Abstract
Assisted Living (AL) has become an important residential long-term care option in the US, yet very little is known about the nature and quality of care received in this setting by racial/ethnic minorities or residents dually eligible for Medicare and Medicaid. Using calendar year 2018 Medicare data, we identified 255,564 fee-for-service Medicare beneficiaries age 55+ who resided in 24,108 ALs across the US. We fit several logistic regression models with individual-level covariates and AL-level fixed effects, to examine the association between race/ethnicity and dual status with inpatient hospital admission, 30-day readmission, emergency room use, and nursing home placement. Significant variations in these measures were found both within and across ALs for racial/ethnic minority and dual residents. Our results suggest that disparities in outcomes are most significant by dual eligibility status rather than by race/ethnicity alone. These findings provide important implications for providers, policy-makers, and researchers.
Keywords: disparities, race/ethnicity, duals, assisted living
INTRODUCTION
Long-term care in the United States has been undergoing a transformation marked by a shift from care provided in nursing homes (NH) to home and community-based services (HCBS). This has included a rapid growth of assisted living (AL) communities, which while designed to fill the gap between independent living and NH care now serve an increasingly frail population of residents, most age 85+, with multiple co-morbidities, and functional/cognitive impairments. Most AL residents are relatively affluent, and AL communities tend to predominantly serve white residents who are not Medicaid-eligible. (Harris-Kojetin et al., 2019) Today, African-Americans remain largely under-represented in ALs, but there is a significant variation across communities.(Fabius & Thomas, 2019; Howard et al., 2002) As the demographics of older Americans change, and with states rebalancing long-term care from institutional to HCBS, these trends have been changing and are likely to continue evolving. In 2014, Medicaid spent over $10 billion (federal and state) on AL services in 48 states.(GAO, 2018) Currently, over 16% of AL residents rely on Medicaid for support with daily care services and almost half of ALs are Medicaid certified.(Harris-Kojetin et al., 2019) The share of AL residents who are Medicare-Medicaid dually eligible varies significantly by state – from 6% in New Hampshire to 40% in New York.(Fabius, Cornell, Zhang, & Thomas, 2021)
ALs are regulated only at the state level, and such regulations and their stringency vary substantially.(Temkin-Greener, Mao, et al., 2020) As a result, there is no uniform collection of data on AL residents or the communities in which they live, and very little is known about the nature and quality of care received by racial/ethnic minorities or by dual AL residents.
Unlike NHs, ALs provide very limited personal care and health services, but the use of health services and residents’ outcomes can be influenced by AL practices and policies. Several studies have identified hospital admissions and readmissions, emergency room (ER) use, and nursing home placement as key quality indicators that are relevant to AL residents and may be influenced by the environment in which they reside. (Bartley, Quigg, Chandra, & Takahashi, 2018; Hogan et al., 2014; Hua et al., 2020; Mor, Thomas, & Rahman, 2018)
Prior research on these measures is scant, has relied largely on survey data or convenience samples, and the results have not always been consistent. (Phillips et al., 2003; Zimmerman, Cohen, Washington, Ward, & Giorgio, 2016) For example, based on AL staff surveys conducted in four states, hospitalization rates of 46%−51% per year were reported.(Zimmerman et al., 2005) A study based on the 2010 National Survey of Residential Care Facilities found 24% of residents to have had a hospital admission in a prior year.(Gimm & Kitsantas, 2016) Others have reported rates ranging from 39% to 48%.(Bartley et al., 2018; Hogan et al., 2014) Wide variations have also been reported in ER use and in 30-day readmissions likely due to both the diversity of AL communities nationally,(Hua et al., 2020) and to the differences in data collection. (Bartley, Quigg, Chandra, & Takahashi, 2018; Caffrey, Harris-Kojetin, Rome, & Schwartz, 2018)
While such variations may be expected to differentially affect racial/ethnic minorities and dual AL residents, empirical evidence in these regards is largely lacking. Studies have shown that compared to white older adults, black older adults are less likely to move into ALs (Morales & Robert, 2020), but when they do, they tend to reside in smaller communities located in rural areas, with lower ratings, for example for cleanliness and maintenance.(Howard et al., 2002) A recent, large national study showed that black Medicare beneficiaries who reside in AL account for 5% of all residents, are younger, disproportionately dually eligible, and have higher levels of acuity compared to white AL residents.(Fabius & Thomas, 2019)
Motivated by these prior studies and by the existing gaps in the literature, we used national-level administrative and claims data representing all Medicare beneficiaries who resided in AL communities in calendar year (CY) 2018. Our objectives were to: 1) examine racial/ethnic and dual-eligibility differences in the use of healthcare services (inpatient hospital and ER) and in residents’ outcomes (30-day hospital readmission and NH placement); and 2) explore whether these differences exist across AL communities as well as within. Differences occurring within AL may be due to unequal treatment or differences in personal resource availability. Differences across ALs may signify disparities in access to high versus low quality communities. Disentangling the sources of disparities is important in identifying potential corrective actions.
New Contribution
This is the first national-level study to report on disparities in health care use and outcomes among AL residents. This study was made possible by the new methodology we have developed using 9-digit ZIP codes to identify Medicare beneficiaries residing in ALs and linking to their Medicare enrollment, claims and assessment data for CY2018. While prior AL research has shown some disparities across AL settings, (Fabius & Thomas, 2019) in this study we examined additional outcomes and decomposed disparities into within and across AL components by adding fixed effects for over 24,000 communities included in the analysis. We also focused on the extent to which the root cause of the observed disparities may be explained by socio-economic status, specifically dual eligibility, rather than by discriminatory practices based solely on race or ethnicity.
