Abstract
Background
Community participation has the potential to improve the effects of interventions and reduce inequalities in child growth. Multidimensional indicators capture such effects and inequalities.
Objectives
The objective of this study was to measure the association between multidimensional child growth and community participation in 2 nutrition-sensitive interventions.
Methods
A Multidimensional Index of Child Growth was calculated with the 5-y-old cohort of the Vietnam Young Lives Survey. Young Lives is a unique dataset that has information on community participation in the design and implementation stages of 2 interventions: a health and a water, sanitation, and hygiene (WASH) intervention. Community participation during the interventions was recorded retrospectively with interviews at the household level. Ordinary least-squares and quantile regressions were estimated using data on 240 children. A Multidimensional Index of Child Advantage, sex, and location (urban/rural) were included as control covariates.
Results
A positive association (post hoc statistical power = 0.859) was estimated for community participation during the design stage of the WASH intervention, particularly for the most deprived children (P < 0.05). Negative effects were estimated for the health intervention during the design stage (P < 0.05) and no significant effects were found for community participation during the implementation stage of the interventions. Instead of the physical dimension, the significant associations in the design stage were related to the nonphysical dimension of child growth. Inequalities in multidimensional growth were found for children living in rural areas, but not for girls.
Conclusions
The association between community participation and multidimensional child growth is indicative of the importance of community participation during the design phase of interventions, in particular for the nonphysical dimensions of child growth related to social and psychological factors. The benefits of participation were greater for urban children compared with rural children, which deserves further attention.
Keywords: multidimensional child growth, community participation, capability approach, Young Lives Survey, nutrition
The association of community participation with multidimensional child growth is calculated for 2 nutrition-sensitive interventions for a cohort of 5-y-old children from Vietnam.
Introduction
The UNICEF framework for malnutrition established in 1990 (1) has contributed to child survival and has guided the development of interventions that helped reduce undernutrition as assessed based on anthropometry―that is, underweight, wasting, and stunting. However, new challenges have arisen as a result of the double burden of malnutrition (2), in which overweight and obesity coexist with undernourishment and micronutrient deficiencies within a single population in many countries. This is indicative of malnutrition as a societal rather than an individual problem or responsibility (3).
A multidimensional approach to child growth has been suggested by the WHO-UNICEF-Lancet Commission for children not only surviving but thriving (4, 5). The Task Force “Towards a Multi-dimensional Index to Child Growth,” of the International Union of Nutritional Sciences, conceptualizes child growth not only as physical growth but rather as the process of continuous physical and nonphysical (psychological and social) change that builds a child's capacities to maximize life chances at the individual and societal level (6). In line with the Convention of the Rights of the Child, this multidimensional approach aims to capture the indirect causes of malnutrition, such as constraints from parents and caregivers, the ability of children to learn within the proximal family environments, and distant factors that affect child (dis)advantage (6, 7). A multidimensional approach can help to improve the understanding of the root causes of malnutrition, it can identify who is accountable for it, and can point towards novel actions to reduce inequalities in child growth (6).
Community participation is considered a potentially useful strategy to reduce inequalities in the effects of nutrition-sensitive interventions (8–11). Community engagement makes interventions more aligned with local priorities, and community participation can give a voice to disadvantaged groups that tend to have poorer health and nutrition conditions (9). The evidence that links community participation with improved health outcomes is, however, not strong (12) and the effects of community-level interventions on child nutritional status have been difficult to assess (2). This could be explained by the outcome metrics and the study design. Studies evaluating the impact of community participation have been based on randomized clinical trials and mono-dimensional outcome indicators, such as weight and height, reflecting the biomedical model that is used as a framework for understanding health outcomes (12). For example, Perry and Zulliger (13) reflect on the role of community health workers in relation to health outcomes such as under-5 mortality, breastfeeding rates, or infectious diseases. Rifkin (14) concludes that this approach may not be suitable for the evaluation of the impact of community participation as both its implementation and effects are highly situational. She argues that we should acknowledge this situational aspect, as it is needed to reach vulnerable populations. Qualitative participatory approaches are able to capture the importance of context in the effectiveness of interventions (15) and can identify barriers or levers (16). For monitoring and evaluation purposes, we would need a quantitative approach that can pick up the multidimensional aspects of the context as in qualitative research. To achieve this goal, we propose a multidimensional index of child growth that accounts for context at the parental and community level, while also allowing the inclusion of multiple dimensions of child growth in the outcomes.
