Abstract
Current clinical management of major mental disorders, such as autism spectrum disorder, depression and schizophrenia, is less than optimal. Recent scientific advances have indicated that deficits in oxidative and inflammation systems are extensively involved in the pathogenesis of these disorders. These findings have led to expanded considerations for treatment. Sulforaphane (SFN) is a dietary phytochemical extracted from cruciferous vegetables. It is an effective activator of the transcription factor nuclear erythroid-2 like factor-2, which can upregulate multiple antioxidants and protect neurons against various oxidative damages. On the other hand, it can also significantly reduce inflammatory response to pathological states and decrease the damage caused by the immune response via the nuclear factor-κB pathway and other pathways. In this review, we introduce the biological mechanisms of SFN and the pilot evidence from its clinical trials of major mental disorders, hoping to promote an increase in psychiatric clinical studies of SFN.
Keywords: Psychiatry
Introduction
Sulforaphane (SFN, 4-methylsulfinylbutyl isothiocyanate) is a dietary phytochemical abundant in the seeds and sprouts of cruciferous plants. It is present in plants as its biologically inactive precursor, glucoraphanin (GR).1 When cut or chewed, GR is hydrolysed into the corresponding isothiocyanate SFN either by the plant thioglucosidase myrosinase or by bacterial thioglucosidase in the colon.2 Pharmacokinetic studies in both humans and animals revealed that the plasma concentration of SFN and its metabolites increase rapidly, with peak plasma concentration 1–3 hours after administration of SFN.3 Furthermore, SFN can cross the blood–brain barrier (BBB) and accumulate in the brain. A mouse study demonstrated that after SFN gavage, SFN is able to cross the BBB, accumulate in the ventral midbrain and striatum, attain a peak concentration in 15 min and then disappear after 2 hours,4 suggesting that it may have potential pharmacological activity in the central nervous system.
SFN has a wide range of biological activities, including antioxidant, anti-inflammatory, anticancer and cytoprotective effects.1 5 Its involvement in the pathological process of tumours, diabetes, ageing, cardiovascular disease and many other diseases has been proven.6–8
Mental disorders create a major public health burden worldwide, but current therapies provide relatively modest efficacy and noticeable adverse effects.9 The potential application of SFN to mental disorders has attracted much attention from researchers. Recently, several studies have reported findings suggesting that SFN might confer neuroprotective effects on mental disorders by inhibiting oxidative stress, neuroinflammation and neuronal death.10 11
Biological mechanisms of SFN
Antioxidation
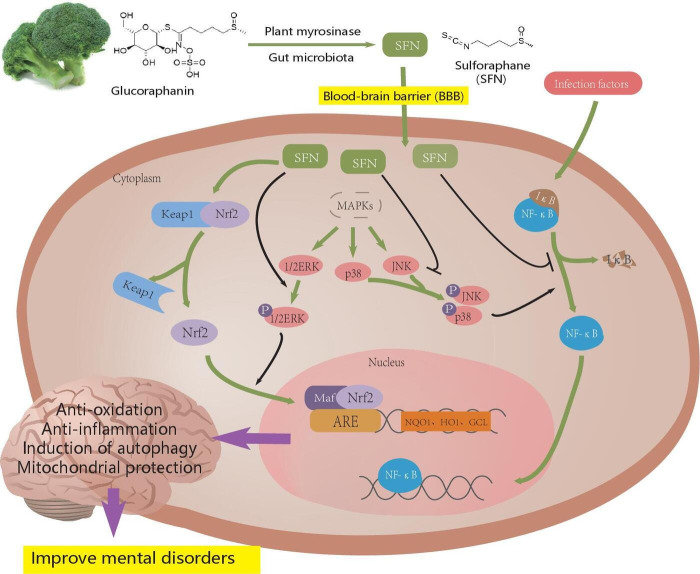
One of the key mechanisms of SFN is the activation of nuclear factor erythroid 2-related factor 2 (Nrf2). Under physiological conditions, Nrf2 forms a complex with Kelch-like ECH-associated protein 1 (Keap1) in the cytoplasm. Keap1 is a redox-sensitive E3 ubiquitin ligase substrate adaptor that inhibits the effect of Nrf2 and promotes the ubiquitination and degradation of Nrf2 through the ubiquitin-proteasome system.12 After entering the cell, SFN chemically reacts with reactive cysteine residues on Keap1,13 and subsequently Nrf2 is diverted from the inactivated Keap1. It translocates to the nucleus, where it forms a heterodimer with small Maf proteins (MafG, MafK, MafF), which endow it with a DNA-binding capacity to attach to its consensus sequence, the antioxidant response element (ARE) of phase 2 genes, to activate their transcription.14 15 In addition to bonding with Keap1, SFN can also enhance the activity of Nrf2 by suppressing the activity of glycogen synthase kinase-3β (GSK-3β),16 reducing methylation of the first 15 CpGs of Nrf2 promoters17 and altering the translocation and stability of Nrf2.8 18 ARE induction by Nrf2 can upregulate its downstream products, including NAD(P)H quinone dehydrogenase 1,19 20 haem oxygenase 1 (HO-1)20 21 and glutamate cysteine ligase,21–23 and protect neuronal cell lines against various oxidative damages22–25 (figure 1).
