Abstract
Introduction
Emollients reduce the severity of dermatitis-associated symptoms. Antioxidant supplementation may be helpful to control inflammatory processes and consequential skin damage. The clinical performance and safety of an emollient medical device for topical treatment enriched with antioxidant ingredients in adults with mild-to-moderate dermatitis is presented in this manuscript.
Methods
We performed a monocenter, open‐label, uncontrolled clinical trial. Participants applied the product twice a day for 28 days. No other medication or moisturizer was allowed. Changes in dermatitis severity were assessed at days 14 and 28 by study investigators. Subjects self-assessed pruritus, Dermatology Life Quality Index, and product satisfaction. At the end of the study, a global evaluation of the product was done both by patient-reported outcomes and investigators’ evaluations.
Results
Forty subjects were enrolled in the study (mean age 35 years). Treatment success was achieved in 87.5% of subjects (p < 0.0001) after 28 days. Mean Investigator’s Global Assessment (IGA) and Eczema Area and Severity Index (EASI) scores decreased at days 14 and 28 (p < 0.0001). Subjects reported a reduction in pruritus severity and improvement of quality of life (p < 0.0001), along with satisfaction with the product. At the end of the study, skin condition improved in more than 90% of subjects. No safety issues were identified.
Conclusion
The medical device studied for topical use in this clinical trial is considered safe and reduces pruritus in adults with atopic and contact dermatitis.
Keywords: Atopic dermatitis, Contact dermatitis, Topical use, Medical device, Antioxidants
Key Summary Points
| Why carry out this study? |
| Recent data point to a role for oxidative stress in the pathology of atopic dermatitis (AD). |
| The addition of antioxidants may enhance the emollient action of topical moisturizers by minimizing the effect of oxidative stress and reactive oxidative species on the skin. |
| In this study, we assessed the clinical performance and safety of a novel antioxidant-enriched emollient in adults with mild-to-moderate dermatitis. |
| What was learned from the study? |
| Skin condition improved in more than 90% of subjects without treatment-related adverse events. |
| Pruritus decreased and the quality of life improved throughout the study. |
| The novel nonsteroidal topical treatment under study was effective, safe, and well tolerated. |
Introduction
Eczematous dermatitis ranks in the top 50 most common causes of disease, with a global prevalence of over 200 million (229,761,000) in 2010 [1]. Contact sensitization (allergic contact dermatitis) affects up to 20% of the general population [2]. Atopic dermatitis (AD), also named atopic eczema, impacts up to 20% of children and 2–8% of adults. [3]
Pruritus is a cardinal symptom of dermatitis, which is characterized by epidermal barrier dysfunction and inflammation [4]. Itching leads to constant scratching and the appearance of skin alterations (lichenification, excoriations), further disrupting the epidermal barrier [5]. The severity of pruritus and associated secondary symptoms is variable but frequently interferes with patients’ daily lives. Patients commonly complain about sleep disturbance, difficulty concentrating, and irritability, altogether negatively impacting their quality of life [5]. Patients with atopic dermatitis often present comorbidities, including geographic tongue and alopecia areata, further increasing the burden of the disease [6, 7]. The burden experienced by patients with AD, both children and adults, has a deep impact on the health-related quality of life. All domains of daily activity are affected: school, work, leisure, and personal relationships. Bullying at school and career discrimination at work are frequent complaints. As a result, patients with AD, regardless of the severity of the disease, are more commonly affected by psychiatric comorbidities—including depression, anxiety, and suicidal ideation—than the general population [8, 9].