The aim of this study is to measure the association between community participation and multidimensional child growth calculated with the Young Lives (YL) cohort of 5-y-old children in Vietnam (YL round 2, 2006). The YL is a unique dataset with information on community participation in the design and implementation stages of 2 nutrition-sensitive interventions: a health intervention and a water, sanitation, and hygiene (WASH) intervention. Community participation is considered to be beneficial during the design and implementation stages of interventions, but there is little evidence on the effect of community participation in terms of outcomes at both the community and individual level (11, 12). Moreover, there is no standard definition of “community” and “participation” (12), as community participation is an elastic concept, open-ended over what a community is and what behaviors satisfy participation (17). Based on a previous meta-analysis (9), a community can be defined as a group of people with some common feature, like their geographical location, since most people tend to identify the spatial locality in which they live and work as their community (18). In YL, geographical locations are called sentinel sites and represent a commune with an average population of approximately 7000 persons who have a local government, a primary school, a health center, post office, and a market (19).
Participation, in turn, can be defined as the involvement of an active group of people in an intervention or the involvement of a person who is representative of the group (11, 20). In our study, being informed, being consulted, and have taken part in the decision-making process were all considered forms of participation. Even if the degree of involvement could be low when people are only informed or consulted, both being informed and consulted imply social inclusion and are considered forms of participation in Arnstein's and Pretty's typologies of participation. Arnstein's ladder of participation (21) goes from no participation to tokenism and then to effective citizen power, with tokenism being a form of participation that includes being informed or consulted (22). In Pretty's typology (18, 22, 23), being informed is a passive form of participation, while participation by consultation implies playing a key role defining problems and dictating directions (18).
Previous research (9) argued that in order to assess the potentially diverse impacts of community engagement in interventions, researchers need to consider a spectrum of outcome measures. In our study, we considered a spectrum of multidimensional indicators of child growth at physical and nonphysical levels as potential outcomes. Multidimensional indicators are needed to identify inequalities in both the physical and nonphysical dimensions of human development (3), because mono-dimensional indicators of nutrition based on anthropometry only measure inequalities at the physical level. A multidimensional approach grasps the complex interaction between physical and nonphysical determinants of child growth, and hence can suggest new routes for improving the outcomes of nutrition-sensitive interventions. For example, recent evidence (24) indicates that physical growth and cognitive development respond differently to interventions: nutrient supplementation improves physical growth in children, and at the same time, nonphysical determinants like responsive caregiving, nurturing, and stimulation improve cognitive development.
Methods
Description of data
Young Lives is an international study on childhood poverty that has data on anthropometry and includes rich contextual information about the children's lives and facilities available to them. Four countries are included in the YL study: Ethiopia, Peru, India, and Vietnam. Round 1 of the YL study followed 2000 children aged between 6 and 18 mo in 2002 and their households, from both urban and rural communities, in each of the 4 countries (8000 children in total). Round 2 of the study returned to the same children who were aged 1 y old in round 1 but were aged approximately 5 y old at the time of collecting data for round 2. Finally, in round 3, the information was collected for the same children when they were aged 7 to 8 y. The information of the cohort of children aged 5 y old in round 2 of the YL study for Vietnam was used to calculate a Multidimensional Index of Child Growth (MICG) and a Multidimensional Index of Child Advantage (MICA), since the experiences during early childhood shape biological and psychological structures and functions in ways that affect health and well-being throughout the life course (25).
The round 2 cohort of Vietnam has information on 5-y-old children living in the provinces of Lao Cai, Hung Yen, Da Nang, Phu Yen, and Ben Tre. Rather than being randomly selected across the country, YL selected 100 children living in the 20 geographic clusters that were chosen because these clusters 1) are located in the northern, central, and southern areas of Vietnam; 2) include urban, rural, and mountainous areas; 3) are relatively poor; and 4) reflect some unique factors of the country, such as areas prone to natural disasters and areas heavily affected by past wars (26). Face-to-face interviews using structured questionnaires were used to collect the data in the YL survey. The caregivers and the children (if the children in the household are old enough) were interviewed by fieldworkers every 3 to 4 y with a quantitative survey. The height and weight of each child were measured, and community-level questionnaires were completed for each geographical cluster at every data-collection round. The questionnaires, including the age-5 younger cohort household questionnaire as well as the community questionnaire, can be downloaded from the YL website (https://www.younglives.org.uk/content/round-2-questionnaires).
Community participation and nutrition-sensitive interventions in Vietnam
In the YL study, fieldworkers asked retrospectively the level of participation during the design stage and during the implementation stage―procurement, management, and operations―of 2 nutrition-sensitive interventions: a health intervention and a WASH intervention. The health intervention is related to the creation of infrastructure for medical stations in the sentinel sites of Vietnam, whereas the WASH intervention is a clean-water project for the whole commune. This type of water and sanitation project can improve children's health and well-being through indirect mechanisms, such as reducing the time needed for obtaining and transporting water (2) or, in the case of the intervention of Vietnam, by improving the quality of water for the commune (19).