Figure 1.
Biological mechanisms of sulforaphane. ARE, antioxidant response element; ERK, extracellular signal-regulated kinase; GCL, glutamate cysteine ligase; HO1, haem oxygenase 1; IκB, inhibitor of NF-κB; JNK, c-Jun N-terminal kinase; Keap1, Kelch-like ECH-associated protein 1; MAPK, mitogen-activated protein kinase; NF-κB, nuclear factor-κB; NQO1, NAD(P)H quinone dehydrogenase 1; Nrf2, nuclear factor erythroid 2-related factor 2.
Accumulating evidence reveals that oxidative stress is a crucial factor in the initiation and development of mental disorders. SFN can attenuate the oxidative stress in the periphery and brain of autism spectrum disorder (ASD) mouse models by upregulating the expression of enzymatic antioxidants, including superoxide dismutase 1, glutathione peroxidase 1 and glutathione reductase, as well as reducing the level of lipid peroxides.26 SFN can also reduce oxidative stress by normalising the decreased expression of HO-1 and glutathione (GSH) in subjects with ASD and depression.27–29 Recently, studies using postmortem brain samples showed that compared with healthy controls, patients with a history of mental disorders, such as depression and schizophrenia, have fewer Keap1 and Nrf2 proteins in their brain.30 Similar variation is observed in mice with a depression-like phenotype, which can be restored by SFN, suggesting that SFN is likely to protect the neurons from antioxidant damage through the Nrf2 pathway.27 31
Anti-inflammation
Inflammation and immune dysregulation are widely accepted physiological aberrations in individuals with mental disorders. The mechanism by which SFN regulates the inflammatory response is probably associated with nuclear factor-κB (NF-κB). NF-κB is sequestered as an inactive form in the cytoplasm by inhibitor of NF-κB (IκB) family members.32 When an infection factor activates specific immune signalling pathways, the IκB proteins are ubiquitinated and degraded, leading to the translocation of NF-κB to the nucleus.32 Subsequently, NF-κB binds to DNA and induces the expression of proinflammatory cytokines, including tumour necrosis factor-α (TNF-α), interleukin 1β (IL-1β) and interleukin 6 (IL-6), as well as prostaglandin E2 (PGE2), inducible nitric oxide synthase (iNOS), cyclo-oxygenase-2 (COX-2), vascular adhesion molecules and others.33 SFN can exert anti-inflammatory effects by reducing the expression of NF-κB and its nuclear translocation and DNA-binding ability.26 34 In addition to the NF-κB pathway, SFN also inhibits neuroinflammation by regulating mitogen-activated protein kinases (MAPKs), including p38, c-Jun N-terminal kinase (JNK) and extracellular signal-regulated kinase (ERK),35 and by promoting the polarisation of the microglia from M1 to an anti-inflammatory M2 type.36
A study conducted by Qin et al37 suggested that SFN attenuated the proinflammatory response induced by lipopolysaccharides (LPS) via downregulating the MAPK/NF-κB signalling pathway and reducing the mRNA and protein of proinflammatory mediators such as TNF-α, IL-1β, IL-6 and iNOS in a concentration-dependent manner in BV-2 cells, thereby indirectly inhibiting microglia-mediated neuroinflammation and neuronal damage. Their study also indicated that the MAPK signalling pathway is upstream of NF-κB p65. Similar results have been reported by Subedi and colleagues.33 They found that SFN reduced the JNK phosphorylation levels, which subsequently downregulated the NF-κB pathway, resulting in decreased expression of the inflammatory mediators (iNOS, COX-2, nitric oxide and PGE2) and proinflammatory cytokines (TNF-α, IL-6 and IL-1β) in LPS-activated microglia. Furthermore, in a recent clinical trial, SFN treatment also significantly downregulated the expression of inflammatory markers, including IL-6, TNF-α and IL-1β, in subjects with ASD compared with the placebo group.29 These results suggest a possibility that SFN could be applied to mental illness by modulating neuroinflammation.
