Abstract
Purpose
To evaluate the measurement reliability of the geometric features of tibiofemoral joint on conventional knee MRI and also identify the features associated with increased risk of ACL injury.
Methods
This retrospective case-control study included knee MRIs of 60 patients with ACL injury (34 men, 26 women; mean age 34 ± 13.6 SD) and 60 normal individuals (31 men, 29 women; mean age 36 ± 11.4 SD). Geometric features of distal femur (intercondylar notch width, transcondylar width, and intercondylar notch angle) and tibial plateau (medial tibial plateau slope, lateral tibial plateau slope, and medial tibial plateau depth) were independently measured by two radiologists for each of the patients. Intraclass correlation coefficient (ICC) values were calculated to assess the reliability of the measurements. Variables with acceptable ICC values were included in the final logistic regression model, but the remaining were only reported descriptively.
Results
There was good to excellent agreement between the radiologist in the measurement of ICNW and TCW. However, the agreement between the radiologists was not acceptable for the rest of the variables. The univariate logistic regression model showed as ICNW decreases, the risk of ACL injury increases (OR = 0.12, 95% CI [0.02, 0.60], p = 0.01).
Conclusions
Our results suggest that ICNW and TCW are the only geometric features of the tibiofemoral joint that can be reliably measured on conventional knee MRI. Moreover, decreased ICNW is associated with an increased risk of ACL injury.
Keywords: Anterior cruciate ligament injuries, Risk factor, Tibia, Tibial plateau, Femur, Intercondylar notch, Reliability of results
1. Introduction
The anterior cruciate ligament (ACL) injury is most commonly encountered in young athletes [26]. The treatment of ACL injury is not always absolutely successful. A recent systematic review and meta-analysis has reported that only about 50% of injured athletes return to their pre-injury sports activity after ACL reconstruction surgery [2]. It has also been proposed that osteoarthritis has a 3-fold increased prevalence among patients treated with reconstruction surgery than healthy unaffected populations [3]. Accordingly, identifying the risk factors of ACL injury, which can possibly result in developing preventive measures, can be of great value.
The geometric features of tibial plateau (medial tibial plateau slope, lateral tibial plateau slope, medial tibial plateau depth) and the geometric features of the distal part of the femur (intercondylar notch width, transcondylar width, and intercondylar notch angle) are among the most commonly studied anatomic risk factors [20], [21]. To the best of our knowledge, most of the studies published on this topic have shown that the risk of ACL injury increases as ICNW decreases [4], [5], [6], [10], [17], [27]. However, discrepant data have been reported in the literature regarding the remainder of the geometric variables [8], [10], [11], [12], [17], [18], [24]. It remains unclear why the reported data have been so discrepant.
Different studies have used different techniques for the measurement of these geometric variables. More importantly, not enough attention has been paid to the evaluation of the reproducibility of these measurements. We designed a retrospective case-control study with two main purposes. First, to evaluate the reproducibility of the geometric measurements of tibiofemoral joint on conventional knee MRI (since possible limitations in reproducibility of these measurements can be an explanation for the observed discrepancies). Second, to evaluate the impact of these geometric features on the risk of ACL injury.
2. Materials and methods
2.1. Study design and setting
This retrospective case-control study was conducted in a tertiary care center northwest of (blinded for review process). The study was approved by our local institutional review board (IRB) (approval No. blinded for review process) and was conducted in accordance with the declaration of Helsinki.
3. Participants
3.1. Case group
We extracted the medical records of the patients who had undergone surgical reconstruction of the ACL in our center between April 2015 and April 2021. We reviewed the medical histories of all these patients, and consecutively selected those with non-contact mechanism of ACL injury. Knee MRIs of the selected patients were then extracted and reviewed. Patients having any fracture or any degree of osteoarthritic changes on knee MRIs, and also those patients in whom the length of the depicted part of the femur or tibia was less than 5 cm on MRIs were excluded (since at least 4–5 cm of the length of the femur and tibia was needed to be able to draw the longitudinal axis of these bones). Finally, 143 records met the criteria above, from which we randomly selected 60 patients and entered them into the case group of the study (random selection was performed by simple computer-based random number generation).
