Abstract
To describe the presentation of both new-onset and reactivation of thyroid eye disease (TED) following COVID-19 vaccination. Single-institution retrospective case series of patients presenting with symptoms and signs of new or reactivated TED coinciding with recent COVID-19 vaccination. Data collected included patient age, gender, presenting symptoms, ocular history, clinical signs, and interval duration between vaccination and onset of ocular symptoms. Three female patients were identified. All patients were over 18 years of age (range 45–66 years). Patients received either the Moderna or Pfizer COVID-19 vaccine and presented with symptoms of TED within 24 h to 21 days of receiving their first or second dose. None of the patients had previous infections with severe acute respiratory syndrome coronavirus 2. Two patients had a history of inactive TED with stable thyroid function tests: One of these patients had stable disease for at least 15 years and the other had stable disease for 5 years. The third patient had no previous history of thyroid dysfunction or TED and presented with low levels of thyroid-stimulating hormone. All three cases presented with proptosis. In two of three cases, periorbital edema, eyelid retraction, and diplopia were present. None were current smokers. One had prior facial hyaluronic acid filler injections. Symptoms in all cases were improving at 4 to 8 months. While the possibility of unrelated TED flaring concurrently with COVID-19 vaccination exists, questions remain on the effects of the COVID-19 vaccine in patients with autoimmune ophthalmic diseases. Physicians should be aware of this potential association and counsel patients appropriately.
Keywords: Autoimmune, COVID-19 vaccination, Graves’ disease, thyroid eye disease
Introduction
Thyroid eye disease (TED) is an autoimmune disease characterized by enlargement of the extraocular muscles and fatty and connective tissue with an incidence rate of approximately 19 in 100,000 people/year.[1,2] TED is commonly associated with Graves’ disease but also occurs in patients with other autoimmune thyroid diseases, including Hashimoto's thyroiditis. TED is a serious, debilitating condition that can lead to blindness in severe cases.
In response to the severe acute respiratory syndrome coronavirus 2 pandemic, several vaccines have been developed to protect against COVID-19 infection. The American College of Rheumatology noted a possible risk of reactivation of autoimmune disease after COVID-19 vaccination,[3] and there have been several reports of autoimmune disease flares following COVID-19 vaccination, including rheumatoid arthritis and myasthenia gravis.[4,5,6,7] In addition, there have been a few cases of new-onset Graves’ disease and subacute thyroiditis following COVID-19 vaccination reported.[8,9,10,11]
To the best of our knowledge, only one case of new-onset TED after COVID-19 vaccination has been previously reported,[12] and this is the first description of a TED reactivation following COVID-19 vaccination. This study describes the presentation of both new-onset and reactivation of TED in temporal association with COVID-19 vaccination.
The collection and evaluation of protected patient health information were Health Insurance Portability and Accountability Act compliant, and patient consent was obtained.
Case Report
Case 1
A 66-year-old nonsmoking female presented with new-onset diplopia, bilateral eye-bulging, and pain with eye movement [Figure 1]. She reported constant vertical diplopia, needing to use chin-up posture to achieve a single vision. Symptom onset was 3 weeks after receiving the second dose of the messenger ribonucleic acid (mRNA)-1273 (Moderna) COVID-19 vaccine. She had a history of Grave's disease treated with radioactive iodine and TED, stable for over 15 years, treated with bilateral orbital decompression and bilateral strabismus surgery over 20 years ago. Recent thyroid function tests were stable on levothyroxine. Visual acuity was 20/20 OU. Confrontational visual fields were full bilaterally. Pupils were symmetric and reactive with no afferent pupillary defect. Margin reflex distance 1 was 3.5 mm OU. Hertel exophthalmometry measurements were 21 mm OU at a base of 63. External examination showed bilateral periorbital edema and proptosis. The conjunctiva was mildly injected bilaterally. The clinical activity score was 6. Repeat laboratory testing showed normal free thyroxine (1.70 ng/dL), low thyroid-stimulating hormone (0.04 uIU/mL), and elevated thyroid-stimulating immunoglobulin (3.91 IU/L) and thyrotropin receptor antibody (5.51 IU/L). Magnetic resonance imaging of the orbits demonstrated asymmetric enhancement, edema, and enlargement of the inferior rectus muscles. The patient was started on teprotumumab infusion, and her symptoms were improving at 5 months.
Figure 1.
