Abstract
Background:
Rates of both depression and alcohol use are disproportionately higher among American Indian (AI) adolescents than adolescents in the general population. The co-occurrence of depression and alcohol use is highly comorbid and clinically relevant given reciprocal negative influences on outcomes. Family factors may be especially relevant for conferring some buffering effect in this relationship due to the importance of kinship and community in AI communities. The purpose of the current study is to examine the roles of family warmth and parent monitoring in the association between depressive symptoms and alcohol use in a large, nationally representative sample of AI adolescents.
Methods:
Data collected from 2009–2013 included 3,498 AI 7th-12th graders residing on or near a reservation (47.8% female). Participants reported on their depressive symptoms, family factors, and alcohol use.
Results:
Depressive symptoms were statistically significantly positively associated with alcohol use (r=.11, p<.001). Greater depressive symptoms were associated with statistically significantly less perceived family warmth (β=−.09, 95%CI [−.13, −.06]), which was associated with statistically significantly greater alcohol use (β=−.39, 95%CI [−.55, −.23]). Family warmth was found to statistically significantly account for the association between depressive symptoms and alcohol use at high (β=.04, SE=.02, 95%CI [.004, .09]), but not low, levels of parent monitoring (β=.02, SE=.02, 95%CI [−.002, .06]).
Conclusions:
Results of the present study suggest the importance of developing culturally sensitive prevention and treatment approaches focusing on increasing both family warmth and parent monitoring to address the co-occurrence of AI adolescent depression and alcohol misuse.
Keywords: American Indian, depression, alcohol use, family warmth, parent monitoring
Introduction
Alcohol use has been identified by American Indian (AI) communities as among their most pressing public health concerns (Hawkins et al., 2004, Spillane and Venner, 2018). There is a high degree of variability in rates of alcohol use across AI individuals, but it is well-established that AI individuals as a group experience disproportionate harm associated with alcohol use compared to other racial/ethnic groups (Spillane et al., 2020, Swaim and Stanley, 2018). One nationally representative sample of reservation-based AI adolescents found higher rates of lifetime alcohol use: 39.7%, 52.9%, and 72.5% for 8th, 10th, and 12th graders, respectively, compared to 22.8%, 43.4%, and 61.2% for 8th, 10th, and 12th graders, respectively, in a sample collected from Monitoring the Future representing the general population of U.S. adolescents (Swaim and Stanley, 2018). Simultaneously, other research finds higher rates of abstinence in AI communities compared to other racial/ethnic groups (US Department of Health and Human Services, 2010). These observed differences likely reflect the high degree of variability that exists across AI individuals. Previous work has found evidence for variability based on individuals’ context and living situation; for example, reservation-based AI adolescents report significantly higher rates of alcohol use and initiate alcohol use earlier compared to urban AI adolescents (Yu & Stiffman, 2007). Yet, AI adolescents who do drink alcohol tend to initiate drinking alcohol early and experience high rates of binge and heavy drinking and consequences related to alcohol use (Spillane et al., 2015, Vaeth et al., 2017, Schick et al., 2021). These factors increase risk for greater negative alcohol-related outcomes in early adulthood among AI individuals (e.g., likelihood of a lifetime alcohol use disorder diagnosis; Henry et al., 2011).
One factor that has been found to contribute to risk for alcohol use among non-AI adolescents is depressive symptoms (Ganz and Sher, 2009, Kandel et al., 1999, Clark et al., 2003). In the U.S., AI adolescents have the highest prevalence rates of lifetime and past-year major depressive episodes compared to monoracial adolescents from other racial/ethnic groups (U.S. Department of Health and Human Services, 2019). The co-occurrence of depressive symptoms and alcohol use is clinically relevant given their reciprocal negative impact on outcomes. For example, alcohol use among non-AI individuals reporting depressive symptoms has been found to be associated with increased severity and duration of depressive episodes and likelihood of suicidal ideation (Hasin et al., 1996, Boschloo et al., 2011; Gadermann et al., 2012). Among AI youth, adolescents who report greater depressive symptoms tend to initiate alcohol use at younger ages (Cheadle and Whitbeck, 2011). Further, there is qualitative support for the role of alcohol in one’s ability to manage depressive symptoms among AIs (i.e., 15 out of 19 adolescents in one study describing drinking as a means to avoid and regulate negative affective states, including depression; Tingey et al., 2017). Depressive symptoms, alcohol use, and their co-occurrence have been identified as important contributors to suicide (Gaynes et al., 2004; Hawton et al., 2013). This is of concern, as AIs have disproportionately high rates of suicidal ideation, suicide attempts, and death by suicide compared to all other racial groups in the U.S. (Centers for Disease Control and Prevention, 2020). Thus, to address these important health disparities, there is a need for research to identify factors that confer risk and protection for co-occurring depressive symptoms and alcohol use and explain this connection among AI adolescents to inform targets for prevention and intervention strategies.
Family factors may be important to consider in the relation between depressive symptoms and alcohol use among AI adolescents. Family is recognized as the cornerstone of AI communities; it is the mechanism through which Indigenous beliefs, values, and practices are transmitted (Red Horse, 1980). Being close-knit is a central feature of healthy AI families (Martin and Yurkovich, 2014) and is inclusive of family warmth; or features of trust, support, emotional closeness, open and honest communication, caregiver responsiveness and attentiveness to children’s needs, and mutual respect (Kopak and Hawley, 2012). Further, while the relative importance of parents and family in decision making regarding engagement in risk behaviors (such as substance use) tends to decline during adolescence in favor of peer influence, this decline is less pronounced for AI adolescents. Parents and families have been found to remain influential, even when controlling for peer influence, in this decision-making process throughout the adolescent years for AIs (Swaim et al., 1993; Swaim & Stanley, 2016). In particular, family warmth has been empirically linked to a number of positive outcomes, including greater well-being and lower risk for mental health concerns and for engagement in health-compromising behaviors (Huppert et al., 2010, Shakya et al., 2012, Yap et al., 2014). Parental Acceptance-Rejection Theory, which describes the causes and consequences of parental acceptance and rejection, states that a child’s perception of experiencing warmth in their families is more impactful on outcomes than objective measures or parent reports of warmth (Rohner et al., 2012). Specifically, perceived family warmth has been found to be associated with significantly lower odds of endorsing depressive symptoms among AI adolescents (Barney, 2001, Henson et al., 2017). Further, a sense of family warmth has been found to be associated with lower rates of alcohol use in AI adolescents (King et al., 1992, Allen et al., 2006, Hurdle et al., 2003).
While there is a clear connection between depressive symptoms and alcohol use as well as between family warmth and both depressive symptoms and alcohol use separately, the relations among these three factors together remains underexplored. Nonetheless, there is good reason to suggest a relationship; it may be that depressive symptoms lead AI adolescents to believe that their family members care less about them as a result of common cognitive distortions associated with depression (e.g., feelings of worthlessness, discounting positive evidence; Orchard et al., 2019). Additionally, previous literature has found depressive symptoms to be negatively correlated with perceived family support (Tezel et al., 2011) and to be prospectively associated with decreased perceived emotional support from one’s family (Slavin & Rainer, 1990); this same relationship may hold for depressive symptoms and family warmth. Low perceived family warmth may be particularly detrimental to AI adolescents given the traditionally strong reliance on familial bonding in AI communities (Garrett and Garrett, 1994). Subsequently, AI adolescents may turn to alcohol use to cope with negative mood (Yuan et al., 2010) stemming from these beliefs. Indeed, negative reinforcement (Baker et al., 2004) and self-medication (Khantzian, 1997) models suggest a central function of affect modulation for alcohol use broadly and specifically in the context of depression (Turner et al., 2018, Bolton et al., 2009), including among AI communities (Skewes and Blume, 2015, Stewart et al., 2011).
