Abstract
Background:
A subset of patients with femoroacetabular impingement (FAI) fail arthroscopic management. It is not clear which patients will fail surgical management; however, several surgical and patient factors, such as type of procedure and age, are thought to be important predictors.
Purpose:
This time-to-event analysis with a 27-month follow-up analysis compared the effect of (1) arthroscopic osteochondroplasty with or without labral repair versus (2) arthroscopic lavage with or without labral repair on the time to reoperation in adults aged 18 to 50 years with FAI.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
Eligible participants had been randomized in a previous study trial to a treatment of arthroscopic osteochondroplasty or arthroscopic lavage with or without labral repair. Using the comprehensive data set from the Multinational Femoroacetabular Impingement Randomized controlled Trial, all reoperations until 27 months after surgery were identified. The analysis was conducted using a Cox proportional hazards model, with percentage of patients with a reoperation evaluated in a time-to-event analysis as the outcome. The independent variable was the procedure, with age and impingement subtype explored as potential covariates. The effects from the Cox model were expressed as the hazard ratio (HR). All tests were 2-sided, with an alpha level of .05.
Results:
A total of 108 patients in the osteochondroplasty group and 106 patients in the lavage group were included. The mean age of the patients included in the study was 36 ± 8.5 years. Overall, 27 incident reoperations were identified within the 27-month follow-up, with an incidence rate of 6 per 100 person-years. Within the osteochondroplasty group, 8 incident reoperations were identified (incidence rate, 3.4 per 100 person-years), while within the lavage group, 19 incident reoperations were identified (incidence rate, 8.7 per 100 person-years). The hazard of reoperation for patients undergoing osteochondroplasty was 40% of that of patients undergoing lavage (HR, 0.40 [95% CI, 0.17-0.91] P = .029).
Conclusion:
This study demonstrated that for adults between the ages of 18 and 50 years with FAI, arthroscopic osteochondroplasty was associated with a 2.5-fold decrease in the hazard of reoperation at any point in time compared with arthroscopic lavage.
Registration:
NCT01623843 (ClinicalTrials.gov identifier).
Keywords: femoroacetabular impingement, arthroscopic surgery, osteochondroplasty, femoroplasty, hip labral tear, labral repair, hip impingement
Femoroacetabular impingement (FAI) is a condition whereby a mismatch in shape and size between the femoral head and the acetabulum causes debilitating hip pain in young adults, and it is recently becoming better understood. There are 2 major morphology subtypes of FAI: (1) the cam-type—a misshaped femoral head—and (2) the pincer-type—an overcovered or deep socket. 15 Many patients have a combination of these deformities, which are referred to as a mixed type. 3 These abnormal bony structures cause impingement with movement of the hip, particularly with flexion and internal rotation. The impingement is proposed to cause damage to structures within the hip joint, such as the cartilage and the labrum, which leads to pain and disability for many young adults with the condition. 9
While patients with FAI generally improve after surgical management, there are some who do not respond as well, with reported failure rates up to 13% in previous studies. 4,5,12 In patients who fail the initial surgical management and thus require revision surgery, further labral tears and residual osseous deformity of the femoral head-neck junction are commonly reported. 13,20,21 It is not completely clear which patients undergoing surgical management of FAI will have a successful outcome; however, several surgical and patient factors that may predict success or failure have been reported. Labral debridement alone, older age, and elevated body mass index (BMI) are some factors that have been associated with negative outcomes in previous studies. 23
The recently completed Femoroacetabular Impingement Randomized controlled Trial (FIRST) is a multicenter, international randomized controlled trial (RCT) that evaluated the effect of arthroscopic osteochondroplasty versus arthroscopic lavage in 220 adults aged 18 to 50 years diagnosed with FAI. 2 Using data from this trial, the purpose of this study was to assess and compare the effect of (1) arthroscopic osteochondroplasty with or without labral repair versus (2) arthroscopic lavage with or without labral repair on the time to reoperation in adults aged 18 to 50 with FAI using a time-to-event analysis over a 27-month follow-up. Our hypothesis was that arthroscopic osteochondroplasty would result in a decreased hazard of reoperation compared with arthroscopic lavage.
Methods
The FIRST trial protocol was registered at clinicaltrials.gov (NCT01623843), and ethics approval was granted to the Methods Center at McMaster University as well as at each participating site.
