Abstract
Background
Staphylococcus aureus (S. aureus) is the leading nosocomial (hospital acquired) pathogen in hospitals throughout the world. Traditionally, control of S. aureus has been focused on preventing cross‐infection between patients, however, it has been shown repeatedly that a large proportion of nosocomial S. aureus infections originate from the patient's own flora. Nasal carriage of S. aureus is now considered a well defined risk factor for subsequent infection in various groups of patients. Local antibiotic treatment with mupirocin ointment is often used to eradicate nasal S. aureus.
Objectives
To determine whether the use of mupirocin nasal ointment in patients with identified S. aureus nasal carriage reduced S. aureus infection rates.
Search methods
For this first update we searched the Cochrane Wounds Group Specialised Register (searched 9 September 2010); The Cochrane Central Register of Controlled Trials (CENTRAL) ‐ The Cochrane Library 2010 Issue 3; Ovid MEDLINE (2007 to September Week 1 2010); Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations, September 10, 2010);Ovid EMBASE (2007 to 2010 Week 36); and EBSCO CINAHL (2007 to 10 September 2010). No language or publication restrictions were applied.
Selection criteria
Randomised controlled trials (RCTs) comparing nasal mupirocin with no treatment or placebo or alternative nasal treatment in the prevention of S. aureus infections in nasal S. aureus carriers were included.
Data collection and analysis
Titles, abstracts and full‐text articles of studies retrieved from the search process were independently assessed by two authors for inclusion. From included studies a data extraction form was made and the quality of the trial was assessed. The primary outcome was the S. aureus infection rate (any site). Secondary outcomes were time to infection, mortality, adverse events and infection rate caused by micro‐organisms other than S. aureus.
Main results
Nine RCTs involving 3396 participants met the inclusion criteria. Patient populations varied and several types of nosocomial S. aureus infection were described including bacteraemia, exit‐site infections, peritonitis, respiratory tract infections, skin infections, surgical site infections (SSI) and urinary tract infections. After pooling the eight studies that compared mupirocin with placebo or with no treatment, there was a statistically significant reduction in the rate of S. aureus infection associated with intranasal mupirocin (RR 0.55, 95% CI 0.43 to 0.70). A planned subgroup analysis of surgical trials demonstrated a significant reduction in the rate of nosocomial S. aureus infection rate associated with mupirocin use (RR 0.55, 95% CI 0.34 to 0.89) however this effect disappeared if the analysis only included surgical site infections caused by S. aureus (RR 0.63, 95% CI 0.38 to 1.04), possibly due to a lack of power. The infection rate caused by micro‐organisms other than S. aureus was significantly higher in patients treated with mupirocin compared with control patients (RR 1.38 95% CI 1.118 to 1.72).
Authors' conclusions
In people who are nasal carriers of S. aureus, the use of mupirocin ointment results in a statistically significant reduction in S. aureus infections.
Plain language summary
Using mupirocin ointment to reduce staphylococcus aureus infection rates in people who are nasal carriers of staphylococcus aureus.
Staphylococcus aureus (S. aureus) is the main hospital acquired pathogen and although the focus has been on preventing cross‐infection between patients, it has been shown that a large number of S. aureus infections start from the patient's own flora. Nasal carriage of S. aureus is a risk factor for infection in hospital patients and using a local antibiotic treatment of mupirocin ointment is often used to eradicate nasal S.aureus. It has been found that if people are nasal carriers of S. aureus then using mupirocin ointment reduces the level of S aureus infections.
Background
Staphylococcus aureus (S. aureus) is the leading nosocomial (hospital acquired) pathogen in hospitals throughout the world. Infection with S. aureus is associated with substantial morbidity and mortality ‐ a trend that is increasing due to the widespread dissemination of meticillin‐resistant S. aureus (MRSA) (NNIS 2004). MRSA is not more pathogenic (disease‐causing) than S. aureus, but therapy is more problematic.
Staphylococcal infections occur regularly in hospitalised patients and can have severe consequences including postoperative wound infections, nosocomial pneumonia, and catheter‐related bacteremia (bacteria in the blood that can cause disease, e.g. endocarditis, elsewhere in the body) (Kaplowitz 1988; Kluytmans 1995; Kluytmans 1997; Yu 1986; Yzerman 1996). A recent study of over seven million hospital admissions in the US estimated that 0.8% of all patients suffered from infection with S. aureus, corresponding to a total of nearly 300,000 patients in US hospitals in 2003. After controlling for confounders the annual impact in the US was estimated to be 2.7 million additional days in hospital, US$9.5 billion excess costs, and at least 12,000 in‐patient deaths (Noskin 2005). Since the consequences of these infections are immense, effective prevention strategies are essential.
Traditionally, control of S. aureus has been focused on preventing cross‐infection between patients (Pittet 2000), however, it has been shown repeatedly that a large proportion of nosocomial S. aureus infections originate from patients' own flora (non‐pathogenic bacteria normally present on the patient) (Kluytmans 1995; Von Eiff 2001; Wertheim 2004a). Nasal carriage (presence in the nose) of S. aureus is now considered a well defined risk factor for subsequent infection in various groups of patients, including those on dialysis; with cirrhosis of the liver; undergoing surgery; and with intravascular devices or in intensive care (Kluytmans 1997; Mangram 1999).
Three approaches to the elimination of S. aureus carriage are available: local application of antibiotics or antiseptics; administration of systemic antibiotics; and the harnessing of bacterial interference through active culture of a minimally‐pathogenic strain of S. aureus (bacterial interference is the term given to the effect that different micro‐organisms can have on each other when they are present simultaneously). This interference can result in partial or complete inhibition of one micro‐organism ‐ desired in this case ‐ though sometimes activity may be increased. The first strategy, namely local application of antibiotics or antiseptics is the most common, for example mupirocin nasal ointment, applied twice daily for five days, is particularly highly used. Mupirocin can be used for the eradication of both meticillin sensitive and meticillin resistant S. aureus, although MRSA resistance for mupirocin has been shown (Henkel 1999).
Objectives
To determine whether mupirocin nasal ointment reduces rates of S. aureus infection in patients who are nasal carriers of S. aureus.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) irrespective of language or publication status.
Types of participants
Studies of nasal carriers (identified by microbiological culture) of S. aureus (both meticillin‐resistant and meticillin‐sensitive) that are using hospital services (either as inpatient or outpatient) were included. We included studies of patients from any population, gender and age.
Types of interventions
Trials in which participants were randomly allocated intranasal mupirocin ointment or an alternative were included. Eligible control group treatments were placebo, no treatment or alternative topical treatment. We excluded studies that had systemic antibiotics or active colonization as a comparator.
Types of outcome measures
Primary outcomes
S. aureus infection rate ‐ determined according to well‐defined criteria (for example Centers for Disease Control (CDC) guidelines). The infection rate consists of the number of infected patients per study group. Infection caused by both meticillin‐resistant and meticillin‐sensitive S. aureus was included.
Secondary outcomes
Where reported, the following outcomes were recorded:
Time to infection.
Mortality.
Adverse events.
Infection rate caused by other micro‐organisms than S. aureus
Search methods for identification of studies
For details of the search methods used in the original version of this review please see Appendix 1
Electronic searches
For this first update we searched the following electronic databases for relevant trial reports:
Cochrane Wounds Group Specialised Register (searched 9 September 2010);
The Cochrane Central Register of Controlled Trials (CENTRAL) ‐ The Cochrane Library 2010 Issue 3;
Ovid MEDLINE (2007 to September Week 1 2010);
Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations, September 10, 2010);
Ovid EMBASE (2007 to 2010 Week 36);
EBSCO CINAHL (2007 to 10 September 2010)
The following search strategy was used for CENTRAL and modified, where appropriate, for other databases: #1 MeSH descriptor Mupirocin explode all trees #2 mupirocin #3 bactroban #4 centany #5 eismycin #6 plasimine #7 pseudomonic acid #8 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7) #9 MeSH descriptor Staphylococcus aureus explode all trees #10 MeSH descriptor Staphylococcal Infections explode all trees #11 staphylococ* #12 "S aureus" #13 (#9 OR #10 OR #11 OR #12) #14 (#8 AND #13)
The search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found in Appendix 2, Appendix 3 and Appendix 4 respectively. The MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximizing version (2008 revision); Ovid format (Lefebvre 2009). The EMBASE and CINAHL searches were combined with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2008). There was no restriction made on the basis of language or publication status.
Searching other resources
Citation lists from the studies identified by the above methods were searched.
Data collection and analysis
Selection of studies
Titles and abstracts of studies retrieved by the search were independently assessed by two review authors (JK, MvR) for their eligibility for inclusion in the review. Studies that were clearly ineligible were discarded. Full versions of all potentially relevant studies were obtained and independently assessed for inclusion by two review authors. Disagreements were resolved by discussion or by reference to a third review author (MB). When more than one published report of a trial existed, all publications were considered and maximal data were extracted however, only a single set of data was used in any meta‐analysis. If data were missing from reports, then attempts were made to contact the study authors to obtain the missing information.