Other potential mechanisms
SFN also protects neurons through autophagy.38 Studies have shown that SFN activates ERK by increasing reactive oxygen species, thereby increasing neuronal autophagy flux marker microtubule-associated protein 1 light chain 3-II levels and inducing autophagy whose dysfunction could lead to ASD-like synaptic pruning defects and ultimately create ASD-like social behaviours.39 40
In addition, SFN activates Nrf2 to protect mitochondrial complex I, II and IV from dysfunction and promotes mitochondrial biogenesis, which has proven involvement in the prevention and treatment of mental disorders.41 A randomised controlled trial showed that the mitochondrial dysfunction was significantly improved in subjects treated with SFN but not in those treated with a placebo. The improvement in mitochondrial parameters correlated with the improvement in ASD symptoms.42
Moreover, SFN also improves the synaptic plasticity for neuroprotection. Zhang and colleagues43 found that in LPS-induced depression-like mice, the levels of brain synaptic markers, including postsynaptic density protein 95 (PSD95) and GluA1, as well as brain-derived neurotrophic factor (BDNF) and dendritic spine density, were markedly decreased in the prefrontal cortex (PFC), dentate gyrus (DG) and CA3 of the hippocampus and markedly increased in the nucleus accumbens (NAc)—all of which were subsequently recovered to control levels by SFN. Moreover, dietary intake of 0.1% GR also prevented the decrease of PSD95, GluA1, BDNF and dendritic spine density in PFC, CA3 and DG, and the increase of BDNF and dendritic spine density in NAc. Yao et al44 likewise found that SFN increased the number of neurite outgrowth cells in PC12 cells in a concentration-dependent manner.
Furthermore, a new theory suggests neuronal protection from apoptosis by SFN. Lee et al21 found that SFN treatment attenuated the apoptotic characteristics of cells, including activation of c-Jun N-terminal kinase (c-JNK), changes in the mitochondrial membrane potential, increased expression of BCL-2 gene and DNA fragmentation. A further study conducted by Zhou et al38 revealed that SFN probably exerts neuroprotective effects by inhibiting the mammalian target of rapamycin-dependent neuronal apoptosis.
Clinical efficacy of SFN for mental disorders
Autism spectrum disorder
ASD is a neurodevelopmental disorder characterised by deficits in social interactions and communication, restricted interest, and repetitive behaviours, starting in early childhood and affecting about 1 in 68 children aged 8 years in the USA.45
Over the past 8 years, SFN has been clinically studied and has proved beneficial for individuals with ASD (table 1).46 The first placebo-controlled, double-blind, randomised trial was reported in 2014, lasting 18 weeks and comprising 44 males aged 13–27 with a diagnosis of ASD. It found that compared with placebo, participants receiving SFN showed significant improvement in the Aberrant Behavior Checklist (ABC) scores by 34% and in the Social Responsiveness Scale (SRS) scores by 17%, as well as improvement in social interaction, abnormal behaviour and verbal communication on the Clinical Global Impression Improvement Scale. However, when the administration of SFN stopped, the total scores of all scales returned to pretreatment levels.47 It was noted that those in the follow-up case series from this trial also reported positive results. After completing the intervention phase of the original trial, many subjects continued to use SFN supplements to try to maintain improvements similar to those noted during the intervention. During the intervention phase and the subsequent 3-year follow-up, many subjects reported positive effects from SFN.48
Table 1.
Characteristics and findings of reviewed clinical studies
| Disorder and first author (year) | Study design, participant age and group | SFN treatment (route/dose) | Study duration | Main findings |
| ASD, Singh (2014)47 | RCT, 13–27 years. SFN (n=26), placebo (n=14). |
Oral route. Weight-based dose: 50 µmol (<45.36 kg), 100 µmol (45.81–90.26 kg) or 150 µmol (>90.72 kg) per day. |
22 weeks (18 weeks of treatment; 4 weeks of follow-up without treatment). | SFN significantly improved ABC and SRS scores by 34% (p<0.001) and 17% (p=0.017), respectively, as well as improved the social interaction (p=0.007), abnormal behaviour (p=0.014) and verbal communication (p=0.015) on CGI-I. When the administration of sulforaphane stopped, the total scores of all scales returned to pretreatment levels. |
| ASD, Bent (2018)49 | Open-label study, 5–22 years. SFN (n=15). |
Oral route. Weight-based dose: 1.14 µmol/kg. |
12 weeks. | SFN significantly improved the ABC score by 7.1 points (-7.1) (95% CI: −17.4 to 3.2, p=0.18) and SRS score by 9.7 points (-9.7) (95% CI: −18.7 to −0.8, p=0.03). |
| ASD, Momtazmanesh (2020)50 | RCT, 4–12 years. Risperidone+SFN (n=30), risperidone+placebo (n=30). |
Oral route. Weight-based dose: 50 µmol (≤45 kg) or 100 µmol (>45 kg) per day. |