Trial Design
The full methodological details of the trial have been published previously. 7,22 The trial involved 10 centers across Canada, Denmark, and Finland between October 2012 and November 2017. Patients were eligible for inclusion in the study if they had the cam- or the mixed-type FAI confirmed with radiography after at least 6 months of nonoperative management and if they were between the ages of 18 and 50 years. Eligible participants were then randomized to undergo surgical management with either arthroscopic osteochondroplasty (ie, surgical correction of the hip impingement morphology) or arthroscopic lavage (ie, washing out the hip joint) with or without labral repair using a centralized, 24-hour, internet-based randomization system. In the osteochondroplasty group, bony lesions were resected using fluoroscopic guidance. In the lavage group, no osteochondroplasty was performed after lavage of the joint with 3 L of normal saline. In both groups, significant and obvious labral tears and cartilage damage were addressed with repair or debridement. The final follow-up for each patient was intended to be 27 months after one’s initial respective surgical intervention. The event of interest in this study was reoperation of the ipsilateral hip. A reoperation was defined as any unplanned revision surgery of the trial hip to relieve pain, treat infection, or improve function. Each reoperation, as well as the date, was recorded, and the event was reviewed by a blinded, independent adjudication committee to determine whether it was a true reoperation event according to prespecified criteria.
Covariates for Assessment
The covariates chosen for the assessment in this study were based on clinical rationale, as well as previous reports in the literature, and included impingement subtype and age. 10,11,19 The impingement subtype was assessed before the surgical management, as patients were deemed to have the cam or the mixed type of appearance on the arthroscopic examination. Other covariates measured but not included in the model were sex, ethnicity, BMI, baseline sport activity, degree of osteoarthritis, and impingement severity. The baseline sport activity was self-defined by participants included in the study as none, light, moderate, or vigorous. The Tönnis and Heinecke classification was used to grade osteoarthritis, with grade 0 indicating no sign of osteoarthritis, grade 1 slight narrowing of the joint, grade 2 increased narrowing of the joint and moderate loss of sphericity of the femoral head, and grade 3 obliteration of the joint space with severe deformity of the femoral head. 25 Impingement severity was classified as severe (alpha angle >83°), moderate (alpha angle ≥60°), or mild (alpha angle <60°).
Time Origin and Scale
Time-on-study was used as the time scale, with the time origin taken as the time of initial surgery for all patients, and the reoperation time was taken as time (number of days) from the initial surgery to the reoperation. Data were censored at either the 27-month (final) follow-up visit or the last available follow-up visit for those lost to follow-up early.
Statistical Analysis
Descriptive statistics were calculated, including counts, frequencies, and percentages for categorical variables, means, standard deviations, and standard errors for normally distributed variables, and medians and ranges for nonnormally distributed data. Patients were analyzed in the group to which they were randomized (as per the intention-to-treat principle). The person-years incidence rate was calculated as the number of patients with reoperations divided by the sum of the final follow-up or event times for each patient. 8 The 1-year incidence was calculated as the number of patients with reoperations before 1 year divided by the number of patients who completed follow-up assessments at 1 year. All analyses were conducted using SAS Version 9.3 (SAS Institute Inc).
Primary Outcome Analysis
Kaplan-Meier curves were constructed to depict the time to reoperation. The mean survival times were calculated as the integral under the Kaplan-Meier curves until the 27-month follow-up. The primary analysis was conducted using a proportional hazards model, with the percentage of patients with a reoperation analyzed in a time-to-event analysis as the outcome. The independent variable was the procedure (osteochondroplasty vs lavage), with age and impingement subtype explored as potential covariates. It was anticipated that a total of approximately 25 to 30 events (reoperations) would be recorded at the final follow-up of 27 months, and therefore it was decided a priori that no more than 2 covariates could be included in the model to prevent an overfitted, unstable model. Cox proportional hazards regression modeling was used to estimate the effect of osteochondroplasty as compared with lavage on the time to reoperation. A test for nonproportional hazards was performed using the approach of cumulative sums of martingale residuals over time as described by Lin et al. 14 A Kolmogorov-Smirnov type of supremum test based on a sample of 1000 simulated residual patterns was then computed. Furthermore, plot testing the proportional hazards assumption with Schoenfeld residuals of each included variable over time was assessed. 24 If the proportionality assumption was not met, the results would be stratified, if appropriate.
The selection of possible covariates for inclusion in the final models was guided by clinical judgment, univariate analyses, and the change-in-estimate criterion. The goodness-of-fit of the models was also compared using the Akaike information criterion (AIC). 1 Given that the treatment group was randomly allocated, the proportions of covariates within each group were expected to be approximately similar. Therefore, covariates were only included in the final model if their inclusion in the model changed the effect size of the treatment group by a cutoff of more than 10%, as per the change-in-estimate criterion. 16 The effects from the Cox model were expressed as a hazard ratio (HR), the corresponding 95% CI, and the associated P value. All tests were 2-sided, with an alpha level of .05.
Sensitivity Analysis
A sensitivity analysis was run to assess the robustness of the outcome findings to possible informative censoring by examining 2 scenarios in the patients who were censored early (before 27 months). The first scenario considered all these patients as not having a reoperation, with a follow-up time (censored) of 27 months. The second scenario considered all these patients as having a reoperation at the median follow-up time. This represents an analysis similar to the best- and worst-case scenario. Another sensitivity analysis assessed the outcome in a Cox model that included prespecified covariates, which were excluded in the final Cox model. A maximum of 2 covariates were included given the 27 events.
