Abstract
Background
The Regulatory T cell (Treg) lineage is defined by the transcription factor FOXP3, which controls immune-suppressive gene expression profiles. Tregs are often recruited in high frequencies to the tumor microenvironment where they can suppress antitumor immunity. We hypothesized that pharmacological inhibition of FOXP3 by systemically delivered, unformulated constrained ethyl-modified antisense oligonucleotides could modulate the activity of Tregs and augment antitumor immunity providing therapeutic benefit in cancer models and potentially in man.
Methods
We have identified murine Foxp3 antisense oligonucleotides (ASOs) and clinical candidate human FOXP3 ASO AZD8701. Pharmacology and biological effects of FOXP3 inhibitors on Treg function and antitumor immunity were tested in cultured Tregs and mouse syngeneic tumor models. Experiments were controlled by vehicle and non-targeting control ASO groups as well as by use of multiple independent FOXP3 ASOs. Statistical significance of biological effects was evaluated by one or two-way analysis of variance with multiple comparisons.
Results
AZD8701 demonstrated a dose-dependent knockdown of FOXP3 in primary Tregs, reduction of suppressive function and efficient target downregulation in humanized mice at clinically relevant doses. Surrogate murine FOXP3 ASO, which efficiently downregulated Foxp3 messenger RNA and protein levels in primary Tregs, reduced Treg suppressive function in immune suppression assays in vitro. FOXP3 ASO promoted more than 70% reduction in FOXP3 levels in Tregs in vitro and in vivo, strongly modulated Treg effector molecules (eg, ICOS, CTLA-4, CD25 and 4-1BB), and augmented CD8+ T cell activation and produced antitumor activity in syngeneic tumor models. The combination of FOXP3 ASOs with immune checkpoint blockade further enhanced antitumor efficacy.
Conclusions
Antisense inhibitors of FOXP3 offer a promising novel cancer immunotherapy approach. AZD8701 is being developed clinically as a first-in-class FOXP3 inhibitor for the treatment of cancer currently in Ph1a/b clinical trial (NCT04504669).
Keywords: Immunity, Cellular; Immunotherapy; Therapies, Investigational; Tumor Microenvironment; Lymphocytes, Tumor-Infiltrating
Introduction
Regulatory T cells (Tregs) play critical roles in promoting immunologic self-tolerance and immune homeostasis by suppressing aberrant or excessive immune responses to self-antigens and pathogens.1 2 However, as critical as Tregs are to the maintenance of immune homeostasis, they pose a barrier in mounting an effective host response to tumor cells.3 Consistent with this, intratumoral Tregs may contribute to a poor prognosis in several cancers.4–8 In addition, the suppressive function of Tregs can also dampen the efficacy of several anticancer immunotherapies9–11 suggesting that therapies capable of selectively inhibiting Treg function would be promising additions to the cancer immunotherapy arsenal.
The forkhead-box family transcription factor FOXP3 is the key driver of the gene expression program underlying the immune suppressive function of Tregs.12 13 Mutations to the gene encoding FOXP3 lead to fatal autoimmune disorders in both mice and human patients with immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome, confirming the critical role of this factor in regulating the immunosuppressive properties of Tregs.14 In preclinical tumor models, transient genetic depletion of FOXP3 in Tregs improves effectiveness of therapeutic vaccination against established melanoma tumors suggesting FOXP3 may be a highly attractive target for cancer immunotherapy.15 16 However, transcription factors such as FOXP3 are notoriously difficult to target with conventional therapeutic modalities and are often considered undruggable.
Therapeutic nucleic acid-based approaches, including antisense oligonucleotides (ASOs), offer the potential to yield drugs, based on gene sequence information alone, for targets that have proven to be intractable to alternative drug modalities.17 18 ASOs are short synthetic single-stranded nucleotide polymers that selectively bind to a target RNA through Watson-Crick base pairing and, based on the ASO chemistries employed, can be designed to (i) recruit the cellular enzyme RNase H1 leading to the catalytic destruction of the target RNA, or (ii) alter the processing (eg, splicing) of their RNA targets.18 19 Generation 2.0 ASOs have common chemical and biological properties, are generally safe and well-tolerated in the clinic leading to several recent new drug approvals including Tegsedi, Waylivra and the blockbuster drug Sprinraza, for the treatment of patients with the devastating neurodegenerative disease spinal muscular atrophy.17 19 20
Continued efforts to improve the stability and potency of ASOs have resulted in the discovery of a class of ASOs that employ 2’−4’ constrained ethyl (cEt) residues and exhibit significantly enhanced in vitro and in vivo potency compared with earlier generation ASO molecules.21 22 More recently, these cEt-containing ASOs targeted to previously undruggable tumor cell targets have shown therapeutic promise for the treatment of cancer.22–24
In this work we optimized and characterized ASOs targeting the Treg lineage-defining transcription factor FOXP3 in mouse preclinical models and in human primary Tregs. These studies ultimately support the development of a human FOXP3 inhibitor and selection of AZD8701 as the first-in-class human clinical candidate ASO inhibitor of FOXP3 for the treatment of cancer.
Materials and methods
Additional Materials and Methods can be found in online supplemental materials.
jitc-2021-003892supp001.pdf (5.8MB, pdf)
Mice and in vivo tumor studies
BALB/c mice were purchased from Envigo, Shanghai Lingchang Bio-Technology or Charles River and female C57BL/6 mice were purchased from Charles River or The Jackson Laboratory and housed under specific pathogen-free conditions. All procedures were carried out in accordance with UK home office (local) regulations and with approved institutional guidelines. Studies run at Ionis Pharmaceuticals or CrownBio were performed in accordance with the guidelines established by the internal Institutional Animal Care and Use Committee. Mice were housed under pathogen-free conditions in individually ventilated cages under controlled conditions of temperature (19°C–23°C), humidity (55%±10%), photoperiod (12 hours light/12 hours dark), air exchange with food and water provided ad libitum. All animal manipulations were conducted in a biosafety cabinet maintained under positive pressure. The Ionis Pharmaceuticals facilities have been accredited by Assessment and Accreditation of Laboratory Animal Care.
ID8-VEGF (3–5×106 cells/mouse), A20 (3×105–1×107 cells/mouse), MC-38 (1×107 cells/mouse) tumor cells were implanted subcutaneously (s.c.) in the left flank of syngeneic mice. 4T1 (1×104 cells/mouse) were implanted in mammary fat pads of female BALB/c mice. Twelve days before (MC-38 and 4T1) or 1 day after (A20 and ID8-VEGF) implantation, mice were randomized into groups by body weight and dosed s.c. with FOXP3 ASOs 895310, 895317 or control ASO 792169 in phosphate buffered saline (PBS) or intrapertioneally with anti-programmed cell death 1 (PD-1) (BioXcell, RMP1-14, rat IgG2a) or anti-programmed cell death ligand 1 (PD-L1) (mouse IgG1, clone D265A; AstraZeneca). Tumor volumes were calculated using the following formula based on caliper measurements of length (l) and width (w): volume=(pi/6)×l×w.2
For downstream flow cytometric experiments, cells were liberated from tumors using a mouse tumor dissociation kit and tissue dissociator (Miltenyi) according to the manufacturer’s instructions.
For non-tumor bearing studies, BALB/c female mice were dosed s.c. 2–5 times per week with 20 or 50 mg/kg FOXP3 ASOs 895310, 895317 or control ASO 792169 in PBS for 4–6 weeks. At the end of each week, whole blood (cardiac puncture, under terminal isoflurane anesthesia) and spleens were removed and processed for flow cytometry, the remaining carcass was submerged into 10% buffered formalin and certain tissues were processed for histological analysis.
Humanized mice
Female NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice were implanted with 1×107 human peripheral blood mononuclear cells (PBMC) per mouse (JAX). Seven days post PBMC implantation, humanized mice were s.c. treated with indicated doses of ASOs for four consecutive days. Spleens were harvested 24 hours after the last dose and processed for RNA isolation and flow cytometry analysis.
Human CD4 cells were isolated from splenocytes of humanized PBMC mice by the combination of negative magnetic purification steps using a mouse and human EasySep CD4 T cell purification kits (Stemcell Technologies). Purified human CD4 cells were cultured in ImmunoCult-XT T cell expansion media (Stemcell Technologies) supplemented with 30 ng/mL of human recombinant interleukin (IL)-2 (Stemcell Technologies). CD4 cells were treated ex vivo with oligonucleotides by free uptake in a dose-response study for 72 hours. Cells were activated for 24 hours in the presence of ImmunoCult human CD3/CD28/CD2 T cell activator (Stemcell Technologies). Cells were collected and evaluated for changes in the levels of FOXP3 messenger RNA (mRNA) by RT-qPCR and levels of FOXP3 protein by flow cytometry.
ASOs
All ASOs used in this study were 16 nucleotides in length, connected sequentially by phosphorothioate internucleoside linkages. The three nucleotides at both the 5' and 3' ends are composed of 2’−4’ cEt-modified ribonucleotides, which confer an increased affinity to the target mRNA and increased resistance to exo and endonucleases within the cell.20 The central portion is composed of 10 deoxynucleotides, enabling RNase H1 to recognize and cleave the target mRNA in the ASO:RNA duplex. The sequence of the human FOXP3 lead ASO AZD8701/IONIS-1063734 was GATTTTGACATTCTGC. The sequences of the mouse FOXP3 ASOs used in this study were ION-895310 (ATATGTATAGCTGGTT), ION-895317 (GTAAATATTAGGATGG), ION-895545 (TAGCATGTAGTACAGG) and ION-895562 (TAGTTTTGGGTTGAGG). The simple letters indicate DNA and the italicized/underlined letters indicate cEt-modified RNA bases.
Statistics
Error bars relate to SEM unless indicated in figure legends. Appropriate statistical testing was performed using GraphPad Prism (V.7 or V.8). Statistical significance is indicated as follows: *p≤0.05, **p≤0.01, ***p≤0.001, ****p≤0.0001.