10 weeks. | SFN showed significant improvement in irritability score (p=0.001) and hyperactivity/non-compliance score (p=0.015), as well as significant time by treatment effect for irritability (p=0.007) and hyperactivity/non-compliance (p=0.008). |
| ASD, Zimmerman (2021)29 | RCT, 3–12 years. SFN (n=22), placebo (n=23). |
Oral route. Weight-based dose: 2.2 µmol/kg/day. |
36 weeks (15 weeks of treatment; open-label SFN treatment of all children for 15 weeks; 6 weeks of follow-up without treatment). |
SFN showed significant improvement on the ABC scale at 15 weeks (p<0.02) and a tendency to improve the total score on OACIS-I at 7 and 15 weeks. |
| Depression, Ghazizadeh-Hashemi (2021)51 | RCT, 40–65 years+cardiac intervention history. SFN (n=30), placebo (n=30). |
Oral route 30 mg/day. | 6 weeks. | The sulforaphane group exhibited greater improvement on HAM-D scores (p<0.001), higher rate of response to treatment (30% vs 6.67%, p=0.042) and an upward tendency towards remission (23.33% vs 3.33%, p=0.052). |
| Schizophrenia, Shiina (2015)54 |
Open-label study, 20–65 years. SFN (n=7). |
Oral route 30 mg/day. | 8 weeks. | After SFN treatment, the mean scores in the OCLT showed a significant increase from 0.88 to 0.95 (p=0.043). |
| Schizophrenia, Dickerson (2021)55 | RCT, 18–65 years. SFN (n=29), placebo (n=29). |
100 µmol/day. | 18 weeks (2 weeks of single-blind placebo treatment followed by 16 weeks of double-blind SFN or placebo treatment). | No significant difference in psychiatric symptoms or cognitive function was observed between the SFN or placebo group. |
ABC, Aberrant Behavior Checklist; ASD, autism spectrum disorder; CGI-I, Clinical Global Impression Improvement Scale; HAM-D, Hamilton Rating Scale for Depression; OACIS-I, Ohio Autism Clinical Impressions Scale-Improvement; OCLT, One Card Learning Task; RCT, randomised clinical trials; SFN, sulforaphane; SRS, Social Responsiveness Scale.
Another 12-week, open-label study of 15 children with ASD also showed significant improvement in ABC scores by 7.1 points and SRS scores by 9.7 points.49 In addition, Momtazmanesh and fellows50 conducted a 10-week, randomised, double-blind, placebo-controlled clinical trial with 30 children in SFN and placebo groups, respectively, showing the safety and efficacy of SFN as an adjunctive treatment to significantly improve irritability and hyperactivity symptoms of children with ASD. More recently, a phase III, 36-week, randomised controlled trial with 45 children aged 3–12 years with ASD also observed significant improvement on ABC scales and a tendency to improve the total score of the Ohio Autism Clinical Impressions Scale-Improvement (OACIS-I) after treatment of SFN versus placebo.29 All of these studies highlight the potential of SFN to benefit patients with ASD in the future clinically.
Depression
Depression is a severe public health problem with a high prevalence worldwide. About one-third of patients with depression do not respond well to antidepressants. SFN is currently considered a potential agent for depression therapy.
A randomised, double-blind, placebo-controlled clinical trial was recently conducted in patients with a cardiac intervention history. Compared with the placebo group (n=30), the SFN group (n=30) exhibited greater improvement in the Hamilton Rating Scale for Depression scores, higher rates of response to treatment and an upward tendency towards remission.51 Another randomised, double-blind, placebo-controlled, parallel-group clinical trial of SFN for depression is ongoing in China.52
Schizophrenia
Schizophrenia is a severe psychotic disorder characterised by cognitive impairment and positive and negative symptoms, affecting about 1% of the world’s population.53 The illness is lifelong, and unfortunately the efficacy of antipsychotics is not optimal for many patients, leading to high rates of mental disability among populations with schizophrenia. It has been hypothesised that deficits in antioxidation and anti-inflammation systems play vital roles in the pathophysiological mechanisms of schizophrenia,11 driving researchers to examine the clinical value of SFN for patients with this illness.
Cognitive impairment is schizophrenia’s core symptom. An open study involving seven patients with schizophrenia found that the average score in the accuracy component of the One Card Learning Task increased significantly after an 8-week SFN administration; this highlighted the potential of SFN to improve some domains of cognitive function in patients with schizophrenia.54 However, another randomised, double-blind, placebo-controlled trial found no difference in psychotic symptoms or cognitive function between the active (n=29) or placebo (n=29) group after SFN or placebo treatment, respectively, for 16 weeks.55 These results suggest that additional randomised clinical trials (RCTs) with large sample sizes are necessary to examine the efficacy of SFN for schizophrenia.