CONCEPTUAL MODEL
For this study, we adapted the conceptual framework proposed by Kilbourne and colleagues, which guides health disparities research along three dimensions: detection; identification of determinants; and disparities reduction. (Kilbourne, Switzer, Hyman, Crawley-Matoka, & Fine, 2007) We focused on the first two dimensions, following existing empirical evidence of disparities in quality of care among NH residents. Based on prior research (Rathore & Krumholz, 2004; United States Congress, 2003), we defined disparities as differences in health care use or outcomes, occurring between more and less vulnerable subgroups of the population, that are clinically observed and statistically significant.
In detecting differences, it is important to consider selection or illness severity, which can contribute to the observed but not always real quality differences. Nursing home research shows that minority residents, and those who are dually entitled to Medicaid and Medicare, tend to receive poorer care quality than whites or non-duals. (Konetzka & Werner, 2009; Mor, Zinn, Angelelli, Teno, & Miller, 2004) For example, minority individuals are more likely to reside in facilities with limited resources, fewer staff, and with more deficiency citations. (Feng, Fennell, Tyler, Clark, & Mor, 2011; Li et al., 2014; Li, Harrington, Mukamel, Cen, Cai, Temkin-Greener, 2015; Li et al., 2015; Mor et al., 2004) AL research also shows demographic and residential differences among black and white residents, with blacks more often being duals and concentrated in smaller communities with fewer white residents. (Fabius et al., 2021; Fabius & Thomas, 2019) Most studies reporting disparities in healthcare use and outcomes have focused on racial and ethnic groups, often neglecting to explore interaction with other factors such as socio-economic status. While only 5% of AL residents are black, almost 17% are dually eligible for Medicare and Medicaid. Thus, it is important to understand the extent to which disparities in care quality are due to racial/ethnic factors alone or to differences in dual status. We hypothesized that dual status may be associated with most, but not all observed disparities. While our conceptual model does not offer a test for root causes of disparities, it does identify where such disparities exist and what observable factors may be associated with these disparities.
Understanding disparities necessitates identifying determinants of gaps in care. Research focusing on NHs suggests that provider factors and practice patterns are important contributors. (Grabowski & McGuire, 2009) For example, dual NH residents tend to have higher rates of hospitalizations than private-pay residents within the same facility, because NHs are more financially incentivized to discharge duals, rather than private-pay residents, to hospitals even for potentially-avoidable conditions.(Cai et al., 2011) Compared to white NH decedents with dementia, blacks were shown to have a higher risk of end-of-life hospitalizations, occurring both within and across homes. (Temkin-Greener, Yan, Wang, & Cai, 2021) Thus disentangling the source of disparities in AL is important as different strategies are needed when disparities are due to unequal within-AL treatment as opposed to differences in care across ALs. Therefore, we also decomposed the source of disparities in health services use and outcomes among AL residents. This was an exploratory rather than a hypothesis-driven objective.
METHODS
Data Sources & Study Population
We employed multiple sources of CY2018-2019 data: national inventory of AL communities; Medicare Beneficiary Summary File (MBSF); Medicare Provider and Review (MedPAR); Minimum Data Set 3.0 (MDS); and Medicare outpatients claims. We also used publicly available Area Health Resource Files (AHRF) to identify county characteristics within which AL communities were located. Rural-Urban Commuting Area Codes (RUCA) were used to identify rural versus urban locations.
In a prior study, we catalogued AL communities in each state. Using the 9-digit ZIP codes associated with the physical address of each AL, we obtained Medicare beneficiary identification numbers from the Medicare enrollment database.(Temkin-Greener, Guo, Mao, Cai, & Li, 2020) For this study, we identified a cohort of fee-for-service (FFS) Medicare beneficiaries, age 55 or older who resided in ALs in CY2018. AL residents were linked to the Medicare data at the individual level. We limited our study cohort to residents 55+ because younger individuals do not represent the typical AL population. Since the information on chronic conditions for Medicare beneficiaries enrolled in the Medicare Advantage (MA) plans is not available in the MBSF, they were also excluded. We identified 266,766 Medicare FFS residents, age 55+ who resided in 24,990 ALs. After excluding ALs with missing bed sizes, and further limiting the sample to white, black or Hispanic residents, our analytical cohort included 255,564 individuals (95.8%) and 24,108 ALs (96.5%).
Variables
Four outcome measures were selected to serve as the dependent variables. For each resident, we identified the presence or absence of a short-stay acute inpatient admission, 30-day readmission (only for those with a prior index admission in CY2018), ER visit, and NH placement occurring in CY2018. Short-stay hospital stays were identified using MedPAR. ER visits resulting in a hospital stay were identified using MedPAR, and those not resulting in a hospitalization were identified using outpatient Medicare claims. Readmissions that occurred within 30 days of an index hospital admission, and were unplanned, were identified based on MedPAR and followed the established CMS methodology.(Horwitz, Partovian, Lin, Jerrin, & Grady, 2013) Placement in NHs was identified using the MDS and defined as custodial (long-term) if a stay was equal to or longer than 101 days.(RTI, 2016) To account for all readmissions that occurred following a CY2018 index hospitalizations, and for all NH stays with CY2018 admissions, we examined CY2019 MedPAR through the end of January, and the MDS through the end of April.
The key independent variables were residents’ race, ethnicity and dual eligibility status. Race was categorized as white (non-Hispanic) or black (non-Hispanic), and ethnicity as Hispanic or not, based on the validated RTI classification.(Jarrin, Nyandege, Grafova, Dong, & Lin, 2020) For those residing in AL in January of 2018, dual eligibility was based on the MBSF indicator for that month. For those entering AL during CY2018, dual status was based on the MBSF for the month of entry.
Individual-level covariates that may be associated with the outcome measures were defined as continuous, count or dichotomous, based on the three MBSF segments - base, chronic conditions and other chronic or potentially disabling conditions. These covariates included demographic factors (gender and age), number of chronic conditions, and presence of specific conditions such as cardiovascular disease, dementia, diabetes, mental illness (schizophrenia, psychosis, bipolar disorder), and others. For each outcome, we included a slightly different set of chronic conditions, based on previous literature that identified the most relevant risk factors.