Another family-related factor that may play an important role in the relation of depressive symptoms to alcohol use in AI adolescents is parent monitoring, a set of parenting behaviors involving attention to a child’s whereabouts and activities (Dishion and McMahon, 1998), including through parents’ own efforts to find out what their children are doing (referred to as solicitation and control) and through children’s choice to divulge information about what they are doing (referred to as child disclosure; Kerr & Stattin, 2000; Stattin & Kerr, 2000). Settler colonialism has led to the disruption of traditional parenting practices, family structures, and relationships in AI communities as a result of forced removal of children from their homes to be adopted into White families and institutionalization in residential schools, as well as criminalization of important cultural practices (Brave Heart, 1999). Indeed, qualitative studies examining the effects of residential boarding schools (i.e., the forced removal of AI children from their homes, whereby many children experienced significant trauma), report that AI individuals who were raised in boarding school settings feel unprepared in their roles as parents and a sense of confusion with respect to how to raise children in a healthy way (Brave Heart, 1999). These effects have been hypothesized as contributing to the stark health disparities seen among AI communities (Walters et al., 2011) and to alcohol-related health disparities in particular (Brave Heart, 1999). Lower parent monitoring has been found to be robustly associated with increased risk for adolescent substance use (Whitesell et al., 2014, Rodgers-Farmer, 2001), while greater parent monitoring is associated with increased communication and perceived support within child-parent relationships (Bacchini et al., 2011, Ceballo et al., 2003).
Parent monitoring may also modify the relation between depressive symptoms and family warmth by influencing the degree to which depression affects an adolescent’s perception that their family cares about them. Youth whose parents engage in greater monitoring may experience protection against the negative effects of depressive symptoms because their parents are more likely to communicate their support, which may then indirectly reduce those youth’s risk for alcohol use. Parent monitoring may also modify the relation between family warmth and alcohol use. Parenting styles characterized by a high degree of warmth and a low degree of monitoring (i.e., permissive parenting) have been found to be associated with deleterious adolescent outcomes, including increased risk of substance use (Berge et al., 2016; Cohen & Rice, 1997). It is likely that family warmth is protective against alcohol use, such as in the context of depressive symptoms, only when parents are also effectively monitoring their behavior. Further, parent monitoring may serve to limit the availability of alcohol (which is among the strongest predictors of adolescent alcohol use; Kuntsche et al., 2008, Ryan et al., 2010), thereby limiting the opportunity for adolescents to use alcohol in response to higher depressive symptoms. Yet, no work to date has examined the role of parent monitoring in these associations.
The present study aims to extend previous literature by examining the relations among depressive symptoms, perceived family warmth, parent monitoring, and alcohol use in AI adolescents. First, we examined the direct association between depressive symptoms and alcohol use; we hypothesized that AI adolescents with greater depressive symptoms would report more alcohol use. Next, we examined family warmth as a potential explanatory variable; we hypothesized that greater depressive symptoms would be associated with lower levels of perceived family warmth, which, in turn, would relate to more alcohol use. Finally, we explored parent monitoring as a potential moderator of the indirect effect of depressive symptoms on alcohol use through perceived family warmth; we expected that perceived family warmth would account for the association between depressive symptoms and alcohol use at high but not low levels of parent monitoring.
Materials and Methods
Participants and Procedures
Data used in the current study were collected as part of a larger study examining levels of substance use as well as risk and protective factors associated with substance use among AI adolescents. Following data collection, data used for the current study were made publicly available through the National HIV and Addiction Data Archive, with all potentially identifying information regarding specific participating tribal groups or communities removed to protect their privacy and confidentiality. Schools were invited to participate if they were on or near an AI reservation and if at least 20% of their student body were AI. They were stratified into six geographic regions in which reservation-based AIs live (Snipp, 2005). Within those regions, tribal and/or school board authority approvals were obtained, as appropriate, and surveys were administered during classes by staff at 33 identified schools. Parents were able to opt their children out of participation by contacting the school, and students could decline to participate by leaving their surveys blank. However, less than 1% of children either declined to participate or were opted out by their parents (Stanley et al., 2014a). Participants for the present study were a subsample of 7–12th graders who identified as AI (n = 3,498, 47.7% female) drawn from a larger sample of adolescents (N = 5,744, 47.0% female). More than half of participants in the present study reported that they had ever drank alcohol (n = 2,082, 59.7%). Of those reporting lifetime alcohol use, 71.9% reported that they had ever drank alcohol until they were intoxicated (n = 1,492). Demographic characteristics of the sample are presented in Table 1.
Table 1.
Sample Characteristics (N = 3,498)
| n (%) | M (SD) | Range | |
|---|---|---|---|
| Age | 14.76 (1.70) | 10 – 21 | |
| Sex | |||
| Male | 1,708 (50.5%) | ||
| Female | 1,672 (49.5%) | ||
| Grade in School | |||
| 7th grade | 775 (22.2%) | ||
| 8th grade | 728 (20.8%) | ||
| 9th grade | 601 (17.2%) | ||
| 10th grade | 521 (14.9%) | ||
| 11th grade | 508 (14.5%) | ||
| 12th grade | 365 (10.4%) | ||
| Depressive Symptoms | 6.57 (5.59) | 0 – 21 | |
| Perceived Family Warmth | 8.16 (1.79) | 0 – 9 | |
| Parent Monitoring | 8.14 (3.16) | 0 – 12 | |
| Alcohol Use | |||
| Lifetime Alcohol Use | 2,082 (59.7%) | ||
| Lifetime Intoxication | 1,523 (43.7%) | ||
| Alcohol Use | 2.69 (4.41) | 0 – 28 |
Note: Percentages reflect valid percentages.
Measures
Participants were administered the adolescent form of the American Drug and Alcohol Survey (ADAS; Oetting et al., 1985). This measure was listed in the 2007 SAMHSA Measures and Instruments Resource Guide and has been used in the national Our Youth our Future Project conducted by the Colorado State University Tri-Ethnic Center for Prevention Research since 1974 to assess rates and correlates of substance use among AI adolescents living on or near reservations (Oetting et al., 1985; Stanley et al., 2014a; Swaim & Stanley, 2018). ADAS domains/items evaluated in the present study are described below.
Depressive symptoms
Depressive symptoms were measured with seven items assessing depressive affect (e.g., one question asks students how depressed they feel). Participants rate each item based on how much they believe it describes them using a 4-point scale (0 = not at all, 3 = a lot). Item scores are summed to create a total scale score ranging from 0 to 21, with higher scores reflecting greater depressive symptoms. Reliability in the current sample was excellent (Cronbach’s α = .92). This scale has been previously used in research focusing on substance use among AI adolescents (Swaim, 2015).