Recently, the potential value of SFN in the prevention of psychosis has attracted much attention from researchers. The aberrant expression of numerous inflammatory cytokines and oxidative stress-related biomarkers has been reported in the prodromal stage of psychosis.56 Subjects at clinical high risk (CHR) of psychosis provide a golden opportunity for examining the value of SFN in decreasing the psychosis conversion rate. A randomised, double-blind, placebo-controlled, clinical multicentre trial to evaluate the efficacy of SFN versus placebo in reducing risk and conversion rates in CHR individuals is ongoing in China.57 Expectations about its findings are high, as psychosis prevention remains a considerable challenge in psychiatry.
Conclusion and future perspective
The oxidative and inflammation system deficits are extensively involved in the pathogenesis of major mental disorders, such as ASD, depression and schizophrenia. Considering its good pharmacokinetics and safety, SFN is a promising choice for treating these mental disorders due to its antioxidation and anti-inflammation capabilities. RCTs with large sample sizes and high-quality designs are urgently needed to clarify the evidence on SFN clinical efficacy.
Acknowledgments
We would like to thank Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine for helping us produce our work.
Biography
Wensi Zheng obtained her bachelor degree from the Shanghai Jiao Tong University School of Medicine, China in 2021. She is now a PHD candidate in Shanghai Jiao Tong University School of Medicine in China. Her research interests include the early identification and intervention for psychiatric disorders.

Footnotes
Contributors: All authors contributed to the idea for the article and performed the literature search. WZ wrote the paper. JW read and edited the manuscript.
Funding: This work is supported by the following: National Natural Science Foundation of China (grants 82151314, 81971251, 81671329, 81871050, 82171497, 82101582 and 82001406); Clinical Research Center at Shanghai Mental Health Center (grants CRC2018ZD01, CRC2018ZD04, CRC2018YB01, CRC2019ZD02 and 2020-FX-02); Clinical Research Center at Shanghai Jiao Tong University School of Medicine (DLY201817 and 20190102); Shanghai Science and Technology Committee Foundation (19411950800, 16ZR1430500, 19411969100, 19410710800, 21ZR1481500, 20ZR1448600, 21S31903100 and 19ZR14451); Shanghai Clinical Research Center for Mental Health (19MC1911100); Project of the Key Discipline Construction, Shanghai 3-Year Public Health Action Plan (GWV-10.1-XK18); and Shanghai Municipal Science and Technology Major Project (no: 2018SHZDZX01 and 2018SHZDZX05).
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Fahey JW, Wade KL, Wehage SL, et al. Stabilized sulforaphane for clinical use: phytochemical delivery efficiency. Mol Nutr Food Res 2017;61. 10.1002/mnfr.201600766. [Epub ahead of print: 08 02 2017]. [DOI] [PubMed] [Google Scholar]
- 2.Matusheski NV, Juvik JA, Jeffery EH. Heating decreases epithiospecifier protein activity and increases sulforaphane formation in broccoli. Phytochemistry 2004;65:1273–81. 10.1016/j.phytochem.2004.04.013 [DOI] [PubMed] [Google Scholar]
- 3.Egner PA, Chen JG, Wang JB, et al. Bioavailability of sulforaphane from two broccoli sprout beverages: results of a short-term, cross-over clinical trial in Qidong, China. Cancer Prev Res 2011;4:384–95. 10.1158/1940-6207.CAPR-10-0296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jazwa A, Rojo AI, Innamorato NG, et al. Pharmacological targeting of the transcription factor Nrf2 at the basal ganglia provides disease modifying therapy for experimental parkinsonism. Antioxid Redox Signal 2011;14:2347–60. 10.1089/ars.2010.3731 [DOI] [PubMed] [Google Scholar]
- 5.Vanduchova A, Anzenbacher P, Anzenbacherova E. Isothiocyanate from broccoli, sulforaphane, and its properties. J Med Food 2019;22:121–6. 10.1089/jmf.2018.0024 [DOI] [PubMed] [Google Scholar]
- 6.Russo M, Spagnuolo C, Russo GL, et al. Nrf2 targeting by sulforaphane: a potential therapy for cancer treatment. Crit Rev Food Sci Nutr 2018;58:1391–405. 10.1080/10408398.2016.1259983 [DOI] [PubMed] [Google Scholar]