Results
Description of Cohort
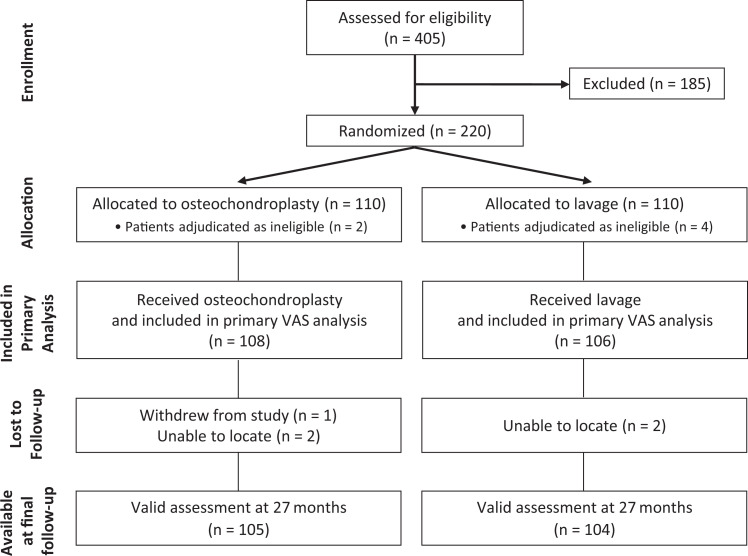
A total of 220 patients with FAI were first enrolled in the study between October 26, 2012, and November 9, 2017. Six patients were later found to be ineligible—2 patients decided against surgery, 2 patients were found to have neither the cam- nor the mixed-type FAI on arthroscopic exploration, 1 patient was older than 50 years, and 1 patient did not undergo documented physical therapy for the hip before surgery—resulting in 108 total patients included in the osteochondroplasty group and 106 patients in the lavage group (Figure 1). Of the total cohort, 212 and 209 patients had a valid assessment at 12 and 27 months, respectively. The reasons for early censoring/loss to follow-up are provided in Figure 1.
Figure 1.
Flow diagram for patients included and those with complete follow-up. VAS, visual analog scale.
The mean age of the patients included in the study was 36 ± 8.5 years (36.7 ± 8.2 years in the osteochondroplasty group and 35.4 ± 8.8 years in the lavage group). The cam-type impingement was reported in 64 patients in the osteochondroplasty treatment group (59.3%) and 61 patients (57.5%) in the lavage group. Overall, the baseline characteristics were well-balanced between treatment groups, with the full details of the patient characteristics/baseline data of the treatment group available in Table 1. A similar proportion of patients in the osteochondroplasty group (20/108 [18.5%]) and the lavage group (20/106 [18.9%]) had a labral resection performed because of a labral tear that was deemed to be unrepairable intraoperatively. Only 1 patient (0.9%) in the osteochondroplasty group required no capsulotomy, while 8 patients (7.5%) in the lavage group had no capsulotomy done. Capsule closure was performed in 33 (30.6%) of patients in the osteochondroplasty group compared with 14 (13.2%) of patients in the lavage group.
Table 1.
Patient and Hip Characteristics a
| Osteochondroplasty (n = 108) | Lavage (n = 106) | Total (N = 214) | |
|---|---|---|---|
| Age, y, mean ± SD | 36.7 ± 8.2 | 35.4 ± 8.8 | 36 ± 8.5 |
| Sex, n (%) | |||
| Male | 66 (61.1) | 67 (63.2) | 133 (62.1) |
| Female | 42 (38.9) | 39 (36.8) | 81 (37.9) |
| Ethnicity, n (%) | |||
| Native | 4 (3.7) | 0 (0) | 4 (1.9) |
| Asian | 3 (2.8) | 4 (3.8) | 7 (3.3) |
| Black | 0 (0) | 3 (2.8) | 3 (1.4) |
| White | 100 (92.6) | 95 (89.6) | 195 (91.1) |
| Mixed race | 1 (0.9) | 4 (3.8) | 5 (2.3) |
| BMI, kg/m2 | |||
| <18.5 | 4 (3.7) | 1 (0.9) | 5 (2.3) |
| 18.5 to <25 | 35 (32.4) | 37 (34.9) | 72 (33.6) |
| 25 to <30 | 46 (42.6) | 31 (29.2) | 77 (36) |
| 30 to <40 | 22 (20.4) | 35 (33) | 57 (26.6) |
| ≥40 | 1 (0.9) | 2 (1.9) | 3 (1.4) |
| Baseline sport activity, n (%) | |||
| None | 22 (20.4) | 18 (17) | 40 (18.7) |
| Light | 28 (25.9) | 31 (29.2) | 59 (27.6) |
| Moderate | 37 (34.3) | 43 (40.6) | 80 (37.4) |
| Vigorous | 21 (19.4) | 14 (13.2) | 35 (16.4) |
| Affected hip | |||
| Left | 46 (42.6) | 50 (47.2) | 96 (44.9) |
| Right | 62 (57.4) | 56 (52.8) | 118 (55.1) |
| Tönnis and Heinecke classification, n (%) | |||
| Grade 0 | 47 (43.5) | 51 (48.1) | 98 (45.8) |
| Grade 1 | 56 (51.9) | 41 (38.7) | 97 (45.3) |
| Grade 2 | 5 (4.6) | 13 (12.3) | 18 (8.4) |
| Grade 3 | 0 (0) | 1 (0.9) | 1 (0.5) |
| Labral tears present, n (%) | |||
| None | 16 (14.8) | 15 (14.2) | 31 (14.5) |
| Anterior only | 78 (72.2) | 84 (79.2) | 162 (75.7) |
| Posterior only | 2 (1.9) | 1 (0.9) | 3 (1.4) |
| Superior/lateral only | 7 (6.5) | 4 (3.8) | 11 (5.1) |
| Anterior and superior/lateral only | 5 (4.6) | 2 (1.9) | 7 (3.3) |
| Impingement subtype from surgical form, n (%) | |||
| Mixed | 44 (40.7) | 45 (42.5) | 89 (41.6) |
| Cam | 64 (59.3) | 61 (57.5) | 125 (58.4) |
