Abstract
Although diabetic kidney disease (DKD) remains the leading cause of end-stage kidney disease eventually requiring chronic kidney replacement therapy, the prevalence of DKD has failed to decline over the past 30 years. In order to reduce disease prevalence, extensive research has been ongoing to improve prediction of DKD onset and progression. Although the most commonly used markers of DKD are albuminuria and estimated glomerular filtration rate, their limitations have encouraged researchers to search for novel biomarkers that could improve risk stratification. Considering that DKD is a complex disease process that involves several pathophysiologic mechanisms such as hyperglycemia induced inflammation, oxidative stress, tubular damage, eventually leading to kidney damage and fibrosis, many novel biomarkers that capture one specific mechanism of the disease have been developed. Moreover, the increasing use of high-throughput omic approaches to analyze biological samples that include proteomics, metabolomics, and transcriptomics has emerged as a strong tool in biomarker discovery. This review will first describe recent advances in the understanding of the pathophysiology of DKD, and second, describe the current clinical biomarkers for DKD, as well as the current status of multiple potential novel biomarkers with respect to protein biomarkers, proteomics, metabolomics, and transcriptomics.
Keywords: Biomarkers, Diabetic nephropathies, Inflammation, Metabolomics, Oxidative stress, Pathophysiology, Proteomics, Transcriptome
INTRODUCTION
Diabetic kidney disease (DKD) occurs in 25% to 40% of patients with diabetes mellitus (DM), and is the leading cause of kidney failure worldwide [1]. Given this high-risk of progressive kidney function decline, resulting in end-stage kidney disease (ESKD) eventually requiring kidney replacement therapy, early identification of high-risk patients is important. Although our understanding of this disease process has improved over the years, unlike other diabetic complications, the prevalence of DKD has failed to decline over the past 30 years [2].
Clinically, DKD is defined as persistent albuminuria of an albumin-to-creatinine ratio above 30 mg/g of creatinine, with a progressive decline in kidney function. It is a microvascular complication of diabetes, characterized by hyperfiltration and mesangial matrix expansion, leading to kidney hypertrophy, thickening of the glomerular basement membrane, subsequent podocyte and glomerular injury, as well as tubular damage, all of which result in glomerulosclerosis and tubulointerstitial fibrosis. The pathogenesis of DKD is multifactorial with numerous structural, hemodynamic, and inflammatory pathophysiological processes being involved in the initiation and progression of the disease [3,4].
According to the Kidney Diseases: Improving Global Outcomes (KDIGO) clinical practice guideline for the diagnosis and management of chronic kidney disease (CKD), both functional and structural markers are used to diagnose and classify CKD, where estimated glomerular filtration rate (eGFR) is used for functional assessment, and albuminuria is used to assess structural damage of the kidney [5]. Both biomarkers are strong predictors of kidney disease progression, cardiovascular disease (CVD) and mortality in DKD patients [6]. However, the prognostic significance of these two biomarkers is not specific to DKD. In order to improve the risk stratification of patients with DKD, although several novel biomarkers have been developed and their predictive value have been extensively tested, most studies to date have only reported modest improvements in prediction of novel biomarkers over conventional biomarkers such as eGFR and albuminuria.
The aim of this review is first to describe recent advances in the understanding of the pathophysiology of DKD, and second, to describe the current clinical biomarkers for DKD, as well as the current status of multiple novel biomarkers with respect to protein biomarkers, proteomics, and metabolomics.
PATHOPHYSIOLOGY OF DIABETIC KIDNEY DISEASE
Hyperglycemia
In clinical studies, intensive glucose control reduced the incidence of albuminuria by 50% [7], and each ~1% reduction in glycosylated hemoglobin (HbA1c) reduced the risk of microalbuminuria by 33% [8]. In two landmark trials, intensive glucose control was associated with lower rates of albuminuria, although not in patients with type 2 diabetes mellitus (T2DM) and advanced CKD [9,10]. Although strict glycemic control may slow DKD progression in those with higher levels of albuminuria, it may not be able to completely halt disease progression [11,12]. This notion is supported by the fact that approximately 20% of patients with T2DM develop DKD in the absence of albuminuria [13]. Hyperglycemia is known to cause hypertrophy of the kidneys by generating advanced glycation end products (AGEs), oxidative injury, and hypoxia (Fig. 1). Several pathways such as the polyol, protein kinase C (PKC), and the hexosamine pathway are also involved in the development of DKD from hyperglycemia. All of these pathways are known stimulate several growth factors that include insulin like growth factor-1, epidermal growth factor, platelet-derived growth factor, vascular endothelial growth factor, transforming growth factor-β (TGF-β), and angiotensin II (Ang II) [14-17]. Of the several growth factors, TGF-β has been one of the most studied growth factor involved in the pathogenesis of DKD. In experimental diabetic models, TGF-β neutralizing antibodies attenuated kidney hypertrophy and preserved kidney function [18,19]. However, administration of TGF-β neutralizing antibodies failed to reduce albuminuria [19]. Similarly, in a randomized clinical trial of 77 subjects with diabetic nephropathy, administration of pirfenidone, an inhibitor of TGF-β production, failed to reduce urine levels of TGF-β [20].
Fig. 1.
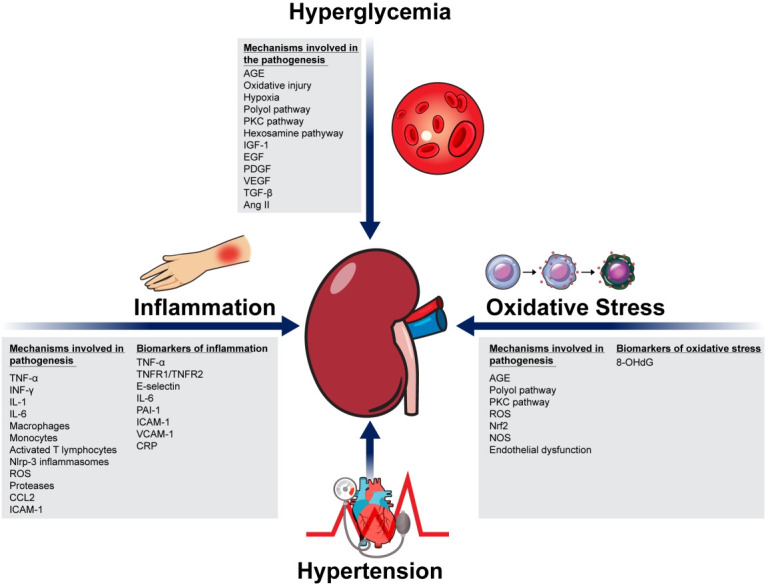
The pathophysiology of potential and novel biomarkers of diabetic kidney disease classified by their target pathophysiological pathways. AGE, advanced glycation end products; PKC, protein kinase C; IGF-1, insulin like growth factor-1; EGF, epidermal growth factor; PDGF, platelet-derived growth factor; VEGF, vascular endothelial growth factor; TGF-β, transforming growth factor-β; Ang II, angiotensin II; TNF-α, tissue necrosis factor-α; INF-γ, interferon-γ; IL-1, interleukin-1; IL-6, interleukin-6; Nlrp3, nod-like receptor protein-3; ROS, reactive oxygen species; CCL2, C-C motif chemokine 2; ICAM-1, intracellular adhesion molecule 1; TNFR1, tissue necrosis factor receptor 1; TNFR2, tissue necrosis factor receptor 2; PAI-1, plasminogen activator inhibitor-1; VCAM-1, vascular cell adhesion protein-1; CRP, C-reactive protein; Nrf2, nuclear factor erythroid 2-related factor; NOS, nitric oxide synthase; 8-OHdG, 8-Hydroxy-2’-deoxyguanosine.
Hypertension
Hypertension is another significant factor that contributes to the progression of DKD [21,22]. Normotensive patients with DKD show slower disease progression than those with hypertension [23]. In type 1 diabetes mellitus (T1DM), the cause of hypertension is primarily due to parenchymal disease, and blood pressure starts to increase only when the patient progresses from micro- to macroalbuminuria. In contrast, in patients with T2DM, hypertension is found in about one-third of patients at the time of diagnosis, suggesting that hypertension in T2DM may be a feature of metabolic syndrome [24]. Nevertheless, regardless of the type of DM, studies have indicated that uncontrolled hypertension accelerates the development of DKD. In the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial that included 11,140 participants with T2DM, a reduction in the systolic blood pressure resulted in a relative risk reduction of 9% for DKD complication [9]. However, in the more recent Action to Control Cardiovascular Risk in Diabetes (ACCORD) blood pressure trial (ACCORD-BP) and the International Verapamil-Trandolapril (INVEST) trial, lowering systolic blood pressures to below 130/80 mm Hg failed to substantially reduce clinical endpoints compared to standard anti-hypertensive therapy [25,26].
The optimal blood pressure target for patients with DKD remains controversial. The American Heart Association and American College of Cardiology joint 2017 guidelines recommend the lower target of <130/80 mm Hg [27], whereas the American Diabetes Association and Joint National Committee 8 recommend the higher target of 140/80 mm Hg for patients with DKD [28,29]. Although the recent Systolic Blood Pressure Intervention Trial (SPRINT) showed benefits of targeting lower blood pressures of <120 mm Hg, but the trial was performed mainly in non-diabetic elderly patients [30]. In a post hoc analysis of SPRINT-eligible participants in the ACCORD-BP trial, intensive blood pressure control reduced CVD outcomes in a cohort of participants with T2DM and additional CVD risk factors [31]. However, further studies are needed to assess whether lower blood pressure targets also benefit patients with DKD.