AL community-level and county-level factors were also included. AL characteristics included AL size (categorized as small if <= 25 beds and “larger” otherwise), urban/rural location, and percent of residents who were black/Hispanic, categorized (based on the distribution) as no minorities (0%), low proportion of minorities (<32.8% of minorities) and high proportion of minorities (>=32.8% of minorities). We used AHRF to determine county-level factors such as population aged 65 or over and the percent of duals among population aged 65 or older. Herfindahl-Hirschman Index (HHI) for each county was calculated to measure AL competition, ranging from 0 to 1, with higher values indicating lower competition.
Analyses
Analyses were conducted at the resident level. We first compared, by race and ethnicity, all outcomes of interest and the individual characteristics. To investigate the relationship between race/ethnicity and dual status, with the outcomes of interest, we combined race/ethnicity and dual status into 6 groups: white-nondual (reference category); white-dual; black-nondual; black-dual; Hispanic-nondual; and Hispanic-dual. First, a simple logistic regression model was fit to examine the race/ethnicity and dual status differences in each outcome. Second, we fit a model that adjusted for individual-level covariates. Finally, for each outcome, we fit a model with individual-level factors and with AL-level fixed effects. Robust standard errors were estimated in these models to account for AL-level clustering. The effect of race/ethnicity and dual status estimated from the fixed-effect models represents the within-AL community differences in the risk of outcomes. The effects of race/ethnicity combined with dual status, were tested between the risk-adjusted and risk-adjusted fixed-effect models using the Wald statistics. If the AL effects are homogenous, meaning there are no across AL differences, then the estimates of the two models should not be statistically significantly different from each other. Otherwise, statistically significant differences indicate the existence of heterogeneity across AL communities.
Furthermore, we performed a separate linear regression to examine the relationship between facility/county characteristics and the percent of dual AL residents. All statistical analyses were performed with Stata version 14.2 (Stata Corporation, College Station, TX).
This study was reviewed and approved by the institutional review board.
RESULTS
Overall, blacks represent only 5.2% of AL residents and Hispanics account for 3.1% (Table 1). Unadjusted differences in the outcomes of interest between the racial/ethnic groups are statistically significant. The proportion of all residents who had any ER visits during the year was 47.5%, with blacks (46.4%) and Hispanics (41.9%) showing lower proportions than whites (47.8%). Similar relationship appears to have held for the percent of residents with any inpatient admission – 27.8% for whites, 25.8% for blacks, and 26.1% for Hispanics. However, with regard to NH placement, blacks showed a higher proportion (5.7%) compared to Hispanics (4.5%) and whites (3.9%). Hispanics had a higher proportion of 30 day-readmissions (6.4%), compared to whites (5.5%) and blacks (5.6%).
Table 1:
Characteristics of Assisted Living Medicare-Eligible Residents: By Residents’ Race and Ethnicity
| AL Residents | p-value | Total Sample | |||
|---|---|---|---|---|---|
| White | Black | Hispanic | |||
| Number of AL residents (%) | 234,287 (91.2) | 13,164 (5.2) | 8,113 (3.1) | 255,564 (100) | |
| Outcome Variables | |||||
| Pct. with any hospital admission | 27.8 | 25.8 | 26.1 | *** | 27.7 |
| Pct. with any ER visits | 47.8 | 46.4 | 41.9 | *** | 47.5 |
| Pct. NH placement (>100 days) | 3.9 | 5.7 | 4.5 | *** | 4.0 |
| Pct. with 30-day inpatient readmission | 5.5 | 5.6 | 6.4 | *** | 5.5 |
| Individual Characteristics | |||||
| Age (SD) | 83.7 (9.68) | 73.3 (10.52) | 75.8 (10.47) | *** | 82.9 (10.1) |
| Pct. female | 66.2 | 51.2 | 56.1 | *** | 65.1 |
| Pct. dually eligible | 13.9 | 47.5 | 47.9 | *** | 16.7 |
| No. chronic conditions (SD) | 14.60 (6.10) | 13.62 (8.00) | 13.43 (8.76) | *** | |
| Pct. diagnosed with: (1) | |||||
| Alzheimer’s disease & related dementias (ADRD) | 47.9 | 46.0 | 46.3 | *** | 47.7 |
| Chronic obstructive pulmonary disease (COPD) | 40.1 | 36.7 | 38.4 | *** | 39.8 |
| Congestive heart failure (CHF) | 47.4 | 42.3 | 40.6 | *** | 46.9 |
| Diabetes | 41.8 | 59.1 | 57.5 | *** | 43.2 |
| Mobility impairment | 11.1 | 17.5 | 11.8 | *** | 11.5 |
| Chronic kidney disease | 52.6 | 55.7 | 49.1 | *** | 52.6 |
| Hip fracture (in CY2018) | 3.0 | 0.8 | 1.4 | *** | 2.9 |
| Ischemic heart disease | 65.1 | 54.6 | 56.7 | *** | 64.3 |
| Rheumatoid arthritis | 78.7 | 58.1 | 61.6 | *** | 77.1 |
| Stroke (in CY2018) | 8.4 | 10.7 | 7.4 | *** | 8.5 |
| Anxiety/depression | 66.1 | 59.9 | 61.4 | *** | 65.6 |
| Mental illness (2) | 21.1 | 37.1 | 33.3 | *** | 22.3 |
| Obesity | 26.3 | 33.3 | 30.7 | *** | 26.8 |
| Peripheral vascular disease (PVD) | 49.4 | 46.5 | 45 | *** | 49.1 |
| Pressure ulcers (in CY2018) | 12.9 | 11.7 | 12.6 | *** | 12.8 |
| Cataracts | 83.6 | 54.5 | 58.9 | *** | 81.3 |
| Glaucoma | 33.1 | 31.1 | 28.1 | *** | 32.8 |
| Osteoporosis | 42.0 | 16.1 | 28.3 | *** | 40.3 |
| Anemia | 77.4 | 70.4 | 66.8 | *** | 76.7 |
| Hypertension | 90.4 | 86.2 | 79.7 | *** | 89.8 |
| Hypotension | 44.0 | 28.0 | 35.8 | *** | 42.9 |
| Epilepsy | 6.8 | 14.3 | 10.7 | *** | 7.3 |
| Visual impairment | 3.8 | 4.7 | 9.3 | *** | 4.1 |
| Atrial fibrillation | 31.1 | 13.7 | 14.8 | *** | 29.7 |
| Cancer (any) | 22.4 | 15.1 | 13.6 | *** | 21.8 |
| Drug abuse | 7.8 | 16.0 | 10.6 | *** | 8.3 |
Note:
p<0.01
p<0.05
p<0.1
Unless otherwise noted, chronic conditions refer to diagnoses ever recorded.