| Impingement severity | |||
| Severe | 12 (11.1) | 6 (5.7) | 18 (8.4) |
| Moderate | 54 (50) | 61 (57.5) | 115 (53.7) |
| Mild | 42 (38.9) | 39 (36.8) | 81 (37.9) |
a Table adapted from Ayeni et al. 2 BMI, body mass index.
Incidence of Reoperation
Overall, a total of 27 incident reoperations were identified within 27 months of follow-up (cumulative incidence of 12.6% [N = 214 patients]), with an unadjusted reoperation (person-time) incidence rate of 6 per 100 person-years (Figure 2). All 27 of the reoperations involved revision hip arthroscopy of the ipsilateral hip. The most common indications for reoperation were worsened hip pain (n = 15), reinjury of the labrum (n = 11), and heterotopic ossification (n = 1). Seven patients had a reoperation within 12 months, for an overall first-year incidence of reoperation of 3.3% (95% CI, 1.6%-6.8%). The indications for reoperation within 12 months were similarly worsened hip pain (n = 4) and reinjury of the labrum (n = 3).
Figure 2.

Kaplan-Meier survival plot for time to reoperation.
Within the osteochondroplasty group, a total of 8 incident reoperations were identified within 27 months of follow-up (cumulative incidence, 7.4% [n = 108 patients]), with an unadjusted reoperation (person-time) incidence rate of 3.4 per 100 person-years. Using the 27-month follow-up period of this study, the mean time-to-reoperation within the osteochondroplasty group was 791.5 days (SE, 10.9). Two patients had a reoperation within 12 months for a first-year incidence of reoperation of 1.9% (95% CI, 0.4%-7.3%).
Within the lavage group, a total of 19 incident reoperations were identified within 27 months of follow-up (cumulative incidence, 17.9% [n = 106 patients]), with an unadjusted reoperation (person-time) incidence rate of 8.7 per 100 person-years. Using the 27-month follow-up period of this study, the mean time-to-reoperation within the lavage group was 762.5 days (SE, 13.9). Five patients had a reoperation within 12 months for an overall first-year incidence of reoperation of 4.8% (95% CI, 2%-11.1%). Figure 3 depicts Kaplan-Meier curves stratified by treatment group.
Figure 3.

Kaplan-Meier survival plot for time to reoperation stratified by treatment group.
Model Selection
Univariate Cox analyses for the covariates age (P = .88) and impingement subtype (P = .78) both had nonsignificant results (Table 2). After running univariate analyses, Cox models were run, including the treatment group and each of the covariates under consideration. The AIC values in each of these scenarios were higher than the AIC in the model with the treatment group alone. In each case, the HR for the treatment group was not changed more than 10% with the inclusion of either age or impingement subtype in the model (Table 2). Therefore, the final model included only the treatment group variable as the independent variable with no additional covariates included in the final Cox model.
Table 2.
Summary of Model Selection Results a
| Univariate Analysis Result | Cox Model With Treatment Group | |||
|---|---|---|---|---|
| Covariate | HR (95% CI) | P | Treatment Group HR (95% CI) | Change in AIC vs Treatment Group Alone |
| Age | 1 (0.96-1.05) | .88 | 0.40 (0.17-0.90) | +1.9 |
| Impingement subtype | 1.12 (0.50-2.5) | .78 | 0.40 (0.17-0.91) | +1.9 |
a The first 2 columns represent the results from univariate Cox analyses for each of the assessed covariates. The second 2 columns represent the HR in the treatment group after the addition of each covariate in a Cox model with the treatment group, as well as the change in the AIC from this model compared with the model with the treatment group alone. AIC, Akaike information criterion; HR, hazard ratio.