Inflammation
Hyperglycemia causes cellular injury, which triggers the release of proinflammatory mediators that include chemokines such as tissue necrosis factor-α (TNF-α) and interleukin-1 (IL1), adhesion molecules, and damage-associated molecular patterns (Fig. 1) [15-17]. This results in the recruitment of inflammatory cells such as macrophages, monocytes, activated T lymphocytes, and nod-like receptor protein-3 (Nlrp-3) inflammasomes, to the kidney [32,33]. Accumulation of macrophages in the glomerulus produces cytokines, reactive oxygen species (ROS), and proteases, which cause kidney damage and fibrosis, leading to DKD progression [34]. In mouse models of both T1DM and T2DM, deletion of the C-C motif chemokine 2 (CCL2; also known as monocyte chemoattractant protein-1) and intracellular adhesion molecule 1 (ICAM-1), which are known promote macrophage infiltration in the kidneys, decreased albuminuria and inflammation levels [35-37]. Due to the beneficial effects of CCL2 inhibition, clinical trials of the CCL2 inhibitor emapticap pegol (emapticap; NOX-E36, Noxxon Pharma AG, Berlin, Germany) are currently ongoing. In one phase II trial, a 29% reduction in albuminuria was observed with this inhibitor [38].
Of the inflammatory cytokines, TNF-α has been the most extensively studied molecule to date [39]. Patients with DKD are generally known to have higher TNF-α levels compared to healthy individuals. Of these patients, those with albuminuria have even higher TNF-α levels, when compared to those without albuminuria [40]. Due to the role of TNF-α in the progression of DKD, many therapeutic agents have been developed to target this inflammatory cytokine. Pentoxifylline, which is a phosphodiesterase inhibitor that has anti-inflammatory properties, as well as the ability to reduce TNF-α, interferon-γ, IL-1, and IL-6 levels, is one of the therapeutic agents that is currently being extensively studied [41]. In a prospective study of 61 patients with DKD and residual albuminuria, the addition of pentoxifylline to Ang II receptor blockade resulted in an additive anti-proteinuric effect associated with a reduction of urinary TNF-α excretion [42]. A post hoc analysis of the Pentoxifylline for Renoprotection in Diabetic Nephropathy (PREDIAN) trial also indicated that pentoxifylline also increased serum and urinary klotho levels, suggesting that pentoxifylline most likely provides anti-proteinuric effect by decreasing inflammation levels [43]. However, a recent meta-analysis of 17 studies and a total of 991 participants indicated that although pentoxifylline seemed to offer some beneficial effects in kidney function improvement and reduction in albuminuria, most studies were poorly reported, insufficient in sample size, and methodologically flawed. Further prospective, large-scale studies are needed to develop recommendations for routine use of this medication in patients with DKD [44].
Oxidative stress
Chronic hyperglycemia also stimulates the production of AGEs, the polyol pathway, and activates PKC, all of which leads to the increase in levels of ROS and oxidative stress (Fig. 1) [15-17]. Increase in ROS levels of the kidneys lead to damage of essential cellular components and DNA [45-47], as well as endothelial dysfunction, which is a hallmark feature of T2DM and DKD [3,48]. Endothelial dysfunction is characterized by reduced bioavailability of nitric oxide and increased oxidative stress [48]. Reduced endothelial nitric oxide synthases, resulting in enhanced production of ROS and oxidative stress are associated with the progression of DKD in experimental animal models [49,50].
Early animal studies of antioxidants in animal models of DKD have indicated that administration of GKT137831, a small molecule inhibitor of Nox1 and Nox4, in diabetic mice provided similar degree of renoprotection when compared to that observed in Nox4 knockout mice [51]. This was further investigated in a study of OVE26 mice, a model of T1DM, where administration of GKT137831 significantly reduced glomerular hypertrophy, mesangial matrix expansion, urinary albumin excretion, and loss of podocyte [52]. More recently, a novel pan-Nox inhibitor, APX-115, was shown to prevent kidney injury such as albuminuria, glomerular hypertrophy, tubular injury, podocyte injury, fibrosis, inflammation, and oxidative stress in diabetic mice. Observed effects were similar to those observed after losartan treatment of diabetic mice [53].
Although the results of animal studies have been promising, therapeutic effects of antioxidants in human studies have been largely unconvincing [17]. Currently, most therapies mainly target oxidative stress reduction by means of strict glucose control by anti-diabetic agents, as well as use of anti-hypertensive and anti-dyslipidemic agents [54,55]. For example, pioglitazone has been shown to markedly reduce glomerular sclerosis, hypertrophy, tubulointerstitial fibrosis, and albuminuria in a DKD animal model [56]. These effects may decrease levels of oxidative stress by means of reduction of hyperglycemia and insulin resistance. More recently, whether sodium-glucose cotransporter 2 (SGLT2) inhibitors can reduce oxidative stress and improve endothelial function has been investigated [57]. In mouse models, SGLT2 inhibitors protected against endothelial dysfunction, but vasodilatory effect was also found to be primarily due to reduced inflammation and reductions in oxidative stress levels [58]. Results from human studies have been more conflicting. In the randomized, controlled Dapagliflozin Effectiveness on Vascular Endothelial Function and Glycemic Control in T2DM (DEFENCE) study of 80 patients with T2DM, use of dapagliflozin (Farxiga, AstraZeneca, Cambridge, UK) improved endothelial function, as measured by change in flow-mediated dilation [59]. However, in the Effect of Empagliflozin on Endothelial Function in Cardiovascular High Risk Diabetes Mellitus: Multi-Center Placebo-Controlled Double-Blind Randomized Trial (EMBLEM), which included patients with T2DM and established CVD, use of empagliflozin (Jardiance, Boehringer Ingelheim, Ingelheim, Germany) failed to improve endothelial function [60], suggesting that CVD benefits associated with the use of SGLT2 inhibitors may have been attributable to mechanisms other than reduced inflammation and endothelial dysfunction [61]. Although positive kidney outcomes from the Canagliflozin and Renal Endpoints in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) trial, which enrolled patients with T2DM and DKD, led to U.S. Food and Drug Administration approval of canagliflozin (Invokana, Janssen, Beerse, Belgium) for the treatment of DKD [62], uncertainties regarding the use of SGLT2 inhibitors remain due to the lack of long-term clinical trials testing the kidney protective effects of every SGLT2 inhibitor in a broad range of patients with T2DM [63].
In addition to the above anti-diabetic agents, the development of antioxidants that more specifically target oxidative stress has been ongoing. Most recently, in The Phase 2 Study of Bardoxolone Methyl in Patients with Chronic Kidney Disease and Type 2 Diabetes (TSUBAKI) study, administration of bardoxolone methyl (Reata Pharmaceuticals, Plano, TX, USA), an activator of nuclear factor erythroid 2-related factor (Nrf2) that protects against oxidative stress, improved measured glomerular filtration rate [64]. However, considering that the phase 3 Bardoxolone Methyl Evaluation in Patients with Chronic Kidney Disease and Type 2 Diabetes Mellitus: the Occurrence of Renal Events (BEACON) study indicated that bardoxolone methyl increased the risk of early-onset fluid overload in patients with risk factors for heart failure [65], further studies examining safety concerns are needed before use in routine clinical practice [66].
CURRENT GUIDELINES OF DKD EVALUATION
To date, the most commonly used markers of DKD are albuminuria and eGFR [67]. These markers have strong predictive abilities of not only DKD progression, but also CVD and allcause mortality. However, these two markers have several limitations. Approximately 30% of patients with DKD do not have albuminuria and therefore, eGFR is the only biomarker available to predict DKD development and progression [13,68]. Although the metabolic syndrome, which is associated with insulin resistance, obesity, and hypertension, is strongly associated with the development of CKD and albuminuria [69], not all patients with the metabolic syndrome and T2DM develop albuminuria [70]. Moreover, not all DKD patients with microalbuminuria progress to macroalbuminuria, as some patients may also regress to normoalbuminuria [71]. This makes it difficult to predict development and progression of DKD using albuminuria. Limitation of using eGFR to predict disease progression include different equations used to eGFR such as the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI), Modification of Diet in Renal Disease (MDRD) equation, and eGFR calculated using cystatin C instead of creatinine [5], which may under- or overestimate risk of DKD development or progression depending on the equation used to calculate eGFR. In a study of diabetic adults to investigate the population based incidence rate of CKD depending on the eGFR equation used, incident rates of CKD were higher when the MDRD equation was used, compared to when the CKD-EPI equation was used [72]. Moreover, considering that creatinine is released from muscle tissue, creatinine based eGFR equations may fail to accurately reflect actual kidney function, particularly in patients with low muscle mass. Although the cystatin C, which is independent of muscle mass, overcomes this limitation of creatinine, several other factors such as inflammation and fat mass are also known to affect serum levels of this molecule [73], and thus may potentially confound the predictive ability of eGFR in DKD development or progression.
POTENTIAL BIOMARKERS OF DKD
In order to improve the prediction of DKD progression, the search for novel biomarkers to improve early identification of high-risk patients has been ongoing. Over the last decade, there have been numerous studies investigating novel biomarkers for DKD [74]. Such novel biomarkers will not only improve risk stratification of patients with DKD, but will also provide further insights into the complex pathophysiology of the disease, as well as potential novel therapeutic targets. Typically, such biomarkers capture one specific mechanism of the disease process such as glomerular or tubular damage, inflammation, or oxidative stress (Table 1) [75]. However, considering that DKD is a heterogeneous disease with a complex pathophysiology, it is more likely that no one biomarker may be able to predict the prognosis of DKD, and a multi-marker approach may be needed to predict disease progression.
Table 1.
