Mini Abstract
The extent to which advanced practice providers have been integrated into surgical practice, and their impact on surgical outcomes and access is unclear. Our objective was to assess the effects of adding advanced practice providers to surgical practices on surgical complications, readmissions, mortality, episode spending, length of stay and access to care.
Keywords: quality, access, cost
Introduction
Borne out of the need to meet the growing demand for primary care, there has been tremendous growth in the number of nurse practitioners and physician assistants (collectively referred to as advanced practice providers) in the U.S., with more than 350,000 such providers currently.1 Further, the role of these advanced practice providers is expanding rapidly, with nearly a third of primary care involving shared or independent care models.2 Importantly, the quality of care provided by advanced practice providers in many cases is similar to that of their physician counterparts3,4 and is associated with better patient satisfaction and a lower risk of hospitalization and mortality in select patients.5 Not surprisingly, healthcare systems have integrated advanced practice providers into their delivery models to improve access, quality and care coordination.6
However, the extent to which advanced practice providers have been integrated into surgical practice is unclear. These providers can potentially function in both the inpatient (i.e., operating room, postoperative hospital-based care) and outpatient (i.e., postoperative ambulatory care) settings. A central advantage of this delivery model is to improve access to surgical care by allowing surgeons to perform procedures more efficiently (e.g., assistance in the operating room, management of inpatients) or to see new patients who may have need of their services (e.g., by offloading established patient visits). Further, in primary care, advanced practice providers have been shown to be better at coordinating care compared with physicians,3,4,7 which has the potential to improve outcomes (e.g., complications, readmissions) postoperatively. Potential disadvantages of this model relate to the relative inexperience of advanced practice providers with respect to postoperative care, which may result in delayed complication recognition and increased resource use (e.g., through greater use of diagnostic testing or consulting physicians), both of which may contribute to worse patient outcomes (e.g., mortality) and increased spending.
For these reasons, we used national Medicare data to assess the effects of advanced practice providers integrated into single-specialty surgical practices. With anticipated shortfalls in access to surgery, both due to growing demand and stagnant supply,8 understanding the implications of surgeon extenders is paramount to ensuring access to high quality surgical care.
Methods
Data and study population
Using a 20% sample of national Medicare claims, we performed a retrospective cohort study of fee-for-service beneficiaries undergoing one of four major procedures (coronary artery bypass graft [CABG], colectomy, major joint [hip or knee] replacement, and cystectomy) between 2010 and 2016. We chose these procedures because they are either common among the elderly (CABG, major joint replacement) or are associated with higher rates of morbidity and/or mortality (colectomy, cystectomy). We identified procedures using Part B claims and linked them with the corresponding hospitalizations in MEDPAR. All patients were followed for at least 90 days after the index surgery. We limited the cohort to patients 66 years of age and older to allow for assessment of baseline health status in the year preceding the index procedure.9 Only patients with continuous enrollment in Medicare Parts A and B for one year before and 90 days after the procedure were included. Patients participating in Medicare managed care plans were excluded to ensure the availability of complete claims.
Direct interactions of advanced practice providers with patients are incompletely captured in claims perioperatively, either due to payment incentives (i.e., advanced practice providers are reimbursed 85% of physicians when billing independently vs. 100% when billing under the physician NPI as a shared visit)10 or to the global period of surgery (e.g., postoperative visits are not captured because they are included with reimbursement for the procedure itself). Thus, we further limited our study population for each procedure to patients treated by single-specialty surgical groups to ensure that advanced practice providers, who are embedded within them, have direct interactions with its surgeons and patients. For this purpose, each surgeon was associated with a group practice, based on tax-identification number (TIN), using data from the Medicare Data on Provider Practice and Specialty (MD-PPAS) file version 2 from the Centers for Medicare & Medicaid Services.11 This file provides data on Medicare providers (surgeons and advanced practice providers), including their specialties and TINs. Because there has been significant horizontal and vertical integration over the time period, with associated loss of some TINs and change in practice context (e.g., single-specialty group is acquired by a hospital), we limited our study to practices with 3 consecutive years of claims during which the practice added at least one advanced practice provider for the first time in the middle year of the period; such practices could then be studied with a pre-post model specification. The middle year (i.e., the year of addition) served as a wash-out-period.