3.2. Control group
We searched the MRI directory of our radiology department to track down knee MRIs that had received normal code between April 2015 and August 2020 in our center (MRIs without any remarkable findings are saved with a specific code in our center). The exclusion criteria were identical to the exclusion criteria for the case group. Finally, a large number of records met the criteria above, from which we randomly selected 60 normal controls.
3.3. MRI acquisition
The Knee joint MRIs were performed on an 8-channel 1.5-T system (Siemens MAGNETOM Avanto). Knees were in feet first position, full extension, and 15 degrees external rotation. MRIs were acquired in accordance with the routine knee MRI protocol in our center: Proton Density images in transverse, coronal, and sagittal planes (TR: 3000 ms, TE: 10 ms, slice thickness: 3 mm, inter-slice gap: 0 mm, FOV: 180 mm, acquisition time: 2 min 2 s); T2-weighted images in sagittal plane (TR: 4000 ms, TE: 93 ms, slice thickness: 3.5 mm, inter-slice gap: 1.4 mm, FOV: 180 mm, acquisition time: 1 min 54 s); T1-weighted images in Sagittal plane (TR: 426 ms, TE: 14 ms, slice thickness: 4 mm, inter-slice gap: 0.8 mm, FOV: 234 mm, acquisition time: 2 min 15 s).
3.4. Variables and measurements
We aimed to evaluate six variables (medial tibial plateau slope (MTPS), lateral tibial plateau slope (LTPS), medial tibial plateau depth (MTPD), intercondylar notch angle (INA), intercondylar notch width (ICNW), and transcondylar width (TCW)) as possible predictors of ACL injury. The measuring method of the each of variables was as follows:
3.5. Measurements pertaining to tibial plateau
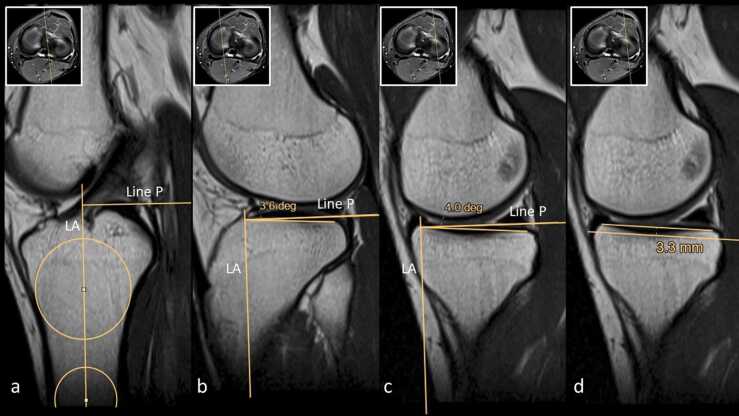
The anatomic variables of tibial plateau (MTPS, LTPS, and MTPD) were measured using a method similar to that of Hashemi et al. [7]. First of all, we used the most proximal axial cut of the tibia as a scout image and identified the sagittal cut which passed through the center of the tibia plateau (Fig. 1). On this sagittal cut, we draw two circles, centers of which were at least 4 cm apart and were connecting the anterior and posterior cortices of the proximal tibia. The line that connected the centers of these two circles was called the longitudinal axis of proximal tibia. Another line (line p) was drawn perpendicular to the longitudinal axis of proximal tibia. Using the axial scout image, we identified the sagittal cuts which passed through the centers of the medial and lateral articulation surfaces of tibia. Line p was reproduced on each of these sagittal images. Then a line was drawn on each of these sagittal images connecting the anterior and posterior peak points of the tibial plateau. The angle formed between the line p and the lines connecting the peak points of the medial and lateral tibial plateau was called MTPS and LTPS, respectively. To measure the depth of the concavity of the medial tibial plateau, we used the same sagittal image in which MTPS was measured. We draw the line connecting the anterior and posterior peak points of the medial tibial plateau. Then we drew another line which was parallel to this line and was touching the floor of the concavity of the medial tibial plateau. The distance between these two parallel lines was recorded as medial tibial plateau depth.