Summary of studies reporting on potential and omics-based novel biomarkers in diabetic kidney disease
| Biomarker | Study | Sample size | Study population | Main results | Adjustments | ||
|---|---|---|---|---|---|---|---|
| Potential | |||||||
| Biomarkers of tubular damage | |||||||
| Plasma KIM-1, TNFR-1, and TNFR-2 | Coca et al. [77] | Nested case-control study (n=380) | T2DM | Doubling in KIM-1, TNFR-1, and TNFR-2 levels were associated with higher risk of eGFR decline | Treatment arm, baseline eGFR, albuminuria, age, race, systolic and diastolic blood pressure, medications | ||
| Prospective cohort study (n=1,156) | T1DM and T2DM | ||||||
| Plasma KIM-1, TNFR-1, TNFR-2, and MCP-1 | Schrauben et al. [78] | Case-cohort study (n=894) | Higher plasma levels of KIM-1, TNFR-1, TNFR-2, and MCP-1 were associated with risk of progression of DKD | Age, sex, race/ethnicity, education, clinical center, systolic and diastolic blood pressure, BMI, hsCRP, HbA1c, antihypertensive medication use, smoking status, baseline eGFR, and UPCR | |||
| Urinary KIM-1 and NGAL | de Carvalho et al. [79] | Cross-sectional study (n=117) | T2DM | Urinary KIM-1 and NGAL were increased in T2DM patients with normal or mildly increased albuminuria | HbA1c, LDL cholesterol, fasting glucose, and medication | ||
| Urinary NGAL | Yuruk Yildirim et al. [80] | Cross-sectional study (n=111) | T1DM | Urinary NGAL level increase in the early phase of T1DM before microalbuminuria development | No adjustments | ||
| Serum NGAL | Lacquaniti et al. [81] | Cross-sectional study (n=85) | T1DM | NGAL increases in patients with T1DM before onset of microalbuminuria | No adjustments | ||
| Urinary L-FABP | Nielsen et al. [82] | Prospective cohort study (n=165) | T1DM | High levels of urinary L-FABP predict the initiation and progression to DKD and all- cause mortality | Age, sex, HbA1c, systolic and diastolic blood pressure, albuminuria, serum creatinine, smoking | ||
| Urinary L-FABP | Panduru et al. [84] | Prospective cohort study (n=1,549) | T1DM | High urinary L-FABP levels were found to be a strong and independent predictor of DKD progression | Risk factors of DKD and albuminuria | ||
| Urinary cystatin C | Kim et al. [85] | Prospective cohort study (n=237) | T2DM | Urinary cystatin C and albuminuria may be sensitive and specific markers for predicting kidney impairment | Age, HbA1c, systolic blood pressure, uric acid, albuminuria, baseline eGFR, use of RAS inhibitors and lipid-lowering agents, serum cystatin C | ||
| Biomarkers of inflammation | |||||||
| Plasma TNF-α, TNFR1, TNFR2 | Niewczas et al. [89] | Prospective cohort study (n=410) | T2DM | Elevated circulating TNFR levels are strong predictors of progression to ESKD in subjects with and without proteinuria | Age, HbA1c, albuminuria, eGFR | ||
| Serum TNFR | Skupien et al. [90] | Prospective cohort study (n=349) | T1DM | Circulating TNFR2 is a major determinant of kidney function decline | No adjustments | ||
| Serum TNFR1, TNFR2, E-selectin | Lopes-Virella et al. [91] | Prospective cohort study (n=1,237) | T1DM | High levels of E-selectin and soluble TNFR1 and TNFR2 levels were important predictors of incident albuminuria | Treatment, albuminuria, use of RAS inhibitors, baseline retinopathy, sex, age, HbA1c, diabetes duration | ||
| Biomarkers of oxidative stress | |||||||
| Urinary 8-OHdG | Xu et al. [93] | Cross-sectional study (n=69) | T2DM | Individuals with T2DM have higher levels of 8-OHdG compared to healthy individuals | No adjustments | ||
| Plasma 8-OHdG | Sanchez et al. [94] | Prospective cohort study (n=704) | T1DM | Higher levels of 8-OHdG were associated with increased risk of kidney disease | Age, sex, cohort, duration of diabetes, HbA1c, insulin therapy, systolic blood pressure, use of antihypertensive drugs, RAS inhibitors, diabetic retinopathy stage, lipid-lowering drugs, eGFR, albuminuria | ||
| Urinary 8-OHdG | Serdar et al. [95] | Cross-sectional study (n=92) | T2DM | Although urinary 8-OHdG levels increase in diabetic patients, their levels do not improve prediction of progressive DKD over and above measuring albuminuria | No adjustments | ||
| Omics-based novel biomarkers | |||||||
| Proteomics | |||||||
| Urinary haptoglobin | Bhensdadia et al. [97] | Prospective cohort study (n=204) | T2DM | The haptoglobin to creatinine ratio may be useful to predict risk of DKD before the development of albuminuria or kidney function decline | Treatment arm, use of ACEi | ||
| Urinary CKD-273 | Zurbig et al. [99] | Prospective cohort study (n=35) | T1DM and T2DM | CKD-273 predicted progression to macroalbuminuria 5 years prior to actual onset | Age, sex, DM type, albuminuria, eGFR, systolic and diastolic blood pressure, HbA1c, glucose | ||
| Urinary CKD-273 | Roscioni et al. [100] | Prospective cohort study (n=88) | T2DM | CKD-273 predicted development of albuminuria independent of other kidney biomarkers used to predict DKD development or progression | Albuminuria, eGFR, use of RAS inhibitors | ||
| Urinary CKD-273 | Zurbig et al. [101] | Prospective cohort study (n=1,014) | T1DM and T2DM | In patients with T1DM or T2DM, baseline eGFR ≥70 mL/min/1.73 m2, and normoalbuminuria, CKD-273 was able to identify progression to eGFR <60 mL/min/1.73 m2 in the absence of albuminuria | Age, baseline eGFR, systolic and diastolic blood pressure | ||
| Urinary CKD-273 | Tofte et al. [102] | Prospective cohort study (n=1,775) | T2DM | High-risk patients defined by CKD-273 were more likely to develop microalbuminuria | Age, sex, HbA1c, systolic blood pressure, retinopathy, albuminuria, eGFR | ||
| Urinary CKD-273 | Lindhardt et al. [103] | Prospective cohort study (n=737) | T2DM | CKD-273 predicted development of albuminuria | Treatment group, age, sex, systolic blood pressure, albuminuria, eGFR, HbA1c, diabetes duration | ||
| Metabolomics | |||||||
| 35 Serum non-esterified and 32 serum esterified fatty acids | Han et al. [106] | Cross-sectional study (n=150) | T2DM | Non-esterified and esterified fatty acid discriminated albuminuria stages | No adjustments | ||
| 19 Serum metabolites | Hirayama et al. [107] | Cross-sectional study (n=78) | T2DM | Combination of 19 serum metabolites enabled accurate discrimination of DKD | No adjustments | ||
| Serum leucine, dihydrosphingosine, phytosphingosine | Zhang et al. [108] | Cross-sectional study (n=66) | T2DM | Serum metabolite levels of leucine, dihydrosphingosine, and phytosphingosine were significantly different in patients with T2DM and healthy controls | No adjustments | ||
| Urine hexose, glutamine, tysorine, plasma butenoylcarnitine, histidine | Pena et al. [109] | Prospective cohort study (n=90) | T2DM | Urine hexose, glutamine, tyrosine, plasma butenoylcarnitine and histine predicted development of albuminuria | Albuminuria, eGFR, RAS inhibitors | ||
| 207 Serum biomarkers that included dimethylarginine, C16-acylcarnitine | Looker et al. [110] | Nested case-control study (n=307) | T2DM | A panel of 14 biomarkers that included the symmetric to asymmetric dimethylarginine ratio, and C16-acylcarnitine increased the predictive ability of rapid progression | Age, sex, baseline eGFR, albuminuria, HbA1c, use of RAS inhibitors | ||
| Urinary 3-hydroxy-isobutyrate, 3-methyl-crotonyglycine, aconitic acid, citric acid | Kwan et al. [111] | Prospective cohort study (n=1,001) | T1DM and T2DM | 3-Hydroxyisobutyrate and 3-methylcrotonygly- cine had a significant negative association with eGFR slope, while aconitic and citric acid showed a positive association. | Age, race, sex, smoking, body mass index, HbA1c, mean arterial pressure, albuminuria, baseline eGFR | ||
| Urinary leucine, valine, isoleucine, pseudouridine, threonine, citrate, 2-hydroxyiso- butyrate, pyroglutamate, tyrosine, alanine | Mutter et al. [112] | Prospective cohort study (n=2,670) | T1DM | 7 Urinary metabolites that included leucine, valine, isoleucine, pseudouridine, threonine, and citrate were associated with DKD progression. 6 amino acids and pyroglutamate were associated with DKD progression in those with macroalbuminuria | Baseline albuminuria, baseline glycemic | ||
| Transcriptomics | |||||||
| Let-7c-5p, miR-29a-3p, let-7b- 5p, miR-21-5p, miR-29c-3p | Pezzolesi et al. [113] | Prospective cohort study (n=116) | T1DM | Baseline miRNA levels of let-7c-5p and miR-29a- 3p were independently associated with more than a 50% reduction in the risk of rapid progression to ESKD, while levels of let-7b-5p and miR-21-5p were associated with a higher risk of ESKD | Age, sex, HbA1c, duration of diabetes | ||
| 18 miRNAs | Argyropoulos et al. [114] | Prospective cohort study (n=30) | T1DM | 18 miRNAs were associated with the development of albuminuria, while 15 miRNAs exhibited gender-related differences in expression | Sex | ||
| miR-130a, miR-145, miR-155, miR-424 | Barutta et al. [115] | Cross-sectional study (n=24) | T1DM | 22 of 377 urinary EV-miRNAs were differentially expressed in patients with normoalbuminuria compared to albuminuric patients | No adjustments | ||
KIM-1, kidney injury molecule 1; TNFR-1, tissue necrosis factor receptor 1; TNFR-2, tissue necrosis factor receptor 2; T2DM, type 2 diabetes mellitus; eGFR, estimated glomerular filtration rate; MCP-1, monocyte chemoattractant protein 1; T1DM, type 1 diabetes mellitus; DKD, diabetic kidney disease; BMI, body mass index; hsCRP, high-sensitivity C-reactive protein; HbA1c, hemoglobin A1c; UPCR, urine protein-to-creatinine ratio; NGAL, neutrophil gelatinase-associated lipocalin; LDL, low-density lipoprotein; L-FABP, liver fatty acid-binding protein; RAS, renin-angiotensin system; TNF-α, tissue necrosis factor α; ESKD, end-stage kidney disease; 8-OHdG, 8-hydroxydeoxyguanosine; ACEi, angiotensin-converting enzyme inhibitor; DM, diabetes mellitus; CKD-273, chronic kidney disease 273.