Contact dermatitis (CD) occurs when the skin is exposed to substances that irritate or trigger an allergic reaction, causing the skin to become erythematous, blistered, dry, scaly, and cracked. The first step in CD treatment should be to identify and avoid further contact with the causative agent. AD is a chronic disease, with recurrent red and itchy lesions usually located on hands and skin flexures in adolescents and adults [10–12]. Epidermal barrier alterations, genetic susceptibility, and immune dysfunction are involved in disease development. Still, in the absence of a cure, the disease remains a therapeutic challenge. Available therapies include systemic and topical treatments to alleviate symptoms. Steroid-based therapies are considered one of the most effective treatment but have the potential to cause serious side effects, particularly in the long term. This leads to fears of using topical corticosteroids (steroid phobia) among patients, which affect treatment compliance, and limits the use in delicate areas (i.e., face) and patients of younger age, that is, infant and children. Therefore, alternative steroid-free (nonsteroidal) therapeutic options would be useful [13, 14]. Current guidelines for AD management recommend using topical moisturizers either alone or with steroidal-based treatments in the most severe cases (https://doi.org/10.1111/dth.13121) [15]. Topical calcineurin inhibitors can also be used as steroid-sparing, antiinflammatory agents in AD both during flares and as maintenance therapy (proactive therapy), as recommended by recent guidelines [15]. The regular use of moisturizers may be enough to control mild symptoms and reduce the dose of steroids needed in severe AD [16]. Recent findings also point to a role of oxidative stress in developing inflammatory skin disorders [17]. The classical formulation of topical moisturizers is based on occlusive and humectant ingredients. These molecules allow the formation of a physical barrier on the skin and increase hydration, thus creating an optimal environment for barrier regeneration [18].
More recently, these formulations have been supplemented with different ingredients to improve the action on the skin. The new-generation topical emollients device enriched with antioxidant agents such as furfuryl palmitate and tocopherol may provide effective and safe steroid-sparing options for AD [17]. Indeed, recent data support the hypothesis of an interplay between oxidative stress, immune dysregulation, pruritus, and altered skin barrier permeability in the pathology of AD [17]. Therefore, the addition of antioxidants would enhance the emollient action of these products by minimizing the effect of oxidative stress and reactive oxidative species on the skin’s cellular components [17]. This investigation was undertaken to assess the clinical performance and safety of an antioxidant-enriched medical device for topical use in adults with mild-to-moderate dermatitis.
Methods
Study Design
This was a monocenter, single-arm, non-controlled, post-market clinical follow-up investigation conducted between May and June 2019 in Italy. This clinical study aimed to examine the efficacy and safety of a medical device (Relizema cream, from RELIFE SRL, Italy) containing furfuryl palmitate, glycerin, tocopherol (vitamin E), castor oil, and vitamin F for topical use in adults with mild-to-moderate atopic or contact dermatitis.
The study’s primary objective was to evaluate and confirm the performance of Relizema cream in the improvement of eczematous dermatitis, as seen by a reduction in disease severity and symptoms after 28 days of treatment as assessed by IGA scores (successful threshold established as reduction of 1 point of the IGA score with respect to baseline value). Secondary objectives were: to evaluate the performance of the product after 14 days of treatment as assessed by IGA scores; to evaluate the eczema improvement after 14 and 28 days of treatment with EASI score; to evaluate pruritus improvement at day 14 and 28, as reported by the subject through everyday report in a diary; to assess the improvement in the quality of life of the subject related to their dermatitis, through the Dermatology Life Quality Index (DLQI) questionnaire; to evaluate the subject’s adherence to treatment from daily diary compilation and product accountability; to evaluate the subject’s and investigator’s global evaluation of the performance of the cream; to assess the subject’s overall acceptability of the treatment. Tolerability and safety objectives consisted of evaluating the local and general tolerability and adverse events (AE) observed during the study. Subjects were given recommendations for personal hygiene. Throughout the treatment phase, subjects were required to avoid soap and use only the product Relizema lipid-replenishing cleanser (also registered as DermoRelizema or Dermarel), indicated for dry and sensitive skin.
The clinical investigation protocol was regularly submitted to the competent ethics committee and notified to the Italian Ministry of Health, as for post-market clinical follow-up studies. The clinical study was approved by the ethics committee (Comitato Etico dell’Area Vasta Emilia Nord, Italy) on 5 February 2019. The study was conducted in full accordance with the Declaration of Helsinki, ISO 14155:2011, and good clinical practice (GCP). All participants provided informed written consent.
Subjects
Eligibility criteria included healthy male and female subjects aged between 18 and 65 years (inclusive), with eczematous dermatitis, including atopic dermatitis (AD), irritant contact dermatitis (ICD), or allergic contact dermatitis (ACD) of mild-to-moderate severity defined as follows: IGA score 2 (mild) or 3 (moderate), and EASI score 1.1–7.0 (mild) or 7.1–21.0 (moderate). Dermatitis could be affecting one or more body areas (face, legs, arms, etc.). The diagnosis of contact dermatitis was based on clinical assessment and patch testing. Patch testing was performed following the most recent Italian guidelines [19].
