Abstract
Introduction: Telemedicine across many specialties in clinical practice has been established in the literature regarding technology platforms, privacy issues, cost, and clinical effectiveness. However, the lack of data in these areas applicable to spinal cord injury telerehabilitation (teleSCI) still exists. The gaps in these knowledge areas continue to hinder its widespread implementation and serve as pathways for focused efforts in teleSCI research.
Objective: This systematic review aims to substantiate the clinical effectiveness and potential barriers to teleSCI implementation by verifying the statistical significance of various clinical outcomes from randomized trials published within the recent past decade.
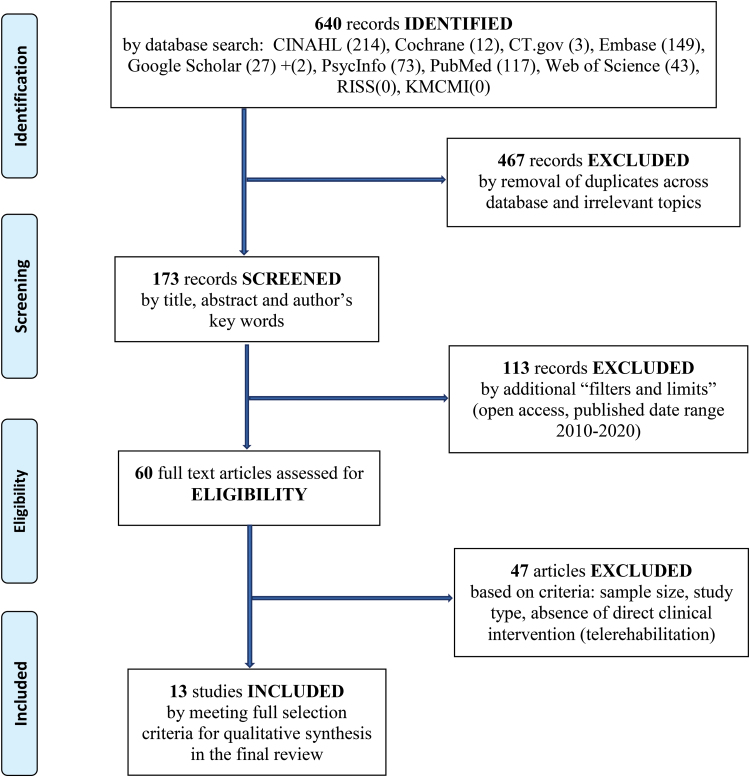
Methods: A qualitative synthesis of randomized studies, conducted across various regions, was systematically reviewed after identifying relevant records from database search engines. Applied filters in the search included publication dates (2010–2020), humans, full-text, and no language preference. The 13 studies were selected per Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram, and the risk of bias across studies was evaluated by using the Physiotherapy Evidence Database scale of quality assessment.
Results: Quantitative outcome measurements demonstrated positive impact across studies: 79.1% (34/43) of all measurements were statistically significant for positive outcomes and 18.6% (8/43) yielded no effect but were significant. Primary outcomes addressed various spinal cord injury (SCI) management areas; 38.5% (5/13) of studies also assessed secondary outcomes. Interventional platforms were conventional technologies used in telemedicine. One study (7.7%) achieved data encryption; no studies presented cost-analysis data.
Conclusion: The majority of studies demonstrated significant positive outcomes to validate teleSCI clinical effectiveness through conventional technology. These results further expand our understanding of teleSCI's impact and its demonstrated potential for improving SCI individuals' lives. However, heterogeneity of selected studies limits the conclusive recommendations to address potential barriers to its widespread implementation. Moreover, the development of new data is warranted to promote “buy-in” of widespread teleSCI implementation.
Keywords: SCI, spinal cord injury, technology, telemedicine, telerehabilitation
Introduction
Spinal cord injury or dysfunction (SCI/D) can result from either traumatic or nontraumatic occurrences and renders life-altering events. Its clinical manifestations involve changes in underlying strength, sensation, and other bodily function that causes paralysis and disability.1 Other consequences manifest in varying degrees with profoundly compromised function in necessary life activities.2 Furthermore, secondary medical complications associated with multiorgan systems including neurogenic bowel, lower urinary tract disorder, pressure ulcers, endocrine and metabolic abnormalities, and cardiopulmonary and hemodynamic instability along with sexual dysfunction commonly occur after discharge from acute inpatient rehabilitation.3 These comorbidities can lead to unfortunate losses physically, emotionally, socially, and economically.4
Secondary complications require costly and time-consuming medical management by qualified specialty care providers in a clinical setting. The morbidities yield severely compromised levels of activity and participation, ultimately impacting the quality of life (QoL) for many, with death resulting in severe cases.5 The situation can be devastating not only for patients but also for caregivers and clinical providers involved in their care. Therefore, it is essential to prevent and systematically manage these complications. However, continuous and appropriate health services for SCI/D individuals are denied under many circumstances. Many of these individuals cannot access specialty clinics due to barriers in economic burdens, transportation, and remote locations.6
In the efforts to combat such barriers, the advent of telemedicine has propelled ways for the delivery of medical care from remote locations through information telecommunication technology (ICT).7 The evolving field of telemedicine, in past decades, has revealed innovative options in telerehabilitation to address underlying challenges in remotely managing patients requiring rehabilitation. In 2016, the concept of spinal cord injury telerehabilitation (teleSCI) was officially introduced at the International Spinal Cord Society Annual Scientific Meeting in Vienna, Austria, by an international panel of leaders through an instructional telemedicine course.8 Furthermore, evidence in the literature shows the efficacious role of telemedicine within other clinical specialties—internal medicine and mental health—with high levels of satisfaction among patients who reside in remote locations.9
Telerehabilitation in spinal cord injury (SCI) management has been applied and reported to have had successful outcomes in some global areas.10 It is especially beneficial for those who are disadvantaged by barriers to accessing specialty care clinics. From the perspective of “taking ownership,” Kryger et al. validate that appropriate use of technology enhances empowerment to participants promoting a sense of responsibility in being more involved and better educated about their care and overall well-being.11 However, mobile and telehealth interventions appear to be used less commonly in teleSCI management.12,13
Furthermore, there has been insufficient evidence generated, even in the recent past decade, which validates its clinical efficacy in SCI individuals. The lack of data is particularly evident throughout many Asian countries, presumably influenced by economic, political, and cultural factors.10 In the Republic of Korea (S. Korea), debates regarding the feasibility of teleSCI among health care experts are ongoing, whereas uncertainties in cost-effectiveness leave doubts in physicians' minds regarding widespread implementation across medical specialties.14
Health care experts still consider teleSCI to be in its developing stages, which require fine tuning in many aspects.15 The associated privacy concerns present as deterrence for policymakers. The data regarding cost–benefits are insufficient to convince health economic experts, whereas sparse evidence regarding clinical efficacy and reimbursement inevitably fails to reach a consensus among physicians.16–18 These are some of the demanding challenges remaining to be addressed and require solutions to overcome the lingering concerns toward telemedicine implementation. Gaps in these knowledge areas continue to maintain uncertainties in teleSCI clinical practice and research. This systematic review aims to substantiate the clinical effectiveness of teleSCI and confirm existing potential barriers in its widespread global implementation by verifying the statistical significance of clinical outcomes from randomized trials published within the recent past decade.