Fig. 1.
Measurement of the medial and lateral tibial plateau slopes (MTPS, LTPS) and medial tibial plateau depth (MTPD). Using the most proximal axial image of the tibia as a scout image (white boxes), sagittal cuts running through (a) center of the tibial plateau, (b) center of the lateral and (c, d) medial articulation surfaces of tibial plateau were identified. (a) On the sagittal cut running through the center of the tibial plateau, two circles were drawn, which were connecting the anterior and posterior cortices of the proximal tibia and centers of which were at least 4 cm apart. The line connecting the centers of these two circles was drawn and called longitudinal axis (LA) of proximal tibia. Then line P was drawn perpendicular to the longitudinal axis of the tibia. Line P was reproduced on the (b) lateral and (c, d) medial sagittal cuts. On each of these sagittal cuts, anterior and posterior peak pints of tibial plateau were connected using a line. The angles formed between these lines and line P were called (b) LTPS and (c) MTPS. On the medial sagittal cut (d) a new line which was touching the floor of the concavity of the medial tibial plateau and was parallel to the line connecting the anterior and posterior peak points was drawn. The distance between these two parallel lines was measured and recorded as medial tibial plateau depth.
3.6. Measurements pertaining to the distal part of femur
The INA was measured according to the method described by Bouras et al. [4]. The sagittal cut of the femur in which the roof of the intercondylar notch was entirely depicted was chosen (Fig. 2). A line passing parallel to the roof of the intercondylar notch (Blumensaat line) and the line representing the longitudinal axis of the femur were drawn, and the angle formed between these two lines was recorded as INA. The line representing the longitudinal axis of the femur was identified by connecting the centers of the two circles, which were connecting the anterior and posterior cortices of the femur and were at least 4 cm apart.
Fig. 2.
Measurement of the intercondylar notch angle (INA). The sagittal image of the femur in which the roof of the intercondylar notch was entirely depicted was chosen. The longitudinal axis (LA) of femur was identified by connecting the centers of the two circles, which were connecting the anterior and posterior cortices of the femur and were at least 4 cm apart. The line passing parallel to the roof of the intercondylar notch (line B) was drawn. The angle formed between line A and line B was recorded as intercondylar notch angle.
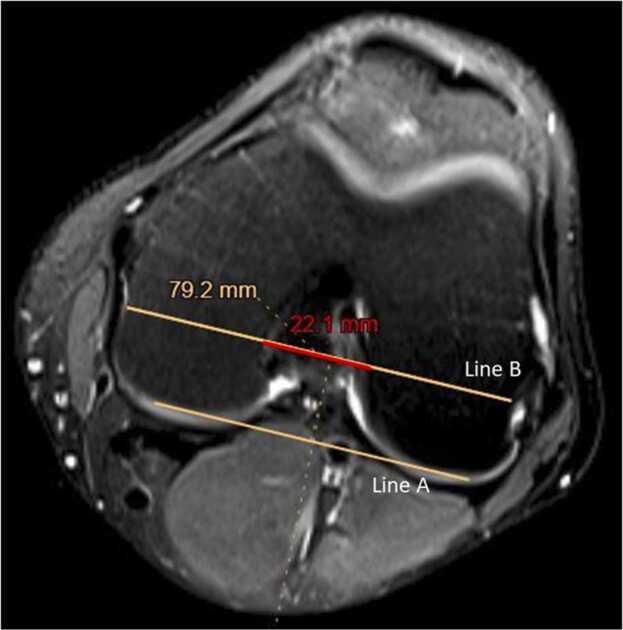
The ICNW and TCW were measured according to the method described by Herzog et al. [9] and Souryal et al. [23]. First, we chose the transverse cut of the femur in which the popliteal groove was fully depicted (Fig. 3). In this transverse image, we draw a line connecting the anterior peaks of the condyles of the femur. Then we draw another line parallel to this line, which passed through the center of the popliteal groove. As shown in Fig. 3, the length of this line was recorded as TCW. Then the ICNW was measured on the same line as shown in Fig. 3. We calculated the intercondylar notch width index (NWI) by dividing the ICNW by the TCW.