Outcomes
All outcomes of the study were measured for the year before (“pre”) and the year after (“post”) the addition of the first advanced practice provider to a single-specialty surgical group practice. The primary outcomes were assessed at the patient level using claims from MEDPAR. Outcomes were assessed at both 30- and 90-days post-procedure. One set of measures reflected perioperative quality and included complications (i.e., a composite measure based on the occurrence of at least one AHRQ patient safety indicator),12 readmission and mortality. A second set reflected utilization and included length of stay for the index hospitalization and episode payments, as advanced practice providers may impact care coordination during the hospitalization and resource use post-discharge. Episode payments were inclusive of all payments made by Medicare for the 30- and 90-day periods after the index procedure. All payments were inflated to 2016 dollars. As a secondary outcome, we assessed access to surgeons at the practice-level. We hypothesized that adding advanced practice providers could increase the number of patients seen by a practice in the ambulatory setting. For this purpose, we ascribed all new and established evaluation and management codes billed to Medicare to all NPI’s, inclusive of both surgeons and advanced practice providers, within a surgical practice. The measure was standardized to the number of surgeons within a practice to account for growth or contraction in each group’s size. We determined the ratio of the number of evaluation and management visits performed in both the pre- and post- years divided by the number of surgeons in the practice for that year (i.e., in the case of CABG, the relevant included specialty codes were 33 [thoracic surgery] and 78 [cardiac surgery]).
Analysis
For each of the procedure cohorts, we first compared patient characteristics in the year before the addition of an advanced practice provider to a surgical practice with the year after. Socioeconomic class, measured at the level of the patient’s zip code,13 and comorbidity9 were enumerated using established methods. We used the t-test and Chi Square test for continuous and discrete data, respectively.
Next, for each dichotomous outcome (complications, readmission and mortality) we fit logistic regression models inclusive of all procedure cohorts, separately for 30- and 90-day post-procedure endpoints. For each outcome, all procedure types were combined to increase statistical power and to allow us to observe the effect of surgical practice type. For all models, the patient was the unit of analysis and the exposure of interest was the post-addition year, with the pre-addition year serving as the reference. Models were adjusted for patient characteristics (i.e., age, race, sex, comorbidity, socioeconomic class at the zip code level) and procedure type (i.e., CABG, colectomy, major joint replacement and cystectomy). We used linear regression to assess patient-level length of stay for the index procedure and episode spending at 30- and 90-days post-procedure, adjusting for the aforementioned characteristics.
With respect to our secondary outcome of access, we used linear regression to assess the effect of the addition of advanced practice providers on the ratio of office visits to relevant practice specialists. A higher ratio indicated more patient access per surgeon.
All analyses were carried out using SAS 9.4 (Cary, NC). Model predicted probabilities were derived using the lsmeans command. All tests were two-sided with probability of Type 1 error (alpha) set at 0.05. This study used de-identified claims data and was deemed exempt from review by the institutional review board.
