Abstract
Radiotherapy is an essential and effective treatment modality for cancer. Excessive levels of reactive oxygen species (ROS) induced by ionizing radiation disrupt the redox homeostasis and lead to oxidative stress that may result in cell death. However, the tumor cell microenvironment is dynamic and responds to radiotherapy by activating numerous cellular signaling pathways. By scavenging excess ROS, the activity levels of the endogenous antioxidant enzymes result in radioresistance and worsen the clinical outcomes. To assess the full potential of radiotherapy, it is essential to explore the underlying mechanisms of oxidative stress in radiotherapy for potential target identification. The present review article summarized recent data demonstrating nuclear factor-erythroid factor 2-related factor 2 (Nrf2) as a powerful transcription factor and one of the major cellular defense mechanisms that protect against oxidative stress in response to radiotherapy; the glutathione (GSH) and thioredoxin (Trx) systems complement each other and are effective antioxidant mechanisms associated with the protection of cancer cells from radiation damage. In addition, it is suggested that dual targeting to inhibit GSH and Trx enzymes may be a potential strategy for the development of radiosensitive and radioprotective drugs.
Keywords: oxidative stress, radiotherapy, radiosensitivity, glutathione metabolism, thioredoxin
1. Introduction
Oxidative stress generally originates from toxic by-products resulting from the imbalance between radicals and antioxidants, which primarily arises from the accumulation of reactive oxygen species (ROS) (1,2). The redox balance is maintained by complex cellular biochemical and genetic mechanisms. Redox imbalance may have profound effects on physiological and pathophysiological mechanisms (3,4). ROS disrupt cellular processes by non-specific modifications on critical amino acid residues in proteins (resulting in protein oxidation), fatty acids in lipids (to cause lipid peroxidation) and nucleic acids (inducing DNA damage and strand breaks) (5-8). ROS mainly includes the superoxide anion (O2−), hydrogen peroxide (H2O2), hydroxyl radical (·OH) and singlet oxygen (1O2) (9). Among these, ·OH is the most reactive ROS and is able to react with almost any tissue directly, thereby causing more effective cellular damage than any other ROS (10). Under pathological conditions, tumor cells produce elevated levels of ROS compared with those of normal cells (11-13). Tumor cells always adjust their metabolism to increase intracellular ROS levels and maintain their survival and proliferation during tumorigenesis (14,15). However, ROS have a dual role in cancer development. ROS may lead to epigenetic alterations that promote the acceleration of tumor progression. By contrast, higher levels of ROS promote genome instability, inducing activation of cancer cell death or inhibiting resistance to anticancer treatment (16-19).
Theoretically, radiotherapy is able to more precisely target the tumor. The relative toxicity caused by radiation to the surrounding normal tissues is limited (20). However, several antioxidant transcription factors may be activated in response to radiotherapy, resulting in the inhibition of ROS-dependent damaging effects induced by radiation and in the reduced effectiveness of the treatment (21). In addition, the source of ROS is considered to be a double-edged sword, which has a key initiator role in ionizing radiation (IR)-associated normal tissue injury (22). The radioresistance and tumor recurrence following radiotherapy are significant problems to overcome, which may contribute to treatment failure and tumor relapse. Specific modifications in the production of ROS and the concentrations of antioxidants have pivotal roles in cancer radiotherapy (12,23,24). Current research demonstrates that targeting oxidative stress may benefit patients with radiation resistance during radiotherapy (25). Therefore, the identification of the mechanisms of oxidative stress has been the focus of various studies. In the present review article, the mechanisms underlying the regulation of oxidative stress induced by radiotherapy were summarized and the benefits of using radio-protectors or radio-sensitizers were discussed.
2. Molecular mechanisms and pathways of oxidative stress
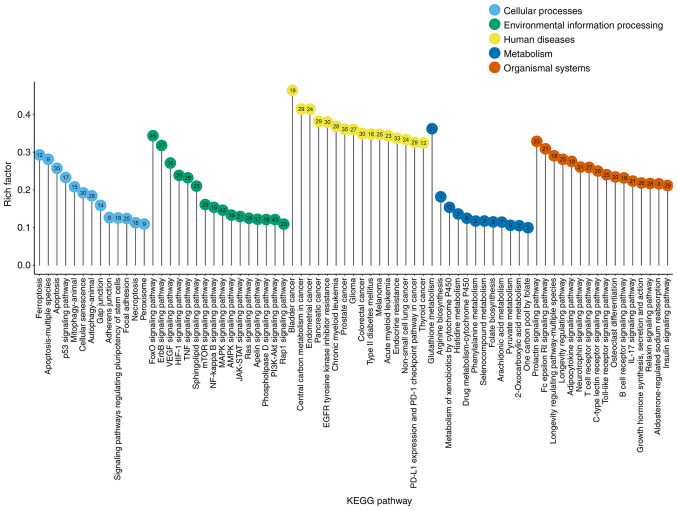
The current literature was reviewed and oxidative stress-related genes were extracted from pertinent papers (Table SI). Finally, 198 gene symbols were confirmed with the HUGO Gene Nomenclature Committee Multi-symbol checker tool (https://www.genenames.org/tools/multi-symbol-checker). Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis by R software was used to identify the signaling pathways that were mainly enriched by oxidative stress-related genes. Fig. 1 indicates the significant pathways identified (rich factor >0.1), which were sub-grouped by the KEGG main class. The top significant pathways with roles in cellular processes were as follows: Ferroptosis, apoptosis, p53 signaling pathway, mitophagy, cellular senescence pathway and autophagy. In addition, the forkhead box protein O (FoxO), Erb-b receptor tyrosine kinase (ErbB), vascular endothelial growth factor receptor (VEGF), hypoxia inducible factor-1 (HIF-1), TNF, mTOR, NF-κB, MAPK, 5′AMP-activated protein kinase, Janus kinase/signal transducer and activator of transcription, Ras and PI3K/AKT signaling pathways were the most represented pathways according to environmental information processing. Glutathione (GSH) metabolism was dominant in the metabolism category.
Figure 1.
KEGG pathway enrichment analysis of oxidative stress-related genes. The rich factor resembles the ratio of the number of target genes annotated in this pathway. KEGG, Kyoto Encyclopedia of Genes and Genomes.
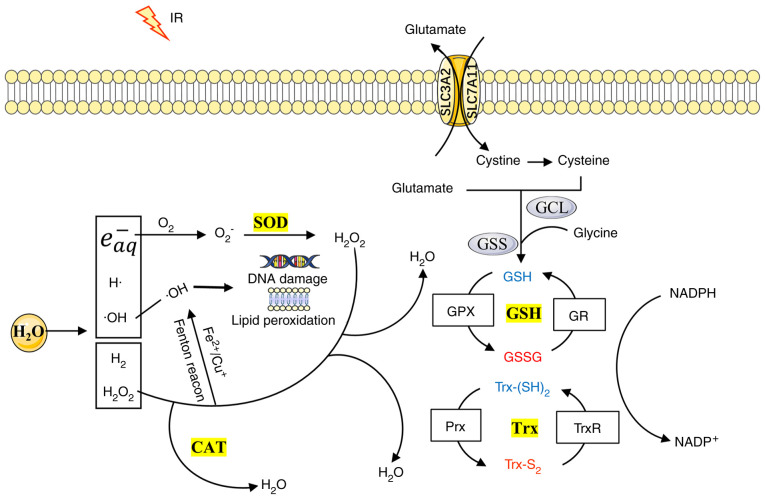
As protectors of cancer cells from the effects of ROS, the superoxide dismutase (SOD), GSH reductase (GPX), thioredoxin (Trx) reductase (TrxR) and catalase (CAT) antioxidant enzymes were investigated, which have a major role in ROS scavenging (26-28). Fig. 2 indicates the response of the antioxidant system to radiotherapy. SODs may function in different cellular compartments to rapidly catalyze O2− into H2O2 and O2. The other antioxidant enzymes, including CAT, GPX and TrxR, convert H2O2 into water (29). In mammalian cells, the following three types of SOD exist: A copper and zinc SOD termed CuZn-SOD or SOD1, which is mainly found in the cytosol, a manganese SOD, termed Mn-SOD or SOD2, which is found in the mitochondrial matrix, and an extracellular SOD termed EC-SOD or SOD3 (30). CAT is located primarily in the peroxisomes and is a widespread and highly efficient antioxidant enzyme present in almost all living organisms, which uses either iron or manganese as a cofactor (31). The GSH system, which is composed of glutathione reductase (GR), GSH and NADPH, is the most abundant cellular thiol antioxidant system and is regulated by its biosynthesis, redox state and cellular export (32). Its redox cycle is regulated by GPX and GR (33). At least eight isoforms of GPX enzymes (GPX1-GPX8) have been found in mammals, of which GPX4 is the only one that is able to reduce phospholipid hydroperoxides (34,35). The solute carrier family 7 member 11 (SLC7A11) has a pivotal role in intracellular cysteine balance and GSH biosynthesis (36). Similar to the GSH system, Trx is another powerful cellular disulfide reductase involved in the control of cellular redox homeostasis, which comprises TrxR, Trx and NADPH (37). The mammalian Trx consists of the following three isoforms: Trx1 in the cytosol, Trx2 in the mitochondria and a testis-specific Trx. The following three types of TrxRs have been characterized: Cytosolic TrxR1, mitochondrial TrxR2 and testis-specific TrxR3 (38). Trx donates electrons to peroxyredoxin (Prx) to remove H2O2. Typically, the Trx and GSH systems are functioning in parallel, and several types of reciprocal crosstalk have been identified between these two systems, indicating that the components of one system may be a backup to those of the other (38).
