for females). As expected, among respondents with diminished confidence in the future there was a higher prevalence of females (C.I 34.2–60.6% vs. 32.6–45.7% for males).
Figure 2.
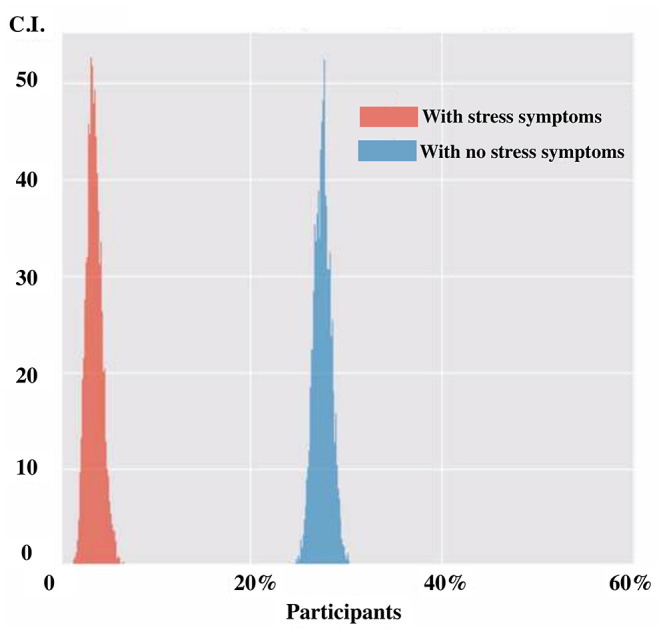
Need for psychological support in participants with and without stress symptoms.
Figure 3.
Need for psychological support according to professional categories.
High-Risk Categories for Developing Stress Symptoms Among Healthcare Workers
Plotting the data by country, the confidence in the future in the last three weeks was more lowered in respondents from Italy as compared to Switzerland (C.I. 46.0–52.3% vs. 34.2–41.1%) (see Figure 4). This difference did not change by plotting data either by work category or by age or length of career. Surprisingly, by plotting the decreased confidence in the future for the type of hospital work, all categories were equally affected except of ambulance services (C.I. 16.1–33.6% vs. 40.0–51.2% for other categories).
Figure 4.
Confidence in the future among healthcare workers divided by geographical region (Nothern Italy, Southern Italy and Swiss).
The decision tree analysis showed a higher probability of sleeping less than normal (accuracy 62.2%) in respondents aged >30 from Italy and having one or more children in their family. In particular, nurses of critical care with a history of anxiety. Finally, history of anxiety resulted to be an independent factor associated to reduced confidence in the future (C.I. 47.7–60.2 vs. 37.6–42.5% with and without a history of anxiety, respectively).
Discussion
The present study highlights elevated stress levels in a cohort of Italian-speaking hospital workers during the early phases of the outbreak of Sars-Cov2 infection due to the novel COVID-19, independently from the appurtenance to different countries (Italy and Swiss). To the best of our knowledge, our study was the earliest to explore the psychological impact of this novel pandemic on healthcare workers among Italian-speaking countries (Italy and Italian-speaking regions of Switzerland). From our analysis, being female, working as a nurses and subjects having previous problems of anxiety has been the main predictor for referring stress symptoms (Figure 3).
Generally speaking, healthcare workers have been firstly involved in the catastrophic events caused by the massive COVID-19 outbreak (10–12). Beyond demanding clinical and logistic issues, hospital employees have to deal with their own physical and mental health (17–23). Work-related stress has shown to impact physician's mental health, patients' care quality, and the efficiency of the healthcare system (20). Consequences in terms of mental health in the context of maxi-emergency situations may be even more pronounced than normal. Feelings of inadequacy, insufficiency or confusion are common and hospital workers may even experience negative behavioral reactions, depression and illness, possibly leading to lack of effectiveness and efficiency at work (4–6).
The large number of responses and the small percentage of uncompleted surveys (2, 7%) in less than 40 h indicates the high interest in the subject among healthcare personnel. This may also express the need among healthcare workers to communicate, to be heard, and understood that encompasses professional attitude and rules of conduct and touches the psyche and emotions.
More than 50% of survey participants were physicians, likely because the survey promoters were physicians both in southern Switzerland and northern Italy and invitations to participate were sent through personal contacts and social media. However, the high turnout rate of several other hospital categories could mirror the concept that the present is a common burden among all health workers.
Demographics, Social and Working Distribution
The group aged 26–45 represents the majority of the sample, probably because it is, are more likely to be reached by social media. The small number of respondents aged between 18 and 25 is likely to reflect the relatively low number of very young respondents working in hospitals as confirmed by the fact that medical trainees under 26-years of age are not yet medical doctors in Italy and Switzerland. The distribution of worked years in the hospitals roughly reflects the age distribution.