Fig. 3.
Measurement of the transcondylar width (TCW) and Intercondylar notch width (ICNW). The transverse cut of the femur in which the popliteal groove was fully depicted was chosen. On this transverse cut, the line that connected the anterior peak points of the femur condyles was drawn (line A). Another line (line B), which was parallel to line A and was passing through the center of the popliteal groove was drawn. The total length of line B was recorded as transcondylar width (TCW). The intercondylar notch width (ICNW) was also measured on line B.
3.7. Interobserver agreement
Each of the measurements were taken independently by two radiologists (both with at least 10 years of experience in general radiology and MRI). The radiologists were blinded to the gender and age of the patients but were aware of the hypotheses of the study and also the fact that discrepant data existed in the literature regarding the direction and magnitude of the correlations. We performed intraclass correlation coefficient (ICC) analysis to assess the inter-observer agreement of the measurements. ICC values were interpreted as described by Koo et al. [13].
3.8. Statistical analysis
Variables having acceptable ICC values in their measurements were included in the final logistic regression model. Those variables which failed to show acceptable ICC values were only reported descriptively and were not entered into the final model. All statistical analyses were performed using SPSS (IBM Corp, Armonk, NY). P-values less than 0.05 were considered statistically significant.
4. Results
A total number of 60 cases (34 men, 26 women; mean age 34.1 ± 13.65 SD) and 60 controls (31 men, 29 women; mean age 36.30 ± 11.46 SD) were included in the study. Baseline characteristics of the patients are shown in Table 1. There was no significant difference between the case and control groups regarding age, gender, and side of the affected knee. ACL injuries had occurred with non-contact mechanisms (during sports or non-sports activities) in all patients. MRIs of both knees were available for nine patients in the case group (in 2 of the opposite side knees, ACL was torn, and in 3 of them, ACL was reconstructed) and for three patients in the control group (none of them had an ACL injury in the opposite knee). Mean values measured for each of the variables have been summarized in Table 2 (All of the measurements were taken by two radiologists and we have reported the mean of the two radiologists).
Table 1.
Baseline characteristics of the subjects.
| ACL-injured | Control | P-value | |
|---|---|---|---|
| patients (N) | 60 | 60 | |
| Age | 0.14a | ||
| Range | 18–75 | 20–70 | |
| Mean | 34.10 | 36.30 | |
| SD | 13.65 | 11.46 | |
| Gender N (%) | 0.35b | ||
| Men | 34 (56) | 31 (51) | |
| Women | 26 (43) | 29 (48) | |
| Affected knee N (%) | 0.28b | ||
| Right | 37 (61) | 33 (55) | |
| Left | 23 (38) | 27 (45) |
Mean values were compared using Mann–Whitney U test.
P-value was calculated using Fisher's Exact Test.
Table 2.