Subjects were excluded if they had other concomitant skin disorders (including infections); if they had other diseases, such as cancer (or have had cancer in the previous five years), diabetes, congenital or acquired immunodepression, immunologic or infectious diseases, active infections; if they were allergic or intolerant to the device ingredients; if they had any clinically significant condition that in the investigator’s opinion could interfere with the study evaluations. Subjects were also excluded if: taking antibiotics in the previous 7 days; using any topical medication for dermatitis in the last 14 days or any topical product for dermatitis in the 2 days before inclusion; taking any systemic treatment or procedure that could influence dermatitis activity within the previous 30 days (or five half-lives); taking any corticosteroids, immunosuppressant drugs, or immunotherapy within the last 30 days (or five half-lives); taking oral antihistamines and antidepressants in the previous 30 days; participating in another interventional clinical study over the last 3 months; planning exposure to sun or tanning booths or UV sources during the study period.
Treatment Protocol
The study cream was topically applied to all areas affected by dermatitis twice a day for 28 consecutive days by the subjects. Investigator-based assessments were performed at baseline and days 14 and 28.
Efficacy Assessments
The study’s primary outcome measure was how the Investigator’s Global Assessment (IGA) scores changed from baseline to 28 days of treatment with the medical device for topical use. The IGA assesses atopic/contact dermatitis severity on a six-point scale (0 = clear; 1 = almost clear; 2 = mild; 3 = moderate; 4 = severe; 5 = very severe). Other investigator-assessed efficacy measurements were IGA score at 14 days and EASI scores at baseline and 14 and 28 days. The Eczema Area and Severity Index (EASI) tool measures extent and severity of eczema on the basis of four body regions (head and neck, trunk, upper limbs, and lower limbs). The percentage of skin affected by eczema in each region is correlated with an area score (0 = 0%: no eczema in this region; 1 = 1–9%; 2 = 10–29%; 3 = 30–49%; 4 = 50–69%; 5 = 70–89%; 6 = 90–100%: the entire region is affected by eczema). A severity score (0 = none, 1 = mild, 2 = moderate, or 3 = severe) is then recorded for each of the four regions identified for the following four signs: redness (erythema, inflammation); thickness (induration, papulation, swelling—acute eczema); scratching (excoriation); lichenification (lined skin, prurigo nodules—chronic eczema).
Subjects assessed pruritus severity and the impact on their quality of life. Each subject was requested to register in their diaries, at the end of each day, the severity of pruritus by placing a vertical mark on a 100 mm visual analog scale (VAS). The rating was scored as the distance from the left side of the scale (0 mm) to the subject’s mark.
Subjects were asked to complete the DLQI questionnaire to assess the impact on quality of life. The DLQI is composed of ten questions, covering the following topics: symptoms, embarrassment, shopping and home care, clothes, social and leisure, sport, work or study, close relationships, sex, treatment. Each question refers to the impact of skin disease on the patient’s life over the previous week. Each item is scored from 0 to 3, giving a possible score range from 0 (meaning no impact of skin disease on quality of life) to 30 (meaning maximum impact on quality of life).
Safety and Adherence to Treatment
Adverse events (AEs) and local tolerability at the administration site (e.g., skin increased itching or redness or irritation) were reported and summarized. The number of applications written in the subject’s diary and product accountability were used to demonstrate treatment adherence.
Treatment Satisfaction
The subject and investigator’s evaluation of the global performance of the medical device for topical use was assessed on a seven-point scale (1 = very much improved, 2 = improved, 3 = minimally improved, 4 = no change, 5 = minimally worse, 6 = worse, 7 = very much worse). These assessments were performed at the end of treatment (visit 3).
Subjects also assessed the overall acceptability with treatment. The evaluation considered two aspects: the pleasant or unpleasant feeling with the product and the ease of use. Both aspects were graded on a five-point scale (1 = very much satisfied, 2 = satisfied, 3 = neither satisfied nor dissatisfied, 4 = dissatisfied, 5 = very much dissatisfied) at the end of treatment.
Statistical Analysis
The sample size estimation was based on an exact binomial test with a nominal 5% two-sided significance level that should have 80% power to detect the difference between the null hypothesis proportion, π0 of 0.5 (i.e., 50% of patients with treatment success) and the alternative proportion, π1, of 0.75 (i.e., 75% of patients with treatment success) when the sample size was 30 subjects. Forty subjects were estimated to be necessary for enrollment by assuming a possible 25% dropout rate.