Parent monitoring
Parent monitoring was measured with four items assessing participants’ beliefs of how much their parents monitored their actions (e.g., one question asks whether student’s parents allow them to stay out late). Participants rate each item on a 4-point scale (0 = very true, 3 = not at all true). Item scores are summed to create a total scale score ranging from 0 to 12, with higher scores reflecting greater parent monitoring. Reliability in the current sample was good (Cronbach’s α = .84). This scale has been previously used in research focusing on substance use among AI adolescents (Spillane et al., 2017; Swaim & Stanley, 2016).
Perceived family warmth
Perceived family warmth was measured with three items assessing participants’ perceptions of their family’s attitudes towards them, the participants’ perceptions of their family’s attitudes towards their actions, as well as the participants’ attitudes towards their family (e.g., one question asks how much a student’s family cares about them). Participants rate each item on a 4-point scale (0 = not at all, 3 = a lot). Item scores are summed to create a total scale score ranging from 0 to 9, with higher scores reflecting a greater sense of family warmth. Reliability in the current sample was good (Cronbach’s α = .84). This scale has been previously used in research focusing on substance use among AI adolescents (Nalven et al., 2020).
Alcohol Use
Alcohol Use was measured with five items assessing the frequency of various drinking behaviors. Two questions ask about frequency of drinking alcohol and being intoxicated in the past year on a 6-point scale (0 = none, 5 = 50 or more times). Two questions ask about frequency of drinking alcohol and being intoxicated in the past month on a 5-point scale (0 = none, 4 = 20 or more times). One item asks about frequency of heavy drinking in the past two weeks (i.e., having four or more drinks on one occasion) on an 11-point scale (0 = none, 10 = 10 or more times). Items are summed to create a total scale score ranging from 0 to 28, with higher scores reflecting greater alcohol use. Reliability in the current sample was good (Cronbach’s α = .88). This scale has been previously used in research focusing on alcohol use among AI adolescents (Schick et al., 2020).
Demographic characteristics
Demographic characteristics including age, sex (coded such that 0 = male and 1 = female), grade, and race/ethnicity were collected.
Analytic Plan
As recommended by Tabachnick et al. (2007), all study variables were assessed for adherence to generalized linear model assumptions. Then, Pearson product-moment and point-biserial correlations were calculated between relevant study variables to explore their bivariate associations. Next, moderated mediation analyses were conducted to examine whether parent monitoring moderated the associations among depressive symptoms, perceived family warmth, and alcohol use using the PROCESS SPSS macro (Model 59) as recommended by Hayes (2018). The PROCESS procedures use ordinary least squares regression and bootstrapping methodology, which confers more statistical power than do standard approaches to statistical inference and does not rely on distributional assumptions. The model examined whether parent monitoring moderated each of the paths in the mediation model (i.e., the paths between depressive symptoms and family warmth [a path], between family warmth and alcohol use [b path], and between depressive symptoms and alcohol use [c path]) and the indirect effect (a x b). The indirect effect is considered statistically significant if the 95% confidence interval does not contain zero (Preacher and Hayes, 2004). Predictor variables were Z-standardized and models were re-run with these standardized variables to attain standardized regression outputs to serve as a measure of effect size and allow for comparison of the magnitude of effects. Bootstrapping was done with 10,000 random samples generated from the observed covariance matrix to estimate the standard errors of parameter estimates and the bias-corrected 95% confidence intervals (CIs) of the indirect effects (Preacher and Hayes, 2004, MacKinnon et al., 2002).
Results
Bivariate Correlations
Pearson product-moment correlations revealed small negative associations between depressive symptoms and perceived family warmth (r = −.11, p < .001) and parent monitoring (r = −.09, p < .001) and a small positive association between depressive symptoms and alcohol use (r = .11, p < .001). Perceived family warmth demonstrated a small positive association with parent monitoring (r = .14, p < .001). Alcohol use demonstrated a small negative association with perceived family warmth (r = −.11, p < .001) and a medium negative association with parent monitoring (r = −.22, p < .001).
Primary Analyses1
A moderated mediation model was examined to further explore the relations among depressive symptoms, parent monitoring, perceived family warmth, and alcohol use, controlling for the effects of age and sex; this model is depicted in Figure 1. The model predicting family warmth (a path) was statistically significant (F[5, 2938] = 21.47, p < .001, R2 = .04), as was the overall model predicting alcohol use (F[7, 4936] = 48.95, p < .001, R2 = .11). Depressive symptoms were statistically significantly associated with less perceived family warmth (b = −.03, SE = .01, β = −.09, t = −5.21, p < .001, 95%CI[−.04, −.02]), which in turn was statistically significantly associated with greater alcohol use (b = −.22, SE = .05, β = −.39, t = −4.87, p < .001, 95%CI[−.30, −.13]). Greater parent monitoring was statistically significantly associated with both more perceived family warmth (b = .07, SE = .01, β = .13, t = 7.01, p < .001, 95%CI [.05, .09]) and with less alcohol use (b = −.29, SE = .03, β = −.94, t = −11.72, p < .001, 95%CI [−.34, −.24]). Further, parent monitoring was found to statistically significantly interact with perceived family warmth to predict alcohol use (path b; b = −.03, SE = .01, β = −.19, t = −3.22, p = .001, 95%CI [−.05, −.01]). Parent monitoring did not statistically significantly interact with depressive symptoms to predict perceived family warmth (path a; b = .002, SE = .002, β = .03, t = 1.49, p = .14, 95%CI [−.001, .01]) nor with depressive symptoms to predict alcohol use (path c’; b = .01, SE = .004, β = .08, t = 1.16, p = .25, 95%CI [−.003, .01]).
Figure 1. Summary of Moderated Mediation Analyses Explicating the Mediating Role of Perceived Family Warmth and the Moderating Role of Parent Monitoring in the Relation Between Depressive Symptoms and Alcohol Use.