Results
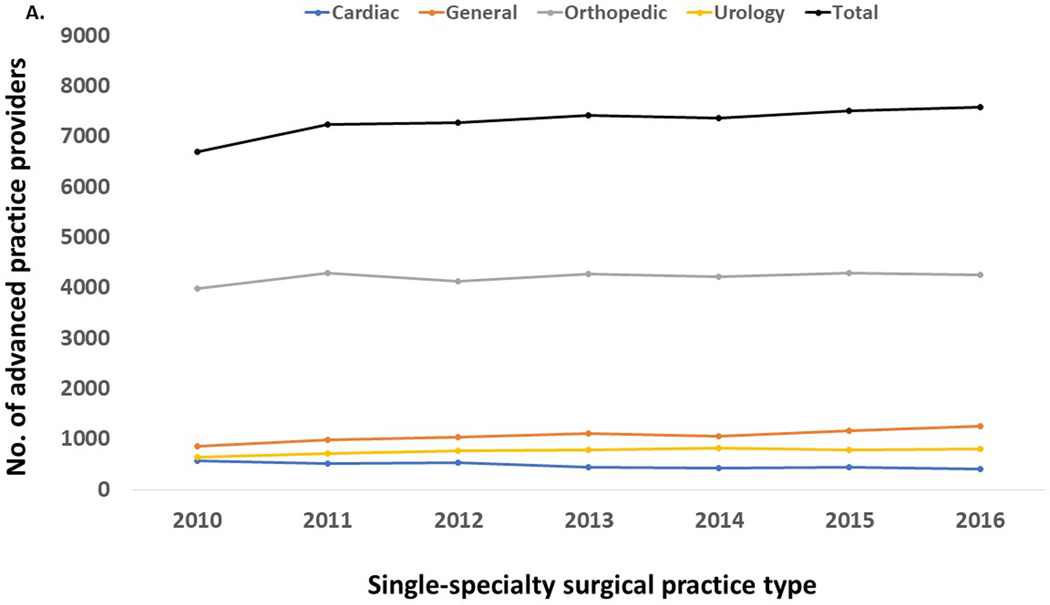
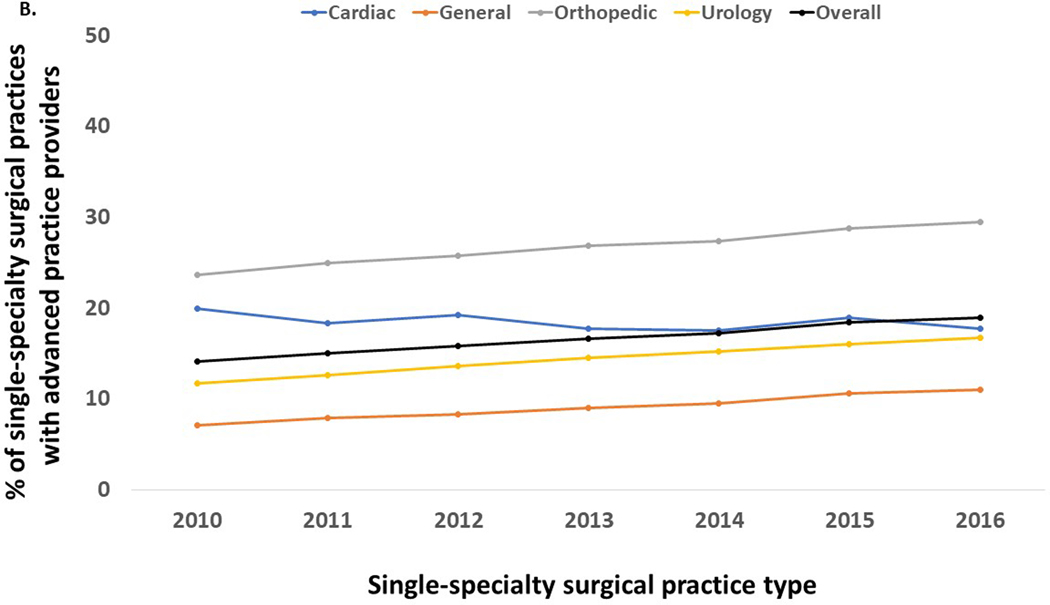
The number of advanced practice providers embedded within single specialty surgical practices increased by 13%, from 6,713 to 7,596 between 2010 and 2016 (Figure 1a). Overall, the percentage of surgical practices with advanced practice providers increased from 14.1% in 2010 to 19.0% in 2016 (Figure 1b). The largest relative increases in the addition of advanced practice providers occurred in general and urology group practices, which grew by 46.9% and 27.6%, respectively. In contrast, the number of advanced practice providers in cardiac group practices decreased over the study period by 25.7%, or from 568 in 2010 to 422 in 2016.
Figure 1.
The number of advanced practice providers (nurse practitioners and physician assistants) in single-specialty surgical practices (a), and the percentage of single specialty surgical practices with at least 1 advanced practice provider (b).
We found 6,282 patients that met our inclusion criteria (407 CABG, 939 colectomy, 4,835 joint replacement, 101 cystectomy).
