Abstract
The aim of this case report is to present an early individualized rehabilitative plan for a post-stroke patient with limb spasticity given that stroke is a leading cause for disability that involves prolonged hospital stay and neurorehabilitation strategies. The rehabilitation plan consisted of conventional physical therapy and radial extracorporeal shock wave therapy (rESWT), and the results were evaluated through clinical assessment together with an innovative gait analysis system. Two rESWT sessions and conventional physical therapy program decreased spasticity grade and pain intensity, and improved ankle range of motion, balance and gait.
Keywords: Stroke, spasticity, neurologic rehabilitation, extracorporeal shock wave therapy
Introduction
Stroke is a major cause of disability implying spasticity, muscle weakness, impaired sensorimotor function, poor balance, or altered gait [1].
Adapted rehabilitation therapies and clinical evaluations should be implemented from the subacute phase of stroke (according to Stroke Recovery and Rehabilitation Round-table consensus-2017, time points for subacute stroke recovery are defined between 7 days and 3 months).
During the past years, extracorporeal shock wave therapy (ESWT) has been used as a non-invasive therapy with promising results for post-stroke spasticity treatment and management [2,3].
After stroke, balance and motor recovery depend on neuronal plasticity and the structural reorganization of the brain, consisting of a wide variety of complex processes, thus the necessity of early initiation of rehabilitation programs [4,5].
In this article we aimed to investigate the efficacy of conventional physical therapy and radial extracorporeal shock wave therapy (rESWT) on lower limb spasticity in a patient in the subacute phase of stroke.
Gait and functionality are commonly affected in stroke patients, and objective evaluation tools are needed in addition to the clinical assessments.
Apart from the Modified Ashworth Scale for grading spasticity and different international scales and scores, a gait analysis system was added to the clinical evaluation, and results were correlated with clinical parameters.
Further outcomes focused on pain intensity, passive range of motion, mobility, ambulation capacity, and adverse events.
The case of a 75-year-old female presenting post-stroke spasticity is described and radial extracorporeal shock wave therapy together with classical conventional physical therapy program were applied.
Case Report
In order to participate in this study conducted according to the Declaration of Helsinki, the patient signed the written consent.
A 75-year-old female was hospitalized to the Physical and Rehabilitation Medicine Department, Elias University Emergency Hospital with post-stroke spasticity and right hemiparesis due to an ischemic stroke.
Regarding the spasticity of the upper and lower limbs, the patient presented grade 2 on the Modified Ashworth Scale (MAS) at admission.
At clinical examination also presented left-sided hemiparesis and mild lower limb pain.
By the time the patient was found unconscious at home, she suffered a traumatic brain injury, also presenting periorbital and epicranial hematoma.
The clinical examination was otherwise unremarkable.
The patient’s past medical history was significant for hypertension, dyslipidemia, and severe carotid artery stenosis.
Otherwise, her past surgical history was not significant.
Based on the clinical grounds and laboratory tests, a conventional physical therapy program combined with radial extracorporeal shock wave therapy (rESWT) were initiated from the admission.
Conventional physical therapy includes therapies and techniques conducted in accordance to each rehabilitation center or facility.
Consequently, we initiated therapies involving rESWT (by using Endopuls 811), balance and gait training, stretching, physical agents, active and passive range of motion exercises, and core stability exercises.
Regarding the rESWT, the patient received 2000 shots with a frequency of 10Hz, and energy density of 60mJ on the myotendinous junction of the gastrocnemius and the soleus muscles.
The patient received one rESWT session/week during two weeks, and she tolerated the intervention without any difficulty or adverse events.
The clinical outcomes focused on spasticity grade according to the MAS, pain intensity assessed by the Visual Analogue Scale (VAS), balance and gait evaluated through Tinetti Assessment Tool and Functional Ambulation Categories (FAC), and ankle passive mobility was evaluated using the passive range of motion (PROM) using a hand-held goniometer.
For stance and gait evaluation, Walker View system (TecnoBody®, Bergamo, Italy) was used to provide a full analysis through real-time visual feedback.