Results
AZD8701 potently reduces FOXP3 expression in vitro and in vivo, reversing human Treg immunosuppressive function in primary cells
To identify the most potent human FOXP3 ASOs approximately 2500 compounds were screened in FOXP3-expressing an anaplastic cell lymphoma line SUPM2 in vitro. Approximately 100 of the most effective FOXP3 ASOs selected from this primary screen were evaluated for potency in dose-response experiments in SUPM2 cells (online supplemental figure 1A), in primary Tregs isolated from humanized mice (online supplemental figure 1B) or human PBMCs (online supplemental figure 1C). The most potent and selective FOXP3 ASOs were further evaluated for activity in vivo versus human Tregs in humanized PBMC mice. Several ASOs produced significant reductions of FOXP3 mRNA and protein in human Tregs in humanized PBMC mice (online supplemental figure 1D). AZD8701 emerged as the best human FOXP3 antisense inhibitor, with robust activity in primary human Tregs in vitro and Tregs in humanized PBMC mice in vivo as well as acceptable tolerability profiles in rodents and non-human primates. Structurally, AZD8701 binds to the intronic site on FOXP3 pre-mRNA which is present in all known FOXP3 RNA isoforms (online supplemental figure 1E).
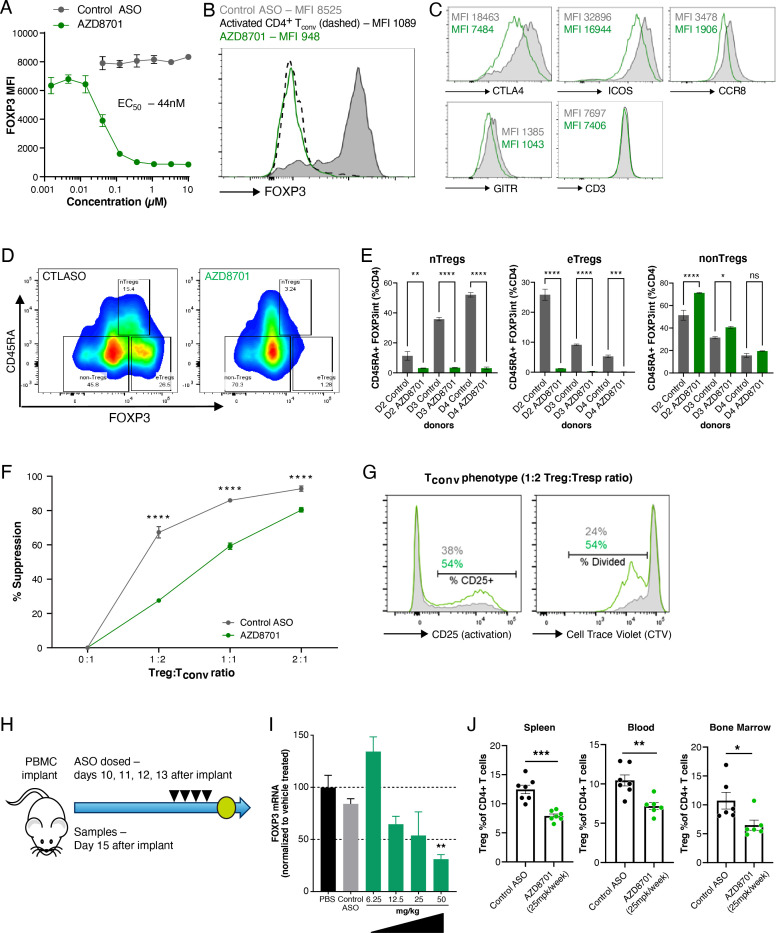
AZD8701 showed potent dose-dependent FOXP3 protein knockdown in primary human Tregs (65.2 nM±6.7 SEM, range 44–78 nM in six donors), and was highly efficacious, with doses >1 µM promoting near-complete extinction of target protein expression (figure 1A, B). AZD8701 downregulated the expression of canonical FOXP3 targets CTLA4, ICOS, GITR and CCR8 at 1 µM dose (figure 1C), and in a dose-dependent manner (online supplemental figure 2A). We evaluated the relationship between FOXP3 knockdown and modulation of downstream pharmacodynamic biomarkers in a range of in vitro Treg samples treated with multiple FOXP3 ASOs at different concentrations. Correlation analysis corroborated the relationship between FOXP3 modulation and CTLA4, ICOS, GITR, CCR8 but not CD3 expression in primary Tregs (online supplemental figure 2B). AZD8701 strongly reduced FOXP3 protein expression in thymic natural Tregs (nTreg) and effector Tregs (eTReg) subsets, defined by CD45RA and FOXP3 expression in PBMCs from healthy donors (figure 1D, E). FOXP3 can be transiently expressed at low levels in conventional T cells but without showing immunosuppressive activity.25 26 Some recent data suggest that FOXP3 expression on CD8 +T cells is an early and tumor-related event that may limit antitumor efficacy.27 We also detected FOXP3 expression in in vitro-stimulated human PBMCs and stimulated CD4+ and CD8+ conventional T cells (online supplemental figure 2C). Furthermore, FOXP3 ASOs with potency similar to AZD8701 modulated a wider 96-gene expression signature of immune-related genes and including canonical FOXP3 target genes (online supplemental figure 3).
Figure 1.
AZD8701 is a highly potent clinical candidate ASO targeting human FOXP3. (A–C) Primary human Tregs were isolated from human PBMCs and cultured with AZD8701 or control ASO in duplicates for a total of 9 days, in the presence of Dynabeads human T-activated CD3/CD28 for the final 2 days of culture. (A) Line graph and (B) histogram show FOXP3 protein abundance in cultured Tregs as measured by flow cytometry. Histogram shows representative data for Tregs cultured with 1 µM ASO. (C) Histograms show the abundance of indicated proteins from a representative treatment with 1 µM AZD8701. (D–E) Contour plot and quantification of FOXP3 knockdown in human PBMC nTRegs and eTRegs with AZD8701 by flow cytometry. Data shown for three healthy donors. (F–G) iTregs were differentiated and cultured in the presence of ASOs in quadruplicates. Data represent ≥3 independent experiments and a total of ≥6 independent donors. (F) Line graph shows ability of iTregs to inhibit proliferation of effector cells in an in vitro suppression assay. (G) Histograms show representative CD25 or CellTrace Violet (CTV) staining on effector cells cultured at a 1:2 iTreg:Teffector ratio. (H) NSG mice were humanized by the infusion of human PBMC and treated systemically for four consecutive days with different AZD8701 doses. (I) FOXP3 messenger RNA expression was quantified by RT-qPCR. N=4 per group. (J) FOXP3 protein levels were quantified by flow cytometry in spleen, blood and bone marrow of humanized mice treated as in (F). N=7 per group. Data in figure is representative of ≥2 independent experiments. Error bars are ±SEM *, p≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.0001 by one-way analysis of variance (ANOVA) with Dunnett’s post-test for E and J and two-way ANOVA with Dunnett’s post-test for F. Differences are calculated relative to control ASO (E, F and J) or saline (I). ASOs, antisense oligonucleotides; eTreg, effector Tregs; iTreg, inducible Tregs; nTreg, natural Tregs; PBS, phosphate buffered saline; Treg, regulatory T cells.
Intratumoral Treg conversion from dominant conventional T cells (Tconv) may have a major impact on the tumor microenvironment (TME). Treg enrichment may result from the expansion of nTreg, but also through the conversion of Tconv into induced Treg (iTreg) under antigen stimulation or tumor-suppressive conditions. Tumor cells can secrete tumor growth factor β (TGF-β) that may directly or indirectly induce naïve T cell conversion to FOXP3+ iTregs.28 AZD8701 reduced human iTreg functions in suppression assays in vitro (figure 1F, G). In vivo, AZD8701 promoted dose-dependent FOXP3 knockdown, an essential parameter for a potential therapeutic agent. When administered to mice engrafted with human PBMCs (humanized mice) (figure 1H), AZD8701 inhibited FOXP3 mRNA (figure 1I) and promoted significant downregulation of FOXP3 protein levels in splenic, blood and bone marrow Tregs (figure 1J). Together, these data show AZD8701 drives dose-dependent modulation of FOXP3 expression, changes in downstream FOXP3-dependent immunosuppressive biomarker expression, reduction of Treg suppressive function ex vivo and FOXP3 knockdown in vivo at clinically achievable doses.
Pharmacological targeting of murine FOXP3 in vivo results in immune activation without promoting overt autoimmunity
To further explore the pharmacology of FOXP3 ASOs, mouse surrogate ASOs with equivalent potency and tolerability to AZD8701 were used to investigate the consequences of modulating Tregs and other immune markers in vitro, and in peripheral tissues and tumors in vivo. We first determined the ability of cEt-modified ASOs to reduce Foxp3 mRNA in primary murine Tregs in vitro. Tregs were expanded in mice in vivo by injection of IL-2-anti-IL-2 antibody complex29 and total Treg-enriched CD4 T cells were purified from spleen and treated with a panel of murine Foxp3 ASOs for 72 hours. FOXP3 ASOs produced robust dose-dependent inhibition of FOXP3 mRNA expression in primary murine Tregs with the most potent ASOs demonstrating IC50 values between 0.1 and 0.2 µM (online supplemental figure 4A, B).