- 7.Sun Y, Zhou S, Guo H, et al. Protective effects of sulforaphane on type 2 diabetes-induced cardiomyopathy via AMPK-mediated activation of lipid metabolic pathways and Nrf2 function. Metabolism 2020;102:154002. 10.1016/j.metabol.2019.154002 [DOI] [PubMed] [Google Scholar]
- 8.Kubo E, Chhunchha B, Singh P, et al. Sulforaphane reactivates cellular antioxidant defense by inducing Nrf2/ARE/Prdx6 activity during aging and oxidative stress. Sci Rep 2017;7:14130. 10.1038/s41598-017-14520-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiang P, Sun X, Ren J, et al. Effects of the combination of second-generation antipsychotics on serum concentrations of aripiprazole and dehydroaripiprazole in Chinese patients with schizophrenia. Gen Psychiatr 2021;34:e100423. 10.1136/gpsych-2020-100423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schepici G, Bramanti P, Mazzon E. Efficacy of sulforaphane in neurodegenerative diseases. Int J Mol Sci 2020;21. 10.3390/ijms21228637. [Epub ahead of print: 16 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang C, Wu J, Chen D, et al. Effects of sulforaphane in the central nervous system. Eur J Pharmacol 2019;853:153–68. 10.1016/j.ejphar.2019.03.010 [DOI] [PubMed] [Google Scholar]
- 12.Zalachoras I, Hollis F, Ramos-Fernández E, et al. Therapeutic potential of glutathione-enhancers in stress-related psychopathologies. Neurosci Biobehav Rev 2020;114:134–55. 10.1016/j.neubiorev.2020.03.015 [DOI] [PubMed] [Google Scholar]
- 13.Dinkova-Kostova AT, Kostov RV, Canning P. Keap1, the cysteine-based mammalian intracellular sensor for electrophiles and oxidants. Arch Biochem Biophys 2017;617:84–93. 10.1016/j.abb.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pu D, Zhao Y, Chen J, et al. Protective effects of sulforaphane on cognitive impairments and AD-like lesions in diabetic mice are associated with the upregulation of Nrf2 transcription activity. Neuroscience 2018;381:35–45. 10.1016/j.neuroscience.2018.04.017 [DOI] [PubMed] [Google Scholar]
- 15.Silva-Palacios A, Ostolga-Chavarría M, Zazueta C, et al. Nrf2: molecular and epigenetic regulation during aging. Ageing Res Rev 2018;47:31–40. 10.1016/j.arr.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 16.Shang G, Tang X, Gao P, et al. Sulforaphane attenuation of experimental diabetic nephropathy involves GSK-3 beta/Fyn/Nrf2 signaling pathway. J Nutr Biochem 2015;26:596–606. 10.1016/j.jnutbio.2014.12.008 [DOI] [PubMed] [Google Scholar]
- 17.Su Z-Y, Zhang C, Lee JH, et al. Requirement and epigenetics reprogramming of Nrf2 in suppression of tumor promoter TPA-induced mouse skin cell transformation by sulforaphane. Cancer Prev Res 2014;7:319–29. 10.1158/1940-6207.CAPR-13-0313-T [DOI] [PubMed] [Google Scholar]
- 18.Magesh S, Chen Y, Hu L. Small molecule modulators of Keap1-Nrf2-ARE pathway as potential preventive and therapeutic agents. Med Res Rev 2012;32:687–726. 10.1002/med.21257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao F, Zhang J, Chang N. Epigenetic modification of Nrf2 by sulforaphane increases the antioxidative and anti-inflammatory capacity in a cellular model of Alzheimer's disease. Eur J Pharmacol 2018;824:1–10. 10.1016/j.ejphar.2018.01.046 [DOI] [PubMed] [Google Scholar]
- 20.Soane L, Li Dai W, Fiskum G, et al. Sulforaphane protects immature hippocampal neurons against death caused by exposure to hemin or to oxygen and glucose deprivation. J Neurosci Res 2010;88:1355–63. 10.1002/jnr.22307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee C, Park GH, Lee S-R, et al. Attenuation of β-amyloid-induced oxidative cell death by sulforaphane via activation of NF-E2-related factor 2. Oxid Med Cell Longev 2013;2013:313510. 10.1155/2013/313510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alfieri A, Srivastava S, Siow RCM, et al. Sulforaphane preconditioning of the Nrf2/HO-1 defense pathway protects the cerebral vasculature against blood-brain barrier disruption and neurological deficits in stroke. Free Radic Biol Med 2013;65:1012–22. 10.1016/j.freeradbiomed.2013.08.190 [DOI] [PubMed] [Google Scholar]