Methods
Database search
The first author performed the initial search using key search terms and appropriate Boolean phrases: telerehabilitation OR telemedicine AND “spinal cord injury” OR “SCI.” Search engines included CINAHL (n = 214), PubMed (n = 117), and Clinicaltrials.gov (n = 3). A research assistant independently performed a search (March 15, 2020) on two Korean databases: Research Information Sharing Service and Korea Medical Citation Medical Index. However, these did not yield any relevant articles based on our search criteria. Our salient efforts involved a comprehensive search of the gray literature using Web of Science (n = 43), EMBASE (n = 149), Cochrane Library (n = 12), PsyINFO (n = 73), and Google Scholar (n = 29). We assessed a total of 640 records identified from 10 search engines aforementioned to narrow the selection field. The following filters were applied: (1) publication date range from January 1, 2010 to January 1, 2020, (2) human subjects, (3) open access with full-text articles, and (4) no language preference specified. The flow diagram in Figure 1 shows the summary of database research.
FIG. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart: selection of studies by database literature search.
Screening and eligibility criteria
The identified records were assessed by research assistants, giving attention to the title, abstract contents, and key phrases per our selection criteria. This review focused uniquely on randomized trials, including feasibility and pilot studies with respect to the study design. Our criteria for inclusion and exclusion are outlined in detail.
Inclusion
a. Randomized controlled or clinical trials (RCTs) including pilot and feasibility studies.
b. Study participants with underlying SCI/D (spinal cord injury or dysfunction).
c. Study participants are adult males or females of 18 years or greater.
d. Sample size greater than eight participants per study.
e. Health care and related services delivered through teleSCI platform with outcomes assessment in SCI/D management.
f. Intervention delivered using technology from home or community setting with interactions between participants and clinical providers (physicians, nurses, allied health professionals, and licensed or qualified rehabilitation counselors).
Exclusion
We excluded case studies, case series presentations, observational studies, articles with fewer than eight study participants, and all review types of studies. Study protocols merely proposing a study design without resultant data or interventional outcomes were all excluded. Since telerehabilitation is still considered evolving and require fine tuning,19 particularly in technology advancements, our review focused on current research spanning the past decade. Studies published outside of the specified date range—between 2010 and 2020—were also excluded. After eliminating duplicates and other irrelevant articles, 13 studies met our criteria and were included in this review.
Data collection process
The first author performed data extraction from 13 selected articles. At the time of data acquisition, one of the designated coauthors withdrew and was pre-empted from further collaboration. Subsequently, any discrepancies were resolved by consensus among the three coauthors.
Extracted data information
The computing system in the research laboratory served as the central management system for acquired data storage. Record keeping of all information was maintained separately on an excel spreadsheet. Addendum notes were also generated for organizing or information and recorded using a word document. The items of extracted data were categorized as follows: characteristics of (1) selected studies, (2) study population, (3) study methods, and (4) study results with outcome data. The summary of these data categories is given in Table 1.
Table 1.
Summary of Data Extracted
| Data categories | |
|---|---|
| Selected studies | Author, title, institution, country of origin, objectives, digital object identifier, first date of article submission and final publication dates |
| Study population | Sample size, age, gender, SCI level or type (ASIA scale classification), comorbidities |
| Study methods | Design, setting, geographic location, data collection method and tools, process of recruitment, randomization and allocation concealment, follow-up period, interventional platform, secondary technology, and data security |
| Results and data outcome | Primary and secondary outcomes, observed outcome measurements, intervention results and statistics analysis, adverse events, and attrition rate |
ASIA, American Spinal Injury Association; SCI, spinal cord injury.
Information for assessment of the risk of bias
The quality of the selected studies was evaluated by assessing the risk of bias, using the quality checklist assessment formulated by Physiotherapy Evidence Database (PEDro) scale in reporting data.20 In systematic reviews, evaluating the quality of RCTs is common practice. However, the reliability of data obtained with most quality assessment scales has not been established.21 Maher et al.21 described in their report of two studies designed to investigate the reliability of data obtained with the PEDro scale developed to rate RCTs' quality evaluating physical therapist interventions. The scale is a valid measure of the methodological quality of clinical trials.
Results
Selection and characteristics of studies
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram shown in Figure 1 summarizes the systematic approach to our record search. Identified records were assessed based on our selection criteria. Through a stepwise process of screening and exclusion, 13 total studies met our criteria. The characteristics of the selected studies included in the final review are summarized in Table 2.
Table 2.