Figure 2.
Antioxidant system response to radiotherapy. H2O2 is generated through water radiolysis, which may be transformed into the highly reactive OH through the Fenton reaction. SOD is an important metalloenzyme that catalyzes O2− to molecular oxygen O2 and H2O2. H2O2 may be transformed to H2O by the enzymes CAT, GPX or TrxR. CAT is a common antioxidant enzyme from the family of oxyreductases. GSH and Trx are two thiol-dependent redox systems acting in concert, which have been identified as powerful antioxidant mechanisms. These enzymes may effectively scavenge H2O2. The yellow color corresponds to the four main antioxidant enzyme systems. Oxidized and reduced states are indicated by red or blue color, respectively. H2O2, hydrogen peroxide;·OH, hydroxyl radical; SOD, superoxide dismutase; CAT, catalase; GPX, glutathione peroxidase; Trx, thioredoxin; TrxR, Trx reductase; GSH, glutathione; O2, molecular oxygen; O −2, superoxide anion; GCL, glutamate-cysteine ligase; GSS, GSH synthetase; GR, GSH reductase; Prx, peroxiredoxin; IR, ionizing radiation; SLC3A2, solute carrier family 3 member 2; e−aq, hydrated electrons.
3. Functional characterization of oxidative stress in radiotherapy
Radiotherapy has been recognized as one of the mainstay regimens for various types of cancer treatment (39,40). The changes in the biological effectiveness of the targeted tissues caused by IR are related to the energy deposits observed in the encountered molecules of specific cell signaling pathways (41,42). Oxidative stress has a powerful function in cancer progression and in the response to radiotherapy. IR-induced cell damage may originate from direct or indirect actions. Direct damage to the cell mainly relies on the radiation that affects the DNA molecules and results in the formation of either single- or double-strand breaks (43). By contrast, water radiolysis rapidly produces ROS; the elevated intracellular levels of ROS cause oxidative stress, which results in indirect damage. Approximately 80% of the cellular content is composed of water, which has a leading role in IR-induced biological effects (42,44).
The radiolysis of water leads to the formation of free radicals, such as hydrated electrons (e−aq), ·OH, and H·, and certain molecular products (H2, H2 O2) (45,46). E−aq are able to indirectly form O−2 with molecular oxygen (47). In addition, H2O2 and O2− may be transformed into the highly reactive ·OH via the Fenton or the Haber-Weiss reactions in the presence of transition redox metals, such as iron or copper (48). IR generates ROS that readily interact with cellular membrane lipids, proteins and nucleic acids, resulting in the alteration of membrane permeability, proteolytic degradation, DNA damage and genomic instability. This eventually induces radiation damage and tumor cell death (49). Consequently, radiotherapy may efficiently induce massive cell death by increasing intracellular ROS levels. Furthermore, the radiation damage also affects adjacent normal cells via the bystander effect (50-52). Radiotherapy used in cancer treatment may cause problems in the heart, as well as in the hematopoietic, intestinal and nervous systems (53,54).
4. Activation of oxidative stress pathways by radiotherapy
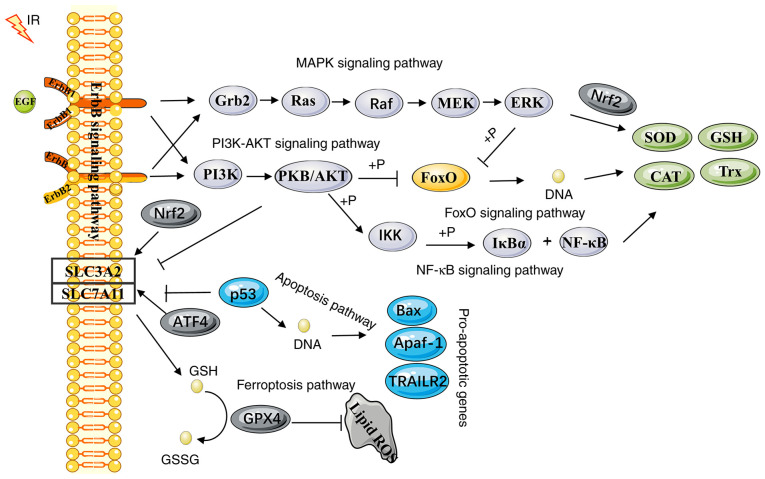
The results of the KEGG pathway analysis revealed that the dominant pathways that regulate oxidative stress were the ferroptotic (Fig. S1), apoptotic (Fig. S2), FoxO (Fig. S3) and ErbB (Fig. S4) signaling pathways. All of these pathways may be activated by radiotherapy (55-58). To respond to IR-induced oxidative stress and the change in redox environmental conditions, multiple signal transduction pathways crosstalk with each other (Fig. 3). Depending on the IR dose, the dose rate, the quality and the time period of treatment, these mechanisms may affect the antioxidant or pro-oxidant effects in a different manner. To clarify the crosstalk between oxidative stress and the intracellular IR response, the corresponding molecular mechanisms were investigated. These molecular events were involved in the relationship between the major pathways linked to oxidative stress and the response of the antioxidant defense pathways to radiotherapy.
Figure 3.
Activation of oxidative stress-related pathways by radiotherapy. In response to IR, activated ErbB1 and ErbB2 (via interaction with one of the ligand-bound partners) induce the subsequent activation of downstream signaling pathways that include MAPK, PI3K/AKT and FoxO. The activation of the MAPK and PI3K/AKT signaling pathways increases the expression levels of Nrf2, thereby activating several antioxidant systems in response to oxidative stress. The FoxO-target genes include various genes encoding antioxidant proteins, which have a complex role in the induction of oxidative stress. It may not only activate the antioxidant system to promote tumor cell survival, but also promote apoptosis. NF-κB is another key pathway regulating the fine balance of the cellular redox status. The binding of the NF-κB proteins to DNA regulates the transcription of various potential antioxidant targets. In addition, IR activates the SLC7A11/GPX4 axis, which is considered to be one of the most important means of regulating oxidative stress via the ferroptotic pathway. IR, ionizing radiation; ErbB, Erb-b receptor tyrosine kinase; FoxO, forkhead box protein O; SLC7A11, solute carrier family 7 member 11; GPX4, glutathione reductase 4; SOD, superoxide dismutase; CAT, catalase; Trx, thioredoxin; Nrf2, nuclear factor-erythroid factor 2-related factor 2.
Ferroptotic pathway
Ferroptosis is a recently described form of regulated cell death, which differs from apoptosis and necrosis and is characterized by the accumulation of iron-dependent lipid peroxidation (59,60). The critical role of ferroptosis in radiotherapy has been established in recent studies (55). The cell membrane is the major target of IR-induced ROS, since membrane lipids are easily peroxidized, resulting in structural and functional damage (61). Glutathione metabolism is one of the main mechanisms governing ferroptosis. GPX4 and SLC7A11 are key regulators of glutathione metabolism, which have a crucial role in limiting lipid peroxidation (62).
Radiotherapy results in downregulation of SLC7A11 expression and induces lipid oxidative damage to promote tumor-associated ferroptosis (63). IR may also cause significant downregulation in the expression levels of GPX4 (64). However, in certain cases, IR may induce SLC7A11 or GPX4 expression as an adaptive response to protect cells from ferroptosis (65). In addition, p53 and nuclear factor-erythroid factor 2-related factor 2 (Nrf2) may be rapidly activated by IR, which has an important role in the regulation of ferroptosis. p53 is able to inhibit the cellular uptake of cystine by transcriptionally restricting SLC7A11 expression to reduce antioxidant capacity, resulting in ferroptosis (66,67). The transcription factor Nrf2 is considered to have a central role in the upregulation of the expression levels of specific anti-ferroptotic defense biomarkers. Nrf2 promotes cell survival in irradiated cells via activation of specific downstream regulator target genes, including SLC7A11. These genes aim to prevent oxidative damage (68-71). In addition, the Trx system may also protect cells from lipid peroxidation (72). Nrf2 is able to bind to the TrxR1 and Trx1 promoter antioxidant responsive element (ARE) and improve its activity (73). In addition, it has been indicated that Nrf2 is able to bind to the ARE sequence of various other antioxidant proteins, namely GPX2, Prx1, Prx6 and glutamate-cysteine ligase catalytic subunit (74-77).
Apoptotic pathway
Apoptosis is a form of regulated cell death. Oxidative stress is considered to be a strong inducer of apoptosis (78). Apoptosis is triggered by the following two major signaling pathways: The extrinsic and the intrinsic pathway. These pathways are independent but interact with each other (79). It is suggested that both the intrinsic pathway (activated by mitochondrial outer membrane permeabilization) and the extrinsic pathway (initiated by plasma membrane receptors) may be activated following IR treatment (80).
However, studies have demonstrated that radiotherapy primarily acts through the intrinsic pathway (80-82). The signatures of several intrinsic pathway proteins are associated with radiosensitivity, such as p53, Bcl-2 and Bax (83,84). In response to IR-induced oxidative stress, p53 has an essential role in the regulation of the redox state (85,86). The activation of p53 is largely dependent on the ATM kinase that phosphorylates p53 shortly after IR (87). A previous research study suggested that p53 regulated radiotherapy efficacy by targeting Bcl-2 proteins to release Bax, which in turn promoted apoptosis or inactivated invasiveness (88). In addition, p53 was also able to activate the expression levels of SOD2 and GPX1 by binding to their promoters, which stimulates an antioxidant response (89). It is known that TNFα is a potent pro-apoptotic molecule, which promotes the expression of several inflammatory factors. However, TNFα also has a role in cell survival mechanisms (90-92). TNFα is able to increase the transcription of GPX4 (93). Activation of the transcription factor NF-κB has a central role in regulating apoptosis (94). In addition to its apoptotic activity, NF-κB induces the expression of specific genes, which may attenuate ROS production and promote survival (95). For instance, the NF-κB pathway may lead to SOD2 gene activation (96,97). Experimental evidence also suggests that GPX4 is transcriptionally regulated by NF-κB (93).