Biomarkers of tubular damage
Markers of tubular damage include kidney injury molecule 1 (KIM-1), neutrophil gelatinase-associated lipocalin (NGAL), α-1-microglobulin, N-acetyl-β-D-glucosaminidase (NAG), cystatin C, and liver-type fatty acid-binding protein (L-FABP). The markers that have been most extensively studied are KIM-1, NGAL, L-FABP, and cystatin C.
KIM-1 is a protein expressed on the apical membrane of the proximal tubule cells of the kidney. Urinary concentrations of KIM-1 increase in response to acute kidney injury [76]. In a nested case-control study and a prospective cohort study, KIM-1 was independently associated with higher risk of eGFR decline in persons with early or advanced DKD [77]. More recently, in a case-cohort study of 894 participants with DKD from the Chronic Renal Insufficiency Cohort (CRIC) cohort, higher plasma levels of KIM-1 were associated with increased risk of progression of DKD [78].
NGAL is a 25 kDa protein belonging to the lipocalin superfamily that was initially found in activated neutrophils, but also produced in kidney tubular cells in response to tubular damage. Elevated levels of urinary NGAL have been shown to be present in DKD patients with normoalbuminuria [79], and it has also been demonstrated to precede microalbuminuria in T1DM [80,81]. In another study of 117 patients with T2DM, high values of urinary NGAL have been observed in T2DM patients with normoalbuminuria, and rose progressively in those with micro- and macroalbuminuria, suggesting that tubular injuries may be occurring even in very early stages of DKD [79].
Urinary L-FABP levels have been shown to be associated with DKD progression. In patients with T1DM, high levels of urinary L-FABP predicted the initiation and progression of DKD and all-cause mortality, independent of the severity of albuminuria and other established risk factors [82]. In another cross-sectional and longitudinal study of 140 patients with T2DM without DKD and 412 healthy control subjects, urinary L-FABP levels accurately reflected the severity of DKD, and these levels were particularly high in those with normoalbuminuria [83]. High urinary L-FABP levels were found to be a strong and independent predictor of progression of DKD [84].
Cystatin C, which is a 13-kDa molecule that is freely filtered across the glomerulus and then completely reabsorbed and metabolized by the proximal tubule, is another marker of tubular damage that is commonly used in current practice. Considering that urinary cystatin C concentrations rise after tubular damage, the urinary cystatin C to creatinine ratio has been demonstrated to independently predict development of CKD stage 3 in patients with T2DM. However, in a separate analysis of patients with eGFR >60 mL/min/1.73 m2 and without baseline albuminuria, the ratio was not associated with the rate of eGFR decline [85].
Biomarkers of inflammation
Markers of inflammation such as TNF-α and IL-1β are also known to predict DKD progression [39]. The possibility that both markers could contribute to the development of DKD was first postulated in a study of diabetic mouse, where macrophages incubated with glomerular basement membranes produced significantly greater levels of both TNF-α and IL-1β than those incubated with membranes of normal non-diabetic mouse [86]. TNF-α binds to type 1 (TNFR1) and type 2 (TNFR2) TNF-α receptors, and both are found in circulation as soluble forms. TNF-α is known to exert cytotoxic effects on glomerular and mesangial cells, and thus, induces kidney injury [87]. Animal and human studies have suggested that urinary TNF-α excretion and serum TNF-α levels are both elevated in DKD [88]. Studies of TNFR levels have also suggested that circulating TNFR levels may be good predictors of ESKD in patients with DKD [89]. More recently, in the Joslin cohort, TNFR2 levels were the strongest determinant of eGFR decline in patients with T1DM and albuminuria [90].
Other inflammatory markers that have been studied include serum E-selectin, IL-6, plasminogen activator inhibitor-1 (PAI-1), ICAM-1, vascular cell adhesion protein-1 (VCAM-1), and C-reactive protein (CRP). In the Diabetes Control and Complications Trial (DCCT) study, which enrolled 1,237 patients who were both free of albuminuria and CVD at baseline, high levels of inflammatory markers, mainly E-selectin and soluble TNFR1 and TNFR2 levels were important predictors of incident albuminuria in patients with T1DM [91]. In the Joslin cohort, although markers that included TNF, ICAM-1, VCAM-1, PAI-1, IL-6, and CRP were studied, only elevated concentrations of circulating TNFR in patients with T2DM were strong predictors of subsequent progression to ESKD in individuals with and without albuminuria [90].
Biomarkers of oxidative stress
8-Hydroxy-2’-deoxyguanosine (8-OHdG) is a product of oxidative DNA damage, and is excreted in the plasma and urine upon DNA repair by nuclease activity [92]. This allows 8-OHdG to be used as a biomarker of oxidative DNA damage. As such, several previous studies have indicated that individuals with T2DM generally have higher levels of 8-OHdG compared to healthy individuals [93]. A recent cohort study of patients with T1DM also similarly demonstrated that higher plasma concentrations of 8-OHdG were independently associated with increased risk of kidney disease, suggesting that 8-OHdG may be useful in evaluating the progression of DKD [94]. However, another study suggested that measurements of urinary 8-OHdG did not improve prediction of progressive DKD over and above measuring albuminuria [95].
OMICS BASED NOVEL BIOMARKERS OF DKD
The omics platform-based approach
Over the past years, the use of high-throughput omic approaches to analyze biological samples that include proteomics, metabolomics, and transcriptomics has significantly increased. An omics test is an assay composed of multiple molecular measurements that allows quantification of all RNAs, proteins, and metabolites present in biological samples. Advantages of omics platforms are that not only can they measure a full spectrum of peptides or metabolites in a short amount of time, but they also produce large sets of unbiased data that can be used for diagnosis, outcome prediction, and treatment responses. As a result, this omics platform-based approach has emerged as a strong tool in biomarker discovery in recent years (Table 1).
Proteomics
Proteomics allows for the full assessment of proteins present within plasma, serum, or urine. Since urine collection is relatively simple, non-invasive, and available in abundant volumes, urinary proteomics has gained much attention as a tool for the identification of diagnostic and prognostic biomarkers of kidney diseases [96]. For example, in a study of patients with DKD from the Veterans Affairs Diabetes Trial (VADT), urinary haptoglobin was identified as a candidate biomarker to predict early kidney functional decline [97].
At present, the most studied and validated proteomic classifier is the capillary electrophoresis-mass spectrometry-based urinary peptide classifier, CKD-273. This mass spectrometry-based method combines data of 273 urinary peptides into a combined score that has high accuracy of predicting the new onset of albuminuria. The diagnostic utility of this proteomic classifier was first developed in a cross-sectional study of 3,600 CKD patients with different CKD etiologies, where the classifier showed a sensitivity of 85% and a specificity of 100% for the diagnosis of CKD [98]. This classifier was subsequently validated across several cohorts consisting of patients with T2DM, where CKD-273 was shown to predict both development and progression of albuminuria in patients with DKD. In a prospective study of 35 patients with either T1DM or T2DM, CKD-273 was able to predict progression to macroalbuminuria 5 years prior to actual onset [99], and another study indicated that CKD-273 was able to predict development of albuminuria independent of any other kidney biomarker used to predict DKD development or progression [100]. Most recently, in a study of 1,014 individuals with T1DM or T2DM, baseline eGFR ≥70 mL/min/1.73 m2, and normoalbuminuria, CKD-273 was able to identify patients with DM who will progress to eGFR <60 mL/min/1.73 m2 in the absence of albuminuria, independent of age, blood pressure, and baseline eGFR [101].
In the Proteomic Prediction and Renin Angiotensin Aldosterone System Inhibition Prevention of Early Diabetic nephropathy In Type 2 Diabetic Patients with Normoalbuminuria (PRIORITY) trial, the efficacy of CKD-273 in predicting development of DKD was investigated in a prospective cohort comprised of 1,775 patients with T2DM and normoalbuminuria. After a median follow-up of 2.5 years, high-risk patients defined by CKD-273 were more likely to develop microalbuminuria, even after adjustments for baseline risk factors such as HbA1c, systolic blood pressure, baseline albuminuria and eGFR [102]. In a post hoc analysis of the Diabetic Retinopathy Candesartan Trials-progression of retinopathy in T2DM (DIRECT-Protect 2) study that consisted of patients with T2DM and normoalbuminuria, the CKD273-classifier predicted development of albuminuria during follow-up independent of treatment, age, sex, blood pressure, albuminuria, eGFR, HbA1c, and diabetes duration, suggesting that proteomics may help identify high-risk normoalbuminuric patients for prevention of DKD [103].
Although both plasma and serum are alternatives to urine samples, proteomics derived from blood samples are not as common as urine proteomics. Profiling of circulating proteins in the blood is difficult to perform due to the large heterogeneity and spread in abundance of proteins in blood and high exposure to proteolytic activity, which may confound the interpretation of the blood proteome [104]. Regardless of the sample used for proteomic analysis, use of proteomics for early diagnosis of DKD is limited by the absence of a robust and well-validated diagnostic criteria. Further validation studies are needed before widespread implementation of proteomics analyses in DKD.