Data extraction and management
Types of information and data extracted included the following:
Study authors.
Year of publication.
Country where study performed.
Study design (RCT).
Patient population.
Baseline characteristics of participants per treatment group (gender, age, and prevalence of co‐morbidity such as diabetes).
Length, dose and timing of mupirocin treatment.
Methods used for identifying micro‐organisms.
Criteria used for identifying infections / definition of infection used.
Withdrawals (per group with numbers and reasons).
Numbers of S. aureus nasal carriers in mupirocin and placebo treated patients.
Number of nosocomial S. aureus infections among mupirocin and placebo treated patients.
Healthcare setting.
Adverse events.
Assessment of risk of bias in included studies
The quality of the included studies was assessed independently by JK and MvR without blinding to authorship or journal using the criteria described below. The results of the validity criteria were summarised in a table and taken into account in the conclusions and discussion.
Quality checklist All included trials were assessed for quality using a quality checklist that considered the following points:
1. Allocation concealment Trials were awarded the following grades for allocation concealment: A = Adequate: a randomisation method described that would not allow an investigator/participant to know or influence an intervention group before an eligible participant entered the study. B = Unclear: trial states that it is 'randomised', but no information on the method used is available. C = Inadequate: inadequate method of randomisation used, such as alternate medical record numbers or unsealed envelopes; or any information in the study that indicated that investigators or participants could influence the intervention group.
2. Blinding The following points were graded as 'yes' for present, 'no' for absent, and 'not stated' if the relevant information is not stated in the trial report: a. Blinding of investigators. b. Blinding of participants. c. Blinding of outcome assessor. d. Blinding of data analysis. The above was considered not to have been blinded if the treatment group can be identified in > 20% of participants because of any side effects of the treatment.
3. Intention‐to‐treat analysis: This evaluated whether participants were analysed in the groups to which they were originally randomised, and was graded as: Yes ‐ specifically stated by authors that intention‐to‐treat analysis was undertaken, and this was confirmed on study assessment. Yes ‐ not specifically stated, but confirmed on study assessment. No ‐ not reported, and lack of intention‐to‐treat analysis confirmed on study assessment. (Patients who were randomised were not included in the analysis because they did not receive the study intervention, they withdrew from the study or were not included because of protocol violation) No ‐ stated, but not confirmed upon study assessment. Not stated.
4. Completeness of follow up Percentage of participants excluded or lost to follow up was recorded.
Data synthesis
Primary and secondary outcomes of the studies were analysed for each study individually, and, where appropriate combined across studies.
Infection rates and mortality were expressed as relative risk (RR) with 95% confidence intervals (CI). In the first instance, data from all studies were pooled in a forest plot using the random‐effects model. Levels of heterogeneity were analysed using the chi‐square test and the I2 statistic (Higgins 2002; Higgins 2003). Values of I2 over 50% indicate a substantial level of heterogeneity. If heterogeneity over 50% was detected the studies were presented in a narrative summary.
It was planned to analyse time to event data as hazard ratios, pooling where appropriate.
Subgroup analysis and investigation of heterogeneity
Subgroup analyses were planned where obvious differences existed between the included study groups; these differences might have existed in the following variables: age, healthcare setting (for example surgical compared with non surgical), or length, timing, and dose of treatment. The performed subgroup analyses were based on healthcare setting, i.e. subgroup analyses were performed for surgical patients and for dialysis patients. No other subgroup analyses were performed because no obvious differences existed in age, or length, timing, and dose of treatment.
Results
Description of studies
Results of the search
The search for the original review resulted in 217 hits. 193 of these were excluded after reading the abstracts. Full‐text assessment of 24 potentially eligible papers identified 9 eligible RCTs reported in 12 publications (Boelaert 1989; Garcia 2003; Harbarth 1999; Kalmeijer 2002; Konvalinka 2006; Mup Study Group 1996; Pérez‐Fontan 1992; Perl 2002; Wertheim 2004b, see Characteristics of included studies). Twelve papers did not meet the inclusion criteria (see Characteristics of excluded studies). The search for this first update resulted in 42 citations, 3 studies are currently awaiting assessment (Bode 2010; Golan 2010; Jabbour 2010) pending retrieval of full text.
Included studies
Nine RCTs were included in this review.
PATIENT POPULATIONS
The nine included trials (Boelaert 1989; Garcia 2003; Harbarth 1999; Kalmeijer 2002; Konvalinka 2006; Mup Study Group 1996; Pérez‐Fontan 1992; Perl 2002; Wertheim 2004b) described different patient populations. Four trials (Garcia 2003; Kalmeijer 2002; Konvalinka 2006; Perl 2002) described surgical patients (cardiac, orthopaedic, general, gynaecological or neurological surgery), three trials described dialysis patients (two trials of continuous ambulatory peritoneal dialysis (CAPD) (Mup Study Group 1996; Pérez‐Fontan 1992) and one haemodialysis (Boelaert 1989)), one trial (Wertheim 2004b) non surgical patients and one trial confined itself to people colonised with MRSA (Harbarth 1999). The mean age of patients treated with mupirocin varied from 50.7 years (Perl 2002) to 82.0 years (Harbarth 1999). In the control group the mean age ranged between 48.0 (Pérez‐Fontan 1992) and 74.0 years (Harbarth 1999). Seven studies reported that no statistically significant differences existed between the patient characteristics at baseline, i.e. age, sex and underlying disease, between the treatment and control group (Boelaert 1989; Garcia 2003; Harbarth 1999; Kalmeijer 2002; Mup Study Group 1996; Pérez‐Fontan 1992; Wertheim 2004b). Konvalinka found COPD was more prevalent in the mupirocin group (p<0.01) and Perl noted that patients receiving placebo were more likely to have had a renal disease (p=0.04). The number of included patients varied significantly between the included studies (Characteristics of included studies), i.e. Pérez‐Fontan included 11 patients in the mupirocin treatment group, while Wertheim included 793 patients in this group. Garcia 2003; Kalmeijer 2002; and Perl 2002 included both S. aureus nasal carriers and non‐carriers. Data for carriers only were extracted for this review. The other trials included carriers only. In total, 1690 patients with nasal carriage were treated with mupirocin and 1706 patients were allocation to control groups, i.e. they received placebo, no treatment or nasal neomycin.
INTERVENTIONS
In all 9 trials mupirocin ointment was given intranasally to S. aureus carriers. In the surgical trials patients received mupirocin pre‐operatively (Garcia 2003; Kalmeijer 2002; Konvalinka 2006; Perl 2002). In seven trials control patients were treated with a placebo (Boelaert 1989; Harbarth 1999; Kalmeijer 2002; Konvalinka 2006; Mup Study Group 1996; Perl 2002; Wertheim 2004b) . Garcia gave the control group no treatment. Pérez‐Fontan compared mupirocin with nasal neomycin. The application of mupirocin varied from twice daily for 5 days in surgical patients to thrice daily for two weeks and subsequent three times weekly for a total of nine months in hemodialysis patients and twice daily for 5 days and every four weeks for a maximum of 18 months in CAPD patients.
OUTCOMES
The primary outcome of S. aureus infection rate was reported in all nine papers. The secondary outcomes reported varied between the papers. Time to infection was described in one paper (Wertheim 2004b). Mortality was described in five papers (Boelaert 1989; Mup Study Group 1996; Perl 2002; Wertheim 2004b; Konvalinka 2006). Six papers described the adverse events (Boelaert 1989; Konvalinka 2006; Mup Study Group 1996; Pérez‐Fontan 1992; Perl 2002; Wertheim 2004b) and the infection rate caused by other micro‐organisms than S. aureus was described in four papers (Konvalinka 2006; Mup Study Group 1996; Pérez‐Fontan 1992; Perl 2002).
Excluded studies
Twelve papers did not meet the inclusion criteria (Characteristics of excluded studies). The main reasons for exclusion were that the research described was not an RCT; that the study evaluated skin rather than nasal mupirocin, that the study reported elimination rather than infection data or that the intervention involved a combination of several interventions.