Results
Subjects
Forty subjects were enrolled in the study, which was conducted between May and June 2019. The baseline characteristics of the subjects are presented in Table 1. The mean age was 35.3 years (ranging from 19 to 59 years). Most subjects were female (67.5%). All subjects were affected either by atopic dermatitis (47.5%) or contact dermatitis (52.5%); contact dermatitis was of allergic origin in most cases (90.5%). All subjects were Caucasian. Atopic dermatitis affected the face, legs, arms, and other body parts; contact dermatitis mainly affected arms and other parts of the body, like hands and feet. The severity of atopic or contact dermatitis was mild (n = 29, 72.5%) to moderate (n = 11, 27.5%), as assessed by IGA scores. The mean EASI score was 4.49 ± 3.87 (1.20–14.80), and the mean DLQI score was 7.23 ± 4.54 (0–18).
Table 1.
Subject characteristics (n = 40)
| Characteristics | |
|---|---|
| Sex | |
| Female | 27 (67.5) |
| Male | 13 (32.5) |
| Age (years) | |
| Mean ± SD | 35.3 ± 9.81 |
| Median, range | 32.5, 19–59 |
| IGA score | |
| Mean ± SD | 2.28 ± 0.45 |
| Median, range | 2.00, 2.00–3.00 |
| EASI score | |
| Mean ± SD | 4.49 ± 3.87 |
| Median, range | 2.70, 1.20–14.80 |
| DLQI score | |
| Mean ± SD | 7.23 ± 4.54 |
| Median, range | 7.00, 0–18 |
| Type of dermatitis | |
| Atopic dermatitis | 19 (47.50) |
| Contact dermatitis | 21 (52.50) |
DLQI Dermatology Life Quality Index, EASI Eczema Area and Severity Index, IGA Investigator’s Global Assessment, SD standard deviation
One subject did not complete the pruritus severity VAS at baseline before treatment start. This subject was excluded from the pruritus severity analysis. One subject began a forbidden concomitant treatment (an oral antibiotic) for a non-treatment-related adverse event between day 14 and day 28. According to the statistical analysis plan, the primary endpoint analysis was done as intention-to-treat and as per-protocol (including and excluding the subject).
Efficacy and Safety
A statistically significant reduction in mean IGA scores was seen at 28 days on intention-to-treat analysis (−1.20; 95% CI −1.41, −0.99) (Fig. 1A). A similar result was seen on per-protocol analysis: at 28 days, the reduction in mean IGA scores was also statistically significant (p < 0.0001; −1.21; 95% CI −1.41, −0.99). Treatment success, which was defined as a decrease in IGA scores between baseline and day 28 of one or more points, was achieved in 87.5% of patients [intention-to-treat (ITT) analysis; Table 2]. Of note, no subject experienced worsening during the study period.
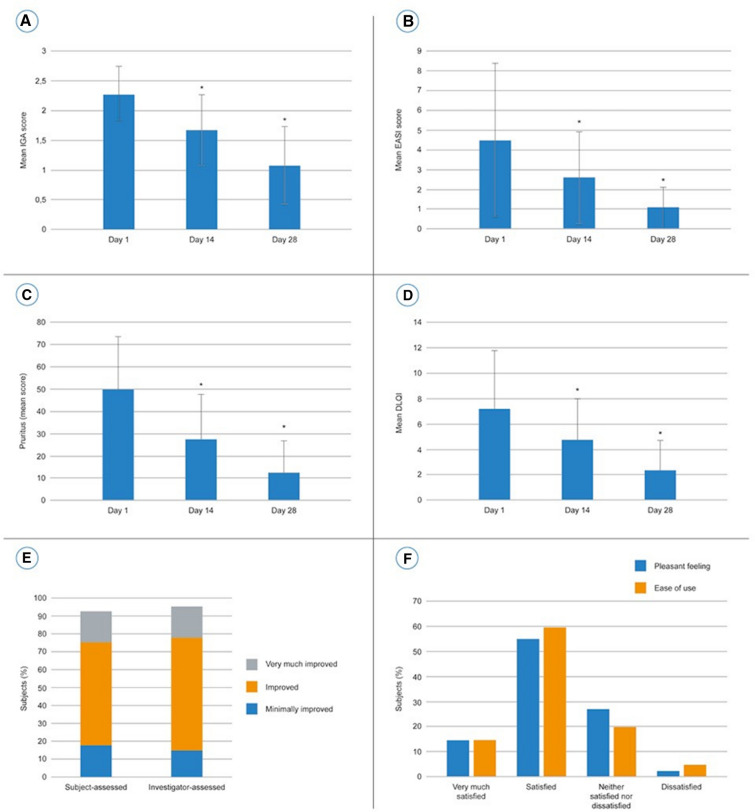
Fig. 1.