Community participation is understood as having been informed, having been consulted, or having taken part in the decision-making process of the health and WASH interventions in the sentinel sites (communes) of YL. The answers of the YL study “veto in decision making, vote in decision making, consulted during decision-making process and informed, but not involved in decision making” are considered wide forms of community participation in the interventions of the sentinel sites of YL, and were coded as “with participation,” while the answer of “no participation” was coded as “no participation.”
Multidimensional indicators
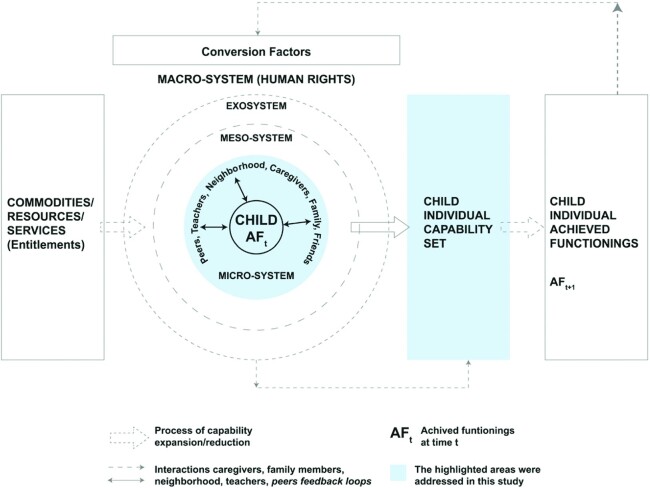
The YL round 2 cohort of Vietnam was used to build an MICG and an MICA. The empirical estimates of MICG and MICA were constructed building on the theoretical framework of capabilities for child growth (Figure 1) that is grounded in the Convention of the Rights of the Child (3, 6, 7).
FIGURE 1.
Theoretical capability framework for multidimensional child growth. Adapted from (7). Reproduced with permission from Springer Nature Customer Service Centre.
The construction of the indices was dependent on the data available in the survey—hence, the choice of the YL survey as a contextually rich database that includes nonphysical indicators besides anthropometry. A detailed description of the construction of the indices using YL data is given in Supplemental Table 1. In short, MICG was constructed from 29 indicators that measure the physical and nonphysical capabilities for a child's well-being (27). MICA is constructed from 21 indicators at the parental, household, and community level. MICG includes physical indicators of growth (overweight, stunting, and wasting), nutrition (frequency and diversity of food intake), and nonphysical indicators like, for example, those related to the love that children receive from parents and caregivers, leisure activities of children, cognitive and verbal development, or time autonomy (hours of domestic tasks). MICA, in turn, includes mediators―called conversion factors in the capability approach, as indicated in Figure 1―that capture situational effects at the parental, household, and community level, like, for example, information on whether both parents are alive or not, the mother's BMI and height, parity, household economic situation and access to services, crowding, and community-level variables such as the existence of health and educational facilities and the occurrence of natural disaster in a community.
The multidimensional indicators were aggregated into a single index using the Alkire-Foster (AF) method (28). In the AF method, deprivation cutoffs are defined for each indicator, and the cutoffs are applied to identify deprived children. For example, for the indicator “stunting” in the physical dimension, a child is considered deprived if she/he has a length/height-for-age z score of less than 2 SDs, while in the nonphysical dimension, a child is considered deprived for the indicator “verbal development” if she/he has a Peabody Picture Vocabulary Test (PPVT) below the first quintile. Finally, a weight is assigned to each indicator, and the MICG and MICA indices are calculated as 1 less the weighted sum of deprivations, to signify multidimensional growth, as they are expressed as achievements. Higher values of MICG and MICA indicate higher multidimensional achievements. The deprivation threshold for each indicator and the weights are displayed in Supplemental Table 1 and Supplemental Table 2.
Ordinary least squares and quantile regressions
The association of community participation with MICG was estimated with ordinary least squares (OLS) and quantile regressions (29, 30). OLS provides a summary of the association of community participation with the average distribution of multidimensional child growth. As OLS only estimates average effects, quantile regressions are included in the analysis to measure the effects for children with low and high multidimensional growth—that is, the effects of community participation on the lower and upper quantiles of the MICG distribution.