Assessment of the Model Assumptions
In the assessment of the treatment group variable for the proportional hazards assumption, the Kolmogorov-Smirnov type of supremum test for the proportional hazards assumption yielded a nonsignificant result (P = .350), supporting that the treatment variable satisfies the proportional hazards assumption (Appendix Figure A1). Assessment of the plot of Schoenfeld residuals of the treatment group over time showed that the data centered around zero, again supporting that the treatment variable satisfies the proportional hazards assumption (Appendix Figure A2). Last, on assessment of the interaction of the treatment variable with time within the Cox model, the time interaction term was not significant (P = .38), further supporting that the treatment variable satisfied the proportional hazards assumption.
Effect of Treatment Group on Hazard of Reoperation
For patients with FAI, the hazard of reoperation for patients undergoing osteochondroplasty was 40% of that of patients undergoing lavage (HR, 0.40 [95% CI, 0.17-0.91]; P = .029).
Sensitivity Analysis
On sensitivity analysis of the robustness of the result to possible informative censoring, 2 scenarios were assessed. The first scenario considered none of the early censored individuals to have had an event at 27 months’ follow-up. In this scenario, the hazard of reoperation for patients undergoing osteochondroplasty was 40% of that of patients undergoing lavage (HR, 0.40 [95% CI, 0.17-0.90]; P = .03). The second scenario considered all the early censored individuals to have had an event at the mean survival time. In this scenario, the hazard of reoperation for patients undergoing osteochondroplasty was 49% of that of patients undergoing lavage (HR, 0.49 [95% CI, 0.22-0.99]; P = .05).
Two covariates were considered for inclusion within the sensitivity Cox model: (1) age and (2) impingement subtype, based on clinical rationale. The Kolmogorov-Smirnov type of supremum test for the proportional hazards assumption yielded a nonsignificant result for these 2 covariates (P = .73 and P = .22, respectively). Within the sensitivity analysis of this Cox model, the hazard of reoperation for patients undergoing osteochondroplasty was 40% of that of patients undergoing lavage (HR, 0.40 [95% CI, 0.17-0.91]; P = .03), and the HRs for age (P = .78) and morphology (P = .32) were not significant.
Discussion
The most important finding within this study was that osteochondroplasty resulted in a 2.5-fold decreased hazard of reoperation in patients with FAI compared with lavage with or without labral repair in a time-to-event analysis. The incidence of reoperation in patients undergoing osteochondroplasty was 3.4 per 100 person-years, while that in patients undergoing lavage alone was 8.7 per 100 person-years. Age and morphology subtype had no impact on the hazard of reoperation in patients in this study.
Overall, the cumulative incidence of reoperation of patients included in this study at 27-month follow-up was 12.6%. This rate is almost identical to that reported by Degen et al 5 in 8267 primary hip arthroscopy cases, where the 2-year cumulative reoperation rate was reported as 11.9%. However, the reoperations in that study included both revision hip arthroscopy and total hip replacement. Another study by Gupta et al 10 reported a 2-year cumulative revision hip arthroscopy rate of 7.7%, in addition to a cumulative incidence of reoperation in the form of total hip arthroplasty of 9.1%. Both Degan et al 5 (HR, 2.09) and Malviya et al 17 (HR, 4.65) found that patients aged 50 years and older had a higher risk of reoperation. While the present study did not find any significant association between age and time to reoperation, a strong explanation for this finding would be the exclusion of patients over the age of 50, many of whom will undergo a reoperation in the form of a total hip replacement. While it has previously been reported that patients with labral repair have a lower risk of requiring a reoperation, 5 these findings were not identified within the FIRST trial where 17 of 27 (63%) of patients requiring reoperation had a labral repair compared with 112 of 187 (60%) in those not requiring a reoperation. 2 However, the relatively small number of patients in the reoperation cohort in the FIRST study could be one explanation for this discrepancy. Before the FIRST trial, the effect of osteochondroplasty on the need for revision surgery had not previously been reported.
Continued hip pain and reinjury of the labrum accounted for more than 95% of the reoperations reported in this study, with heterotopic ossification accounting for only 1 reoperation case. A previous study reported that retears of the labrum were present in 86% of hips at the time of revision hip arthroscopy. 18 Another study of revision hip arthroscopy procedures by Philippon et al 20 found that 36 of 37 cases had a residual bony appearance that was either not addressed or deemed to be inadequately resected during the index surgery. Similarly, Ross et al 21 compared postoperative computed tomography scans in patients with successful surgical procedures with patients with continued symptoms and found that 90% of the symptomatic group had residual osseous deformity. In the largest series published to date on patients undergoing revision hip arthroscopy for residual FAI by Larson et al, 13 it was found that 80 of 85 hips (>94%) had residual cam-type deformity. Notably, the study found that more than 70% of hips were found to have new chondral or labral causes at the time of the revision. Furthermore, it has been demonstrated that labral tears rarely occur without underlying bony structural abnormalities, with isolated labral tears identified in only 13% of patients presenting with a tear of the labrum. 26 Therefore, it could be hypothesized that the 2.5-fold higher rate of reoperations in patients not undergoing osteochondroplasty in this study could be caused by residual aberrant bony appearance of the joint as it pertains to the natural history of cartilage breakdown.