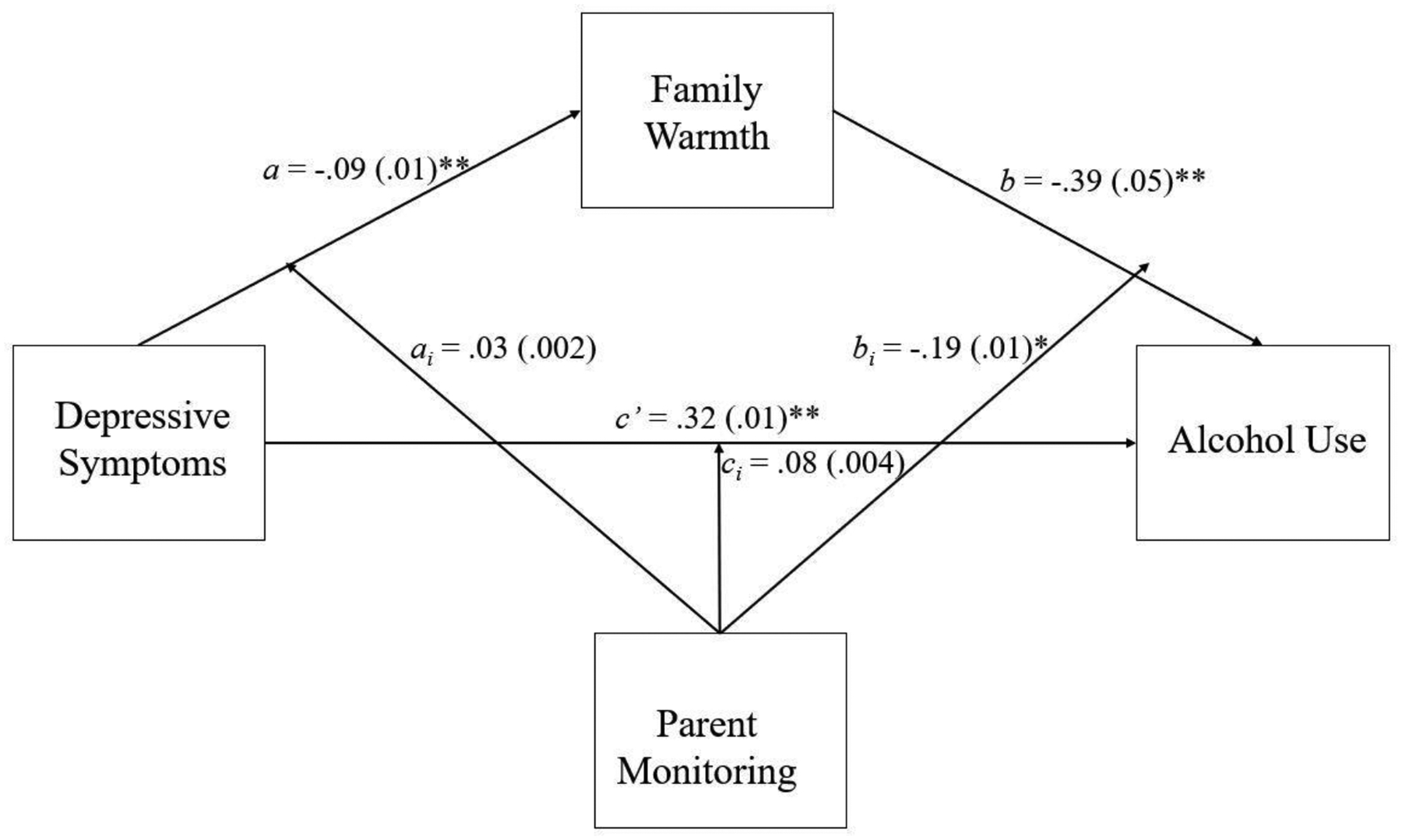
Note. Values presented are standardized bs, values in parentheses are standard errors based on unstandardized regression coefficients; path labels denoted with i represent interaction effects; age and sex are not depicted here but were included as covariates in the model; *p < .01, **p < .001.
Analysis of the statistically significant moderation effect indicated that the path between perceived family warmth and alcohol use was stronger at high levels (1 SD above the mean; b = −.32, SE = .06, β = −.58, t = −5.56, p < .001, 95%CI [−.44, −.21]) of parent monitoring than at low levels (1 SD below the mean; b = −.11, SE = .05, β = −.20, t = −2.14, p = .03, 95%CI [−.22, −.01]). Further, the indirect effect of depressive symptoms on alcohol use through the pathway of perceived family warmth was found to be statistically significant at high (1 SD above the mean; b = .01, SE = .004, β = .04, 95%CI [.00, .02]) but not low levels of parent monitoring (1 SD below the mean; b = .004, SE = .003, β = .02, 95%CI [.00, .01]).
Discussion
The goal of the present study was to examine the roles of perceived family warmth and parent monitoring in the association between depressive symptoms and alcohol use among AI adolescents. First, as expected, we found that depressive symptoms were positively associated with alcohol use at zero-order. This finding extends a large body of literature focusing on non-AI individuals that finds depression and alcohol use to be robustly related (Boden and Fergusson, 2011, Brière et al., 2014) by finding a similar association in a sample of AI adolescents. There is a notable lack of literature focusing on the association between depressive symptoms and alcohol use among AI adolescents; thus, this paper represents a novel and important contribution. Our findings suggest that, when working with AI adolescents presenting for treatment reporting alcohol use, clinicians should assess for depressive symptoms, as they may represent an important risk factor. Conversely, AI adolescents presenting for treatment as a result of depressive symptoms should be screened for alcohol use given that depressive symptoms may increase risk for drinking alcohol. Further, these findings provide support for future research to investigate whether interventions targeting depressive symptoms may have a subsequent positive impact on adolescent alcohol use and vice versa.
As expected, greater perceived family warmth was negatively associated with both depressive symptoms and alcohol at the bivariate level. These results support previous literature finding that families are an important source of strength and resilience for AI adolescents (Limb et al., 2014) and that family environments characterized by conflict (which may be related to low family warmth) are associated with increased risk for alcohol use (Stanley et al., 2014b). It may be that, because AI communities tend to be highly family-oriented and place great importance on the role of the extended family and community (Garrett and Garrett, 1994), low perceived family warmth is associated with negative outcomes like alcohol use. With respect to the observed association between family warmth and depressive symptoms, it may also be that youth who are more depressed perceive their family to care less about them, possibly because of cognitive distortions (e.g., feelings of worthlessness) common in depression (Orchard et al., 2019).
Next, we found that depressive symptoms were associated with less perceived family warmth, which in turn was associated with increased alcohol use, and that these effects were moderated by parent monitoring. Perceiving greater family warmth may suggest that adolescents also have stronger family relationships, which has been identified by AI adolescents as an important alternative reinforcer to alcohol use (Spillane et al., 2020). Further, parent monitoring was shown to moderate this mediation model, such that the negative association between family warmth and alcohol use was stronger at high (versus low) levels of parent monitoring, suggesting that family warmth and parent monitoring both reflect important components of family functioning and that parent monitoring may increase the positive effects of family warmth, or could offset the negative effects of low family warmth, as it relates to youth alcohol use. This finding is supported by existing literature showing that parent monitoring is an important protective factor for AI adolescent substance use (Rodgers-Farmer, 2001, Nalven et al., 2020, Spillane et al., 2017) and that family environments characterized by both warmth and consistent monitoring protect against engagement in health-compromising behaviors, such as alcohol use, among adolescents who are members of historically marginalized racial and ethnic groups (Springer et al., 2002). While traditional approaches to parenting are often non-intrusive and indirect (BigFoot and Funderburk, 2011), previous work focused on AI families has found that more direct monitoring reduces the likelihood that adolescents will engage in alcohol use (Moon et al., 2016, Boyd-Ball et al., 2014).
Findings of the present study have potentially important implications for future research and clinical practice. For instance, family-level interventions may benefit from providing parents with skills focused on strategies to communicate a sense of warmth and to monitor their adolescents. Importantly, such interventions should aim to enhance both warmth and monitoring (or should first aim to enhance warmth then to enhance monitoring rather than promoting monitoring indiscriminately in the absence of behaviors which communicate warmth), given previous research suggesting that children whose parents use authoritative parenting styles (i.e., high warmth and monitoring) report decreased depression and alcohol use compared to those whose parents use authoritarian (i.e., low warmth and high monitoring) or permissive (i.e., high warmth and low monitoring) styles (Piko and Balázs, 2012, Ebrahimi et al., 2017). It is likely that increasing the extent to which parent’s communicate warmth to their youth might facilitate communication and promote child disclosure, a form of parent monitoring which has been found to be most strongly related to reducing risky adolescent behavior (Stattin & Kerr, 2000).