In addition to clinical outcome measures, data provided through Walker View system offered an integrated analysis, and all outcome measures were correlated aiming an objective assessment.
Clinical evaluation and computed analysis were performed at three different timeframes T0 (baseline), T1 (the end of the rehabilitation plan), and T2 (8 weeks after patient discharge), respectively.
The patient showed significant improvement at T1 and T2, suggesting long-term efficacy of the classical conventional rehabilitative program combined with rESWT as non-invasive therapy for patients experiencing pain, gait and balance deficits due to post-stroke spasticity.
The spasticity grade decreased by one point according to the ranking of the Modified Ashworth Scale (MAS), and it maintained the same level at 8 weeks follow-up. The gain was significant at T1 and T2 evaluations for ankle passive range of motion (PROM).
The score decreased by one point at T1 and maintained at T2, concerning the pain intensity evaluated through the Visual Analogue Scale (VAS).
The patient also showed improved mobility, balance, and gait on the short-term and on the long-term, according to the scores of the Tinetti Assessment Tool and Functional and Ambulation Categories (FAC).
Regarding the gait analysis through recent technology such as Walker View system, the gait pattern improved at T1, maintaining a satisfying level at 8 weeks follow-up.
The step length and contact time improved significantly at T1 compared to the assessment conducted at T0.
Regarding the stance phase, the foot flexion-extension and eversion-inversion improved at T1 assessment and maintained at T2. As for the swing phase, the eversion-inversion showed improvement at T1 and T2 compared to the assessment at T0.
However, concerning the foot flexion-extension during swing, it only showed improvement at T1.
A complete review of clinical outcomes and Walker View analysis is presented in Table 1.
Table 1.
Clinical outcome measures and Walker View analysis at T0, T1, T2
|
Clinical outcome measures and Walker View analysis |
T0 |
T1 |
T2 |
|
MAS |
3 |
2 |
2 |
|
Ankle PROM (degrees) |
38 |
48 |
45 |
|
VAS |
2 |
1 |
1 |
|
Tinetti Assessment Tool |
12 |
20 |
20 |
|
FAC |
4 |
5 |
5 |
|
Trunk flexion-extension (degrees) |
8.4 |
10.5 |
10.2 |
|
Trunk lateral flexion (degrees) |
4.2 |
6.6 |
6.5 |
|
Left hip flexion-extension (degrees) |
6.4 |
12.8 |
12 |
|
Left knee flexion-extension (degrees) |
28.5 |
35.5 |
34 |
|
Left foot pitch (degrees) |
52 |
55 |
60 |
|
Left foot roll (degrees) |
8 |
12 |
17 |
Note: Abbreviations: FAC: Functional Ambulation Categories; MAS: Modified Ashworth Scale; PROM: passive range of motion; VAS: Visual Analogue Scale. T0: baseline evaluation; T1: assessment at the end of the rehabilitation plan; T2: assessment at 8 weeks after discharge
Additionally, compared to T0, the foot pitch and foot roll scored improvements at T1 and T2. Post-processing data were performed through MATLAB (R2016a, The MathWorks, Inc, Natick, MA, USA), and the results are highlighted in Figure 1 and Figure 2.
Figure 1.
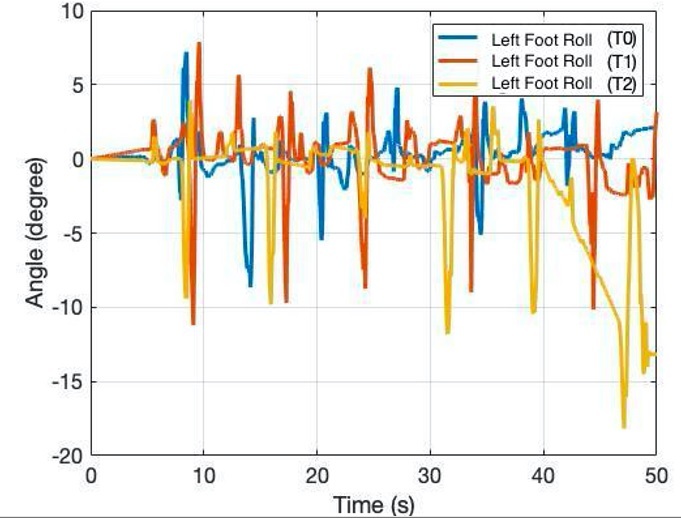
Left foot roll assessment through Walker View system (data processed in MATLAB)
Figure 2.