Risk of bias in included studies
The methodological quality of the included studies varied from high to low quality. Seven (Boelaert 1989; Harbarth 1999; Kalmeijer 2002; Konvalinka 2006; Mup Study Group 1996; Perl 2002; Wertheim 2004b) out of nine studies were double‐blind RCTs; and in four (Kalmeijer 2002; Konvalinka 2006; Perl 2002; Wertheim 2004b) out of these all other quality indicators, i.e. blinding, intention‐to‐treat, description of loss of follow‐up, were also met. These four studies were classified as studies of high quality. Although not specified in the protocol we judged studies to be of high quality if they concealed allocation, undertook blinding and an ITT analysis. Two out of nine studies were of low quality (Garcia 2003; Pérez‐Fontan 1992). Although not specified in the protocol we judged studies to be of low quality if they did not conceal allocation or if the method of allocation was unclear, no blinding was achieved or reported and an ITT analysis was not reported or confirmed.The allocation concealment of Garcia was inadequate because they used consecutive numbers, patients with even numbers were allocated to the treatment group and patients with odd numbers were control patients. In this study no placebo was used, so the study was not double‐blind. A sensitivity analysis removing the unblinded study of Garcia was undertaken, although this was not pre specified in the protocol. Pérez‐Fontan did not describe any blinding. This trial was analysed separately for all outcomes because they compared mupirocin with neomycin ointment, whilst all the other studies compared mupirocin with placebo or no treatment. Seven of nine studies performed an a priori sample size calculation based on the estimated infection rate in the control group and the aimed reduction rate in the treatment group (Garcia 2003; Harbarth 1999; Kalmeijer 2002; Konvalinka 2006; Mup Study Group 1996; Perl 2002; Wertheim 2004b).
1.
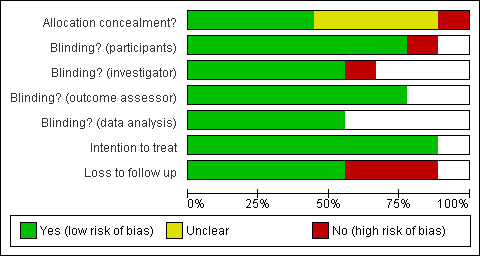
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
2.
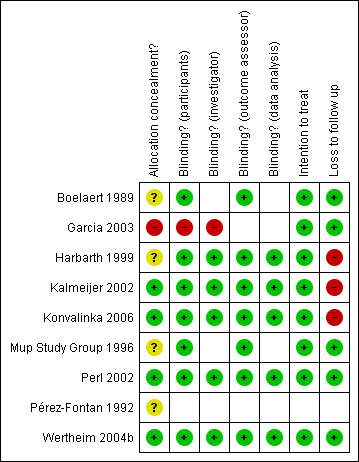
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Effects of interventions
In total, 1690 patients with nasal carriage were treated with mupirocin and 1706 patients were control patients, i.e. they received placebo, no treatment or nasal neomycin.
Comparison 1: Mupirocin compared with placebo or no treatment
Primary outcome S. aureus infection rate (8 RCTs, 3374 participants)
In seven studies (Boelaert 1989; Harbarth 1999; Kalmeijer 2002; Konvalinka 2006; Mup Study Group 1996; Perl 2002; Wertheim 2004b) control patients were treated with placebo and in one study control patients did not receive any treatment (Garcia 2003). Harbarth reported the infection rate caused by meticillin‐resistant S. aureus, while the other studies reported the overall S. aureus infection rate caused by both meticillin‐sensitive and meticillin‐resistant S. aureus.
Looking at individual study results, two trials (Mup Study Group 1996; Perl 2002) showed a significant effect of mupirocin on reducing the S. aureus infection rate, whilst the remaining trials found no significant difference between mupirocin and control. Pooling the eight studies (I2 = 3%) demonstrated a statistically significant reduction in S. aureus infection rate associated with mupirocin (RR 0.55 95% CI 0.43 to 0.70, fixed‐effect) (Analysis 1.1). Whilst there was little or no statistical heterogeneity in this analysis, the trials included diverse patient populations comprising surgical patients, non‐surgical patients and both haemodialysis and CAPD patients. This diversity of patient populations was also demonstrated in the range of types of S. aureus infections reported (bacteraemia, exit‐site infections, episodes of peritonitis, respiratory tract infections, skin infections, surgical site infections (SSI) and urinary tract infections).
1.1. Analysis.
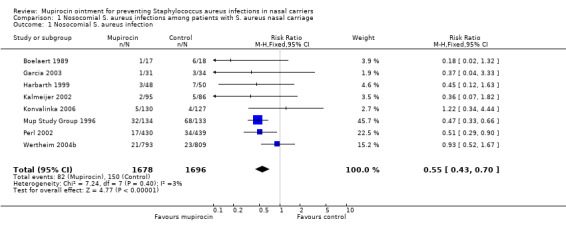
Comparison 1 Nosocomial S. aureus infections among patients with S. aureus nasal carriage, Outcome 1 Nosocomial S. aureus infection.
Pooling together only those studies which were judged to be of high quality, (i.e. studies meeting all quality criteria) (Kalmeijer 2002; Konvalinka 2006; Perl 2002; Wertheim 2004b), also demonstrated a statistically significant reduction in S. aureus infection rate associated with mupirocin (RR 0.69 95% CI 0.47 to 1.00, fixed‐effect) (Analysis 1.2).
1.2. Analysis.
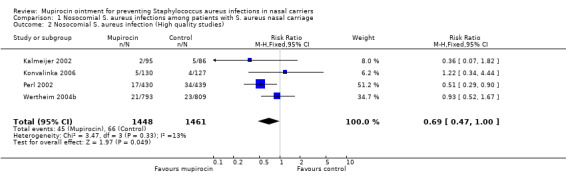
Comparison 1 Nosocomial S. aureus infections among patients with S. aureus nasal carriage, Outcome 2 Nosocomial S. aureus infection (High quality studies).
We pre‐specified in the protocol our plans to investigate whether there were differential effects of mupirocin in different groups, particularly surgical and non‐surgical patients. Four trials (Garcia 2003; Kalmeijer 2002; Konvalinka 2006; Perl 2002) were confined to surgical patients and involved 686 patients in the treatment and 686 in the control group. These trials were pooled (I2 = 0%, fixed‐effect) and showed a statistically significant reduction of the nosocomial S. aureus rate (RR 0.55 95% CI 0.34 to 0.88)(Analysis 2.1). This significant reduction was not affected by the exclusion of the low quality, non‐blinded study (Garcia 2003) (RR 0.56 95% CI 0.34 to 0.91)(Analysis 2.2). When the analysis was confined to the outcome of S. aureus surgical site infection (this analysis was not pre‐specified and therefore can only be described as exploratory) there was no longer a statistically significant effect of mupirocin however the comparison probably lacks statistical power (4 trials, 688 patients treated with mupirocin, 686 control patients, RR 0.63 95% CI 0.38 to 1.04)(Analysis 2.3).
2.1. Analysis.
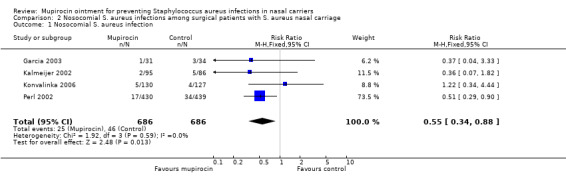
Comparison 2 Nosocomial S. aureus infections among surgical patients with S. aureus nasal carriage, Outcome 1 Nosocomial S. aureus infection.
2.2. Analysis.
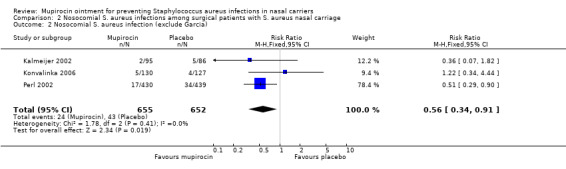
Comparison 2 Nosocomial S. aureus infections among surgical patients with S. aureus nasal carriage, Outcome 2 Nosocomial S. aureus infection (exclude Garcia).
2.3. Analysis.
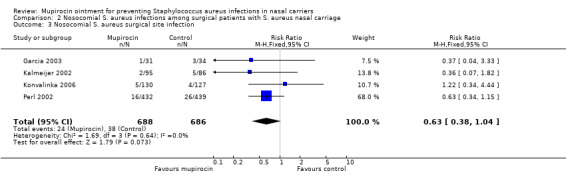
Comparison 2 Nosocomial S. aureus infections among surgical patients with S. aureus nasal carriage, Outcome 3 Nosocomial S. aureus surgical site infection.
A further subgroup analysis in dialysis patients (which was not pre‐specified in the protocol and can only be regarded as exploratory) (2 trials (Boelaert 1989; Mup Study Group 1996)(n = 151 mupirocin, 151 control) showed a statistically significant reduction in the overall S. aureus infection rate associated with mupirocin (fixed‐effect, I2 = 0%, RR 0.44, 95% 0.32 to 0.62)(Analysis 3.1).
3.1. Analysis.
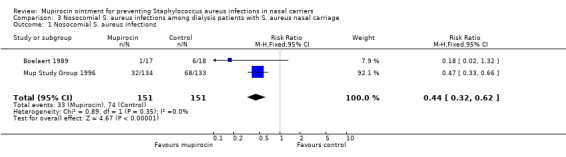
Comparison 3 Nosocomial S. aureus infections among dialysis patients with S. aureus nasal carriage, Outcome 1 Nosocomial S. aureus infections.