Additionally, prevention and treatment programs targeting youth depressive symptoms and aiming to reduce alcohol use may benefit from the inclusion of family, as has been recommended in previous literature when working with AI individuals (Sue et al., 2019). Such approaches may also reflect a trauma-informed approach given the effects of historical trauma related to colonization and residential boarding schools on family structures and traditional parenting practices (Walls and Whitbeck, 2012, Whitbeck et al., 2014). Future research should continue to examine the nature of the associations among variables of interest in the present study to inform the optimal timing of interventions, as alternative models may provide other important insights. For example, it is likely that the relations examined in the present study are actually bidirectional in nature, though we are not able to test this given the nature of these data. For instance, while we examined depressive symptoms as a predictor of perceived family warmth and alcohol use, longitudinal investigations suggest that parental rejection (similar to low perceived warmth) are prospectively associated with later depressive symptoms (Hipwell et al., 2008; Lloyd et al., 2017). It may be that depression leads adolescents to perceive their families as caring about them less and that this decreased sense of warmth subsequently leads to worsening depressive symptoms. Future research may also benefit from efforts to develop measures including a focus on family monitoring and warmth by members of the extended family and by fictive kin (as opposed to only parent monitoring) given the importance of extended kinship networks in AI communities and the unique role that the extended community plays in monitoring AI youth (Mooradian et al., 2007, Walls and Whitbeck, 2012).
Findings of the present study should be considered in the context of several limitations. First, the cross-sectional and correlational nature of these data precludes our ability to examine the exact nature and directions of these associations; our findings support examining these factors prospectively within a longitudinal framework. Second, this study relied exclusively on self-report measures of depressive symptoms, family factors, and alcohol use. It may be that adolescents have poor insight into their emotional experiences or that their retrospective reports of depressive symptoms and alcohol use were over- or under-inflated (Brener et al., 2003). Additionally, while the measures used in the present study have been used in previous research focusing on substance use among AI adolescents, additional research is needed to examine their psychometric properties. Third, the nature of school-based samples precludes examination of these associations among adolescents who have dropped out of school, including those who may have dropped out of school as a consequence of severe depressive symptoms or patterns of alcohol use, for whom these associations may be especially important (Dupéré et al., 2018). Fourth, this study was a secondary analysis of de-identified data; thus, a community advisory board or tribal IRB review representing the individual communities whose youth are represented in these data was not possible. Future research should ensure that they are incorporating AI community input in the design and conduct of research studies and interpretation of research findings, such as through community-based participatory research methods (Israel et al., 2005). Finally, while the large sample of AI adolescents attending schools on or near reservation communities across 11 states is a notable strength of the present study, it warrants mention that this does not capture the experiences of all AI youth and that the data was collected (in some cases) more than a decade ago. For instance, it is possible that urban versus rural AI youth, or youth who are more or less acculturated, would experience these associations differently. Further, given the relatively low correlation coefficients and small indirect effect identified in the present study, it is likely that there are other factors that would more fully explain the association between depressive symptoms and alcohol use. For instance, socioeconomic status (Steele et al., 2007), mental health stigma (Corrigan et al., 2014; Gary, 2005), and mistrust of medical providers (Goodkind et al., 2011) may contribute to a decreased likelihood of accessing mental health services for depressive symptoms, thereby increasing the likelihood of individuals turning to maladaptive coping strategies, such as alcohol use. Additionally, emotion dysregulation, lack of coping skills, and diminished reinforcement from alternative activities to alcohol use in the context of depressed mood might explain the association between depressive symptoms and alcohol use (Audrain-McGovern et al., 2011; Schick et al., 2019; Wang et al., 2018). Future studies should consider these important contextual factors and should replicate these analyses to understand whether there has been a change in these associations over time.
In summary, results of the present study suggest that family context plays an important role in the association between depressive symptoms and alcohol use among AI adolescents. These findings underscore the importance of recognizing families as a source of protection against alcohol use, especially among AI adolescents also struggling with depressive symptoms. Specifically, parents and other caregivers of AI adolescents who are endorsing depressive symptoms and drinking alcohol should be encouraged to communicate warmth and be equipped with tools to effectively monitor their AI adolescents.
Table 2.
Bivariate Correlations among Variables of Interest
| Construct | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Age | - | .002 | −.04* | .05** | −.09*** | .21*** |
| 2. Sex | - | .10*** | .04* | .18*** | .05** | |
| 3. Depressive Symptoms | - | −.11*** | −.09*** | .11*** | ||
| 4. Perceived Family Warmth | - | .13*** | −.11*** | |||
| 5. Parent Monitoring | - | −.23*** | ||||
| 6. Alcohol Use | - |
Note:
p < .05.
p < .01,
p < .001;
sex is coded such that 0 = male and 1 = female
Table 3.
Summary of Moderated Mediation Analyses
| Path | b | SE | β | t | p | 95% CI |
|---|---|---|---|---|---|---|
| a path | ||||||
| Depressive Symptoms → Family Warmth | −.03 | .01 | −.09 | −5.21 | <.001 | [−.04, −.02] |
| Parent Monitoring → Family Warmth | .07 | .01 | .13 | 7.01 | <.001 | [.05, .09] |
| Age → Family Warmth | .07 | .02 | .07 | 3.92 | <.001 | [.04, .11] |
| Sex → Family Warmth | .09 | .06 | .03 | 1.41 | .16 | [−.04, .22] |
| Depressive Symptoms X Parent Monitoring → Family Warmth | .002 | .002 | .03 | 1.49 | .14 | [−.001, .01] |
| b path | ||||||
| Family Caring → Alcohol Use | −.22 | .05 | −.39 | −4.87 | <.001 | [−.30, −.13] |
| Parent Monitoring → Alcohol Use | −.29 | .03 | −.94 | −11.72 | <.001 | [−.34, −.24] |
| Age → Alcohol Use | .48 | .05 | .82 | 10.68 | <.001 | [.39, .57] |
| Sex → Alcohol Use | .69 | .15 | .34 | 4.45 | <.001 | [.38, .99] |
| Family Warmth X Parent Monitoring → Alcohol Use | −.03 | .01 | −.19 | −3.22 | .001 | [−.05, −.01] |
| c’ path | ||||||
| Depressive Symptoms → Alcohol Use | .06 | .01 | .32 | 4.13 | <.001 | [.03, .08] |
| Depressive Symptoms X Parent Monitoring → Alcohol Use | .01 | .004 | .08 | 1.16 | .25 | [−.003, .01] |
Note. Sex is coded such that 0 = male and 1 = female
Role of Funding Source:
This project was supported by the National Institute on Drug Abuse grant R01DA003371. Work on this paper by the fourth author was supported by National Institutes of Health grants K23DA039327 and P20GM125507.
Footnotes
An additional model was examined with a dichotomously scored lifetime alcohol use variable (coded such that 0 = no lifetime alcohol use and 1 = any lifetime alcohol use) as the outcome to examine whether this model may be more relevant in considering presence (versus absence) of alcohol use versus alcohol use severity. In this model, depressive symptoms remained significantly associated with family monitoring (β = −.09, p < .001) and with lifetime alcohol use (β = .27, p < .001). However, family caring was no longer significantly related to lifetime alcohol use (β = −.02, p = .59), and the indirect effect of depressive symptoms on lifetime alcohol use through the pathway of family warmth was not significant at any level of parent monitoring.