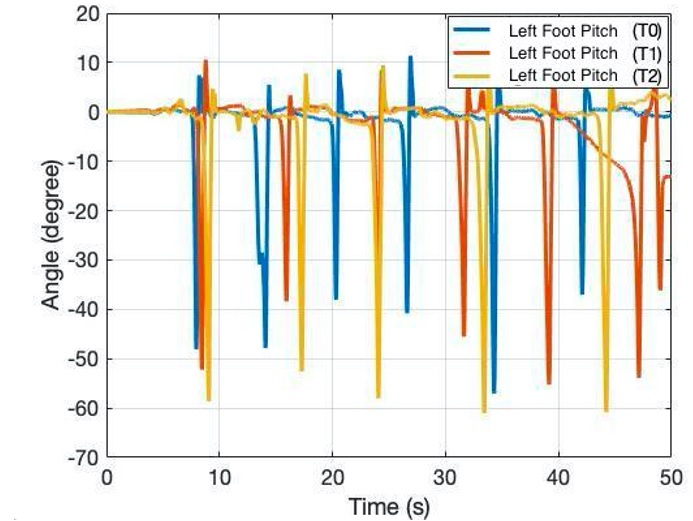
Left foot pitch assessment through Walker View system (data processed in MATLAB)
The patient showed satisfying functional mobility, decreased spasticity grade and pain intensity, improved balance and gait proving effectiveness of early phase neurorehabilitation strategies implementation at discharge and at 8 weeks follow-up.
Satisfying levels of these outcomes at 8 weeks follow-up for a patient who underwent an early individualized rehabilitative program consisting of conventional physical therapy and two rESWT sessions, showed long-term effectiveness of these therapies for all outcomes.
No adverse events were reported during or afterwards the rESWT application or during the neurorehabilitation program.
Discussion
The aim of this paper was to assess the benefit of early initiation of the rehabilitation program for a patient in the subacute phase of stroke, suffering from left spastic hemiplegia.
The rehabilitation program consisted of conventional physical therapy and two sessions of radial extracoporeal shock wave therapy (rESWT), showing efficacy for the MAS grade and ankle passive range of motion (PROM), the results being consistent with those from other studies [2,3].
Additionally, through sessions of radial extracorporeal shock wave therapy which induced long-term tissue regeneration, anthalgic and anti-inflammatory properties, pain intensity also decreased upon muscles and tendons [6].
Correlated with the gait analysis provided through Walker View system, the Tinetti Assessment Tool and Functional Ambulation Categories (FAC) also showed improvement.
The gait pattern was ameliorated, and improvements were significant both for the stance and the swing phase through a full stance and gait analysis.
As a tool added to the clinical evaluation, quantitative gait analysis through Walker View system provided objective parameters.
Since the rehabilitation process for post-stroke patients requires a significant amount of time, data can be stored on the system and used anytime during hospital stay or tele-rehabilitation program, as it can offer comparative evaluations [7].
During coronavirus disease (COVID-19) pandemic context, tele-medicine and especially tele-rehabilitation approach could be taken into account as strategies which can enhance classical rehabilitation programs, assist the patient, and improve quality of care and satisfaction for persons with chronic conditions [8,9,10].
To promote the rehabilitation program with satisfying results for post-stroke patients, we proposed the initiation of the rehabilitative program from the subacute phase of stroke.
We were able to clinically assess spasticity grade, functional capacity, mobility, pain intensity, and gait and to associate them with data from a recent technological assessment.
By tracking progress and leading to a more adapted rehabilitation plan and evaluation, this strategy provided objective data.
Another important aspect is that in addition to the clinical evaluation, through stance and gait analysis, classic rehabilitation programs for stroke survivors are more easily adapted and assessed, leading to a more significant functional improvement for such patients.