Summary of the Characteristics of Selected Studies
| Author | Title | Title | Journal | Design | Sample | Population | Intervention technology | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Hossain et al.6 | A pilot randomized trial of community-based care following discharge from hospital with a recent spinal cord injury in Bangladesh | May, 2016 | Clinical Rehabilitation | Randomized trial (pilot) | N = 30 | SCI | “Care Pack” = Telephone contacts and home-visits | 24 months |
| Houlihan et al.32 | A pilot study of a telehealth intervention for persons with spinal cord dysfunction | June, 2013 | Spinal Cord | RCT | N = 142 | SCI, MS | “Care Call” = automated interactive voice response system | 6 months |
| Migliorini et al.22 | A randomized control trial of an internet-based cognitive behavior treatment for mood disorder in adults with chronic spinal cord injury | December, 2015 | Spinal Cord | RCT (prospective parallel waitlist) | N = 48 | SCI | Telephone-interview: ePACT | 15 months |
| Arora et al.23 | Cost-effectiveness analysis of telephone-based support for the management of pressure ulcers in people with spinal cord injury in India and Bangladesh | August, 2017 | Spinal Cord | RCT | N = 115 | SCI | Telephone-based support | 12 weeks |
| Kowalczewski et al.24 | In-home telerehabilitation improves tetraplegic hand function | March, 2011 | Neurorehabilitation and Neural Repair | RCT (cross-over) | N = 13 | SCI | Tele-supervised exercise therapy | 9 months |
| Hearn and Finlay25 | Internet-delivered mindfulness for people with depression and chronic pain following spinal cord injury: a randomized, controlled feasibility trial | March, 2018 | Spinal Cord | Randomized trial (feasibility) | N = 67 | SCI | Web-based online mindfulness training | 8 weeks |
| Houlihan et al.26 | Randomized trial of a peer-led, telephone-based empowerment intervention for persons with chronic spinal cord injury improves health self-management | March, 2017 | Archives of PM&R | RCT | N = 84 | SCI | Telephone-based, text and e-mail support by peer-health coaches | 6 months |
| Kryger et al.11 | The effect of the interactive mobile health and rehabilitation system on health and psychosocial outcomes in spinal cord injury: a RCT | August, 2019 | Journal of Medical Internet Research | RCT | N = 38 | SCI | Smart-device interactive mobile application modules and web-based portal monitoring | 9 months |
| Coulter et al.27 | The effectiveness and satisfaction of web-based physiotherapy in people with spinal cord injury: a pilot RCT | 2017 | Spinal Cord | RCT (pilot) | N = 24 | SCI | Web-based PT exercise program with telephone interview | 8 weeks |
| Worobey et al.28 | Investigating the efficacy of web-based transfer training on independent wheelchair transfers through RCTs | 2018 | Archives of PM&R | RCT | N = 71 | SCI, MS, amputees, others | Web-based training of wheelchair transfers | 1–2 days postintervention |
| Rimmer et al.29 | Telehealth weight management intervention for adults with physical disabilities a RCT | December, 2013 | American Journal of PM&R | RCT | N = 102 | SCI, MS, CP, spina bifida, CVA, SLE | Web-based remote coaching and telephone support | 9 months |
| Dorstyn et al.30 | Work and SCI: a pilot randomized controlled study of an online resource for job-seekers with spinal cord dysfunction | September, 2018 | Spinal Cord | RCT (pilot) | N = 48 | SCI/D | Web-based online informational intervention | 4 weeks |
| Shen et al.31 | Clinical treatment of orthostatic hypotension after spinal cord injury with standing training coupled with a remote monitoring system | December, 2014 | Medical Science Monitor | RCT | N = 36 | SCI/D | Remote monitoring of electric bed uprise training with wearable remote wireless multi-parameter dynamic monitoring system | 30 days |
CP, cerebral palsy; CVA, cerebrovascular accident; ePACT, electronic personal admin of cognitive therapy; MS, multiple sclerosis; PT, physical therapy; RCT, randomized controlled or clinical trial; SCI/D, spinal cord injury or dysfunction; SLE, systemic lupus erythematosus.
Risk of bias across studies
The risk of bias was assessed across studies using the PEDro scale. Nine studies scored 9 or greater out of 11, whereas three studies scored 7 out of 11, and one study scored 6 out of 11. Potential bias across studies appears to be associated with blinding and allocation concealment. Quality assessment based on the PEDro scale revealed that 38.5% (5/13) of selected studies achieved allocation concealment. Blinding of participants, clinicians administering interventions, and assessors measuring outcome were reported as 46.2% (6/13), 15.4% (2/13), and 46.2% (6/13) across studies, respectively. Table 3 gives a summary of the assessment.
Table 3.
Summary of the Characteristics of Selected Studies, Primary Outcomes and Measurements
| Author | Intervention setting | Geographic location | Data encryption | PEDro scale risk of bias | Attrition rate | Primary outcomes | Outcomes measurement |
|---|---|---|---|---|---|---|---|
| Hossain et al.6 | Home, community | Bangladesh | None reported | 8/11 | 6.7% | All cause mortality | Two participants died; mortality rate of 7% (95% CI: 2 to 21) |
| Houlihan et al.32 | Community | United States | None reported | 8/11 | 6.3% | Reduced presence of pressure ulcers at 6 months in women (p < 0.0001); reduced 6-month severity of depression (age and gender adjusted; p < 0.047) | No significant impact on health-care utilization (OR = 1.8, p = 0.07) |
| Migliorini et al.22 | Home | Australia | None reported | 8/11 | 22.9% | Mood improvement with life satisfaction | Within-group analyses showed significant mood improvement (ES = 0.4), anxiety (ES = 0.4), stress (ES = 0.3) and higher life-satisfaction (ES = 0.2) |
| Arora et al.23 | Tertiary care center | Bangladesh, India | None reported | 9/11 | Not reported | Cost–benefit and health outcomes (ulcer size reduction and QALY gained | Between-group difference for mean reduced pressure ulcer size (95% CI: −3.12 to −4.32), corresponding QALYs = 0.027 (95% CI: 0.004 to 0.051), 87% cost-effectiveness by sensitivity analyses |
| Kowalczewski et al.24 | Home | Australia, Canada | None reported | 10/11 | All participants completed study | ARAT | Arm and hand strengths' score (p < 0.01) improved after ET |
| Hearn and Finlay25 | Home, community | United Kingdom | Data encrypted | 8/11 | 35.8% | Depression symptom severity | Depression significantly reduced more by mindfulness than psychoeducation (mean_diff = −1.50; 95% CI: −2.43 to −0.58) |
| Houlihan et al.26 | Home, community | Canada, United States | None reported | 8/11 | 9.9% | Health self-management | Peer-led health self-management yielded significant change in PAM scores (p = 0.047) |
| Kryger et al.11 | Home | United States | None reported | 9/11 | 13.2% | Health outcomes = UTI, pressure sores, emergency room visits, hospital admissions | Intervention significantly reduced UTIs (p = 0.03) with nonsignificant psychosocial outcomes trending toward reduced mood symptoms |
| Coulter et al.27 | Home, community | United Kingdom | None reported | 7/11 | 12.5% | 6 MPT or 6 MWT depending on mobility | Between-group differences were not significant but more pronounced for 6-MWT |
| Worobey et al.28 | Home | United States | None reported | 8/11 | 7% | Transfer techniques @ baseline, skills-acquisition immediate post-training, and skills-retention post 1–2 days follow-up | Web-based transfer training showed improvement (p = 0.05) |
| Rimmer et al.29 | Home | United States | None reported | 7/11 | 10.8% | Biomed = weight, body mass index; barriers to activity; activity = aerobic exercise; strength exercise; total-exercise; nutrition = fat score; fiber score; fruit/veggie score | Bodyweight difference between groups was significant in group and time interaction on statistic analysis (p < 0.01) |
| Dorstyn et al.30 | Home, community | Australia | None reported | 7/11 | 36% | 25-item JSES | High uptake of work and SCI resources through learning module; high attrition rate observed with intention-to-treat analyses failing to reach statistical significance |
| Shen et al.31 | Home | China | None reported | 6/11 | 11.1% | Responses to electric uprise bed training and compare training efficiency | Tilt-table training improved in systolic and diastolic orthostatic blood pressure changes |
ARAT, Action Research Arm Test; CI, confidence interval; ES, effect size; ET, exercise therapy; JSES, Job Procurement Self-Efficacy Scale; MPT, Min Push Test; MWT, Min Walk Test; OR, odds ratio; PAM, Patient Activation Measure; PEDro, Physiotherapy Evidence Database; QALY, quality-adjusted life years; UTI, urinary tract infection.