References
- ALLEN J, MOHATT GV, RASMUS SM, HAZEL KL, THOMAS L & LINDLEY S 2006. The tools to understand: Community as co-researcher on culture-specific protective factors for Alaska Natives. Journal of Prevention & Intervention in the Community, 32, 41–59. [DOI] [PubMed] [Google Scholar]
- AUDRAIN-MCGOVERN J, RODRIGUEZ D RODGERS K, & CUEVAS J 2011. Declining alternative reinforcers link depression to young adult smoking. Addiction, 106, 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BACCHINI D, CONCETTA MIRANDA M & AFFUSO G 2011. Effects of parental monitoring and exposure to community violence on antisocial behavior and anxiety/depression among adolescents. Journal of interpersonal violence, 26, 269–292. [DOI] [PubMed] [Google Scholar]
- BAKER TB, PIPER ME, MCCARTHY DE, MAJESKIE MR & FIORE MC 2004. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological review, 111, 33–51. [DOI] [PubMed] [Google Scholar]
- BARNEY DD 2001. Risk and protective factors for depression and health outcomes in American Indian and Alaska Native adolescents. Wicazo Sa Review, 16, 135–150. [Google Scholar]
- BERGE J, SUNDELL K, ÖJEHAGEN A, & HÅKANSSON A 2016. Role of parenting styles in adolescent substance use: Results from a Swedish longitudinal cohort study. BMJ Open, 6, e008979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BIGFOOT DS & FUNDERBURK BW 2011. Honoring children, making relatives: The cultural translation of parent-child interaction therapy for American Indian and Alaska Native families. Journal of psychoactive drugs, 43, 309–318. [DOI] [PubMed] [Google Scholar]
- BODEN JM & FERGUSSON DM 2011. Alcohol and depression. Addiction, 106, 906–914. [DOI] [PubMed] [Google Scholar]
- BOLTON JM, ROBINSON J & SAREEN J 2009. Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Affective Disorders, 115, 367–375. [DOI] [PubMed] [Google Scholar]
- BOSCHLOO L, VOGELZANGS N, SMIT JH, VAN DEN BRINK W, VELTMAN DJ, BEEKMAN AT & PENNINX BW 2011. Comorbidity and risk indicators for alcohol use disorders among persons with anxiety and/or depressive disorders: findings from the Netherlands Study of Depression and Anxiety (NESDA). Journal of Affective Disorders, 131, 233–242. [DOI] [PubMed] [Google Scholar]
- BOYD-BALL AJ, VÉRONNEAU M-H, DISHION TJ & KAVANAGH K 2014. Monitoring and peer influences as predictors of increases in alcohol use among American Indian youth. Prevention Science, 15, 526–535. [DOI] [PubMed] [Google Scholar]
- BRAVE HEART MYH 1999. Oyate ptayela: Rebuilding the Lakota Nation through addressing historical trauma among Lakota parents. In: WEAVER HN (ed.) Voicses of First Nations people: Human services considerations. New York, NY: Haworth Press. [Google Scholar]
- BRENER ND, BILLY JO & GRADY WR 2003. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. Journal of adolescent health, 33, 436–457. [DOI] [PubMed] [Google Scholar]
- BRIÈRE FN, ROHDE P, SEELEY JR, KLEIN D & LEWINSOHN PM 2014. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Comprehensive psychiatry, 55, 526–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CEBALLO R, RAMIREZ C, HEARN KD & MALTESE KL 2003. Community violence and children’s psychological well-being: Does parental monitoring matter? Journal of Clinical Child and Adolescent Psychology, 32, 586–592. [DOI] [PubMed] [Google Scholar]
- CENTERS FOR DISEASE CONTROL AND PREVENTION, NATIONAL CENTER FOR HEALTH STATISTICS. 2020. 1998–2018 Wide Ranging Online Data for Epidemiological Research (WONDER), Multiple Cause of Death files. Retrieved from http://wonder.cdc.gov/uch-icd10.html
- CHEADLE JE & WHITBECK LB 2011. Alcohol use trajectories and problem drinking over the course of adolescence: A study of North American indigenous youth and their caretakers. Journal of Health and Social Behavior, 52, 228–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CLARK DB, DE BELLIS MD, LYNCH KG, CORNELIUS JR & MARTIN CS 2003. Physical and sexual abuse, depression and alcohol use disorders in adolescents: onsets and outcomes. Drug and alcohol dependence, 69, 51–60. [DOI] [PubMed] [Google Scholar]
- COHEN DA, & RICE J 1997. Parenting styles, adolescent substance use, and academic acheivement. Journal of Drug Education, 27, 199–211. [DOI] [PubMed] [Google Scholar]
- CORRIGAN PW, DRUSS BG, & PERLICK DA 2014. The impact of mental illness stigma on seeking and participating in mental health care. Psychological Science in the Public Interest, 15, 37–70. [DOI] [PubMed] [Google Scholar]
- DISHION TJ & MCMAHON RJ 1998. Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical formulation. Clinical Child and Family Psychology Review, 1, 61–75. [DOI] [PubMed] [Google Scholar]
- DUPÉRÉ V, DION E, NAULT-BRIÈRE F, ARCHAMBAULT I, LEVENTHAL T & LESAGE A 2018. Revisiting the link between depression symptoms and high school dropout: Timing of exposure matters. Journal of Adolescent Health, 62, 205–211. [DOI] [PubMed] [Google Scholar]
- EBRAHIMI L, AMIRI M, MOHAMADLOU M & REZAPUR R 2017. Attachment styles, parenting styles, and depression. International Journal of Mental Health and Addiction, 15, 1064–1068. [Google Scholar]
- GADERMANN AM, ALONSO J, VILAGUT G, ZASALAVSKY AM, & KESSLER RC 2012. Comorbidity and disease burden in the National Comorbidity Survey Replication (NCS-R). Depression and Anxiety, 29, 797–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GANZ D & SHER L 2009. Suicidal behavior in adolescents with comorbid depression and alcohol abuse. Minerva Pediatrica, 61, 333–347. [PubMed] [Google Scholar]
- GARRETT J & GARRETT MW 1994. The path of good medicine: Understanding and counseling Native American Indians. Journal of Multicultural Counseling and development, 22, 134–144. [Google Scholar]
- GAYNES BN, WEST SL, FORD CA, FRAME P, KLEIN J, & JOHN KN 2004. Screening for suicide risk in adults: A summary of the evidence for the U.S. Preventative Services Task Force. Annals of Internal Medicine, 140, 822–835. [DOI] [PubMed] [Google Scholar]
- GARY FA 2005. Stigma: Barrier to mental health care among ethnic minorities. Issues in Mental Health Nursing, 26, 979–999. [DOI] [PubMed] [Google Scholar]
- GOODKIND JR, ROSS-TOLEDO K, JOHN S, HALL JL, ROSS L, FREELAND L, COLETTA E, BECENTI-FUNDARK T, POOLA C, & ROANHORSE R 2011. Rebuilding trust: A community, multiagency, state, and university partnership to improve behavioral health care for American Indian youth, their families, and communities. Journal of Community Psychology, 39, 452–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HASIN DS, TSAI WY, ENDICOTT J, MUELLER TI, CORYELL W & KELLER M 1996. The effects of major depression on alcoholism: Five-year course. The American Journal on Addictions, 5, 144–155. [DOI] [PubMed] [Google Scholar]
- HAWKINS EH, CUMMINS LH & MARLATT GA 2004. Preventing substance abuse in American Indian and Alaska Native youth: promising strategies for healthier communities. Psychological Bulletin, 130, 304. [DOI] [PubMed] [Google Scholar]
- HAWTON K, I COMABELLA CC, HAW C, & SAUNDERS K 2013. Risk factors for suicide in individuals with depression: A systematic review. Journal of Affective Disorders, 147, 17–28. [DOI] [PubMed] [Google Scholar]