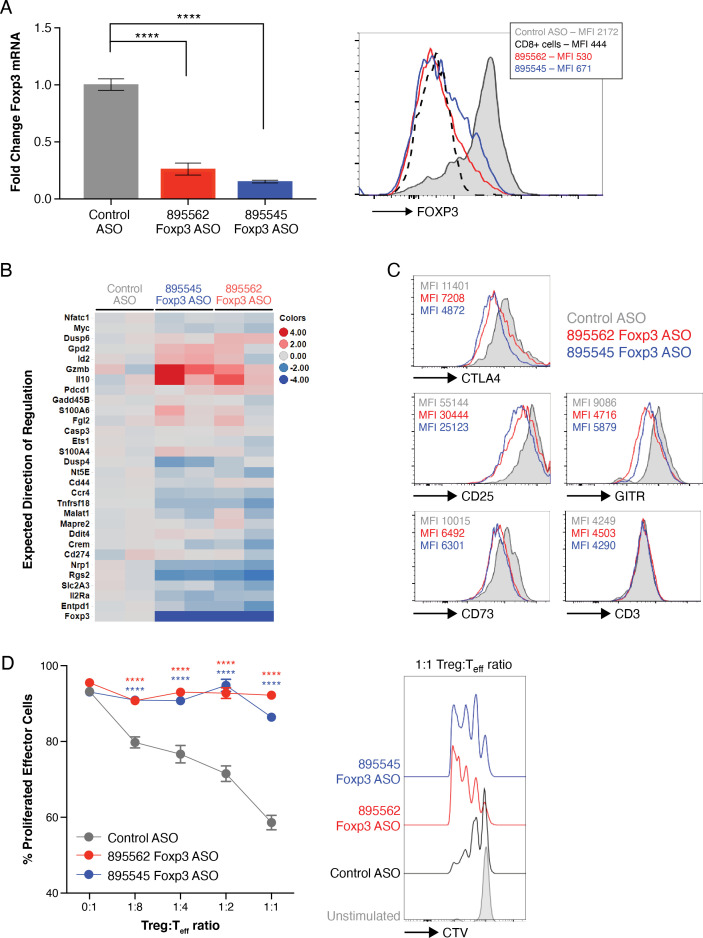
Two mouse FOXP3 ASOs (895562 and 895545) were selected as they effectively downregulated FOXP3 in primary Tregs isolated from spleens of unmanipulated WT mice. Culturing Tregs in the presence of FOXP3 ASOs (5 µM) for 7 days promoted >75% reduction in FOXP3 mRNA and protein (figure 2A). To evaluate whether FOXP3 knockdown also modulated a wider immunosuppressive gene expression profile in murine Treg, we examined a subset of previously characterized Treg signature genes, revealing downregulation of several downstream suppressive genes (figure 2B).30–32 Moreover, protein expression of the canonical FOXP3 targets CTLA4, CD25, GITR and CD73 were also downregulated with FOXP3 ASO treatment (figure 2C). FOXP3 ASOs could also reverse immunosuppressive Treg functions in suppression assays in vitro. iTregs were differentiated from naïve CD4 T cells in the presence of FOXP3 or control ASOs. Naive T cells were then activated with soluble αCD3 and B-cell APCs in the presence of the iTregs. While iTregs cultured in the presence of control ASOs maintained an ability to suppress effector T cell (Teff) proliferation, FOXP3 ASO treatment abrogated iTreg suppressive capability (figure 2D). Consistent with the human FOXP3 ASOs, mouse FOXP3 ASOs can target FOXP3 RNA for degradation, resulting in loss of Treg suppressive phenotypes and functions in vitro.
Figure 2.
Antisense-mediated knockdown of mouse FOXP3 promotes loss of Treg suppressive phenotypic markers and function. (A) Primary Tregs were isolated from mouse spleen and cultured with ASOs (5 µM) in triplicates for 7 days. Bar chart shows relative FOXP3 mRNA expression measured by RT-qPCR, histogram shows FOXP3 protein expression measured by flow cytometry. (B) Inducible Tregs (iTregs) were differentiated and cultured in the presence of ASO for a total of 7 days. Heatmap shows expression of FOXP3-dependent mRNA genes as measured by Fluidigm. (C) Histograms show abundance of indicated proteins in primary Tregs. (D) iTregs were differentiated and cultured in the presence of ASOs and evaluated for their ability to inhibit proliferation of effector cells in an in vitro suppression assay in duplicates. Histograms show representative CellTrace Violet (CTV) staining on effector cells cultured at a 1:1 Treg:Teffector ratio. Data in figure represent ≥2 independent experiments. *, P≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.0001 by one-way analysis of variance (ANOVA) with Dunnett’s post-test for (A) and two-way ANOVA with Dunnett’s post-test for (D). Differences are calculated relative to control ASO. ASOs, antisense oligonucleotides; mRNA, messenger RNA; Tregs, regulatory T cells.
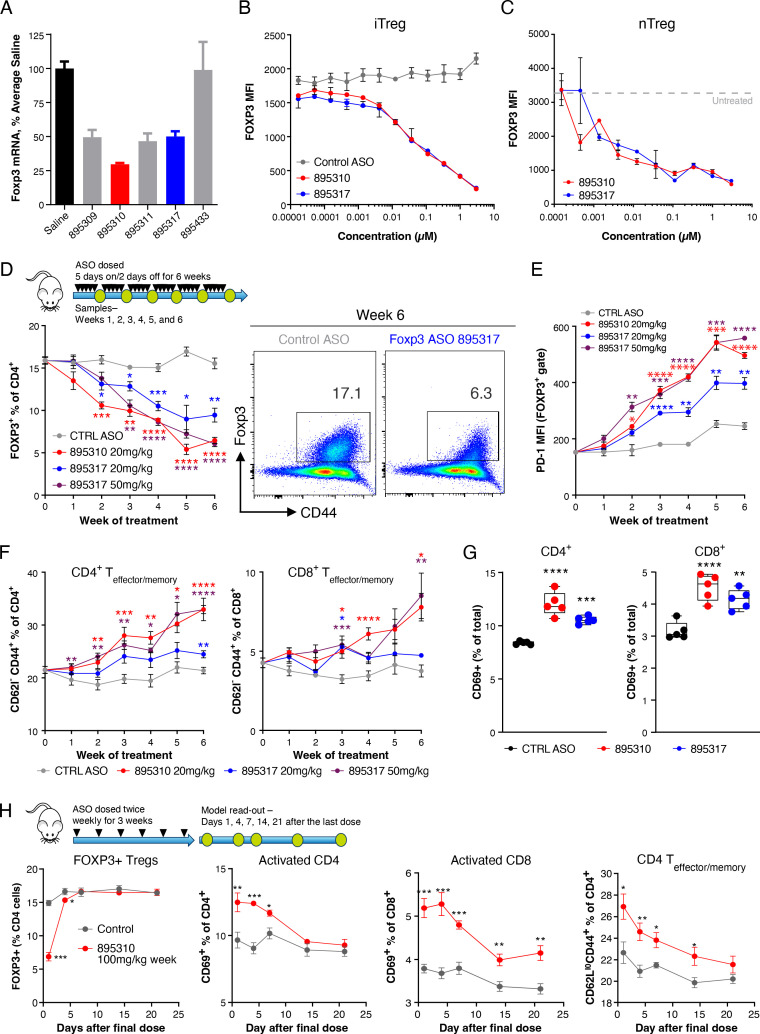
Next, we characterized the pharmacology of murine FOXP3 ASO in Tregs in vivo and the consequences of ASO-mediated FOXP3 inhibition in normal mice. Murine FOXP3 ASOs with optimal in vivo properties, for example, activity and tolerability, were identified from a set of 20 FOXP3 ASOs that produced the best pharmacology in Tregs in vitro (online supplemental figure 4B). Mice were systemically treated with FOXP3 ASOs for 3 weeks. Murine FOXP3 ASOs 895310 and 895317 emerged as the most well-tolerated compounds in vivo and they produced significant Foxp3 mRNA knockdown in preliminary single-dose studies (figure 3A). When benchmarked to previous tool compounds in vitro, 895310 and 895317 were equipotent inhibitors of FOXP3 protein induction in iTregs (figure 3B). Moreover, both compounds were active in primary nTregs, isolated directly from murine spleens (figure 3C).
Figure 3.
Mouse FOXP3 ASOs promote FOXP3 knockdown in vivo, which associates with phenotypes indicative of immunopotentiation. (A) Mice were systemically treated with FOXP3 ASOs for 3 weeks at 100 mg/kg/week dose. CD4 T cells were isolated from spleens and FOXP3 messenger RNA was measured by RT-qPCR. ASOs selected for further in vivo evaluation are highlighted in red and blue. N=4 per group. (B) iTregs were differentiated in the presence of ASO in duplicates for 5 days, and FOXP3 protein abundance was measured by flow cytometry. (C) Primary splenic nTregs were cultured in the presence of indicated ASOs in duplicates for 7 days, and FOXP3 protein abundance was measured by flow cytometry. (D–G) 20 mg/kg and 50 mg/kg FOXP3 ASOs or 50 mg/kg control ASO were administered to BALB/c mice via subcutaneously route 5 days on 2 days off. N=5 per group. (D) The line graph shows the frequency of gated FOXP3+ cells within the splenic CD4+ population. Pseudocolor density plots show representative FOXP3+ gating. (E) Line graph shows programmed cell death 1 protein expression on detectable FOXP3+ cells. (F) Line graphs show the frequency of CD62LloCD44hi T-memory cells within the total CD4+ T-cell population. (G) Scatter bar charts show the frequency of CD69+ cells within the CD4+ or CD8+ populations at the week six time point. (H) ASOs were dosed (100 mg/kg two times per week) for 3 weeks before spleens from cohorts of mice were analyzed by flow cytometry at indicated time points following cessation of treatment. N=5 per group. Data represent two independent experiments. Error bars are SEM data in figure represent ≥2 independent experiments. *, P≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.0001 by one-way analysis of variance (ANOVA) with Dunnett’s post-test for (A and G) and two-way ANOVA with Dunnett’s post-test for (D, E, F and H). Differences are calculated relative to control ASO (D–H) or saline (A). ASOs, antisense oligonucleotides; iTreg, inducible Tregs; nTreg, natural Tregs; Tregs, regulatory T cells.
We next characterized the kinetics of FOXP3 target engagement in vivo. FOXP3 ASOs were formulated in PBS and administered two times per week (BIW) via s.c. injection to WT mice, resulting in a progressive decrease in FOXP3+ Treg cell frequencies in the spleen (figure 3D). Benoist and colleagues recently described mouse models harboring loss-of-function (LoF) mutations in Foxp3, which exhibit elevated expression of the exhaustion/activation biomarker PD-1 in the regulatory T-cell compartment.33 Consistent with this, PD-1 induction on the residual FOXP3+ cells was detected in FOXP3 ASO-treated mice (figure 3E), suggesting a potential loss of Treg suppressive functions conferred by FOXP3 ASOs in vivo. Consistent with this, treated mice also expanded CD4+ and CD8+ lineage cells that were CD62lloCD44hi, resembling Teffector/memory (Tem) cells (figure 3F). The early activation marker CD69 was induced on T-cells following FOXP3 ASO administration, suggesting that enhanced steady-state activation may underlie elevated Tem phenotypes (figure 3G). Importantly, the immune cell differentiation and in particular the immuno-potentiating phenotypes conferred by mouse FOXP3 ASO administration were reversible. WT mice were dosed with FOXP3 ASO for 3 weeks, and FOXP3+ Treg and CD69+/Tem population frequencies were tracked by flow cytometry after cessation of dosing, revealing a return of FOXP3+ Treg population to baseline levels followed by normalization of CD69+/Tem population frequencies within 2 weeks after the last ASO dose (figure 3H).