Schizophrenia, psychosis, bipolar disorders.
White AL residents tended to be substantially older than blacks or Hispanics (83.7 years on average versus 73.3 and 75.8, respectively). Significant variations between these groups also existed in the average number of chronic conditions and in specific diagnoses. For example, compared to whites, blacks and Hispanics were more likely to have diabetes (41.8% versus 59.1% and 57.5%) and mental illness (21.1% versus 37.1% and 33.3%), but they were less likely to have other conditions such as cancer, hypotension, or rheumatoid arthritis.
Blacks and Hispanics were three-fold as likely to be dual (47.5% and 47.9%, respectively) as whites (13.9%). The unadjusted outcomes, for combined race/ethnicity and dual status, are presented in Table 2. Compared to non-dual whites, non-dual blacks and Hispanics showed lower proportions of hospital admissions (26.8% versus 19.7% and 17.6%, respectively), but higher 30-day readmissions (16.9% versus 17.8% and 18.6%, respectively). Among duals, blacks had lower rates of hospitalizations but higher rates of 30 day readmissions than whites (32.5% vs. 33.9% and 20.9% vs 19.1%, respectively), while Hispanics experienced higher rates of hospital admissions and 30-day readmissions.
Table 2:
Unadjusted Outcomes (%) by Race/Ethnicity and Dual Status
| White Non-Dual | White Dual | Black Non-Dual | Black Dual | Hispanic Non-Dual | Hispanic Dual | Overall | |
|---|---|---|---|---|---|---|---|
| Number of AL residents (%) | 201,792 (78.9%) | 32,495 (12.7%) | 6,914 (2.7%) | 6,250 (2.5%) | 4,230 (1.7%) | 3,883 (1.5%) | 255,564 (100%) |
|
| |||||||
|
Outcome Variables
|
|||||||
| Pct. with any hospital admission |
26.8 | 33.9 | 19.7 | 32.5 | 17.6 | 35.3 | 27.7 |
| Pct. with any ER visits |
46.2 | 57.6 | 37.0 | 56.9 | 30.7 | 54.2 | 47.5 |
| Pct. NH placement (>100 days) |
3.0 | 9.1 | 2.8 | 8.8 | 1.8 | 7.4 | 4.0 |
| Pct. with 30-day inpatient readmission* | 16.9 | 19.1 | 17.8 | 20.9 | 18.6 | 24.5 | 17.5 |
Denominator is based on individuals with an index hospital stay
The fully adjusted effects of combined race/ethnicity and dual status on each outcome are presented in Figure 1, along with the Wald test results comparing the coefficient estimates (odds ratios, ORs) of models with and without fixed-effects. Full model results are available in supplementary Tables S1 and S2. Compared to white non-duals, black non-duals within the same AL experienced lower odds of inpatient admissions (OR=0.892; p<0.01), higher odds of NH placement (OR=1.355; p<0.01), and showed no difference in the risk of ER visits or 30-day readmissions. Hispanic non-duals showed no significant difference in any outcomes when compared to white non-duals within the same AL. There were largely no racial/ethnic differences in these outcomes across ALs among the non-duals.