FoxO signaling pathway
The FoxO family includes several pivotal transcription factors activated in response to oxidative stress, such as FoxO1, FoxO3a, FoxO4 and FoxO6. The majority of previously published studies have focused on the first three members (98,99). The interaction of FoxO and p53 proteins may coordinate tumor suppression via the regulation of various common target genes, such as p21, growth arrest and DNA damage, protein phosphatase 1D and sestrin 1 (57). A previous study revealed that JNK is able to phosphorylate FoxO1, FoxO3a, and FoxO4 to facilitate nuclear entry of FoxO, leading to the upregulation of the expression levels of antioxidant genes (98).
FoxO3a is a crucial effector of IR-induced apoptosis in response to genotoxic stress (100). FOXO3a promotes the cell survival pathway by directly binding to the SOD2 promoter, causing increased expression of SOD2. The activation of the latter protects the cells from oxidative stress-mediated injury (101). By contrast, FoxO3a may effectively increase cellular antioxidant capacity by enhancing the levels of CAT and Prx3 to protect against oxidative stress (102,103). However, the regulation of oxidative stress by FoxO3a is complex. A previous study indicated that depletion of FoxO3a expression profoundly reduced kelch-like ECH associated protein 1 protein levels, thereby activating Nrf2 signaling (104). It was also indicated that FoxO4 was able to bind to the SOD2 promoter to upregulate SOD2 expression (105). FoxO1 was able to promote activating transcription factor 4 expression, which acts as an important transcription factor for SLC7A11, leading to GSH synthesis (106,107).
ErbB signaling pathway
The ErbB family of proteins is also termed the epithelial growth factor receptor (EGFR) family and consists of the four following members: EGFR (ErbB1 or Her1), ErbB2 or Her2, ErbB3 or Her3, and ErbB4 or Her4 (108). In response to IR, the ErbB receptor tyrosine kinase family is rapidly activated, leading to subsequent activation of multiple downstream pathways (58,109). The activated downstream pathways mainly include PI3K/AKT, MAPK/ERK1/2, Ras and the mTOR signaling pathways, leading to alteration in cell proliferation, apoptosis, autophagy, migration and invasion (110-112). The EGFR transactivation caused by ROS results in the protection of the cells against oxidative stress with extensive crosstalk occurring among these pathways (113).
ErbB receptors, notably EGFR and ErbB2, are closely associated with the induction of oxidative stress (114). EGFR may stimulate HIF signaling activity to improve cellular survival (115). A previous research study has identified a functional transcription start site for GPX3, which is used for binding with HIF-1 (116). Several mechanisms have also been reported to explain the increase in Nrf2 transcription by the PI3K/AKT and Kras signaling pathways (117). The study also indicated that ErbB2 activated Nrf2 transcriptional activity through direct protein-protein interactions, which caused the induction of the expression of antioxidant and detoxification proteins (118). Moreover, Sakurai et al also reported that overexpression of Nrf2 augmented the TrxR1 promoter activity (119). In addition, it has been demonstrated that the restriction of ErbB2 receptor contributes to cell death through the production of ROS (120).
It is important to note that IR-induced ROS leads to cellular oxidizing stress that has an important role in radiotherapy. Several proteins are related to the regulation of the antioxidant systems. These proteins control the expression of various antioxidant genes and may defend against the induction of oxidative stress by IR (Table I). Consequently, the effects of various types of anticancer treatment may be diminished.
Table I.
Regulation of radiotherapy by targeting antioxidant enzyme systems.
| Gene name | Targeting antioxidant system | Mechanism of effect | (Refs.) |
|---|---|---|---|
| SLC7A11 | GSH system | Contributes to GSH synthesis | (65) |
| GPX4 | GSH system | Converts GSH into oxidized glutathione | (65) |
| Nrf2 | Trx system | Targets Trxr1 activity | (73,119) |
| Nrf2 | Trx system | Targets Trx1 activity | (73) |
| Nrf2 | Trx system | Targets Prx1 activity | (75) |
| Nrf2 | GSH system | Targets Prx6 activity | (76) |
| Nrf2 | GSH system | Targets GPX2 activity | (74) |
| Nrf2 | GSH system | Targets GCLC activity | (77) |
| Nrf2 | GSH system | Targets SLC7A11 activity | (71) |
| HIF-1 | GSH system | Targets GPX3 activity | (116) |
| NF-κB | GSH system | Targets GPX4 activity | (93) |
| NF-κB | SOD system | Targets SOD2 activity | (96,97) |
| TNFα | GSH system | Targets GPX4 activity | (93) |
| p53 | GSH system | Targets GPX1 activity | (89) |
| p53 | SOD system | Targets SOD2 activity | (89) |
| FoxO3a | SOD system | Targets SOD2 activity | (101,103) |
| FoxO4 | SOD system | Targets SOD2 activity | (105) |
| FoxO3a | Trx system | Targets Prx3 activity | (102,103) |
| FoxO3a | CAT system | Targets CAT activity | (102,103) |
GSH, glutathione; HIF, hypoxia-inducible factor; ErbB, Erb-b receptor tyrosine kinase; FoxO, forkhead box protein O; SLC7A11, solute carrier family 7 member 11; GPX4, glutathione reductase 4; SOD, superoxide dismutase; CAT, catalase; Trx, thioredoxin; Trxr, Trx reductase; Nrf2, nuclear factor-erythroid factor 2-related factor 2; Prx, peroxiredoxin.
5. Oxidative stress acts as a mediator of radiosensitivity
IR-induced oxidative stress is not only involved in cancer cell death but also in the activation of the damage-repair and survival signaling to relieve the induction of oxidative damage. These activations are responsible for radioresistance in cancer (85). The inhibition of oxidative stress appears to be the main mechanism, established by the intracellular antioxidant system, responsible for tumor radioresistance (121). As presented in Table II, increasing evidence has demonstrated that antioxidant system inhibitors promote radiation sensitization.
Table II.
Summary of targeting antioxidant system agents as radiosensitizers.
| Name | Mechanism of effect | Types of cancer | Stages of development | (Refs.) |
|---|---|---|---|---|
| Sulfasalazine | Inhibits SLC7A11 | Lung cancer | In vivo (A549, patient-derived xenograft) | (65) |
| RSL3 | Inhibits GPX4 | Lung cancer | In vitro (A549) | (65) |
| Auranofin | Inhibits Trxr | Liver cancer, breast cancer | In vitro (Huh7, HepG2), In vivo (4T1, EMT6) | (72,130) |
| Platinum complexes | Inhibits Trxr | Melanoma | In vitro (A375) | (20) |
| Selenadiazole | Inhibits Trxr | Melanoma, cervical cancer | In vitro (A375, HeLa) | (131,132) |
| ML385 | Inhibits Nrf2 | Breast cancer | In vitro (SUM149, SUM159) | (124) |
| IM3829 | Inhibits Nrf2 | Lung cancer | In vitro (H1299, A549) | (126) |
| Brusatol | Inhibits Nrf2 | Lung cancer | In vitro (A549) | (125) |
| Halofuginone | Inhibits Nrf2 | Lung cancer | In vitro (A549), In vivo (A549) | (127) |
| Butyrate | Activates FoxO3a | Colorectal cancer | In vitro (primary cancer) | (128) |
| Resveratrol | Activates FoxO3a | Cervical cancer | In vitro (HeLa) | (129) |
| Lapatinib | Inhibits EGFR or ErbB2 | Pancreas adenocarcinoma | In vivo (Capan-2) | (134) |
| Icotinib | Inhibits EGFR | Lung cancer | In vivo (H1650) | (135) |
| APG-115 | Inhibits MDM2-p53 | Gastric cancer | In vivo (MKN45) | (136) |
SLC7A11, solute carrier family 7 member 11; ErbB, Erb-b receptor tyrosine kinase; FoxO, forkhead box protein O; GPX4, glutathione reductase 4; Trxr, thioredoxin reductase; Nrf2, nuclear factor-erythroid factor 2-related factor 2; EGFR, epithelial growth factor receptor.