Comparison 2: Mupirocin compared with neomycin
Primary outcome S. aureus infection rate (1 RCT, 22 participants)
Pérez‐Fontan compared mupirocin with topical neomycin. During the study period one catheter‐related infection was caused by S. aureus in the mupirocin group (n=12) and two S aureus infections were identified in the neomycin group (n=10); one case of peritonitis and one case of catheter‐related infection. There was no statistically significant difference in rates of S. aureus infection between these two treatment groups, however this study was underpowered to detect anything other than extremely large treatment effects (RR 0.42 95% CI 0.04 to 3.95)(Analysis 4.1).
4.1. Analysis.
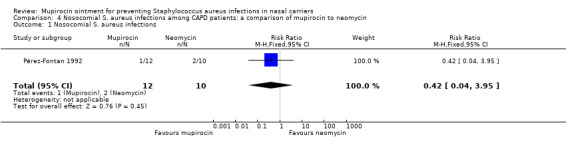
Comparison 4 Nosocomial S. aureus infections among CAPD patients: a comparison of mupirocin to neomycin, Outcome 1 Nosocomial S. aureus infections.
Comparisons 1 and 2: Secondary outcomes
Time to infection
Wertheim 2004b described the median time between treatment and development of S. aureus infection. Analysis of time to infection of patients from the intention‐to‐treat analysis showed no difference between the groups (mupirocin: 25 days, placebo: 12 days, p=0.28 in Mann‐Whitney test). This result should be treated with caution as the authors did not undertake an appropriate analysis for time to event‐type data (i.e. log‐rank rest or Cox proportional hazards regression model).
Mortality
Five trials reported mortality (Boelaert 1989; Konvalinka 2006; Mup Study Group 1996; Perl 2002; Wertheim 2004b) . However, Perl reported mortality in both carriers and non‐carriers, separate data on carriers were not available, so this study was not included in the mortality analysis. There was no statistically significant difference in mortality between treated and untreated carriers (RR 0.91 95% CI 0.64 to 1.31)(Analysis 5.1). Only one study described whether mortality was from any cause or due to an infection (Konvalinka 2006). In the placebo group two of the five deaths were from an infection, i.e. one death was related to a surgical site infection caused by S. aureus and one to pneumonia escalating to multi‐organ failure. None of the four deaths in the mupirocin group were due to infections. Perl stated that no deaths were attributed to mupirocin therapy.
5.1. Analysis.
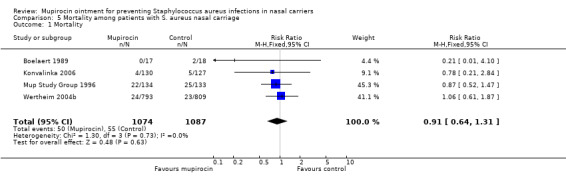
Comparison 5 Mortality among patients with S. aureus nasal carriage, Outcome 1 Mortality.
Adverse Events
Six studies reported data about adverse events due to mupirocin (Boelaert 1989; Pérez‐Fontan 1992; Konvalinka 2006; Mup Study Group 1996; Perl 2002; Wertheim 2004b). Boelaert and Konvalinka reported that no side effects occurred in any of the 35 and 257 participants, respectively. Pérez‐Fontan described slight nasal pruritus and an unpleasant smell immediately after administration of mupirocin (number of patients was not described). In the trial of the Mupirocin Study Group side effects were infrequent and mild, being equally common in treatment and placebo groups, and only a few patients were unable to tolerate the ointment (number of patients was not described). Perl reported the number of adverse events in both carriers and non‐carriers. Data for carriers only were not available. 97 of the 2012 patients in the mupirocin group (4.8%) and 96 of the 2018 patients in the placebo group (4.8%) showed side effects such as rhinorrhea and itching at the application site. Five patients (one treated with mupirocin and four with placebo) withdrew from the study because of adverse events such as nasal burning, nasal bleeding, and headache. Perl stated that no deaths were attributed to mupirocin therapy. Wertheim mentioned 4 patients with an itching or burning sensation of the nose, of which 2 patients received mupirocin (n=793) and 2 placebo (n=809). No serious adverse events were observed or reported.
Infection rate caused by micro‐organisms other than S. aureus
Four studies described the infection rate caused by micro‐organisms other than S. aureus (Mup Study Group 1996; Pérez‐Fontan 1992; Perl 2002; Konvalinka 2006). Data from the Mup Study Group, Perl and Konvalinka were pooled. Pérez‐Fontan was analysed separately because the control group was treated with neomycin.
Pooling three trials (Konvalinka 2006; Mup Study Group 1996; Perl 2002) showed significantly more infections caused by other micro‐organisms in the mupirocin group (RR 1.38 95% CI 1.11 to 1.72)(Analysis 6.1). These infections were caused by both gram‐positive and gram‐negative micro‐organisms, i.e. CNS, Streptococcus pneumoniae, Enterobacter cloacae, Klebsiella pneumoniae, Pseudomonas aeruginosa. (Konvalinka 2006; Mup Study Group 1996; Pérez‐Fontan 1992). There was no difference between both treatment groups in prevalence of gram‐positive or gram‐negative micro‐organisms (RR 0.88 95% CI 0.55 to 1.41 and RR 1.65 95% CI 0.78 to 3.47)(Analysis 6.2; Analysis 6.3).
6.1. Analysis.
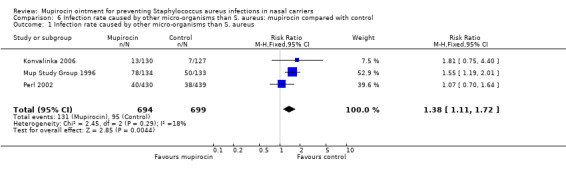
Comparison 6 Infection rate caused by other micro‐organisms than S. aureus: mupirocin compared with control, Outcome 1 Infection rate caused by other micro‐organisms than S. aureus.
6.2. Analysis.
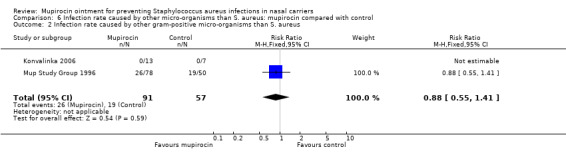
Comparison 6 Infection rate caused by other micro‐organisms than S. aureus: mupirocin compared with control, Outcome 2 Infection rate caused by other gram‐positive micro‐organisms than S. aureus.
6.3. Analysis.
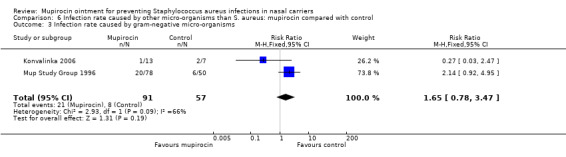
Comparison 6 Infection rate caused by other micro‐organisms than S. aureus: mupirocin compared with control, Outcome 3 Infection rate caused by gram‐negative micro‐organisms.
Pérez‐Fontan found that 7 of the 8 infections in the mupirocin group (n=12) were caused by other micro‐organisms compared with 3 of the 5 infections in the neomycin group (n=10) (RR 1.33 95% CI 0.64 to 2.79)(Analysis 7.1).
7.1. Analysis.
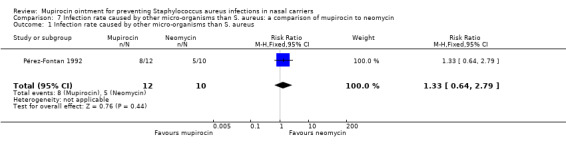
Comparison 7 Infection rate caused by other micro‐organisms than S. aureus: a comparison of mupirocin to neomycin, Outcome 1 Infection rate caused by other micro‐organisms than S. aureus.
Discussion
REDUCTION OF S. AUREUS INFECTIONS BY APPLICATION OF MUPIROCIN
Previously, several reviews in this area have been performed but these included both carriers and non‐carriers of S. aureus (Kallen 2005; Laupland 2003; Strippoli 2004; Trautmann 2008). Strippoli 2004 evaluated the use of different antimicrobial approaches to prevent peritonitis in peritoneal dialysis patients. Nasal mupirocin compared with placebo significantly reduced the exit‐site and tunnel infection rate but not peritonitis rate. Kallen 2005 found no significant effect of mupirocin on the surgical site infection rate after general surgery. However, in non general surgery (cardiothoracic surgery, orthopedic surgery, neurosurgery) a significant reduction was found. In contrast, Trautmann concluded that mupirocin prophylaxis did not reduce the S. aureus surgical site infection rate in patients undergoing orthopedic, gastrointestinal, and cardiothoracic surgery. Laupland 2003 reported that prophylactic treatment of patients with intranasal mupirocin in large trials did not lead to a significant reduction in the overall rate of infections. However, subgroup analyses and several small studies revealed lower rates of S. aureus infection among selected populations of patients with nasal carriage treated with mupirocin. Our review is the first one that included nasal S. aureus carriers only. Nasal mupirocin ointment reduced the overall S. aureus infection rate in nasal carriers. This analysis included surgical patients, non surgical patients and dialysis patients. Subgroup analysis revealed a significant effect in dialysis patients and surgical patients. When the surgical site infections were analysed as primary outcome in surgical patients, no statistically significant effect was found.