A Changes in mean IGA score from baseline. B Changes in mean EASI score from baseline. C Subject-reported symptom scores—pruritus severity. D Subject-reported symptom scores—DLQI. E Subject and investigator’s global evaluation of performance. F Subject-assessed overall acceptability of the product
Table 2.
Disease severity and treatment success as assessed by investigators using the IGA score
| Category, Full analysis set (FAS) (n = 40) | Day 1 (baseline) | Day 14 | Day 28 |
|---|---|---|---|
| IGA score, n (%) | |||
| Clear | 0 (0.0) | 0 | 7 (17.5) |
| Almost clear | 0 (0.0) | 18 (45.0) | 23 (57.5) |
| Mild | 29 (72.5) | 17 (42.5) | 10 (25) |
| Moderate | 11 (27.5) | 5 (12.5) | 0 (0.0) |
| Severe | 0 (0.0) | 0 | 0 (0.0) |
| p-Value versus baseline | – | < 0.0001 | |
| Treatment success, n (%) | |||
| Decrease from baseline ≥ 1 | – | 24 (60.0) | 35 (87.5) |
| p-Value versus baseline | – | < 0.0001 |
A decrease in disease severity, as assessed by the IGA score, was seen after only 14 days, the first control visit. There was a statistically significant reduction (p < 0.0001) in IGA from baseline to day 14 (−0.60; 95% CI −0.79, −0.41) (Fig. 1A).
Accordingly, disease severity was also reduced at 14 and 28 days when measured using the EASI score. EASI scores were reduced after 14 days of treatment (first control visit) compared with baseline (−1.90; p < 0.0001, 95% CI −2.72, −1.08) (Fig. 1B). On day 28, the change in EASI scores from baseline was even more pronounced (−3.41; p < 0.0001; 95% CI −4.51, −2.31).
Subjects reported a statistically significant reduction in pruritus severity from baseline to day 14 (−21.92; 95% CI −27.07, −16.77; p < 0.0001) and day 28 (−37.13; 95% CI −44.71, −29.54; p < 0.0001; Fig. 1C). The improvement in symptom severity had a positive effect on the self-reported DLQI questionnaires (Fig. 1D). Subjects reported a statistically significant improvement in quality of life at day 14 (−2.43; 95% CI −3.23, −1.62; p < 0.0001) and day 28 (−4.83; 95% CI −5.88, −3.77; p < 0.0001).
Only one adverse event, not related to the study treatment, was observed. Local tolerability at the site of administration of the cream was good. Compliance with treatment was generally very good, ranging from 88.5% to 100%.
Treatment Satisfaction
Treatment satisfaction was assessed using a global evaluation of the performance at the end of the study (Fig. 1E). Most subjects (92.5%, n = 37) evaluated their skin condition as “improved.” Among these, seven subjects evaluated their skin as “very much improved,” 23 as “improved,” and seven as “minimally improved.” Only one subject reported his skin condition as worse at the end of treatment.
According to the Investigator’s assessment, the skin condition of most subjects (95%) was “improved”: seven subjects were identified as “very much improved”, 25 as “improved”, and six as “minimally improved”. Only one subject was evaluated as worse at the end of the study.
The overall acceptability of the treatment was also assessed by the subjects (Fig. 1F). Most subjects thought the product was pleasant (70%, n = 28). Only one subject was dissatisfied with the feeling of the product (2.5%). Most subjects were either “very much satisfied” or “satisfied” (75%, n = 30) regarding the ease of use. Only two patients were not satisfied with the ease of use (5%).