Previous studies have suggested that Nrf2 is a key transcription factor that regulates the expression of various antioxidant proteins (122,123). Nrf2 inhibitors may be an effective approach against radioresistance. ML385 is a specific Nrf2 inhibitor that binds this transcription factor and blocks the downstream target gene expression, leading to the sensitization of breast cancer stem cells to IR (124). Brusatol selectively reduces the protein levels of Nrf2 by enhancing ubiquitination and degradation of Nrf2 and enhances the radiosensitivity of tumors (125). In addition, IM3829 markedly enhances the radiosensitivity of human lung cancer cells by inhibiting the mRNA and protein expression levels of Nrf2 (126). Halofuginone, a less-toxic febrifugine derivative, is considered to be particularly promising for cancer treatment. This compound rapidly suppresses the accumulation of the Nrf2 protein in therapy-resistant cancer cells (127). Although FoxO3a may be activated by IR, leading to an increase in the expression levels of antioxidant markers, FoxO3a-induced apoptosis has received increasing attention in response to radiation. Butyrate (128) and resveratrol (129) have demonstrated the potential to overcome the radioresistance effect by enhancing the activation of FoxO3a transcription. During radioresistance, ferroptosis inducers also have a key role. A previous study revealed that sulfasalazine (inhibitor of SLC7A11) and RSL3 (inhibitor of GPX4) exert significant radiosensitizing effects in vitro (65). TrxR inhibitors enhance radiosensitivity by triggering excessive oxidative stress. Specific examples of these compounds include auranofin (72,130), platinum complexes (20) and selenadiazole (131,132). Since Trx and GSH perform crosstalk with each other, their dual inhibition has synergetic antitumor effects in cancer therapy by inducing ROS production (133). EGFR or ErbB2 inhibitors (e.g. lapatinib) led to increased radiosensitivity in wild-type K-ras pancreatic cancer (134). The EGFR inhibitor icotinib has been indicated to increase radiosensitivity by enhancing apoptosis and downregulating the MAPK-AKT and ERK signaling pathways (135). In addition, combination treatment with radiotherapy and an MDM2-p53 inhibitor (APG-115) made tumors overcome radioresistance and enhance the antitumor effects (136).
6. Antioxidants act as radioprotective agents
Typically, IR causes the accumulation of endogenous ROS in irradiated cells, as a consequence of the activation of intracellular signaling pathways (137-139). These effects result in an ongoing inflammatory cascade, which may contribute to continuous damage that surpasses the initial insult and responses noted in non-irradiated cells, which are neighboring to irradiated cells (IR-induced bystander effects) (140). The side effects of IR mostly result from the increased oxidative stress and inflammation generated during radiotherapy (141). Therefore, it is of particular importance that the induction of tumor cell death during radiotherapy occurs without producing extensive damage to surrounding healthy tissues (142).
To reduce these adverse effects, radioprotectors are employed to protect against IR damage to healthy tissues. These compounds act by different mechanisms, which are mainly associated with the modulation of the antioxidant defense (49). p53 inhibition may reduce damage to normal tissues and this strategy has been experimentally tested in mice by using a small-molecule inhibitor of p53 (pifithrin-α) (143). Isofraxidin may have a radioprotective effect in human leukemia cells through decreasing ROS levels in a p53-independent manner (144). Resveratrol has been indicated to attenuate IR enteritis by inhibiting oxidative stress and apoptosis through the activation of the Sirtuin 1/FoxO3a and PI3K/AKT signaling pathways (145). In addition, the endogenous compounds melatonin and vitamin D are considered to be potent radioprotectors for the protection against oxidative damage caused by IR (146). Melatonin has been reported to possess significant potency in inhibiting the induction of oxidative stress via regulation of the expression levels of certain antioxidant genes (including Nrf2) and the activities of ROS/nitric oxide-producing enzymes (147). In addition, this hormone may directly scavenge free radicals to alleviate oxidative injury induced by IR in different cells or organs (147). In previous studies, plant and plant-derived products, such as herbal medicine, have been extensively examined for their effectiveness and compatibility in conferring radioprotection (49). Mn porphyrins are powerful SOD mimics, which have been indicated to possess radioprotective effects in different cells, animal models and tissues, including the lung, the prostate and the brain (148,149). The lead Mn porphyrins, such as MnTE-2-PyP5+ (BMX-010, AEOL10113), MnTnBuOE-2-PyP5+ (BMX-001) and MnTnHex-2-PyP5+ have entered clinical trials for the assessment of their efficacy in the radioprotection of normal tissues during cancer radiotherapy (149).
7. Conclusions
Accumulating evidence suggests that a rational combination of antioxidants or oxidants with IR is an attractive approach to improve the tumor treatment response. In the present review article, the molecular pathways and potential candidate targets that control the induction of oxidative stress in radiosensitivity and radioprotection were discussed. Nrf2 was identified as a key transcriptional target involved in the resistance of cancer cells to radiotherapy. In addition, Trx and GSH complement each other. They are parts of powerful antioxidant mechanisms connected with the protection of cancer cells from radiation resistance. However, due to the limitations of the present study, further experiments should be performed to completely uncover the roles of these antioxidant enzyme systems in radiotherapy. A deeper understanding of the mechanisms underlying oxidative stress in cancer radiotherapy may reveal novel therapeutic opportunities.
Supplementary Data
Acknowledgments
Parts of the figures were adapted using Servier Medical Art (https://smart.servier.com/), licensed under Creative Commons Attribution 3.0 Unported (CC BY 3.0).
Funding Statement
The present study was supported by grants from the National Natural Science Foundation of China (grant nos. 81773363, 81872558, 81972969 and 81673092).
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Authors' contributions
RL and YB contributed to the preparation, bioinformatics analyses and drafting of the manuscript. RL, YB, LL and LCL performed the relevant literature search, assisted in obtaining data and revised the manuscript. XDL and SMM supervised the preparation of the manuscript and critically reviewed the manuscript. All authors have read and approved the final version of the manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Zhang Z, Rong L, Li YP. Flaviviridae viruses and oxidative stress: Implications for viral pathogenesis. Oxid Med Cell Longev. 2019;2019:1409582. doi: 10.1155/2019/1409582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pizzino G, Irrera N, Cucinotta M, Pallio G, Mannino F, Arcoraci V, Squadrito F, Altavilla D, Bitto A. Oxidative stress: Harms and benefits for human health. Oxid Med Cell Longev. 2017;2017:8416763. doi: 10.1155/2017/8416763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hayes JD, Dinkova-Kostova AT, Tew KD. Oxidative stress in cancer. Cancer Cell. 2020;38:167–197. doi: 10.1016/j.ccell.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beyfuss K, Hood DA. A systematic review of p53 regulation of oxidative stress in skeletal muscle. Redox Rep. 2018;23:100–117. doi: 10.1080/13510002.2017.1416773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pisoschi AM, Pop A, Iordache F, Stanca L, Predoi G, Serban AI. Oxidative stress mitigation by antioxidants-An overview on their chemistry and influences on health status. Eur J Med Chem. 2021;209:112891. doi: 10.1016/j.ejmech.2020.112891. [DOI] [PubMed] [Google Scholar]
- 6.Zuo L, Wijegunawardana D. Redox role of ROS and inflammation in pulmonary diseases. Adv Exp Med Biol. 2021;1304:187–204. doi: 10.1007/978-3-030-68748-9_11. [DOI] [PubMed] [Google Scholar]
- 7.Czarnocka W, Karpiński S. Friend or foe? Reactive oxygen species production, scavenging and signaling in plant response to environmental stresses. Free Radic Biol Med. 2018;122:4–20. doi: 10.1016/j.freeradbiomed.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Samavarchi Tehrani S, Mahmoodzadeh Hosseini H, Yousefi T, Abolghasemi M, Qujeq D, Maniati M, Amani J. The crosstalk between trace elements with DNA damage response, repair, and oxidative stress in cancer. J Cell Biochem. 2018 Oct 30; doi: 10.1002/jcb.27617. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Ping Z, Peng Y, Lang H, Xinyong C, Zhiyi Z, Xiaocheng W, Hong Z, Liang S. Oxidative stress in radiation-induced cardiotoxicity. Oxid Med Cell Longev. 2020;2020:3579143. doi: 10.1155/2020/3579143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang XQ, Wang W, Peng M, Zhang XZ. Free radicals for cancer theranostics. Biomaterials. 2021;266:120474. doi: 10.1016/j.biomaterials.2020.120474. [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Duan D, Song ZL, Liu T, Hou Y, Fang J. Small molecules regulating reactive oxygen species homeostasis for cancer therapy. Med Res Rev. 2021;41:342–394. doi: 10.1002/med.21734. [DOI] [PubMed] [Google Scholar]