The MICA, sex, and location (urban/rural) were used as control covariates in the regressions. MICA was incorporated in the regressions as an aggregate covariate―instead of separate individual indicators―to increase degrees of freedom and reduce multicollinearity. Interaction terms were included in the regressions to account for the influence of community location on the relation between participation and MICG. As noted by Clark et al. (2), community engagement is different in urban settlements compared with rural communities; hence, the interaction between participation and location (urban/rural) was included as an explanatory variable in the regressions to estimate the differences between community participation in urban communes against community participation in rural communes.
Results
The effective sample size in the YL cohort of Vietnam (round 2) is 1971 children. A complete dataset needed to calculate the indicators of MICG and MICA is available for 1731 children, and of those 1731 children, only 240 children―110 male children (46%) and 130 female children (54%)―live in communes where the health and the WASH interventions took place. The post hoc statistical power to detect effects of community participation on child growth for the sample size of 240 children is equal to 0.8586 (85.9%), given a significance level of 10% and an effect size (delta) of 0.0383 (3.83%), and is equal to 0.7748 (77.48%) for a significance level of 5% and the same effect size. See Supplemental Materialfor details about the power calculations and the representativeness of the subsample of 240 children against the complete sample in the YL cohort of Vietnam. No differences in MICG and MICA were found between the subsample of 240 children and the larger sample of 1731 children.
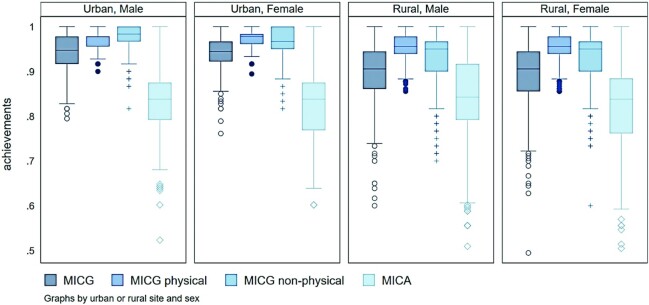
Table 1 shows descriptive statistics of the data used to estimate the multidimensional child growth and the regressions. Of the 240 children, 99 (41%) live in households where caregivers participated in the design stage of the health intervention, 139 (58%) live in households that participated in the design stage of the WASH intervention, 124 (52%) live in households that participated in the implementation stage of the health intervention, and 141 (59%) live in households that participated in the implementation stage of the WASH intervention. Figure 2 shows the distribution of the MICG and the MICA calculated with the information of the 240 children in Vietnam. More dispersion (heterogeneity) in child growth is observed in rural regions, compared with urban areas, particularly for the nonphysical dimensions.
TABLE 1.
Descriptive statistics of the data used in the study1
| Design stage | Implementation stage | ||||||
|---|---|---|---|---|---|---|---|
| Intervention | Community participation | Male | Female | Total | Male | Female | Total |
| Health | No participation | 63 | 78 | 141 | 52 | 64 | 116 |
| (26.3) | (32.5) | (58.8) | (21.7) | (26.7) | (48.3) | ||
| With participation | 47 | 52 | 99 | 58 | 66 | 124 | |
| (19.6) | (21.7) | (41.3) | (24.2) | (27.5) | (51.7) | ||
| Total | 110 | 130 | 240 | 110 | 130 | 240 | |
| WASH | No participation | 48 | 53 | 101 | 50 | 49 | 99 |
| (20) | (22.1) | (42.1) | (20.8) | (20.4) | (41.3) | ||
| With participation | 62 | 77 | 139 | 60 | 81 | 141 | |
| (25.8) | (32.1) | (57.9) | (25) | (33.8) | (58.8) | ||
| Total | 110 | 130 | 240 | 110 | 130 | 240 | |
Percentage of total is shown in parentheses below each frequency. WASH, water, sanitation, and hygiene.
FIGURE 2.
Differences in the distribution of MICG and MICA for female and male children living in urban and rural areas. The distribution is similar between female and male children, but rural children have lower physical and non-physical multidimensional growth, as well as a more dispersed MICA. MICA, Multidimensional Index of Child Advantage; MICG, Multidimensional Index of Child Growth.