Discussion
Skin barrier dysfunction is a major hallmark of atopic and contact dermatitis and has a primary pathogenic role in disease development and manifestations [4]. In fact, skin barrier deficiency is responsible for increased access of environmental agents into the skin, which triggers an immune response and inflammation cascade. Moreover, recurrent and chronic skin inflammation further attenuates skin barrier function, generating a positive feedback loop between the epidermis and the immune system that drives the disease process [17]. Moisturization with creams improves barrier function without the side effects associated with corticosteroids [16]. The use of topical emollients is recommended as baseline treatment in both AD and CD. However, little is known about how emollient capacity can be enhanced with other products, which can trigger the inflammatory cascade and immune system response mechanisms. Understanding the mechanisms of skin barrier degeneration and related phenomena is essential for improving the management of contact and atopic dermatitis and limiting downstream manifestations. Recently the role of oxidation in AD has been investigated, and antioxidant molecules have been proposed to improve skin barrier repair [17]. However, few studies have investigated the effect of emollient in combination with antioxidants on skin disease course and how patients perceive it in terms of clinical results and quality of life [20]. Here, we investigated a novel nonsteroidal topical emollient medical device formulated and enriched with antioxidant for topical use applied twice a day for 28 days and documented symptom reduction and improvement of the quality of life in adult patients with mild-to-moderate atopic and contact eczema. The topical treatment was well tolerated, and no treatment-related AEs were observed. Most patients thought the product was pleasant and were satisfied with the ease of use.
The medical device for topical use was formulated as a cream that creates a physical barrier on the skin, isolating it from the surrounding environment. This physical action improves skin barrier protection, which generates optimal conditions for improving moisturization beyond skin barrier repair. The formulation includes antioxidant agents, such as furfuryl palmitate and tocopherol, and hence represents a treatment targeted toward oxidative stress, beyond the trinity pathophysiologic factors (pruritus / itch, inflammation, and skin barrier defect). Recent studies have highlighted the possible involvement of oxidative stress in skin disorders, particularly atopic dermatitis. An imbalance in the release of antioxidant species may increase damage in cellular components and enhance the production of inflammatory cytokines [21]. Several studies have shown that emollients enriched with antioxidant agents significantly improve eczema in both children and adult patients (reviewed by Pigatto and Diani) [18]. Indeed, Pigatto and Diani reviewed data from six clinical trials, five of which point to a positive role of furfuryl-enriched creams in contrasting signs and symptoms of mild-to-moderate eczema [18]. Furfuryl palmitate is an ester with antioxidant effect due to its ability to quench singlet oxygen. Singlet oxygen is a reactive oxygen species with a role in the pathogenesis of several skin diseases, including atopic dermatitis. Of note, in a randomized clinical trial, 40 adult patients with atopic dermatitis were treated either with a furfuryl-palmitate-based cream or a topical corticosteroid twice daily for 14 days [22]. Symptoms were significantly improved in both groups compared with baseline, while no statistically significant differences were observed between groups.
Results from our study are in line with these findings. Mean IGA and EASI scores decreased at days 14 and 28 compared with baseline (p < 0.0001). Subjects reported a reduction in pruritus severity and, consequently, improved quality of life (p < 0.0001). This statistically significant reduction in pruritus severity and rapid itch reduction will help patients to avoid sleep disturbance, to have better sleep quality in their daily life. At the end of the study, skin condition improved in more than 90% of subjects, as reported by investigators and subject self-assessment. In addition, our research shows that most subjects liked the product characteristics and the ease of use, which is confirmed by the high treatment compliance. In conclusion, this study demonstrates that the addition of antioxidants in emollients is safe and an effective treatment strategy targeted toward oxidative stress to improve the beneficial effect of skin moisturization and promote effective skin healing. Moreover, the quality of the emollient should be designed to guarantee the best barrier effect as well as the best hydrating capacity, keeping in mind that its texture and cosmetic characteristics should be compatible with the specific needs of eczematous skin and subjective perception to improve patient compliance.
The study is not without limitations. The open label design and the lack of a control group limit the interpretation of the efficacy results. Further studies with control groups are needed to confirm the effects of the antioxidant-enriched topical cream under study.