Synthesis of results
Selected studies
The following is a summary of the characteristics of the selected studies included in this review.6,11,22–31 The affiliated institution, country of origin, study title, study objectives, journals in which they were published, along with digital object identifier numbers and date of articles' first submission were extracted. After agreement by coauthors, studies were included, following independent search and screening efforts without the assistance of a librarian. Our criteria for publication date ranged between 2010 and 2020 since a decade was believed to be an extended period for advancements in IT device technology for their potential application in telemedicine. The earliest publication among selected studies was from 2011, whereas the most recent was from 2019.
Study population
The total number of participants across studies was 818 and ranged from 13 to 142, with a mean of 62.9 participants.32,24 The mean of male participants across all studies was 62.96% (n = 515/818). Three of the studies included >50% female participants in both experimental and control groups,24 and two studies had >71% in female participants.27,28 Age was reported in years by mean with standard deviation, among seven studies according to intervention (range 29–51.5) and control (range 38–52.8) groups.6,11,22,23,27,28,31
Ten studies focused strictly on SCI, whereas one study included multiple sclerosis (MS).23 One study included MS and amputees,28 whereas another study included MS, cerebral palsy (CP), stroke, spina bifida, and lupus.29 Two studies reported on the American Spinal Injury Association (ASIA) scale classification with SCI type by specific neurological levels of injury.21,25 Majority did not use ASIA scale classification, whereas some labeled participants as “tetraplegia” versus “paraplegia” without detailed neurological levels.11,22,24,27,28,30,31 Six studies reported completeness or incompleteness of injury.11,22,24,27,30,31 One study that included MS participants reported only neurological levels of injury for its SCI participants.32 Two studies, which included disabilities of varying disorders (MS, CP, stroke, amputees, and lupus), did not specify neurological levels of injury nor ASIA classification.28,29 One study did not report types or levels of injury.23
Comorbidities of participants reported by seven studies included pressure ulcers,11,23,32 depression,11,22,32 pain,25 diabetes,26 and cardiovascular abnormalities.26,31 The remaining six studies did not report comorbidities of participants.6,24,27–30
Study methods
The settings for conducting the intervention were in the participants' home for all studies (some studies indicated “community” as a designated remote location and that was considered as “home”). In contrast, one study was conducted in a laboratory-simulated home setting.23 Geographically, studies were conducted in various countries including the United States,26,27–29,32 Canada,24,26 Australia,22,24,30 United Kingdom,25,27 Bangladesh,21 India,23 and China.31
Various methods of data collection were reported, including telephone interviews and/or in combination with written questionnaires.6,21–23,25,26,27–30,32 One study added home visits with telephone interviews.6 Other studies used clinical assessment,23,24,31 survey forms,29 and web-portal with software applications.11 Most studies used one or more standardized tools for data collection. Among these, various tools were used to assess the QoL6,11,23,25,30: WHO-QOL-BREF, HR-QoL, PWI, SCL-EWL, PHQ-9, QALY, and PUSH. Pain, depression, and anxiety symptoms were assessed by respective authors in the studies using NRS, PCS, CES Depression Scale, DASS-21, BDI-II, and HADS. Levels of disability, activity, and independence were measured by CHART-SF, PADS, SCI-SC scale, SCIM-III, COPM, WHODAS, and CHART-SF. Mindfulness of self-management in health was also measured using FFMQ, PAM, PACIC, ASIS, and CHIEF-SF. Other tools used in studies included ARAT and RAHFT to measure hand function and strength, whereas TAI scores evaluated the performance of wheelchair transfer techniques.24 Self-reported measures for seeking employment were measured using JSES and LOT-R.29 Refer to Appendix A1 for abbreviations.
All studies in this review are RCTs. Four of these are pilot or feasibility studies.6,25,27,30 Six studies reported in detail on the process of recruitment, randomization, and ascertaining of allocation concealment.6,22,26,27,28,30 Five reported on only the recruitment process.23–25,27,29 Two studies neglected to provide any information regarding these processes in their study design.25,32 The quality assessment across studies (Table 4) revealed that six studies achieved blinding of all study participants.6,22–26 Two studies secured blinding among those who administered intervention.11,24 Blinding of those who assessed at least one key outcome was attained in 6 of the 13 studies.6,11,23–25,29
Table 4.
Physiotherapy Evidence Database Scale for Assessing Quality: Risk of Bias in Studies
| Hossain et al.6 | Houlihan et al.32 | Migliorini et al.22 | Arora et al.23 | Kowalczewski et al.24 | Hearn and Finlay25 | Houlihan et al.26 | |
|---|---|---|---|---|---|---|---|
| 1. Eligibility criteria were specified | p.782, Methods | Table 1 | p.695, Methods | p.1072, Participants | p.413, Participants | p.751, Participants | p.1068, Participants |
| 2. Subjects were randomly allocated to groups | p.782, Methods | p.716, Participants | p.696, Methods | p.1072, Intervention | p.413, Participants | p.752, Procedure | p.1068, Trial design |
| 3. Allocation was concealed | p.782, Methods | N | p.695, Methods | p.3, Figure 1{Arora&Harve} | N | N | N |
| 4. Groups were similar at baseline regarding the most important prognostic indicators | Table 1 | Table 3 | Table 1 | Table 1 | Table 1 | Table 2 | Table 2 |
| 5. There was blinding of all subjects | p.782, Methods | Abstract | p.696, Methods | N | p.413, Design | p.752, Procedure | p.1068, Trial design |
| 6. There was blinding of all therapists who administered the therapy | N | N | N | N | p.415, Primary outcome | N | N |
| 7. There was blinding of all assessors who measured at least one key outcome | p.783, Methods | N | N | p.3, Assignment | p.415, Primary outcome | p.752, Procedure | N |
| 8. Measures of at least one key outcome were obtained from >85% of the subjects initially allocated to groups | Table 2 | Table 4, Figures 2a, 2b | N | Tables 3, 4 | p.413, Table 2 and Participants | N {p.755, Compliance} | p.1071, Results |
| 9. All subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome were analyzed by “intention to treat” | Table 2, Figure 1 | p.717, Stats analysis | p.697, Analyses | Tables 3, 4 | Table 2 | p.754, Results | p.1071, Engagement |
| 10. Results of between-group statistical comparisons are reported for at least one key outcome | N | p.717, Results | Table 2 | Table 5 | p.417, Comparison | Table 3 | Table 4 |
| 11. The study provides both point measures and measures of variability for at least one key outcome | N | Figures 2a, 2b | Tables 3, 4 | Table 5 | p.417, Effect size | p.756, Effects | Table 4 |
| Total | 8/11 | 8/11 | 8/11 | 9/11 | 10/11 | 8/11 | 8/11 |
| Information in each cell indicates the corresponding “page number” or “section” (Abstract, Methods, Results, Participants, Design, Statistics analysis, Outcomes, Comparison, Effect size, Tables, Figures, etc.) under which each of the 11 areas of quality assessment was reported by respective authors in the original article. | |||||||
| N, none reported. | |||||||
| Kryger et al.11 | Coulter et al.27 | Worobey et al.28 | Rimmer et al.29 | Dorstyn et al.30 | Shen et al.31 | ||
|---|---|---|---|---|---|---|---|
| 1. Eligibility criteria were specified |
p.3, Recruitment |
p.384, Methods |
p.10, Participants |
p.1085, Participants |
p.222, Eligibility |
p.2768, Subjects |
|
| 2. Subjects were randomly allocated to groups |