Summary results Mean (SD).
| ACL status (N) | INA (degrees) | ICNW (cm) | TCW (cm) | NWI | MTPS (degrees) | MTPD (mm) | LTPS (degrees) |
|---|---|---|---|---|---|---|---|
| Injured ACL (60) | 37.71 (4.03) | 2.16 (0.22) | 7.22 (0.59) | 0.29 (0.02) | 3.81 (2.24) | 2.35 (0.87) | 5.16 (3.91) |
| Intact ACL (60) | 39.30 (3.79) | 2.27 (0.24) | 7.17 (0.55) | 0.31 (0.03) | 4.77 (2.55) | 1.90 (0.81) | 3.93 (3.26) |
| P-value | 0.02 | 0.008 | 0.58 | 0.001 | 0.03 | 0.005 | 0.06 |
INA: Intercondylar Notch Angle, NWI: Intercondylar Notch Width Index, MTPS: Medial Tibial Plateau Slope, MTPD: Medial Tibial Plateau Depth, LTPS: Lateral Tibial Plateau Slope, CTPS: Coronal Tibial Plateau Slope
5. Interobserver agreement
As shown in Table 3, there was good to excellent agreement between the radiologist in measuring the ICNW and TCW. However, the agreement between the two radiologists was not acceptable for the rest of the variables. This indicated that values recorded for INA, LTPS, MTPS, and MTPD were not reliable. Hence, we only reported these values descriptively without entering them to the final logistic regression model. However, values recorded for ICNW (and its correlations: TCW, NWI) proved reliable and were entered into the final analysis.
Table 3.
Assessment of reliability of the measurements (interobserver agreements).
| INA | ICNW | TCW | MTPS | MTPD | LTPS | |
|---|---|---|---|---|---|---|
| ICC value | 0.49 | 0.90 | 0.92 | 0.64 | 0.71 | 0.68 |
| 95% CI | 0.27–0.64 | 0.86–0.93 | 0.89–0.94 | 0.48–0.75 | 0.59–0.80 | 0.54–0.77 |
| Interpretation of reliabilitya | Poor to moderate | Good to excellent | Good to excellent | Poor to good | Moderate to good | Moderate to good |
Interpreted as described by Koo et al. [23], ICC: Intra Class Correlation, CI: Confidence Interval.
6. The final univariate logistic regression model
A simple logistic regression model was constructed to see if ICNW is a predictor of ACL injury. This model showed that as ICNW decreases, the risk of ACL injury increases (OR = 0.12, 95% CI [0.02, 0.60], p = 0.01). The goodness-of-fit of the model was evaluated using the Receiver Operating Characteristics (ROC) analysis in which the area under the curve (AUC) was 0.63 (95% CI [0.53, 0.73], p = 0.01).
We repeated the simple logistic regression analysis by replacing the ICNW with the NWI and TCW in the model. NWI was also negatively correlated with ACL injury (p = 0.003), but TCW was not correlated with ACL injury (p = 0.58).
7. Discussion
In the present study, the main objective was to evaluate the reliability of measuring the geometric features of tibiofemoral joint on conventional knee MRIs. Accordingly, the main finding of the study was that ICNW and TCW are the only geometric features of the tibiofemoral joint that can be reliably measured on conventional knee MRI.
To the best of our knowledge, two main methods have been described in the literature to identify the longitudinal axis of tibia [7], [11]. Using the first method [7], centers of the proximal tibia have to be identified on the mid-sagittal section of the tibia in two separate points which are at least 4 cm apart along the longitudinal axis of the tibia (in the original method, these two central points are the centers of the two horizontal lines which are connecting the anterior and posterior cortices of the proximal tibia and are at least 4 cm apart). Accordingly, the line connecting these two points is designated as the longitudinal axis of the proximal tibia. Using the second method [11] two circles have to be drawn in the proximal portion of the tibia (the proximal circle touching the anterior, posterior, and superior cortices of the proximal tibial and the distal circle touching the anterior and posterior cortices of the proximal tibial while its center lying on the circumference of the proximal circle). Accordingly, the line connecting the centers of these two circles is designated as the longitudinal axis of the proximal tibia. In the present study, the longitudinal axis of the tibia was identified using a method similar to the first method described. In the present study, the two central points along the longitudinal axis of the tibia were identified by drawing two circles lying at least 4 cm apart and touching the anterior and posterior cortices of the proximal tibia.