- 23.Sedlak TW, Paul BD, Parker GM, et al. The glutathione cycle shapes synaptic glutamate activity. Proc Natl Acad Sci U S A 2019;116:2701–6. 10.1073/pnas.1817885116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santín-Márquez R, Alarcón-Aguilar A, López-Diazguerrero NE, et al. Sulforaphane - role in aging and neurodegeneration. Geroscience 2019;41:655–70. 10.1007/s11357-019-00061-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun Y, Yang T, Mao L, et al. Sulforaphane protects against brain diseases: roles of cytoprotective enzymes. Austin J Cerebrovasc Dis Stroke 2017;4. 10.26420/austinjcerebrovascdisstroke.2017.1054. [Epub ahead of print: 16 02 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nadeem A, Ahmad SF, Al-Harbi NO, et al. Nrf2 activator, sulforaphane ameliorates autism-like symptoms through suppression of Th17 related signaling and rectification of oxidant-antioxidant imbalance in periphery and brain of BTBR T+tf/J mice. Behav Brain Res 2019;364:213–24. 10.1016/j.bbr.2019.02.031 [DOI] [PubMed] [Google Scholar]
- 27.Ferreira-Chamorro P, Redondo A, Riego G, et al. Sulforaphane inhibited the nociceptive responses, anxiety- and depressive-like behaviors associated with neuropathic pain and improved the anti-allodynic effects of morphine in mice. Front Pharmacol 2018;9:1332. 10.3389/fphar.2018.01332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang W, Wei C, Quan M, et al. Sulforaphane reverses the amyloid-β oligomers induced depressive-like behavior. J Alzheimers Dis 2020;78:127–37. 10.3233/JAD-200397 [DOI] [PubMed] [Google Scholar]
- 29.Zimmerman AW, Singh K, Connors SL, et al. Randomized controlled trial of sulforaphane and metabolite discovery in children with autism spectrum disorder. Mol Autism 2021;12:38. 10.1186/s13229-021-00447-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang J-C, Yao W, Dong C, et al. Keap1-Nrf2 signaling pathway confers resilience versus susceptibility to inescapable electric stress. Eur Arch Psychiatry Clin Neurosci 2018;268:865–70. 10.1007/s00406-017-0848-0 [DOI] [PubMed] [Google Scholar]
- 31.Li S, Yang C, Fang X, et al. Role of Keap1-Nrf2 signaling in anhedonia symptoms in a rat model of chronic neuropathic pain: improvement with sulforaphane. Front Pharmacol 2018;9:887. 10.3389/fphar.2018.00887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saha S, Buttari B, Panieri E, et al. An overview of Nrf2 signaling pathway and its role in inflammation. Molecules 2020;25. 10.3390/molecules25225474. [Epub ahead of print: 23 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Subedi L, Lee JH, Yumnam S, et al. Anti-Inflammatory effect of sulforaphane on LPS-activated microglia potentially through JNK/AP-1/NF-κB inhibition and Nrf2/HO-1 activation. Cells 2019;8. 10.3390/cells8020194. [Epub ahead of print: 22 02 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Heiss E, Herhaus C, Klimo K, et al. Nuclear factor kappa B is a molecular target for sulforaphane-mediated anti-inflammatory mechanisms. J Biol Chem 2001;276:32008–15. 10.1074/jbc.M104794200 [DOI] [PubMed] [Google Scholar]
- 35.Sun J, Nan G. The mitogen-activated protein kinase (MAPK) signaling pathway as a discovery target in stroke. J Mol Neurosci 2016;59:90–8. 10.1007/s12031-016-0717-8 [DOI] [PubMed] [Google Scholar]
- 36.Hernández-Rabaza V, Cabrera-Pastor A, Taoro-González L, et al. Hyperammonemia induces glial activation, neuroinflammation and alters neurotransmitter receptors in hippocampus, impairing spatial learning: reversal by sulforaphane. J Neuroinflammation 2016;13:41. 10.1186/s12974-016-0505-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qin S, Yang C, Huang W, et al. Sulforaphane attenuates microglia-mediated neuronal necroptosis through down-regulation of MAPK/NF-κB signaling pathways in LPS-activated BV-2 microglia. Pharmacol Res 2018;133:218–35. 10.1016/j.phrs.2018.01.014 [DOI] [PubMed] [Google Scholar]
- 38.Zhou Q, Chen B, Wang X, et al. Sulforaphane protects against rotenone-induced neurotoxicity in vivo: involvement of the mTOR, Nrf2, and autophagy pathways. Sci Rep 2016;6:32206. 10.1038/srep32206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee J-H, Jeong J-K, Park S-Y. Sulforaphane-induced autophagy flux prevents prion protein-mediated neurotoxicity through AMPK pathway. Neuroscience 2014;278:31–9. 10.1016/j.neuroscience.2014.07.072 [DOI] [PubMed] [Google Scholar]
- 40.Rossignol DA, Frye RE. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry 2012;17:290–314. 10.1038/mp.2010.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang Y, Luo L, Cai X, et al. Nrf2 inhibits oxaliplatin-induced peripheral neuropathy via protection of mitochondrial function. Free Radic Biol Med 2018;120:13–24. 10.1016/j.freeradbiomed.2018.03.007 [DOI] [PubMed] [Google Scholar]