p.3, Design |
p.384, Methods |
p.10, Participants |
p.1086, Recruitment |
p.223, Procedure |
p.2768, Subjects |
|
| 3. Allocation was concealed |
N |
N |
p.10, Participants |
N |
p.223, Procedure |
N |
|
| 4. Groups were similar at baseline regarding the most important prognostic indicators |
Table 1
|
Table 1
|
Table 1
|
Table 2
|
Table 1
|
Table 1
|
|
| 5. There was blinding of all subjects |
N |
N |
N |
N |
N |
N |
|
| 6. There was blinding of all therapists who administered the therapy |
p.3, Design |
N |
N |
N |
N |
N |
|
| 7. There was blinding of all assessors who measured at least one key outcome |
p.3, Design |
N |
N |
p.1087, Measures |
N |
N |
|
| 8. Measures of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups |
p.6, Results, Figure 2
|
p.384, Results |
p.13, TAI, Table 1
|
N |
N |
N |
|
| 9. All subjects for whom outcome measures were available received the treatment or control condition as allocated or, where this was not the case, data for at least one key outcome were analyzed by “intention to treat” |
Table 3
|
Table 2
|
Table 1
|
p.1088, Stats analysis |
p.225, Preliminary effects |
Table 5
|
|
| 10. Results of between-group statistical comparisons are reported for at least one key outcome |
Figures 3, 4
|
Table 2
|
p.13, Regression, Tables 2, 3
|
Table 3
|
Table 2
|
Table 3
|
|
| 11. The study provides both point measures and measures of variability for at least one key outcome |
p.10, Findings |
Table 2
|
Tables 2, 3 |
Table 4
|
p.225, Prelim effects |
Table 5
|
|
| Total | 9/11 | 7/11 | 8/11 | 7/11 | 7/11 | 6/11 |
Information in each cell indicates the page number or section (Abstract, Methods, Results, Participants, Design, Statistics analysis, Outcomes, Comparison, Effect size, Tables, Figures, etc.) under which each of the 11 areas of quality assessment was reported by the study authors.
TAI, transfer assessment instrument.
Telephones and computers were the more commonly used technology for delivery of the intervention, and all required internet connection.6,22,23,26,27,29 Computer-based platform was used for automated interactive voice response system,32 videoconferencing,24 and web-based internet communications.11,27 One study required smartphones while another used a wearable remote wireless monitoring device.31 Three studies also required secondary technology equipment, including computers for online data tracking system,22,24,26 and one study provided participants with laptops, computers, and web-cams.24
In this review, one study addressed privacy concerns in protecting participants' personal information acquired through an online survey.25 All other studies did not report achieving data encryption or securing of personal information in adherence to Heath Insurance Portability and Accountability Act (HIPAA) guidelines.
Study results and outcomes data
Primary outcomes observed were as follows: all-cause mortality,6 pressure ulcer and depression,32 mood improvement with life satisfaction,32 costs and health outcomes with quality-adjusted life years gained,23 upper limb strength and function,24 depression symptoms severity,25 self-management in health techniques,26 health and psychosocial outcomes,11 6-min walk or push test,27 changes in score for wheelchair transfer techniques,28 biomedical (weight, body mass index, barrier to activity), physical activities, nutritional status (scores in fat, fiber, and fruit/veggie),29 securing employment, and depression symptoms severity.30
Secondary outcomes were assessed in five studies: medical complications, depression, participation, QoL; hand (grasp and pinch forces) function; anxiety, pain perception, catastrophizing, and mindfulness; global ratings of services or resource use; and quality of primary care.6,25,26,28,30
Outcome measurements were primarily quantitative and demonstrated a positive impact. Among 43 total measurements tested across studies for statistical significance, 34 (79.1%) were significant for positive outcomes, whereas 8 (18.6%) yielded no effect but were significant. There was one negative impact by statistical testing,23 and one study reported no significant testing for outcome measures.6 Table 3 summarizes the primary outcomes and measurements.
Attrition rates across all studies ranged from 6.7% (2 out of 30)6 to 36% (9 out of 40 unaccounted for in final analysis).30 Only one study had all of their participants complete the study,25 and one study did not report any information on attrition.23 Three participants withdrew due to disinterest,11 and seven withdrew for unspecified reasons.30 Adverse events across studies were as follows: three deaths,6,11 seven hospitalizations for pressure ulcers,6,29 one participant started dialysis,29 and two participants had acute illnesses.30
Discussion
Telemedicine concepts and application in clinical practice have demonstrated their feasibility over the past decade. However, teleSCI is yet to become widely implemented worldwide. The focused areas of investigation among the reviewed studies included community-based care after discharge from inpatient rehabilitation, wound care management, orthostatic hypotension, mental health, chronic pain, hand function, home physiotherapy, wheelchair transfer training, bodyweight management, promoting self-management in health, psychosocial support, and securing of employment for community-dwelling individuals with SCI.6,11,22–32
In our search, 13 teleSCI studies met inclusion criteria, which were finally included in this review. This is a significant contrast from a review of telemedicine studies in managing other conditions—asthma, chronic obstructive pulmonary disease, diabetes, heart failure, and hypertension—as demonstrated by Wootton that identified >1300 publications.33 And thus, the observation validates the reality of sparse data in the literature on teleSCI investigations.
Our review of selected studies was representative of the SCI population across characteristics such as gender, age, and type of injury. A review of global prevalence and incidence of traumatic SCI shows a high male-to-female ratio34 and is consistent with the majority of the studies reviewed. The average age of injury, at 42 years,35 is consistent with the central tendency of participant ages represented within the studies. The predominant injury type reported was incomplete SCI, consistent with epidemiological trends (66.3% of all SCI).35 All studies were published in English, with many having conducted in North America. However, given the absence of an accurate global prevalence estimate, establishing geographic representation is problematic34,36,37 and is indicative of the need for standardization of guidelines for global SCI reporting.36,37
The lack of standardized neurological levels of injury reporting was evident across studies. This deficit can potentially lead to challenges in clinical practice and in understanding current works and future needs in SCI research.36,37 However, in this review, only two studies appropriately reported neurological levels of injury using the standardized ASIA impairment scale classification.6,11 The majority of studies used generalized terms such a “tetraplegics” or “paraplegics.” Others merely reported types of injury, such as “complete” or “incomplete.” Reviewers must be aware of these inconsistencies as critical barriers to accuracy in the reporting of results. The consistency with standardized reporting is compulsory since it minimizes doubts and errors while enhancing clear communication between research scientists and clinicians within the academic community. By a committee of international experts, these limitations have been recognized and prompted to promote global standards of reporting in future SCI studies.38 One area of standardization suggested by the committee is shared data and minimum information standards38,39 to ensure highly improved results from systematic review studies.