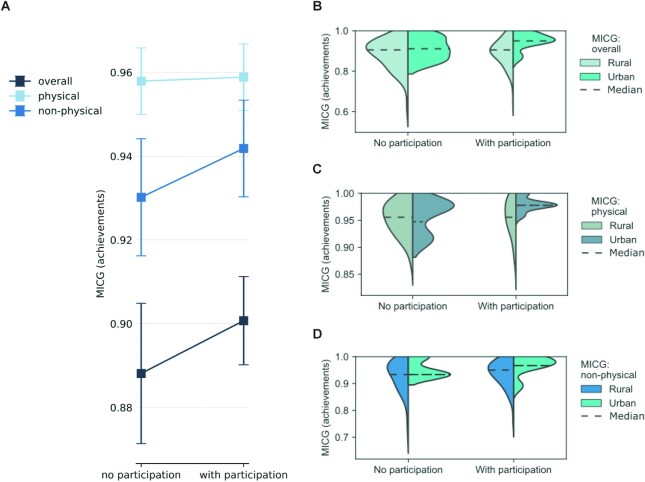
Table 2 shows the results of estimating the relation of MICG with community participation, after controlling for sex, rural/urban location, and child advantage (MICA). On average, differences in multidimensional growth were observed when community participation takes place during the design stage of the interventions, instead of the implementation stage. Positive effects were estimated for the WASH intervention (P < 0.10), particularly for the most deprived children (P < 0.05)―that is, for those children with low multidimensional child growth (the first quintile of MICG). No significant main effects were found for children in the fourth quintile, and no statistically significant results were obtained for community participation in the implementation stage. The main effects of community participation on child growth were related to the nonphysical dimension (P < 0.10)―which includes social and psychological characteristics―instead of the physical dimension that includes anthropometric indicators such as overweight, stunting, and wasting.
TABLE 2.
Regression results: association of community participation with multidimensional child growth1
| Quantile regressions | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Ordinary least squares (average MICG) | First quintile (low MICG) | Fourth quintile (high MICG) | |||||||
| Covariate | Overall | Physical | Nonphysical | Overall | Physical | Nonphysical | Overall | Physical | Nonphysical |
| Main effects | |||||||||
| MICA | 0.281*** | 0.0837*** | 0.1973*** | 0.3636*** | 0.1385*** | 0.2118* | 0.2057*** | 0.0400 | 0.0706 |
| Sex (female) | 0.0022 | 0.0061 | −0.0039 | −0.0007 | 0.0064 | −0.0147 | −0.0025 | 0.0026 | −0.0023 |
| Rural regions | −0.0131 | −0.0062 | −0.0069 | −0.0231 | −0.0214 | −0.0157 | 0.006 | 0.0119 | −0.0131 |
| Community participation during designstage | |||||||||
| WASH intervention | 0.0218* | 0.0048 | 0.0170* | 0.0389** | 0.0171 | 0.0392 | 0.0076 | 0.0109 | 0.0023 |
| Health intervention | −0.0278** | −0.0100 | −0.0178 | −0.0382 | −0.0218 | −0.0373 | −0.0263 | −0.0063 | −0.0029 |
| Community participation duringimplementation stage | |||||||||
| WASH intervention | −0.0061 | −0.0021 | −0.0041 | −0.0263 | −0.0009 | −0.0157 | 0.004 | −0.0061 | 0.0000 |
| Health intervention | 0.0049 | −0.0008 | 0.0057 | 0.0145 | 0.0004 | 0.0304 | 0.0016 | −0.0043 | −0.0082 |
| Interaction terms: community participation andtype of site (urban vs. rural) | |||||||||
| Community participation during design stage(urban areas) | |||||||||
| WASH intervention | 0.1067*** | 0.0681*** | 0.0386*** | 0.0549 | 0.0504** | −0.0206 | 0.1322*** | 0.0735*** | 0.0595** |
| Health intervention | −0.0327 | −0.046*** | 0.0133 | 0.0453 | −0.0171 | 0.102 | −0.0857** | −0.0694*** | −0.0526* |
| Community participation during implementationstage (urban areas) | |||||||||
| WASH intervention | −0.0498* | −0.0503*** | 0.0005 | 0.0096 | −0.0378 | 0.0559 | −0.0984 | −0.0528 | −0.0552 |
| Health intervention | 0.0183 | 0.0532*** | −0.0349 | −0.0551 | 0.0269 | −0.148 | 0.0908 | 0.08 | 0.0637 |
n = 240. Standard errors were calculated with a robust variance-covariance matrix. The ordinary least squares regression was estimated with robust clusterized errors, using the community as the cluster. First quintile: percentile 20, third quintile: percentile 80. In the interaction terms, rural areas are the base category. *P < 0.1, **P < 0.05, ***P < 0.01. MICA, Multidimensional Index of Child Advantage; MICG, Multidimensional Index of Child Growth; WASH, water, sanitation, and hygiene.
In terms of estimated marginal effects, no statistically significant difference in MICG was observed between male and female children, but significant differences were found between urban and rural areas. The interaction between rural/urban status and community participation indicates that deprived children in urban areas benefited more from community participation than those in rural areas, both in the physical and nonphysical dimensions of child growth (P < 0.01). Figure 3 illustrates these differences by plotting marginal effects with 95% CIs against the empirical distribution of MICG in rural and urban regions. On average, higher marginal effects were observed in communities with parti-cipation during the design stage of the WASH intervention, particularly for the nonphysical dimensions of child growth (Figure 3A). Compared with rural regions, however, higher multidimensional growth was observed in the median of overall MICG of children living in urban communities with participation (Figure 3B), in both the physical dimension (Figure 3C) and the nonphysical dimension of child growth (Figure 3D).