Although frequently used for limb spasticity, the botulinum toxin injection was not used in this early stage of rehabilitation as we chose to promote recovery through non-invasive therapies.
At a new follow-up, after clinical and ultrasound evaluations we will assess the spasticity grade and will also consider using the botulinum toxin injection added to rESWT and classical rehabilitation.
Conclusion
The patient presented a lower spasticity grade and pain intensity, stance, balance and gait improvement at discharge and at 8 weeks follow-up.
The interventions proved long-term effectiveness and a good safety profile.
Through objective evaluation, the case highlighted the long-term effectiveness of the classical conventional physical therapy and the non-invasive technique of radial extracorporeal shock wave therapy (rESWT) for a patient in the subacute phase of stroke with lower limb spasticity.
In addition, predictive analysis could lead to more adapted rehabilitative techniques in different clinical and rehabilitation centers.
These results have to be confirmed in a future work by new clinical trials and also, future research should focus on timely adapted approaches, neurorehabilitation techniques and objective assessment tools.
Conflict of interests
None to declare.
References
- 1.Katan M, Luft A. Global Burden of Stroke. Semin Neurol. 2018;38(2):208–211. doi: 10.1055/s-0038-1649503. [DOI] [PubMed] [Google Scholar]
- 2.Wu YT, Chang CN, Chen YM, Hu CG. Comparison of the effect of focused and radial extracorporeal shock waves on spastic equinus in patients with stroke: a randomized controlled trial. Eur J Phys Rehabil Med. 2018;54(4):518–525. doi: 10.23736/S1973-9087.17.04801-8. [DOI] [PubMed] [Google Scholar]
- 3.Mihai EE, Dumitru L, Mihai IV, Berteanu M. Long-Term Efficacy of Extracorporeal Shock Wave Therapy on Lower Limb Post-Stroke Spasticity: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Med. 2020;10:86–86. doi: 10.3390/jcm10010086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koroleva ES, Kazakov SD, Tolmachev IV, Loonen AJM, Ivanova SA, Alifirova VM. Clinical Evaluation of Different Treatment Strategies for Motor Recovery in Poststroke Rehabilitation during the First 90 Days. J Clin Med. 2021;10(16):3718–3718. doi: 10.3390/jcm10163718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pollock A, Baer G, Pomeroy V, Langhorne P. Physiotherapy treatment approaches for the recovery of postural control and lower limb function following stroke. Cochrane Database Syst Rev. 2003;2:CD001920–CD001920. doi: 10.1002/14651858.CD001920. [DOI] [PubMed] [Google Scholar]
- 6.Mariotto S, de Prati AC, Cavalieri E, Amelio E, Marlinghaus E, Suzuki H. Extracorporeal shock wave therapy in inflammatory diseases: molecular mechanism that triggers anti-inflammatory action. Curr Med Chem. 2009;16(19):2366–2372. doi: 10.2174/092986709788682119. [DOI] [PubMed] [Google Scholar]
- 7.Mohan DM, Khandoker AH, Wasti SA, Ismail Ibrahim Ismail Alali S, Jelinek HF, Khalaf K. Assessment Methods of Post-stroke Gait: A Scoping Review of Technology-Driven Approaches to Gait Characterization and Analysis. Front Neurol. 2021;12:650024–650024. doi: 10.3389/fneur.2021.650024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Capra R, Mattioli F. Tele-health in neurology: an indispensable tool in the management of the SARS-CoV-2 epidemic. J Neurol. 2020;267(7):1885–1886. doi: 10.1007/s00415-020-09898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hau YS, Kim JK, Hur J, Chang MC. How about actively using telemedicine during the COVID-19 pandemic. J Med Syst. 2020;44(6):108–108. doi: 10.1007/s10916-020-01580-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mihai EE, Popescu MN, Beiu C, Gheorghe L, Berteanu M. Tele-Rehabilitation Strategies for a Patient With Post-stroke Spasticity: A Powerful Tool Amid the COVID-19 Pandemic. Cureus. 2021;13(11):e19201–e19201. doi: 10.7759/cureus.19201. [DOI] [PMC free article] [PubMed] [Google Scholar]