- 12.Moloney JN, Cotter TG. ROS signalling in the biology of cancer. Semin Cell Dev Biol. 2018;80:50–64. doi: 10.1016/j.semcdb.2017.05.023. [DOI] [PubMed] [Google Scholar]
- 13.Zou Z, Chang H, Li H, Wang S. Induction of reactive oxygen species: An emerging approach for cancer therapy. Apoptosis. 2017;22:1321–1335. doi: 10.1007/s10495-017-1424-9. [DOI] [PubMed] [Google Scholar]
- 14.Rodic S, Vincent MD. Reactive oxygen species (ROS) are a key determinant of Cancer's metabolic phenotype. Int J Cancer. 2018;142:440–448. doi: 10.1002/ijc.31069. [DOI] [PubMed] [Google Scholar]
- 15.Wang S, Luo J, Zhang Z, Dong D, Shen Y, Fang Y, Hu L, Liu M, Dai C, Peng S, et al. Iron and magnetic: New research direction of the ferroptosis-based cancer therapy. Am J Cancer Res. 2018;8:1933–1946. [PMC free article] [PubMed] [Google Scholar]
- 16.Snezhkina AV, Kudryavtseva AV, Kardymon OL, Savvateeva MV, Melnikova NV, Krasnov GS, Dmitriev AA. ROS Generation and antioxidant defense systems in normal and malignant cells. Oxid Med Cell Longev. 2019;2019:6175804. doi: 10.1155/2019/6175804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Helfinger V, Schröder K. Redox control in cancer development and progression. Mol Aspects Med. 2018;63:88–98. doi: 10.1016/j.mam.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 18.Sánchez-Sánchez AM, Martín V, García-Santos G, Rodríguez-Blanco J, Casado-Zapico S, Suarez-Garnacho S, Antolín I, Rodriguez C. Intracellular redox state as determinant for melatonin antiproliferative vs cytotoxic effects in cancer cells. Free Radic Res. 2011;45:1333–1341. doi: 10.3109/10715762.2011.623700. [DOI] [PubMed] [Google Scholar]
- 19.Klaunig JE. Oxidative stress and cancer. Curr Pharm Des. 2018;24:4771–4778. doi: 10.2174/1381612825666190215121712. [DOI] [PubMed] [Google Scholar]
- 20.Xie Q, Lan G, Zhou Y, Huang J, Liang Y, Zheng W, Fu X, Fan C, Chen T. Strategy to enhance the anticancer efficacy of X-ray radiotherapy in melanoma cells by platinum complexes, the role of ROS-mediated signaling pathways. Cancer Lett. 2014;354:58–67. doi: 10.1016/j.canlet.2014.07.046. [DOI] [PubMed] [Google Scholar]
- 21.Galeaz C, Totis C, Bisio A. Radiation resistance: A matter of transcription factors. Front Oncol. 2021;11:662840. doi: 10.3389/fonc.2021.662840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sonis ST. Superoxide dismutase as an intervention for radiation therapy-associated toxicities: Review and profile of avasopasem manganese as a treatment option for radiation-induced mucositis. Drug Des Devel Ther. 2021;15:1021–1029. doi: 10.2147/DDDT.S267400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perillo B, Di Donato M, Pezone A, Di Zazzo E, Giovannelli P, Galasso G, Castoria G, Migliaccio A. ROS in cancer therapy: The bright side of the moon. Exp Mol Med. 2020;52:192–203. doi: 10.1038/s12276-020-0384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim SJ, Kim HS, Seo YR. Understanding of ROS-inducing strategy in anticancer therapy. Oxid Med Cell Longev. 2019;2019:5381692. doi: 10.1155/2019/5381692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hu J, Li Y, Li H, Shi F, Xie L, Zhao L, Tang M, Luo X, Jia W, Fan J, et al. Targeting Epstein-Barr virus oncoprotein LMP1-mediated high oxidative stress suppresses EBV lytic reactivation and sensitizes tumors to radiation therapy. Theranostics. 2020;10:11921–11937. doi: 10.7150/thno.46006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poprac P, Jomova K, Simunkova M, Kollar V, Rhodes CJ, Valko M. Targeting free radicals in oxidative stress-related human diseases. Trends Pharmacol Sci. 2017;38:592–607. doi: 10.1016/j.tips.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 27.Jiang H, Wang H, De Ridder M. Targeting antioxidant enzymes as a radiosensitizing strategy. Cancer Lett. 2018;438:154–164. doi: 10.1016/j.canlet.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 28.Jaganjac M, Milkovic L, Sunjic SB, Zarkovic N. The NRF2, Thioredoxin, and Glutathione system in tumorigenesis and anticancer therapies. Antioxidants (Basel) 2020;9:E1151. doi: 10.3390/antiox9111151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reczek CR, Chandel NS. The two faces of reactive oxygen species in cancer. Ann Rev Cancer Biol. 2017;1:79–98. doi: 10.1146/annurev-cancerbio-041916-065808. [DOI] [Google Scholar]
- 30.Koyama H, Nojiri H, Kawakami S, Sunagawa T, Shirasawa T, Shimizu T. Antioxidants improve the phenotypes of dilated cardiomyopathy and muscle fatigue in mitochondrial superoxide dismutase-deficient mice. Molecules. 2013;18:1383–1393. doi: 10.3390/molecules18021383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ighodaro OM, Akinloye OA. First line defence antioxidantssuperoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): Their fundamental role in the entire antioxidant defence grid. Alexandria J Med. 2018;54:287–293. doi: 10.1016/j.ajme.2017.09.001. [DOI] [Google Scholar]
- 32.Haddad M, Hervé V, Ben Khedher MR, Rabanel JM, Ramassamy C. Glutathione: An old and small molecule with great functions and new applications in the brain and in Alzheimer's disease. Antioxid Redox Signal. 2021;35:270–292. doi: 10.1089/ars.2020.8129. [DOI] [PubMed] [Google Scholar]
- 33.Marrocco I, Altieri F, Peluso I. Measurement and clinical significance of biomarkers of oxidative stress in humans. Oxid Med Cell Longev. 2017;2017:6501046. doi: 10.1155/2017/6501046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang ML, Wu HT, Chen WJ, Xu Y, Ye QQ, Shen JX, Liu J. Involvement of glutathione peroxidases in the occurrence and development of breast cancers. J Transl Med. 2020;18:247. doi: 10.1186/s12967-020-02420-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu X, Zhang Y, Zhuang L, Olszewski K, Gan B. NADPH debt drives redox bankruptcy: SLC7A11/xCT-mediated cystine uptake as a double-edged sword in cellular redox regulation. Genes Dis. 2021;8:731–745. doi: 10.1016/j.gendis.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu J, Xia X, Huang P. xCT: A critical molecule that links cancer metabolism to redox signaling. Mol Ther. 2020;28:2358–2366. doi: 10.1016/j.ymthe.2020.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lu J, Chew EH, Holmgren A. Targeting thioredoxin reductase is a basis for cancer therapy by arsenic trioxide. Proc Natl Acad Sci USA. 2007;104:12288–12293. doi: 10.1073/pnas.0701549104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ren X, Zou L, Zhang X, Branco V, Wang J, Carvalho C, Holmgren A, Lu J. Redox signaling mediated by thioredoxin and glutathione systems in the central nervous system. Antioxid Redox Signal. 2017;27:989–1010. doi: 10.1089/ars.2016.6925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu TI, Lu TY, Yang YC, Chang SH, Chen HH, Lu IL, Sabu A, Chiu HC. New combination treatment from ROS-Induced sensitized radiotherapy with nanophototherapeutics to fully eradicate orthotopic breast cancer and inhibit metastasis. Biomaterials. 2020;257:120229. doi: 10.1016/j.biomaterials.2020.120229. [DOI] [PubMed] [Google Scholar]
- 40.Shevtsov M, Sato H, Multhoff G, Shibata A. Novel approaches to improve the efficacy of immuno-Radiotherapy. Front Oncol. 2019;9:156. doi: 10.3389/fonc.2019.00156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rabus H. Nanodosimetry-on the 'tracks' of biological radiation effectiveness. Z Med Phys. 2020;30:91–94. doi: 10.1016/j.zemedi.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 42.Wang H, Jiang H, Van De Gucht M, De Ridder M. Hypoxic radioresistance: Can ROS be the key to overcome it? Cancers (Basel) 2019;11:112. doi: 10.3390/cancers11010112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Alizadeh E, Orlando TM, Sanche L. Biomolecular damage induced by ionizing radiation: The direct and indirect effects of low-energy electrons on DNA. Annu Rev Phys Chem. 2015;66:379–398. doi: 10.1146/annurev-physchem-040513-103605. [DOI] [PubMed] [Google Scholar]
- 44.Baskar R, Dai J, Wenlong N, Yeo R, Yeoh KW. Biological response of cancer cells to radiation treatment. Front Mol Biosci. 2014;1:24. doi: 10.3389/fmolb.2014.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Le Caër S. Water Radiolysis: Influence of oxide surfaces on H2 production under ionizing radiation. Water. 2011;3:235–253. doi: 10.3390/w3010235. [DOI] [Google Scholar]
- 46.Baldacchino G, Brun E, Denden I, Bouhadoun S, Roux R, Khodja H, Sicard-Roselli C. Importance of radiolytic reactions during high-LET irradiation modalities: LET effect, role of O2 and radiosensitization by nanoparticles. Cancer Nanotechnol. 2019;10:3. doi: 10.1186/s12645-019-0047-y. [DOI] [Google Scholar]