The final Cox model used within this study considered the treatment group as an independent variable, with no other covariates included in the model. Although age and impingement subtype were considered for inclusion in the model, none of these variables changed the HR of the treatment group by more than 10% with their inclusion. Furthermore, a sensitivity analysis demonstrated an almost identical result in the HR of the treatment group when covariates were included in the model compared with when no covariates were included. Since patients included in this trial were randomized by treatment group, patients within each treatment group were expected to have approximately equal levels of each covariate. The characteristics data of patients included within this study by treatment group confirmed a relatively equal distribution. Therefore, the need to include only the treatment variable within the Cox model was what might have been expected, given the methodological design of this study. Balancing covariates in each treatment group is one of the major advantages of an RCT over other trial designs.
In the methodology of this study, a Cox proportional hazards model was used with HRs as the primary outcome. This methodology (time-to-event analysis) is preferable over a comparison of the treatment groups at a single point in time (eg, at the conclusion of the study) using a logistic regression. Benefits of the Cox model over analyses that are not time-to-event include the ability to incorporate censored data and prevent random obscuring of the true treatment effect that could occur by looking at only a single time point in an analysis that is not time-to-event. 6 Furthermore, the use of a Cox model was valid in this study as demonstrated via assessment of the proportional hazards assumption.
A limitation of this study included a relatively small sample size (N = 214) and number of events (n = 27) for reoperation as a time-to-event analysis. Although no covariates were included in the final model, a maximum of 2 covariates would have been permitted for inclusion, given the number of events, to prevent an overfitted unstable model. Therefore, a larger sample size would have been preferable to answer the aim of this study from a time-to-event perspective. Alternatively, the follow-up time within this study may have been insufficient to identify the majority of reoperation events. A previous study with a 10-year follow-up has reported that the cumulative incidence of reoperations at 2-year follow-up was only approximately one-half of the ultimate cumulative incidence of reoperations at the final follow-up of 10 years. 5 Further analysis of this study at longer follow-up times would likely yield a larger number of reoperation events for assessment. Furthermore, given the age of patients in this study (<50 years) a longer follow-up time could provide important information with respect to the effect of osteochondroplasty on time to total hip arthroplasty, in addition to the need for revision hip arthroscopy. As we may have expected given their age, no patients in this study underwent hip arthroplasty at 27-month follow-up. Another limitation relates to the relative difference in capsule management across patients in this study, which can affect outcomes after the surgical management of FAI.
Conclusion
This randomized, time-to-event analysis with 27-month follow-up demonstrated that for adults between the ages of 18 and 50 years with FAI, arthroscopic osteochondroplasty was associated with a 2.5-fold decrease in the hazard of reoperation at any point compared with arthroscopic lavage with or without labral repair.
AUTHORS