This review's selected studies are all randomized trials, of which four are pilot or feasibility studies.6,11,25,30 Six studies reported details, following Consolidated Standards of Reporting Trials (CONSORT) guidelines, in recruitment, randomization, and ascertaining of allocation concealment.6,22,26,27,28,30 Two studies neglected to report any information on these processes.23,32 Among the reviewed studies, <50% (6 of 13) achieved blinding of participants,6,22–26 whereas some studies secured blinding of research staff involved in either the delivery of interventions (2 of 13)11,24 or assessing outcomes data (6 of 13).6,11,23–25,29 Thus, potential biases across studies appear to be associated with blinding and allocation concealment. Our quality assessment based on PEDro scale20 revealed that <40% of all studies achieved allocation concealment, and a mere 46% of studies incorporated blinding in their study designs (Table 4). Based on this rating scale assessment, it is plausible that 81.8% (9 of 13) of the reviewed studies are likely to be reliable.
We observed primarily positive outcome measures (79.1%) across studies. Similarly, most secondary outcome measures (38.5%) were positive and focused on psychosocial issues in the management of mood and depression.25,26,32 One area, which lacked the attention that it deserves among these individuals, is erectile dysfunction. The highly prevalent condition among SCI males resulting in sexual dysfunction and infertility issues severely impacts life quality.40 Among the reviewed studies, this area represents a knowledge gap, which indicates the need for further research in SCI sexual rehabilitation.41 In contrast, it is arguable that SCI men who are confronted by this issue may be more inclined to prefer personalized face-to-face attention in addressing this sensitive area in the rehabilitation process.
The studies used various methods to support SCI patients in the home and community through teleSCI interventions using various technologies. The common mode of intervention delivery included telephones and computers for videoconferencing, interactive voice response, and online data messaging systems. Web-based platforms, as expected, were widely used and still remain the conventional technology. This is consistent with the general trend in telemedicine practices for other medical conditions.42,43 However, judging from the consistency of traditional technologies used in earlier studies considered to date,42,43 not much has evolved to yield innovative or cutting edge technology in recent years, at least not in the extent to which it would have been considered applicable to drastically impact telerehabilitation practices. The void brought on by this lack of technology advancement—observed across studies of recent years—maintains use of conventional platforms as status quo.42,43
Although earlier innovations may have served as driving forces toward the significant development of telemedicine, technological performance and applicability may be one of the biggest challenges to implementing teleSCI across the globe. Secondary technologies were also required in many situations. These included webcams, smartphones, speakers, microphones, portable laptops, remote wireless monitoring systems, and wearable devices. The concurrent reality is that many elderly patients who require ongoing rehabilitation are unfamiliar with using smart devices, whereas individuals with limited function likely require assistance in operating technological devices. Reliable internet connections with adequate speed and the need for secondary equipment with knowledge in their operability are tangible challenges44,45 to stabilizing and ensuring the flawless delivery of interventions for these patients' optimal clinical care. These challenges are limiting factors and serve as catalysts in the future direction for teleSCI research and clinical practice.
The advent of smart technology has given birth to a myriad of lifestyle conveniences. It has also served to be pivotal in the delivery of health care through telemedicine. Ironically, it has also resulted in costly losses for many victims falling akin to hacking schemes and identity theft due to personal information security deficiencies. Data security and maintenance of the privacy of personal information are critical issues in clinical practice. Those involved in handling such sensitive information must abide by HIPAA compliance standards and other security regulations.46–48 In contrast, most studies in our review failed to address privacy issues and data protection. Patients' records should be kept highly secured, intact, and protected from third-party theft or access without consent.49 They should be accessible solely to authorized individuals only when needed, strictly for purposes of health care delivery or medicolegal situations. Security systems such as the Intrusion Detection System—automatically detect malicious activities and report to security service providers50—or similar security systems should be mandated to handle data acquisition of private and personal information in research activities. The prevention of unintended leakage of and securing personal data remain a critical challenge in teleSCI. Hall and McGraw validate this by asserting in the title of their article: “for telemedicine to succeed, privacy and security risks must be identified and addressed.”48
The burdensome question of cost-effectiveness and benefits to both patients and providers alike will likely impact decisions regarding the implementation of teleSCI.51 Telemedicine practices in other specialties have shown reduced costs compared with traditional face-to-face visits. It yields an overall decrease in treatment costs and transportation costs by minimizing the frequency of in-person clinic appointments.50 Furthermore, it reduces time out of office costs for employees and employers by eradicating the need to take time off from work. Arora et al.—whose study failed to meet inclusion criteria and thus excluded in this review—validated the cost–benefits of teleSCI intervention using technology among participants with pressure injuries.52 Since SCI rehabilitation is an ongoing and expensive process, the use of teleSCI may decrease financial burdens on patients and the health care system. However, further studies are needed to draw meaningful conclusions in areas of cost-effectiveness for SCI management.
Limitations
Although the studies in this systematic review addressed different aspects of SCI management using conventional technology platforms, the study's inclusion criteria served to be a limitation by failing to capture a sizable compilation of journal articles. Consequently, the included studies' heterogeneity made comparison difficult across selected studies, particularly for quantitative analysis of outcome measures.
Conclusion
The majority of studies in this review demonstrated significant positive outcomes to validate current teleSCI practices' clinical effectiveness using conventional technology. The qualitative synthesis results further expand our understanding of teleSCI's impact and its demonstrated potential for improving SCI individuals' lives. However, the development of new data generated by ongoing research efforts to promote the “buy-in” toward widespread teleSCI implementation is warranted.
Acknowledgments
The authors acknowledge Yunhwan Lee, Kim Dongwan, Jung Seongwoo for their assistance with this article.