- 47.Gong L, Zhang Y, Liu C, Zhang M, Han S. Application of radiosensitizers in cancer radiotherapy. Int J Nanomedicine. 2021;16:1083–1102. doi: 10.2147/IJN.S290438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Collin F. Chemical basis of reactive oxygen species reactivity and involvement in neurodegenerative diseases. Int J Mol Sci. 2019;20:2407. doi: 10.3390/ijms20102407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dayal R, Singh A, Pandey A, Mishra KP. Reactive oxygen species as mediator of tumor radiosensitivity. J Cancer Res Ther. 2014;10:811–818. doi: 10.4103/0973-1482.146073. [DOI] [PubMed] [Google Scholar]
- 50.Azzam EI, Jay-Gerin JP, Pain D. Ionizing radiation-induced metabolic oxidative stress and prolonged cell injury. Cancer Lett. 2012;327:48–60. doi: 10.1016/j.canlet.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Robinett ZN, Bathla G, Wu A, Clark JJ, Sibenaller ZA, Wilson T, Kirby P, Allen BG, Hansen MR. Persistent oxidative stress in vestibular schwannomas after stereotactic radiation therapy. Otol Neurotol. 2018;39:1184–1190. doi: 10.1097/MAO.0000000000001935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Buonanno M, de Toledo SM, Pain D, Azzam EI. Long-Term consequences of radiation-induced bystander effects depend on radiation quality and dose and correlate with oxidative stress. Radiat Res. 2011;175:405–415. doi: 10.1667/RR2461.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang QY, Wang FX, Jia KK, Kong LD. Natural product interventions for chemotherapy and radiotherapy-induced side effects. Front Pharmacol. 2018;9:1253. doi: 10.3389/fphar.2018.01253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Musa AE, Shabeeb D, Alhilfi HSQ. Protective effect of melatonin against radiotherapy-induced small intestinal oxidative stress: Biochemical evaluation. Medicina (Kaunas) 2019;55:308. doi: 10.3390/medicina55060308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lei G, Mao C, Yan Y, Zhuang L, Gan B. Ferroptosis, radiotherapy, and combination therapeutic strategies. Protein Cell. 2021;12:836–857. doi: 10.1007/s13238-021-00841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu B, Bhatt D, Oltvai ZN, Greenberger JS, Bahar I. Significance of p53 dynamics in regulating apoptosis in response to ionizing radiation and polypharmacological strategies. Sci Rep. 2014;4:6245. doi: 10.1038/srep06245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zanella F, Link W, Carnero A. Understanding FOXO, new views on old transcription factors. Curr Cancer Drug Targets. 2010;10:135–146. doi: 10.2174/156800910791054158. [DOI] [PubMed] [Google Scholar]
- 58.Schmidt-Ullrich RK, Contessa JN, Lammering G, Amorino G, Lin PS. ERBB receptor tyrosine kinases and cellular radiation responses. Oncogene. 2003;22:5855–5865. doi: 10.1038/sj.onc.1206698. [DOI] [PubMed] [Google Scholar]
- 59.Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, Patel DN, Bauer AJ, Cantley AM, Yang WS, et al. Ferroptosis: An iron-dependent form of non-apoptotic cell death. Cell. 2012;149:1060–1072. doi: 10.1016/j.cell.2012.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhu J, Xiong Y, Zhang Y, Wen J, Cai N, Cheng K, Liang H, Zhang W. The molecular mechanisms of regulating oxidative stress-induced ferroptosis and therapeutic strategy in tumors. Oxid Med Cell Longev. 2020;2020:8810785. doi: 10.1155/2020/8810785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barrera G. Oxidative stress and lipid peroxidation products in cancer progression and therapy. ISRN Oncol. 2012;2012:137289. doi: 10.5402/2012/137289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stockwell BR, Jiang X, Gu W. Emerging mechanisms and disease relevance of ferroptosis. Trends Cell Biol. 2020;30:478–490. doi: 10.1016/j.tcb.2020.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lang X, Green MD, Wang W, Yu J, Choi JE, Jiang L, Liao P, Zhou J, Zhang Q, Dow A, et al. Radiotherapy and immunotherapy promote tumoral lipid oxidation and ferroptosis via synergistic repression of SLC7A11. Cancer Discov. 2019;9:1673–1685. doi: 10.1158/2159-8290.CD-19-0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li X, Duan L, Yuan S, Zhuang X, Qiao T, He J. Ferroptosis inhibitor alleviates Radiation-induced lung fibrosis (RILF) via down-regulation of TGF-β1. J Inflamm (Lond) 2019;16:11. doi: 10.1186/s12950-019-0216-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lei G, Zhang Y, Koppula P, Liu X, Zhang J, Lin SH, Ajani JA, Xiao Q, Liao Z, Wang H, Gan B. The role of ferroptosis in ionizing radiation-induced cell death and tumor suppression. Cell Res. 2020;30:146–162. doi: 10.1038/s41422-019-0263-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li J, Cao F, Yin HL, Huang ZJ, Lin ZT, Mao N, Sun B, Wang G. Ferroptosis: Past, present and future. Cell Death Dis. 2020;11:88. doi: 10.1038/s41419-020-2298-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jiang L, Kon N, Li T, Wang SJ, Su T, Hibshoosh H, Baer R, Gu W. Ferroptosis as a p53-mediated activity during tumour suppression. Nature. 2015;520:57–62. doi: 10.1038/nature14344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dodson M, Castro-Portuguez R, Zhang DD. NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol. 2019;23:101107. doi: 10.1016/j.redox.2019.101107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cameron BD, Sekhar KR, Ofori M, Freeman ML. The role of Nrf2 in the response to normal tissue radiation injury. Radiat Res. 2018;190:99–106. doi: 10.1667/RR15059.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sekhar KR, Freeman ML. Nrf2 promotes survival following exposure to ionizing radiation. Free Radic Biol Med. 2015;88:268–274. doi: 10.1016/j.freeradbiomed.2015.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Feng L, Zhao K, Sun L, Yin X, Zhang J, Liu C, Li B. SLC7A11 regulated by NRF2 modulates esophageal squamous cell carcinoma radiosensitivity by inhibiting ferroptosis. J Transl Med. 2021;19:367. doi: 10.1186/s12967-021-03042-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lippmann J, Petri K, Fulda S, Liese J. Redox modulation and induction of ferroptosis as a new therapeutic strategy in hepatocellular carcinoma. Transl Oncol. 2020;13:100785. doi: 10.1016/j.tranon.2020.100785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jakobs P, Serbulea V, Leitinger N, Eckers A, Haendeler J. Nuclear factor (Erythroid-Derived 2)-Like 2 and Thioredoxin-1 in atherosclerosis and ischemia/reperfusion injury in the heart. Antioxid Redox Signal. 2017;26:630–644. doi: 10.1089/ars.2016.6795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Banning A, Deubel S, Kluth D, Zhou Z, Brigelius-Flohé R. The GI-GPx Gene Is a target for Nrf2. Mol Cell Biol. 2005;25:4914–4923. doi: 10.1128/MCB.25.12.4914-4923.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim YJ, Ahn JY, Liang P, Ip C, Zhang Y, Park YM. Human prx1 gene is a target of Nrf2 and is up-regulated by hypoxia/reoxygenation: Implication to tumor biology. Cancer Res. 2007;67:546–554. doi: 10.1158/0008-5472.CAN-06-2401. [DOI] [PubMed] [Google Scholar]
- 76.Fisher AB. Peroxiredoxin 6: A Bifunctional enzyme with glutathione peroxidase and phospholipase A2 activities. Antioxid Redox Signal. 2011;15:831–844. doi: 10.1089/ars.2010.3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yang H, Magilnick N, Lee C, Kalmaz D, Ou X, Chan JY, Lu SC. Nrf1 and Nrf2 regulate rat glutamate-cysteine ligase catalytic subunit transcription indirectly via NF-kappaB and AP-1. Mol Cell Biol. 2005;25:5933–5946. doi: 10.1128/MCB.25.14.5933-5946.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sinha K, Das J, Pal PB, Sil PC. Oxidative stress: The mitochondria-dependent and mitochondria-independent pathways of apoptosis. Arch Toxicol. 2013;87:1157–1180. doi: 10.1007/s00204-013-1034-4. [DOI] [PubMed] [Google Scholar]
- 79.Chen KW, Demarco B, Heilig R, Shkarina K, Boettcher A, Farady CJ, Pelczar P, Broz P. Extrinsic and intrinsic apoptosis activate pannexin-1 to drive NLRP3 inflammasome assembly. EMBO J. 2019;38:e101638. doi: 10.15252/embj.2019101638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cao X, Wen P, Fu Y, Gao Y, Qi X, Chen B, Tao Y, Wu L, Xu A, Lu H, Zhao G. Radiation induces apoptosis primarily through the intrinsic pathway in mammalian cells. Cell Signal. 2019;62:109337. doi: 10.1016/j.cellsig.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 81.Liu C, Mann D, Sinha UK, Kokot NC. The molecular mechanisms of increased radiosensitivity of HPV-positive oropharyngeal squamous cell carcinoma (OPSCC): An extensive review. J Otolaryngol Head Neck Surg. 2018;47:59. doi: 10.1186/s40463-018-0302-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mendes F, Sales T, Domingues C, Schugk S, Abrantes AM, Gonçalves AC, Teixo R, Silva R, Casalta-Lopes J, Rocha C, et al. Effects of X-radiation on lung cancer cells: the interplay between oxidative stress and P53 levels. Med Oncol. 2015;32:266. doi: 10.1007/s12032-015-0712-x. [DOI] [PubMed] [Google Scholar]