Figure 1:
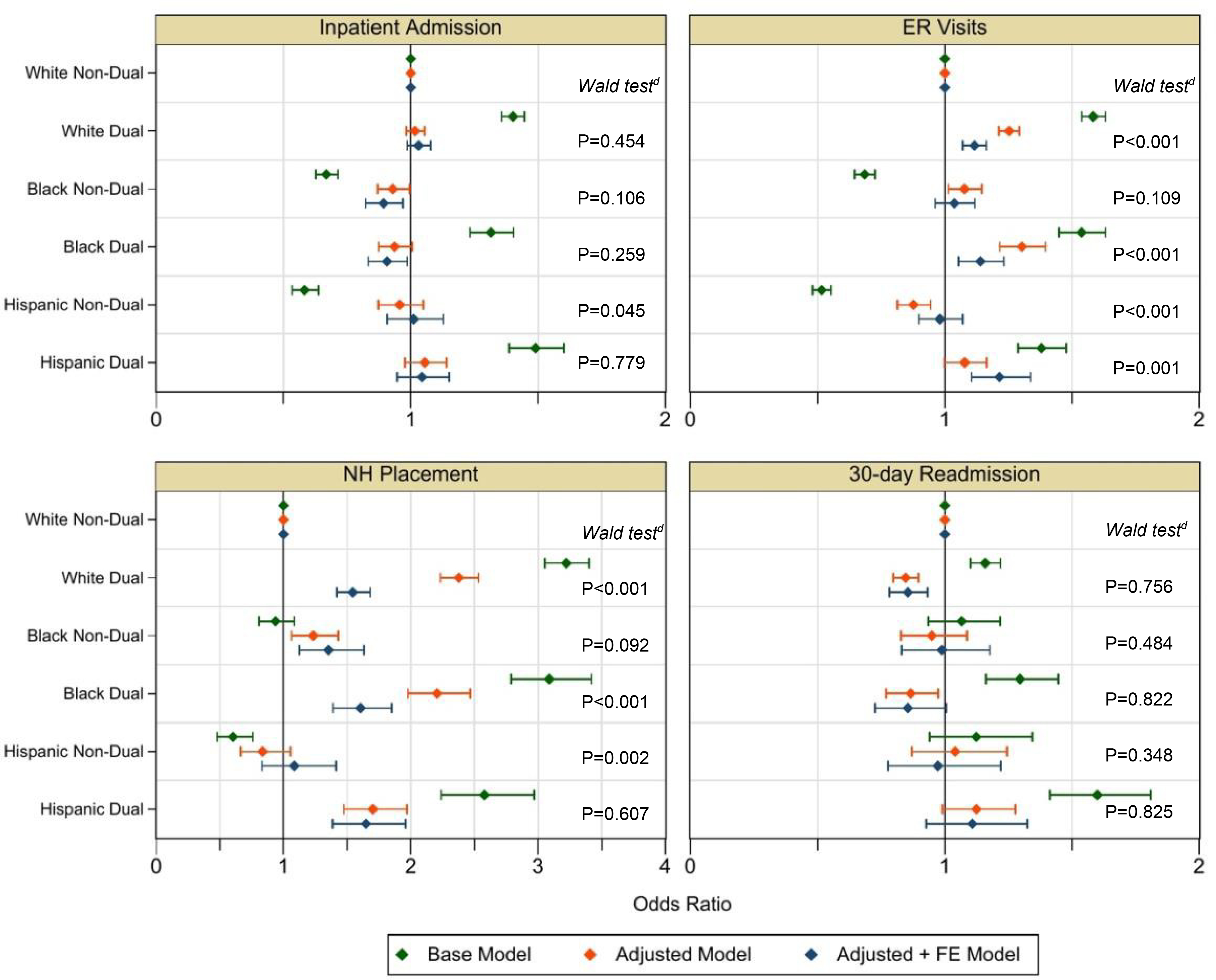
Adjusted Healthcare Outcomes: By Race/Ethnicity and Dual Status
Notes: Wald testd for the effect of race and dual eligibility status combined, comparing the adjusted models to adjusted with FE
The dually eligible had substantially higher likelihood of ER use than the non-duals regardless of race/ethnicity. In the same AL, white duals (OR=1.117; p<0.01), black duals (OR=1.140; p<0.01), and Hispanic duals (OR=1.215; p<0.01) had higher odds of ER visits relative to white non-duals. Inpatient admission risk was similar between duals and non-duals with one exception: black duals had 9.4% lower odds of inpatient admission relative to white non-duals (p<0.05). White and black duals had significantly lower odds of 30-day readmissions (OR=0.854; p<0.01 and OR=0.854; p<0.05, respectively), within the same AL, but the differences were not statistically significant across ALs. The odds of NH placement were substantially higher for all duals; 1.544 (p<0.01) for dual whites, 1.604 (p<0.01) for dual blacks, and 1.648 (p<0.01) for dual Hispanics, within the same ALs. For dual whites and dual blacks, but not for dual Hispanics, these differences persisted across ALs.
AL communities with higher proportions of dual residents were significantly different along a number of dimensions (Table 3). Compared to communities without any minority residents (67% of ALs), ALs with a low proportion of blacks or Hispanics (17%) had 9.48 percentage points (pp) more duals (β = 9.48; p<0.01) and those with a higher proportion of minorities (16%) had over 17 pp more duals (β = 17.21; p<0.01). AL communities with more beds were less likely to have duals (β = −2.65; p<0.01). AL communities with more dual residents were more likely to be in large or small rural locations (β = 7.37; p<0.01 and β =16.19; p<0.01, respectively), rather than in urban areas. The concentration of older duals (age 65+) in the county where the AL is located was associated with a higher proportion of duals within the AL (β = 0.56; p<0.01). Population aged 65 and older at the county level was negatively associated with the proportion of duals in AL communities (β = −0.59; p<0.01). Less competitive AL markets were also associated with greater concentrations of dual AL residents (β = −3.41; p<0.05).
Table 3:
Association of AL Community and County Characteristics with the Proportion of Dual Residents (N=24,945 ALs)
| Coefficient | |
|---|---|
| AL Characteristics | (SE) |
| Reference: No Black or Hispanic Residents in AL (N=16,659; 67%) | |
| Low proportion of black/Hispanic residents (N=4,197; 17%) | 9.48*** |
| (0.59) | |
| High proportion of blacks/Hispanic (N=4,089; 16%) | 17.21*** |
| (0.62) | |
| AL with >25 beds (ref: <=25 beds) | −2.65*** |
| (0.46) | |
| Large rural location (ref: urban) | 7.37*** |
| (0.80) | |
| Small rural location (ref: urban) | 16.19*** |
| (0.90) | |
| Population age =>65 per 100K | −0.59*** |
| (0.10) | |
| Percent of dually eligible population age =>65 | 0.56*** |
| (0.02) | |
| HHI | −3.41** |
| (1.40) | |
| Observations | 23,366 |
| R-squared | 0.096 |
SE = standard error; HHI= Herfindahl-Hirschman Index
p<0.01
p<0.05
p<0.1
DISCUSSION
Prior studies have shown that minority residents tend to live in different AL communities. (Fabius & Thomas, 2019) As suggested by our findings, this separation is exacerbated by dual status. In our study sample, 67% of ALs had neither black nor Hispanic residents. AL communities with higher proportions of minorities were disproportionately more likely to have dually eligible residents. These ALs were also more likely to be located in small rural areas and in counties with a higher proportion of duals among its older population. Our findings also demonstrate presence of both within and across AL differences in health outcomes occurring between residents who are dual and those who are not, but largely not by race/ethnicity alone.