Our results showed that tibiofemoral joint geometrics (INA, ICNW, TCW, MTPS, LTPS, and MTPD) cannot be reliably measured on conventional knee MRI except for ICNW and TCW. We suspect the limitations observed in the reliability of the measurements might have originated from several issues: First, selecting the central cut of the tibial plateau (or the mid articular cuts) is prone to subjectivity. In many cases, a radiologist cannot decide which cut precisely runs through the center of the tibial plateau. Usually, two adjacent cuts can be chosen since both of them seem to be running through the center. Second, bone cortex (low signal on MRI) does not have clear-cut boundaries. Hence determining the exact points at which the circles or lines touch the cortex is substantially prone to subjectivity. Slight differences in the exact location of the circles or lines drawn make 1–2 degrees of mismatch between the final angles measured, which is enough to revolutionize the final results.
Another possible explanation for the observed limitations in the inter-rater reliability could be that the measurements had been implemented improperly by one of the radiologists in the present study. To rule out this possibility, we randomly selected 40 patients (20 cases and 20 controls), and each of the radiologists performed the measurements for a second time on these patients to evaluate the intra-rater reliability of the measurements. Intra-rater reliabilities, concordant to the inter-rater reliabilities, were unacceptable for INA, MTPS, LTPS, and MTPD but were excellent for ICNW and TCW. These results strengthened the possibility that the observed limitations in the reliability of the measurements, at least in part, had originated from the methodology described in the literature, per se. Moreover, it can be proposed that both approaches introduced in the literature for measuring the geometric features of the tibiofemoral joint on conventional MRI are prone to the aforementioned subjectivities, and choosing one over the other will not alter the reproducibility of the measurements.
Besides the reliability, the validity of the measurements has to be also taken into account. Although there is paucity of research evaluating the validity of these two methods, the reason why we chose to use the first method, described above, was that this method seemed to be more valid for identification of the longitudinal axis of the proximal tibia (simply because more length of the bone is used to estimate the real longitudinal axis of proximal tibia compared to the second method which relies on just a small portion of the proximal tibia).
The association between tibial plateau geometrics (MTPS, LTPS, MTPD) and the risk of ACL injury has been a controversial subject in the literature. Both decreased and increased MTPS, LTPS, MTPD have been proposed to be associated with increased risk of ACL injury [8], [11], [12], [14], [17], [18], [24]. Also, there are studies suggesting no association [10]. We suspect that this controversy may have arisen, at least in part, from the limitations in the reliability of the measurements on conventional knee images.
Second major finding of our study was that decreased ICNW (or index) is associated with increased risk of ACL injury (OR = 0.12, 95% CI [0.02, 0.60], p = 0.01). This finding is in concordance with the results of several previous studies evaluating the association between ICNW and the risk of ACL injury on knee radiograph [15], [16], [22], [25], computed tomography (CT) scan [1], and MRI [4], [5], [6], [10], [17], [18]. A possible explanation can be that ACL is more prone to impingement in narrower intercondylar notch of femur.
State-of-the-art technology, 3D imaging, and artificial intelligence may be beneficial in this area. By using conventional MRI and conventional measurement techniques, we rely on just a single sagittal cut to determine the longitudinal axis of tibia or femur. Tibial slopes are also determined in just a single sagittal cut. It is feared that the longitudinal axes and slopes determined on a limited number of cuts would not represent the real axes and slopes. To the best of our knowledge, only one study has based its evaluations on 3D visualization of the tibia and femur [19]. They have determined the longitudinal axis of tibia by automated detection of the centroids of the tibia on multiple transverse cuts; also, the tibial plateau slopes by automated detection of the overall axis of the entire subchondral surface of tibial plateau. The authors of this study have finally concluded that decreased ICNW and increased LTPS can be potential risk factors for ACL injury [19]. Future studies on this topic should adopt 3D imaging methods and artificial intelligence to potentially improve the reliability and validity of measurements.