Genetic or induced ablation of FOXP3 results in profound autoimmune manifestations and rapid death in mice,13 34 while transient/partial Treg depletion is well-tolerated.35 Similarly, partial LoF FOXP3 mutations are associated with minor inflammatory manifestations with a late onset (>35 weeks of age).33 To evaluate whether FOXP3 ASOs promote immune-related phenotypes or toxicities, mice were treated with FOXP3 ASOs for an extended chronic time course.12 13 FOXP3 ASO administration was not associated with clinical signs, nor did we observe body weight reductions over >35 days of treatment (online supplemental figure 5A). While FOXP3 deficient mice and patients are typified by elevated circulating cytokines,13 36 no histopathological findings associated with autoimmunity (online supplemental figure 5B) and negligible cytokine elevation was observed in plasma up to 12 weeks of mouse FOXP3 ASO dosing (online supplemental figure 5C). Moreover, no unexpected inflammatory responses or differential serum antibody production was observed following an acute vaccine challenge in FOXP3 ASO-treated mice (online supplemental figure 5D). Together, these results demonstrate that FOXP3 ASOs can titrate Treg FOXP3 levels to enhance immunopotentiation phenotypes in a reversible manner and are not associated with overt autoimmune/inflammatory manifestations.
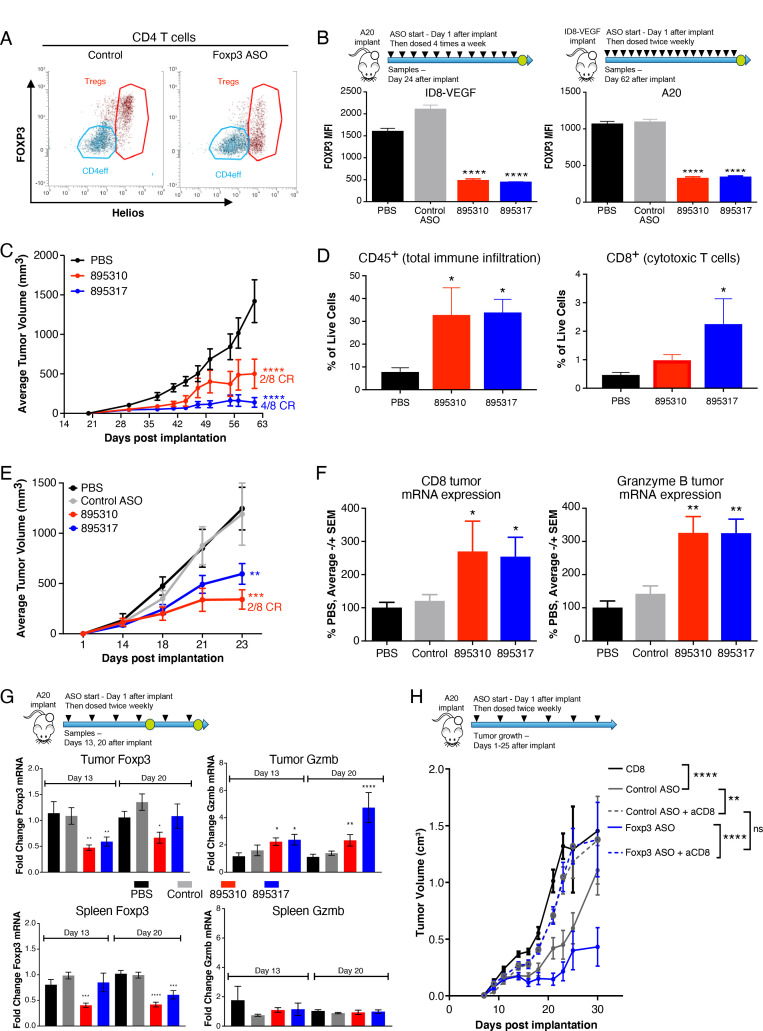
Foxp3 ASOs promote antitumor effects in vivo as a monotherapy or in combination with immune checkpoint blockade
Having established that human and murine FOXP3 ASOs were able to reduce FOXP3 expression in Tregs, decreasing Treg-mediated immunosupression, we hypothesized that FOXP3 ASOs would modulate Treg function in the TME. Mice bearing syngeneic tumors were treated with murine FOXP3 ASOs to reduce FOXP3 expression in intratumoral Tregs and modulate antitumor immunity. By flow cytometry, we confirmed that the majority of the FOXP3+ Tregs in the tumor were positive for a Treg-enriched surrogate marker Helios,37 enabling assessment of the relative change in FOXP3 protein levels in these cells (figure 4A). Following treatment with FOXP3 ASO, the total fraction of Helios+ CD4 T cells was unchanged indicating a non-depleting mechanism. FOXP3 ASO treatment (with both 895310 and 895317) conferred up to 70% reduction in FOXP3 protein—in two different syngeneic models, ID8-VEGF and A20 (figure 4B) after 62 days and 24 days after implantation, respectively. Moreover, the growth of ID8-VEGF and A20 tumors was significantly attenuated in FOXP3 ASO-treated but not control ASO-treated animals with 25%–50% of the animals achieving complete regressions (figure 4C, D, E). FOXP3 ASO treatment resulted in the marked increased recruitment of leukocytes (CD45+) and cytotoxic CD8+ T cells to the tumors in ID8-VEGF (figure 4D) and increased leukocyte cytotoxic marker GzmB in A20 model (figure 4F). Finally, to evaluate the kinetics of FOXP3 ASO-mediated antitumor immunity, we measured changes in inflammatory biomarkers in the A20 model at an early (day 13), and later (day 20) time point (figure 4G). We observed a progressive induction of GzmB expression, which preceded tumor growth inhibition, and was localized to the TME (figure 4G). Depletion of CD8+ T cells in vivo ablated FOXP3 ASO-mediated antitumor immunity (figure 4H). Collectively, these data suggested that inhibition of Treg immunosuppressive function through FOXP3 knockdown led to the enhancement of a highly specific T effector cell-mediated antitumor immune response.
Figure 4.
Single-agent antitumor efficacy mediated by mouse FOXP3 ASOs. (A–F) ID8-VEGF or A20 tumor-bearing mice were systemically treated with FOXP3 ASOs starting at day 1 after implant at 50 mg/kg BIW until day 62 (ID8-VEGF) or four times per week until day 24 (A20). N=8 per group. (A) Tumors were dissociated and tumor-infiltrating Tregs were analyzed by flow cytometry. Helios +CD4 Tregs are shown in red. (B) FOXP3 protein expression was measured in Helios +CD4 Tregs. Line graphs show (C) ID8-VEGF and (E) A20 tumor volumes. The number of complete responses (CR) vs total number of animals in the group is indicated next to lines. (D) ID8-VEGF tumors were dissociated, and abundance of total tumor-infiltrating leukocytes (CD45 +cells) and CTL (CD8 +T cells) were analyzed by flow cytometry. (F) Total RNA from A20 tumors was analyzed for the mRNA expression of CTL marker CD8 and immune cell activation marker GzmB. (G) A20 tumor-bearing mice were treated with indicated ASO or vehicle control 50 mg/kg BIW and tumors analyzed by flow cytometry at day 13 or day 20 time points. N=10 per group. Bar charts show tumor or spleen Foxp3 and GzmB expression measured by RT-qPCR. (H) CD8+ T cells were depleted in vivo with an αCD8 blocking antibody in A20 tumor-bearing mice that were treated with indicated ASO or control at 50 mg/kg BIW. N=12 per group. Data represent >4 independent experiments in (A–F), two independent experiments in (G) and a single cell depletion experiments in (H). *, P≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.000 by one-way analysis of variance (ANOVA) with Dunnett’s post-test for (B, D, F and G) and two-way ANOVA with Dunnett’s post-test for (C, E and H). Differences are calculated relative to PBS (B–G) or as indicated on the panel (H). ASOs, antisense oligonucleotides; BIW, two times per week; mRNA, messenger RNA; PBS, phosphate buffered saline; VEGF, vascular endothelial growth factor.
Given the striking observations that mouse FOXP3 ASOs promote antitumor immunity and efficacy, we next evaluated the monotherapy efficacy of the FOXP3 ASOs in the A20 model with a dose-response to define a minimally efficacious dose in that preclinical model. We observed evidence for dose-dependent efficacy (online supplemental figure 6A) and FOXP3 knockdown in both tumors and spleen with coincident increase in CD4 effector T cell activation (online supplemental figure 6B, C). These data suggested that even relatively low doses of FOXP3 ASOs producing modest FOXP3 inhibition are sufficient to modify the TME and immune activation state to confer antitumor benefit in mice.
Next, we investigated the characteristics that may typify a FOXP3 ASO-sensitive tumor. The FOXP3 ASO sensitive ID8-VEGF and A20 tumors have a high accumulation of FOXP3+ Tregs in the TME as sensitive models.38 39 In contrast, models with low FOXP3+ Treg infiltrate in the TME (eg, 4T1 and MC-38) showed low sensitivity to FOXP3 inhibition (online supplemental figure 7). Despite the limited number of available models, the data support the hypothesis that FOXP3 positivity may predict which tumors have a greater likelihood of response to FOXP3 ASO administration.