Conclusion
The combination of therapies with nanotechnologies to deliver topicals is emerging as a good strategy to improve patients’ adherence to treatment, particularly during the past 2 years in which many patients struggled to continue their routines and daily treatments owing to the COVID-19 pandemic [23–25]. The novel nonsteroidal topical treatment (Relizema cream) was effective, safe, and well tolerated. This antioxidant-enriched emollient medical device offers valuable treatment options, of a steroid-free treatment for patients with AD and CD, which will improve patients’ treatment compliance. Most importantly, this clinical study confirms its effectiveness in reducing the severity of symptoms in adults with AD and CD with a continuous improvement of patients’ condition from the first control visit (day 14) to the end of the study (day 28), reaching a statistically significant improvement in both primary and secondary endpoints. This clinical study highlights the importance of addressing the interplay of multiple pathogenesis factors of barrier dysfunction, pruritus/inflammation, dysfunctional immune response, and oxidative stress as a new treatment target in dermatitis.
Acknowledgements
Funding
This study and the journals rapid service fee were sponsored by RELIFE, Italy.
Medical Writing, Editorial, and Other Assistance
Medical writing and editorial support were provided by ERA MS, Italy, and funded by RELIFE, Italy.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Conceptualization, G. P.; writing—original draft preparation, MB. G, L.B, T.A, M.R., S.L; writing—review and editing MB. G, L.B, T.A, M.R., S.L, G.P. Acquisition, analysis, or interpretation of data: A. A. H. All authors contributed to data analyses, drafting, and revising the manuscript.
Disclosures
Dr. Adelaide Ann Hebert and Dr. Giovanni Pellacani: Scientific speaker for RELIFE (Menarini Group). International editor of this clinical study publication. Dr Mario Bruno Guanti, Dr Laura Bonzano, Dr Marco Rivi, Dr Tatiana Alicandro and Serena Liberati have nothing to disclose.
Compliance with Ethics Guidelines
The clinical investigation protocol was regularly submitted to the competent Ethics Committee and notified to the Italian Ministry of Health, as for post-market clinical follow-up studies. The clinical study was approved by the Ethics Committee (Comitato Etico dell’Area Vasta Emilia Nord (Italy)) on February 5th, 2019. The study was conducted in full respect of the Helsinki Declaration, ISO 14155:2011, and GCP. All participants provided informed written consent.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134(6):1527–1534. doi: 10.1038/jid.2013.446. [DOI] [PubMed] [Google Scholar]
- 2.Koppes SA, Engebretsen KA, Agner T, et al. Current knowledge on biomarkers for contact sensitization and allergic contact dermatitis. Contact Dermatitis. 2017;77(1):1–16. doi: 10.1111/cod.12789. [DOI] [PubMed] [Google Scholar]
- 3.Wollenberg A, Barbarot S, Bieber T, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol. 2018;32(5):657–682. doi: 10.1111/jdv.14891. [DOI] [PubMed] [Google Scholar]
- 4.Zug KA, McKay M. Eczematous dermatitis: a practical review. Am Fam Physician. 1996;54(4):1243–1250. [PubMed] [Google Scholar]
- 5.Abramovits W, Hebert AA, Boguniewicz M, et al. Patient-reported outcomes from a multicenter, randomized, vehicle-controlled clinical study of MAS063DP (Atopiclair™ ) in the management of mild-to-moderate atopic dermatitis in adults. J Dermatol Treat. 2008;19(6):327–332. doi: 10.1080/09546630802232799. [DOI] [PubMed] [Google Scholar]
- 6.Damiani G. Cutaneous and oral comorbidities in patients with geographic tongue: a multicenter multidisciplinary cross-sectional observational study. J Biol Regul Homeost Agents. 2021 doi: 10.23812/21-2supp1-33. [DOI] [PubMed] [Google Scholar]
- 7.Conic RZ, Tamashunas NL, Damiani G, et al. Comorbidities in pediatric alopecia areata. J Eur Acad Dermatol Venereol. 2020;34(12):2898–2901. doi: 10.1111/jdv.16727. [DOI] [PubMed] [Google Scholar]