Abbreviations Used
- ARAT
Action Research Arm Test
- CI
confidence interval
- CP
cerebral palsy
- ePACT
electronic personal admin of cognitive therapy
- ES
effect size
- ET
exercise therapy
- HIPAA
Heath Insurance Portability and Accountability Act
- JSES
Job Procurement Self-Efficacy Scale
- MPT
Min Push Test
- MS
multiple sclerosis
- MWT
Min Walk Test
- OR
odds ratio
- PAM
Patient Activation Measure
- PEDro
Physiotherapy Evidence Database
- QALY
quality-adjusted life years
- QoL
quality of life
- RCT
randomized controlled or clinical trial
- SCI
spinal cord injury
- SCI/D
spinal cord injury or dysfunction
- teleSCI
spinal cord injury telerehabilitation
Appendix A1
Appendix A1. Abbreviations
| WHO-QOL-BREF | WHO-QoL-Brief Instrument Form |
| HR-QoL | health related-QoL |
| PWI | Personal Well-being Index |
| SCLWL | Spinal Cord Lesion Emotional Well-being |
| PHQ-9 | Patient Health Questionnaire-9 |
| QALY | quality-adjusted life years |
| PUSH | Pressure Ulcer Scale for Healing |
| NRS | numerical rating scale |
| PCS | Pain Catastrophizing Scale |
| CES-D | CES Depression Scale |
| DASS-21 | Depression Anxiety and Stress Scale |
| BDI-II | Beck Depression Inventory-II |
| HADS | Hospital Anxiety and Depression Scale |
| CHART-SF | Craig Handicap Assessment and Reporting Technique Short Form |
| PADS | Physical Activity and Disability Survey |
| SCI-SC | SCI Secondary Conditions Scale |
| SCIM-III | Spinal Cord Independence Measure |
| COPM | Canadian Occupational Performance Measure |
| WHODAS | WHO Disability Assessment Schedule |
| CHART-SF | Craig Handicap Assessment and Reporting Technique Short Form |
| FFMQ | Five Facet Mindfulness Questionnaire |
| PAM | Patient Activation Measure |
| PACIC | Patient Assessment of Chronic Illness Care |
| ASIS | Adolescent Self-Management and Independence Scale |
| CHIEF-SF | Craig Hospital Inventory of Environmental Factors-Short Form |
| ARAT | Action Research Arm Test |
| RAHFT | ReJoyce Automated Hand Function Test |
| TAI | Transfer Assessment Instrument |
| JSES | Job Procurement Self-Efficacy Scale |
| LOT-r | Life Orientation Test-Revised. |
Author Disclosure Statement
The authors declare no conflict of interest.
Funding Information
This article was made possible by Korea Health Technology R&D Project and funded by the Minister of Health and Welfare, Republic of Korea (Grant No. HI18C0552). A grant was also provided from the Brain Pool Scholar's program of the National Research Foundation of Korea (Grant No. 2019H1D3A2A01101579).
Cite this article as: Lee S, Kim J, Kim J (2021) Substantiating clinical effectiveness and potential barriers to the widespread implementation of spinal cord injury telerehabilitation: a systematic review and qualitative synthesis of randomized trials in the recent past decade, Telemedicine Reports 2:1, 64–77, DOI: 10.1089/tmr.2020.0026.
References
- 1. Liem NR, McColl MA, King W, et al. Aging with a spinal cord injury: factors associated with the need for more help with activities of daily living. Arch Phys Med Rehabil 2004;85:1567–1577. [DOI] [PubMed] [Google Scholar]
- 2. Fonseca L, Tigra W, Navarro B, et al. Assisted grasping in individuals with tetraplegia: improving control through residual muscle contraction and movement. Sensors MDPI 2019;19:4532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Amatachaya S, Wannapakhe J, Arrayawichanon P, et al. Functional abilities, incidences of complications and falls of patients with spinal cord injury 6 months after discharge. Spinal Cord 2011;49:520–524. [DOI] [PubMed] [Google Scholar]
- 4. Krueger H, Noonan VK, Trenaman LM, et al. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can 2013;33:113–122. [PubMed] [Google Scholar]
- 5. Korea Spinal Cord Injury Association. Available at www.kscia.org/board/view/menu03_05/21450 Accessed February 1, 2020.
- 6. Hossain MS, Harvey LA, Rahman MA, et al. A pilot randomised trial of community-based care following discharge from hospital with a recent spinal cord injury in Bangladesh. Clin Rehabil 2017;31:781–789. [DOI] [PubMed] [Google Scholar]
- 7. Lai B, Rimmer J, Barstow B, et al. Tele-exercise for persons with spinal cord injury: a mixed-methods feasibility case series. JMIR Rehabil Assist Technol 2016;3:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Irgens I, Rekand T, Arora M, et al. Telehealth for people with spinal cord injury: a narrative review. Spinal Cord 2018;56:643–655. [DOI] [PubMed] [Google Scholar]
- 9. Akhtar R, Alam S, Siddiquee NKA. Telemedicine: an ICT based healthcare approach to ensure health service for all. Int J Community Med Public Health 2019;6:3732–3738. [Google Scholar]
- 10. Scott R, Mars M. Telehealth in the developing world: current status and future prospects. Smart Homecare Technol Telehealth 2015;2015:25–37. [Google Scholar]
- 11. Kryger MA, Crytzer TM, Fairman A, et al. The effect of the interactive mobile health and rehabilitation system on health and psychosocial outcomes in spinal cord injury: randomized controlled trial. J Med Internet Res 2019;21:e14305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dugas M, Gao GG, Agarwal R. Unpacking mHealth interventions: a systematic review of behavior change techniques used in randomized controlled trials assessing mHealth effectiveness. Digit Health 2020;6:2055207620905411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Marcolino MS, Oliveira JAQ, D'Agostino M, et al. The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth 2018;6:e23. doi: 10.2196/mhealth.8873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim AY, Choi WS. Considerations on the implementation of the telemedicine system encountered with stakeholders' resistance in COVID-19 pandemic. Telemed eHealth 2020. [DOI] [PubMed] [Google Scholar]
- 15. van de Pol E, Lucas K, Geraghty T, et al. The delivery of specialist spinal cord injury services in Queensland and the potential for telehealth. BMC Health Serv Res 2016;16:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Varshneya R. 7 telemedicine concerns and how to overcome them. The Arizona Telemedicine Program. October 11, 2018. Available at https://telemedicine.arizona.edu/blog/7-telemedicine-concerns-and-how-overcome-them Accessed December 21, 2020.