- 83.Mortezaee K, Najafi M, Farhood B, Ahmadi A, Potes Y, Shabeeb D, Musa AE. Modulation of apoptosis by melatonin for improving cancer treatment efficiency: An updated review. Life Sci. 2019;228:228–241. doi: 10.1016/j.lfs.2019.05.009. [DOI] [PubMed] [Google Scholar]
- 84.Qin C, Chen X, Bai Q, Davis MR, Fang Y. Factors associated with radiosensitivity of cervical cancer. Anticancer Res. 2014;34:4649–4656. [PubMed] [Google Scholar]
- 85.Kim W, Lee S, Seo D, Kim D, Kim K, Kim E, Kang J, Seong KM, Youn H, Youn B. Cellular stress responses in radiotherapy. Cells. 2019;8:1105. doi: 10.3390/cells8091105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chang HW, Lee M, Lee YS, Kim SH, Lee JC, Park JJ, Nam HY, Kim MR, Han MW, Kim SW, Kim SY. p53-dependent glutamine usage determines susceptibility to oxidative stress in radioresistant head and neck cancer cells. Cell Signal. 2021;77:109820. doi: 10.1016/j.cellsig.2020.109820. [DOI] [PubMed] [Google Scholar]
- 87.Maya R, Balass M, Kim ST, Shkedy D, Leal JF, Shifman O, Moas M, Buschmann T, Ronai Z, Shiloh Y, et al. ATM-dependent phosphorylation of Mdm2 on serine 395: Role in p53 activation by DNA damage. Genes Dev. 2001;15:1067–1077. doi: 10.1101/gad.886901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kim EM, Jung CH, Kim J, Hwang SG, Park JK, Um HD. The p53/p21 complex regulates cancer cell invasion and apoptosis by targeting Bcl-2 family proteins. Cancer Res. 2017;77:3092–3100. doi: 10.1158/0008-5472.CAN-16-2098. [DOI] [PubMed] [Google Scholar]
- 89.Budanov AV. The role of tumor suppressor p53 in the antioxidant defense and metabolism. Subcell Biochem. 2014;85:337–358. doi: 10.1007/978-94-017-9211-0_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rastogi S, Rizwani W, Joshi B, Kunigal S, Chellappan SP. TNF-α response of vascular endothelial and vascular smooth muscle cells involve differential utilization of ASK1 kinase and p73. Cell Death Differ. 2012;19:274–283. doi: 10.1038/cdd.2011.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Feltham R, Jamal K, Tenev T, Liccardi G, Jaco I, Domingues CM, Morris O, John SW, Annibaldi A, Widya M, et al. Mind bomb regulates cell death during TNF signaling by suppressing RIPK1's cytotoxic potential. Cell Rep. 2018;23:470–484. doi: 10.1016/j.celrep.2018.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kokolakis G, Sabat R, Krüger-Krasagakis S, Eberle J. Ambivalent effects of tumor necrosis factor alpha on apoptosis of malignant and normal human keratinocytes. Skin Pharmacol Physiol. 2021;34:94–102. doi: 10.1159/000513725. [DOI] [PubMed] [Google Scholar]
- 93.Stoytcheva ZR, Berry MJ. Transcriptional regulation of mammalian selenoprotein expression. Biochim Biophys Acta. 2009;1790:1429–1440. doi: 10.1016/j.bbagen.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ross MJ, Martinka S, D'Agati VD, Bruggeman LA. NF-kappaB regulates Fas-mediated apoptosis in HIV-associated nephropathy. J Am Soc Nephrol. 2005;16:2403–2411. doi: 10.1681/ASN.2004121101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Morgan MJ, Liu Z. Crosstalk of reactive oxygen species and NF-κB signaling. Cell Res. 2011;21:103–115. doi: 10.1038/cr.2010.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li Q, Sun Y, Liu B, Li J, Hao X, Ge W, Zhang X, Bao S, Gong J, Jiang Z, et al. ACT001 modulates the NF-κB/MnSOD/ROS axis by targeting IKKβ to inhibit glioblastoma cell growth. J Mol Med (Berl) 2020;98:263–277. doi: 10.1007/s00109-019-01839-0. [DOI] [PubMed] [Google Scholar]
- 97.Kumar S, Clair DS. Radioresistance in prostate cancer: Focus on the interplay between NF-κB and SOD. Antioxidants (Basel) 2021;10:1925. doi: 10.3390/antiox10121925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Soh R, Hardy A, Zur Nieden NI. The FOXO signaling axis displays conjoined functions in redox homeostasis and stemness. Free Radic Biol Med. 2021;169:224–237. doi: 10.1016/j.freeradbiomed.2021.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ponugoti B, Dong G, Graves DT. Role of forkhead transcription factors in diabetes-induced oxidative stress. Exp Diabetes Res. 2012;2012:939751. doi: 10.1155/2012/939751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yang JY, Xia W, Hu MC. Ionizing radiation activates expression of FOXO3a, Fas ligand, and Bim, and induces cell apoptosis. Int J Oncol. 2006;29:643–648. [PMC free article] [PubMed] [Google Scholar]
- 101.Lim SW, Jin L, Luo K, Jin J, Shin YJ, Hong SY, Yang CW. Klotho enhances FoxO3-mediated manganese superoxide dismutase expression by negatively regulating PI3K/AKT pathway during tacrolimus-induced oxidative stress. Cell Death Dis. 2017;8:e2972. doi: 10.1038/cddis.2017.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tseng AH, Wu LH, Shieh SS, Wang DL. SIRT3 interactions with FOXO3 acetylation, phosphorylation and ubiquitinylation mediate endothelial cell responses to hypoxia. Biochem J. 2014;464:157–168. doi: 10.1042/BJ20140213. [DOI] [PubMed] [Google Scholar]
- 103.Wang Y, Chen S, Li H. Hydrogen peroxide stress stimulates phosphorylation of FoxO1 in rat aortic endothelial cells. Acta Pharmacol Sin. 2010;31:160–164. doi: 10.1038/aps.2009.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Guan L, Zhang L, Gong Z, Hou X, Xu Y, Feng X, Wang H, You H. FoxO3 inactivation promotes human cholangiocarcinoma tumorigenesis and chemoresistance through Keap1-Nrf2 signaling. Hepatology. 2016;63:1914–1927. doi: 10.1002/hep.28496. [DOI] [PubMed] [Google Scholar]
- 105.Araujo J, Breuer P, Dieringer S, Krauss S, Dorn S, Zimmermann K, Pfeifer A, Klockgether T, Wuellner U, Evert BO. FOXO4-dependent upregulation of superoxide dismutase-2 in response to oxidative stress is impaired in spinocerebellar ataxia type 3. Hum Mol Genet. 2011;20:2928–2941. doi: 10.1093/hmg/ddr197. [DOI] [PubMed] [Google Scholar]
- 106.Rached MT, Kode A, Xu L, Yoshikawa Y, Paik JH, DePinho RA, Kousteni S. FoxO1 is a positive regulator of bone formation by favoring protein synthesis and resistance to oxidative stress in osteoblasts. Cell Metab. 2010;11:147–160. doi: 10.1016/j.cmet.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ye P, Mimura J, Okada T, Sato H, Liu T, Maruyama A, Ohyama C, Itoh K. Nrf2- and ATF4-dependent upregulation of xCT modulates the sensitivity of T24 bladder carcinoma cells to proteasome inhibition. Mol Cell Biol. 2014;34:3421–3434. doi: 10.1128/MCB.00221-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang Z. ErbB receptors and cancer. Methods Mol Biol. 2017;1652:3–35. doi: 10.1007/978-1-4939-7219-7_1. [DOI] [PubMed] [Google Scholar]
- 109.Valerie K, Yacoub A, Hagan MP, Curiel DT, Fisher PB, Grant S, Dent P. Radiation-induced cell signaling: Inside-out and outside-in. Mol Cancer Ther. 2007;6:789–801. doi: 10.1158/1535-7163.MCT-06-0596. [DOI] [PubMed] [Google Scholar]
- 110.Appert-Collin A, Hubert P, Crémel G, Bennasroune A. Role of ErbB receptors in cancer cell migration and invasion. Front Pharmacol. 2015;6:283. doi: 10.3389/fphar.2015.00283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wee P, Wang Z. Epidermal growth factor receptor cell proliferation signaling pathways. Cancers (Basel) 2017;9:52. doi: 10.3390/cancers9050052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rezatabar S, Karimian A, Rameshknia V, Parsian H, Majidinia M, Kopi TA, Bishayee A, Sadeghinia A, Yousefi M, Monirialamdari M, Yousefi B. RAS/MAPK signaling functions in oxidative stress, DNA damage response and cancer progression. J Cell Physiol. 2019 Feb 27; doi: 10.1002/jcp.28334. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 113.Kim MJ, Choi WG, Ahn KJ, Chae IG, Yu R, Back SH. Reduced EGFR level in eIF2α PhosphorylationDeficient hepatocytes is responsible for susceptibility to oxidative stress. Mol Cells. 2020;43:264–275. doi: 10.14348/molcells.2020.2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang W, Yang H, Zhu L, Luo Y, Nie L, Li G. Role of EGFR/ErbB2 and PI3K/AKT/e-NOS in Lycium barbarum polysaccharides ameliorating endothelial dysfunction induced by oxidative stress. Am J Chin Med. 2019;47:1523–1539. doi: 10.1142/S0192415X19500782. [DOI] [PubMed] [Google Scholar]
- 115.Boeckx C, Van den Bossche J, De Pauw I, Peeters M, Lardon F, Baay M, Wouters A. The hypoxic tumor microenvironment and drug resistance against EGFR inhibitors: Preclinical study in cetuximab-sensitive head and neck squamous cell carcinoma cell lines. BMC Res Notes. 2015;8:203. doi: 10.1186/s13104-015-1197-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bierl C, Voetsch B, Jin RC, Handy DE, Loscalzo J. Determinants of human plasma glutathione peroxidase (GPx-3) expression. J Biol Chem. 2004;279:26839–26845. doi: 10.1074/jbc.M401907200. [DOI] [PubMed] [Google Scholar]