In our sample, two-thirds of survey participants were female, which could be interpreted to a growing percentage of female medical professionals. In our sample, percentages of married, single, divorced etc., and other demographic characteristics were grossly comparable to the Swiss and Italian population (24, 25).
Nearly one third of hospital workers in our study had to increase their working activity. It represents the first, well-recognized stress factor, proportional to the increase of worked hours (26). As expected, health care professionals having to increase their working hours, are those employed either in critical care settings or general practitioners, the first categories having to be confronted with the COVID-19 emergency. On the other hand, in several hospitals in northern Italy and southern Switzerland, a dramatic reduction of surgical elective cases and outpatient clinic activity has been deemed necessary to contain virus spread and, as a consequence, surgeons as a category experienced a reduction in working hours. Notwithstanding, a reduction of working hours should be considered insidious, as it could nonetheless jeopardize the mental status and could lead to depressive symptoms, hopelessness, and uselessness (27).
Stress Symptoms
Sleep disturbances can be caused by stress and be related to Post-Traumatic Stress Disorder (PTSD) and the first response is generally considered a period of arousal and wakefulness (28, 29). A great proportion of hospital workers in our study declared to sleep less than normal and to feel less restored by sleep in general, presumably as a reaction to the stressful circumstances and it is likely to reflect the high prevalence of sleep arousal and anxiety symptoms in healthcare professionals.
The correlation analysis showed a relatively higher prevalence of stress symptoms among young professionals with at least one child to care for, as a response of having to face the COVID-19 outburst emergency.
Similarly, an increase or a decrease in in food intake may mirror a reaction to a stressful situation and, actually, in our sample, only 40% of the interviewed reported no change (30). Moreover, among smokers, there was a high proportion of participants that declared to have increased the number of cigarettes per day in the first 3 weeks since the outbreak onset. A smaller, but significant proportion of respondents reported an increase in alcohol consumption. All these behavioral changes can be considered stress symptoms (31, 32). In our study, a strong correlation was found between the above-mentioned symptoms and the need for psychological support. Respondents reporting such symptoms were more prone to report the need for psychological support. As far as we know, this is the first time that such a need is quantified within the emergency of COVID-19.
Need for Psychological Support
Interestingly, respondents with children reported the most stressful answers and felt the need for professional psychological support more often than their non-parenting peers (accuracy 62.2%). Despite some might consider this obvious, such data are nonetheless of outstanding importance, as hospital employees are often in the fertile age range. In the setting of a massive viral outbreak, hospital caregivers experience important issues in caring for their children because of the closure of schools and other facilities. Parents probably do not experience only the stress related to future uncertainty but also the fear of getting infected and possibly transmit such an infectious disease to their offspring. Specifically, COVID-19 has shown to be particularly infective also for hospital workers and casualties have been reported among hospital staff (10–12). Coherently, many hospital workers with children (nearly 95%) declared to have reduced physical contact with other family components.
Almost all subcategories of hospital workers perceive the stress related to the outbreak equally. Only long-career workers and ambulance service personnel reported needing psychological support less as compared to other categories. This may be explained by the high level of experience and long-standing training in stress management in long-career employees. On the other hand, emergency services personnel may be used to address stressful situations, as they are part of a coordinated and ordered emergency response and have to constantly handle very high levels of stress (33, 34).
The actual outbreak could be a repeated trauma for many healthcare categories, putting them at risk of psychiatric sequelae such as PTSD (8, 35). It is of outstanding importance in such a critical situation to promptly implement measures to mitigate the impact of the emotional burden of the present COVID-19 pandemic while at the same time dealing with its clinical challenges (2, 4).
Positive behaviors such as healthy eating, sport practicing, and sleeping an adequate number of hours have shown to impact and reduce the impact of stress (36). Many other strategies have also shown to be effective, such as the implementation of debriefing sessions and group therapies to share experiences and relieve the sorrow related to challenging and stressful situations. Programs of de-escalation of tension through mindfulness techniques could be also cost-effective and easily implemented in routine practice to prevent future development of acute and chronic PTSD, major depression or suicidal behaviors (37–39).
Our study has several limitations. Firstly, our data were collected in a completely anonymized and we have not certainty on their truthfulness. Moreover, a biased sample of subjects' more at risk of developing stress symptoms could have been more induced to answer the survey or, on the contrary, maybe busiest, or more stressed healthcare workers did not access social media. In addition, another limitation that has to be mentioned is the fact that we did not have enough data for discriminating stress symptoms among healthcare workers that were asked to do professional tasks out of their area of expertise.