Metabolomics
Metabolomics is the measurement of low weight intermediates and small end products of biochemical processes in biological fluids. They have emerged as another potential tool in the discovery of novel biomarkers for kidney diseases. Compared to biological information from the genome, transcriptome, and proteome, metabolomes are often regarded as a better platform in the assessment of a patient’s molecular phenotype. However, their results are often difficult to interpret due to various confounders, including lifestyle, medications, and nutritional status [105].
There are numerous cross-sectional studies that have investigated the progression of kidney disease in patients with T2DM. Most studies have investigated products of lipid metabolism that include esterified and non-esterified fatty acids, phospholipids, as well as amino acid metabolism, carnitine, nucleotide metabolism. In those that investigated plasma phospholipids, one study demonstrated that non-esterified and esterified fatty acid discriminated albuminuria stages in T2DM [106]. In another study of 78 diabetic patients, combination of 19 serum metabolites enabled accurate discrimination of patients with DKD. For example, when five metabolites that included γ-butyrobetaine, symmetric dimethylarginine (SDMA), azelaic acid and two unknowns were selected from the panel of metabolites, the area under curve (AUC) value for diagnosis of DKD was 0.927 for the whole data set [107]. Another study that included healthy controls and patients with T2DM indicated that serum metabolite levels of leucine, dihydrosphingosine and phytosphingosine were significantly different in these two patient groups [108]. However, all of the aforementioned studies are cross-sectional, and does not allow for the assessment of the predictive value of these metabolites.
There are even fewer prospective studies in the field of metabolomics. In a study of 90 patients with T2DM, urine hexose, glutamine, tyrosine, plasma butenoylcarnitine and histidine levels predicted development of albuminuria, independent of baseline albuminuria, eGFR and use of RAS-blockers [109]. In the Surrogate markers for micro- and macro-vascular hard end points for Innovative diabetes Tools program (SUMMIT) study, a total of 207 serum biomarkers were measured, of which 30 biomarkers showed significant associations with rapid progression, all adjusted for clinical characteristics. A panel of 14 biomarkers increased the predictive ability, where the addition of biomarkers to clinical data improved baseline AUC from 0.706 to 0.868. Biomarkers included in the predictive model consisted of fibroblast growth factor-21, the symmetric to asymmetric dimethylarginine ratio, β2-microglobulin, C16-acylcarnitine, and KIM-1 [110]. Another study from the CRIC consisting of 1,001 participants with diabetes and CKD, after adjustments for clinical variables, levels of metabolites 3-hydroxyisobutyrate (3-HIBA) and 3-methylcrotonyglycine had a significant negative association with eGFR slope, while aconitic and citric acid showed a positive association. 3-HIBA levels and aconitic acid levels were each associated with higher and lower risks of ESKD requiring kidney replacement therapy, respectively [111]. Most recently, in 2,670 individuals with T1DM from the Finnish Diabetic Nephropathy study, which collected 24-hour urine samples and measured metabolite concentrations by nuclear magnetic resonance, seven urinary metabolites that included leucine, valine, isoleucine, pseudouridine, threonine, and citrate were associated with DKD progression after adjustment for baseline albuminuria and CKD stage. Moreover, 2-hydroxyisobutyrate was associated with progression of DKD in individuals with normoalbuminuria, and six amino acids and pyroglutamate were associated with progression of DKD in those with macroalbuminuria [112].
Although there have been significant advances in the field of metabolomics for patients with DKD, replication of current findings in other cohorts are needed in order to inform therapeutic targets for DKD and improve clinical management of DKD.
Transcriptomics
Transcriptomic studies of DKD utilize micro RNAs (miRNAs), which are small non-coding RNAs that regulate gene expression via suppression of target mRNAs. Profiling of miRNAs can be performed by either traditional microarray/reverse transcription-polymerase chain reaction platforms or by RNA sequencing. In a study of T1DM patients with albuminuria and normal kidney function, baseline levels of circulating TGF-β1-regulated miRNAs were associated with progression to ESKD requiring chronic dialysis. Baseline miRNA levels of let-7c-5p and miR-29a-3p were independently associated with more than a 50% reduction in the risk of rapid progression to ESKD, while miRNA levels of let-7b-5p and miR-21-5p were independently associated with a more than 2.5-fold increase in the risk of ESKD [113]. Another small prospective study of patients with T1DM without albuminuria revealed that 18 miRNAs were associated with the development of albuminuria and nine of them were used to define a gene signature for microalbuminuria [114]. Another study assessed the urinary extracellular vesicles (EV)-miRNA profiles of patients with T1DM, where 22 of 377 urinary EV-miRNAs were differentially expressed in patients with normoalbuminuria compared to albuminuric patients. Results showed that miR-130a and miR-145 were enriched, while miR-155 and miR-424 were reduced in urinary exosomes for patients with albuminuria [115]. Although several other studies have investigated transcriptomics in patients with diabetes and kidney diseases, there is no overlap in the specific miRNAs being reported as being relevant to DKD, and rather than a single miRNA, a combination of miRNAs may be needed for early detection of DKD [116]. Thus, the evidence to support a clinically useful role of miRNAs in the prediction of DKD prognosis remains uncertain.
CURRENT PRACTICE AND FUTURE PERSPECTIVES
Despite the large number of studies reporting on potential novel biomarkers to predict DKD prognosis, they only modestly improve the performance of current available biomarkers. Therefore, assessment of eGFR and albuminuria still remain the cornerstone of diagnosis and risk stratification of DKD in daily clinical practice. However, both eGFR and albuminuria have its limitations as prognostic biomarkers. Considering that DKD is a complex disease involving several pathophysiologic mechanisms, biomarkers for the risk stratification of patients with DKD should consist of factors that are derived from multiple pathophysiological mechanisms of the DKD disease process. Although large discovery panels through novel omic approaches have enormous potential for biomarker discovery in DKD, progress in this field has been hampered by inadequate data analysis approaches, and lack of samples for replication. Biomarkers measured on different platforms are not easy to implement across various clinical settings.
While awaiting further advances in this field, considering that general treatment measures such as strict glucose control, anti-hypertensive and anti-dyslipidemic therapies all contribute to slowing down the rate of disease progression, physicians should pay attention to these aspects of treatment as they may enhance predictive accuracy for detecting those at the highest risk for development and progression of DKD. Moreover, in order to obtain comparable and reproducible data, future studies that utilize novel omic approaches will likely require consensus protocols for sample collection, processing, and analysis. Analysis and interpretation of findings from these studies will require specialized bioinformatics tools to turn big data into biomarker discovery.
Acknowledgments
The authors thank the Medical Illustration & Design team of the Medical Research Support Services of Yonsei University College of Medicine for all artistic support related to this work.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
FUNDING
None
REFERENCES
- 1.Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol. 2017;12:2032–45. doi: 10.2215/CJN.11491116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. 2014;370:1514–23. doi: 10.1056/NEJMoa1310799. [DOI] [PubMed] [Google Scholar]
- 3.Thomas MC, Brownlee M, Susztak K, Sharma K, JandeleitDahm KA, Zoungas S, et al. Diabetic kidney disease. Nat Rev Dis Primers. 2015;1:15018. doi: 10.1038/nrdp.2015.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anders HJ, Huber TB, Isermann B, Schiffer M. CKD in diabetes: diabetic kidney disease versus nondiabetic kidney disease. Nat Rev Nephrol. 2018;14:361–77. doi: 10.1038/s41581-018-0001-y. [DOI] [PubMed] [Google Scholar]
- 5.Kidney Disease: Improving Global Outcomes (KDIGO) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150. doi: 10.1038/ki.2013.243. [DOI] [PubMed] [Google Scholar]
- 6.Jones RH, Hayakawa H, Mackay JD, Parsons V, Watkins PJ. Progression of diabetic nephropathy. Lancet. 1979;1:1105–6. doi: 10.1016/s0140-6736(79)91788-4. [DOI] [PubMed] [Google Scholar]