Table 1 contrasts patient characteristics in the pre and post periods for each of the procedure cohorts. Patients undergoing major joint replacement were slightly younger in the post period group (74.1 vs. 74.5 years, p=0.04), though this difference was small and likely of limited clinical significance. The colectomy and major joint cohorts had a significantly higher percentage of non-white patients in the post-addition year (NB. the racial breakdown for the cystectomy cohort is masked due to cell size and CMS requirements). With the exception of colectomy, patients were similar in terms of comorbidity in the pre and post period cohorts for each of the procedure groups. Among patients undergoing colectomy, those in the post period group had more comorbidity (2.9 vs. 2.5, p<0.01).
Table 1.
Characteristics of patients undergoing major surgery cared for by single-specialty surgical practices that add an advanced practice provider for the first time.
| Characteristic | Procedure | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CABG | Colectomy | Major Joint | Cystectomy | |||||||||
| Pre year N=203 | Post year N=204 | p-value | Pre year N=449 | Post year N=490 | p-value | Pre year N=2309 | Post year N=2526 | p-value | Pre year N=48 | Post year N=53 | p-value | |
| Age, mean (SD) | 74.7 (6.0) | 75.5 (5.7) | 0.18 | 76.7 (7.3) | 76.3 (7.1) | 0.46 | 74.5 (6.1) | 74.1 (6.1) | 0.04 | 75 (6.5) | 75.6 (6.3) | 0.62 |
| Race, n (%) | 0.83 | 0.02 | <0.01 | 0.76 | ||||||||
| White | 190 (93.6) | 192 (94.1) | 426 (94.9) | 445 (90.8) | 2187 (94.7) | 2341 (92.7) | * | * | ||||
| Non-white | 13 (6.4) | 12 (5.9) | 23 (5.1) | 45 (9.2) | 122 (5.3) | 185 (7.3) | * | * | ||||
| Male, n (%) | 133 (65.5) | 144 (70.6) | 0.27 | 203 (45.2) | 201 (41.0) | 0.20 | 819 (35.5) | 985 (39.0) | 0.01 | 38 (79.2) | 40 (75.5) | 0.66 |
| Socioeconomic class, n (%) | 0.71 | 0.11 | 0.32 | 0.94 | ||||||||
| Low | 65 (32.0) | 61 (29.9) | 143 (31.8) | 184 (37.6) | 854 (37.0) | 915 (36.2) | 16 (33.3) | 16 (30.2) | ||||
| Middle | 70 (34.5) | 85 (41.7) | 142 (31.6) | 142 (29.0) | 741 (32.1) | 789 (31.2) | 13 (27.1) | 17 (32.1) | ||||
| High | 68 (33.5) | 58 (28.4) | 164 (36.5) | 164 (33.5) | 714 (30.9) | 822 (32.5) | 19 (39.6) | 20 (37.7) | ||||
| Comorbidity, mean (SD) | 3.0 (1.6) | 2.7 (1.7) | 0.17 | 2.5 (1.7) | 2.9 (2.0) | <0.01 | 2.1 (1.4) | 2.1 (1.5) | 0.44 | 2.8 (1.8) | 3.3 (1.7) | 0.15 |
Cells masked per CMS requirements due to cell size <11 in a cell
As illustrated in Table 2, the adjusted odds of complications were 17% and 16% lower in the year after the addition of an advanced practice provider at 30- and 90-days post-procedure, respectively. Relative to the year prior to the addition, patients had an 18% lower odds of readmission within 90 days of the procedure (adjusted OR 0.82, 95% CI 0.70–0.95). Further, length of stay was significantly shorter for the index hospitalization (−0.33 days, 95% CI −0.49 to −0.17) following the addition of an advanced practice provider. Average 30-day episode spending went from $16,263.61 before the addition of an advanced practice provider to $14,968.88 after (p<0.001)—a net savings of $1,294.73. Average 90-day episode spending was $17,772.12 for the year before and $16,344.35 for the year after an advanced practice provider was added (p<0.001)—a net savings of $1,427.76.
Table 2.