SECONDARY OUTCOMES
Wertheim did not find a significant difference in number of infections between non surgical patients treated with mupirocin or placebo, but they reported a significantly longer time to infection in the per‐protocol analysis of patients treated with mupirocin (p=0.02). So, possibly mupirocin protects patients from getting infected for the first period after treatment. However, this outcome was only reported in one study and no significance was found in their intention‐to‐treat analysis, although they did not use the correct statistical analysis. The mortality between mupirocin and control groups was not significantly different and no serious adverse events were mentioned. Analysis of the infection rate caused by micro‐organisms other than S. aureus showed significant more infections caused by other micro‐organisms in the mupirocin group (RR 1.38 95% CI 1.11 to 1.72). It is possible that infections with other micro‐organisms replace the infections caused by S. aureus. Maybe by reducing the S. aureus carriage, it makes someone more susceptible to other micro‐organisms. More research in this field is required.
DEVELOPMENT OF RESISTANCE
Up till now routine use of mupirocin has not been applied in many hospitals, mainly because due to concern about the development of mupirocin resistance and the absence of convincing evidence that mupirocin reduces the infection rate. Resistance has been observed when mupirocin was used for prolonged periods, especially when it was used as a skin ointment (Hudson 1994). However, Fawley 2006 observed no trend towards increasing prevalence of mupirocin resistance during a 4‐year study period with mupirocin use in surgical patients. In our review, five studies reported that no development of resistance to mupirocin in the isolated S. aureus strains was found during the study period (Boelaert 1989; Kalmeijer 2002; Konvalinka 2006; Pérez‐Fontan 1992; Wertheim 2004b). During the 4‐year study Perl found 6 of the 1021 tested S. aureus isolates were resistant to mupirocin. In the study of Harbarth 4 strains acquired low‐level mupirocin resistance during mupirocin therapy. The Mup Study Group showed that low‐level and high‐level resistance occurred in both groups, but there was no evidence that treatment with mupirocin resulted in colonisation with resistant S. aureus. It can be concluded that mupirocin resistance will not be a problem after short‐term intranasal use in surgical or dialysis patients.
ENDOGENOUS INFECTIONS
Mupirocin is applied to prevent patients infecting themselves with endogenous bacteria and therefore, although this was not prespecified in the protocol, it is interesting to know how many of the infections were caused by the endogenous strain. Included studies mentioned that in about 80% of the infections the S. aureus strain isolated from the nares was identical to that isolated from the infected site (Boelaert 1989; Perl 2002; Wertheim 2004b). They did not describe the number of endogenous infections in the mupirocin and placebo groups separately, so it was impossible to analyse the difference in the number of endogenous infections between both groups. Probably, in both the mupirocin and control group there will be a comparable number of infections caused by strains from the environment, for example from the health care workers in the operation room, while a higher number of endogenous infections is expected to be found in the control group. Kalmeijer described fewer endogenous infections in the mupirocin group, but this was not statistically significant (RR 0.19 95% CI 0.02 to 1.62). However, in this analysis both carriers and non‐carriers were included. When patients treated with mupirocin develop an infection with the nose strain, it can be assumed that mupirocin treatment failed. Nasal carriage is eliminated in about 80% of patients treated with mupirocin and 30% in those treated with placebo (Kalmeijer 2002; Konvalinka 2006; Perl 2002). The number of endogenous infections was not prespecified in our protocol, but should be considered in future studies/reviews.
LIMITS
There are several limitations of the included studies and the review. The quality of the studies varied from high to low quality, i.e. only four of the nine included studies were studies of high quality (Kalmeijer 2002; Konvalinka 2006; Perl 2002; Wertheim 2004b). Second, the primary outcomes were reported by all studies, but there was limited information for some of the secondary outcomes, i.e. time to infection was described in one of the nine included studies (Wertheim 2004b), mortality in 5 studies (Boelaert 1989; Konvalinka 2006; Mup Study Group 1996; Perl 2002; Wertheim 2004b), adverse events in 6 studies (Boelaert 1989; Konvalinka 2006; Pérez‐Fontan 1992; Mup Study Group 1996; Perl 2002; Wertheim 2004b) and the infection rate caused by other micro‐organisms than S. aureus in 4 studies (Konvalinka 2006; Mup Study Group 1996; Pérez‐Fontan 1992; Perl 2002). Third, the possibility of publication bias was not assessed in the review. It is likely that studies without a significant reduction of the infection rate are harder to publish than studies with a significant effect. Fourth, although no statistical heterogeneity was found, a lot of clinical heterogeneity existed between patient populations of the included studies. Furthermore, we assessed the S. aureus infection rate as primary outcome, i.e. both meticillin‐susceptible and meticillin‐resistant S. aureus infections were included. Only one study assessed the number of meticillin‐resistant infections (Harbarth 1999), so no subgroup analysis could be performed to study the effect of mupirocin on the infection rate caused by meticillin‐resistant S. aureus in patients with nasal carriage of this variant of S. aureus.
Authors' conclusions
Implications for practice.
Up till now routine use of mupirocin has not been applied in many hospitals, mainly due to concern about the development of mupirocin resistance and the absence of convincing evidence that mupirocin reduces the infection rate. Short‐term use of intranasal mupirocin ointment does not seem to be associated with resistance. Intranasal mupirocin should be considered for use in proven nasal carriers of S. aureus in hospitalised surgical, dialysis and non surgical patient groups at risk of infection.
Implications for research.
This review shows that the effectiveness of mupirocin is related to carriers only. Recent technological advances in rapid diagnostics have provided the ability to detect nasal carriage of S. aureus within hours rather than days (Francois 2003; Paule 2004), which makes it possible to treat nasal carriers rapidly. At the moment, rapid tests that can discriminate MRSA from MSSA are being evaluated. Application of these tests will result in timely, appropriate prescription of anti microbials (both local and systemic).
What's new
| Date | Event | Description |
|---|---|---|
| 14 January 2011 | New search has been performed | new search, 3 studies awaiting assessment (Bode 2010; Golan 2010; Jabbour 2010), no change to conclusions. |
History
Protocol first published: Issue 4, 2006 Review first published: Issue 4, 2008
| Date | Event | Description |
|---|---|---|
| 23 May 2008 | Amended | Converted to new review format. |
Acknowledgements
The authors would like to thank the Cochrane Wounds Group Editors (David Margolis, Joan Webster and Gill Worthy) and referees (Allen Holloway, David Leaper, Barbara Postle, Rachel Richardson, Mark Rodgers and Jack Tweed) and copy editor (Elizabeth Royle) for their comments on the protocol and the review.
Appendices
Appendix 1. Search methods for original version ‐ 2008
Electronic searches
We systematically searched the following electronic databases for relevant trial reports:
Cochrane Wounds Group Specialised Register (Searched 28/5/08);
The Cochrane Central Register of Controlled Trials (CENTRAL, Issue 2 2008);
Ovid MEDLINE (1950 to May Week 2 2008);
Ovid EMBASE (1980 to 2008 Week 21);
Ovid CINAHL ( 1982 to May Week 4 2008)
Search strategy for CENTRAL: #1 MeSH descriptor Mupirocin explode all trees #2 mupirocin #3 bactroban #4 centany #5 eismycin #6 plasimine #7 pseudomonic acid #8 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7) #9 MeSH descriptor Staphylococcus aureus explode all trees #10 MeSH descriptor Staphylococcal Infections explode all trees #11 staphylococ* #12 "S aureus" #13 (#9 OR #10 OR #11 OR #12) #14 (#8 AND #13)
The Ovid MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximizing version (2008 revision); Ovid format (Lefebvre 2009) and the EMBASE and CINAHL searches were combined with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2008).
Searches for unpublished trials and unfinished studies were conducted in:
The System for Information on Grey Literature (SIGLE);
Index to Theses (ASLIB Index);
mRCT (http://www.controlled‐trials.com/mrct/);
ClinicalTrials.gov
No language or date restrictions were applied
Searching other resources
Citation lists from the identified studies were searched. The authors, who are experts in this field with a long standing interest in this subject, searched their personal archives, including the abstracts from the following major scientific meetings from 1995 to 2007:
Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC)
European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
The Society for Healthcare Epidemiology of America (SHEA)
Unpublished trials and unfinished studies were identified by contacting researchers and the manufacturer of mupirocin (GlaxoSmithKline BV, Zeist, The Netherlands).