- 8.Stingeni L, Fortina AB, Baiardini I, Hansel K, Moretti D, Cipriani F. Atopic dermatitis and patient perspectives: insights of bullying at school and career discrimination at work. J Asthma Allergy. 2021;14:919–928. doi: 10.2147/JAA.S317009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barrett A, Hahn-Pedersen J, Kragh N, Evans E, Gnanasakthy A. Patient-reported outcome measures in atopic dermatitis and chronic hand eczema in adults. Patient. 2019;12(5):445–459. doi: 10.1007/s40271-019-00373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trusler AR, Clark AK, Sivamani RK, Shi VY. The endocannabinoid system and its role in eczematous dermatoses. Dermatitis. 2017;28(1):22–32. doi: 10.1097/DER.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 11.Rundle CW, Bergman D, Goldenberg A, Jacob SE. Contact dermatitis considerations in atopic dermatitis. Clin Dermatol. 2017;35(4):367–374. doi: 10.1016/j.clindermatol.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Weidinger S, Beck LA, Bieber T, Kabashima K, Irvine AD. Atopic dermatitis. Nat Rev Dis Primer. 2018;4(1):1. doi: 10.1038/s41572-018-0001-z. [DOI] [PubMed] [Google Scholar]
- 13.Hanifin JM, Cooper KD, Ho VC, et al. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology (AAD)/American Academy of Dermatology Association “Administrative Regulations for Evidence-Based Clinical Practice Guidelines”. J Am Acad Dermatol. 2004;50(3):391–404. doi: 10.1016/j.jaad.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006;54(1):1–15. doi: 10.1016/j.jaad.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 15.Damiani G, Calzavara-Pinton P, Stingeni L, et al. Italian guidelines for therapy of atopic dermatitis—adapted from consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) Dermatol Ther. 2019 doi: 10.1111/dth.13121. [DOI] [PubMed] [Google Scholar]
- 16.Lodén M. Effect of moisturizers on epidermal barrier function. Clin Dermatol. 2012;30(3):286–296. doi: 10.1016/j.clindermatol.2011.08.015. [DOI] [PubMed] [Google Scholar]
- 17.Hebert AA. Oxidative stress as a treatment target in atopic dermatitis: the role of furfuryl palmitate in mild-to-moderate atopic dermatitis. Int J Womens Dermatol. 2020;6(4):331–333. doi: 10.1016/j.ijwd.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pigatto PD, Diani M. Beneficial effects of antioxidant furfuryl palmitate in non-pharmacologic treatments (prescription emollient devices, PEDs) for atopic dermatitis and related skin disorders. Dermatol Ther. 2018;8(3):339–347. doi: 10.1007/s13555-018-0239-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.On behalf of “Skin Allergy” group of SIDeMaST and “SIDAPA” (Società Italiana di Dermatologia Allergologica, Professionale e Ambientale) Stingeni L, Bianchi L, et al. Italian guidelines in patch testing—adapted from the European Society of Contact Dermatitis (ESCD) G Ital Dermatol Venereol. 2019 doi: 10.23736/S0392-0488.19.06301-6. [DOI] [PubMed] [Google Scholar]
- 20.van Zuuren EJ, Fedorowicz Z, Arents BWM. Emollients and moisturizers for eczema: abridged Cochrane systematic review including GRADE assessments. Br J Dermatol. 2017;177(5):1256–1271. doi: 10.1111/bjd.15602. [DOI] [PubMed] [Google Scholar]
- 21.Ji H, Li XK. Oxidative stress in atopic dermatitis. Oxid Med Cell Longev. 2016;2016:1–8. doi: 10.1155/2016/2721469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lauriola MM, Pigatto PD, Pedrelli V. A single-center, randomized, perspective, investigator blinded controlled trial to examine efficacy and safety of a furpalmate cream in comparison to topical corticosteroid in atopic dermatitis of hands of hands of 40 adult patients. In: Poster session 20th EADV Congress, 20–24 October 2011, Lisbon, Portugal.
- 23.Pacifico A, Iacovelli P, Damiani G, et al. ‘High dose’ vs. ‘medium dose’ UVA1 phototherapy in Italian patients with severe atopic dermatitis. J Eur Acad Dermatol Venereol. 2019;33(4):718–724. doi: 10.1111/jdv.15362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Damiani G, Eggenhöffner R, Pigatto PDM, Bragazzi NL. Nanotechnology meets atopic dermatitis: current solutions, challenges and future prospects. Insights and implications from a systematic review of the literature. Bioact Mater. 2019;4:380–386. doi: 10.1016/j.bioactmat.2019.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bragazzi NL, Riccò M, Pacifico A, et al. COVID-19 knowledge prevents biologics discontinuation: data from an Italian multicenter survey during RED-ZONE declaration. Dermatol Ther. 2020 doi: 10.1111/dth.13508. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.