- 17. Elkins MR, Herbert RD, Moseley AM, et al. Rating the quality of trials in systematic reviews of physical therapy interventions. Cardiopulm Phys Ther J 2010;21:20–26. [PMC free article] [PubMed] [Google Scholar]
- 18. Nazviya M, Kodukula S. Evaluation of critical success factors for telemedicine implementation. Int J Comput Appl 2011;12:0975–8887. [Google Scholar]
- 19. Leochico CFD, Espiritu AI, Ignacio SD, et al. Challenges to the emergence of telerehabilitation in a developing country: a systematic review. Front Neurol 2020;11:1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 2009;55:129–133. [DOI] [PubMed] [Google Scholar]
- 21. Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 2003;83:713–721. [PubMed] [Google Scholar]
- 22. Migliorini C, Sinclair A, Brown D, et al. A randomised control trial of an Internet-based cognitive behaviour treatment for mood disorder in adults with chronic spinal cord injury. Spinal Cord 2016;54:695–701. [DOI] [PubMed] [Google Scholar]
- 23. Arora M, Harvey LA, Glinsky JV, et al. Cost-effectiveness analysis of telephone-based support for the management of pressure ulcers in people with spinal cord injury in India and Bangladesh. Spinal Cord 2017;55:1071–1078. [DOI] [PubMed] [Google Scholar]
- 24. Kowalczewski J, Chong SL, Galea M, et al. In-home tele-rehabilitation improves tetraplegic hand function. Neurorehabil Neural Repair 2011;25:412–422. [DOI] [PubMed] [Google Scholar]
- 25. Hearn JH, Finlay KA. Internet-delivered mindfulness for people with depression and chronic pain following spinal cord injury: a randomized, controlled feasibility trial. Spinal Cord 2018;56:750–761. [DOI] [PubMed] [Google Scholar]
- 26. Houlihan BV, Brody M, Everhart-Skeels S, et al. Randomized trial of a peer-led, telephone-based empowerment intervention for persons with chronic spinal cord injury improves health self-management. Arch Phys Med Rehab 2017;98:1067–1076. [DOI] [PubMed] [Google Scholar]
- 27. Coulter EH, McLean AN, Hasler JP, et al. The effectiveness and satisfaction of web-based physiotherapy in people with spinal cord injury: a pilot randomized controlled trial. Spinal Cord 2017;55:383–389. [DOI] [PubMed] [Google Scholar]
- 28. Worobey LA, Rigot SK, Hogaboom NS, et al. Investigating the efficacy of web-based transfer training on independent wheelchair transfers through randomized controlled trials. Arch Phys Med Rehab 2018;99:9–16. [DOI] [PubMed] [Google Scholar]
- 29. Rimmer JH, Wang E, Pellegrini CA, et al. Telehealth weight management intervention for adults with physical disabilities: a randomized controlled trial. Am J Phys Med Rehabil 2013;92:1084–1094. [DOI] [PubMed] [Google Scholar]
- 30. Dorstyn D, Roberts R, Murphy G, et al. Work and SCI: a pilot randomized controlled study of an online resource for job-seekers with spinal cord dysfunction. Spinal Cord 2019;57:221–228. [DOI] [PubMed] [Google Scholar]
- 31. Shen D, Huang H, Yuan H, et al. Clinical treatment of orthostatic hypotension after spinal cord injury with standing training coupled with a remote monitoring system. Med Sci Monit 2014;20:2767–2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Houlihan BV, Jette A, Friedman RH, et al. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord 2013;51:715–720. [DOI] [PubMed] [Google Scholar]
- 33. Wootton R. Twenty years of telemedicine in chronic disease management—an evidence synthesis. J Telemed Telecare 2012;18:211–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Singh A, Tetreault L, Kalsi-Ryan S, et al. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol 2014;6:309–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kang Y, Ding H, Zhou HX, et al. Epidemiology of worldwide spinal cord injury: a literature review. J Neurorestoratol 2018;6:1–9. [Google Scholar]
- 36. Furlan J, Sakakibara B, Miller W, et al. Global incidence and prevalence of traumatic spinal cord injury. Canad J Neurolog Sci 2013;40:456–464. [DOI] [PubMed] [Google Scholar]
- 37. World Health Organization. International perspectives on spinal cord injury. November 2013. Available at https://www.who.int/publications/i/item/international-perspectives-on-spinal-cord-injury Accessed December 21, 2020.
- 38. Noonan V, Elaine Chan, Bassett-Spiers K, et al. Facilitators and barriers to international collaboration in spinal cord injury: results from a survey of clinicians and researchers. J Neurotrauma 2018;35:478–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Biering-Sørensen B, Noonan V. Standardization of data for clinical use and research in spinal cord injury. Brain Sci 2016;6: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Litwin MS, Nied RJ, Dhanani N. Health-related quality of life in men with erectile dysfunction. J Gen Intern Med 1998;13:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Anderson R, Moses R, Lenherr S, et al. Spinal cord injury and male infertility—a review of current literature, knowledge gaps, and future research. Transl Androl Urol 2018;7(Suppl. 3):S373–S382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wilson L, Maeder A. Recent directions in telemedicine: review of trends in research and practice. Healthcare Informat Res 2015;21:213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cao MD, Shimizu S, Antoku Y, et al. Emerging technologies for telemedicine. Korean journal of radiology 2012;13(Suppl. 1):S21–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kahn JM. Virtual visits—confronting the challenges of telemedicine. N Engl J Med 2015;372:1684–1685. [DOI] [PubMed] [Google Scholar]
- 45. Harst L, Timpel P, Otto L, et al. Identifying barriers in telemedicine-supported integrated care research: scoping reviews and qualitative content analysis. J Public Health 2020;28:583–594. [Google Scholar]
- 46. Luxton D, Kayl RA, Mishkind MC. mHealth data security: the need for HIPAA-compliant standardization. Telemed eHealth 2012;18:284–288. [DOI] [PubMed] [Google Scholar]
- 47. Zhou L, Thieret R, Watzlaf V, et al. A telehealth privacy and security self-assessment questionnaire for telehealth providers: development and validation. Int J Telerehabil 2019;11:3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hall J, McGraw D. For telehealth to succeed, privacy and security risks must be identified and addressed. Health Affairs 2014;33:216–221. [DOI] [PubMed] [Google Scholar]
- 49. Gill KS, Saxena S, Sharma A. Taxonomy of security attacks on cloud environment: a case study on telemedicine. In: 2019. Amity International Conference on Artificial Intelligence, Dubai, UAE, February 4–6, 2019, pp. 454–460. IEEE. [Google Scholar]
- 50. Gill KS, Sharma A. IDPS based framework for security in green cloud computing and comprehensive review on existing frameworks and security. In: 2015. International Conference on Computing, Communication and Security (ICCCS), Pamplemousses, Mauritius, December 4–5, 2015, pp. 1–6. IEEE. [Google Scholar]
- 51. Noel H, Vogel D, Erdos J, et al. Home telehealth reduces healthcare costs. Telemed J E Health 2004;10:170–183. [DOI] [PubMed] [Google Scholar]
- 52. Arora M, Harvey LA, Hayes AJ, et al. Effectiveness and cost-effectiveness of telephone-based support versus usual care for treatment of pressure ulcers in people with spinal cord injury in low-income and middle-income countries: study protocol for a 12-week randomised controlled trial. BMJ Open 2015;5:e008369. [DOI] [PMC free article] [PubMed] [Google Scholar]