The present study had several limitations, the most important probably being the small sample size, which prevented us from performing subgroup analyses based on age and gender. The second limitation was the retrospective design of the study. All the knee MRIs were acquired using routine knee protocol in our center; however, in a prospectively designed study, MRI acquisition protocol could be specified to permit depiction of more length of the bones. The third limitation was that we were not able to collect more detailed information regarding the participants' body mass index (BMI), and type and level of sports activities.
In conclusion, our study suggests that intercondylar notch width (ICNW) and transcondylar width (TCW) of the femur are the only geometric features of the tibiofemoral joint that can be reliably measured on conventional knee MRI. Moreover, decreased ICNW is associated with an increased risk of ACL injury.
Ethics
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Tabriz University of Medical Sciences (IRB approval No. IR.TBZMED.REC.1399.872).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
All three authors (Ali Akhavi Milani, Mina Motallebzadeh, Masoud Mahmoudpour) contributed substantially to all aspects of this research including Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Validation, Writing − original draft, Writing − review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
References
- 1.Anderson A.F., Lipscomb A.B., Liudahl K.J., Addlestone R.B. Analysis of the intercondylar notch by computed tomography. Am. J. Sports Med. 1987;15:547–552. doi: 10.1177/036354658701500605. [DOI] [PubMed] [Google Scholar]
- 2.Ardern C.L., Webster K.E., Taylor N.F., Feller J.A. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br. J. Sports Med. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 3.Barenius B., Ponzer S., Shalabi A., Bujak R., Norlen L., Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am. J. Sports Med. 2014;42:1049–1057. doi: 10.1177/0363546514526139. [DOI] [PubMed] [Google Scholar]
- 4.Bouras T., Fennema P., Burke S., Bosman H. Stenotic intercondylar notch type is correlated with anterior cruciate ligament injury in female patients using magnetic resonance imaging. Knee Surg. Sports Trauma. Arthrosc. 2018;26:1252–1257. doi: 10.1007/s00167-017-4625-4. [DOI] [PubMed] [Google Scholar]
- 5.Domzalski M., Grzelak P., Gabos P. Risk factors for Anterior Cruciate Ligament injury in skeletally immature patients: analysis of intercondylar notch width using Magnetic Resonance Imaging. Int Orthop. 2010;34:703–707. doi: 10.1007/s00264-010-0987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernández-Jaén T., López-Alcorocho J.M., Rodriguez-Iñigo E., Castellán F., Hernández J.C., Guillén-García P. The importance of the intercondylar notch in anterior cruciate ligament tears. Orthop. J. Sports Med. 2015;3 doi: 10.1177/2325967115597882. 2325967115597882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hashemi J., Chandrashekar N., Gill B., Beynnon B.D., Slauterbeck J.R., Schutt R.C., Jr., et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J. Bone Jt. Surg. Am. Vol. 2008;90:2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hashemi J., Chandrashekar N., Mansouri H., Gill B., Slauterbeck J.R., Schutt R.C., Jr., et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am. J. Sports Med. 2010;38:54–62. doi: 10.1177/0363546509349055. [DOI] [PubMed] [Google Scholar]
- 9.Herzog R.J., Silliman J.F., Hutton K., Rodkey W.G., Steadman J.R. Measurements of the intercondylar notch by plain film radiography and magnetic resonance imaging. Am. J. Sports Med. 1994;22:204–210. doi: 10.1177/036354659402200209. [DOI] [PubMed] [Google Scholar]