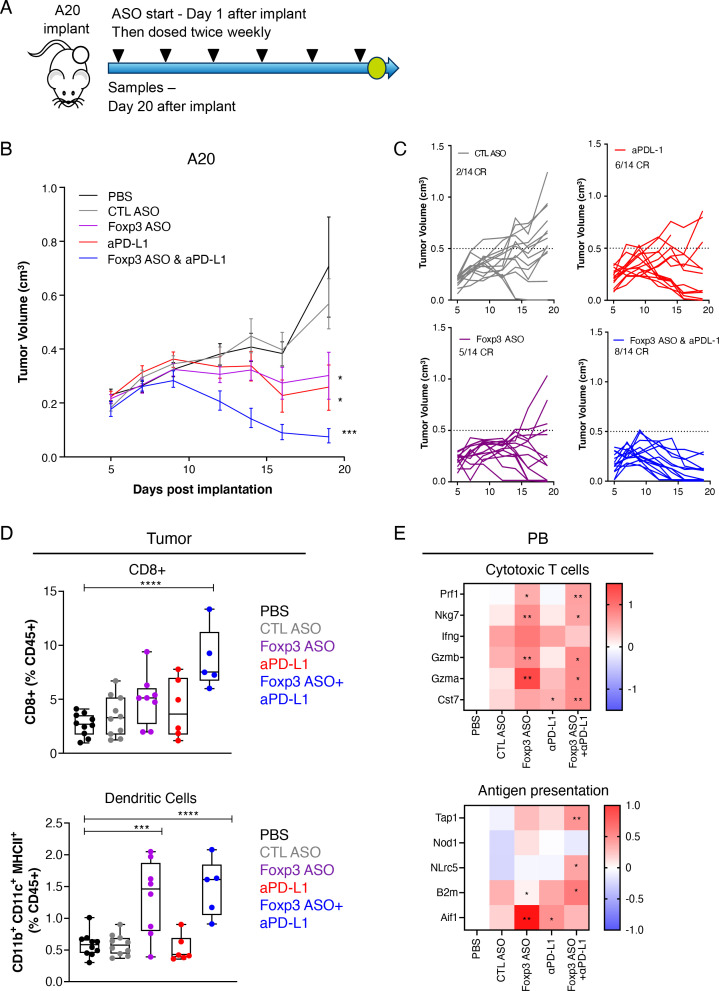
Treg cells have been suggested to play a role in innate or acquired resistance to immunotherapy, and limit checkpoint inhibitor efficacy.10 11 In the A20 tumor model combination of mouse FOXP3 ASO with αPD-L1 significantly decreased tumor growth (figure 5A, B) and increased complete response (CR) rate compared with control groups and monotherapies (figure 5C). The combination promoted an increased infiltration of CD8+ T cells assessed by flow cytometry, and significant increase in dendritic cells in the TME in the FOXP3 ASO—treated arms (figure 5D). The changes in immune activation following treatment were systemic, with peripheral blood from treated mice exhibiting a significant increase in cytotoxic T cell and antigen presentation gene expression signatures (figure 5E).
Figure 5.
FOXP3 ASOs promote antitumor efficacy when combined with αPD-L1 immune checkpoint blockade. (A) Mice were treated with mouse FOXP3 ASO (895317) (50 mg/kg BIW) and αPD-L1 (10 mg/kg BIW) alone or in combination from day 1 post A20 tumor-implantation and dosed two times per week for the duration of the experiment. N=14 per group. (B) Mean tumor and (C) individual tumor volumes and indicated number of complete responses (CR). (D-E) Tumor samples and peripheral blood (PB) were analyzed at day 20 by flow cytometry and RNA levels, respectively. (D) Frequency of CD8 +T cells and dendritic cells in tumor and (E) cytotoxic T cell and antigen-presenting cell gene markers in PB. *, P≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.0001 by one-way analysis of variance (ANOVA) with Dunnett’s post-test for (D and E) and two-way ANOVA with Dunnett’s post-test for (B). Differences are calculated relative to PBS. ASOs, antisense oligonucleotides; BIW, two times per week; PBS, phosphate buffered saline; PD-1, programmed cell death 1; PD-L1, programmed cell death ligand 1.
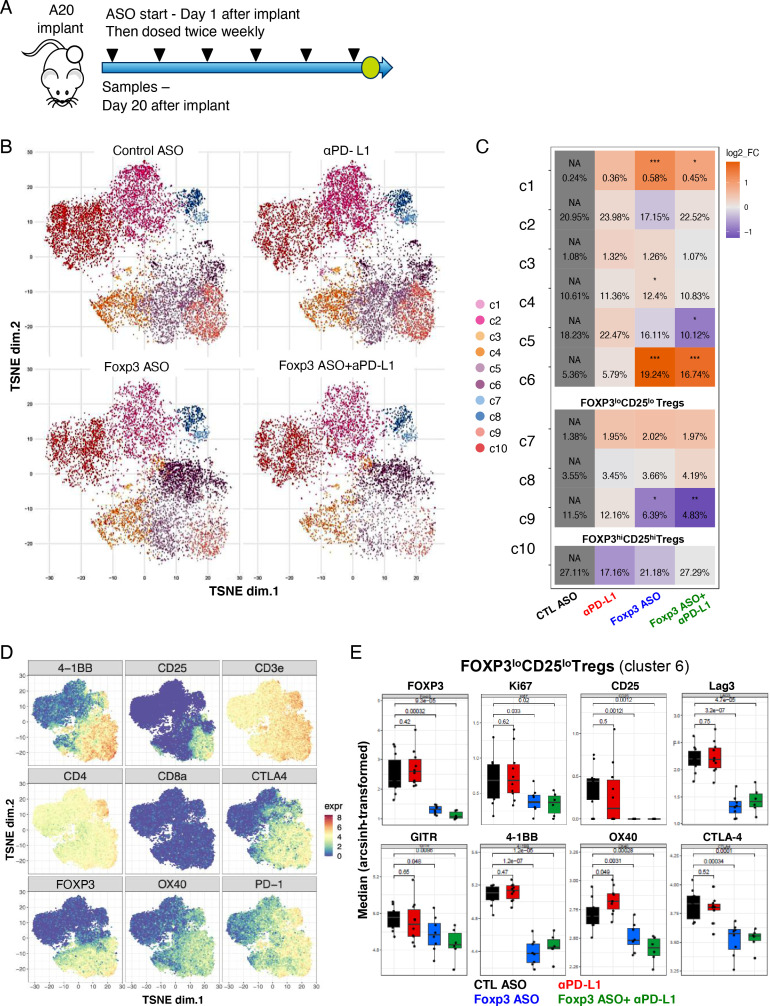
To gain greater insight into the broader effects of reducing FOXP3 expression on CD4 +T cells we performed a detailed analysis of the effects of FOXP3 ASO monotherapy and combination with αPD-L1 on CD4+ T cells in the TME by mass cytometry. Mice were treated with FOXP3 ASO and/or αPD-L1, and tumors collected for immunoprofiling at day 20 of treatment (figure 6A), time point preceding tumor regression when we had previously identified enhanced immune activation (figure 4G). T-distributed stochastic neighbor embedding (t-SNE) clustering showed significant changes in frequencies of different tumor CD4+ T cell populations (figure 6B) with a significant decrease in FOXP3hiCD25hi Tregs from 11.5% to 6.3% in the FOXP3 ASO group and 4.8% in the combination groups. The FOXP3loCD25lo Treg fraction was significantly increased from 5.3% to 19.2% and 16.7% in the FOXP3 ASO and combination groups, respectively (figure 6C). Phenotypically, FOXP3loCD25lo Tregs showed significantly less Ki67 expression and lower expression of Treg effector molecules such as GITR, LAG3, 4-1BB, CD25, OX40 and CTLA-4, which were driven primarily by the FOXP3 ASO and not αPD-L1 treatments (figure 6D, E). Taken together, these data support the mechanism of action of FOXP3 ASO in reprogramming Tregs into a low suppressive state in the TME, allowing us to dissect a discrete and complementary mechanism of action to αPD-L1 treatment.
Figure 6.
FOXP3 ASOs reprogram Treg effector cell phenotype in vivo in combination with αPD-L1 immune checkpoint blockade. (A) Mice were treated with ASO (50 mg/kg BIW) and αPD-L1 (10 mg/kg BIW) alone or in combination from day 1 post A20 tumor-implantation. N=14 per group. Tumors were analyzed by mass cytometry at day 20 after implantation. (B) t-SNE analysis of tumor-infiltrating CD4+ T cells. (C) Relative changes of CD4 +T cell clusters compared with control group. (D) Expression map of T cells and Tregs markers. (E) Quantification of Treg activation expression markers. Error bars are SD *, p≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.0001 by one-way analysis of variance with Dunnett’s post-test relative to control ASO. ASOs, antisense oligonucleotides; BIW, two times per week; t-SNE, t-distributed stochastic neighbor embedding; PD-L1, programmed cell death ligand 1; Treg, Regulatory T cells.