Furthermore, the CwCOVID-19 questionnaire had not been previously validated. This may limit the comparisons with other studies but enables the evaluation of pandemic-related stress symptoms. This approach was inspired by similar studies during other pandemics (9) or the present (10).
Nonetheless, our data denote a certain internal coherence, that can be interpreted as trustworthiness. Here we present the very first evaluation on stress symptoms in a representative sample of healthcare professionals in the European continent, that was composed of (mainly) medical doctors but also of several types of healthcare workers.
Conclusions
Perceived psychological burden among healthcare workers should be considered relevant since the early phases of an infectious disease widespread. COVID-19 outbreak has, therefore, to be considered as a major stressor, that was able, since the beginning, to threaten the physiological and psychological integrity of healthcare professionals. This may lead hospital efficiency at jeopardization. Facing the following events of 2020 and the still ongoing 2021, healthcare workers should be under close psychological monitoring and long-term psychological counseling for them should be provided.
Further studies in different time points of the outbreak are needed to understand the impact of COVID-19 emergency on healthcare workers' psychology and mental health.
Author's Note
LU is an Emergency Medicine specialist (MD, PhD) who received a 4-year-special-training in Cognitive Behavioral Therapy at the Cognitive Behavioral Therapy School of Milan (https://studicognitivi.it). SaU (MD) is a psychiatrist and neurologist trained in developmental medicine. All the authors have scientifically and clinically shared working experience, have published past researches on impacted journals and are committed to ameliorate healthcare workers job conditions.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LU, SaU, and LP designed the study. LU was involved in constructing the dataset, interpreting data, and drafting the manuscript. PM-H, FM, StU, CZ, and LP helped in data collection and revising the final questionnaire. All authors discussed the results and commented on the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This work was developed within the framework of the DINOGMI Department of Excellence of MIUR 2018–2022 (law 232/2016). The authors acknowledge all healthcare workers among them, and the ones who participated into the survey.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.768036/full#supplementary-material
References
- 1.Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. (2020) 92:548–51. 10.1002/jmv.25722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiat. (2020) 7:e15–6. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiat. (2020) 7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacobowitz W, Moran C, Best C, Mensah L. Post-Traumatic stress, trauma-informed care, and compassion fatigue in psychiatric hospital staff: a correlational study. Issues Ment Health Nurs. (2015) 36:890–9. 10.3109/01612840.2015.1055020 [DOI] [PubMed] [Google Scholar]
- 5.Xiao H, Zhang Y, Kong D, Li S, Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. (2020) 26:e923549. 10.12659/MSM.923549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinberg A, Creed F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet. (2000) 355:533–7. 10.1016/S0140-6736(99)07366-3 [DOI] [PubMed] [Google Scholar]
- 7.Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. (2020) 88:916–9. 10.1101/2020.02.29.20029322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Chapter: “Trauma- and Stressor-Related Disorders”: American Psychiatric Association (2013). 10.1176/appi.books.97808904255968723190 [DOI] [Google Scholar]
- 9.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uccella S, De Grandis E, De Carli F, D'Apruzzo M, Siri L, Preiti D, et al. Impact of the COVID-19 outbreak on the behavior of families in italy: a focus on children and adolescents. Front Public Health. (2021) 9:608358. 10.3389/fpubh.2021.608358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. (2020) 369:m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Firew T, Sano ED, Lee JW, Flores S, Lang K, Salman K, et al. Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers' infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open. (2020) 10:e042752. 10.1136/bmjopen-2020-042752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kinder M. Essential but undervalued: millions of health care workers aren't get- ting the pay or respect they deserve in the COVID-19 pandemic. Brookings 2020 published online May 28. Available online at: https://www.brookings.edu/research/essen. 10.1353/eca.2020.0007 [DOI]
- 14.Fricker RD. Sampling methods for web and e-mail surveys. In: The SAGE Handbook of Online Research Methods: SAGE Publications, Ltd (2008). p. 195–216. 10.4135/9780857020055.n11 [DOI] [Google Scholar]
- 15.Kruschke JK. Bayesian estimation supersedes the t-test. J Exp Psychol Gen. (2013) 142:573–603. 10.1037/a0029146 [DOI] [PubMed] [Google Scholar]