- 10.K S, Chamala T., Kumar A. Comparison of anatomical risk factors for non-contact anterior cruciate ligament injury using magnetic resonance imaging. J. Clin. Orthop. Trauma. 2019;10:143–148. doi: 10.1016/j.jcot.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan M.S., Seon J.K., Song E.K. Risk factors for anterior cruciate ligament injury: assessment of tibial plateau anatomic variables on conventional MRI using a new combined method. Int Orthop. 2011;35:1251–1256. doi: 10.1007/s00264-011-1217-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kızılgöz V., Sivrioğlu A.K., Ulusoy G.R., Aydın H., Karayol S.S., Menderes U. Analysis of the risk factors for anterior cruciate ligament injury: an investigation of structural tendencies. Clin. Imaging. 2018;50:20–30. doi: 10.1016/j.clinimag.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Koo T.K., Li M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016;15:155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar Panigrahi T., Das A., Mohanty T., Samanta S., Kumar Mohapatra S. Study of relationship of posterior tibial slope in anterior cruciate ligament injury. J. Orthop. 2020;21:487–490. doi: 10.1016/j.jor.2020.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LaPrade R.F., Burnett Q.M., 2nd Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am. J. Sports Med. 1994;22:198–202. doi: 10.1177/036354659402200208. discussion 203. [DOI] [PubMed] [Google Scholar]
- 16.Shelbourne K.D., Davis T.J., Klootwyk T.E. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. Am. J. Sports Med. 1998;26:402–408. doi: 10.1177/03635465980260031001. [DOI] [PubMed] [Google Scholar]
- 17.Shen L., Jin Z.G., Dong Q.R., Li L.B. Anatomical risk factors of anterior cruciate ligament injury. Chin. Med J. (Engl. ) 2018;131:2960–2967. doi: 10.4103/0366-6999.247207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shen X., Xiao J., Yang Y., Liu T., Chen S., Gao Z., et al. Multivariable analysis of anatomic risk factors for anterior cruciate ligament injury in active individuals. Arch. Orthop. Trauma Surg. 2019;139:1277–1285. doi: 10.1007/s00402-019-03210-x. [DOI] [PubMed] [Google Scholar]
- 19.Simon R.A., Everhart J.S., Nagaraja H.N., Chaudhari A.M. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J. Biomech. 2010;43:1702–1707. doi: 10.1016/j.jbiomech.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith H.C., Vacek P., Johnson R.J., Slauterbeck J.R., Hashemi J., Shultz S., et al. Risk factors for anterior cruciate ligament injury: a review of the literature-part 2: hormonal, genetic, cognitive function, previous injury, and extrinsic risk factors. Sports Health. 2012;4:155–161. doi: 10.1177/1941738111428282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith H.C., Vacek P., Johnson R.J., Slauterbeck J.R., Hashemi J., Shultz S., et al. Risk factors for anterior cruciate ligament injury: a review of the literature - part 1: neuromuscular and anatomic risk. Sports Health. 2012;4:69–78. doi: 10.1177/1941738111428281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Souryal T.O., Freeman T.R. Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. Am. J. Sports Med. 1993;21:535–539. doi: 10.1177/036354659302100410. [DOI] [PubMed] [Google Scholar]
- 23.Souryal T.O., Moore H.A., Evans J.P. Bilaterality in anterior cruciate ligament injuries: associated intercondylar notch stenosis. Am. J. Sports Med. 1988;16:449–454. doi: 10.1177/036354658801600504. [DOI] [PubMed] [Google Scholar]
- 24.Stijak L., Herzog R.F., Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg. Sports Trauma. Arthrosc. 2008;16:112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 25.Uhorchak J.M., Scoville C.R., Williams G.N., Arciero R.A., St, Pierre P., Taylor D.C. Risk factors associated with non-contact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am. J. Sports Med. 2003;31:831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 26.Ytterstad K., Granan L.-P., Ytterstad B., Steindal K., Fjeldsgaard K.A., Furnes O., et al. Registration rate in the Norwegian Cruciate Ligament Register: large-volume hospitals perform better. Acta Orthop. 2012;83:174–178. doi: 10.3109/17453674.2012.678800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zeng C., Gao S.G., Wei J., Yang T.B., Cheng L., Luo W., et al. The influence of the intercondylar notch dimensions on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg. Sports Trauma. Arthrosc. 2013;21:804–815. doi: 10.1007/s00167-012-2166-4. [DOI] [PubMed] [Google Scholar]