Outcomes in the year after adding an advanced practice provider compared to the year before the addition, adjusted for patient age, race, gender, socioeconomic class and procedure type.
| Outcome | Post-discharge | Odds Ratio (95% CI) | p-value |
|---|---|---|---|
| Complication | 30 days | 0.83 (0.72–0.97) | 0.02 |
| 90 days | 0.84 (0.73–0.97) | 0.02 | |
| Readmission | 30 days | 0.84 (0.69–1.03) | 0.10 |
| 90 days | 0.82 (0.70–0.95) | <0.01 | |
| Mortality | 30 days | 0.97 (0.66–1.43) | 0.88 |
| 90 days | 0.99 (0.72–1.36) | 0.95 |
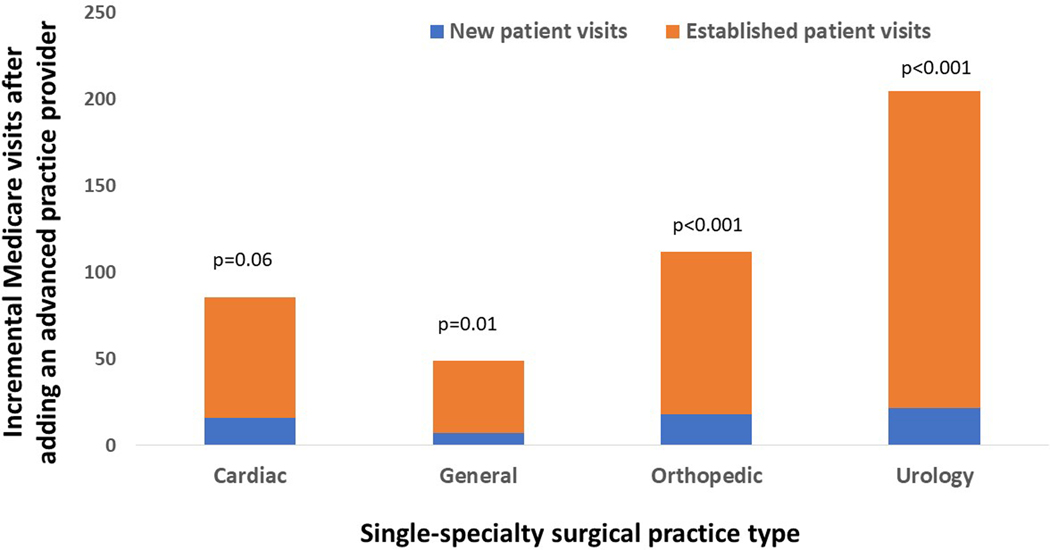
As a measure of access, we also explored new and established patient visits at the surgical group practice level. As illustrated in Figure 2, there were significant gains in the number of Medicare patients seen by general, orthopedic and urology group practices. For general surgical practices, the increase was driven by established patients with an increase of 42.1 visits per surgeon (95% CI 12.5–71.5 visits) in the year after the addition of advanced practice providers. Orthopedic and urologic surgical practices realized significant increases in both established and new patient visits per surgeon, with incremental gains of 112.0 (95% CI 83.0–140.5 visits) and 205.0 (95% CI 117.5–292.0 visits) overall visits per surgeon, respectively.
Figure 2.
At the surgical practice level, the average number of incremental new and established patient visits per surgeon in the year after adding an advanced practice provider (relative to the year before), by surgical practice type.
Discussion
The use of advanced practice providers has increased in general, orthopedic and urologic single-specialty surgical practices but decreased in cardiac practices. The addition of an advanced practice provider to a single-specialty surgical practice is associated with a reduced likelihood of complications and readmissions after the index procedure. Further, compared with patients treated in the year prior to the addition of an advanced practice provider, those treated in the year after had a significantly shorter length of stay and inflation-adjusted episode spending at 30- and 90- days post-procedure. Finally, groups that added an advanced practice provider improved access by allowing for more Medicare patients to be seen among general, orthopedic and urologic single-specialty surgical practices, even after adjusting for the number of surgeons within a group.