- HAYES AF 2018. Introduction to Mediation, Moderation and Conditional Process Analysis: A Regression-Based Approach, New York, NY, The Guilford Press. [Google Scholar]
- HENRY KL, MCDONALD JN, OETTING ER, SILK WALKER P, WALKER RD & BEAUVAIS F 2011. Age of onset of first alcohol intoxication and subsequent alcohol use among urban American Indian adolescents. Psychology of addictive behaviors, 25, 48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HENSON M, SABO S, TRUJILLO A & TEUFEL-SHONE N 2017. Identifying protective factors to promote health in American Indian and Alaska Native adolescents: A literature review. The Journal of Primary Prevention, 38, 5–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIPWELL A, KEENAN K, KASZA K, LOEBER R, STOUTHAMER-LOEBER M, & BEAN T 2008. Reciprocal influences between girls’ conduct problems and depression, and parental punishment and warmth: A six year prospective analysis. Journal of Abnormal Child Psychology, 36, 663–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HUPPERT FA, ABBOTT RA, PLOUBIDIS GB, RICHARDS M & KUH D 2010. Parental practices predict psychological well-being in midlife: life-course associations among women in the 1946 British birth cohort. Psychological Medicine, 40, 1507–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HURDLE DE, OKAMOTO SK & MILES B 2003. Family influences on alcohol and drug use by American Indian youth: Implications for prevention. Journal of Family Social Work, 7, 53–68. [Google Scholar]
- ISRAEL BA, ENG E, SCHULZ AJ, & PARKER EA 2005. Methods in community-based participatory research for health. San Francisco: Jossey-Bass. [Google Scholar]
- KANDEL DB, JOHNSON JG, BIRD HR, WEISSMAN MM, GOODMAN SH, LAHEY BB, REGIER DA & SCHWAB-STONE ME 1999. Psychiatric comorbidity among adolescents with substance use disorders: Findings from the MECA study. Journal of the American Academy of Child & Adolescent Psychiatry, 38, 693–699. [DOI] [PubMed] [Google Scholar]
- KERR M & STATTIN H 2000. What parents know, how they know it, and several forms of adolescent adjustment: Further support for a reinterpration of monitoring. Developmental Psychology, 36, 366–380. [PubMed] [Google Scholar]
- KHANTZIAN EJ 1997. The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harvard Review of Psychiatry, 4, 231–244. [DOI] [PubMed] [Google Scholar]
- KING J, BEALS J, MANSON SM & TRIMBLE JE 1992. A structural equation model of factors related to substance use among American Indian adolescents. Drugs & Society, 6, 253–268. [Google Scholar]
- KOPAK AM & HAWLEY FF 2012. Family warmth and delinquency among Mexican American and White youth: Detailing the causal variables. Journal of Juvenile Justice, 1, 52–67. [Google Scholar]
- KUNTSCHE E, KUENDIG H & GMEL G 2008. Alcohol outlet density, perceived availability and adolescent alcohol use: a multilevel structural equation model. Journal of Epidemiology & Community Health, 62, 811–816. [DOI] [PubMed] [Google Scholar]
- LIMB GE, SHAFER K & SANDOVAL K 2014. The impact of kin support on urban American Indian families. Child & Family Social Work, 19, 432–442. [Google Scholar]
- LLOYD B, MACDONALD JA, YOUSSEF GJ, KNIGHT T, LETCHER P, SANSON A, & OLSSON CA 2017. Negative reactivity and parental warmth in early adolescence and depressive symptoms in emerging adulthood. Australian Journal of Psychology, 69, 121–129. [Google Scholar]
- MACKINNON DP, LOCKWOOD CM, HOFFMAN JM, WEST SG & SHEETS V 2002. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MARTIN D & YURKOVICH E 2014. “Close-knit” defines a healthy Native American Indian family. Journal of Family Nursing, 20, 51–72. [DOI] [PubMed] [Google Scholar]
- MOON H, ROH S, LEE Y-S & GOINS RT 2016. Disparities in health, health care access, and life experience between American Indian and White adults in South Dakota. Journal of Racial and Ethnic Health Disparities, 3, 301–308. [DOI] [PubMed] [Google Scholar]
- MOORADIAN JK, CROSS SL & STUTZKY GR 2007. Across generations: Culture, history, and policy in the social ecology of American Indian grandparents parenting their grandchildren. Journal of Family Social Work, 10, 81–101. [Google Scholar]
- NALVEN T, SPILLANE NS & SCHICK MR 2020. Risk and Protective Factors for Opioid Misuse in American Indian Adolescents. Drug and Alcohol Dependence, 206, 107736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OETTING E, EDWARDS R & BEAUVAIS F 1985. Reliability and discriminant validity of the Children’s Drug-Use Survey. Psychological Reports, 56, 751–756. [DOI] [PubMed] [Google Scholar]
- ORCHARD F, PASS L & REYNOLDS S 2019. ‘I Am Worthless and Kind’; the specificity of positive and negative self‐evaluation in adolescent depression. British Journal of Clinical Psychology, 58, 260–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PIKO BF & BALÁZS MÁ 2012. Authoritative parenting style and adolescent smoking and drinking. Addictive behaviors, 37, 353–356. [DOI] [PubMed] [Google Scholar]
- PREACHER KJ & HAYES AF 2004. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior research methods, instruments, & computers, 36, 717–731. [DOI] [PubMed] [Google Scholar]
- RED HORSE JG 1980. Family structure and value orientation in American Indians. Social casework, 61, 462–467. [Google Scholar]
- RODGERS-FARMER AY 2001. Parental monitoring and peer group association: Their influence on adolescent substance use. Journal of Social Service Research, 27, 1–18. [Google Scholar]
- ROHNER RP, KHALEQUE A, & COURNOYER DE 2012. Introduction ro parental acceptance-rejection theory, methods, evidence, and implications. Journal of Family Theory & Review, 2, 73–87. [Google Scholar]
- RYAN SM, JORM AF & LUBMAN DI 2010. Parenting factors associated with reduced adolescent alcohol use: a systematic review of longitudinal studies. Australian and New Zealand Journal of Psychiatry, 44, 774–783. [DOI] [PubMed] [Google Scholar]
- SCHICK MR, GOLDSTEIN SC, NALVEN T & SPILLANE NS 2021. Alcohol-and drug-related consequences across latent classes of substance use among American Indian adolescents. Addictive behaviors, 113, 106682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCHICK MR, NALVEN T, & SPILLANE NS 2020. The factor structure of self-esteem and its association with alcohol use in American Indian adolescents. American Journal of Orthopsychiatry, 90(6), 712–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCHICK MR, WEISS NH, CONTRACTOR A, DIXON-GORDON KL, & SPILLANE NS 2019. Depression and risky alcohol use: An examination of the role of difficulties regulating positive emotions in trauma-exposed individuals. The American Journal of Drug and Alcohol Abuse, 45, 323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHAKYA HB, CHRISTAKIS NA & FOWLER JH 2012. Parental influence on substance use in adolescent social networks. Archives of pediatrics & adolescent medicine, 166, 1132–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SKEWES MC & BLUME AW 2015. Ethnic identity, drinking motives, and alcohol consequences among Alaska Native and non-native college students. Journal of Ethnicity in Substance Abuse, 14, 12–28. [DOI] [PubMed] [Google Scholar]