- 42.Gan N, Wu Y-C, Brunet M, et al. Sulforaphane activates heat shock response and enhances proteasome activity through up-regulation of Hsp27. J Biol Chem 2010;285:35528–36. 10.1074/jbc.M110.152686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang J-chun, Yao W, Dong C, et al. Prophylactic effects of sulforaphane on depression-like behavior and dendritic changes in mice after inflammation. J Nutr Biochem 2017;39:134–44. 10.1016/j.jnutbio.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 44.Yao W, Zhang J-C, Ishima T, et al. Role of Keap1-Nrf2 signaling in depression and dietary intake of glucoraphanin confers stress resilience in mice. Sci Rep 2016;6:30659. 10.1038/srep30659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Christensen DL, Baio J, Van Naarden Braun K, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years--autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ 2016;65:1–23. 10.15585/mmwr.ss6503a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McGuinness G, Kim Y. Sulforaphane treatment for autism spectrum disorder: a systematic review. Excli J 2020;19:892–903. 10.17179/excli2020-2487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singh K, Connors SL, Macklin EA, et al. Sulforaphane treatment of autism spectrum disorder (ASD). Proc Natl Acad Sci U S A 2014;111:15550–5. 10.1073/pnas.1416940111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lynch R, Diggins EL, Connors SL, et al. Sulforaphane from broccoli reduces symptoms of autism: a follow-up case series from a randomized double-blind study. Glob Adv Health Med 2017;6:2164957X17735826. 10.1177/2164957X17735826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bent S, Lawton B, Warren T, et al. Identification of urinary metabolites that correlate with clinical improvements in children with autism treated with sulforaphane from broccoli. Mol Autism 2018;9:35. 10.1186/s13229-018-0218-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Momtazmanesh S, Amirimoghaddam-Yazdi Z, Moghaddam HS, et al. Sulforaphane as an adjunctive treatment for irritability in children with autism spectrum disorder: a randomized, double-blind, placebo-controlled clinical trial. Psychiatry Clin Neurosci 2020;74:398–405. 10.1111/pcn.13016 [DOI] [PubMed] [Google Scholar]
- 51.Ghazizadeh-Hashemi F, Bagheri S, Ashraf-Ganjouei A, et al. Efficacy and safety of sulforaphane for treatment of mild to moderate depression in patients with history of cardiac interventions: a randomized, double-blind, placebo-controlled clinical trial. Psychiatry Clin Neurosci 2021;75:250–5. 10.1111/pcn.13276 [DOI] [PubMed] [Google Scholar]
- 52.Wu C, Chen X, Lai J, et al. The efficacy and safety of sulforaphane as an adjuvant in the treatment of bipolar depressive disorder: study protocol for a randomized, double-blinded, placebo-controlled, parallel-group clinical trial. Medicine 2020;99:e20981. 10.1097/MD.0000000000020981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fei X, Wang S, Zheng X, et al. Global research on cognitive behavioural therapy for schizophrenia from 2000 to 2019: a bibliometric analysis via CiteSpace. Gen Psychiatr 2021;34:e100327. 10.1136/gpsych-2020-100327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shiina A, Kanahara N, Sasaki T, et al. An open study of sulforaphane-rich broccoli sprout extract in patients with schizophrenia. Clin Psychopharmacol Neurosci 2015;13:62–7. 10.9758/cpn.2015.13.1.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dickerson F, Origoni A, Katsafanas E, et al. Randomized controlled trial of an adjunctive sulforaphane nutraceutical in schizophrenia. Schizophr Res 2021;231:142–4. 10.1016/j.schres.2021.03.018 [DOI] [PubMed] [Google Scholar]
- 56.Zeni-Graiff M, Rizzo LB, Mansur RB, et al. Peripheral immuno-inflammatory abnormalities in ultra-high risk of developing psychosis. Schizophr Res 2016;176:191–5. 10.1016/j.schres.2016.06.031 [DOI] [PubMed] [Google Scholar]
- 57.Li Z, Zhang T, Xu L, et al. Decreasing risk of psychosis by sulforaphane study protocol for a randomized, double-blind, placebo-controlled, clinical multi-centre trial. Early Interv Psychiatry 2021;15:585–94. 10.1111/eip.12988 [DOI] [PubMed] [Google Scholar]