Advanced practice providers have long been viewed as a means to improve access by addressing the shortage of physicians, particularly in primary care.10 Currently, it is estimated that a third of primary care is deliver through either a shared (i.e., seen with a physician) or independent visit by an advanced practice provider.2 The implications of this evolution in care delivery are mixed in this context. On the one hand, quality of care appears to be similar for patients managed by advanced practice providers and physicians.3,4 For example, among patients with congestive heart failure, those whose care was managed via an independent or shared model were more likely to receive guideline-recommended medications.7 Further, a large meta-analysis of 24 randomized trials suggest that nurse-led care is associated with improved patient satisfaction, and decreases in both hospital admission and mortality.5 On the other hand, advanced practice providers tend to have a more intensive practice style that manifests as lower thresholds for specialist referral3 and greater use of diagnostic testing.14
Though there is evidence of expanding roles of advanced practice providers among surgical specialty practices,15–17 the impact on health outcomes and spending is virtually unstudied. Similar to primary care, the Association of American Medical Colleges projects a significant shortfall of physicians in the surgical specialties over the next decade.18 In the context of surgical practice, advance practice providers have the potential to play roles in both the inpatient and outpatient settings that can mitigate, at least in part, the impact of this anticipated shortage. Functioning in an inpatient role, advanced practice providers can assist with managing post-surgical patients on the floor, offering enhanced access to patient needs that may allow for earlier identification of complications and mitigate their consequences. In the outpatient setting, advanced practice providers can enhance access to a surgical practice by offloading selected visits from the surgeons. Further, advanced practice providers have the potential to improve continuity of care between the outpatient and inpatient settings, a significant problem in the Medicare population.19 Our findings of reductions in length of stay, complications and readmissions are supportive of both mechanisms of improvement.
However, the precise pathway that APPs improve outcomes in surgical populations will need further investigation through qualitative and/or observation based studies. In our experience, APPs tend to spend more time directly on inpatient floors, coordinating care with caretakers and arranging discharge plans. While this type of careful care transition may help with the prevention of long term readmissions (e.g., 90-day readmissions), prolonged length of stay and some postoperative complications (e.g., DVT), it is unlikely to reduce severe surgical complications that lead to death and short-term readmissions for issues such as bowel leak or postoperative sepsis. Our finding that APPs reduced complications and 90-day readmissions, but not mortality is consistent with this theory.
This study should be interpreted in the context of three limitations. First, this study is limited to single-specialty surgical practice to facilitate line-of-sight on the implications of the addition of an advanced practice provider for a surgical group. is study design decision impacts the total number of patients in our study. While hospitals and multispecialty groups have integrated these providers into their delivery models,6 their functionality is masked within these heterogeneous systems and further obfuscated by reimbursement incentives that favor billing under the physician in a shared care model. Second, our study design does not lend itself to imply causal inference. Specifically, because the year in which our outcome measures were recorded always followed the exposure year by 2 years, our estimates include unmeasured secular trend, which may favor improved quality and access and reduced spending. Therefore, our findings may represent an upper bound on the effects of incorporating advanced practice providers into surgical practice. Third, this study is limited to fee-for-service Medicare beneficiaries. As many surgical practices care for younger patients, we are likely underestimating the impact of adding advanced practice providers on patient access to surgical care.
The addition of advanced practice providers to single-specialty surgical groups is associated with improvements in length of stay, complications, and readmission, and decreased episode spending. Further, adding an advanced practice provider improves access to general, orthopedic and urological surgical groups for Medicare beneficiaries. Future work should clarify the functionalities of advanced practice providers within surgical practice and understand how these diverse functions contribute to outcomes to identify best practices for deployment.
Acknowledgments
Funding: This work was supported by research funding from the NIA (R01 AG-048071) to BKH. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the United States government.
Role of the Funder/Sponsor: No funder had a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: No disclosures were reported.