- 7.Diabetes Control and Complications Trial Research Group. Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulindependent diabetes mellitus. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association 6. Glycemic targets: standards of medical care in diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S55–64. doi: 10.2337/dc18-S006. [DOI] [PubMed] [Google Scholar]
- 9.ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560–72. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 10.Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376:419–30. doi: 10.1016/S0140-6736(10)60576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tamborlane WV, Puklin JE, Bergman M, Verdonk C, Rudolf MC, Felig P, et al. Long-term improvement of metabolic control with the insulin pump does not reverse diabetic microangiopathy. Diabetes Care. 1982;5 Suppl 1:58–64. [PubMed] [Google Scholar]
- 12.Ciavarella A, Vannini P, Flammini M, Bacci L, Forlani G, Borgnino LC. Effect of long-term near-normoglycemia on the progression of diabetic nephropathy. Diabete Metab. 1985;11:3–8. [PubMed] [Google Scholar]
- 13.Caramori ML, Fioretto P, Mauer M. Low glomerular filtration rate in normoalbuminuric type 1 diabetic patients: an indicator of more advanced glomerular lesions. Diabetes. 2003;52:1036–40. doi: 10.2337/diabetes.52.4.1036. [DOI] [PubMed] [Google Scholar]
- 14.Brownlee M, Vlassara H, Cerami A. Nonenzymatic glycosylation and the pathogenesis of diabetic complications. Ann Intern Med. 1984;101:527–37. doi: 10.7326/0003-4819-101-4-527. [DOI] [PubMed] [Google Scholar]
- 15.Lin YC, Chang YH, Yang SY, Wu KD, Chu TS. Update of pathophysiology and management of diabetic kidney disease. J Formos Med Assoc. 2018;117:662–75. doi: 10.1016/j.jfma.2018.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Sharma D, Bhattacharya P, Kalia K, Tiwari V. Diabetic nephropathy: new insights into established therapeutic paradigms and novel molecular targets. Diabetes Res Clin Pract. 2017;128:91–108. doi: 10.1016/j.diabres.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Warren AM, Knudsen ST, Cooper ME. Diabetic nephropathy: an insight into molecular mechanisms and emerging therapies. Expert Opin Ther Targets. 2019;23:579–91. doi: 10.1080/14728222.2019.1624721. [DOI] [PubMed] [Google Scholar]
- 18.Sharma K, Jin Y, Guo J, Ziyadeh FN. Neutralization of TGFbeta by anti-TGF-beta antibody attenuates kidney hypertrophy and the enhanced extracellular matrix gene expression in STZ-induced diabetic mice. Diabetes. 1996;45:522–30. doi: 10.2337/diab.45.4.522. [DOI] [PubMed] [Google Scholar]
- 19.Ziyadeh FN, Hoffman BB, Han DC, Iglesias-De La Cruz MC, Hong SW, Isono M, et al. Long-term prevention of renal insufficiency, excess matrix gene expression, and glomerular mesangial matrix expansion by treatment with monoclonal antitransforming growth factor-beta antibody in db/db diabetic mice. Proc Natl Acad Sci U S A. 2000;97:8015–20. doi: 10.1073/pnas.120055097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharma K, Ix JH, Mathew AV, Cho M, Pflueger A, Dunn SR, et al. Pirfenidone for diabetic nephropathy. J Am Soc Nephrol. 2011;22:1144–51. doi: 10.1681/ASN.2010101049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parving HH, Andersen AR, Smidt UM, Svendsen PA. Early aggressive antihypertensive treatment reduces rate of decline in kidney function in diabetic nephropathy. Lancet. 1983;1:1175–9. doi: 10.1016/s0140-6736(83)92462-5. [DOI] [PubMed] [Google Scholar]
- 22.Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and metaanalysis. Lancet. 2016;387:435–43. doi: 10.1016/S0140-6736(15)00805-3. [DOI] [PubMed] [Google Scholar]
- 23.Patney V, Whaley-Connell A, Bakris G. Hypertension management in diabetic kidney disease. Diabetes Spectr. 2015;28:175–80. doi: 10.2337/diaspect.28.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005;28:164–76. doi: 10.2337/diacare.28.1.164. [DOI] [PubMed] [Google Scholar]
- 25.ACCORD Study Group. Cushman WC, Evans GW, Byington RP, Goff DC, Jr, Grimm RH, Jr, et al. Effects of intensive bloodpressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–85. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304:61–8. doi: 10.1001/jama.2010.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71:1269–324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 28.Passarella P, Kiseleva TA, Valeeva FV, Gosmanov AR. Hypertension management in diabetes: 2018 update. Diabetes Spectr. 2018;31:218–24. doi: 10.2337/ds17-0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Armstrong C, Joint National Committee JNC8 guidelines for the management of hypertension in adults. Am Fam Physician. 2014;90:503–4. [PubMed] [Google Scholar]
- 30.SPRINT Research Group. Wright JT, Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buckley LF, Dixon DL, Wohlford GF, 4th, Wijesinghe DS, Baker WL, Van Tassell BW. Intensive versus standard blood pressure control in SPRINT-Eligible participants of ACCORD-BP. Diabetes Care. 2017;40:1733–8. doi: 10.2337/dc17-1366. [DOI] [PubMed] [Google Scholar]
- 32.Chow F, Ozols E, Nikolic-Paterson DJ, Atkins RC, Tesch GH. Macrophages in mouse type 2 diabetic nephropathy: correlation with diabetic state and progressive renal injury. Kidney Int. 2004;65:116–28. doi: 10.1111/j.1523-1755.2004.00367.x. [DOI] [PubMed] [Google Scholar]
- 33.Shahzad K, Bock F, Dong W, Wang H, Kopf S, Kohli S, et al. Nlrp3-inflammasome activation in non-myeloid-derived cells aggravates diabetic nephropathy. Kidney Int. 2015;87:74–84. doi: 10.1038/ki.2014.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barrera-Chimal J, Jaisser F. Pathophysiologic mechanisms in diabetic kidney disease: a focus on current and future therapeutic targets. Diabetes Obes Metab. 2020;22 Suppl 1:16–31. doi: 10.1111/dom.13969. [DOI] [PubMed] [Google Scholar]
- 35.Okada S, Shikata K, Matsuda M, Ogawa D, Usui H, Kido Y, et al. Intercellular adhesion molecule-1-deficient mice are resistant against renal injury after induction of diabetes. Diabetes. 2003;52:2586–93. doi: 10.2337/diabetes.52.10.2586. [DOI] [PubMed] [Google Scholar]
- 36.Giunti S, Barutta F, Perin PC, Gruden G. Targeting the MCP1/CCR2 system in diabetic kidney disease. Curr Vasc Pharmacol. 2010;8:849–60. doi: 10.2174/157016110793563816. [DOI] [PubMed] [Google Scholar]
- 37.Boels MG, Koudijs A, Avramut MC, Sol WM, Wang G, van Oeveren-Rietdijk AM, et al. Systemic monocyte chemotactic protein-1 inhibition modifies renal macrophages and restores glomerular endothelial glycocalyx and barrier function in diabetic nephropathy. Am J Pathol. 2017;187:2430–40. doi: 10.1016/j.ajpath.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 38.Menne J, Eulberg D, Beyer D, Baumann M, Saudek F, Valkusz Z, et al. C-C motif-ligand 2 inhibition with emapticap pegol (NOX-E36) in type 2 diabetic patients with albuminuria. Nephrol Dial Transplant. 2017;32:307–15. doi: 10.1093/ndt/gfv459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elmarakby AA, Sullivan JC. Relationship between oxidative stress and inflammatory cytokines in diabetic nephropathy. Cardiovasc Ther. 2012;30:49–59. doi: 10.1111/j.1755-5922.2010.00218.x. [DOI] [PubMed] [Google Scholar]
- 40.Moriwaki Y, Yamamoto T, Shibutani Y, Aoki E, Tsutsumi Z, Takahashi S, et al. Elevated levels of interleukin-18 and tumor necrosis factor-alpha in serum of patients with type 2 diabetes mellitus: relationship with diabetic nephropathy. Metabolism. 2003;52:605–8. doi: 10.1053/meta.2003.50096. [DOI] [PubMed] [Google Scholar]
- 41.Donate-Correa J, Tagua VG, Ferri C, Martin-Nunez E, Hernandez-Carballo C, Urena-Torres P, et al. Pentoxifylline for renal protection in diabetic kidney disease: a model of old drugs for new horizons. J Clin Med. 2019;8:287. doi: 10.3390/jcm8030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Navarro JF, Mora C, Muros M, Garcia J. Additive antiproteinuric effect of pentoxifylline in patients with type 2 diabetes under angiotensin II receptor blockade: a short-term, randomized, controlled trial. J Am Soc Nephrol. 2005;16:2119–26. doi: 10.1681/ASN.2005010001. [DOI] [PubMed] [Google Scholar]
- 43.Navarro-Gonzalez JF, Sanchez-Nino MD, Donate-Correa J, Martin-Nunez E, Ferri C, Perez-Delgado N, et al. Effects of pentoxifylline on soluble klotho concentrations and renal tubular cell expression in diabetic kidney disease. Diabetes Care. 2018;41:1817–20. doi: 10.2337/dc18-0078. [DOI] [PubMed] [Google Scholar]
- 44.Shan D, Wu HM, Yuan QY, Li J, Zhou RL, Liu GJ. Pentoxifylline for diabetic kidney disease. Cochrane Database Syst Rev. 2012;2:CD006800. doi: 10.1002/14651858.CD006800.pub2. [DOI] [PubMed] [Google Scholar]
- 45.Honda T, Hirakawa Y, Nangaku M. The role of oxidative stress and hypoxia in renal disease. Kidney Res Clin Pract. 2019;38:414–26. doi: 10.23876/j.krcp.19.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Verma S, Singh P, Khurana S, Ganguly NK, Kukreti R, Saso L, et al. Implications of oxidative stress in chronic kidney disease: a review on current concepts and therapies. Kidney Res Clin Pract. 2021;40:183–93. doi: 10.23876/j.krcp.20.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sasaki S, Inoguchi T. The role of oxidative stress in the pathogenesis of diabetic vascular complications. Diabetes Metab J. 2012;36:255–61. doi: 10.4093/dmj.2012.36.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goligorsky MS, Chen J, Brodsky S. Workshop: endothelial cell dysfunction leading to diabetic nephropathy: focus on nitric oxide. Hypertension. 2001;37(2 Pt 2):744–8. doi: 10.1161/01.hyp.37.2.744. [DOI] [PubMed] [Google Scholar]