Appendix 2. Ovid MEDLINE search strategy
1 exp Mupirocin/ 2 mupirocin.mp. 3 bactroban.mp. 4 centany.mp. 5 eismycin.mp. 6 plasimine.mp. 7 pseudomonic acid.mp. 8 or/1‐7 9 exp Staphylococcus aureus/ 10 exp Staphylococcal Infections/ 11 staphylococ$.mp. 12 S aureus.mp. 13 or/9‐12 14 8 and 13
Appendix 3. Ovid EMBASE search strategy
1 exp Mupirocin/ 2 exp Pseudomonic Acid/ 3 (mupirocin or bactroban or centany or eismycin or plasimine or pseudomonic acid).mp. 4 or/1‐3 5 exp Staphylococcus Aureus/ 6 exp Staphylococcus Infection/ 7 staphylococ$.mp. 8 S aureus.mp. 9 or/5‐8 10 (nasal or naso$).mp. 11 and/4,9‐10
Appendix 4. EBSCO CINAHL search strategy
S9 S3 and S8 S8 S4 or S5 or S6 or S7 S7 TI S aureus or AB S aureus S6 TI staphylococ* or AB staphylococ S5 (MH "Staphylococcal Infections+") S4 (MH "Staphylococcus Aureus+") S3 S1 or S2 S2 TI (mupirocin or bactroban or centany or eismycin or plasimine or pseudomonic acid) or AB (mupirocin or bactroban or centany or eismycin or plasimine or pseudomonic acid) S1 (MH "Mupirocin")
Data and analyses
Comparison 1. Nosocomial S. aureus infections among patients with S. aureus nasal carriage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Nosocomial S. aureus infection | 8 | 3374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.43, 0.70] |
| 2 Nosocomial S. aureus infection (High quality studies) | 4 | 2909 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.47, 1.00] |
Comparison 2. Nosocomial S. aureus infections among surgical patients with S. aureus nasal carriage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Nosocomial S. aureus infection | 4 | 1372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.34, 0.88] |
| 2 Nosocomial S. aureus infection (exclude Garcia) | 3 | 1307 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.34, 0.91] |
| 3 Nosocomial S. aureus surgical site infection | 4 | 1374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.38, 1.04] |
Comparison 3. Nosocomial S. aureus infections among dialysis patients with S. aureus nasal carriage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Nosocomial S. aureus infections | 2 | 302 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.32, 0.62] |
Comparison 4. Nosocomial S. aureus infections among CAPD patients: a comparison of mupirocin to neomycin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Nosocomial S. aureus infections | 1 | 22 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 3.95] |
Comparison 5. Mortality among patients with S. aureus nasal carriage.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 4 | 2161 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.64, 1.31] |
Comparison 6. Infection rate caused by other micro‐organisms than S. aureus: mupirocin compared with control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Infection rate caused by other micro‐organisms than S. aureus | 3 | 1393 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [1.11, 1.72] |
| 2 Infection rate caused by other gram‐positive micro‐organisms than S. aureus | 2 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.55, 1.41] |
| 3 Infection rate caused by gram‐negative micro‐organisms | 2 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.65 [0.78, 3.47] |
Comparison 7. Infection rate caused by other micro‐organisms than S. aureus: a comparison of mupirocin to neomycin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Infection rate caused by other micro‐organisms than S. aureus | 1 | 22 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.64, 2.79] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Boelaert 1989.
| Methods | Double‐blind, randomised controlled trial | |
| Participants | Hemodialysis patients. All carriers. Mupirocin: 17. Placebo: 18. No significant difference between both groups. | |
| Interventions | Mupirocin or placebo. Thrice daily for 2 weeks and subsequent 3 times weekly for a total of 9 months. | |
| Outcomes | S. aureus infection rate Mortality Adverse events | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Unclear |
| Blinding? participants | Low risk | |
| Blinding? outcome assessor | Low risk | |
| Intention to treat | Low risk | not reported but confirmed |
| Loss to follow up | Low risk | Mupirocin:41 Placebo:17 |
Garcia 2003.
| Methods | Randomised, prospective trial | |
| Participants | Cardiothoracic patients. Both carriers and non‐carriers. Mupirocin: 31 carriers, Placebo: 34 carriers. No significant difference between both groups. | |
| Interventions | Mupirocin twice daily for 5 days. Controls received no treatment. | |
| Outcomes | S. aureus infection rate. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | Inadequate |
| Blinding? participants | High risk | |
| Blinding? investigator | High risk | |
| Intention to treat | Low risk | not reported but confirmed by author |
| Loss to follow up | Low risk | Mupirocin:13 Control:15 |
Harbarth 1999.
| Methods | Double‐blind, randomised controlled trial | |
| Participants | Patients colonized with MRSA. Mupirocin: 48 Placebo: 50. No significant difference between both groups. | |
| Interventions | Mupirocin or placebo. Twice daily for 5 days. | |
| Outcomes | S. aureus infection rate. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Unclear |
| Blinding? participants | Low risk | |
| Blinding? investigator | Low risk | |
| Blinding? outcome assessor | Low risk | |
| Blinding? data analysis | Low risk | |
| Intention to treat | Low risk | reported and confirmed |
| Loss to follow up | High risk | |
Kalmeijer 2002.
| Methods | Double‐blind, randomised controlled trial | |
| Participants | Orthopedic surgery patients. Both carriers and non‐carriers. Mupirocin: 95 carriers. Placebo: 86 carriers. No significant difference between both groups. | |
| Interventions | Mupirocin or placebo. Twice daily from the day of admission (day before surgery) to the hospital until the day of surgery. | |
| Outcomes | S. aureus infection rate. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Adequate |
| Blinding? participants | Low risk | |
| Blinding? investigator | Low risk | |
| Blinding? outcome assessor | Low risk | |
| Blinding? data analysis | Low risk | |
| Intention to treat | Low risk | reported and confirmed |
| Loss to follow up | High risk | |
Konvalinka 2006.
| Methods | Double‐blind, randomised controlled trial | |
| Participants | Elective cardiac surgery patients. All carriers. Mupirocin: 130. Placebo: 127. Only COPD was more prevalent in the mupirocin group (p<0.01) | |
| Interventions | Mupirocin or placebo. Twice daily for 7 days, before surgery. | |
| Outcomes | S. aureus infection rate. Mortality. Adverse events. Infection rate caused by other micro‐organisms than S. aureus. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Adequate |
| Blinding? participants | Low risk | |
| Blinding? investigator | Low risk | |
| Blinding? outcome assessor | Low risk | |
| Blinding? data analysis | Low risk | |
| Intention to treat | Low risk | reported and confirmed |
| Loss to follow up | High risk | |
Mup Study Group 1996.
| Methods | Double‐blind, randomised controlled trial | |
| Participants | CAPD patients. All carriers. Mupirocin: 134. Placebo: 133. No significant difference between both groups. | |
| Interventions | Mupirocin or placebo. Twice daily for 5 days every 4 weeks, for maximal 18 months. | |
| Outcomes | S. aureus infection rate. Mortality. Adverse events. Infection rate caused by other micro‐organisms than S. aureus. | |
| Notes | This study was sponsored by the manufacturers of mupirocin (SmithKline Beecham, Baxter Health Care) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Unclear |
| Blinding? participants | Low risk | |
| Blinding? outcome assessor | Low risk | |
| Intention to treat | Low risk | reported and confirmed |
| Loss to follow up | Low risk | Mupirocin:1 Placebo:1 |
Perl 2002.
| Methods | Double‐blind, randomised controlled trial | |
| Participants | General, gynaecologic, neurologic and cardiothoracic. patients. Both carriers and non‐carriers. Mupirocin: 430 carriers. Placebo: 439 carriers. Patients that received placebo were more likely to have had renal disease (p=0.04). | |
| Interventions | Mupirocin or placebo. Twice daily for up to 5 days, before the operation. | |
| Outcomes | S. aureus infection rate. Mortality. Adverse events. Infection rate caused by other micro‐organisms than S. aureus. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Adequate |
| Blinding? participants | Low risk | |
| Blinding? investigator | Low risk | |
| Blinding? outcome assessor | Low risk | |
| Blinding? data analysis | Low risk | |
| Intention to treat | Low risk | reported and confirmed |
| Loss to follow up | Low risk | Mupirocin 10.4 Placebo 13.2 |
Pérez‐Fontan 1992.
| Methods | Randomised, prospective trial. | |
| Participants | CAPD patients. All carriers. Mupirocin: 11. Neomycin: 8. No significant difference between both groups. | |
| Interventions | Mupirocin or Neomycin. Mupirocin thrice daily for 7 days. Neomycin sulphate thrice daily for 7 days. | |
| Outcomes | S. aureus infection rate. Adverse events. Infection rate caused by other micro‐organisms than S. aureus. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Unclear |
Wertheim 2004b.