- SLAVIN LA, & RAINER KL 1990. Gender differences in emotional support and depressive symptoms among adolescents: A prospective analysis. American Journal of Community Psychology, 18, 407–421. [DOI] [PubMed] [Google Scholar]
- SNIPP CM 2005. American Indian and Alaska Native children: Results from the 2000 census. Washington, DC: Population Reference Bureau. [Google Scholar]
- SPILLANE NS, GREENFIELD B, VENNER K & KAHLER CW 2015. Alcohol use among reserve-dwelling adult First Nation members: Use, problems, and intention to change drinking behavior. Addictive behaviors, 41, 232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPILLANE NS, KIRK-PROVENCHER KT, SCHICK MR, NALVEN T, GOLDSTEIN SC & KAHLER CW 2020. Identifying Competing Life Reinforcers for Substance Use in First Nation Adolescents. Substance Use & Misuse, 55, 886–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPILLANE NS & VENNER K 2018. American Indian Adolescents. In: MONTI PM, COLBY SM & O’LEARY TA (eds.) Brief Interventions for Adolescent Alcohol and Substance Abuse. New York, NY: The Guilford Press. [Google Scholar]
- SPILLANE NS, WEYANDT L, OSTER D & TRELOAR H 2017. Social contextual risk factors for stimulant use among adolescent American Indians. Drug and Alcohol Dependence, 179, 167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SPRINGER JF, SAMBRANO S, SALE E, KASIM R & HERMAN J 2002. Preventing substance abuse: Major findings from the National Cross-Site Evaluation of High-Risk Youth Programs, Rockville, MD. [DOI] [PubMed] [Google Scholar]
- STANLEY LR, HARNESS SD, SWAIM RC & BEAUVAIS F 2014a. Rates of substance use of American Indian students in 8th, 10th, and 12th grades living on or near reservations: Update, 2009–2012. Public Health Reports, 129, 156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STANLEY LR, MILLER KA, BEAUVAIS F, WALKER PS & WALKER RD 2014b. Predicting an alcohol use disorder in urban American Indian youths. Journal of Child & Adolescent Substance Abuse, 23, 101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- STATTIN H & KERR M 2000. Parental monitoring: A reinterpretation. Child Development, 71, 1072–1085. [DOI] [PubMed] [Google Scholar]
- STEELE L, DEWA C, & LEE K 2007. Socioeconomic status and self-reported barriers to mental health service use. The Canadian Journal of Psychiatry, 52, 201–206. [DOI] [PubMed] [Google Scholar]
- STEWART SH, SHERRY SB, COMEAU MN, MUSHQUASH CJ, COLLINS P & VAN WILGENBURG H 2011. Hopelessness and excessive drinking among aboriginal adolescents: The mediating roles of depressive symptoms and drinking to cope. Depression research and treatment, 2011, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SUE DW, SUE D, NEVILLE HA & SMITH L 2019. Counseling the culturally diverse: Theory and practice, John Wiley & Sons. [Google Scholar]
- SWAIM RC, OETTING ER, THURMAN PJ, BEAUVAIS F, & EDWARDS RW 1993. American Indian adolescent drug use and socialization characteristics: A cross-cultural comparison. Journal of Cross-Cultural Psychology, 24, 53–70. [Google Scholar]
- SWAIM RC 2015. The moderating effects of perceived emotional benefits on inhalant initiation among American Indian and White youth. The American Journal on Addictions, 24(6), 554–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SWAIM RC & STANLEY LR 2016. Multivariate family factors in lifetime and current marijuana use among American Indian and White adolescents residing on or near reservations. Drug and Alcohol Dependence, 169, 92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SWAIM RC & STANLEY LR 2018. Substance use among American Indian youths on reservations compared with a national sample of US adolescents. JAMA network open, 1, e180382–e180382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TABACHNICK BG, FIDELL LS & ULLMAN JB 2007. Using multivariate statistics, Pearson Boston, MA. [Google Scholar]
- TEZEL A, KARABULUTLU E, & ŞAHIN Ö 2011. Depression and perceived social support from family in Turkish patients with chronic renal failure treated by hemodialysis. Journal of Research in Medical Sciences, 16, 666–673. [PMC free article] [PubMed] [Google Scholar]
- TINGEY L, CWIK M, CHAMBERS R, GOKLISH N, LARZELERE-HINTON F, SUTTLE R, LEE A, ALCHESAY M, PARKER A & BARLOW A 2017. Motivators and Influences on American Indian Adolescent Alcohol Use and Binge Behavior: A Qualitative Exploration. Journal of Child & Adolescent Substance Abuse, 26, 75–85. [Google Scholar]
- TURNER S, MOTA N, BOLTON J & SAREEN J 2018. Self‐medication with alcohol or drugs for mood and anxiety disorders: A narrative review of the epidemiological literature. Depression and anxiety, 35, 851–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES. 2019. 2019 NSDUH Detailed Tables [Online]. Available: https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect9pe2019.htm#tab9-5a [Accessed].
- US DEPARTMENT OF HEALTH AND HUMAN SERVICES 2010. Results From the 2009 National Survey on Drug Use and Health, Volume I: Summary of National Findings: 1.1, Summary of NSDUH.
- VAETH PA, WANG‐SCHWEIG M & CAETANO R 2017. Drinking, alcohol use disorder, and treatment access and utilization among US racial/ethnic groups. Alcoholism: Clinical and Experimental Research, 41, 6–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WALLS ML & WHITBECK LB 2012. The intergenerational effects of relocation policies on indigenous families. Journal of Family Issues, 33, 1272–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WALTERS KL, MOHAMMED SA, EVANS-CAMPBELL T, BELTRÁN RE, CHAE DH & DURAN B 2011. Bodies don’t just tell stories, they tell histories: Embodiment of historical trauma among American Indians and Alaska Natives. Du Bois Review: Social Science Research on Race, 8, 179–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WANG K, BURTON CL, & PACHANKIS JE 2018. Depression and substance use: Towards the development of an emotion regulation model of stigma coping. Substance Use and Misuse, 53, 859–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHITBECK LB, WALLS M & HARTSHORN K 2014. Indigenous adolescent development: Psychological, social and historical contexts, Psychology Press. [Google Scholar]
- WHITESELL NR, ASDIGIAN NL, KAUFMAN CE, CROW CB, SHANGREAU C, KEANE EM, MOUSSEAU AC & MITCHELL CM 2014. Trajectories of substance use among young American Indian adolescents: Patterns and predictors. Journal of youth and adolescence, 43, 437–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YAP MBH, PILKINGTON PD, RYAN SM & JORM AF 2014. Parental factors associated with depression and anxiety in young people: A systematic review and meta-analysis. Journal of Affective Disorders, 156, 8–23. [DOI] [PubMed] [Google Scholar]
- YU M, & STIFFMAN AR 2007. Culture and environment as predictors of alcohol abuse/dependence symptoms in American Indian youth. Addictive Behaviors, 32, 2253–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- YUAN NP, EAVES ER, KOSS MP, POLACCA M, BLETZER K & GOLDMAN D 2010. “Alcohol is something that been with us like a common cold”: Community perceptions of American Indian drinking. Substance Use & Misuse, 45, 1909–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]