FIGURE 3.
(A–D) Effects of community participation on multidimensional child growth: WASH intervention—design stage. (A) Marginal effects of community participation on multidimensional child growth calculated with the ordinary least squares regression. Panels B, C, and D show the fit of a kernel density to the distribution of MICG in rural and urban communities. The dotted lines represent the median of the empirical distribution. MICG, Multidimensional Index of Child Growth; WASH, water, sanitation, and hygiene.
Discussion
We developed an MICG with the YL cohort of 5-y-old children in Vietnam as a way to evaluate the association between community participation and MICG in 2 nutrition-sensitive interventions. A significant association was found between multidimensional child growth and community participation that takes place during the design stage of the interventions, instead of during the implementation stage. Larger effects were found for the nonphysical dimensions of growth that include social and psychological indicators, and for children with lower multidimensional growth. Inequalities in child growth were identified for children living in rural areas, but not for female children.
The multidimensional conceptualization of child growth facilitates the evaluation of community participation in the interventions. Multidimensional indicators capture both the physical and nonphysical dimensions of child growth, and hence can identify the direct causes of malnutrition―related to the number of times and the diversity of food groups a child eats every day, both of which directly affect anthropometry―as well as the indirect causes of malnutrition, such as those related to the love and care received from parents and parents’ responsibility. Using anthropometry only, as an indicator in the physical dimension, would have suggested no effects of the interventions. As Rifkin (14) suggests, and as underscored by our research (3, 6), the biomedical framework can fall short in understanding complex life situations. The richer evaluation provided by MICG helps us to disentangle how community participation contributed to other nonphysical indicators of child growth. Hence, programs that fail in 1 dimension may still be relevant in other dimensions of child growth―metrics matter (31), and we need new metrics such as MICG to help us understand the root causes of inequalities in the effects of intervention programs.
In the case of the cohort of children from Vietnam, inequalities in nonphysical dimensions of child growth were found for children living in rural areas, but not for female children. These findings suggest that urban children benefited from community participation more than children living in rural areas, despite the fact that community engagement should give a voice to disadvantaged groups with poorer health and nutrition conditions (9). Ved (32) argues that, in rural areas, a better alignment of health, sanitation, and nutrition committees between village and communes can improve the participation of marginalized populations. Further research in rural areas is needed to establish how participation in community interventions could be leveraged to produce greater benefits for child growth and consequently improve the targeting of the beneficiaries of interventions.
There are some important limitations to this study that need to be considered when interpreting the findings. First, the observational study design does not allow us to demonstrate causal associations. However, our findings are grounded in the complexity of a real-life situation and include contextual factors related to the situation of children, parents, and communities, which are relevant when evaluating the impact of community participation according to Rifkin (14). Second, the YL data were not built to be a representative sample of Vietnam; accordingly, the conclusions are only valid for the sample of children analyzed and cannot be generalized at the country level, as the data do not have expansion factors. Despite these limitations, the MICG can be applied for a ranking of countries, as it is done, for example, with the Human Development Index (33), if representative and contextually rich databases are available. Datasets like the Multiple Indicator Cluster Surveys (MICS) and the Demographic and Health Surveys (DHS) increase representability at the population level and facilitate cross-country comparisons; however, these datasets are focused on the medical perspective of child growth based on anthropometry and are not rich enough―in terms of including social and psychological indicators―to allow a calculation of an MICG such as the one presented in this study. Our results suggest that, in order to further investigate the impacts of community participation, datasets have to be rich enough to build not only mono-dimensional anthropometric indicators but also multidimensional outcomes, as multidimensional outcomes grasp the situational aspects of community participation during the different stages of nutrition-sensitive interventions.
Supplementary Material
ACKNOWLEDGEMENTS
The authors acknowledge the contributions of Pieter Boele Van Hensbroek, Victor O Owino, and Emorn Udomkesmalee as members of the working group “Towards a Multi-dimensional Index for Child Growth.” The authors’ responsibilities were as follows—RGM: designed the research and analyzed the data; RGM, PA, and HH: identified relevant variables for the analysis; HH and RGM: wrote the manuscript; JW, GB, GP, and AD: provided feedback to improve the analysis and the draft versions of the manuscript; HH: had primary responsibility for final content; and all authors: read and approved the final manuscript.