- 49.Xia Y, Dawson VL, Dawson TM, Snyder SH, Zweier JL. Nitric oxide synthase generates superoxide and nitric oxide in arginine-depleted cells leading to peroxynitrite-mediated cellular injury. Proc Natl Acad Sci U S A. 1996;93:6770–4. doi: 10.1073/pnas.93.13.6770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brodsky SV, Gao S, Li H, Goligorsky MS. Hyperglycemic switch from mitochondrial nitric oxide to superoxide production in endothelial cells. Am J Physiol Heart Circ Physiol. 2002;283:H2130–9. doi: 10.1152/ajpheart.00196.2002. [DOI] [PubMed] [Google Scholar]
- 51.Jha JC, Gray SP, Barit D, Okabe J, El-Osta A, Namikoshi T, et al. Genetic targeting or pharmacologic inhibition of NADPH oxidase nox4 provides renoprotection in long-term diabetic nephropathy. J Am Soc Nephrol. 2014;25:1237–54. doi: 10.1681/ASN.2013070810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gorin Y, Cavaglieri RC, Khazim K, Lee DY, Bruno F, Thakur S, et al. Targeting NADPH oxidase with a novel dual Nox1/Nox4 inhibitor attenuates renal pathology in type 1 diabetes. Am J Physiol Renal Physiol. 2015;308:F1276–87. doi: 10.1152/ajprenal.00396.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kwon G, Uddin MJ, Lee G, Jiang S, Cho A, Lee JH, et al. A novel pan-Nox inhibitor, APX-115, protects kidney injury in streptozotocin-induced diabetic mice: possible role of peroxisomal and mitochondrial biogenesis. Oncotarget. 2017;8:74217–32. doi: 10.18632/oncotarget.18540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sakashita M, Tanaka T, Inagi R. Metabolic changes and oxidative stress in diabetic kidney disease. Antioxidants (Basel) 2021;10:1143. doi: 10.3390/antiox10071143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Satirapoj B, Adler SG. Comprehensive approach to diabetic nephropathy. Kidney Res Clin Pract. 2014;33:121–31. doi: 10.1016/j.krcp.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marumo T, Yagi S, Kawarazaki W, Nishimoto M, Ayuzawa N, Watanabe A, et al. Diabetes induces aberrant DNA methylation in the proximal tubules of the kidney. J Am Soc Nephrol. 2015;26:2388–97. doi: 10.1681/ASN.2014070665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.DeFronzo RA, Reeves WB, Awad AS. Pathophysiology of diabetic kidney disease: impact of SGLT2 inhibitors. Nat Rev Nephrol. 2021;17:319–34. doi: 10.1038/s41581-021-00393-8. [DOI] [PubMed] [Google Scholar]
- 58.Salim HM, Fukuda D, Yagi S, Soeki T, Shimabukuro M, Sata M. Glycemic control with ipragliflozin, a novel selective SGLT2 inhibitor, ameliorated endothelial dysfunction in streptozotocin-induced diabetic mouse. Front Cardiovasc Med. 2016;3:43. doi: 10.3389/fcvm.2016.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shigiyama F, Kumashiro N, Miyagi M, Ikehara K, Kanda E, Uchino H, et al. Effectiveness of dapagliflozin on vascular endothelial function and glycemic control in patients with earlystage type 2 diabetes mellitus: DEFENCE study. Cardiovasc Diabetol. 2017;16:84. doi: 10.1186/s12933-017-0564-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tanaka A, Shimabukuro M, Machii N, Teragawa H, Okada Y, Shima KR, et al. Effect of empagliflozin on endothelial function in patients with type 2 diabetes and cardiovascular disease: results from the multicenter, randomized, placebo-controlled, double-blind EMBLEM trial. Diabetes Care. 2019;42:e159–61. doi: 10.2337/dc19-1177. [DOI] [PubMed] [Google Scholar]
- 61.Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393:31–9. doi: 10.1016/S0140-6736(18)32590-X. [DOI] [PubMed] [Google Scholar]
- 62.Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJ, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 63.Oh TJ, Moon JY, Hur KY, Ko SH, Kim HJ, Kim T, et al. Sodium-glucose cotransporter-2 inhibitor for renal function preservation in patients with type 2 diabetes mellitus: a Korean Diabetes Association and Korean Society of Nephrology consensus statement. Kidney Res Clin Pract. 2020;39:269–83. doi: 10.23876/j.krcp.20.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nangaku M, Kanda H, Takama H, Ichikawa T, Hase H, Akizawa T. Randomized clinical trial on the effect of bardoxolone methyl on GFR in diabetic kidney disease patients (TSUBAKI Study) Kidney Int Rep. 2020;5:879–90. doi: 10.1016/j.ekir.2020.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Zeeuw D, Akizawa T, Audhya P, Bakris GL, Chin M, ChristSchmidt H, et al. Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med. 2013;369:2492–503. doi: 10.1056/NEJMoa1306033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yamazaki T, Mimura I, Tanaka T, Nangaku M. Treatment of diabetic kidney disease: current and future. Diabetes Metab J. 2021;45:11–26. doi: 10.4093/dmj.2020.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stevens PE, Levin A, Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–30. doi: 10.7326/0003-4819-158-11-201306040-00007. [DOI] [PubMed] [Google Scholar]
- 68.An JH, Cho YM, Yu HG, Jang HC, Park KS, Kim SY, et al. The clinical characteristics of normoalbuminuric renal insufficiency in Korean type 2 diabetic patients: a possible early stage renal complication. J Korean Med Sci. 2009;24(Suppl 1):S75–81. doi: 10.3346/jkms.2009.24.S1.S75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thomas G, Sehgal AR, Kashyap SR, Srinivas TR, Kirwan JP, Navaneethan SD. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011;6:2364–73. doi: 10.2215/CJN.02180311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vistisen D, Andersen GS, Hulman A, Persson F, Rossing P, Jorgensen ME. Progressive decline in estimated glomerular filtration rate in patients with diabetes after moderate loss in kidney function-even without albuminuria. Diabetes Care. 2019;42:1886–94. doi: 10.2337/dc19-0349. [DOI] [PubMed] [Google Scholar]
- 71.MacIsaac RJ, Ekinci EI, Jerums G. ‘Progressive diabetic nephropathy: how useful is microalbuminuria?: contra’. Kidney Int. 2014;86:50–7. doi: 10.1038/ki.2014.98. [DOI] [PubMed] [Google Scholar]
- 72.Moazzeni SS, Arani RH, Hasheminia M, Tohidi M, Azizi F, Hadaegh F. High incidence of chronic kidney disease among iranian diabetic adults: using CKD-EPI and MDRD equations for estimated glomerular filtration rate. Diabetes Metab J. 2021;45:684–97. doi: 10.4093/dmj.2020.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dedual MA, Wueest S, Challa TD, Lucchini FC, Aeppli TR, Borsigova M, et al. Obesity-induced increase in cystatin c alleviates tissue inflammation. Diabetes. 2020;69:1927–35. doi: 10.2337/db19-1206. [DOI] [PubMed] [Google Scholar]
- 74.Colhoun HM, Marcovecchio ML. Biomarkers of diabetic kidney disease. Diabetologia. 2018;61:996–1011. doi: 10.1007/s00125-018-4567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pena MJ, de Zeeuw D, Mischak H, Jankowski J, Oberbauer R, Woloszczuk W, et al. Prognostic clinical and molecular biomarkers of renal disease in type 2 diabetes. Nephrol Dial Transplant. 2015;30 Suppl 4:iv86–95. doi: 10.1093/ndt/gfv252. [DOI] [PubMed] [Google Scholar]
- 76.Han WK, Bailly V, Abichandani R, Thadhani R, Bonventre JV. Kidney Injury Molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney Int. 2002;62:237–44. doi: 10.1046/j.1523-1755.2002.00433.x. [DOI] [PubMed] [Google Scholar]
- 77.Coca SG, Nadkarni GN, Huang Y, Moledina DG, Rao V, Zhang J, et al. Plasma biomarkers and kidney function decline in early and established diabetic kidney disease. J Am Soc Nephrol. 2017;28:2786–93. doi: 10.1681/ASN.2016101101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schrauben SJ, Shou H, Zhang X, Anderson AH, Bonventre JV, Chen J, et al. Association of multiple plasma biomarker concentrations with progression of prevalent diabetic kidney disease: findings from the Chronic Renal Insufficiency Cohort (CRIC) Study. J Am Soc Nephrol. 2021;32:115–26. doi: 10.1681/ASN.2020040487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.de Carvalho JA, Tatsch E, Hausen BS, Bollick YS, Moretto MB, Duarte T, et al. Urinary kidney injury molecule-1 and neutrophil gelatinase-associated lipocalin as indicators of tubular damage in normoalbuminuric patients with type 2 diabetes. Clin Biochem. 2016;49:232–6. doi: 10.1016/j.clinbiochem.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 80.Yuruk Yildirim Z, Nayir A, Yilmaz A, Gedikbasi A, Bundak R. Neutrophil gelatinase-associated lipocalin as an early sign of diabetic kidney injury in children. J Clin Res Pediatr Endocrinol. 2015;7:274–9. doi: 10.4274/jcrpe.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lacquaniti A, Donato V, Pintaudi B, Di Vieste G, Chirico V, Buemi A, et al. “Normoalbuminuric” diabetic nephropathy: tubular damage and NGAL. Acta Diabetol. 2013;50:935–42. doi: 10.1007/s00592-013-0485-7. [DOI] [PubMed] [Google Scholar]