Bibliography
- 1.Sarzynski E, Barry H. Current evidence and controversies: advanced practice providers in healthcare. American Journal of Managed Care 25(8):366–368, 2019. August. 2019;25(8):366–368. [PubMed] [Google Scholar]
- 2.Xue Y, Goodwin JS, Adhikari D, Raji MA, Kuo YF. Trends in Primary Care Provision to Medicare Beneficiaries by Physicians, Nurse Practitioners, or Physician Assistants: 2008–2014. Journal of Primary Care & Community Health 8(4):256–263, 2017. Oct. 2017;8(4):256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuo YF, Goodwin JS, Chen NW, Lwin KK, Baillargeon J, Raji MA. Diabetes Mellitus Care Provided by Nurse Practitioners vs Primary Care Physicians. Journal of the American Geriatrics Society 63(10):1980–8, 2015. Oct. 2015;63(10):1980–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agarwal A, Zhang W, Kuo Y, Sharma G. Process and Outcome Measures among COPD Patients with a Hospitalization Cared for by an Advance Practice Provider or Primary Care Physician. PLoS ONE [Electronic Resource] 11(2):e0148522, 2016. 2016;11(2):e0148522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martinez-Gonzalez NA, Djalali S, Tandjung R, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Services Research 14:214, 2014. May 12. 2014;14:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moote M, Krsek C, Kleinpell R, Todd B. Physician Assistant and Nurse Practitioner Utilization in Academic Medical Centers.. American Journal of Medical Quality 34(5):465–472, 2019. Sep/Oct. 2019;34(5):465–472. [DOI] [PubMed] [Google Scholar]
- 7.Kuo YF, Adhikari D, Eke CG, Goodwin JS, Raji MA. Processes and Outcomes of Congestive Heart Failure Care by Different Types of Primary Care Models. Journal of Cardiac Failure 24(1):9–18, 2018. January. 2018;24(1):9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.AAMC. The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. 2019. https://aamc-black.global.ssl.fastly.net/production/media/filer_public/31/13/3113ee5c-a038-4c16-89af-294a69826650/2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf. Accessed March 4, 2020. [Google Scholar]
- 9.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. MedCare. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 10.Kuo YF, Loresto FL Jr., Rounds LR, Goodwin JS. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Affairs 32(7):1236–43, 2013. Jul. 2013;32(7):1236–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Medicare Data on Provider Practice and Specialty (MD-PPAS). https://www.resdac.org/cms-data/files/md-ppas. Accessed 10/8/2018.
- 12.AHRQ. Patient Safety Indicators Overview. https://www.qualityindicators.ahrq.gov/modules/psi_overview.aspx. Published 2020. Accessed April 1, 2020.
- 13.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease.[see comment]. New England Journal of Medicine 345(2):99–106. 2001. [DOI] [PubMed] [Google Scholar]
- 14.Hughes DR, Jiang M, Duszak R Jr., Hughes DR, Jiang M, Duszak R Jr. A comparison of diagnostic imaging ordering patterns between advanced practice clinicians and primary care physicians following office-based evaluation and management visits. JAMA Internal Medicine. 2015;175(1):101–107. [DOI] [PubMed] [Google Scholar]
- 15.Duszak R Jr., Walls DG, Wang JM, et al. Expanding roles of nurse practitioners and physician assistants as providers of nonvascular invasive radiology procedures. Journal of the American College of Radiology. 2015;12(3):284–289. [DOI] [PubMed] [Google Scholar]
- 16.Chan KH, Dinwiddie JK, Ahuja GS, et al. Advanced practice providers and children’s hospital-based pediatric otolarynology practices. Int J Pediatr Otorhinolaryngol. 2020;129(109770). [DOI] [PubMed] [Google Scholar]
- 17.Martsolf GR, Barnes H, Richards MR, et al. Employment of Advanced Practice Clinicians in Physician Practices. JAMA Internal Medicine. 2018;178(7):988–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.AAMC. The complexties of physician supply and demand: Projections from 2017 to 2032. 2019. https://www.aamc.org/system/files/c/2/31-2019_update_-_the_complexities_of_physician_supply_and_demand_-_projections_from_2017-2032.pdf. [Google Scholar]
- 19.Sharma G, Fletcher KE, Zhang D, et al. Continuity of outpatient and inpatient care by primary care physicians for hospitalized older adults. Jama. 2009;301(16):1671–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]