Notes
Supported by the Population Research Centre of the University of Groningen. The research was further supported by the International Union of Nutritional Sciences through the Task Force “Towards a Multi-dimensional Index to Child Growth.”
Author disclosures: The authors report no conflicts of interest. The funders played no role in the design, implementation, analysis, and interpretation of the data, which were the responsibility of the authors only.
The data used in this publication come from Young Lives, a 20-y study of childhood poverty and transitions to adulthood in Ethiopia, India, Peru, and Vietnam (www.younglives.org.uk). Young Lives is funded by UK aid from the Foreign, Commonwealth & Development Office (FCDO) and a number of additional funders. The formal approval of the ethical process of Young Lives round 2 (2006) was obtained from the Ethics Committee of the Social Science Division, University of Oxford, in 2006, using the guidelines of the University of Oxford's Department of International Development, the Association of Social Anthropologists of the Commonwealth, and Save the Children Child Protection Policy. Researchers of Young Lives obtained the informed consent from parents and children in relation to how the data will be used. The Research Ethics Committee of the Faculty of Spatial Sciences at the University of Groningen provided a waiver for the secondary data analysis of the Young Lives Survey in this article, through the ethical clearance no. 202202. The views expressed here are those of the authors; they are not necessarily those of Young Lives, the University of Oxford, FCDO, or other funders of the Young Lives Survey.
Supplemental Tables 1 and 2 and Supplemental Material are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/cdn.
Abbreviations used: AF, Alkire-Foster; MICA, Multidimensional Index of Child Advantage; MICG, Multidimensional Index of Child Growth; OLS, ordinary least squares; WASH, water, sanitation, and hygiene; YL, Young Lives.
Contributor Information
Rolando Gonzales Martinez, Population Research Centre, Faculty of Spatial Sciences, University of Groningen, Groningen, The Netherlands.
Jonathan Wells, Institute of Child Health Great Ormond Street, University College London, London, United Kingdom.
Paul Anand, Faculty of Art and Social Sciences, Open University, London, United Kingdom.
Gretel Pelto, Division of Nutritional Sciences, Cornell University, Ithaca, NY, USA.
Muhammad Ali Dhansay, South African Medical Research Council and Stellenbosch University, Cape Town, South Africa.
Hinke Haisma, Email: h.h.haisma@rug.nl, Population Research Centre, Faculty of Spatial Sciences, University of Groningen, Groningen, The Netherlands.
Data Availability
Data described in the manuscript, code book, and analytic code will be made available upon request.
References
- 1. UNICEF . Strategy for improved nutrition of children and women in developing countries. New York (NY): United Nations Children's Fund; 1990. [DOI] [PubMed] [Google Scholar]
- 2. Clark H, Coll-Seck AM, Banerjee A, Peterson S, Dalglish SL, Ameratunga S, Balabanova D, Bhan MK, Bhutta ZA, Borrazzo Jet al. . A future for the world's children? A WHO–UNICEF–Lancet Commission. Lancet. 2020;395(10224):605–58. [DOI] [PubMed] [Google Scholar]
- 3. Haisma H, Pelto G, Venkatapuram S, Yousefzadeh S, Kramer L, Anand P; Members of the Working Group “Towards a Multi-dimensional Index of Child Growth” . Towards a multi-dimensional index of child growth to combat the double burden of malnutrition. Ann Nutr Metab. 2019;75(2):123–6. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization; United Nations Children's Fund; World Bank Group . Nurturing care for early childhood development: a framework for helping children survive and thrive to transform health and human potential. Geneva (Switzerland): World Health Organization; 2018. [Google Scholar]
- 5. Black MM, Lutter CK, Trude ACB. All children surviving and thriving: re-envisioning UNICEF's conceptual framework of malnutrition. Lancet Glob Health. 2020;8(6):e766–7. [DOI] [PubMed] [Google Scholar]
- 6. Haisma H, Yousefzadeh S, Boele Van Hensbroek P. Towards a capability approach to child growth: a theoretical framework. Matern Child Nutr. 2018;14(2):e12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yousefzadeh S, Biggeri M, Arciprete C, Haisma H. A capability approach to child growth. Child Indicators Res. 2019;12(2):711–31. [Google Scholar]
- 8. Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–23. [DOI] [PubMed] [Google Scholar]