- 117.Tonelli C, Chio IIC, Tuveson DA. Transcriptional regulation by Nrf2. Antioxid Redox Signal. 2018;29:1727–1745. doi: 10.1089/ars.2017.7342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kang HJ, Yi YW, Hong YB, Kim HJ, Jang YJ, Seong YS, Bae I. HER2 confers drug resistance of human breast cancer cells through activation of NRF2 by direct interaction. Sci Rep. 2014;4:7201. doi: 10.1038/srep07201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sakurai A, Nishimoto M, Himeno S, Imura N, Tsujimoto M, Kunimoto M, Hara S. Transcriptional regulation of thioredoxin reductase 1 expression by cadmium in vascular endothelial cells: Role of NF-E2-related factor-2. J Cell Physiol. 2005;203:529–537. doi: 10.1002/jcp.20246. [DOI] [PubMed] [Google Scholar]
- 120.Gordon LI, Burke MA, Singh AT, Prachand S, Lieberman ED, Sun L, Naik TJ, Prasad SV, Ardehali H. Blockade of the erbB2 receptor induces cardiomyocyte death through mitochondrial and reactive oxygen species-dependent pathways. J Biol Chem. 2009;284:2080–2087. doi: 10.1074/jbc.M804570200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Allegra AG, Mannino F, Innao V, Musolino C, Allegra A. Radioprotective agents and enhancers factors Preventive and therapeutic strategies for oxidative induced radiotherapy damages in hematological malignancies. Antioxidants (Basel) 2020;9:1116. doi: 10.3390/antiox9111116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Jasek-Gajda E, Jurkowska H, Jasińska M, Lis GJ. Targeting the MAPK/ERK and PI3K/AKT signaling pathways affects NRF2, Trx and GSH antioxidant systems in leukemia cells. Antioxidants (Basel) 2020;9:633. doi: 10.3390/antiox9070633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chen QM, Maltagliati AJ. Nrf2 at the heart of oxidative stress and cardiac protection. Physiol Genomics. 2018;50:77–97. doi: 10.1152/physiolgenomics.00041.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Qin S, He X, Lin H, Schulte BA, Zhao M, Tew KD, Wang GY. Nrf2 inhibition sensitizes breast cancer stem cells to ionizing radiation via suppressing DNA repair. Free Radic Biol Med. 2021;169:238–247. doi: 10.1016/j.freeradbiomed.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sun X, Wang Q, Wang Y, Du L, Xu C, Liu Q. Brusatol enhances the radiosensitivity of A549 cells by promoting ROS production and enhancing DNA damage. Int J Mol Sci. 2016;17:E997. doi: 10.3390/ijms17070997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lee S, Lim MJ, Kim MH, Yu CH, Yun YS, Ahn J, Song JY. An effective strategy for increasing the radiosensitivity of Human lung Cancer cells by blocking Nrf2-dependent antioxidant responses. Free Radic Biol Med. 2012;53:807–816. doi: 10.1016/j.freeradbiomed.2012.05.038. [DOI] [PubMed] [Google Scholar]
- 127.Tsuchida K, Tsujita T, Hayashi M, Ojima A, Keleku-Lukwete N, Katsuoka F, Otsuki A, Kikuchi H, Oshima Y, Suzuki M, Yamamoto M. Halofuginone enhances the chemo-sensitivity of cancer cells by suppressing NRF2 accumulation. Free Radic Biol Med. 2017;103:236–247. doi: 10.1016/j.freeradbiomed.2016.12.041. [DOI] [PubMed] [Google Scholar]
- 128.Park M, Kwon J, Shin HJ, Moon SM, Kim SB, Shin US, Han YH, Kim Y. Butyrate enhances the efficacy of radiotherapy via FOXO3A in colorectal cancer patient-derived organoids. Int J Oncol. 2020;57:1307–1318. doi: 10.3892/ijo.2020.5132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Liu Z, Li Y, She G, Zheng X, Shao L, Wang P, Pang M, Xie S, Sun Y. Resveratrol induces cervical cancer HeLa cell apoptosis through the activation and nuclear translocation promotion of FOXO3a. Pharmazie. 2020;75:250–254. doi: 10.1691/ph.2020.0386. [DOI] [PubMed] [Google Scholar]
- 130.Wang H, Bouzakoura S, de Mey S, Jiang H, Law K, Dufait I, Corbet C, Verovski V, Gevaert T, Feron O, et al. Auranofin radiosensitizes tumor cells through targeting thioredoxin reductase and resulting overproduction of reactive oxygen species. Oncotarget. 2017;8:35728–35742. doi: 10.18632/oncotarget.16113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Xie Q, Zhou Y, Lan G, Yang L, Zheng W, Liang Y, Chen T. Sensitization of cancer cells to radiation by selenadiazole derivatives by regulation of ROS-mediated DNA damage and ERK and AKT pathways. Biochem Biophys Res Commun. 2014;449:88–93. doi: 10.1016/j.bbrc.2014.04.151. [DOI] [PubMed] [Google Scholar]
- 132.Liang YW, Zheng J, Li X, Zheng W, Chen T. Selenadiazole derivatives as potent thioredoxin reductase inhibitors that enhance the radiosensitivity of cancer cells. Eur J Med Chem. 2014;84:335–342. doi: 10.1016/j.ejmech.2014.07.032. [DOI] [PubMed] [Google Scholar]
- 133.Jia JJ, Geng WS, Wang ZQ, Chen L, Zeng XS. The role of thioredoxin system in cancer: Strategy for cancer therapy. Cancer Chemother Pharmacol. 2019;84:453–470. doi: 10.1007/s00280-019-03869-4. [DOI] [PubMed] [Google Scholar]
- 134.Kimple RJ, Vaseva AV, Cox AD, Baerman KM, Calvo BF, Tepper JE, Shields JM, Sartor CI. Radiosensitization of epidermal growth factor receptor/HER2-positive pancreatic cancer is mediated by inhibition of Akt independent of ras mutational status. Clin Cancer Res. 2010;16:912–923. doi: 10.1158/1078-0432.CCR-09-1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang S, Fu Y, Wang D, Wang J. Icotinib enhances lung cancer cell radiosensitivity in vitro and in vivo by inhibiting MAPK/ERK and AKT activation. Clin Exp Pharmacol Physiol. 2018 May 16; doi: 10.1111/1440-1681.12966. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 136.Yi H, Yan X, Luo Q, Yuan L, Li B, Pan W, Zhang L, Chen H, Wang J, Zhang Y, et al. A novel small molecule inhibitor of MDM2-p53 (APG-115) enhances radiosensitivity of gastric adenocarcinoma. J Exp Clin Cancer Res. 2018;37:97. doi: 10.1186/s13046-018-0765-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wang J, Wang H, Qian H. Biological effects of radiation on cancer cells. Mil Med Res. 2018;5:20. doi: 10.1186/s40779-018-0167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Desouky O, Ding N, Zhou G. Targeted and non-targeted effects of ionizing radiation. J Radiation Res App Sci. 2015;8:247–254. [Google Scholar]
- 139.De Ruysscher D, Niedermann G, Burnet NG, Siva S, Lee AWM, Hegi-Johnson F. Radiotherapy toxicity. Nat Rev Dis Primers. 2019;5:13. doi: 10.1038/s41572-019-0064-5. [DOI] [PubMed] [Google Scholar]
- 140.Mukherjee D, Coates PJ, Lorimore SA, Wright EG. Responses to ionizing radiation mediated by inflammatory mechanisms. J Pathol. 2014;232:289–299. doi: 10.1002/path.4299. [DOI] [PubMed] [Google Scholar]
- 141.LeBaron TW, Kura B, Kalocayova B, Tribulova N, Slezak J. A new approach for the prevention and treatment of cardiovascular disorders. Molecular Hydrogen Significantly Reduces the Effects of Oxidative Stress. Molecules. 2019;24:2076. doi: 10.3390/molecules24112076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ebrahimi S, Soltani A, Hashemy SI. Oxidative stress in cervical cancer pathogenesis and resistance to therapy. J Cell Biochem. 2018 Nov 13; doi: 10.1002/jcb.28007. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 143.Gudkov AV, Komarova EA. The role of p53 in determining sensitivity to radiotherapy. Nat Rev Cancer. 2003;3:117–129. doi: 10.1038/nrc992. [DOI] [PubMed] [Google Scholar]
- 144.Li P, Zhao QL, Wu LH, Jawaid P, Jiao YF, Kadowaki M, Kondo T. Isofraxidin, a potent reactive oxygen species (ROS) scavenger, protects human leukemia cells from radiation-induced apoptosis via ROS/mitochondria pathway in p53-independent manner. Apoptosis. 2014;19:1043–1053. doi: 10.1007/s10495-014-0984-1. [DOI] [PubMed] [Google Scholar]
- 145.Qin H, Zhang H, Zhang X, Zhang S, Zhu S, Wang H. Resveratrol attenuates radiation enteritis through the SIRT1/FOXO3a and PI3K/AKT signaling pathways. Biochem Biophys Res Commun. 2021;554:199–205. doi: 10.1016/j.bbrc.2021.03.122. [DOI] [PubMed] [Google Scholar]
- 146.Nuszkiewicz J, Woźniak A, Szewczyk-Golec K. Ionizing radiation as a source of oxidative stress-the protective role of melatonin and vitamin D. Int J Mol Sci. 2020;21:5804. doi: 10.3390/ijms21165804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Farhood B, Goradel NH, Mortezaee K, Khanlarkhani N, Salehi E, Nashtaei MS, Mirtavoos-Mahyari H, Motevaseli E, Shabeeb D, Musa AE, Najafi M. Melatonin as an adjuvant in radiotherapy for radioprotection and radiosensitization. Clin Transl Oncol. 2019;21:268–279. doi: 10.1007/s12094-018-1934-0. [DOI] [PubMed] [Google Scholar]
- 148.Batinic-Haberle I, Tovmasyan A, Spasojevic I. Mn Porphyrin-based redox-active drugs: Differential effects as cancer therapeutics and protectors of normal tissue against oxidative injury. Antioxid Redox Signal. 2018;29:1691–1724. doi: 10.1089/ars.2017.7453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Batinic-Haberle I, Tovmasyan A, Huang Z, Duan W, Du L, Siamakpour-Reihani S, Cao Z, Sheng H, Spasojevic I, Alvarez Secord A. H2O2-Driven Anticancer Activity of Mn Porphyrins and the underlying molecular pathways. Oxid Med Cell Longev. 2021;2021:6653790. doi: 10.1155/2021/6653790. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article.