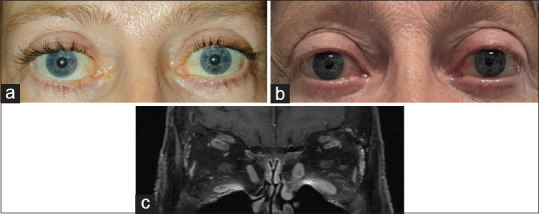
Sixty six-year-old female with a history of Graves disease, stable for at least 15 years, who had undergone bilateral orbital decompression 20 years prior (a), presenting with new-onset bilateral proptosis and periorbital edema 3 weeks after the second dose of the Moderna COVID-19 vaccine (b). Coronal magnetic resonance imaging demonstrating enhancement and edema of the inferior rectus muscles (c)
Case 2
A 53-year-old non-smoking female with no previous history of TED presented to clinic with new-onset bulging and pain with eye movement in the right eye and occasional diplopia [Figure 2]. Symptom onset was within 24 h after receiving the first dose of the BNT162b2 mRNA (Pfizer) COVID-19 vaccine. She was recently started on methimazole elsewhere for low thyroid-stimulating hormone levels after receiving the vaccine. Visual acuity was 20/25 OU. Confrontational visual fields were full bilaterally. Pupils were symmetric and reactive with no afferent pupillary defect. Margin reflex distance 1 was 7.5 mm OD and 5.0 mm OS. Hertel exophthalmometry measurements were 17 OD and 15 OS at a base of 61. External examination showed bilateral periorbital edema and proptosis, right upper lid lag on downgaze, and upper and lower eyelid retraction in the right eye. Laboratory testing showed normal thyroid-stimulating hormone (0.99 uIU/mL), low free thyroxine (0.9 ng/dL), and elevated thyroid-stimulating immunoglobulin (3.21 IU/L). Magnetic resonance imaging of the orbits demonstrated mild edema and diffuse enlargement of the bilateral inferior rectus, right greater than left superior rectus, and bilateral medial rectus and lacrimal gland enhancement. Given that a lacrimal gland mass would be unusual for TED, biopsy of the lacrimal gland was done, and pathology demonstrated lacrimal gland inflammation. One month later, the patient developed worsening pain with eye movements and conjunctival redness. She was started on teprotumumab infusion, and her symptoms were improving at 8 months.
Figure 2.
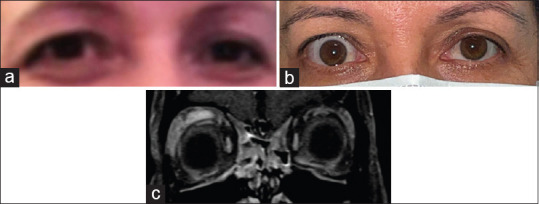
Fifty three-year-old female with no previous history of thyroid eye disease (a) presenting with new-onset proptosis and upper and lower eyelid retraction in the right eye within 24 h after the first dose of the Pfizer COVID-19 vaccine (b). Coronal magnetic resonance imaging demonstrating mild edema and diffuse enlargement of the bilateral inferior rectus, right greater than left superior rectus, and bilateral medial rectus and lacrimal gland enhancement (c)
Case 3
A 45-year-old nonsmoking female presented to clinic with worsening eyelid swelling. Symptom onset was 3 weeks after the first dose of the mRNA-1273 (Moderna) COVID-19 vaccine. Eyelid swelling also worsened after the second dose of the vaccine. She denied pain, redness, or diplopia. She had a history of Hashimoto's thyroiditis, TED, stable for 5 years, and bilateral hyaluronic acid filler injections several months ago. Recent thyroid function tests were stable. Visual acuity was 20/20 OU. Confrontational visual fields were full bilaterally. Pupils were symmetric and reactive with no afferent pupillary defect. Margin reflex distance 1 was 4.0 mm OU. External examination demonstrated trace proptosis, mild bilateral lower eyelid edema worse in the left eye, and bilateral lower eyelid retraction. The patient reported that thyroid function tests done elsewhere were abnormal after she received the vaccine. Four months later, the eyelid swelling reduced, and her thyroid function tests normalized without treatment.
Discussion
While the possibility of unrelated TED flaring concurrently with COVID-19 vaccination exists, the timing of symptoms in all three cases suggests an association between TED and the vaccine. Two of the patients had well-controlled TED for many years before vaccination, and the third patient had no prior history of TED. There were no inciting events, including changes in smoking status, pregnancy, or recent surgeries. While one patient had prior facial hyaluronic acid filler injections, which has been associated with delayed inflammatory reactions after COVID-19 vaccination,[13,14] her presentation was more consistent with TED reactivation. Additionally, in all three cases, the timing of TED and the vaccine was similar to that of the previous reports of autoimmune disease flares after the COVID-19 vaccine.[4,5,6,7]
One case of new-onset TED following COVID-19 vaccination has been previously reported and demonstrated a similar interval duration between vaccination and onset of ocular symptoms, presenting symptoms, and outcome to our cases.[12] However, unlike the case in the literature, the three cases here showed evidence of thyroid dysfunction on laboratory testing after vaccination.