- 9. O'Mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta-analysis. BMC Public Health. 2015;15(1):129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Madon S, Malecela MN, Mashoto K, Donohue R, Mubyazi G, Michael E. The role of community participation for sustainable integrated neglected tropical diseases and water, sanitation and hygiene intervention programs: a pilot project in Tanzania. Soc Sci Med. 2018;202:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haldane V, Chuah FLH, Srivastava A, Singh SR, Koh GCH, Seng CK, Legido-Quigley H. Community participation in health services development, implementation, and evaluation: a systematic review of empowerment, health, community, and process outcomes. PLoS One. 2019;14(5):e0216112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rifkin SB. Examining the links between community participation and health outcomes: a review of the literature. Health Policy Plan. 2014;29(Suppl 2):ii98–ii106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Perry H, Zulliger RH. How effective are community health workers? An overview of current evidence with recommendations for strengthening community health worker programs to accelerate progress in achieving the health-related Millennium Development Goals. Baltimore (MD): Johns Hopkins Bloomberg School of Public Health; 2012. [Google Scholar]
- 14. Rifkin SB. Lessons from community participation in health programmes: a review of the post Alma-Ata experience. Int Health. 2009;1(1):31–6. [DOI] [PubMed] [Google Scholar]
- 15. Luisi D, Hämel K. Community participation and empowerment in primary health care in Emilia-Romagna: a document analysis study. Health Policy. 2021;125(2):177–84. [DOI] [PubMed] [Google Scholar]
- 16. Chakraborty B, Yousefzadeh S, Darak S, Haisma H. “We struggle with the earth everyday”: parents’ perspectives on the capabilities for healthy child growth in Haor region of Bangladesh. BMC Public Health. 2020;20(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Clifford Simplican S. Theorising community participation: successful concept or empty buzzword?. Res Pract Intellect Dev Disabilities. 2019;6(2):116–24. [Google Scholar]
- 18. Kumar S. Community participation in palliative care: reflections from the ground. Progress Palliative Care. 2020;28(2):83–8. [Google Scholar]
- 19. Boyden J. Young Lives: an international study of childhood poverty: round 2, 2006. [data collection]. 3rd ed. Colchester (UK): UK Data Service; 2018. [Google Scholar]
- 20. George AS, Mehra V, Scott K, Sriram V. Community participation in health systems research: a systematic review assessing the state of research, the nature of interventions involved and the features of engagement with communities. PLoS One. 2015;10(10):e0141091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Arnstein SR. A ladder of citizen participation. J Am Inst Plann. 1969;35(4):216–24. [Google Scholar]
- 22. Cornwall A. Unpacking ‘participation’: models, meanings and practices. Community Dev J. 2008;43(3):269–83. [Google Scholar]
- 23. Pretty JN. Participatory learning for sustainable agriculture. World Dev. 1995;23(8):1247–63. [Google Scholar]
- 24. Prado EL, Larson LM, Cox K, Bettencourt K, Kubes JN, Shankar AH. Do effects of early life interventions on linear growth correspond to effects on neurobehavioural development? A systematic review and meta-analysis. Lancet Glob Health. 2019;7(10):e1398–413. [DOI] [PubMed] [Google Scholar]
- 25. Richter L, Black M, Britto P, Daelmans B, Desmond C, Devercelli A, Dua T, Fink G, Heymann J, Lombardi Jet al. . Early childhood development: an imperative for action and measurement at scale. BMJ Glob Health. 2019;4(Suppl 4):e001302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Glewwe P, Chen Q, Katare B. What determines learning among Kinh and ethnic minority students in Vietnam? An analysis of the round 2 Young Lives Data. Asia & The Pacific Policy Studies. 2015;2(3): 494–516. [Google Scholar]
- 27. Biggeri M, Libanora R, Mariani S, Menchini L. Children conceptualizing their capabilities: results of a survey conducted during the first children's world congress on child labour. J Hum Dev. 2006;7(1):59–83. [Google Scholar]
- 28. Alkire S, Roche JM, Ballon P, Foster J, Santos ME, Seth S. Multidimensional poverty measurement and analysis. Oxford (UK): Oxford University Press; 2015. [Google Scholar]
- 29. Koenker R, Bassett G Jr. Regression quantiles. Econometrica. 1978;46(1):33–50. [Google Scholar]
- 30. Koenker R, Hallock KF. Quantile regression. J Econ Perspect. 2001;15(4):143–56. [Google Scholar]
- 31. Stiglitz JE. Measuring what counts: the global movement for well-being. New York (NY): The New Press; 2019. [Google Scholar]
- 32. Ved R, Sheikh K, George AS, Raman VR. Village health sanitation and nutrition committees: reflections on strengthening community health governance at scale in India. BMJ Glob Health. 2018;3(Suppl 3):e000681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McGillivray M, White H. Measuring development? The UNDP's Human Development Index. J Int Dev. 1993;5(2):183–92. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, code book, and analytic code will be made available upon request.