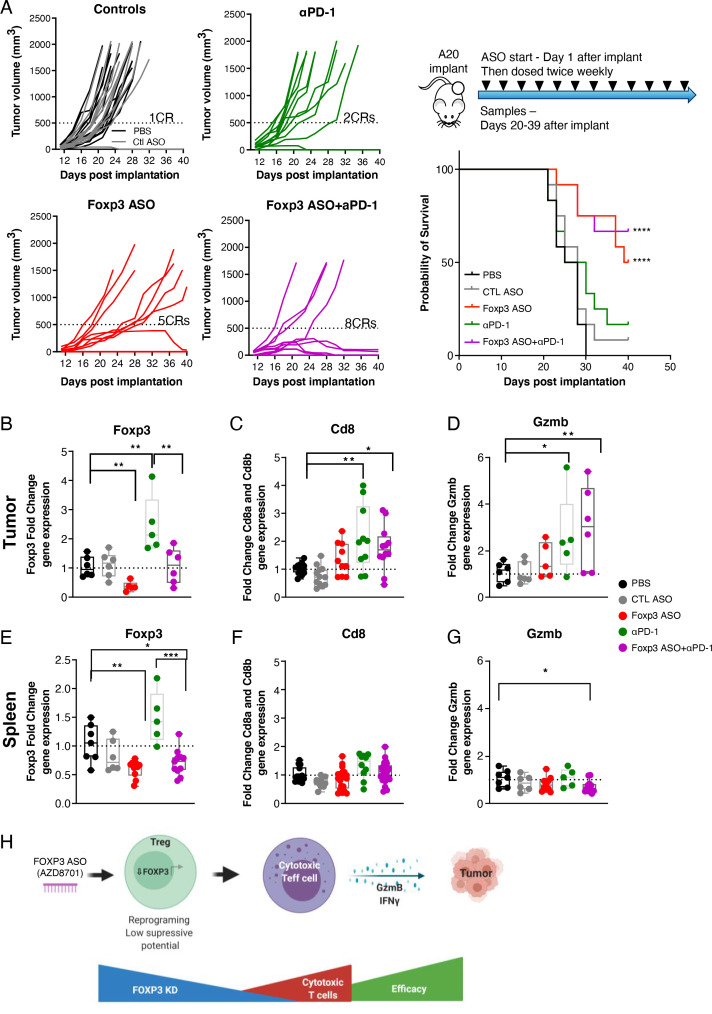
PD-1 blockade monotherapy could lead to the skewing of the Teff/Treg balance in favor of Treg-mediated immunosuppression, limiting the response to immunotherapy.40 41 Therefore, we extended our work to evaluate mouse FOXP3 ASO efficacy in combination with αPD-1 immune checkpoint blocking antibodies in the A20 tumor model. FOXP3 ASOs promoted significant tumor growth inhibition, with CRs observed in a monotherapy arm, and increased the number of CR/near CR mice in combination with αPD-1 (figure 7A). In A20 tumor-bearing mice, αPD-1 immune checkpoint administration increased Foxp3 mRNA expression in tumors and spleens, which could be reduced by FOXP3 ASO coadministration (figure 7B, E). Foxp3 knockdown in the tumor was followed by increased CD8 T cell infiltration (figure 7C) and Gzmb expression (figure 7D). These markers of cytotoxic activity were not observed in spleens (figure 7F, G), supporting previously observed non-systemic T cell activation. Thus, Tregs may represent a non-redundant or non-overlapping immunosuppressive mechanism in tumors that may complement immune checkpoint therapies. When taken together, these data represent a preclinical proof-of-concept that cEt-modified ASOs can efficiently target FOXP3 expression in Tregs, reduce their immunosuppressive phenotype in vivo, and promote antitumor immunity (figure 7H). This mechanism is novel, as it is not cytodepletive, and can be modulated both by dose and kinetics to dynamically regulate the reversal of Treg suppressive function.
Figure 7.
FOXP3 ASOs promote additive efficacy when combined with αPD-1 immune checkpoint blockade. Mice were treated with ASO 895310 (50 mg/kg BIW) and αPD-1 (10 mg/kg BIW) alone or in combination from day 1 post A20 tumor-implantation. ASO was dosed for the duration of the study. αPD-1 was dosed six times. N=12 per group. Mice were sacrificed when tumors exceeded 1500 mm3 or after 40 days. (A) Spider plots indicate tumor volumes. Survival panel shows percent surviving mice vs time. (B–G) Foxp3, CD8a/CD8b and Granzyme messenger RNA expression in tumors and spleens from terminal samples. (H) Model of ASO targeting of FOXP3 expression to reduce Treg immunosuppressive capacity and promote antitumor immunity. Data in figure represent two independent experiments. CR, complete responses. Error bars are ±SEM *, p≤0.05; **, p≤0.01; ***, p≤0.001; ****, p≤0.0001 by one-way analysis of variance with Dunnett’s post-test relative to PBS group. Survival analysis (A) was done by log-rank Mantel-Cox test. ASOs, antisense oligonucleotides; BIW, two times per week; IFN, interferon; PBS, phosphate buffered saline; PD-1, programmed cell death 1.
Discussion
Even in cases where the molecular pathogenesis underlying disease states is well defined, the discovery of effective therapeutic treatments often remains unrealized. In part, this reflects the fact that only approximately 20% of all human genes are thought to be members of what are considered ‘druggable’ protein families.42 Thus, there is a tremendous need to develop technologies to expand the druggable fraction of the genome to treat disease more effectively.
In this study, we demonstrate that antisense technology, and in particular cEt chemistry ASOs, can be effectively deployed to target difficult-to-drug proteins in immune cells including Tregs. Tregs have been long associated with immunosuppression in the TME and the clear association between FOXP3 and Treg immunosuppressive activity provided a known yet previously undruggable target for ASO technology. We have shown that treatment with murine FOXP3 ASOs resulted in monotherapeutic antitumor activity and combination benefit with either αPD-1 or αPD-L1 checkpoint blockade. Profiling of FOXP3 ASO efficacy across a range of discrete tumor models revealed that antitumor efficacy was linked to a high Treg infiltration within the TME, and consequently it may be interesting to investigate whether there is an association between FOXP3 levels and clinical activity for such agents.
The discovery of the human FOXP3 ASO inhibitor AZD8701 opens a novel opportunity to selectively target Treg immunosuppressive function. Several drugs possessing a Treg-depletion mechanism of action have entered early phase clinical development, such as CD25, CTLA-4, CCR4, OX40, ICOS or GITR, but proof of concept has not been established for a specific Treg-targeting agent.43 One major hurdle for these agents is the precision with which Treg depletion can be demonstrably achieved versus off-target depletion.43 FOXP3 ASOs have the potential to be more selective vs other immune cell types, and thus may offer significant advantages over other Treg-targeting mechanisms and modalities. Antibody-dependent cellular cytotoxicity (ADCC)-dependent Treg depleting antibodies such as αCTLA4 or αCD25 have shown preclinical efficacy in tumor models,44 45 but they also deplete subsets of activated effector cells which express CTLA4 and/or CD25.11 46 Moreover, depletion relies on cellular clearance by cell populations bearing relevant Fc receptors, which broadly encompass myeloid and/or natural killer (NK) cells.47 Therefore, the utility of Treg depleting antibodies is limited to TMEs harboring both regulatory T-cell and Fc receptor-bearing innate cells. Furthermore, the clinical utility of such approaches could be limited by toxicities related to non-Treg targeting.48 While additional antibody targets beyond CTLA4 have been proposed to exhibit a mechanism of action based on Treg depletion,49 to our knowledge these molecules have not progressed beyond early clinical proof-of-concept studies in cancer. GITR and OX40 agonist antibodies tested in Ph1 clinical trials depleted tumor Tregs, however, these antibodies only target a subpopulation of tumor Tregs.50 Interestingly, apoptotic Tregs can generate a highly immunosuppressive microenvironment by releasing ATP which is then converted to immunosuppressive adenosine,51 highlighting another caveat of a Treg cell depletion approach. An alternative approach involves targeting Tregs with small molecules, of which several Treg-targeting approaches have been proposed but remain to be tested clinically.52 Deconvoluting Treg-dependent versus independent effects remains a challenge for many of these targets. There is a potential utility of PI3Kδ small molecule inhibitors to selectively reduce intratumoral Treg frequencies in solid tumors,53 however more recent studies have identified additional direct effects of PI3Kδ inhibition on non-Treg populations.54 Recently, new drugs targeting the IL-2 pathway have entered clinical trials aiming to deplete Tregs more selectively55 and results from these studies will be key to address whether selectively targeting Tregs either by depletion or reprograming benefits patients.
Several developmental challenges and biological uncertainties remain around Treg biology. Mice do not faithfully model the toxicities observed with immune-based cancer therapeutics in the clinic, and any clinical application would necessitate a careful evaluation of the therapeutic index. Moreover, while highly activated Tregs have been described in clinical biopsies,7 56 and overall Tregs have been associated with negative patient outcomes across multiple indications, the presence of Tregs has also been linked to positive patient outcomes in some settings.57 FOXP3+ Tregs were associated with improved survival in colorectal, head and neck, and esophageal cancers.4 5 In colorectal cancers, functionally distinct subpopulations of tumor-infiltrating FOXP3+ T cells contribute in opposing ways to determine CRC prognosis and FOXP3 low fraction with a proinflammatory profile showing better overall survival than FOXP3 high.58 Thus, a careful evaluation of clinical opportunities is required to enhance the success of this approach. Nonetheless, provided that a Treg-targeted therapeutic could indeed be safely administered, several exciting clinical opportunities could be explored. Our preclinical data suggest that Treg-targeted therapeutics may be relevant in both monotherapeutic and combination settings (figures 5–7). Several cancers have been characterized by high Treg infiltration,4 including melanoma, non-small-cell lung, gastric and ovarian cancers43 and potentially could respond to FOXP3 ASO monotherapy. FOXP3+ Tregs have also been linked to a lack of response and resistance to PD-1/PD-L1 checkpoint inhibition,40 41 59 and contribution to hyperprogression60 which suggest opportunities for benefit from combination therapy.
Our findings support the use of FOXP3 ASOs as a selective therapeutic approach to target tumor Tregs. Importantly, long-term dosing with FOXP3 ASO showed no signs of overt autoimmunity in immuno-competent mice with quick recovery of FOXP3 knockdown and immune activation. In the assay conditions tested, and preclinical models investigated, we have not observed a switch to either a Th1 or Th17 repolarization of Tregs that lost FOXP3, but alternative model systems such as lineage-tracing mouse models could be explored in the future for a more precise evaluation. We have shown that reducing FOXP3 levels led to reduced iTreg suppressive activity ex vivo, and importantly promoted a reduction of immunosuppressive markers on Tregs and enhanced T cell activation phenotype in tumor models in vivo. There are certain limitations of the iTreg model for example, differences in epigenetic marks, gene expression and stability of immunosuppressive phenotype of iTregs relative to tumor-infiltrating Tregs.61 62 It still remains to be formally demonstrated whether ASO-driven reduction of FOXP3 in tumor Tregs leads to the reduction in their immunosuppressive activity in vivo and whether this is the main mechanism of the antitumor responses in our preclinical models. nTregs and iTregs have specific and overlapping functions in immunosuppressive responses.61 In preliminary work we observed high donor variability in suppressive function of human nTregs isolated from PBMCs with the FOXP3 ASO (data not shown) which did not allow us to conclude reduced suppression. This may be due to differences in Treg subsets such as epigenetic make-up62 or due to these cells being less homogenous than iTregs. Importantly, we showed targeting tumor FOXP3+ Tregs in preclinical tumor models led to antitumor responses. Future studies will be needed to address the exact effects of reducing FOXP3 levels in nTregs and iTregs on Teff cell function as well as the fate of FOXP3-depleted Tregs.63–65
A small subpopulation of human CD4+ and CD8+ T cells was shown to transiently up-regulate FOXP3 on in vitro stimulation for example, T cell receptor (TCR) stimulation.27 Although their functional role is yet to be fully defined, there is no evidence that they become immunosuppressive or suppress Th1 polarization but seem to have a role in limiting antitumor efficacy.27 66–68 We have shown that AZD8701 can suppress FOXP3 expression in all T cell subsets aligned with extensive characterization of ASO uptake and activity in human T cells and in preclinical models.69
Finally, these findings highlight the opportunity to selectively modulate the Treg immuno-suppressive program through inhibition of the previously undruggable transcription factor FOXP3 with AZD8701 and will allow clinical testing of therapeutic hypotheses in patients with cancer with tumors having high Treg infiltration. The combination of FOXP3 inhibition in conjunction with checkpoint blockade has the exciting potential to both broaden and further enhance the clinical impact of these established immuno-oncology therapeutics. Clinical studies with AZD8701 are currently ongoing in patients with advanced solid tumors (NCT04504669).