Jeffrey Kay, MD, MSc (McMaster University, Hamilton, Ontario, Canada); Nicole Simunovic, MSc (McMaster University, Hamilton, Ontario, Canada); Olufemi R. Ayeni, MD, PhD (McMaster University, Hamilton, Ontario, Canada); Mohit Bhandari, MD, PhD (McMaster University, Hamilton, Ontario, Canada); Asheesh Bedi, MD (University of Michigan, University of Michigan, Ann Arbor, Michigan, USA); Teppo Järvinen, MD, PhD (University of Helsinki, Helsinki, Finland); Volker Musahl, MD (University of Pittsburgh, Pittsburgh, Pennsylvania, USA); Douglas Naudie, MD, MSc (University of Western Ontario, London, Ontario, Canada); Matti Seppänen, MD (Turku University, Turku, Finland); Gerard Slobogean, MD (University of Maryland, Baltimore, Maryland, USA); Lehana Thabane, PhD (McMaster University, Hamilton, Ontario, Canada); Andrew Duong, MSc (McMaster University, Hamilton, Ontario, Canada); Matthew Skelly, BSc (McMaster University, Hamilton, Ontario, Canada); Ajay Shanmugaraj, BSc (McMaster University, Hamilton, Ontario, Canada); Sarah Crouch, BSc(Pharm) (McMaster University, Hamilton, Ontario, Canada); Sheila Sprague, PhD (McMaster University, Hamilton, Ontario, Canada); Diane Heels-Ansdell, MSc (McMaster University, Hamilton, Ontario, Canada); Lisa Buckingham, BSc (McMaster University, Hamilton, Ontario, Canada); Tim Ramsay, PhD (Ottawa Hospital Research Institute, Ottawa, Ontario, Canada); John Lee, MD, MSc (University of Toronto, Toronto, Ontario, Canada); Petteri Kousa, MD (Sports Clinic Hospital Dextra); Sasha Carsen, MD (University of Ottawa, Ottawa, Ontario, Canada); Hema Choudur, MD (Hamilton Health Sciences, Hamilton, Ontario, Canada); Yan Sim, MD (McMaster University, Hamilton, Ontario, Canada); Kelly Johnston, MD (University of Calgary, Calgary, Alberta, Canada); Ivan Wong, MD, DipSportsMed, MACM (Dalhousie University, Halifax, Nova Scotia, Canada); Ryland Murphy, BSc (Dalhousie University, Halifax, Nova Scotia, Canada); Sara Sparavalo, MSc (Dalhousie University, Halifax, Nova Scotia, Canada); Daniel Whelan, MD, MSc (Saint Michael’s Hospital, Toronto, Ontario, Canada); Ryan Khan, BA, CCRP (Saint Michael’s Hospital, Toronto, Ontario, Canada); Gavin C.A. Wood, MBChB (Kingston Health Sciences Centre, Kingston, Ontario, Canada); Fiona Howells, BPharm (Kingston Health Sciences Centre, Kingston, Ontario, Canada); Heather Grant, MSc (Kingston Health Sciences Centre, Kingston, Ontario, Canada); Bryn Zomar, MSc (London Health Sciences Centre, London, Ontario, Canada); Michael Pollock, MSc (London Health Sciences Centre, London, Ontario, Canada); Kevin Willits, MD (Fowler Kennedy Sport Medicine Clinic, London, Ontario, Canada); Andrew Firth, MSc (Fowler Kennedy Sport Medicine Clinic, London, Ontario, Canada); Stacey Wanlin, BSc (Fowler Kennedy Sport Medicine Clinic, London, Ontario, Canada); Alliya Remtulla, MSc (Fowler Kennedy Sport Medicine Clinic, London, Ontario, Canada); Nicole Kaniki, PhD (Fowler Kennedy Sport Medicine Clinic, London, Ontario, Canada); Etienne L. Belzile, MD (CHU de Québec–Université Laval, Québec City, Québec, Canada); Sylvie Turmel, RN (CHU de Québec–Université Laval, Québec City, Québec, Canada); Uffe Jørgensen, MD, DrMedSci (Odense University Hospital, Odense, Denmark); Annie Gam-Pedersen, RN (Odense University Hospital, Odense, Denmark); Raine Sihvonen, MD, PhD (Hatanpää Hospital, Tampere, Finland); Marko Raivio Sihvonen, MD (Hatanpää Hospital, Tampere, Finland); Pirjo Toivonen Sihvonen, PT (Hatanpää Hospital, Tampere, Finland); and Mari Pirjetta Routapohja, RN (Turku University Hospital, Turku, Finland).
APPENDIX
Figure A1.

Plot of the Kolmogorov-Smirnov–type supremum test to test the proportional hazards assumption for the treatment variable.
Figure A2.

Plot of the Schoenfeld residuals for the treatment group to assess the proportional hazards assumption.
Footnotes
Final revision submitted May 21, 2021; accepted July 26, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research grants were received from the Canadian Institutes of Health Research (to O.R.A., M.B.); the American Orthopaedic Society for Sports Medicine (to O.R.A.); the Canadian Orthopaedic Foundation (to O.R.A.); McMaster Surgical Associates (to O.R.A.); and Hamilton Health Sciences Department of Surgery (to O.R.A.) for the Femoroacetabular Impingement Randomized controlled Trial. V.M. has received education payments from Arthrex; consulting fees from Smith & Nephew and Stryker; and nonconsulting fees from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hamilton Integrated Research Ethics Board (project No. 12-396).