| Methods | Double‐blind, randomised controlled trial | |
| Participants | Nonsurgical patients. All carriers. Mupirocin: 793. Placebo: 809. No significant difference between both groups. | |
| Interventions | Mupirocin or placebo. Twice daily for 5 days, started 1 to 3 days after admission. | |
| Outcomes | S. aureus infection rate. Time to infection. Mortality. Adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Adequate |
| Blinding? participants | Low risk | |
| Blinding? investigator | Low risk | |
| Blinding? outcome assessor | Low risk | |
| Blinding? data analysis | Low risk | |
| Intention to treat | Low risk | reported and confirmed |
| Loss to follow up | Low risk | Mupirocin: 9.7 Placebo:8.3 |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Critchley 2006 | Not a trial. |
| Di Filippo 1999 | No data about carriers. Author could not be contacted for additional information. |
| Klaus 2002 | This was an abstract on the 5th European Peritoneal Dialysis Meeting in Brussels, Belgium, 4‐7 May 2002. Family members of CAPD patients with nasal carriage were treated with mupirocin or placebo. It is unclear whether patients with nasal carriage were treated with mupirocin and how many carriers in both treatment groups (mupirocin/placebo) developed an infection caused by S. aureus. This abstract has not resulted in a paper yet and the author could not be contacted for additional information. |
| Leigh 1993 | Not health‐care related. |
| Martin 1999 | No description of infections. Only data about eradication. |
| Mody 2003 | Not health‐care related. |
| Niwa 1999 | No data about carriers. Author could not be contacted for additional information. |
| Raz 1996 | Not health‐care related. |
| Simor 2007 | Combination of mupirocin treatment with oral antibiotics. |
| Sit 2007 | No data about carriers. Author contacted for additional information. |
| Suzuki 2003 | No data about carriers. Author contacted for additional information, but no reply was received. |
| Wasielewski 2003 | Not a trial. Describes the results of the trial by Perl et al. |
Contributions of authors
J Kluytmans: Conceived the review. Wrote to study author/experts/companies. Performed previous work that was the foundation of the current review and provided data. J Kluytmans & M van Rijen: Designed and coordinated the review. Extracted and checked data. Undertook and checked quality assessment. Performed statistical analysis and interpretation. Completed first draft of the review and subsequent edits. Made an intellectual contribution to the review and approved final review prior to submission. Are guarantors of the review. M Bonten & R Wenzel: Analysed or interpreted data and checked quality assessment. Performed part of writing or editing of the review and made an intellectual contribution to the review. Advised on the review and approved final review prior to submission. R Wenzel: Performed previous work that was the foundation of the current review.
Contributions of editorial base:
Nicky Cullum:Edited the review, advised on methodology, interpretation and review content. Approved the final review prior to submission. Sally Bell‐Syer:Coordinated the editorial process. Advised on methodology, interpretation and content. Edited and copy edited the review and the updated review. Ruth Foxlee: Designed the search strategy, ran the searches and edited the search methods section for the update.
Sources of support
Internal sources
Amphia Hospital Breda, Netherlands.
External sources
No sources of support supplied
Declarations of interest
M van Rijen, R Wenzel and J Kluytmans have declared no conflict of interests. M Bonten has received funding from 3M.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Boelaert 1989 {published data only}
- Boelaert JR, Smedt RA, Baere YA, Godard CA, Matthys EG, Schurgers ML, et al. The influence of calcium mupirocin nasal ointment on the incidence of Staphylococcus aureus infections in haemodialysis patients. Nephrology, Dialysis, Transplantation 1989;4:278‐81. [DOI] [PubMed] [Google Scholar]
Garcia 2003 {published data only}
- Garcia AM, Villa MV, Escudero ME, Gomez P, Vélez MM, Munera MI, et al. Use of nasal mupirocin for Staphylococcus aureus: effect on nasal carriers and nosocomial infections [Uso nasal de la mupirocina para Staphylococcus aureus: efecto en portadores y en infecciones nosocomiales]. Biomédica 2003;23:173‐9. [PubMed] [Google Scholar]
Harbarth 1999 {published data only}
- Harbarth S, Dharan S, Liassine N, Herrault P, Auckenthaler R, Pittet D. Randomised, placebo‐controlled, double‐blind trial to evaluate the efficacy of mupirocin for eradicating carriage of methicillin‐resistant Staphylococcus aures. Antimicrobial Agents and Chemotherapy 1999;43(6):1412‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kalmeijer 2002 {published data only}
- Kalmeijer MD, Coertjens H, Baere GAJ, Stuurman A, Belkum A, Kluytmans JAJW. Postoperative wound infections in orthopedic surgery. The effect of mupirocin nasal ointment. Pharmaceutisch Weekblad 2001;136(20):730‐1. [Google Scholar]
- Kalmeijer MD, Coertjens H, Nieuwland‐Bollen PM, Bogaers‐Hofman D, Baere GAJ, Stuurman A, et al. Surgical site infections in orthopedic surgery: the effect of mupirocin nasal ointment in a double‐blind, randomised, placebo‐controlled study. Clinical Infectious Diseases 2002;35(4):353‐8. [DOI] [PubMed] [Google Scholar]
Konvalinka 2006 {published data only}
- Konvalinka A, Errett L, Fong IW. Impact of treating Staphylococcus aureus nasal carriers on wound infections in cardiac surgery. Journal of Hospital Infection 2006;64(2):162‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mup Study Group 1996 {published data only}
- The Mupirocin Study Group. Nasal mupirocin prevents Staphylococcus aureus exit‐site infection during peritoneal dialysis. Journal of the American Society of Nephrology 1996;7(11):2403‐8. [DOI] [PubMed] [Google Scholar]
Perl 2002 {published data only}
- Perl TM, Cullen JJ, Wenzel RP, Zimmerman MB, Pfaller MA, Sheppard D, et al. Intranasal mupirocin to prevent postoperative Staphylococcus aureus infections. The New England Journal of Medicine 2002;346(24):1871‐906. [DOI] [PubMed] [Google Scholar]
Pérez‐Fontan 1992 {published data only}
- Pérez‐Fontan M, Rosales M, Rodriguez‐Carmona A, Moncalian J, Fernandez‐Rivera C, Cao M, et al. Treatment of Staphylococcus aureus nasal carriers in CAPD with mupirocin. Advances in peritoneal dialysis 1992;8:242‐5. [PubMed] [Google Scholar]
Wertheim 2004b {published data only}
- Wertheim HFL, Vos MC, Ott A, Kluytmans JAJW, Vandenbroucke‐Grauls CMJE, et al. Mupirocin prophylaxis for the prevention of nosocomial infections due to nasal carriers of Staphylococcus aureus is of no use in nonsurgical patients as yet. Nederlands Tijdschrift voor Geneeskunde 2005;149:350‐5. [Google Scholar]
- Wertheim HFL, Vos MC, Ott A, Voss A, Kluytmans JAJW, Vandenbroucke‐Grauls MJE, et al. Mupirocin prophylaxis against nosocomial Staphylococcus aureus infections in nonsurgical patients. Annals of Internal Medicine 2004;140:419‐25. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Critchley 2006 {published data only}
- Critchley IA. Eradication of MRSA nasal colonization as a strategy for infection prevention. Drug Discovery today: Therapeutic Strategies 2006;3(2):189‐95. [Google Scholar]
Di Filippo 1999 {published data only}
- Filippo A, Simonetti T. Endonasal mupirocin in the prevention of nosocomial pneumonia. Minerva Anestesiologica 1999;65(3):109‐13. [PubMed] [Google Scholar]
Klaus 2002 {published data only}
- Klaus G, Baum H, Wuhl E, Schaefer F, and European Pediatric Peritoneal Dialysis Study Group (EPPS). Efficacy of mupirocin prophylaxis in reducing the incidence of peritoneal dialysis (PD)‐related Staphylococcus aureus infections in children on chronic PD: results of a double blind, placebo‐controlled trial. Peritoneal Dialysis International. 2002; Vol. 22, issue 1:149.