Compared to non-dual whites, non-dual blacks had a slightly lower risk of inpatient admission within the same but not across ALs. This is perhaps not surprising, as black residents were on average 10 years younger than white residents. Whites were more likely to have conditions such as COPD, CHF, anemia, and osteoporosis, which very likely contribute to more frequent inpatient admissions. Although our models adjusted for these differences, it is likely that health status also differed in ways that were not fully accounted for due to data limitations. However, the risk of these outcomes increased substantially among the dually eligible, regardless of race/ethnicity, across most measures. Compared to white non-duals, white and Hispanic duals did not have higher odds of inpatient admissions, but duals across all race/ethnicity groups experienced higher rates of ER visits both within and across ALs. Duals of all race/ethnicity groups also had significantly greater risk of NH placement within ALs, and except for Hispanic-duals, also across ALs.
The within AL differences may be due to both individual-level differences and system-level disparities. At the individual-level, dual eligibility status may reflect health risks that were not sufficiently controlled for by the comorbidity covariates. It is also possible that duals face a greater challenge accessing additional personal care services that may help to prevent some ER visits or hospital admissions. While most ALs offer some level of assistance with personal care and medication management (in addition to other core services), the greatest variation appears to be in the intensity and frequency of personal care assistance that a community provides.(Hernandez, 2012) ALs that predominantly serve the dually eligible residents may have fewer resources, and staff, and thus may provide less personal care in their core services, accounting for the across AL differences. Furthermore, unlike their non-dual co-residents, duals have fewer financial resources to pay for such services themselves. While most states provide some level of financial assistance to dual beneficiaries residing in ALs, the level of such support varies considerably from state-to-state. (GAO, 2018)
These disparities are also clearly illustrated with regard to NH placement. Among non-duals, whites and Hispanics did not differ with regard to placement, but blacks faced higher odds, both within and across ALs. It should be noted that black residents were more likely than either whites or Hispanics to have mobility impairments, chronic kidney disease, stroke, and mental illness, conditions that require more personal and specialized care services (e.g., psychiatric care). ALs may not be able or willing to invest in such services at levels of care sufficient to facilitate these residents’ continued stay. It has been shown, for example, that ALs lack adequate ability to assess and provide appropriate care to support mental health needs of their residents.(Morgan, Perez, Frankowski, Nemec, & Bennett, 2016) Black non-dual AL residents may also have more limited resources, compared to their co-residents, to pay for such services on top of their room and board AL expenses (Wiltshire, Elder, Kiefe, & Allison, 2016), and thus may no longer have been able to afford to stay in AL.
At the same time, duals, regardless of race/ethnicity showed substantially greater risk of NH placement than the non-duals, both within and across ALs. At the individual-level, dual residents and/or their family members may have an earlier tipping point in deciding to transition to NH care as Medicaid does not cover AL cost but does pay for NH care. At the provider level, ALs serving duals may have fewer core services that delay or prevent institutional placement and or sufficient levels of staff to support residents’ care needs. At the state-level, although Medicaid HCBS are theoretically available to dual beneficiaries who live in ALs, in practical terms the level of support may be insufficient, in frequency and intensity, to prevent such transitions in care. Further, most states have sizable waitlists, which restrict access to HCBS services.
Disparities in access to AL, particularly for duals versus non-duals have been documented elsewhere (Fabius et al., 2021). We documented differences in health outcomes among AL residents by race and ethnicity, both within and across communities. Our findings suggest that these differences may be more likely due to socio-economic disparities between duals and non-duals than to race or ethnicity alone. ALs serving larger proportions of dual residents are typically lower cost communities, with fewer on-site resources, (Ball et al., 2004) and are located in poorer (higher proportion of dual elders), non-urban areas that are more likely to have fewer community-based resources, including access to personal care workers. In this regard, the disparities previously documented for NHs seem evident in ALs as well.
Furthermore, because ALs are licensed at the state level, (Carder, O’Keeffe, & O’Keeffe, 2015) there are significant state-by-state regulatory differences in domains such as staffing/training, admission/retention, medication management and others. (Temkin-Greener, Mao, et al., 2020) When health-related care needs of a resident exceed an AL community’s ability to provide care within existing regulations, residents will be discharged, often to NHs (Carder 2016). For residents who are dually eligible, this risk is exacerbated by low Medicaid payment rate as well as by the reimbursement type (e.g., flat or tiered rates), both of which are likely to differentially motivate AL providers to discharge residents to NHs. For example, under flat rates, states pay the same daily amount regardless of care needs.(Mollica, 2009) When care needs exceed the payment amount, ALs may be motivated to discharge duals to NHs. (Fabius et al., 2021) States have been working to rebalance Medicaid spending from NHs to HCBS. However, our findings raise some questions about the extent to which Medicaid support for these residents is actually meeting this objective. If dual residents’ increased risk of NH placement is the result of an AL community not being able to provide sufficient support and/or because Medicaid payments for long-term services and supports (LTSS) in this care setting are very limited, then efforts to rebalance long-term care in AL misses the mark.
Several limitations should be mentioned. While the administrative database we used is very comprehensive and national in scope, drawbacks include lack of information on functional status, cognitive status and family caregiver support, among others. Second, although we controlled for differences in AL-level factors with the fixed effects, we were unable to explain how the differences in AL resource and staffing influence the observed variation in health outcomes. Third, we only included AL residents enrolled in FFS Medicare, and thus we cannot generalize from our findings to those enrolled in the Medicare Advantage plans who may have richer access to services through their plans.