Acknowledgments
The authors would like to thank Tracy Reigle and Raul Alonzo for assistance with figures and manuscript preparation. Schematic figure created using Biorender.com.
Footnotes
AR, LSC and CS contributed equally.
Contributors: Conceptualization: AR, LSC, CS, FWG, ARM. Flow and mass cytometry analysis: AR, CS, JW, AMH, LSC, LM, MS, GK, MK. Performed in vitro assays: AR, CS, BJ, AS, DG, AW, LI, DAM. Performed in vivo studies: BJ, LH, AP, MT, MM, MC. Transcriptional analysis: BJ, LH, MAT. IHC and histopathology: MC, SK, VS. Writing manuscript: AR, LSC, CS, FWG, ARM. Resources and conceptual: STB, PL, ME, SF. Guarantors: AR, LSC, CS, FWG, ARM. Manuscript review and approval: All authors.
Funding: AstraZeneca has a governance framework and processes in place to ensure that commercial sources have appropriate patient consent and ethical approval in place for collection of the samples for research purposes including use by for-profit companies. This report is an independent research, NHS Blood & Transplant have provided material in support of the research. The views expressed in this publication are those of the author(s) and not necessarily those of NHS Blood & Transplant. The AstraZeneca Biobank in the UK is licensed by the Human Tissue Authority (License No. 12109) and has National Research Ethics Service Committee (NREC) Approval as a Research Tissue Bank (RTB) (REC No 17/NW/0207) which covers the use of the samples for this project.
Competing interests: The authors are paid employees of AstraZeneca or Ionis Pharmaceuticals, as indicated by their affiliations.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Sakaguchi S, Yamaguchi T, Nomura T, et al. Regulatory T cells and immune tolerance. Cell 2008;133:775–87. 10.1016/j.cell.2008.05.009 [DOI] [PubMed] [Google Scholar]
- 2.Josefowicz SZ, Lu L-F, Rudensky AY. Regulatory T cells: mechanisms of differentiation and function. Annu Rev Immunol 2012;30:531–64. 10.1146/annurev.immunol.25.022106.141623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whiteside TL. What are regulatory T cells (Treg) regulating in cancer and why? Semin Cancer Biol 2012;22:327–34. 10.1016/j.semcancer.2012.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shang B, Liu Y, Jiang S-juan, et al. Prognostic value of tumor-infiltrating FoxP3+ regulatory T cells in cancers: a systematic review and meta-analysis. Sci Rep 2015;5:15179. 10.1038/srep15179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salama P, Phillips M, Grieu F, et al. Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol 2009;27:186–92. 10.1200/JCO.2008.18.7229 [DOI] [PubMed] [Google Scholar]
- 6.Preston CC, Maurer MJ, Oberg AL, et al. The ratios of CD8+ T cells to CD4+CD25+ FOXP3+ and FOXP3- T cells correlate with poor clinical outcome in human serous ovarian cancer. PLoS One 2013;8:e80063. 10.1371/journal.pone.0080063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Plitas G, Konopacki C, Wu K, et al. Regulatory T cells exhibit distinct features in human breast cancer. Immunity 2016;45:1122–34. 10.1016/j.immuni.2016.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beyer M, Schultze JL. Regulatory T cells in cancer. Blood 2006;108:804–11. 10.1182/blood-2006-02-002774 [DOI] [PubMed] [Google Scholar]
- 9.Shitara K, Nishikawa H. Regulatory T cells: a potential target in cancer immunotherapy. Ann N Y Acad Sci 2018;1417:104–15. 10.1111/nyas.13625 [DOI] [PubMed] [Google Scholar]
- 10.Owen DL, Mahmud SA, Sjaastad LE, et al. Thymic regulatory T cells arise via two distinct developmental programs. Nat Immunol 2019;20:195–205. 10.1038/s41590-018-0289-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma A, Subudhi SK, Blando J, et al. Anti-CTLA-4 Immunotherapy Does Not Deplete FOXP3+ Regulatory T Cells (Tregs) in Human Cancers-Response. Clin Cancer Res 2019;25:3469–70. 10.1158/1078-0432.CCR-19-0402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science 2003;299:1057–61. 10.1126/science.1079490 [DOI] [PubMed] [Google Scholar]
- 13.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol 2003;4:330–6. 10.1038/ni904 [DOI] [PubMed] [Google Scholar]
- 14.Bennett CL, Christie J, Ramsdell F, et al. The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat Genet 2001;27:20–1. 10.1038/83713 [DOI] [PubMed] [Google Scholar]
- 15.Klages K, Mayer CT, Lahl K, et al. Selective depletion of Foxp3+ regulatory T cells improves effective therapeutic vaccination against established melanoma. Cancer Res 2010;70:7788–99. 10.1158/0008-5472.CAN-10-1736 [DOI] [PubMed] [Google Scholar]
- 16.Bos PD, Plitas G, Rudra D, et al. Transient regulatory T cell ablation deters oncogene-driven breast cancer and enhances radiotherapy. J Exp Med 2013;210:2435–66. 10.1084/jem.20130762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crooke ST, Witztum JL, Bennett CF, et al. RNA-Targeted therapeutics. Cell Metab 2018;27:714–39. 10.1016/j.cmet.2018.03.004 [DOI] [PubMed] [Google Scholar]
- 18.Bennett CF, Baker BF, Pham N, et al. Pharmacology of antisense drugs. Annu Rev Pharmacol Toxicol 2017;57:81–105. 10.1146/annurev-pharmtox-010716-104846 [DOI] [PubMed] [Google Scholar]
- 19.Crooke ST. Molecular mechanisms of antisense oligonucleotides. Nucleic Acid Ther 2017;27:70–7. 10.1089/nat.2016.0656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seth PP, Siwkowski A, Allerson CR, et al. Short antisense oligonucleotides with novel 2'-4' conformationaly restricted nucleoside analogues show improved potency without increased toxicity in animals. J Med Chem 2009;52:10–13. 10.1021/jm801294h [DOI] [PubMed] [Google Scholar]
- 21.Murray S, Ittig D, Koller E, et al. TricycloDNA-modified oligo-2'-deoxyribonucleotides reduce scavenger receptor B1 mRNA in hepatic and extra-hepatic tissues--a comparative study of oligonucleotide length, design and chemistry. Nucleic Acids Res 2012;40:6135–43. 10.1093/nar/gks273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hong D, Kurzrock R, Kim Y, et al. AZD9150, a next-generation antisense oligonucleotide inhibitor of STAT3 with early evidence of clinical activity in lymphoma and lung cancer. Sci Transl Med 2015;7:ra185. 10.1126/scitranslmed.aac5272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reilley MJ, McCoon P, Cook C, et al. STAT3 antisense oligonucleotide AZD9150 in a subset of patients with heavily pretreated lymphoma: results of a phase 1b trial. J Immunother Cancer 2018;6:119. 10.1186/s40425-018-0436-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chowdhury S, Burris HA, Patel M, et al. A phase I dose escalation, safety and pharmacokinetic (PK) study of AZD5312 (IONIS-ARRx), a first-in-class generation 2.5 antisense oligonucleotide targeting the androgen receptor (AR). Eur J Cancer 2016;69:S145. 10.1016/S0959-8049(16)33031-3 [DOI] [Google Scholar]
- 25.Allan SE, Crome SQ, Crellin NK, et al. Activation-induced FOXP3 in human T effector cells does not suppress proliferation or cytokine production. Int Immunol 2007;19:345–54. 10.1093/intimm/dxm014 [DOI] [PubMed] [Google Scholar]
- 26.Wang J, Ioan-Facsinay A, van der Voort EIH, et al. Transient expression of FOXP3 in human activated nonregulatory CD4+ T cells. Eur J Immunol 2007;37:129–38. 10.1002/eji.200636435 [DOI] [PubMed] [Google Scholar]
- 27.Lozano T, Conde E, Martín-Otal C, et al. TCR-induced FOXP3 expression by CD8+ T cells impairs their anti-tumor activity. Cancer Lett 2022;528:45–58. 10.1016/j.canlet.2021.12.030 [DOI] [PubMed] [Google Scholar]
- 28.Curotto de Lafaille MA, Lafaille JJ, Lafaille Cde. Natural and adaptive foxp3+ regulatory T cells: more of the same or a division of labor? Immunity 2009;30:626–35. 10.1016/j.immuni.2009.05.002 [DOI] [PubMed] [Google Scholar]
- 29.Webster KE, Walters S, Kohler RE, et al. In vivo expansion of T reg cells with IL-2-mAb complexes: induction of resistance to EAE and long-term acceptance of islet allografts without immunosuppression. J Exp Med 2009;206:751–60. 10.1084/jem.20082824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marson A, Kretschmer K, Frampton GM, et al. Foxp3 occupancy and regulation of key target genes during T-cell stimulation. Nature 2007;445:931–5. 10.1038/nature05478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zheng L, Sharma R, Gaskin F, et al. A novel role of IL-2 in organ-specific autoimmune inflammation beyond regulatory T cell checkpoint: both IL-2 knockout and Fas mutation prolong lifespan of Scurfy mice but by different mechanisms. J Immunol 2007;179:8035–41. 10.4049/jimmunol.179.12.8035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gavin MA, Rasmussen JP, Fontenot JD, et al. Foxp3-dependent programme of regulatory T-cell differentiation. Nature 2007;445:771–5. 10.1038/nature05543 [DOI] [PubMed] [Google Scholar]