- 16.Eng J. Sample size estimation: how many individuals should be studied? Radiology. (2003) 227:309–13. 10.1148/radiol.2272012051 [DOI] [PubMed] [Google Scholar]
- 17.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. China novel coronavirus investigating and research team. a novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schwartz J, King CC, Yen MY. Protecting health care workers during the COVID-19 coronavirus outbreak-lessons from Taiwan's SARS response. Clin Infect Dis. (2020) 71:858–860. 10.1093/cid/ciaa255Q19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Lancet Null . COVID-19: protecting health-care workers. Lancet. (2020) 395:922. 10.1016/S0140-6736(20)30644-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiat. (2020) 7:e14. 10.1016/S2215-0366(20)30047-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiat. (2020) 7:e20. 10.1016/S2215-0366(20)30076-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rasool SF, Wang M, Zhang Y, Samma M. Sustainable work performance: the roles of workplace violence and occupational stress. Int J Environ Res Public Health. (2020) 17:912. 10.3390/ijerph17030912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seo D, Ahluwalia A, Potenza MN, Sinha R. Gender differences in neural correlates of stress-induced anxiety. J Neurosci Res. (2017) 95:115–25. 10.1002/jnr.23926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Istat.it Popolazione e famiglie [Internet] . Available online at: https://www.istat.it/it/popolazione-e-famiglie?dati. [accessed July, 1 2020]
- 25.Statistik B, für. Bundesamt für Statistik [Internet]. Available online at: https://www.bfs.admin.ch/bfs/de/home.html. [accessed June, 29 2020]
- 26.Wong K, Chan AHS, Ngan SC. The effect of long working hours and overtime on occupational health: a meta-analysis of evidence from 1998 to 2018. Int J Environ Res Public Health. (2019) 16:2102. 10.3390/ijerph16122102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagae M, Sakamoto M, Horikawa E. Work-sharing and male employees' mental health during an economic recession. Occup Med. (2017) 67:648–51. 10.1093/occmed/kqx135 [DOI] [PubMed] [Google Scholar]
- 28.Fan F, Zhou Y, Liu X. Sleep disturbance predicts posttraumatic stress disorder and depressive symptoms: a cohort study of Chinese adolescents. J Clin Psychiatry. (2017) 78:882–8. 10.4088/JCP.15m10206 [DOI] [PubMed] [Google Scholar]
- 29.Sanford LD, Suchecki D, Meerlo P. Stress, arousal, and sleep. Curr Top Behav Neurosci. (2015) 25:379–410. 10.1007/7854_2014_314 [DOI] [PubMed] [Google Scholar]
- 30.Ulrich-Lai YM, Fulton S, Wilson M, Petrovich G, Rinaman L. Stress exposure, food intake, and emotional state. Stress. (2015) 18:381–99. 10.3109/10253890.2015.1062981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Damron KR. Review of the relationships among psychosocial stress, secondhand smoke, and perinatal smoking. J Obstet Gynecol Neonatal Nurs. (2017) 46:325–33. 10.1016/j.jogn.2017.01.012 [DOI] [PubMed] [Google Scholar]
- 32.Ramchandani VA, Stangl BL, Blaine SK, Plawecki MH, Schwandt ML, Kwako LE, et al. Stress vulnerability and alcohol use and consequences: from human laboratory studies to clinical outcomes. Alcohol. (2018) 72:75–88. 10.1016/j.alcohol.2018.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berge JM, Tate A, Trofholz A, Fertig AR, Miner M, Crow S, et al. Momentary parental stress and food-related parenting practices. Pediatrics. (2017) 140:e20172295. 10.1542/peds.2017-2295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carley S, Mackway-Jones K, Donnan S. Major incidents in Britain over the past 28 years: the case for the centralised reporting of major incidents. J Epidemiol Community Health. (1998) 52:392–8. 10.1136/jech.52.6.392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bloomfield MAP. Trauma and post-traumatic stress disorder: children should be seen and heard. Lancet Psychiat. (2019) 6:193–4. 10.1016/S2215-0366(19)30037-9 [DOI] [PubMed] [Google Scholar]
- 36.Carmassi C, Gesi C, Corsi M, Cremone IM, Bertelloni CA, Massimetti E, et al. Exploring PTSD in emergency operators of a major University Hospital in Italy: a preliminary report on the role of gender, age, and education. Ann Gen Psychiat. (2018) 17:17. 10.1186/s12991-018-0184-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Phillips C. Brain-derived neurotrophic factor, depression, and physical 1114 activity: making the neuroplastic connection. Neural Plast. (2017) 1115 2017:7260130. 10.1155/2017/7260130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dalton J, Thomas S, Harden M, Eastwood A, Parker G. Updated meta-review of evidence on support for carers. J Health Serv Res Policy. (2018) 23:196–207. [DOI] [PubMed] [Google Scholar]
- 39.Sripada RK, Bohnert KM, Ganoczy D, Blow FC, Valenstein M, Pfeiffer PN. Initial group versus individual therapy for posttraumatic stress disorder and subsequent follow-up treatment adequacy. Psychol Serv. (2016) 13:349–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.