Conclusions and Implications
We found significant variations in the health outcomes of interest both within and across ALs. Our findings suggest some possible differences by race and ethnicity, but strongly indicate that disparities are more significant by dual eligibility status rather than race/ethnicity alone, and these disparities exist both among residents living in the same AL and across ALs. These findings provide some implications for providers, policy-makers, and researchers. For providers serving dual residents, it is important to consider they may have greater personal care needs, but less ability to pay for them. Committing to admit this population may require having a different mix of services such as access to staff with adequate behavioral health training. State policy-makers involved in rebalancing long-term care might more realistically assess the extent to which their state is committed to providing adequate LTSS to dual AL residents. Without sufficient commitment, delaying or preventing institutional placement of these residents may not be realistic. Furthermore, while states regulate AL, the stringency of such regulations varies so substantially that the federal government has called for greater oversight, particularly with regard to Medicaid residents. (GAO, 2018) An absence of minimum standards makes quality assessment and transparency in this care setting difficult, but effecting standards is challenging given variability in the AL population. However, this challenge presents an opportunity for researchers to explore appropriate quality measures and ways of testing and implementing reliable and useful metrics.
Supplementary Material
Funding Source:
This work was supported by the Agency for Healthcare Research and Quality grant number R01HS026893
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
REFERENCES
- Ball MM, Perkins MM, Whittington FJ, Connell BR, Hollingsworth C, King SV, Combs BL (2004). Managing decline in assisted living: The key to aging in place. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 59B, S202–S212. doi:59/4/S202 [pii] [DOI] [PubMed] [Google Scholar]
- Bartley M, Quigg S, Chandra A, & Takahashi P (2018). Health Outcomes From Assisted Living Facilities: A Cohort Study of a Primary Care Practice. JAMDA, 19(3), 1–11. doi: 10.1016/j.jamda.2017.12.079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartley MM, Quigg SM, Chandra A, & Takahashi PY (2018). Health Outcomes From Assisted Living Facilities: A Cohort Study of a Primary Care Practice. J Am Med Dir Assoc, 19(3). doi: 10.1016/j.jamda.2017.12.079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caffrey C, Harris-Kojetin L, Rome V, & Schwartz L (2018). Relationships Between Residential Care Community Characteristics and Overnight Hospital Stays and Readmissions: Results From the National Study of Long-Term Care Providers. Seniors Hous Care J, 26(1), 38–49. [PMC free article] [PubMed] [Google Scholar]
- Cai S, Mukamel DB, Veazie P, Katz P, Temkin-Greener H (2011). Hospitalizations in nursing homes: does payer source matter? Evidence from New York State. Medical care research and review : MCRR, 68, 559–578. doi: 10.1177/1077558711399581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carder P, O’Keeffe J, & O’Keeffe C (2015). Compendium of Residential Care and Assisted Living Regulations and Policy: 2015 Edition, Rockville, MD. [Google Scholar]
- Fabius C, Cornell P, Zhang W, & Thomas K (2021). State Medicaid Financing and Access to Large Assisted Living Settings for Medicare-Medicaid Dual-Eligibles. Medical Care Research and Review. doi: 10.1177/1077558720987666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabius CD, & Thomas KS (2019). Examining Black-White Disparities Among Medicare Beneficiaries in Assisted Living Settings in 2014. J Am Med Dir Assoc, 20(6), 703–709. doi: 10.1016/j.jamda.2018.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Growth of racial and ethnic minorities in us nursing homes driven by demographics and possible disparities in options, 30 1358–1365 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- GAO. (2018). Medicaid Assisted Living Services. Improved Federal Oversight of Beneficiary Health and Welfare is Needed. Washington, DC. Retrieved May 11, 2021; https://www.gao.gov/assets/gao-18-179.pdf [Google Scholar]
- Gimm GW, & Kitsantas P (2016). Falls, Depression, and Other Hospitalization Risk Factors for Adults in Residential Care Facilities. Int J Aging Hum Dev, 83(1), 44–62. doi: 10.1177/0091415016645347 [DOI] [PubMed] [Google Scholar]
- Grabowski DC, & McGuire TG (2009). Black-White Disparities in Care in Nursing Homes. Atl Econ J, 37(3), 299–314. doi: 10.1007/s11293-009-9185-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris-Kojetin L, Sengupta M, Lendon J, Rome V, Valverde R, & Caffrey C (2019). Long-Term Care Providers and services users in the United States: data from the National Study of Long-Term Care Providers, 2015–2016. Vital & health statistics. Series 3 (43), Analytical and epidemiological studies / [U.S. Dept. of Health and Human Services, Public Health Service, National Center for Health Statistics]. Retrieved May 11, 2021: https://www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf [PubMed] [Google Scholar]
- Hernandez M (2012). Disparities in Assisted Living: Does It Meet the HCBS Test? Journal of American Society on Aging, 36(1), 118–125. [Google Scholar]
- Hogan DB, Amuah JE, Strain LA, Wodchis WP, Soo A, Eliasziw M, Maxwell CJ (2014). High rates of hospital admission among older residents in assisted living facilities: opportunities for intervention and impact on acute care. Open Medicine, 8(1), e33–e45. [PMC free article] [PubMed] [Google Scholar]
- Horwitz L, Partovian C, Lin Z, Jerrin J, & Grady JN (2013). Planned Readmission Algorithm. Version 2.1. Retrieved May 11, 2021; https://hscrc.maryland.gov/documents/HSCRC_Initiatives/readmissions/Version-2-1-Readmission-Planned-CMS-Readmission-Algorithm-Report-03-14-2013.pdf