- 82.Nielsen SE, Sugaya T, Hovind P, Baba T, Parving HH, Rossing P. Urinary liver-type fatty acid-binding protein predicts progression to nephropathy in type 1 diabetic patients. Diabetes Care. 2010;33:1320–4. doi: 10.2337/dc09-2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kamijo-Ikemori A, Sugaya T, Yasuda T, Kawata T, Ota A, Tatsunami S, et al. Clinical significance of urinary liver-type fatty acid-binding protein in diabetic nephropathy of type 2 diabetic patients. Diabetes Care. 2011;34:691–6. doi: 10.2337/dc10-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Panduru NM, Forsblom C, Saraheimo M, Thorn L, Bierhaus A, Humpert PM, et al. Urinary liver-type fatty acid-binding protein and progression of diabetic nephropathy in type 1 diabetes. Diabetes Care. 2013;36:2077–83. doi: 10.2337/dc12-1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kim SS, Song SH, Kim IJ, Jeon YK, Kim BH, Kwak IS, et al. Urinary cystatin C and tubular proteinuria predict progression of diabetic nephropathy. Diabetes Care. 2013;36:656–61. doi: 10.2337/dc12-0849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hasegawa G, Nakano K, Sawada M, Uno K, Shibayama Y, Ienaga K, et al. Possible role of tumor necrosis factor and interleukin-1 in the development of diabetic nephropathy. Kidney Int. 1991;40:1007–12. doi: 10.1038/ki.1991.308. [DOI] [PubMed] [Google Scholar]
- 87.Bertani T, Abbate M, Zoja C, Corna D, Perico N, Ghezzi P, et al. Tumor necrosis factor induces glomerular damage in the rabbit. Am J Pathol. 1989;134:419–30. [PMC free article] [PubMed] [Google Scholar]
- 88.Kalantarinia K, Awad AS, Siragy HM. Urinary and renal interstitial concentrations of TNF-alpha increase prior to the rise in albuminuria in diabetic rats. Kidney Int. 2003;64:1208–13. doi: 10.1046/j.1523-1755.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- 89.Niewczas MA, Gohda T, Skupien J, Smiles AM, Walker WH, Rosetti F, et al. Circulating TNF receptors 1 and 2 predict ESRD in type 2 diabetes. J Am Soc Nephrol. 2012;23:507–15. doi: 10.1681/ASN.2011060627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Skupien J, Warram JH, Niewczas MA, Gohda T, Malecki M, Mychaleckyj JC, et al. Synergism between circulating tumor necrosis factor receptor 2 and HbA(1c) in determining renal decline during 5-18 years of follow-up in patients with type 1 diabetes and proteinuria. Diabetes Care. 2014;37:2601–8. doi: 10.2337/dc13-1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lopes-Virella MF, Baker NL, Hunt KJ, Cleary PA, Klein R, Virella G, et al. Baseline markers of inflammation are associated with progression to macroalbuminuria in type 1 diabetic subjects. Diabetes Care. 2013;36:2317–23. doi: 10.2337/dc12-2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wu LL, Chiou CC, Chang PY, Wu JT. Urinary 8-OHdG: a marker of oxidative stress to DNA and a risk factor for cancer, atherosclerosis and diabetics. Clin Chim Acta. 2004;339:1–9. doi: 10.1016/j.cccn.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 93.Xu GW, Yao QH, Weng QF, Su BL, Zhang X, Xiong JH. Study of urinary 8-hydroxydeoxyguanosine as a biomarker of oxidative DNA damage in diabetic nephropathy patients. J Pharm Biomed Anal. 2004;36:101–4. doi: 10.1016/j.jpba.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 94.Sanchez M, Roussel R, Hadjadj S, Moutairou A, Marre M, Velho G, et al. Plasma concentrations of 8-hydroxy-2’-deoxyguanosine and risk of kidney disease and death in individuals with type 1 diabetes. Diabetologia. 2018;61:977–84. doi: 10.1007/s00125-017-4510-1. [DOI] [PubMed] [Google Scholar]
- 95.Serdar M, Sertoglu E, Uyanik M, Tapan S, Akin K, Bilgi C, et al. Comparison of 8-hydroxy-2’-deoxyguanosine (8-OHdG) levels using mass spectrometer and urine albumin creatinine ratio as a predictor of development of diabetic nephropathy. Free Radic Res. 2012;46:1291–5. doi: 10.3109/10715762.2012.710902. [DOI] [PubMed] [Google Scholar]
- 96.Dubin RF, Rhee EP. Proteomics and metabolomics in kidney disease, including insights into etiology, treatment, and prevention. Clin J Am Soc Nephrol. 2020;15:404–11. doi: 10.2215/CJN.07420619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bhensdadia NM, Hunt KJ, Lopes-Virella MF, Michael Tucker J, Mataria MR, Alge JL, et al. Urine haptoglobin levels predict early renal functional decline in patients with type 2 diabetes. Kidney Int. 2013;83:1136–43. doi: 10.1038/ki.2013.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Good DM, Zurbig P, Argiles A, Bauer HW, Behrens G, Coon JJ, et al. Naturally occurring human urinary peptides for use in diagnosis of chronic kidney disease. Mol Cell Proteomics. 2010;9:2424–37. doi: 10.1074/mcp.M110.001917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zurbig P, Jerums G, Hovind P, Macisaac RJ, Mischak H, Nielsen SE, et al. Urinary proteomics for early diagnosis in diabetic nephropathy. Diabetes. 2012;61:3304–13. doi: 10.2337/db12-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Roscioni SS, de Zeeuw D, Hellemons ME, Mischak H, Zurbig P, Bakker SJ, et al. A urinary peptide biomarker set predicts worsening of albuminuria in type 2 diabetes mellitus. Diabetologia. 2013;56:259–67. doi: 10.1007/s00125-012-2755-2. [DOI] [PubMed] [Google Scholar]
- 101.Zurbig P, Mischak H, Menne J, Haller H. CKD273 enables efficient prediction of diabetic nephropathy in nonalbuminuric patients. Diabetes Care. 2019;42:e4–5. doi: 10.2337/dc18-1322. [DOI] [PubMed] [Google Scholar]
- 102.Tofte N, Lindhardt M, Adamova K, Bakker SJ, Beige J, Beulens JW, et al. Early detection of diabetic kidney disease by urinary proteomics and subsequent intervention with spironolactone to delay progression (PRIORITY): a prospective observational study and embedded randomised placebo-controlled trial. Lancet Diabetes Endocrinol. 2020;8:301–12. doi: 10.1016/S2213-8587(20)30026-7. [DOI] [PubMed] [Google Scholar]
- 103.Lindhardt M, Persson F, Zurbig P, Stalmach A, Mischak H, de Zeeuw D, et al. Urinary proteomics predict onset of microalbuminuria in normoalbuminuric type 2 diabetic patients, a sub-study of the DIRECT-Protect 2 study. Nephrol Dial Transplant. 2017;32:1866–73. doi: 10.1093/ndt/gfw292. [DOI] [PubMed] [Google Scholar]
- 104.Kolch W, Neusüss C, Pelzing M, Mischak H. Capillary electrophoresis-mass spectrometry as a powerful tool in clinical diagnosis and biomarker discovery. Mass Spectrom Rev. 2005;24:959–77. doi: 10.1002/mas.20051. [DOI] [PubMed] [Google Scholar]
- 105.Hocher B, Adamski J. Metabolomics for clinical use and research in chronic kidney disease. Nat Rev Nephrol. 2017;13:269–84. doi: 10.1038/nrneph.2017.30. [DOI] [PubMed] [Google Scholar]
- 106.Han LD, Xia JF, Liang QL, Wang Y, Wang YM, Hu P, et al. Plasma esterified and non-esterified fatty acids metabolic profiling using gas chromatography-mass spectrometry and its application in the study of diabetic mellitus and diabetic nephropathy. Anal Chim Acta. 2011;689:85–91. doi: 10.1016/j.aca.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 107.Hirayama A, Nakashima E, Sugimoto M, Akiyama S, Sato W, Maruyama S, et al. Metabolic profiling reveals new serum biomarkers for differentiating diabetic nephropathy. Anal Bioanal Chem. 2012;404:3101–9. doi: 10.1007/s00216-012-6412-x. [DOI] [PubMed] [Google Scholar]
- 108.Zhang J, Yan L, Chen W, Lin L, Song X, Yan X, et al. Metabonomics research of diabetic nephropathy and type 2 diabetes mellitus based on UPLC-oaTOF-MS system. Anal Chim Acta. 2009;650:16–22. doi: 10.1016/j.aca.2009.02.027. [DOI] [PubMed] [Google Scholar]
- 109.Pena MJ, Lambers Heerspink HJ, Hellemons ME, Friedrich T, Dallmann G, Lajer M, et al. Urine and plasma metabolites predict the development of diabetic nephropathy in individuals with type 2 diabetes mellitus. Diabet Med. 2014;31:1138–47. doi: 10.1111/dme.12447. [DOI] [PubMed] [Google Scholar]
- 110.Looker HC, Colombo M, Hess S, Brosnan MJ, Farran B, Dalton RN, et al. Biomarkers of rapid chronic kidney disease progression in type 2 diabetes. Kidney Int. 2015;88:888–96. doi: 10.1038/ki.2015.199. [DOI] [PubMed] [Google Scholar]
- 111.Kwan B, Fuhrer T, Zhang J, Darshi M, Van Espen B, Montemayor D, et al. Metabolomic markers of kidney function decline in patients with diabetes: evidence from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis. 2020;76:511–20. doi: 10.1053/j.ajkd.2020.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mutter S, Valo E, Aittomaki V, Nybo K, Raivonen L, Thorn LM, et al. Urinary metabolite profiling and risk of progression of diabetic nephropathy in 2670 individuals with type 1 diabetes. Diabetologia. 2022;65:140–9. doi: 10.1007/s00125-021-05584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pezzolesi MG, Satake E, McDonnell KP, Major M, Smiles AM, Krolewski AS. Circulating TGF-β1-regulated miRNAs and the risk of rapid progression to ESRD in type 1 diabetes. Diabetes. 2015;64:3285–93. doi: 10.2337/db15-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Argyropoulos C, Wang K, Bernardo J, Ellis D, Orchard T, Galas D, et al. Urinary microRNA profiling predicts the development of microalbuminuria in patients with type 1 diabetes. J Clin Med. 2015;4:1498–517. doi: 10.3390/jcm4071498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Barutta F, Tricarico M, Corbelli A, Annaratone L, Pinach S, Grimaldi S, et al. Urinary exosomal microRNAs in incipient diabetic nephropathy. PLoS One. 2013;8:e73798. doi: 10.1371/journal.pone.0073798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kato M. Noncoding RNAs as therapeutic targets in early stage diabetic kidney disease. Kidney Res Clin Pract. 2018;37:197–209. doi: 10.23876/j.krcp.2018.37.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]