- 33.Kwon H-K, Chen H-M, Mathis D, et al. FoxP3 scanning mutagenesis reveals functional variegation and mild mutations with atypical autoimmune phenotypes. Proc Natl Acad Sci U S A 2018;115:E253–62. 10.1073/pnas.1718599115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams LM, Rudensky AY. Maintenance of the Foxp3-dependent developmental program in mature regulatory T cells requires continued expression of Foxp3. Nat Immunol 2007;8:277–84. 10.1038/ni1437 [DOI] [PubMed] [Google Scholar]
- 35.Mayer CT, Ghorbani P, Kühl AA, et al. Few Foxp3⁺ regulatory T cells are sufficient to protect adult mice from lethal autoimmunity. Eur J Immunol 2014;44:2990–3002. 10.1002/eji.201344315 [DOI] [PubMed] [Google Scholar]
- 36.Barzaghi F, Passerini L, Gambineri E, et al. Demethylation analysis of the FOXP3 locus shows quantitative defects of regulatory T cells in IPEX-like syndrome. J Autoimmun 2012;38:49–58. 10.1016/j.jaut.2011.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elkord E, Al-Ramadi BK. Helios expression in FoxP3(+) T regulatory cells. Expert Opin Biol Ther 2012;12:1423–5. 10.1517/14712598.2012.711310 [DOI] [PubMed] [Google Scholar]
- 38.Mosely SIS, Prime JE, Sainson RCA, et al. Rational selection of syngeneic preclinical tumor models for immunotherapeutic drug discovery. Cancer Immunol Res 2017;5:29–41. 10.1158/2326-6066.CIR-16-0114 [DOI] [PubMed] [Google Scholar]
- 39.Taylor MA, Hughes AM, Walton J, et al. Longitudinal immune characterization of syngeneic tumor models to enable model selection for immune oncology drug discovery. J Immunother Cancer 2019;7:328. 10.1186/s40425-019-0794-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dodagatta-Marri E, Meyer DS, Reeves MQ, et al. α-PD-1 therapy elevates Treg/Th balance and increases tumor cell pSmad3 that are both targeted by α-TGFβ antibody to promote durable rejection and immunity in squamous cell carcinomas. J Immunother Cancer 2019;7:62. 10.1186/s40425-018-0493-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kumagai S, Togashi Y, Kamada T, et al. The PD-1 expression balance between effector and regulatory T cells predicts the clinical efficacy of PD-1 blockade therapies. Nat Immunol 2020;21:1346–58. 10.1038/s41590-020-0769-3 [DOI] [PubMed] [Google Scholar]
- 42.Finan C, Gaulton A, Kruger FA, et al. The druggable genome and support for target identification and validation in drug development. Sci Transl Med 2017;9. 10.1126/scitranslmed.aag1166. [Epub ahead of print: 29 03 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Togashi Y, Shitara K, Nishikawa H. Regulatory T cells in cancer immunosuppression - implications for anticancer therapy. Nat Rev Clin Oncol 2019;16:356–71. 10.1038/s41571-019-0175-7 [DOI] [PubMed] [Google Scholar]
- 44.Arce Vargas F, Furness AJS, Solomon I, et al. Fc-Optimized Anti-CD25 depletes tumor-infiltrating regulatory T cells and synergizes with PD-1 blockade to eradicate established tumors. Immunity 2017;46:577–86. 10.1016/j.immuni.2017.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Selby MJ, Engelhardt JJ, Quigley M, et al. Anti-CTLA-4 antibodies of IgG2a isotype enhance antitumor activity through reduction of intratumoral regulatory T cells. Cancer Immunol Res 2013;1:32–42. 10.1158/2326-6066.CIR-13-0013 [DOI] [PubMed] [Google Scholar]
- 46.Quezada SA, Peggs KS. Lost in translation: deciphering the mechanism of action of anti-human CTLA-4. Clin Cancer Res 2019;25:1130–2. 10.1158/1078-0432.CCR-18-2509 [DOI] [PubMed] [Google Scholar]
- 47.Nimmerjahn F, Ravetch JV. Fcgamma receptors as regulators of immune responses. Nat Rev Immunol 2008;8:34–47. 10.1038/nri2206 [DOI] [PubMed] [Google Scholar]
- 48.Di Giacomo AM, Biagioli M, Maio M. The emerging toxicity profiles of anti-CTLA-4 antibodies across clinical indications. Semin Oncol 2010;37:499–507. 10.1053/j.seminoncol.2010.09.007 [DOI] [PubMed] [Google Scholar]
- 49.Klebanoff CA, Gattinoni L. Stubborn Tregs limit T-cell therapy. Blood 2012;120:2352–4. 10.1182/blood-2012-08-445239 [DOI] [PubMed] [Google Scholar]
- 50.Zappasodi R, Sirard C, Li Y, et al. Rational design of anti-GITR-based combination immunotherapy. Nat Med 2019;25:759–66. 10.1038/s41591-019-0420-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maj T, Wang W, Crespo J, et al. Oxidative stress controls regulatory T cell apoptosis and suppressor activity and PD-L1-blockade resistance in tumor. Nat Immunol 2017;18:1332–41. 10.1038/ni.3868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Crooke ST, Wang S, Vickers TA, et al. Cellular uptake and trafficking of antisense oligonucleotides. Nat Biotechnol 2017;35:230–7. 10.1038/nbt.3779 [DOI] [PubMed] [Google Scholar]
- 53.Ali K, Soond DR, Pineiro R, et al. Inactivation of PI(3)K p110δ breaks regulatory T-cell-mediated immune tolerance to cancer. Nature 2014;510:407–11. 10.1038/nature13444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Carnevalli LS, Sinclair C, Taylor MA, et al. PI3Kα/δ inhibition promotes anti-tumor immunity through direct enhancement of effector CD8+ T-cell activity. J Immunother Cancer 2018;6:158. 10.1186/s40425-018-0457-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Solomon I, Amann M, Goubier A, et al. CD25-Treg-depleting antibodies preserving IL-2 signaling on effector T cells enhance effector activation and antitumor immunity. Nat Cancer 2020;1:1153–66. 10.1038/s43018-020-00133-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.De Simone M, Arrigoni A, Rossetti G, et al. Transcriptional landscape of human tissue lymphocytes unveils uniqueness of tumor-infiltrating T regulatory cells. Immunity 2016;45:1135–47. 10.1016/j.immuni.2016.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lukesova E, Boucek J, Rotnaglova E, et al. High level of Tregs is a positive prognostic marker in patients with HPV-positive oral and oropharyngeal squamous cell carcinomas. Biomed Res Int 2014;2014:1–11. 10.1155/2014/303929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Saito T, Nishikawa H, Wada H, et al. Two FOXP3(+)CD4(+) T cell subpopulations distinctly control the prognosis of colorectal cancers. Nat Med 2016;22:679–84. 10.1038/nm.4086 [DOI] [PubMed] [Google Scholar]
- 59.Huang AC, Orlowski RJ, Xu X, et al. A single dose of neoadjuvant PD-1 blockade predicts clinical outcomes in resectable melanoma. Nat Med 2019;25:454–61. 10.1038/s41591-019-0357-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim CG, Kim KH, Pyo K-H, et al. Hyperprogressive disease during PD-1/PD-L1 blockade in patients with non-small-cell lung cancer. Ann Oncol 2019;30:1104–13. 10.1093/annonc/mdz123 [DOI] [PubMed] [Google Scholar]
- 61.Wei T, Zhong W, Li Q. Role of heterogeneous regulatory T cells in the tumor microenvironment. Pharmacol Res 2020;153:104659. 10.1016/j.phrs.2020.104659 [DOI] [PubMed] [Google Scholar]
- 62.Miyao T, Floess S, Setoguchi R, et al. Plasticity of Foxp3(+) T cells reflects promiscuous Foxp3 expression in conventional T cells but not reprogramming of regulatory T cells. Immunity 2012;36:262–75. 10.1016/j.immuni.2011.12.012 [DOI] [PubMed] [Google Scholar]
- 63.Overacre-Delgoffe AE, Chikina M, Dadey RE, et al. Interferon-γ Drives T reg Fragility to Promote Anti-tumor Immunity. Cell 2017;169:1130–41. 10.1016/j.cell.2017.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chaudhry A, Rudra D, Treuting P, et al. CD4+ regulatory T cells control TH17 responses in a Stat3-dependent manner. Science 2009;326:986–91. 10.1126/science.1172702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Levine AG, Mendoza A, Hemmers S, et al. Stability and function of regulatory T cells expressing the transcription factor T-bet. Nature 2017;546:421–5. 10.1038/nature22360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ahmadzadeh M, Antony PA, Rosenberg SA. IL-2 and IL-15 each mediate de novo induction of FOXP3 expression in human tumor antigen-specific CD8 T cells. J Immunother 2007;30:294–302. 10.1097/CJI.0b013e3180336787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gavin MA, Torgerson TR, Houston E, et al. Single-cell analysis of normal and FOXP3-mutant human T cells: FOXP3 expression without regulatory T cell development. Proc Natl Acad Sci U S A 2006;103:6659–64. 10.1073/pnas.0509484103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tran DQ, Ramsey H, Shevach EM. Induction of FOXP3 expression in naive human CD4+FOXP3 T cells by T-cell receptor stimulation is transforming growth factor-beta dependent but does not confer a regulatory phenotype. Blood 2007;110:2983–90. 10.1182/blood-2007-06-094656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Proia TA, Singh M, Woessner R, et al. STAT3 Antisense Oligonucleotide Remodels the Suppressive Tumor Microenvironment to Enhance Immune Activation in Combination with Anti-PD-L1. Clin Cancer Res 2020;26:6335–49. 10.1158/1078-0432.CCR-20-1066 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2021-003892supp001.pdf (5.8MB, pdf)
Data Availability Statement
Data are available upon reasonable request.