References
- 1. Akaike H. A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19(6):716–723. doi:10.1109/TAC.1974.1100705 [Google Scholar]
- 2. Ayeni OR, Karlsson J, Heels-Ansdell D, et al. Osteochondroplasty and labral repair for the treatment of young adults with femoroacetabular impingement: a randomized controlled trial. Am J Sports Med. 2021;49(1):25–34. doi:10.1177/0363546520952804 [DOI] [PubMed] [Google Scholar]
- 3. Beck M, Kalhor M, Leunig M, Ganz R, Surgeon O. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi:10.1302/0301-620X.87B7 [DOI] [PubMed] [Google Scholar]
- 4. Cvetanovich GL, Weber AE, Kuhns BD, et al. Hip arthroscopic surgery for femoroacetabular impingement with capsular management: factors associated with achieving clinically significant outcomes. Am J Sports Med. 2018;46(2):288–296. doi:10.1177/0363546517739824 [DOI] [PubMed] [Google Scholar]
- 5. Degen RM, Pan TJ, Chang B, et al. Risk of failure of primary hip arthroscopy—a population- based study. J Hip Preserv Surg. 2017;4(3):214–223. doi:10.1093/jhps/hnx018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Farewell D. Study design and statistical analysis: a practical guide for clinicians. Mitchell H. Katz. Cambridge University Press. ISBN 0521826756 (hardback) ($95.00); ISBN 0521534070 (paperback) ($39.99). J Public Health. 2006;28(4):398. doi:10.1093/pubmed/fdl063 [Google Scholar]
- 7. First Investigators. A multi-centre randomized controlled trial comparing arthroscopic osteochondroplasty and lavage with arthroscopic lavage alone on patient important outcomes and quality of life in the treatment of young adult (18-50) femoroacetabular impingement. BMC Musculoskelet Disord. 2015;16:64. doi:10.1186/s12891-015-0500-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Glynn RJ, Buring JE. Ways of measuring rates of recurrent events. Br Med J. 1996;312:364–367. doi:10.1136/bmj.312.7027.364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen osteoarthritis study. Acta Radiol. 2008;49(4):436–441. doi:10.1080/02841850801935567 [DOI] [PubMed] [Google Scholar]
- 10. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? Am J Sports Med. 2016;44(1):74–82. doi:10.1177/0363546514562563 [DOI] [PubMed] [Google Scholar]
- 11. Haefeli PC, Albers CE, Steppacher SD, Tannast M, Büchler L. What are the risk factors for revision surgery after hip arthroscopy for femoroacetabular impingement at 7-year follow-up? Clin Orthop Relat Res. 2017;475(4):1169–1177. doi:10.1007/s11999-016-5115-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris JD, McCormick FM, Abrams GD, et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29(3):589–595. doi:10.1016/j.arthro.2012.11.003 [DOI] [PubMed] [Google Scholar]
- 13. Larson CM, Giveans MR, Samuelson KM, Stone RM, Bedi A. Arthroscopic hip revision surgery for residual femoroacetabular impingement (FAI). Am J Sports Med. 2014;42(8):1785–1790. doi:10.1177/0363546514534181 [DOI] [PubMed] [Google Scholar]
- 14. Lin DY, Wei LJ, Ying Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80(3):557–572. doi:10.1093/biomet/80.3.557 [Google Scholar]
- 15. Lincoln M, Johnston K, Muldoon M, Santore R. Combined arthroscopic and modified open approach for cam femoroacetabular impingement: a preliminary experience. Arthroscopy. 2009;25(4):392–399. doi:10.1016/j.arthro.2008.12.002 [DOI] [PubMed] [Google Scholar]
- 16. Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138(11):923–936. doi:10.1093/oxfordjournals.aje.a116813 [DOI] [PubMed] [Google Scholar]
- 17. Malviya A, Raza A, Jameson S, James P, Reed MR, Partington PF. Complications and survival analyses of hip arthroscopies performed in the National Health Service in England: a review of 6395 cases. Arthrosc. 2015;31(5):836–842. doi:10.1016/j.arthro.2014.12.013 [DOI] [PubMed] [Google Scholar]
- 18. McCarthy JC, Glassner PJ. Correlation of magnetic resonance arthrography with revision hip arthroscopy. Clin Orthop Relat Res. 2013;471(12):4006–4011. doi:10.1007/s11999-013-3202-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum 2-year follow-up. J Bone Joint Surg Br. 2009;91-B(1):16–23. doi:10.1302/0301-620X.91B1.21329 [DOI] [PubMed] [Google Scholar]
- 20. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35(11):1918–1921. doi:10.1177/0363546507305097 [DOI] [PubMed] [Google Scholar]
- 21. Ross JR, Larson CM, Adeoye O, Adeoyo O, Kelly BT, Bedi A. Residual deformity is the most common reason for revision hip arthroscopy: a three-dimensional CT study. Clin Orthop Relat Res. 2015;473(4):1388–1395. doi:10.1007/s11999-014-4069-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Simunovic N, Heels-Ansdell D, Thabane L, Ayeni OR, FIRST Investigators. Femoroacetabular impingement randomised controlled trial (FIRST): a multi-centre randomized controlled trial comparing arthroscopic lavage and arthroscopic osteochondroplasty on patient important outcomes and quality of life in the treatment of young adults. Trials. 2018;19(1):588. doi:10.1186/s13063-018-2965-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sogbein OA, Shah A, Kay J, et al. Predictors of outcomes after hip arthroscopic surgery for femoroacetabular impingement: a systematic review. Orthop J Sports Med. 2019;7(6):2325967119848982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Therneau TM, Grambsch PM. The Cox model BT: modeling survival data: extending the Cox model. In: Dietz K, Gail M, Krickeberg K, Samet J, Tsiatis A, eds. Statistics for Biology and Health. Springer-Verlag New York; 2000:39–77. [Google Scholar]
- 25. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81(12):1747–1770. doi:10.2106/00004623-199912000-00014 [DOI] [PubMed] [Google Scholar]
- 26. Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150. doi:10.1097/01.blo.0000136903.01368.20 [DOI] [PubMed] [Google Scholar]