In these cases, it is possible that TED was triggered by immune activation or non-specific adjuvant effects after COVID-19 vaccination. Autoimmune/inflammatory syndrome induced by adjuvants has been previously described and may occur following exposure to various adjuvants, which comprise many vaccines and are capable of inducing immune reactions, including molecular mimicry.[15]
All vaccinations have risks, and given the efficacy of the COVID-19 vaccines, we believe the benefits outweigh the risk of flares. The American College of Rheumatology also continues to recommend the vaccine to all who are eligible, including those with immune-mediated disease.[3] However, questions remain on the effects of the COVID-19 vaccine in patients with autoimmune ophthalmic diseases, and physicians should be aware of this potential association and counsel patients appropriately.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Generously supported by the Bell Charitable Foundation, Mrs. Toby Wolf, and Research to Prevent Blindness
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Bartley GB, Fatourechi V, Kadrmas EF. Clinical features of Graves’ ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996;121:284–90. doi: 10.1016/s0002-9394(14)70276-4. [DOI] [PubMed] [Google Scholar]
- 2.Bartley GB. The epidemiologic characteristics and clinical course of ophthalmopathy associated with autoimmune thyroid disease in Olmsted County, Minnesota. Trans Am Ophthalmol Soc. 1994;92:477. [PMC free article] [PubMed] [Google Scholar]
- 3.Curtis JR, Johnson SR, Anthony DD, Arasaratnam RJ, Baden LR, Bass AR, et al. American College of Rheumatology guidance for COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases: Version 1. Arthritis Rheumatol. 2021;73:1093–107. doi: 10.1002/art.41734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Terracina KA, Tan FK. Flare of rheumatoid arthritis after COVID-19 vaccination. Lancet Rheumatol. 2021;3:e469–70. doi: 10.1016/S2665-9913(21)00108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishay Y, Kenig A, Tsemach-Toren T, Amer R, Rubin L, Hershkovitz Y, et al. Autoimmune phenomena following SARS-CoV-2 vaccination. Int Immunopharmacol. 2021;99:107970. doi: 10.1016/j.intimp.2021.107970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watad A, De Marco G, Mahajna H, Druyan A, Eltity M, Hijazi N, et al. Immune-mediated disease flares or new-onset disease in 27 subjects following mRNA/DNA SARS-CoV-2 vaccination. Vaccines (Basel) 2021;9:435. doi: 10.3390/vaccines9050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaulen LD, Doubrovinskaia S, Mooshage C, Jordan B, Purrucker J, Haubner C, et al. Neurological autoimmune diseases following vaccinations against SARS-CoV-2: A case series. Eur J Neurol. 2022;29:555–63. doi: 10.1111/ene.15147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vera-Lastra O, Ordinola Navarro A, Cruz Domiguez MP, Medina G, Sánchez Valadez TI, Jara LJ. Two cases of Graves’ disease following SARS-CoV-2 vaccination: An autoimmune/inflammatory syndrome induced by adjuvants. Thyroid. 2021;31:1436–9. doi: 10.1089/thy.2021.0142. [DOI] [PubMed] [Google Scholar]
- 9.İremli BG, Şendur SN, Ünlütürk U. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine: Postvaccination ASIA syndrome. J Clin Endocrinol Metab. 2021;106:2600–5. doi: 10.1210/clinem/dgab373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel KR, Cunnane ME, Deschler DG. SARS-CoV-2 vaccine-induced subacute thyroiditis. Am J Otolaryngol. 2021;43:103211. doi: 10.1016/j.amjoto.2021.103211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soltanpoor P, Norouzi G. Subacute thyroiditis following COVID-19 vaccination. Clin Case Rep. 2021;9:e04812. doi: 10.1002/ccr3.4812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rubinstein TJ. Thyroid eye disease following COVID-19 vaccine in a patient with a history graves’ disease: A case report. Ophthalmic Plast Reconstr Surg. 2021;37:e221–3. doi: 10.1097/IOP.0000000000002059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gotkin RH, Gout U, Sattler S, Piansay-Soriano ME, Wanitphakdeedecha R, Ghannam S, et al. Global recommendations on COVID-19 vaccines and soft tissue filler reactions: A survey-based investigation in cooperation with the International Society for Dermatologic and Aesthetic Surgery (ISDS) J Drugs Dermatol. 2021;20:374–8. doi: 10.36849/JDD.2021.6041. [DOI] [PubMed] [Google Scholar]
- 14.Michon A. Hyaluronic acid soft tissue filler delayed inflammatory reaction following COVID-19 vaccination – A case report. J Cosmet Dermatol. 2021;20:2684–90. doi: 10.1111/jocd.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shoenfeld Y, Agmon-Levin N. ’ASIA’ – Autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36:4–8. doi: 10.1016/j.jaut.2010.07.003. [DOI] [PubMed] [Google Scholar]