Leigh 1993 {published data only}
- Leigh DA, Joy G. Treatment of familial staphylococcal infection ‐ comparison of mupirocin nasal ointment and chlorhexidine‐neomycin (Naseptin) cream in eradication of nasal carriage. Journal of Antimicrobial Chemotherapy 1993;31(6):909‐17. [DOI] [PubMed] [Google Scholar]
Martin 1999 {published data only}
- Martin JN, Perdreau‐Remington F, Kartalija M, Pasi OG, Webb M, Gerberding JL, et al. A randomised clinical trial of mupirocin in the eradication of Staphylococcus aureus nasal carriage in human immunodeficiency virus disease. Journal of Infectious Diseases 1999;180(3):896‐9. [DOI] [PubMed] [Google Scholar]
Mody 2003 {published data only}
- Mody L, Kauffman CA, McNeil SA, Galecki AT, Bradley SF. Mupirocin‐based decolonization of Staphylococcus aureus carriers in residents of 2 long‐term care facilities: a randomised, double‐blind, placebo‐controlled trial. Clinical Infectious Diseases 2003;37(11):1467‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niwa 1999 {published data only}
- Niwa J, Yoshikawa O, Tanigawara T, Kubota T, Chiba M, Mikami T, et al. Prevention of MRSA spread in the neurological field: intranasal application of mupirocin calcium ointment. No Shinkei Geka ‐ Neurological Surgery 1999;27(8):729‐33. [PubMed] [Google Scholar]
Raz 1996 {published data only}
- Raz R, Miron D, Colodner R, Staler Z, Samara Z, Keness Y. A 1‐year trial of nasal mupirocin in the prevention of recurrent staphylococcal nasal colonization and skin infection. Archives of Internal Medicine 1996;156(10):1109‐12. [PubMed] [Google Scholar]
Simor 2007 {published data only}
- Simor AE, Philips E, McGeer A, Konvalinka A, Loeb M, Devlin HR, et al. Randomised controlled trial of chlorhexidine gluconate for washing, intranasal mupirocin, and rifampin and doxycycline versus no treatment for the eradication of methicillin‐resistant Staphylococcus aureus colonization. Clinical Infectious Diseases 2007;44(2):178‐85. [DOI] [PubMed] [Google Scholar]
Sit 2007 {published data only}
- Sit D, Kadiroglu AK, Kayabasi H, Yilmaz ME. Prophylactic intranasal mupirocin ointment in the treatment of peritonitis in continuous ambulatory peritoneal dialysis patients. Advances in Therapy 2007;24(2):387‐93. [DOI] [PubMed] [Google Scholar]
Suzuki 2003 {published data only}
- Suzuki Y, Kamigaki T, Fujino Y, Tominaga M, Ku Y, Kuroda Y. Randomised clinical trial of preoperative intranasal mupirocin to reduce surgical‐site infection after digestive surgery. British Journal of Surgery 2003;90(9):1072‐5. [DOI] [PubMed] [Google Scholar]
Wasielewski 2003 {published data only}
- Wasielewski S. Staphylococcus aureus: Does mupirocin nasal ointment prevent postoperative infections? [Schutzt mupirocin‐nasensalbe vor postoperativen infecktionen?]. Deutsche Apotheker Zeitung 2003;143(18):50‐2. [Google Scholar]
References to studies awaiting assessment
Bode 2010 {published data only}
- Bode LGM, Kluytmans JAJW, Wertheim HFL, Bogaers D, Vandenbroucke‐Grauls CMJE, Roosendaal R, et al. Preventing surgical‐site infections in nasal carriers of Staphylococcus aureus. New England Journal of Medicine 2010;362(1):9‐17. [DOI] [PubMed] [Google Scholar]
Golan 2010 {published data only}
- Golan Y. Decolonization of nostrils and skin of nasal carriers of S. aureus at admission prevented hospital‐associated infection. Annals of Internal Medicine 2010;152(10):JC5‐9. [DOI] [PubMed] [Google Scholar]
Jabbour 2010 {published data only}
- Jabbour H, Madi Jebara S, Jabbour K, Yazigi A, Haddad F, Hayek G, et al. Does nasal decontamination reduce the incidence of infections after cardiac surgery?. Journal Medical Libanais ‐ Lebanese Medical Journal 2010;58(2):65‐70. [PubMed] [Google Scholar]
Additional references
Fawley 2006
- Fawley WN, Parnell P, Hall J, Wilcox MH. Surveillance for mupirocin resistance following introduction of routine peri‐operative prophylaxis with nasal mupirocin. Journal of Hospital Infection 2006;62(3):327‐32. [DOI] [PubMed] [Google Scholar]
Francois 2003
- Francois P, Pittet D, Bento M, Pepey B, Vaudaux P, Lew D, et al. Rapid detection of methicillin‐resistant Staphylococcus aureus directly from sterile or nonsterile clinical samples by a new molecular assay. Journal of Clinical Microbiology 2003;41(1):254‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Henkel 1999
- Henkel T, Finlay J. Emergence of resistance during mupirocin treatment: is it a problem in clinical practice?. Journal of Chemotherapy 1999;11(5):331‐7. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins J, Thompson S. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kallen 2005
- Kallen AJ, Wilson CT, Larson RJ. Perioperative intranasal mupirocin for the prevention of surgical‐site infections: systematic review of the literature and meta‐analysis. Infection Control & Hospital Epidemiology 2005;26(12):916‐22. [DOI] [PubMed] [Google Scholar]
Kaplowitz 1988
- Kaplowitz L, Comstock J, Landwehr D, Dalton H, Mayhall C. Prospective study on microbial colonization of the nose and skin and infection of the vascular access site in hemodialysis patients. Journal of Clinical Microbiology 1988;26(7):1257‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kluytmans 1995
- Kluytmans J, Mouton J, Yzerman E, Vandenbroucke‐Grauls C, Maat A, Wagenvoort, et al. Nasal carriage of Staphylococcus aureus as a major risk factor for wound infections after cardiac surgery. Journal of Infectious Diseases 1995;171(1):216‐9. [DOI] [PubMed] [Google Scholar]
Kluytmans 1997
- Kluytmans J, Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clinical Microbiology Reviews 1997;10(3):505‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laupland 2003
- Laupland KB, Conly JM. Treatment of Staphylococcus aureus colonization and prophylaxis for infection with topical intranasal mupirocin: an evidence‐based review. Clinical Infectious Diseases 2003;37(7):933‐8. [DOI] [PubMed] [Google Scholar]
Lefebvre 2009
- Lefebvre C, Manheimer E, Glanville J, on behalf of the Cochrane Information Retrieval Methods Group. Chapter 6: Searching for studies.. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2009. Available from www.cochrane‐handbook.org.
Mangram 1999
- Mangram A, Horan T, Pearson M, Silver L, Jarvis W. The Hospital Infection Control Practices Advisory Committee Guideline for the prevention of surgical site infection. Infection Control and Hospital Epidemiology 1999;20(4):247‐80. [DOI] [PubMed] [Google Scholar]
NNIS 2004
- National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance System Report, data summary from January 1992 through June 2004. American Journal of Infection Control 2004;32:470‐85. [DOI] [PubMed] [Google Scholar]
Noskin 2005
- Noskin GA, Rubin RJ, Schentag JJ, Kluytmans J, Hedblom EC, Smulders M. The burden of Staphylococcus aureus to US hospitals: an analysis of the 2000‐2001 nationwide inpatients sample database. Archives of Internal Medicine 2005;165(15):1756‐61. [DOI] [PubMed] [Google Scholar]
Paule 2004
- Paule SM, Pasquariello AC, Hacek DM, Fisher AG, Thomson RB Jr, Kaul KL, et al. Direct detection of Staphyloccus aureus from adult and neonate nasal swab specimens using real‐time polymerase chain reaction. Journal Molecular Diagnosis 2004;6(3):191‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pittet 2000
- Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital‐wide programme to improve compliance with hand hygiene. Lancet 2000;356(9238):1307‐12. [DOI] [PubMed] [Google Scholar]
SIGN 2008
- Scottish Intercollegiate Guidelines Network (SIGN). Search filters. http://www.sign.ac.uk/methodology/filters.html#random (accessed 28 May 2008).
Strippoli 2004
- Strippoli GFM, Tong A, Johnson D, Schena FP, Craig JC. Antimicrobial agents for preventing peritonitis in peritoneal dialysis patients. Cochrane Database of Systematic Reviews 2004, Issue 4. [Art. No.: CD004679. DOI: 10.1002/14651858.CD004679.pub2] [DOI] [PubMed] [Google Scholar]
Trautmann 2008
- Trautmann M, Stecher J, Hemmer W, Luz K, Panknin HT. Intranasal mupirocin prophylaxis in elective surgery. A review of published studies. Chemotherapy 2008;54(1):9‐16. [DOI] [PubMed] [Google Scholar]
Von Eiff 2001
- Eiff C, Becker K, Machka K, Stammer H, Peters G. Nasal carriage as a source of Staphylococcus aureus bacteremia. The New England Journal of Medicine 2001;344:11‐6. [DOI] [PubMed] [Google Scholar]
Wertheim 2004a
- Wertheim H, Vos M, Ott A, Belkum A, Voss A, Kluytmans J, et al. Risk and outcome of nosocomial Staphylococcus aureus bacteraemia in nasal carriers versus non‐carriers. Lancet 2004;364:703‐5. [DOI] [PubMed] [Google Scholar]
Yu 1986
- Yu VL, Goetz A, Wagener M, Smith PB, Rihs JD, Hanchett J, et al. Staphylococcus aureus nasal carriage and infection in patients on hemodialysis. The New England Journal of Medicine 1986;315:91‐6. [DOI] [PubMed] [Google Scholar]
Yzerman 1996
- Yzerman EP, Boelens HA, Tjhie JH, Kluytmans JA, Mouton JW, Verbrugh HA. APACHE II for predicting course and outcome of nosocomial Staphylococcus aureus bacteremia and its relation to host defense. Journal of Infectious Diseases 1996;173(4):914‐9. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
van Rijen 2008
- Rijen MML, Bonten M, Wenzel RP, Kluytmans JAJW. Intranasal mupirocin for reduction of Staphylococcus aureus infections in surgical patients with nasal carriage: A systematic review. Journal of Antimicrobial Chemotherapy 2008;61(2):254‐61. [DOI] [PubMed] [Google Scholar]