- Howard DL, Sloane PD, Zimmerman S, Eckert JK, Walsh JF, Buie VC, Koch GG (2002). Distribution of African Americans in residential care/assisted living and nursing homes: more evidence of racial disparity? Am J Public Health, 92(8), 1272–1277. doi: 10.2105/ajph.92.8.1272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua C, Zhang W, Cornell P, Rahman M, Dosa D, & Thomas K (2020). Characterizing Emergency Department Use in Assisted Living. JAMDA, July 6. doi: 10.1016/j.jamda.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrin O, Nyandege A, Grafova I, Dong X, & Lin H (2020). Validity of Race and Ethnicity Codes in the Medicare Administrative Data Compared with Gold-standard Self-reported Race Collected During Routine Home Health Care Visits. Medical Care, 58(1), e1–e8. doi: 10.1097/MLR.0000000000001216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbourne AM, Switzer G, Hyman K, Crawley-Matoka M, & Fine MJ (2007). Advancing Health Disparities Research Within the Health Care System: A Conceptual Framework. American Journal of Public Health, 96(12), 2113–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka RT, & Werner RM (2009). Disparities in long-term care: building equity into market-based reforms. Med Care Res Rev, 66(5), 491–521. doi: 10.1177/1077558709331813 [DOI] [PubMed] [Google Scholar]
- Li Y, Ye Z, Glance LG, & Temkin-Greener H (2014). Trends in family ratings of experience with care and racial disparities among Maryland nursing homes. Medical Care, 52, 641–648. doi: 10.1097/MLR.0000000000000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Harrington C, Mukamel DB, Cen X, Cai X, & Temkin-Greener H (2015). Nurse staffing hours at nursing homes with high concentrations of minority residents, 2001–11. Health Affairs, 34, 2129–2137. doi: 10.1377/hlthaff.2015.0422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Harrington C, Temkin-Greener H, You K, Cai X, Cen X, & Mukamel DBB (2015). Deficiencies In Care At Nursing Homes And Racial/Ethnic Disparities Across Homes Fell, 2006–11. Health Affairs, 34, 1139–1146. doi: 10.1377/hlthaff.2015.0094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollica RL (2009). State Medicaid Reimbursement Policies and Practices in Assisted Living. Prepared for the National Center for Assisted Living. Retrieved May 11, 2021: https://www.ahcancal.org/Assisted-Living/Policy/Documents/MedicaidAssistedLivingReport.pdf
- Mor V, Thomas KS, & Rahman M (2018). Defining and Measuring Nursing Home Placement. J Am Geriatr Soc, 66(10), 1866–1868. doi: 10.1111/jgs.15546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno JM, & Miller SC (2004). Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q, 82(2), 227–256. doi: 10.1111/j.0887-378X.2004.00309.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales J, & Robert S (2020). Black-White Disparities in Moves to Assisted Living and Nursing Homes Among Older Medicare Beneficiaries. Journals of Gerontology: Social Sciences, 75(9), 1972–1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan LA, Perez R, Frankowski AC, Nemec M, & Bennett CR (2016). Mental Illness in Assisted Living: Challenges for Quality of Life and Care. Journal of Housing for the Elderly, 30(2), 185–198. doi: 10.1080/02763893.2016.1162255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips C, Munoz Y, Sherman M, Rose M, Spector W, & Hawes C (2003). Effects of facility characteritics on departures from assisted living: Results from a national study. The Gerontologist, 43, 690–696. [DOI] [PubMed] [Google Scholar]
- Rathore SS, & Krumholz HM (2004). Differences, disparities, and biases: clarifying racial variations in health care use. Ann Intern Med, 141(8), 635–638. doi: 10.7326/0003-4819-141-8-200410190-00011 [DOI] [PubMed] [Google Scholar]
- RTI. (2016). MDS 3.0 Quality Measures: User’s Manual. Retrieved May 11, 2021: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS-30-QM-USERS-MANUAL-v121.pdf
- Temkin-Greener H, Guo W, Mao Y, Cai X, & Li Y (2020). Covid-19 Pandemic in Assisted Living Communities: Results from Seven States. JAGS, 68, 2727–2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temkin-Greener H, Mao Y, Ladwig S, Cai X, Zimmerman S, & Li Y (2020). Variability and Potential Determinants of Assisted Living State Regulatory Stringency. J Am Med Dir Assoc. doi: 10.1016/j.jamda.2020.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temkin-Greener H, Yan D, Wang S, & Cai S (2021). Racial Disparity in End-of-Life Hospitalizations among Nursing Home Residents with Dementia. JAGS, March 22 - early view. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas K, Dosa D, Gozalo P, Grabowski DC, Nazareno J, Makineni R, & Mor V (2018). A Methodology to Identify a Cohort of Medicare Beneficiaries in Large Assisted Living Facilities Using Administrative Data. Medical Care, 56(2):e10–e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States. Congress. House. Committee on Government Reform. Subcommittee on Criminal Justice Drug Policy and Human Resources. (2003). Racial disparities in health care : confronting unequal treatment : hearing before the Subcommittee on Criminal Justice, Drug Policy, and Human Resources of the Committee on Government Reform, House of Representatives, One Hundred Seventh Congress, second session, May 21, 2002. Washington: U.S. G.P.O. : For sale by the Supt. of Docs., U.S. G.P.O. Congressional Sales Office. [Google Scholar]
- Wiltshire JC, Elder K, Kiefe C, & Allison JJ (2016). Medical Debt and Related Financial Consequences Among Older African American and White Adults. Am J Public Health, 106(6), 1086–1091. doi: 10.2105/AJPH.2016.303137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman S, Cohen LW, Washington T, Ward K, & Giorgio P (2016). Evaluating Measures and Instruments for Quality Improvement in Assisted Living | Managed Health Care Connect. Annals of Long-Term Care: Clinical Care and Aging. [Google Scholar]
- Zimmerman S, Sloane PD, Eckert JK, Gruber-Baldini AL, Morgan LA, Hebel JR, Chen CK (2005). How good is assisted living? Findings and implications from an outcomes study. The journals of gerontology. Series B, Psychological sciences and social sciences, 60, S195–204. doi: 10.1093/GERONB/60.4.S195 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


